Abstract
Aims
Heart failure (HF) patients are taught to identify a rapid 5 lb body‐weight gain for early detection of cardiac decompensation. Few data support this common advice. The study aim was to determine whether a 5 lb weight gain in 1 week and signs and symptoms of HF increased risk for unplanned physician or emergency department (ED) visits or hospital admission in rural HF patients.
Methods and results
This was a secondary analysis of a randomized trial. Patients tracked body weight and HF symptoms using diaries. We included patients adherent to daily diaries >50% over 24 months (N = 119). Mean age was 69 ± 11 years; 77% (65) were male, and 67% completed diaries. A weight gain of 5 lb over 7 days was associated with a greater risk for ED visits but not hospital admission [hazard ratio (HR) 1.06, 95% confidence interval (CI) 1.04, 1.08; P < 0.0001 vs. HR 1.01, 95% CI 0.88, 1.16; P = 0.79]. Increased dyspnoea over 7 days was associated with a greater risk of ED visits and hospital admissions (HR 9.64, 95% CI 3.68, 25.22; P < 0.0001 vs. HR 5.89, 95% CI 1.73, 20.04; P = 0.01). Higher diary adherence was associated with older age, non‐sedentary behaviour, lower depression, and HF knowledge.
Conclusions
Heart failure patients are counselled to observe for body‐weight gain. Our data do not support that a 5 lb weight gain was associated with hospital admission. Dyspnoea was a better predictor of ED visits and hospital admissions. Daily tracking of dyspnoea symptoms may be an important adjunct to daily weight to prevent hospitalization.
Keywords: Heart failure, Body weight, Self‐care, Diary, Hospital admission
Introduction
Ubiquitous to the heart failure (HF) clinic visit is the advice that patients contact their providers if they experience a body‐weight gain of 5 lb in 1 week.1, 2 Guidelines for the Heart Failure Society of America and the European Society for Heart Failure both endorse patient education to improve outcomes for patients with HF.3, 4 However, content‐specific HF patient education regarding body weight, such as amount of weight gain, over what time period, and whether weight gain applies to all patients with HF has not been sufficiently investigated.
Additional patient education includes tracking of dyspnoea and oedema. Dyspnoea is a common subjective finding in patients with HF. However, few data describe whether increases in dyspnoea predict hospital admission or emergency department (ED) visits. Oedema is a variable clinical sign influenced by factors such as body position, nutritional status, and dietary sodium intake. It is also unclear if increases in oedema alone or in combination with other HF signs and symptoms signify concern for unplanned physician office visits, ED visits, or hospital admission. Further, no head‐to‐head analysis has been undertaken to determine whether body‐weight gain or HF symptoms, such as dyspnoea or oedema, are better at predicting outcomes such as unplanned physician office visits, ED visits, or hospital admission.
Heart failure‐specific guidelines extol the virtue of HF self‐management as an important strategy for improving outcomes.3, 4 One such method for self‐management can include the use of calendars or diaries. Daily diary use can provide an opportunity for providers and patients to mutually engage in body weight and HF symptom tracking over time.5 Electronic diaries and mobile phone app use have quickly grown over the past decade to support patient engagement in diary use for many chronic conditions.6, 7 HF patients are often instructed to routinely record daily body weight and HF symptoms such as dyspnoea, pillow use, and presence of oedema in their diaries.8, 9 However, few data demonstrate that tracking weight and HF symptoms improve long‐term patient outcomes.10
A challenging aspect of the HF patient clinic visit is to provide patients with evidence‐driven education to support their self‐management efforts. Numerous investigators have developed diary interventions that follow patient experiences such as food intake, mood, and medication use.5, 11 Data show that the use of diaries can improve self‐management skills and clinical outcomes, such as depression, as well as decrease the incidence of medication errors.5, 11
Investigators have determined that memory recall for HF patient body weight is unreliable.12 If diary data demonstrate that a rapid weight gain of 5 lb can predict poor outcomes, then patient education will be data driven and justify daily tracking of body weight. The aim of this secondary analysis of Rural Education to Improve Outcomes in Heart Failure (REMOTE‐HF) diary data was to determine whether a weight gain of 5 lb increased risk of poor clinical outcomes, namely, unplanned physician office visits, ED visits, and HF‐related hospital readmission in rural HF participants.8 We hypothesized that participants who had a body‐weight gain of 5 lb over 1 week would have a higher risk of unplanned office visits, ED visits, and HF‐related hospital readmissions. Our second aim was to determine which, if any, signs and symptoms of HF exacerbation, namely, dyspnoea and oedema, increased risk for poor clinical outcomes.
Methods
Design and sample
The parent study for our secondary analysis was the REMOTE‐HF randomized controlled clinical trial with three arms: control and two intervention arms (Fluid Watcher's LITE and PLUS).8 Both intervention groups included the same nurse‐delivered in‐person education session that focused on self‐care and the use of daily body weight and symptom diaries. Reinforcement of self‐care education for the LITE group included two follow‐up phone calls. The PLUS intervention group received reinforcement of self‐care education with bi‐weekly phone calls until the nurse considered the participant sufficiently understood, and could repeat back, the educational information (mean 5.3 + 3.6, range 1–19). The education intervention (LITE or PLUS groups) did not decrease the combined endpoint of cardiac death or hospitalization for HF. Cardiac mortality was significantly lower for participants in the LITE group over the 2 years of follow‐up.
Eligibility for the study included age ≥ 18 years, rural home address, hospitalized for HF within the past 6 months, English proficiency, and living independently (Figure 1 ). Participant recruitment took place in 12 clinics or hospitals in California, Kentucky, and Nevada. Institutional Review Board approval was obtained at the three major participating sites, and 602 participants were enrolled. Exclusion criteria included serious comorbidity (i.e. disease or illness predicted to cause death within 12 months), current participation in a HF disease management programme, or impaired cognition. Participants were randomized after completing baseline testing, and random selection techniques with 1:1:1 fixed allocation randomization were employed using blocks of five participants (SPSS 18.0, Chicago, IL, USA). Blinding to group assignment took place among all investigators, participants' physicians, and research assistants.
Figure 1.
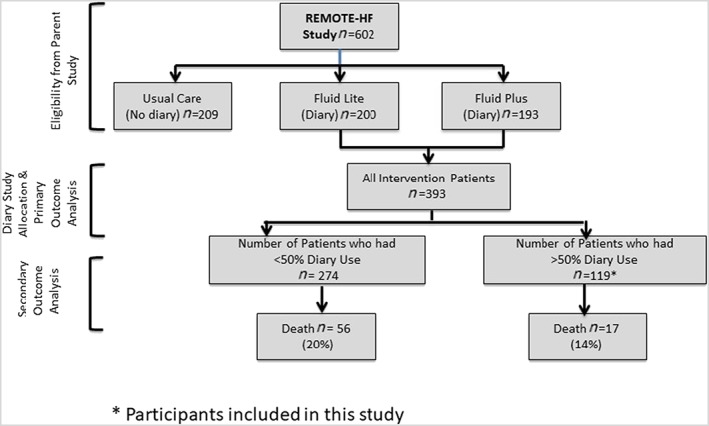
Study flow diagram.
Procedures
All participants in the two intervention arms were instructed to complete daily diaries for 24 months (The control arm did not complete diaries.). The dairies were in calendar format and had prompts to add data on daily body weight and HF symptoms such as dyspnoea, number of pillows used for sleep, and presence of oedema including the date and time when symptoms began. All intervention participants received digital scales with large numbers for improved visibility. If patients had HF‐related health concerns, participants recorded what type of action was required such as a physician's office phone call, ED visit, or other. If participants gained 5 lb in 7 days, they were instructed to call their physician's office using a provided script. Participants personally delivered diaries at follow‐up visits or returned diaries monthly via the mail in self‐addressed stamped envelopes during the 2 year study period. All enrolled participants received large‐print questionnaires and diaries.
Study demographic data were collected face to face via a standardized form and with structured questionnaires. Depression was measured with the 9‐item Patient Health Questionnaire depression scale.13 HF knowledge was assessed with a 20‐item HF Knowledge Scale.14 The Charlson comorbidity index was used to assess the presence of participant co‐morbidities.15 At baseline, the 36‐item Short Test of Functional Health Literacy in Adults measured health literacy using reading comprehension.16
Heart failure‐related unplanned physician office visits, hospital admissions, and cardiac and non‐cardiac death were assessed quarterly using the electronic medical record, physician contact, or by questioning participants. The cause of death was determined by medical record review using a blinded adjudication process, family interview, and physician contact for out‐of‐hospital deaths.
Statistical analysis
Statistical analysis was performed using SAS (version 9.4, SAS Institute Inc., Cary, NC, USA). Characteristics of the sample and differences between participants who used diaries at least 50% of the time vs. less than 50% of the time were analysed using χ2 and Mann–Whitney U‐tests. We employed Cox proportional hazards models to determine whether a body‐weight gain of 5 lb increased risk of clinical outcomes (unplanned office visits, ED visits, or hospital readmission) in HF patients. To solve the potential problem that low adherence to diary use was because of death, we used Cox models with change in body weight and dyspnoea treated as time‐varying covariates (but included participants who used diaries until their time of death). All two‐sided significance levels used were established a priori at 0.05. Cox proportional hazards models with time‐varying covariates were also utilized for the secondary aim, to determine if dyspnoea and oedema increased risk for office visits, ED visits, and hospital admission.
Ethics
The ethical regulations of the study were consistent with the principles outlined in the Declaration of Helsinki. Institutional Review Board approval for ethics was obtained at all three participating institutions in California, Kentucky, and Nevada.17 Written informed consent to participate in the study was obtained from all participants.
Results
Participant demographic and clinical characteristics
We examined risk of events (unplanned office visits, ED visits, and hospital admission) among 393 participants who participated in the intervention parent study and divided the group by those who completed daily body weight and symptom dairies at least 50% of the time (n = 119). We were unable to examine risk of death as the rate of death was too low to provide adequate hazard risk estimates. The parent study participants' New York Heart Association (NYHA) functional classes were the following: NYHA I = 64 (10.6%), II = 325 (54.1%), III = 187 (31.1%), and IV = 25 (4.2%). When combined, 212 (35.2%) of parent study participants had NYHA functional class III/IV, similar to the 103 (38%) current study participants' III/VI functional class.
The mean age of the participants was 69 ± 11 years, 65% were male, and 92% were White (Table 1). Twenty‐one per cent were employed, and 17% had not completed high school. Slightly less than one‐third (28%) had NYHA functional class III or IV. We compared the participants who completed vs. did not complete daily diaries and found that older age, non‐sedentary behaviour, lower depression scores, and lower HF knowledge scores were more often associated with diary use at least 50% of the time.
Table 1.
Baseline characteristics of diary adherence
| Clinical parameters (total = 393) | Diary users < 50% of study days (n = 274) | Diary users ≥ 50% of study days (n = 119) | P value |
|---|---|---|---|
| Age, yearsa | 65 ± 14 | 69 ± 11 | 0.004 |
| Male | 150 (55) | 77 (65) | 0.06 |
| White | 243 (89) | 109 (92) | 0.39 |
| Not completed high school education | 50 (18) | 17 (14) | 0.24 |
| Employed | 38 (14) | 25 (21) | 0.07 |
| Married | 153 (56) | 68 (57) | 0.81 |
| BMI > 25 (kg/m2) | 209 (76) | 85 (71) | 0.25 |
| Sedentary | 144 (53) | 38 (32) | <0.001 |
| NYHA functional class III/IV | 103 (38) | 33 (28) | 0.06 |
| CABG | 87 (32) | 37 (31) | 0.90 |
| Current smoker | 37 (14) | 12 (10) | 0.35 |
| Hypercholesterolaemia | 183 (67) | 77 (65) | 0.69 |
| Arterial hypertension | 215 (79) | 93 (78) | 0.94 |
| Stroke | 36 (13) | 18 (15) | 0.60 |
| Anaemia | 97 (35) | 52 (44) | 0.10 |
| BNP (pg/mL) | 387 ± 544 (268) | 478 ± 1450 (108) | 0.85 |
| Creatinine (mg/dL) | 1.18 ± 0.46 (273) | 1.34 ± 0.94 | 0.37 |
| Charlson comorbidity index score | 3.28 ± 1.76 (274) | 3.12 ± 1.63 | 0.49 |
| PHQ‐9 depression score | 8.32 ± 6.66 (274) | 4.49 ± 4.55 | <0.0001 |
| HF knowledge score | 14 ± 2.43 (274) | 13.3 ± 2.92 | 0.02 |
| Cardiac death | 27 (9.9) | 11 (9) | 0.85 |
| Non‐cardiac death | 29 (10.6) | 6 (5) | 0.07 |
| Hospital readmission | 79 (28.8) | 37 (31) | 0.65 |
BMI, body mass index; BNP, brain natriuretic peptide; CABG, coronary artery bypass grafting; HF, heart failure; NYHA, New York Heart Association; PHQ, Patient Health Questionnaire.
Bold indicates significant findings.
P ≤ 0.05 is significant.
Data are presented as mean ± standard deviation, n (%).
Body weight and symptoms in relation to unplanned office visits
A body‐weight gain of 5 lb over 7 days demonstrated lower risk for physician office visits [hazard ratio (HR) 0.86, 95% confidence interval (CI) 0.75, 0.98; P < 0.03], whereas an increase in dyspnoea over 14 days (HR 5.05, 95% CI 1.12, 22.71; P < 0.03), but not over 7 days (HR 2.51, 95% CI 0.31, 19.7; P = 0.39), was associated with a greater risk for physician office visits (Table 2).
Table 2.
Risk of events: body weight and heart failure symptoms (n = 119)
| Event outcome | Predictor variable | HR | Lower CI (95%) | Upper CI (95%) | P value |
|---|---|---|---|---|---|
| Unplanned/unscheduled physician visit | Weight gain of 5 lb in 14 days (n = 16) | 1.95 | 0.81 | 1.12 | 0.58 |
| Weight gain of 5 lb in 7 days (n = 16) | 0.86 | 0.75 | 0.98 | 0.03 | |
| Dyspnoea increase in 14 days (n = 17) | 5.05 | 1.12 | 22.71 | 0.03 | |
| Dyspnoea increase in 7 days (n = 16) | 2.51 | 0.31 | 19.7 | 0.39 | |
| Peripheral oedema (n = 19) | 1.6 | 0.44 | 5.9 | 0.46 | |
| ED visit | Weight gain of 5 lb in 14 days (n = 23) | 0.97 | 0.84 | 1.12 | 0.69 |
| Weight gain of 5 lb in 7 days (n = 24) | 1.06 | 1.04 | 1.08 | <0.0001 | |
| Dyspnoea increase in 14 days (n = 25) | 9.87 | 2.76 | 35.22 | 0.0004 | |
| Dyspnoea increase in 7 days (n = 25) | 9.64 | 3.68 | 25.22 | <0.0001 | |
| Peripheral oedema (n = 31) | 2.62 | 1.14 | 6.00 | 0.02 | |
| Hospital admission | Weight gain of 5 lb in 14 days (n = 24) | 1.00 | 0.92 | 1.09 | 0.89 |
| Weight gain of 5 lb in 7 days (n = 24) | 1.01 | 0.88 | 1.16 | 0.79 | |
| Dyspnoea increase in 7 days (n = 25) | 5.89 | 1.73 | 20.04 | 0.004 | |
| Dyspnoea increase in 14 days (n = 26) | 3.67 | 1.15 | 11.70 | 0.03 | |
| Peripheral oedema (n = 30) | 0.89 | 0.27 | 2.92 | 0.85 |
CI, 95% confidence intervals; ED, emergency department; HR, hazard ratio.
Bold indicates significant findings.
P ≤ 0.05 is significant.
Body weight and symptoms in relation to emergency department visits
A weight gain of 5 lb over 7 days was associated with greater risk for ED visits (HR 1.06, 95% CI 1.04, 1.08; P < 0.0001), but no greater risk was associated with weight gain of 5 lb over 14 days (HR 0.97, 95% CI 0.84, 1.12; P = 0.69). An increase in dyspnoea at both 7 and 14 days (HR 9.64, 95% CI 3.68, 25.22; P < 0.0001; HR 9.87, 95% CI 2.76, 35.22; P < 0.0004; respectively) was associated with a greater number of ED visits. Peripheral oedema was also significantly associated with greater risk for ED visits (HR 2.62, 95% CI 1.14, 6.00; P < 0.02).
Body weight and symptoms in relation to hospital admission
An increase in body weight by 5 lb over 7 or 14 days was not associated with greater risk of hospital admission (HR 1.01, 95% CI 0.88, 1.16; P = 0.79; HR 1.00, 95% CI 0.92, 1.09; P = 0.89, respectively). However, an increase in dyspnoea over both 7 and 14 days (HR 5.89, 95% CI 1.73, 20.04; P < 0.004; HR 3.67, 95% CI 1.15, 11.70; P < 0.03; respectively) was associated with a greater number of hospital admissions (Table 2). The presence of peripheral oedema was not significantly associated with greater risk for hospital admission (HR 0.89, 95% CI 0.27, 2.92; P = 0.85).
Discussion
These data do not support the common wisdom that a rapid 5 lb body‐weight gain is associated with increased risk of hospital readmission. Nonetheless, a rapid weight gain was associated with increased risk of ED visits. We speculate that there was a lower risk of office visits in association with body‐weight gain because patients had likely presented to the ED instead of calling their provider. Novel to this study is a side‐by‐side comparison of body‐weight gain and HF symptoms in relation to HF outcomes. Surprisingly, dyspnoea, a subjective symptom with high prevalence in HF participants, better predicted ED visits and hospital admission in comparison with a 5 lb weight gain. Unique to this study is that diary use spanned over a lengthy 24 month period. We found that higher diary use was associated with older age, non‐sedentary behaviour, less depression, and lower HF knowledge.
Body‐weight gain
The increase in body weight is used by disease management programmes as a marker of HF decompensation.2 Our data are in contrast from data obtained from a nested case–control study that demonstrated 134 matched case patients experienced body‐weight gain 1 week prior to hospitalization.18 However, these retrospective data do not determine that weight gain was the cause of hospital admission. HF symptoms such as dyspnoea or ED visit rates prior to hospital admission were not examined, making a comparison with our data not possible. In another study, investigators hypothesized that daily electronic transmission of body weight would reduce cardiac hospitalization for HF patients.19 Patients in the intervention group were given an electronic scale, and body weight was automatically transmitted and monitored via the HF clinic. Electronic body‐weight monitoring did not decrease hospitalization rates.
Data demonstrate that not all HF hospital admissions are associated with patients' weight gain.20 In one study, investigators compared a simple rule of thumb algorithm (i.e. 3 lb weight gain in 1 day and 5 lb weight gain in 3 days) to a moving average convergence divergence algorithm to predict episodes of HF exacerbation and hospital admission.20 Although body‐weight gain occurred within the 14 days prior to hospital admission, the rule of thumb algorithm had a much higher false alert rate. The investigators found that the rule of thumb algorithm did not have great value, as many episodes of worsening HF were not associated with an increase of body weight.
Investigators also studied the optimal method to evaluate body‐weight monitoring adherence and found that self‐reported recall of weight monitoring adherence was not associated with fewer HF hospitalizations.12 However, hand‐diary recorded adherence of ≥80% was associated with fewer HF‐related hospitalizations. HF patients tested a home‐based tablet computer system designed to improve self‐care behaviours such as daily weighing.21 At hospital discharge, patients were instructed to record daily body weights and received lifestyle advice via tablet computer at home. Changes in patient body weight were visible on the tablet over time and resulted in improved self‐care and decreased hospital days. It is unclear whether the patient action of weighing and hand recording their own body weight in a diary or tablet can trigger more attention to self‐care, thereby decreasing HF hospitalization rates. There are qualitative data that suggest purposeful reflection may be necessary for the development of self‐care skills.22
Because most HF exacerbations result in hospital admission,23 our data suggest that the patients in our study who presented to the ED with a 5 lb body‐weight gain did not have an HF exacerbation or were readily treated for HF and discharged. An increase in body weight by 5 lb over 7 days demonstrated a lower risk for office visits. We speculate that when HF patients experienced a weight gain, they presented to the ED rather than to their local provider for care. No data provide guidance on whether a 5 lb weight gain can have the same effect on patients with different body mass index. For example, does a 5 lb weight gain cause exacerbation of HF, in a person who weighs 125 vs. 250 lb? Further studies are needed to determine the effect of weight gain on the clinical course of HF patients with various body sizes.
Heart failure signs and symptoms
Our data show that dyspnoea rather than body‐weight gain was a better predictor of unplanned office, ED visits, and hospital admissions. Few investigators have examined HF symptoms as predictors of hospital admissions, but data from the EVEREST trial describe dyspnoea during and after hospitalization.24 Daily assessment of dyspnoea was rated by both physicians and patients to guide timing of discharge. Physician‐rated dyspnoea symptoms differed from patient‐reported dyspnoea, with decreases in dyspnoea during the hospital treatment much more dramatic as assessed by physicians than patients. In‐hospital dyspnoea ratings by both patients and physicians were not found to be independently associated with HF readmission. However, these data do not examine dyspnoea rating before a hospitalization event. Investigators did find in a group of hospitalized HF patients that dyspnoea did predict short‐term cardiac event‐free survival.25 Another group of investigators found that survival rates were improved with diary use that included daily body‐weight monitoring, but hospital readmission rates were not reported.26 Our data show that increases in dyspnoea for 14 days did confer an increased risk for an office visit. This suggests that patients contacted their provider as they perceived a worsening of symptoms.
The mechanism of dyspnoea in HF exacerbations is related to fluid retention, which is typically accompanied by an increase of body weight. One explanation for our data that showed body‐weight gain was not associated with hospital admission but dyspnoea symptoms were is that dyspnoea may precede body‐weight gain and/or be a more sensitive predictor of HF exacerbation than weight gain.
Limitations
Our study has important limitations to consider. The sample size is small and may lack the power to detect outcomes. However, it is the largest study to include daily diary data over a 2 year time period from rural HF patients. Patterns of care in rural areas may differ from those in other geographic areas; therefore, external generalizability may be limited. Future studies that include a comparison of rural, suburban, and urban HF patients will provide more information. Participants who used the diaries were non‐randomized; thus, we cannot determine causality. Not all participants used the dairies on a daily basis. We did not include dietary, medication, or exercise habits of HF patients, making the influence of dietary intake, exercise, or medication adjustment unknown. We did not include baseline pulmonary disease co‐morbidities, making the influence of alternative causes of acute dyspnoea unknown. Diary use may have been influenced by participants who were more healthy overall.
Conclusions
Despite the common wisdom that a 5 lb weight gain is associated with hospital admission, our data do not support this. A 5 lb weight gain was associated with increased risk of ED visits, but these ED visits may not represent HF exacerbations. Dyspnoea was a better predictor of increased office visits, ED visits, and hospital admissions. Guidelines support self‐management as a strategy to improve HF outcomes. The use of diaries is one cost‐effective method to track clinical symptoms and body weight of HF patients. However, dyspnoea may be the more important data to track to prevent HF hospitalization. A prospective randomized controlled trial is needed to definitively determine if a 5 lb body‐weight gain in 7 days increases risk for hospital admission, because this recommendation is a central educational topic in HF patients.
Conflict of interest
None declared.
Funding
K.D., D.M., and M.P. were funded by the NHLBI and NINR as investigators for the REMOTE‐HF trial (5R01HL83176‐5). L.G.P. was funded by the National Institutes of Health (1KL2TR001870‐01). R.A.C. was funded by the Australian Heart Foundation Future Leader Fellowship (2015 FLF 100847). None of the authors were funded for analysis and the writing of this manuscript.
Howie‐Esquivel, J. , Dracup, K. , Whooley, M. A. , McCulloch, C. , Jin, C. , Moser, D. K. , Clark, R. A. , Pelter, M. M. , Biddle, M. , and Park, L. G. (2019) Rapid 5 lb weight gain is not associated with readmission in patients with heart failure. ESC Heart Failure, 6: 131–137. 10.1002/ehf2.12370.
Institutions where work was performed: University of California, San Francisco, University of California, Davis, University of Kentucky, and University of Nevada, Reno.
Clinical trial registration: www.ClinicalTrials.gov. Identifier: NCT00415545.
References
- 1. Kisiangani T. IHI: Good Heart Failure Care Follow Patients Home. http://www.ihi.org/resources/Pages/ImprovementStories/GoodHeartFailureCareFollowsPatientsHome.aspx. (27 February 2015). [Google Scholar]
- 2. Tuso P, Huynh DN, Garofalo L, Lindsay G, Watson HL, Lenaburg DL, Florence B, Jones J, Harvey P, Kanter MH. The readmission reduction program of Kaiser Permanente Southern California—knowledge transfer and performance improvement. Perm J 2013; 17: 58–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González‐Juanatey JR, Harjola V‐P, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, Authors/Task Force Members . 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016; 37: 2129–2200. [DOI] [PubMed] [Google Scholar]
- 4. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Colvin MM, Drazner MH, Filippatos GS, Fonarow GC, Givertz MM, Hollenberg SM, Lindenfeld J, Masoudi FA, McBride PE, Peterson PN, Stevenson LW, Westlake C. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation 2017; 136: e137–e161. [DOI] [PubMed] [Google Scholar]
- 5. Richardson A. The health diary: an examination of its use as a data collection method. J Adv Nurs 1994; 19: 782–791. [DOI] [PubMed] [Google Scholar]
- 6. Park LG, Beatty A, Stafford Z, Whooley MA. Mobile phone interventions for the secondary prevention of cardiovascular disease. Prog Cardiovasc Dis 2016; 58: 639–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Köberich S. Fostering self‐care behaviours through symptom diary use? An exploratory, cross‐sectional study about the use of and attitude towards a symptom diary of patients with heart failure. J Res Nurs 2016; 21: 530–541. [Google Scholar]
- 8. Dracup K, Moser DK, Pelter MM, Nesbitt TS, Southard J, Paul SM, Robinson S, Cooper LS. Randomized, controlled trial to improve self‐care in patients with heart failure living in rural areas. Circulation 2014; 130: 256–264. [DOI] [PubMed] [Google Scholar]
- 9. White MM, Howie‐Esquivel J, Caldwell MA. Improving heart failure symptom recognition: a diary analysis. J Cardiovasc Nurs 2010; 25: 7–12. [DOI] [PubMed] [Google Scholar]
- 10. Clark AM, Spaling M, Harkness K, Spiers J, Strachan PH, Thompson DR, Currie K. Determinants of effective heart failure self‐care: a systematic review of patients' and caregivers' perceptions. Heart 2014; 100: 716–721. [DOI] [PubMed] [Google Scholar]
- 11. Lorig KR, Sobel DS, Stewart AL, Brown BW, Bandura A, Ritter P, Gonzalez VM, Laurent DD, Holman HR. Evidence suggesting that a chronic disease self‐management program can improve health status while reducing hospitalization: a randomized trial. Med Care 1999; 37: 5–14. [DOI] [PubMed] [Google Scholar]
- 12. Jones CD, Holmes GM, DeWalt DA, Erman B, Wu J‐R, Cene CW, Baker DW, Schillinger D, Ruo B, Bibbins‐Domingo K, Macabasco‐O'Connell A, Hawk V, Broucksou K, Pignone M. Self‐reported recall and daily diary‐recorded measures of weight monitoring adherence: associations with heart failure‐related hospitalization. BMC Cardiovasc Disord 2014; 14: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kroenke K, Spitzer RL, Williams JB. The PHQ‐9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16: 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Simons‐Morton DG, Goff DC, Osganian S, Goldberg RJ, Raczynski JM, Finnegan JR, Zapka J, Eisenberg MS, Proschan MA, Feldman HA, Hedges JR, Luepker RV. Rapid early action for coronary treatment: rationale, design, and baseline characteristics. REACT Research Group Acad Emerg Med 1998; 5: 726–738. [DOI] [PubMed] [Google Scholar]
- 15. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–383. [DOI] [PubMed] [Google Scholar]
- 16. Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns 1999; 38: 33–42. [DOI] [PubMed] [Google Scholar]
- 17. Rickham PP. Human experimentation. Code of ethics of the World Medical Association. Declaration of Helsinki. Br Med J 1964; 18: 177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chaudhry SI, Wang Y, Concato J, Gill TM, Krumholz HM. Patterns of weight change preceding hospitalization for heart failure. Circulation 2007; 116: 1549–1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lyngå P, Persson H, Hägg‐Martinell A, Hägglund E, Hagerman I, Langius‐Eklöf A, Rosenqvist M. Weight monitoring in patients with severe heart failure (WISH). A randomized controlled trial. Eur J Heart Fail 2012; 14: 438–444. [DOI] [PubMed] [Google Scholar]
- 20. Zhang J, Goode KM, TEN‐HMS Investigators . Predicting hospitalization due to worsening heart failure using daily weight measurement: analysis of the Trans‐European Network‐Home‐Care Management System (TEN‐HMS) study. Eur J Heart Fail 2009; 11: 420–427. [DOI] [PubMed] [Google Scholar]
- 21. Hägglund E, Lyngå P, Frie F, Ullman B, Persson H, Melin M, Hagerman I. Patient‐centred home‐based management of heart failure. Findings from a randomised clinical trial evaluating a tablet computer for self‐care, quality of life and effects on knowledge. Scand Cardiovasc J 2015; 49: 193–199. [DOI] [PubMed] [Google Scholar]
- 22. Sethares KA, Asselin ME. The effect of guided reflection on heart failure self‐care maintenance and management: a mixed methods study. Heart Lung 2017; 46: 192–198. [DOI] [PubMed] [Google Scholar]
- 23. Collins SP, Pang PS, Fonarow GC, Yancy CW, Bonow RO, Gheorghiade M. Is hospital admission for heart failure really necessary?: The Role of the Emergency Department and Observation Unit in Preventing Hospitalization and Rehospitalization. JACC 2013; 61: 121–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ambrosy AP, Khan H, Udelson JE, Mentz RJ, Chioncel O, Greene SJ, Vaduganathan M, Subacuis HP, Konstam MA, Swedberg K, Zannad F, Maggioni AP, Gheorghiade M, Butler J. Changes in dyspnea status during hospitalization and post‐discharge health‐related quality of life in patients hospitalized for heart failure: findings from the EVEREST trial. Circ Heart Fail 2016; 9: e002458. [DOI] [PubMed] [Google Scholar]
- 25. Zaharias E, Cataldo J, Mackin L, Howie‐Esquivel J. Simple measures of function and symptoms in hospitalized heart failure patients predict short‐term cardiac event‐free survival. Nurs Res Pract 2014; 2014: 815984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lee KS, Lennie TA, Warden S, Jacobs‐Lawson JM, Moser DK. A comprehensive symptom diary intervention to improve outcomes in patients with HF: a pilot study. J Card Fail 2013; 19: 647–654. [DOI] [PubMed] [Google Scholar]


