Abstract
Background: To determine the validity of the Quick Sepsis-Related Organ Failure Assessment (qSOFA) in the prediction of outcome (in-hospital and 1-month mortality, intensive care unit (ICU) admission, and hospital and ICU length of stay) in adult patients with or without suspected infections where qSOFA was calculated and reported; Methods: Cochrane Central of Controlled trials, EMBASE, BIOSIS, OVID MEDLINE, OVID Nursing Database, and the Joanna Briggs Institute EBP Database were the main databases searched. All studies published until 12 April 2018 were considered. All studies except case series, case reports, and conference abstracts were considered. Studies that included patients with neutropenic fever exclusively were excluded. Results: The median AUROC for in-hospital mortality (27 studies with 380,920 patients) was 0.68 (a range of 0.55 to 0.82). A meta-analysis of 377,623 subjects showed a polled AUROC of 0.68 (0.65 to 0.71); however, it also confirmed high heterogeneity among studies (I2 = 98.8%, 95%CI 98.6 to 99.0). The median sensitivity and specificity for in-hospital mortality (24 studies with 118,051 patients) was 0.52 (range 0.16 to 0.98) and 0.81 (0.19 to 0.97), respectively. Median positive and negative predictive values were 0.2 (range 0.07 to 0.38) and 0.94 (0.85 to 0.99), respectively.
Keywords: sepsis, qSOFA, prognosis
1. Introduction
Sepsis has been the focus of intensive research efforts over many years, with good reason [1]. Mortality is high (as high as 28.6% [2]) and treatment is expensive ($18,600 USD per hospital stay in the US [3]).
The first international consensus definition of sepsis dates from 1992 [4,5]. It was not substantially updated until 2016 [6] when the task group for the third international consensus definition for sepsis and septic shock redefined sepsis as a “life-threatening organ dysfunction caused by a dysregulated host response to infection” [6] Alongside with this updated definition, the task group also proposed a novel score to identify patients at risk for sepsis: the Quick Sepsis-Related Organ Failure Assessment (qSOFA). However, like many changes, qSOFA has been controversial [7,8,9].
qSOFA was based on the Sepsis-related Organ Failure Assessment (SOFA) score. The SOFA score was originally developed as a predictor for intensive care unit (ICU) mortality [10], and it consists of both vital signs (respiratory rate and blood pressure) and laboratory assessments (liver function tests, urea and creatinine) [6]. qSOFA was intended for use in patients with suspected infection outside of the ICU setting, and included altered mentation, tachypnea, and hypotension [6].
Prior systematic reviews on the topic tend to focus on patients that have already been identified as having suspected infections, which is how the test was originally designed. However, in an Emergency department (ED), the cause for attendance is not always clear, and a diagnosis of infection is often made much later. We there believe that qSOFA should be applied earlier in the treatment process, before a specific condition is considered. This systematic review aims to determine the validity of qSOFA in the prediction of mortality in all patients, with or without a suspected infection.
Objectives: This systematic review examines the validity of qSOFA in predicting in-hospital mortality and 28/30-days mortality, and determines if qSOFA is able to predict ICU admission, length of ICU stay, length of hospital stay, and diagnosis of sepsis, in patients not already identified with a specific condition.
2. Methodology
We designed our systematic review using the framework set out in the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols (PRISMA-P) 2015 statement developed with elements adapted from the Cochrane Handbook for Systematic Reviews of Interventions [11,12]. The review was registered with PROSPERO (ID CRD42017063976).
2.1. Eligibility Criteria
Types of studies: We considered studies of all designs, except for case series and case reports, i.e., all retrospective and prospective, and all observational and interventional studies. Studies only reported as abstracts were excluded.
Types of participants: All studies with adult patients with or without suspected or confirmed infection, sepsis, severe sepsis, and septic shock were considered. Studies that only included patients with neutropenic fever were excluded from this systematic review, due to the specific nature of this patient group.
Interventions: We considered all studies that reported qSOFA.
Setting: We found studies including patients presenting acutely to Emergency departments and pre-hospital emergency care providers, critical care units (intensive care units and high dependency units), and general wards.
Types of outcome: In-hospital mortality, 1-month mortality, ICU admission, diagnosis of sepsis, length of ICU stay, and length of hospital stay.
Timing: Both retrospective and prospective studies were considered.
Period of review: All studies published until 12 April 2018 were included.
Language: We included articles in languages that the author group could understand (English, Chinese, Danish). Papers with titles that seemed relevant but in languages that were non-comprehensible to the authors are listed in Appendix A (non-English studies).
2.2. Information Sources
Our literature search strategy was developed by using Medical Subject Headings (MeSH) and text words related to qSOFA. We searched the Cochrane Central Register of Controlled Trials (November 2016), EMBASE (1910 to Present), BIOSIS (2001 to 2012), OVID MEDLINE® Epub Ahead of Print, In-Process & Other Non-Indexed Citations and OVID MEDLINE® (1946 to Present with Daily Update), OVID Nursing Database (1946 to January Week 1 2017), and the Joanna Briggs Institute EBP Database, using the OVID interface. The WHO International Clinical Trial Registry Platform, Web of Science, Scopus, and ClinicalTrials.gov were searched independently.
2.3. Search Strategy
We have used the following terms to search ((((qSOFA) OR quick SOFA) OR quick sequential organ failure assessment) OR quick sepsis-related organ failure assessment) AND mortality.
Details may be found in Appendix B, Appendix C, Appendix D, Appendix E and Appendix F (search strategies).
2.4. Study Selection
Duplicates were removed, and records were identified and screened by LL and RL. After this, studies with no results available and studies in languages that our group could not read were also excluded. The remaining studies were discussed in a consensus meeting by CAG, MB, KH, LL, and RL. The results were compared at each stage, and discrepancies were discussed. If no consensus was met, CAG acted as the final adjudicator for the decision of whether a study should be included.
2.5. Data
Data was collected independently and was cross-checked by at least three reviewers. The data items extracted included study type (retrospective/prospective), sample size, patient characteristics such as age and gender, recruitment period, patient setting (location of recruitment), patient group (infection/‘all-comers’), mentation assessment, and the timing of qSOFA.
2.6. Outcomes
Our primary outcome was in-hospital mortality. Secondary outcomes were 1-month mortality, ICU admission, sepsis diagnosis, ICU length-of-stay, and hospital length-of-stay. We performed sub-group analyses for studies that only included patients with infection versus all-comers, the location of recruitment, altered mental status, and timing of qSOFA.
Graphs were generated using MedCalc Statistical Software version 18.11 [13].
2.7. Risk of Bias in Individual Studies
All studies included were assessed by using an adapted version of the Quality in Prognosis Studies instrument [14]. Six potential bias domains were explored: selection bias, bias in definition and measurement, outcome measurement bias, handling of missing data, confounding, and bias of statistics or the presentation of result. These six domains were be graded as “high risk (of bias)”, “low risk (of bias)”, or “unclear”.
Summary measures: The principal summary measure was the area under the receiver operator characteristic (AUROC) curve for the prediction of mortality. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were also collected. All measures were also reported for Intensive Care Units (ICU) admission and sepsis diagnosis.
3. Results
3.1. Study Selection
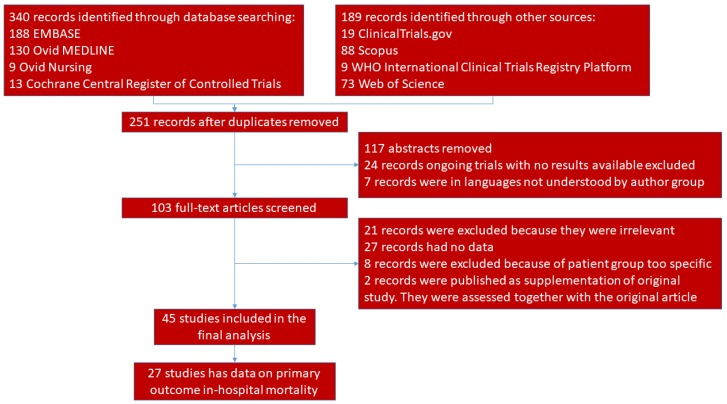
The database search identified 529 records. After duplicates were removed, 251 records were identified and screened by LL and RL. After 117 abstracts were excluded, 24 ongoing trials with no results available, and seven records in languages that our group could not read were also excluded (all seven of these papers appeared to be reviews or articles that contained no original data). The remaining 103 were discussed in a consensus meeting by CAG, MB, KH, LL, and RL. We included 45 papers in the final analysis [15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59] (Figure 1). Excluded studies and the reasons for their exclusion are listed in Appendix G (Table A1).
Figure 1.
Study Flow.
3.2. Study and Sample Characteristics
Of the 45 studies, 27 were retrospective cohorts, 13 had data prospectively collected but retrospectively analyzed, and five were prospective cohorts. The studies recruited a total of 413,634 patients from Europe, North America, Asia, and Australasia, with a median age ranging from 49 to 80 years. Seven studies recruited patients from all settings, 24 studies recruited only ED patients, eight from ICU only, one from all non-ICU settings, one from general wards, one from a pre-hospital setting, and 13 included patients from more than one setting (e.g., ward, ICU, or ED). The recruitment periods ranged from one day (cross-sectional study) to 20 years (1996–2015). Sample sizes ranged from 58 to 184,875. Some 27 studies reported data on in-hospital mortality and 16 reported data on 1-month mortality (Table 1).
Table 1.
Characteristics of the studies included in the systematic review of qSOFA for predicting prognosis.
| Study | Median Age (IQR) Mean Age ± SD |
Location | Male (%) | Sample Size | Study Type | Recruitment Period |
|---|---|---|---|---|---|---|
| Amland et al. [15] | 65 (51–76) | US | 48 | 5992 | Retrospective | January 2016–March 2016 |
| April et al. [16] | 72 (60–79) | Texas, US | 58.9 | 214 | Retrospective | August 2012–February 2015 |
| Askim et al. [17] | 62 (41–78) | Norway | 53 | 1535 | PCDRC | January 2012–December 2012 |
| Boulos et al. [18] | 68.5 ± 17.4 | Monash, Australia | 52 | 646 | Retrospective | January 2015–December 2015 |
| Brabrand et al. [19] | 65 (50–77) | Denmark | 49.2 | 4931 | Retrospective | October 2008–May 2010 |
| Burnham et al. [20] | 61.1 (51.6–69.8) | Missouri, USA | 52 | 510 | Retrospective | June 2009–December 2013 |
| Chen et al. [21] | 73 (62–79) | Beijing, China | 59 | 1641 | PCDRC | January 2012–May 2014 |
| Churpek et al. [22] | 58 ± 18 | Chicago, US | 47 | 30,677 | Retrospective | November 2008–January 2016 |
| de Groot et al. [23] | 61.1 ± 17 | Holland | 57.7 | 2280 | PCDRC | April 2011–February 2016 |
| Donnelly et al. [24] | 68 (61–75) | USA | 47.8 | 2593 | Retrospective | January 2003–October 2007 |
| Du et al. [25] | 56.4 ± 18.1 | Sichuan, China | 65.7 | 565 | Retrospective | August 2015–July 2016 |
| Finkelsztein et al. [26] | 64 (51–75) | New York, USA | 31 | 152 | PCDRC | October 2014–July 2016 |
| Forward et al. [27] | 70 ± ? | Sydney, Australia | 55 | 161 | Prospective | May 2015–August 2015 |
| Freund et al. [28] | 67 (48–81) | Europe | 53 | 879 | Prospective | May 2016–June 2016 |
| Giamarellos-Bourboulis et al. [29] | 76 (IQR: 22) | Greece | ? | 3436 | Retrospective | May 2006–December 2015 |
| Gonzalez del Castillo et al. [30] | 83.6 ± 5.6 | Spain | 50.8 | 1071 | Prospective | October 2015–April 2016 |
| Guirgis et al. [31] | 59 (48–70) | Florida, USA | 49 | 3297 | Retrospective | October 2013–May 2016 |
| Haydar et al. [32] | 71 (range 18–102) | Portland, USA | 55 | 199 | Retrospective | September 2014–September 2015 |
| Henning et al. [33] | 58.4 ± 20.1 | USA | 52.2 | 7754 | PCDRC | December 2003–September 2006 |
| Ho et al. [34] | 57.1 (41–70) | Perth, Australia | 61 | 2322 | PCDRC | January 2008–December 2013 |
| Hu et al. [35] | ? | Zhejiang, China | 62.6 | 329 | Retrospective | January 2015–June 2015 |
| Hwang et al. [36] | 65 (55–73) | Seoul, South Korea | 56 | 1395 | Retrospective | August 2008–September 2014 |
| Innocenti et al. [37] | 75 ± 14 | Florence, Italy | 53 | 742 | Retrospective | June 2008–April 2016 |
| Khwannimit et al. [38] | 62 (45–75) | Songkhla, Thailand | 56.1 | 2350 | Retrospective | January 2007–December 2016 |
| Kim et al. [39] | 72 (59.5–80) | Seoul, South Korea | 62.4 | 125 | Retrospective | January 2014–December 2014 |
| Kolditz et al. [40] | 63 (?) | Germany | 56 | 9327 | Retrospective | October 2002–June 2015 |
| LeGuen et al. [41] | 72 (57–82) | Victoria, Australia | 48 | 258 | Prospective | 6 June 2016, 10 July 2016 |
| Moskowitz et al. [42] | 63.8 ± 18.1 | USA | 50.9 | 24,164 | Retrospective | January 2010–December 2014 |
| Muller et al. [43] | 66 (50–76) | Switzerland | 64.5 | 527 | Retrospective | June 2011–May 2013 |
| Park et al. [44] | 67.4 ± 17.6 | Seoul, South Korea | 45 | 1009 | Retrospective | March 2007–February 2016 |
| Peake et al. [45] | 62.9 ± 16.5 | Australasia | 59.7 | 1591 | PCDRC | October 2008–April 2014 |
| Quinten et al. [46] | 60 (48–71) | Netherlands | 56 | 193 | PCDRC | August 2012–April 2014 |
| Raith et al. [47] | 62.9 ± 17.4 | Australasia | 55.4 | 184,875 | Retrospective | January 2000–December 2015 |
| Rannikko et al. [48] | 68 (58–78) | Finland | 53 | 467 | Retrospective | March 2012–February 2014 |
| Ranzani et al. [49] | 66.1 ± 19 | Barcelona + Valencia, Spain | 62.2 | 6874 | PCDRC | January 1996–December 2015 |
| Seymour et al. [50] | 61 ± 19 | US and Germany | 43 | 74,453 | Retrospective | January 2010–December 2012 |
| Siddiqui et al. [51] | 64.4 ± 12.9 | Singapore | 60 | 58 | Retrospective | January 2015–December 2015 |
| Singer et al. [52] | 54 ± 21 | New York, USA | 47 | 200 | Retrospective | January 2014–March 2015 |
| Sterling et al. [53] | 60 ± 16.7 | USA | ? | 22,530 | PCDRC | August 2004–January 2009 |
| Szakmany et al. [54] | 74 (61–83) | Wales, UK | 47 | 380 | Prospective | 19 October 2016 |
| Tusgul et al. [55] | 80 (69–87) | Switzerland | 52.1 | 886 | Retrospective | January 2012–December 2012 |
| Umemura et al. [56] | ? | Japan | 59.7 | 387 | PCDRC | June 2010–May 2011 |
| Wang J et al. [57] | 73 (60–79) | Beijing, China | 61.8 | 477 | PCDRC | July 2015–December 2015 |
| Wang S et al. [58] | 63 ± 17.3 | Chenzhou, China | 69.5 | 311 | Retrospective | July 2012–June 2016 |
| Williams et al. [59] | 49 (30–69) | Brisbane, Australia | 51.3 | 8871 | PCDRC | October 2007–May 2011 |
qSOFA, quick Sepsis-related Organ Failure Assessment; IQR, Interquartile Range; PCDRC, Prospectively Collected Data Retrospective Cohort; ?, Information not available.
3.3. Risk of Bias within Studies
The individual assessments of risk of bias for the individual studies can be found in Appendix H.
“Selection bias” and “bias in definition” were the most common biases. The most noticeable inconsistency between all of the reviewed studies revolved around the definition of qSOFA. “Outcome measurement bias” was the least common bias (Table 2).
Table 2.
Risk of bias across the studies.
| Author Year | Selection Bias | Bias in Definition and Measurement | Outcome Measurement Bias | Handling of Missing Data | Confounding | Bias of Statistics or Presentation of Result |
|---|---|---|---|---|---|---|
| Amland et al. 2017 | ||||||
| April et al. 2016 | ||||||
| Askim et al. 2017 | ||||||
| Boulos et al. 2017 | ||||||
| Brabrand et al. 2016 | ||||||
| Burnham et al. 2018 | ||||||
| Chen et al. 2016 | ||||||
| Churpek et al. 2017 | ||||||
| de Groot et al. 2017 | ||||||
| Donnelly et al. 2017 | ||||||
| Du et al. 2017 | ||||||
| Finkelsztein et al. 2017 | ||||||
| Forward et al. 2017 | ||||||
| Freund et al. 2016 | ||||||
| Giamarellos-Bourboulis et al. 2016 | ||||||
| Gonzalez del Castillo et al. 2017 | ||||||
| Guirgis et al. 2017 | ||||||
| Haydar et al. 2017 | ||||||
| Henning et al. 2017 | ||||||
| Ho et al. 2016 | ||||||
| Hu et al. 2017 | ||||||
| Hwang et al. 2018 | ||||||
| Innocenti et al. 2016 | ||||||
| Khwannimit et al. 2018 | ||||||
| Kim et al. 2017 | ||||||
| Kolditz et al. 2016 | ||||||
| LeGuen et al. 2017 | ||||||
| Moskowitz et al. 2017 | ||||||
| Muller et al. 2017 | ||||||
| Park et al. 2017 | ||||||
| Peake et al. 2017 | ||||||
| Quinten et al. 2017 | ||||||
| Raith et al. 2017 | ||||||
| Rannikko et al. 2017 | ||||||
| Ranzani et al. 2017 | ||||||
| Seymour et al. 2016 | ||||||
| Siddiqui et al. 2017 | ||||||
| Singer et al. 2016 | ||||||
| Sterling et al. 2017 | ||||||
| Szakmany et al. 2018 | ||||||
| Tusgul et al. 2017 | ||||||
| Umemura et al. 2017 | ||||||
| Wang J et al. 2016 | ||||||
| Wang S et al. 2017 | ||||||
| Williams et al. 2016 |
Green, low risk; Yellow, moderate risk; Red, high risk.
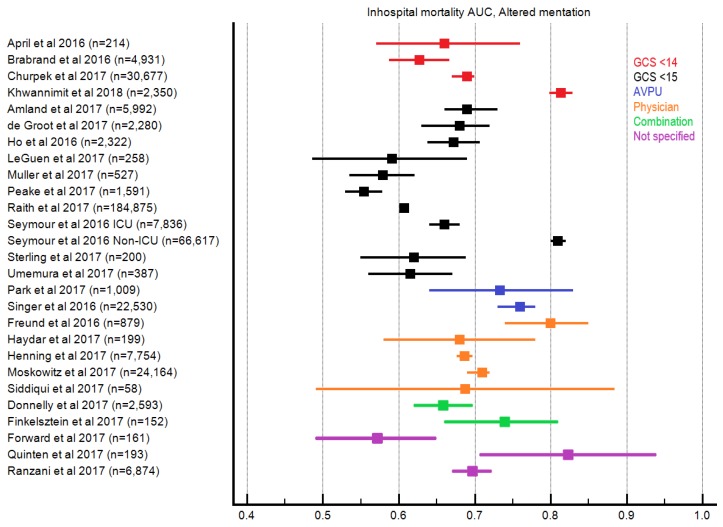
3.3.1. Criteria of qSOFA
The original cut-off values for respiratory rate and systolic blood pressure were followed by most studies. There were large disagreements in the definitions of “altered mentation” between different papers. It was variously defined as different levels of the Glasgow Coma Scale (GCS); different levels of the AVPU (Alert, Pain, Voice, Unresponsive) scale, physician/nursing discretion, and even with more than one criterion being used in the same study, e.g., ‘GCS<14 or anything other than alert on the AVPU scale’.
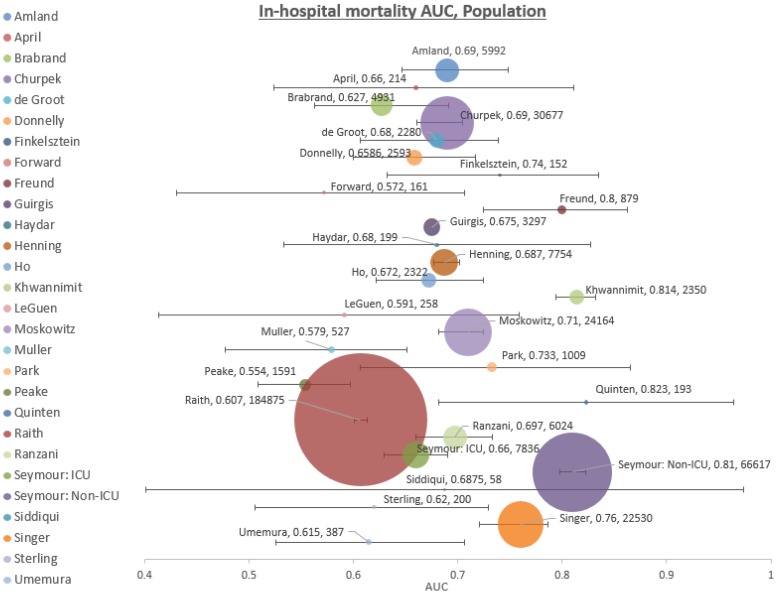
3.3.2. In-Hospital Mortality
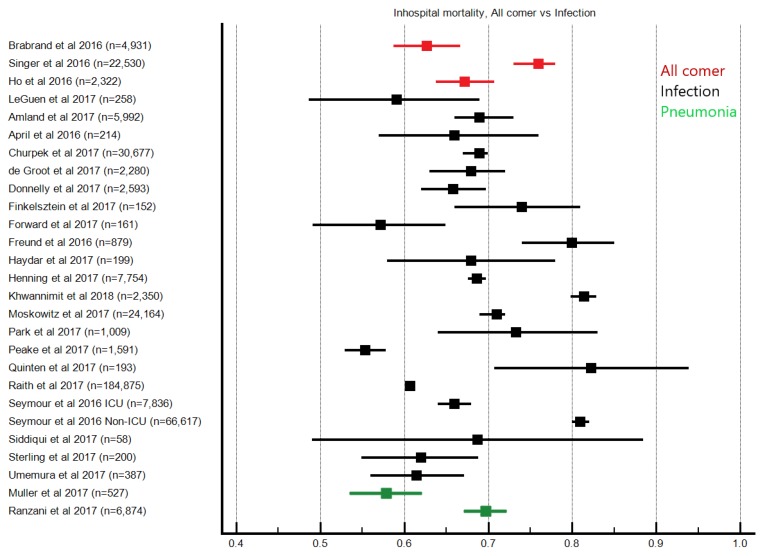
From the 27 studies with a total of 380,041 patients that had data on in-hospital mortality, the median AUROC was 0.68, with a range from 0.55 to 0.82 (Figure 2). A total of 24 studies had data on sensitivity and specificity, ranging from 0.16 to 0.98 (median 0.52) and 0.19 to 0.97 (median 0.81), respectively. Positive and negative predictive values were reported in 18 studies with a range of 0.10–0.38 (median 0.2) and 0.85–0.99 (median 0.95), respectively. Positive and negative likelihood ratios were available in 12 studies, ranging from 1.2 to 4 (median 1.83), and 0.24 to 0.84 (median 0.59), respectively.
Figure 2.
AUROC for in-hospital mortality.
A high heterogeneity was confirmed by meta-analysis, with an I2 of 98.77%. A meta-analysis would therefore not yield meaningful results, with the data being extracted from these studies.
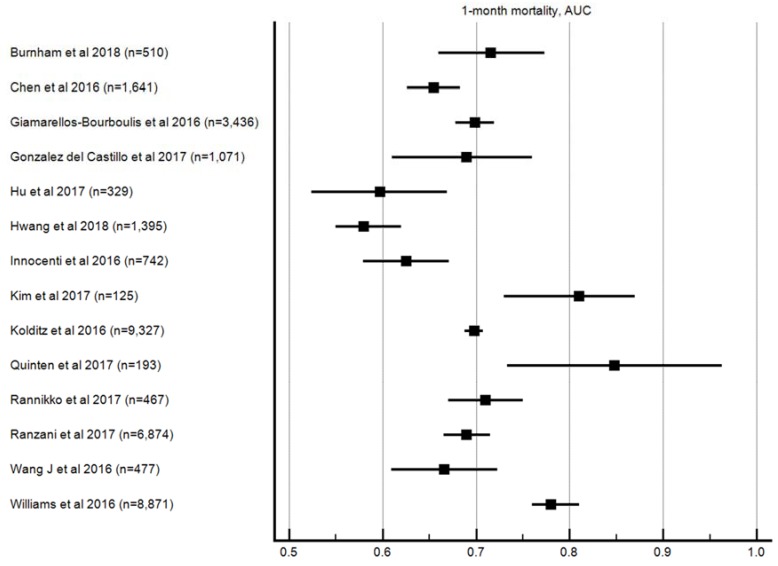
3.3.3. Month (28/30 Day) Mortality
A total of 14 studies, with 35,775 patients reported 1-month mortality data (Figure 3). The median AUROC ranged from 0.58 to 0.85 (median 0.69). Sensitivity data were available in 12 of these studies, which ranged from 0.06 to 0.71 (median 0.43); specificity data were available in 13 studies, and ranged from 0.10 to 1.00 (median 0.84). PPV and NPV data were available in 10 studies, and they ranged from 0.14 to 0.68 (median 0.34) and 0.69 to 0.97 (median 0.91), respectively. Positive and negative likelihood ratio data were available in eight studies, and the values ranged from 1.99 to 4.66 (median 2.22) and 0.3 to 0.9 (median 6.43), respectively.
Figure 3.
AUROC for 1-month mortality.
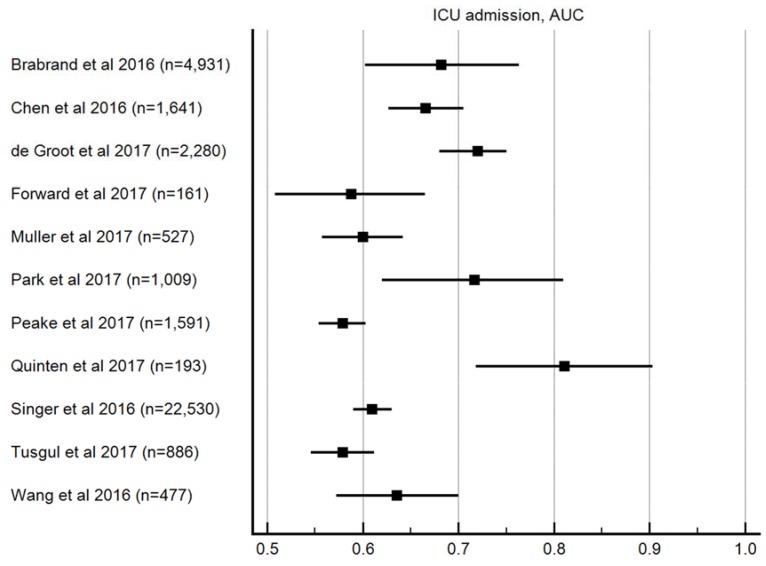
3.3.4. ICU Admission
From the 12 studies that reported data on ICU admission, AUROC ranged from 0.58–0.81 (median 0.65, Figure 4. AUROC for ICU admission). Ten studies had data on sensitivity and specificity, which ranged from 0.1 to 0.74 (median 0.37) and 0.42 to 0.97 (median 0.86), respectively. The positive predictive value and negative predictive value data were 0.089–0.578 (median 0.38) in eight studies, and 0.19–0.99 (median 0.90) in nine studies, respectively. Positive and negative likelihood ratio data were available in eight studies, and ranged from 1.27 to 9.97 (median 2.68) and 0.5 to 0.9 (median 0.63), respectively.
Figure 4.
AUROC for ICU admission.
3.3.5. Hospital and ICU Length-of-Stay (LOS)
There were no studies that reported on the predicted ability of qSOFA for median ICU or hospital LOS. However, three studies that reported on median ICU LOS. Studies reported results that ranged from 2.9 to 3.1 days. Hospital LOS, presented in median time in qSOFA-positive patients were available in five studies, ranging from 5 to 15 days (a median of nine days).
3.3.6. Diagnosis of Sepsis/Infection
Infective/septic diagnostic predictive values were only presented in two studies, Forward et al. [27] reported an AUROC for patients diagnosed with sepsis to be 0.88, and Brabrand et al. [19] reported an AUROC 0.88 for patients with a diagnosis of infection.
3.4. Summary of Results
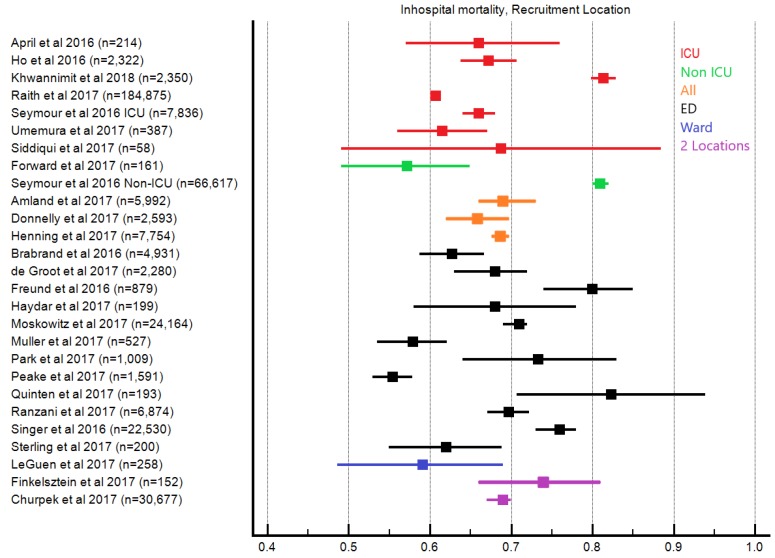
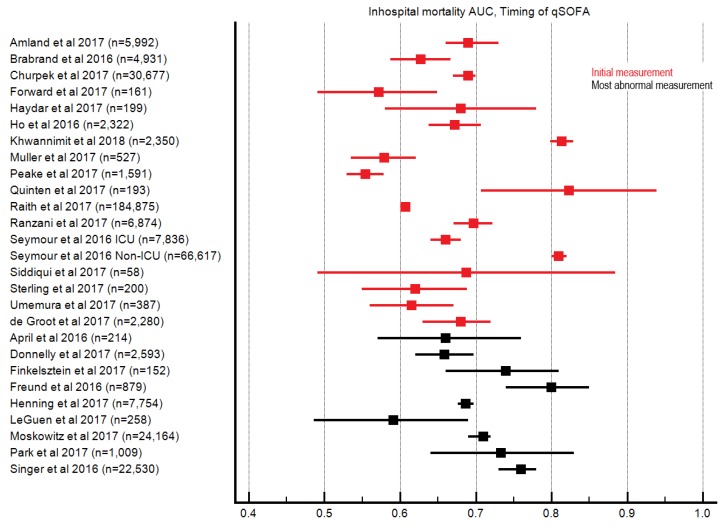
Subgroup analyses of AUROC of in-hospital mortality were inconclusive. There was no obvious difference between location of patients who presented with or without infection (Appendix I/Figure A1), location of recruitment/data collection (Appendix J/Figure A2), how mentation was defined or measured (Appendix K/Figure A3), or the timing of qSOFA (Appendix L/Figure A4). A summary of the prognostic values reported from the studies reviewed may be found in Table 3.
Table 3.
Summary of the prognostic values reported from the studies reviewed.
| qSOFA Median Value Min–Max (Number of Patients that the Value is Derived from) |
|||||||
|---|---|---|---|---|---|---|---|
| Outcomes | AUROC | Sensitivity | Specificity | PPV | NPV | LR+ | LR− |
| In-hospital mortality | 0.68 | 0.52 | 0.81 | 0.2 | 0.94 | 1.83 | 0.59 |
| 0.55–0.82 | 0.16–0.98 | 0.19–0.97 | 0.07–0.38 | 0.85–0.99 | 1.15–4 | 0.24–0.84 | |
| (n = 380,920) | (n = 118,051) | (n = 118,051) | (n = 67,555) | (n = 90,085) | (n = 24,925) | (n = 24,925) | |
| 1-month mortality | 0.69 | 0.43 | 0.84 | 0.34 | 0.91 | 2.22 | 6.43 |
| 0.58–0.85 | 0.06–0.71 | 0.10–1.00 | 0.14–0.68 | 0.69–0.97 | 1.26–3.71 | 2.17–14.4 | |
| (n = 36,415) | (n = 34,462) | (n = 36,415) | (n = 26,603) | (n = 26,603) | (n = 8121) | (n = 8121) | |
| ICU admission | 0.65 | 0.37 | 0.86 | 0.38 | 0.9 | 2.68 | 0.63 |
| 0.58–0.81 | 0.1–0.74 | 0.42–0.97 | 0.09–0.90 | 0.19–0.99 | 1.27–9.97 | 0.5–0.9 | |
| (n = 37,105) | (n = 33,816) | (n = 33,816) | (n = 11,093) | (n = 33,623) | (n = 11,286) | (n = 11,286) | |
qSOFA, quick Sepsis-related Organ Failure Assessment; AUROC, Area Under the Receiver Operating Characteristics curve; PPV, Positive Predicted Value; NPV, Negative Predicted Value; LR+, Positive Likelihood Ratio; LR−, Negative Likelihood Ratio; ICU, Intensive Care Unit.
4. Discussion
This systematic review of 45 studies with 413,634 patients showed that the AUROC of qSOFA for the in-hospital mortality in all patients (with or without suspected infection) was poor, and it showed that it was not suitable for routine clinical use. The AUROC values for other outcomes were also too low for qSOFA to be clinically useful.
qSOFA was developed to predict the likelihood of organ dysfunction in patients with suspected infection [50]. However, the detection of sepsis or infection may be clinically difficult, as symptoms of infection are highly variable [60], and they often mimic other diseases [61]. Misdiagnosis or late diagnosis have been associated with poorer outcomes [62]. Since diagnosis and detection may be difficult to achieve, screening for all patients and not just those with suspected infection would reduce subjectivity and avoidable error in the diagnostic process, and may be a better approach to reduce more severe outcomes and preventable deaths.
When initially introduced, qSOFA was reported to have an AUROC of 0.81 for predicting 1-month mortality. However, this value “was derived from models that include baseline variables plus candidate criteria” [50]. The candidate variables were age, Charlson comorbidity index, race/ethnicity, and gender. A subsequent comparison of the adjusted and unadjusted results in other studies showed that there were substantial differences between the two: Donnelly et al. adjusted 0.76 vs. unadjusted 0.66 [24]; Raith et al. adjusted 0.76 vs. unadjusted 0.61 [48]. We would therefore argue that the adjusted AUROC value reported by the original group bears little relevance for front-line clinicians.
Presenting prognostic predictions using AUROC has limitations [63], as it may be useful on a population scale, but it may not help clinicians on an individual level. In the emergency setting, high sensitivity is particularly important for supporting decisions for triage placement, and for screening and discharging patients; whereas specificity might be more relevant to the ward or ICU setting, to indicate whether a patient’s treatment should be escalated. The data obtained in this review showed the poor sensitivity and mediocre specificity of qSOFA for in-hospital mortality, 1-month mortality, and ICU admission. This suggests qSOFA’s poor utility for screening patients, and its modest value for escalation of care. The positive predictive values were also poor. Although the negative predictive values appeared to be good, the high negative predictive value is likely to reflect on the low incidence of the outcome measure.
The principal idea behind the development of qSOFA was to improve on the pre-existing Systemic Inflammatory Response Syndrome (SIRS) criteria for sepsis identification. Most studies that we reviewed showed that the AUROC for qSOFA outperforms SIRS for predicting in-hospital mortality. However, other scores such as the National Early Warning Score and the Modified Early Warning Score had been reported to have better prognostic values than both SIRS or qSOFA (NEWS 0.77, MEWS 0.73, qSOFA 0.69, and SIRS 0.65) [22]. All three scores had a higher sensitivity at their recommended cut off value when compared to qSOFA (SIRS 0.94, NEWS 0.86, MEWS 0.71, and qSOFA 0.69) [22]. Other systematic reviews focused on the comparison of qSOFA and SIRS, and on qSOFA as a prognostic tool in patients with suspected infection outside of ICU. All three reviews unanimously reported qSOFA’s poor sensitivity [64,65,66].
Two of the three variables in qSOFA are often measured and documented routinely. An assessment of mentation, however, requires experience and clinical judgment. The disagreements in the definition of “altered mentation” were a major source of bias, as they varied between different studies. In Seymour’s original qSOFA paper, the group reported that “the predictive validity of qSOFA was not significantly different when using … the GCS score <15 (p = 0.56), compared with the model with GCS score ≤13.” A standardized definition is required for future studies, and details must be added, to further elaborate on how altered mentation is determined in patients with impaired mental status at baseline, e.g., dementia sufferers. This is significant, as infection and sepsis are common causes of delirium in the older population.
The strengths of this review include the large number of study subjects, the inclusive search strategy, and bias assessment from multiple reviewers. However, there are also limitations to our review. We had taken a pragmatic approach in utilizing the qSOFA score, and we have used it on all-comers, rather than only on those with a suspected infection. Changes in treatment outcomes of sepsis made older studies difficult to compare directly with the more recent ones. The small number of prospective studies also limits the validity and generalizability of the results. There were only three prospective studies among the papers reviewed.
5. Conclusions
In conclusion, our group found that qSOFA is not a clinically useful prognostic tool for in-hospital, 1-month mortality, or ICU admission for all-comers, with or without suspected infection.
Appendix A. Articles in Non-English Languages
German articles:
[67] Christ, M.; Geier, F.; Bertsch, T.; Singler, K. Sepsis in emergency medicine. Dtsch. Med. Wochenschr. 2016, 141, 1074.
[68] Dickmann, P.; Scherag, A.; Coldewey, S.M.; Sponholz, C.; Brunkhorst, FM.; Bauer, M. Epistemology in the intensive care unit—What is the purpose of a definition?: Paradigm shift in sepsis research. Der Anaesth. 2017, 66, 622–625.
[69] Leidel, B.A. The new Sepsis 3 definition—Flop or top? Notf. Rettungsmed. 2017, 20, 383.
[70] Gerlach, J. The new Sepsis 3 definition—A courageous approach. Notf. Rettungsmed. 2017, 20, 385–389.
Spanish article:
[71] Julián-Jiménez, A.; Yañez, M.C.; del Castillo, J.G.; Salido-Mota, M.; Mora-Ordoñez, B.; Arranz-Nieto, M.J.; Chanovas-Borras, M.R.; Llopis-Roca, F.; Mòdol-Deltell, J.M.; Muñoz, G. Poder pronóstico de mortalidad a corto plazo de los biomarcadores en los ancianos atendidos en Urgencias por infección. Enferm. Infecci. Microbiol. Clín. 2017.
Russian article:
[72] Lebedev, N.V.; Klimov, A.E.; Agrba, S.B.; Gaidukevich, E.K. Combined forecasting system of peritonitis outcome. Khirurgiia 2017, 9, 33–37.
French article:
[73] Lemachatti, N.; Freund, Y. Sepsis: définitions et validations. Ann. Fr. Méd. D’urgence 2017, 7, 30–34.
Appendix B. OVID Search Strategy
qSOFA.mp.
quick SOFA.mp.
quick sequential organ failure assessment.mp.
quick sepsis-related organ failure assessment.mp.
1 or 2 or 3 or 4
mortality.mp.
5 and 6
Appendix C. WHO International Clinical Trails Registry Platform
qSOFA OR quick SOFA OR quick sequential organ failure assessment OR quick sepsis-related organ failure assessment AND Mortality.
Appendix D. Web of Science
TOPIC: (qSOFA OR quick SOFA OR quick sequential organ failure assessment OR quick sepsis-related organ failure assessment) AND TOPIC: (mortality) Timespan: All years. Indexes: SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESC.
Appendix E. Scopus
ALL ((qsofa OR quick AND sofa OR quick AND sequential AND organ AND failure AND assessment OR quick AND sepsis-related AND organ AND failure AND assessment) AND mortality).
Appendix F. ClinicalTrials.gov
(qSOFA OR quick SOFA OR quick sequential organ failure assessment OR quick sepsis-related organ failure assessment) AND Mortality.
Appendix G. Studies Excluded
Table A1.
Studies Excluded.
| Author | Title | Decisions |
|---|---|---|
| Andaluz, D., Ferrer, R. | SIRS, qSOFA, and organ failure for assessing sepsis at the emergency department. | Excluded, no original data |
| April, M.D., Lantry, J.H. | Prognostic Accuracy of Quick Sequential Organ Failure Assessment Among Emergency Department Patients Admitted to an ICU. | Excluded, no original data |
| Asai, N., Watanabe, H., Shiota, A., et al. | Could qSOFA and SOFA score be correctly estimating the severity of healthcare-associated pneumonia? | Excluded, no original data |
| Atalan, H.K., Güçyetmez, B. | The effects of the chloride:sodium ratio on acid–base status and mortality in septic patients | Excluded, Study aim irrelevant |
| Awad, A. Bader-El-Den, M., McNicholas, J., et al. | Early hospital mortality prediction of intensive care unit patients using an ensemble learning approach. | Excluded, Study aim irrelevant |
| Becchi, C., Al Malyan, M., Fabbri, L.P., et al. | Mean platelet volume trend in sepsis: Is it a useful parameter? [Andamento del volume piastrinico medio in sepsi: Un parametro utile?] | Excluded, Study aim irrelevant |
| Bhattacharjee, P., Edelson, D.P., Churpek, M.M. | Identifying Patients with Sepsis on the Hospital Wards. | Excluded, no original data |
| Biyikli, E., Kayipmaz, A.E., Kavalci, C. | Effect of platelet–lymphocyte ratio and lactate levels obtained on mortality with sepsis and septic shock. | Excluded, Study aim irrelevant |
| Busani, S., Girardis, M. | PSP/reg: A new stone in sepsis biomarkers? | Excluded, Study aim irrelevant |
| Christ, M., Geier, F., Bertsch, T., et al. | Sepsis in Emergency Medicine. [German] | Language German |
| Cour, M., Hernu, R., Bénet, T., et al. | Benefits of smart pumps for automated changeovers of vasoactive drug infusion pumps: A quasi-experimental study | Excluded, Study aim irrelevant |
| David, N., Roux, N., Clavier, E., et al. | Open repair of extensive thoracoabdominal and thoracic aneurysm: A preliminary single-center experience with femorofemoral distal aortic perfusion with oxygenator and without cerebrospinal fluid drainage | Excluded, Study aim irrelevant |
| Desautels, T., Calvert, J., Hoffman, J., et al. | Prediction of Sepsis in the Intensive Care Unit with Minimal Electronic Health Record Data: A Machine Learning Approach. | Excluded, Study aim irrelevant |
| Dickmann, P., Scherag, A., Coldewey, S.M., et al. | Epistemology in the intensive care unit—What is the purpose of a definition? Paradigm shift in sepsis research | Language German |
| Du, B., Weng, L. | Systemic inflammatory response syndrome, sequential organ failure assessment, and quick sequential organ failure assessment: More pieces needed in the sepsis puzzle | Excluded, no original data |
| Edmark, C., McPhail, M.J.W., Bell, M., et al. | LiFe: A liver injury score to predict outcome in critically ill patients | Excluded, Study aim irrelevant |
| Fukushima, H., Kobayashi, M., Kawano, K., et al. | Performance of qSOFA and SOFA for predicting mortality in patients with acute pyelonephritis associated with upper urinary tract calculi. | Excluded. Patient too specific |
| Gerlach, H. | The new Sepsis 3 definition—a courageous approach | Language German |
| del Castillo, J.G., Carlota, C., Candel, F.J., et al. | New sepsis criteria: do they replace or complement what is known in the approach to the infectious patient? | Excluded, no original data |
| Gul, F., Arslantas, M.K., Cinel, I., et al. | Changing Definitions of Sepsis. [Review] | Excluded, no original data |
| Hou, P.C., Seethala, R.R., Aisiku, I.P. | qSOFA—Welcome to the sepsis alphabet soup | Excluded, no original data |
| Huson, M.A., Kalkman, R., Grobusch, M.P., et al. | Predictive value of the qSOFA score in patients with suspected infection in a resource limited setting in Gabon. | Excluded. Patient too specific |
| Huson, M.A.M., Katete, C., Chunda, L., et al. | Application of the qSOFA score to predict mortality in patients with suspected infection in a resource-limited setting in Malawi. | Excluded. Patient too specific |
| Jacob, J.A. | New sepsis diagnostic guidelines shift focus to organ dysfunction. | Excluded, no original data |
| Jawa, R.S., Vosswinkel, J.A., McCormack, J.E., et al. | Risk assessment of the blunt trauma victim: The role of the quick Sequential Organ Failure Assessment Score (qSOFA). | Excluded. Patient too specific |
| Julian-Jimenez, A., Yanez, M.C., Gonzalez-del Castillo, J., et al. | Prognostic power of biomarkers for short-term mortality in the elderly patients seen in Emergency Departments due to infections. [Spanish] | Language Spanish |
| Kim, M., Ahn, S., Kim, W.Y., et al. | Predictive performance of the quick Sequential Organ Failure Assessment score as a screening tool for sepsis, mortality, and intensive care unit admission in patients with febrile neutropenia. | Excluded. Patient too specific |
| Ladhani, H.A., Sajankila, N., Zosa, B.M., et al. | Utility of Sequential Organ Failure Assessment score in predicting bacteremia in critically ill burn patients. | Excluded. Patient too specific |
| Lebedev, N.V., Klimov, A.E., Agrba, S.B., et al. | [Combined forecasting system of peritonitis outcome]. [Russian] | Language Russian |
| Leclerc, F., Duhamel, A., Deken, V., et al. | Can the pediatric logistic organ dysfunction-2 score on day 1 be used in clinical criteria for sepsis in children? | Excluded. Patient too specific |
| Lee, S.J., Ramar, K., Park, J.G., et al. | Increased fluid administration in the first three hours of sepsis resuscitation is associated with reduced mortality: A retrospective cohort study | Excluded, Study aim irrelevant |
| Leidel, B.A. | The new Sepsis 3 definition—Flop or top? | Language German |
| Lemachatti, N., Freund, Y. | Sepsis: Definitions and validations. [French] | Language French |
| Maegele, M., Lefering, R., Yucel, N., et al. | Early coagulopathy in multiple injury: An analysis from the German Trauma Registry on 8724 patients | Excluded, Study aim irrelevant |
| Marik, P.E., Taeb, A.M. | SIRS, qSOFA, and new sepsis definition | Excluded, no original data |
| McCormack, D., Kulkarni, M., Keller, S.E. | Perspectives and implications of the new sepsis clinical practice guidelines. | Excluded, no original data |
| McLymont, N., Glover, G.W. | Scoring systems for the characterization of sepsis and associated outcomes. | Excluded, no original data |
| Moore, C.C., Hazard, R., Saulters, K.J., et al. | Derivation and validation of a universal vital assessment (UVA) score: a tool for predicting mortality in adult hospitalised patients in sub-Saharan Africa. | Excluded. Patient too specific |
| Patidar, K.R., Shaw, J., Acharya, C., et al. | No Association Between Quick Sequential Organ Failure Assessment and Outcomes of Patients With Cirrhosis and Infections. | Excluded. Patient too specific |
| Peach, BC. | Implications of the new sepsis definition on research and practice. | Excluded, no original data |
| Piano, S., Bartoletti, M., Tonon, M., et al. | Assessment of Sepsis-3 criteria and quick SOFA in patients with cirrhosis and bacterial infections. | Excluded. Patient too specific |
| Rasulo, F.A., Bellelli, G., Ely, E.W., et al. | Are you Ernest Shackleton, the polar explorer? Refining the criteria for delirium and brain dysfunction in sepsis | Excluded, no original data |
| Rhee, C., Klompas, M. | New Sepsis and Septic Shock Definitions Clinical Implications and Controversies | Excluded, no original data |
| Ronco, C., Legrand, M., Goldstein, S.L., et al. | Neutrophil gelatinase-associated lipocalin: Ready for routine clinical use? An international perspective | Excluded, no original data |
| Rothman, M., Levy, M., Dellinger, R.P., et al. | Sepsis as 2 problems: Identifying sepsis at admission and predicting onset in the hospital using an electronic medical record-based acuity score | Excluded, Study aim irrelevant |
| Sager, R., Wirz, Y., Amin, D., et al. | Are admission procalcitonin levels universal mortality predictors across different medical emergency patient populations? Results from the multi-national, prospective, observational TRIAGE study. | Excluded, Study aim irrelevant |
| Scheer, C.S., Kuhn, S.O., Rehberg, S. | Use of the qSOFA score in the emergency department. | Excluded, no original data |
| Schlapbach, L.J., Straney, L., Bellomo, R., et al. | Prognostic accuracy of age-adapted SOFA, SIRS, PELOD-2, and qSOFA for in-hospital mortality among children with suspected infection admitted to the intensive care unit. | Excluded. Patient too specific |
| Scott, M.C. | Defining and Diagnosing Sepsis. | Excluded, no original data |
| Seckel, M.A. | Sepsis-3: The new definitions. | Excluded, no original data |
| Seckel, M.A., Ahrens, T. | Challenges in Sepsis Care: New Sepsis Definitions and Fluid Resuscitation Beyond the Central Venous Pressure. | Excluded, no original data |
| Serafim, R., Gomes, J.A., Salluh, J., et al. | A comparison of the quick-SOFA (qSOFA) and SIRS criteria for the diagnosis of sepsis and prediction of mortality: A systematic review and meta-analysis. | Excluded, no original data |
| Shetty, A., MacDonald, S.P., Williams, J.M., et al. | Lactate ≥ 2 mmol/L plus qSOFA improves utility over qSOFA alone in emergency department patients presenting with suspected sepsis. | Excluded, Study aim irrelevant |
| Singer, M., Deutschman, C.S., Seymour, C., et al. | The third international consensus definitions for sepsis and septic shock (sepsis-3). | Excluded, no original data |
| Solligard, E., Damas, J.K. | SOFA criteria predict infection-related in-hospital mortality in ICU patients better than SIRS criteria and the qSOFA score. | Excluded, no original data |
| Viale, P., Tedeschi, S., Scudeller, L., et al. | Infectious diseases team for the early management of severe sepsis and septic shock in the emergency department | Excluded, Study aim irrelevant |
| Vincent, J.L., Grimaldi, D. | Quick sequential organ failure assessment: Big databases vs. intelligent doctors. | Excluded, no original data |
| Wang, A.Y., Ma, H.P., Kao, W.F., et al. | Red blood cell distribution width is associated with mortality in elderly patients with sepsis. | Excluded, Study aim irrelevant |
| Wang, H.E., Jones, A.R., Donnelly, J.P. | Revised National Estimates of Emergency Department Visits for Sepsis in the United States | Excluded, Study aim irrelevant |
| Zaccone, V., Tosoni, A., Passaro, G., et al. | Sepsis in Internal Medicine wards: Current knowledge, uncertainties and new approaches for management optimization. | Excluded, no original data |
| Zhou, X., Ding, B., Ye, Y., Tang, G., et al. | Authors respond to Both qSOFA score and bedside plasma lactate are the predictors of mortality for patients with infections in ED. | Excluded, no original data |
| Zhou, X., Tang, G. | Quick sepsis-related organ failure assessment (qSOFA) predicting outcomes in patients with infection, some lingering doubts. | Excluded, no original data |
| Zhou, X.D., Zhang, J.Y., Liu, W.Y., et al. | Quick chronic liver failure-sequential organ failure assessment: An easy-to-use scoring model for predicting mortality risk in critically ill cirrhosis patients | Excluded. Patient too specific |
Appendix H. Characteristics of Studies
| First Author (Year) | Amland RC (2017) [15] |
| Title | Quick Sequential [Sepsis-Related] Organ Failure Assessment (qSOFA) and St. John Sepsis Surveillance Agent to Detect Patients at Risk of Sepsis: An Observational Cohort Study. |
| Journal | American Journal of Medical Quality |
| Reviewer | RL, MB, LL |
| Study sponsor | Nil |
| Study type | Multi-centered retrospective cohort (January–March 2016) |
| Location | United States |
Participants
|
5992 48% male 65 (51–76) Hospitalized adults with suspected infection, defined in Sepsis-3 |
| qSOFA criteria | Respiratory rate ≥22 bpm, systolic blood pressure ≤100 mmHg, and Glasgow Coma Score (GCS) <15 |
| Primary outcome Other outcomes |
In-hospital mortality Composite of death or ICU admission |
| Results | In-hospital mortality AUC 0.69 (95% CI 0.66 to 0.73) |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
|
| Bias in definition and measurement |

|
Definition of sepsis is chart-based |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Not mentioned |
| Confounding |

|
Retrospective |
| Bias of statistics or presentation of result |

|
Possible double counting in modelling |
| First Author (Year) | April MD (2016) [16] |
| Title | Sepsis clinical criteria in emergency department patients admitted to an intensive care unit: An external validation study of quick sequential organ failure assessment |
| Journal | The Journal of Emergency Medicine |
| Reviewer | RL, KH, LL, MB, CG |
| Study sponsor | No information given |
| Study type | Retrospective cohort (August 2012–February 2015) |
| Location | Texas, USA |
Participants
|
321 identified, 214 analyzed 58.9% male 72 (60–79) ICU admission from ED with presumed sepsis; Patient with non-infectious etiology excluded |
| qSOFA criteria | Respiratory rate > 22 breaths/min; Glasgow Coma Scale < 14; Systolic blood pressure < 100 mm Hg |
| Primary outcome Other outcomes |
Prognostic accuracy of qSOFA and SIRS for predicting in-hospital mortality (AUROC, sensitivity, specificity, and likelihood ratio) Assessment of the prognostic accuracy of LODS and SOFA criteria, using the same measures |
| Results | 0.66 (95% CI 0.57–0.76) for qSOFA, 89.7% sensitivity, 27.4% specificity, 1.2 positive likelihood ratio, and 0.4 negative likelihood ratio |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Only ICU patients involved; Selective patients |
| Bias in definition and measurement |

|
RR > 22 breaths/min; sBP < 100; Altered mentation: GCS < 14 |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Not explicit |
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
Potential presentation error in Table 3; No selective reporting of results |
| First Author (Year) | Askim A (2017) [17] |
| Title | Poor performance of quick-SOFA (qSOFA) score in predicting severe sepsis and mortality—A prospective study of patients admitted with infection to the emergency department. |
| Journal | Scandinavian Journal of Trauma, Resuscitation & Emergency Medicine |
| Reviewer | RL, CG, MB |
| Study sponsor | Central Norway Regional Health Authority (RHA) and the NorwegianUniversity of Science and Technology (NTNU), Trondheim Norway. |
| Study type | Prospectively Collected Data Retrospective Cohort (January–Decemeber 2012) |
| Location | Norway |
Participants
|
1535 53% male 62 (41–78) All patients with suspected or confirmed infection |
| qSOFA criteria | Respiratory rate ≥ 22 bpm, systolic blood pressure ≤ 100 mmHg, and Glasgow Coma Score (GCS) < 15 |
| Primary outcome Other outcomes |
? |
| Results | qSOFA ≥2 Sensitivity 0.13 (0.05–0.25) Specificity 0.96 (0.95–0.97) PPV 0.14 (0.07–0.23) NPV 0.96 (0.96–0.96) |
| Note | 16 years old and older |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
|
| Bias in definition and measurement |

|
Sepsis defined by SIRS criteria |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
10% missing data |
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
| First Author (Year) | Boulos D (2017) [18] |
| Title | Predictive value of quick Sepsis-Related Organ Failure Scores following sepsis-related Medical Emergency Team calls: A retrospective cohort study |
| Journal | Anesthetic Intensive Care |
| Reviewer | RL, CG, MB |
| Study sponsor | Nil noted |
| Study type | Retrospective cohort (January 2015–Decemeber 2015) |
| Location | Monash Health, Australia |
Participants
|
646 52% male 68.52 ± 17.4 (mean) Patients who had sepsis-related Medical Emergency Team calls |
| qSOFA criteria | Not defined |
| Primary outcome Other outcomes |
28-day, in-hospital mortality ICU admission, need for inotropic or ventilatory support, made not-for-resuscitation, repeat Medical Emergency Team (MET) call |
| Results | 28-day mortality AUC 0.64 for qSOFA |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Ward patients with MET calls only |
| Bias in definition and measurement |

|
SIRS to define sepsis |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Not reported/ Not mentioned |
| Confounding |

|
Could not be assessed |
| Bias of statistics or presentation of result |

|
| First Author (Year) | Brabrand M (2016) [19] |
| Title | Validation of the qSOFA score for identification of septic patients: A retrospective study |
| Journal | European Journal of Internal Medicine |
| Reviewer | RL, KH, LL, MB, CG |
| Study sponsor | No external funding |
| Study type | Retrospective cohort (Letter) |
| Location | Denmark |
Participants
|
4931 analyzed 49.2% male 65 (50–77) ED patients who are acutely admitted under medicine |
| qSOFA criteria | RR greater or equal to 22, sBP lesser or equal to 100, and altered mentation <14 |
| Primary outcome Other outcomes |
Hospital mortality and ICU admission Hospital mortality, and ICU admission individually |
| Results | Hospital mortality AUROC 0.627 (0.587–0.667) |
| Note | The author of this article is also one of the reviewers of this review article |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Only medical patients included |
| Bias in definition and measurement |

|
|
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Not stated in paper but asked in person. |
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
| First Author (Year) | Burnham JP (2018) [20] |
| Title | qSOFA score: Predictive validity in Enterobacteriaceae bloodstream infections. |
| Journal | Journal of Critical Care |
| Reviewer | RL, CG, MB |
| Study sponsor | Nil |
| Study type | Retrospective cohort (June 2009–Decemeber 2013) |
| Location | USA |
Participants
|
510 52% male 61.1 (51.6–69.8) all patients age ≥ 18 with sepsis, severe sepsis, or septic shock, and a positive blood culture for an organism in the Enterobacteriaceae family |
| qSOFA criteria | Altered mental status—Reported by family, RR 32(?) |
| Primary outcome Other outcomes |
All-cause 30-day mortality Nil |
| Results | 30-day mortality AUC 0.716 for qSOFA ≥2 |
| Note | Sepsis as defined by systemic inflammatory response syndrome (SIRS) criteria Second analysis |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Only Enterobacteriaceae |
| Bias in definition and measurement |

|
AMS not well-defined |
| Outcome measurement bias |

|
Hospice discharge considered dead |
| Handling of missing data |

|
Reported missing data, but did not explain how they responded to this |
| Confounding |

|
Young patients and large Afro-American population |
| Bias of statistics or presentation of result |

|
| First Author (Year) | Chen YX (2016) [21] |
| Title | Use of CRB-65 and quick Sepsis-related Organ Failure Assessment to predict site of care and mortality in pneumonia patients in the emergency department: A retrospective study |
| Journal | Critical Care |
| Reviewer | RL, KH, LL, MB, CG |
| Study sponsor | No information provided |
| Study type | Prospectively Collected Data Retrospective Cohort (January 2012–May 2014) |
| Location | Beijing, China |
Participants
|
1769 identified, 1641 analyzed 59% male 73 (62–79) ED patients with new infiltrates on chest radiograph and two or more symptoms consistent with pneumonia (including cough, dyspnea, fever, sputum production, breathlessness, and/or pleuritic chest pain) |
| qSOFA criteria | Respiratory rate ≥22/minute, altered mentation (Glasgow Coma Scale score ≤13) and systolic blood pressure ≤100 mmHg. |
| Primary outcome Other outcomes |
All-cause mortality at 28 days Hospitalization and ICU admission |
| Results | 28 day mortality qSOFA AUC 0.655 (0.626–0.683) |
| Note | Ethics for current study not stated |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Restrictive inclusive criteria Small number of sample |
| Bias in definition and measurement |

|
Cut-off value assumed to be Glasgow Coma Scale ≤13 |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
|
| Confounding |

|
Smoking status of patients not included |
| Bias of statistics or presentation of result |

|
Potential Table 3 error: qSOFA 2 or >2 |
| First Author (Year) | Churpek MM (2017) [22] |
| Title | qSOFA, SIRS, and early warning scores for detecting clinical deterioration in infected patients outside the ICU |
| Journal | American Journal of Respiratory and Critical Care Medicine |
| Reviewer | RL, KH, LL, MB, CG |
| Study sponsor | University of Chicago |
| Study type | Retrospective cohort (November 2008–January 2016) |
| Location | Chicago, USA |
Participants
|
150,288 identified, 30,677 analyzed 47% male Mean 58 years old (SD 18.0) All patients (ED and ward) outside of ICU with suspected infection |
| qSOFA criteria | Systolic blood pressure ≤100 mm Hg, respiratory rate ≥22 breaths per minute, and altered mental status (defined as either a Glasgow Coma Scale score ≤13 or an Alert Voice Pain Unresponsive scale (AVPU) other than “Alert”) |
| Primary outcome Other outcomes |
In-hospital mortality composite of death or ICU stay |
| Results | In-hospital mortality AUC 0.69 (0.67–0.70) |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Definition of sepsis |
| Bias in definition and measurement |

|
|
| Outcome measurement bias |

|
|
| Handling of missing data |

|
66% of admissions were excluded due to missing data |
| Confounding |

|
Not recorded |
| Bias of statistics or presentation of result |

|
| First Author (Year) | de Groot B (2017) [23] |
| Title | The most commonly used disease severity scores are inappropriate for risk stratification of older emergency department sepsis patients: An observational multi-centre study. |
| Journal | Scandinavian Journal of Trauma, Resuscitation & Emergency Medicine |
| Reviewer | RL, CG, MB |
| Study sponsor | Nil |
| Study type | Prospectively Collected Data Retrospective Cohort (April 2011–February 2016) |
| Location | Holland |
Participants
|
2280 57.7% male (mean 61.1 years old (SD17.0)) ED patients with suspected infection and Manchester triage category of yellow, orange, or red with IV ABx |
| qSOFA criteria | Respiratory rate ≥22 bpm, systolic blood pressure ≤100 mmHg, and Glasgow Coma Score (GCS) <15 |
| Primary outcome Other outcomes |
In-hospital mortality ICU or MCU admission, an unanticipated transfer to an ICU or MCU within 48 h after being admitted to a ward [20], and the composite outcome of in-hospital mortality, ICU or MCU admission, or unanticipated transfer to an ICU or MCU within 48 h. |
| Results | AUC (in-hospital mortality?) 0.68 for qSOFA ≥2 |
| Note | 17 years old or olderSuspected infection not defined |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
17 or more years old; categories 1–3 only |
| Bias in definition and measurement |

|
Suspected infection not defined; definition of severe/moderate of severity scores |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
|
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
| First Author (Year) | Donnelly JP (2017) [24] |
| Title | Application of the Third International Consensus Definitions for Sepsis (Sepsis-3) Classification: A retrospective population-based cohort study |
| Journal | Lancet Infectious Disease |
| Reviewer | RL, KH, LL, MB, CG |
| Study sponsor | National Institute of Nursing Research; Center for Clinical and Translational Science and University of Alabama |
| Study type | Retrospective cohort (January 2003–October 2007) |
| Location | USA |
Participants
|
22692 identified, 2593 analyzed 47.8% male 68 (61–75) Stroke study database; >45 years old; serious infection (defined as requiring admission), All patients (ICU, floor, or others) |
| qSOFA criteria | Altered mentation (Glasgow coma score <14 or deemed as non-alert on the alert, voice, pain, unresponsive scale), a systolic blood pressure of 100 mm Hg or lower, or respiratory rate of at least 22 breaths per min |
| Primary outcome Other outcomes |
In-hospital mortality 28-day mortality and 1-year mortality |
| Results | 0.759 AUC in-hospital mortality (Baseline plus qSOFA) |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Patients from a stroke database, higher African–American population |
| Bias in definition and measurement |

|
|
| Outcome measurement bias |

|
|
| Handling of missing data |

|
|
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
| First Author (Year) | Du X (2017) [25] |
| Title | Both qSOFA score and bedside plasma lactate are the predictors of mortality for patients with infections in ED. |
| Journal | American Journal of Emergency Medicine |
| Reviewer | RL, CG, MB |
| Study sponsor | Research Fund of the Ministration of Health of China (201302003) and the Ministration of Health of Chengdu City (CDWSYJ-2016-01). |
| Study type | Retrospective case-controlled study (August 2015–July 2016) |
| Location | China |
Participants
|
565 65.66% male (Mean 56.44 ± 18.1) All ED patients with infections |
| qSOFA criteria | Respiratory rate ≥22 bpm, systolic blood pressure ≤100 mmHg, and Glasgow Coma Score (GCS) <15 |
| Primary outcome Other outcomes |
28-day mortality or/and ICU admission |
| Results | The odds ratio of qSOFA and plasma lactate were 1.652 and 1.444(p value <0.05) |
| Note | Correspondence. Short report. Not enough details for study to be analyzed critically |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
|
| Bias in definition and measurement |

|
Infection not defined |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Large percentage of data missing |
| Confounding |

|
Unclear, cannot be assessed |
| Bias of statistics or presentation of result |

|
Unclear, cannot be assessed |
| First Author (Year) | Finkelsztein EJ (2017) [26] |
| Title | Comparison of qSOFA and SIRS for predicting adverse outcomes of patients with suspicion of sepsis outside the intensive care unit |
| Journal | Critical Care |
| Reviewer | RL, KH, LL, MB, CG |
| Study sponsor | National Institutes of Health Grants |
| Study type | Prospectively Collected Data Retrospective Cohort (October 14—?) |
| Location | NY, USA |
Participants
|
186 identified, 152 analyzed 31% male 64 (51–75) ED or ward to ICU, suspicion of infection |
| qSOFA criteria | Systolic blood pressure of ≤100 mmHg, respiratory rate of ≥22/minute, and altered mental status. The latter was not confined to a Glasgow Coma Scale score of <15, but it included any altered mentation, such as disorientation and somnolence |
| Primary outcome Other outcomes |
All-cause in-hospital mortality ICU-free days from ICU admission to day 28, ventilator-free days from initiation of invasive mechanical ventilation to day 28, organ dysfunction-free days and renal dysfunction free days from ICU admission to day 14 |
| Results | In-hospital AUC 0.74 (0.66–0.81), Sensitivity 90% (73–98), Specificity 42% (33–52) |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Biobank registry. Gender differences were high |
| Bias in definition and measurement |

|
Individual biases |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Not reported |
| Confounding |

|
High numbers of malignancy and immunosuppression |
| Bias of statistics or presentation of result |

|
| First Author (Year) | Forward E (2017) [27] |
| Title | Predictive validity of the qSOFA criteria for sepsis in non-ICU inpatients. |
| Journal | Intensive Care Medicine |
| Reviewer | RL, CG, MB |
| Study sponsor | Nil |
| Study type | Prospective case-controlled study (May–August 15) |
| Location | Sydney, Australia |
Participants
|
161 55% male (mean 70 years old) Adult non-ICU inpatients who triggered the hospital ‘Sepsis Kills’ pathway with acute deterioration and suspected or proven infection |
| qSOFA criteria | respiratory rate ≥22 bpm, systolic blood pressure ≤100 mmHg, and ‘altered mentation’ |
| Primary outcome Other outcomes |
Inpatient sepsis, in-hospital mortality, ICU admission, and blood culture positivity |
| Results | ? |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Triggering of pathway |
| Bias in definition and measurement |

|
Prone to human error |
| Outcome measurement bias |

|
Cannot be assessed |
| Handling of missing data |

|
12% missing with no accounting system |
| Confounding |

|
Cannot be assessed |
| Bias of statistics or presentation of result |

|
Error in Table 1 |
| First Author (Year) | Freund Y (2017) [28] |
| Title | Prognostic accuracy of sepsis-3 criteria for in-hospital mortality among patients with suspected infection presenting to the emergency department |
| Journal | JAMA |
| Reviewer | RL, KH, LL, MB, CG |
| Study sponsor | French Society of Emergency Medicine |
| Study type | Prospective cohort (16 May 16–16 June) |
| Location | International: France, Switzerland, Spain, Belgium |
Participants
|
1088 identified, 879 analyzed 53% male 67 (48–81) ED patients with clinical suspicion of infection |
| qSOFA criteria | Respiratory rate >21 breaths/min; Systolic arterial blood pressure ≤100 mm Hg; or altered mental status (determined clinically by the treating physician) |
| Primary outcome Other outcomes |
In-hospital mortality Admission to ICU, length of ICU stay of more than 72 h, a composite of death, or ICU stay of more than 72 h |
| Results | In-hospital mortality AUC 0.80 (0.74–0.85) Sensitivity 70% (59–80), Specificity 79% (76–82), PPV 24% (18–30), NPV 97% (95–98) |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
|
| Bias in definition and measurement |

|
Altered mental status (determined clinically by the treating physician) |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
|
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
| First Author (Year) | Giamarellos-Bournoulis EJ (2017) [29] |
| Title | Validation of the new Sepsis-3 definitions: Proposal for improvement in early risk identification |
| Journal | Clinical Microbiology and Infection |
| Reviewer | RL, KH, LL, MB, CG |
| Study sponsor | Hellenic Institute for the Study of Sepsis |
| Study type | Retrospective cohort (May 06–Decemeber 15) |
| Location | Greece |
Participants
|
5176 identified, 4487 analyzed ? 76 (22) All patients with signs of infection of onset <24 h ago and at least two signs of SIRS |
| qSOFA criteria | GCS <13, RR>22, sBP <100 |
| Primary outcome Other outcomes |
Sensitivity of qSOFA and of the new sepsis definition to predict 28-day mortality To compare the performance of qSOFA and SIRS criteria for the early prediction of organ dysfunction outside the ICU, and to compare misclassification of severe cases by the 1991 definitions, and by Sepsis-3 definitions separately for non-ICU and ICU patients |
| Results | ? |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
High threshold for inclusion criteria |
| Bias in definition and measurement |

|
High threshold for altered mentation, respiratory rate, and systolic blood pressure |
| Outcome measurement bias |

|
Not defined clearly |
| Handling of missing data |

|
Not stated |
| Confounding |

|
No population characteristics and co-morbidities |
| Bias of statistics or presentation of result |

|
Too limited to be commented on |
| First Author (Year) | González del Castillo (2017) [30] |
| Title | Prognostic accuracy of SIRS criteria, qSOFA score and GYM score for 30-day-mortality in older non-severely dependent infected patients attended in the emergency department. |
| Journal | European Journal of Clinical Microbiology & Infectious Diseases |
| Reviewer | RL, CG, KH |
| Study sponsor | No financial support was used. The promoter of this study has been the Infectious Disease Group of the Spanish Emergency Medicine Society. This group has received financial support from Merck, Tedec-Meiji, Pfizer, Thermo Fisher, Laboratorios Rubio and Novartis in the last year to organize conferences and group meetings. None of the authors have received any financial compensation. |
| Study type | Observational, prospective cohort study (1 and 22 October 2015, 12 and 19 January 2016, and 13 and 27 April 2016) |
| Location | Spain |
Participants
|
1071 50.8% male (mean 83.6 (SD 5.6)) Patients aged 75 years or older who attended for an acute infection, who did not have severe functional dependence (Barthel index >40) |
| qSOFA criteria | Glasgow Coma Scale score <15, systolic blood pressure < 100 mmHg and respiratory rate ≥ 22 per min |
| Primary outcome Other outcomes |
All-cause 30-day mortality |
| Results | All-cause 30-day mortality AUC 0.69 (95% CI 0.61–0.76) for the qSOFA score |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Older patients. Barthel index >40 |
| Bias in definition and measurement |

|
SIRS definition, GCS defined differently |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Not reported |
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
| First Author (Year) | Guirgis (2017) [31] |
| Title | Development of a Simple Sequential Organ Failure Assessment Score for Risk Assessment of Emergency Department Patients with Sepsis |
| Journal | Journal of Intensive Care Medicine |
| Reviewer | RL, CG, KH |
| Study sponsor | National Institutes of General Medical Sciences and NIH Loan Repayment Program |
| Study type | Retrospective cohort (October 13–May 16) |
| Location | Jacksonville, FL, USA |
Participants
|
3297 49% male 59 (48–70) Adult patients admitted through ED and discharge diagnosis of sepsis |
| qSOFA criteria | respiratory rate ≥22 breaths/ minute, altered mental status, or systolic blood pressure ≤100 mm Hg |
| Primary outcome Other outcomes |
in-hospital mortality Sensitivities and specificities were calculated for patients with a discharge diagnosis of sepsis with a score of 2 or more for SOFA, qSOFA, or simple SOFA and were compared to patients with a score of <2 |
| Results | In-hospital mortality AUC 0.68 for qSOFA sensitivity and specificity of qSOFA ≥2 were 38% and 86%, respectively |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
|
| Bias in definition and measurement |

|
AMS relied on nursing documentation |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Listed as missing but not accounted for |
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
| First Author (Year) | Haydar S (2017) [32] |
| Title | Comparison of QSOFA score and SIRS criteria as screening mechanisms for emergency department sepsis. |
| Journal | American Journal of Emergency Medicine |
| Reviewer | RL, CG, KH |
| Study sponsor | Nil |
| Study type | Retrospective study (September 14–September 15) |
| Location | USA |
Participants
|
199 55% male 71 years old (range 18–102) Adult septic Medicare and Medicaid patients treated with antibiotics in the ED for suspected infection, admitted to the hospital, and subsequently discharged with a Center for Medicare Services Diagnosis Related Grouping (DRG) for sepsis |
| qSOFA criteria | Altered mental status (AMS), respiratory rate (RR) >22/min, and systolic blood pressure (SBP) <100 mmHg |
| Primary outcome Other outcomes |
Sensitivity of the qSOFA score in diagnosing sepsis Diagnostic timeliness of qSOFA in diagnosing sepsis when compared to the traditional SIRS criteria |
| Results | AUC 0.68 (0.58–0.78) for qSOFA |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Medicare and Medicaid patients only |
| Bias in definition and measurement |

|
AMS, diagnosis, and suspected infection not defined |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Not accounted for |
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
| First Author (Year) | Henning DJ [33] |
| Title | An Emergency Department Validation of the SEP-3 Sepsis and Septic Shock Definitions and Comparison With 1992 Consensus Definitions |
| Journal | Annals of Emergency Medicine |
| Reviewer | RL, KH, LL, MB, CG |
| Study sponsor | Non stated |
| Study type | Prospectively Collected Data Retrospective Cohort (3 Decemeber–4 September, 5 September –6 September, 4 July–5 June) |
| Location | USA |
Participants
|
7637 identified, 7754 analyzed 52.2% male 56.9 (20.8) All patients (ED, ward, ICU) with suspected infection |
| qSOFA criteria | Respiratory rate greater than or equal to 22 breaths/min, altered mental status (documented by physician), and hypotension defined by a systolic blood pressure of less than or equal to 100 mm Hg. |
| Primary outcome Other outcomes |
All-cause in-hospital mortality, defined as death before hospital discharge. - |
| Results | AUC 0.77, Sens 52(46–57), Spec 86(85–87), PPV 14(13–15), NPV 98(98–98) |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
|
| Bias in definition and measurement |

|
Subject to individual bias |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
|
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
| First Author (Year) | Ho KM (2017) [34] |
| Title | Combining quick Sequential Organ Failure Assessment with plasma lactate concentration is comparable to standard Sequential Organ Failure Assessment score in predicting mortality of patients |
| Journal | Journal of Critical Care |
| Reviewer | RL, KH, LL, MB, CG |
| Study sponsor | Department of Intensive Care Medicine, Royal Perth Hospital |
| Study type | Prospectively Collected Data Retrospective Cohort (8 January–13 Decemeber) |
| Location | Australia |
Participants
|
9549 identified, 2322 analyzed 61% male 57.1 (41–70) All ICU patient during the first hour of admission |
| qSOFA criteria | Respiration rate ≥22 breaths/min, altered mental state (Glasgow Coma Scale score <15), and systolic blood pressure ≤100 mm Hg |
| Primary outcome Other outcomes |
(In)hospital mortality Patients who required invasive mechanical ventilation within 24 h of ICU admission, and a length of ICU stay more than 10 days |
| Results | In-hospital mortality AUC 0.672 (0.638–0.707) |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Database included ICU patients only, Gender imbalance |
| Bias in definition and measurement |

|
|
| Outcome measurement bias |

|
|
| Handling of missing data |

|
|
| Confounding |

|
Identified but not adjusted for |
| Bias of statistics or presentation of result |

|
| First Author (Year) | Hwang SY (2018) [36] |
| Title | Low Accuracy of Positive qSOFA Criteria for Predicting 28-Day Mortality in Critically Ill Septic Patients During the Early Period After Emergency Department Presentation. |
| Journal | Annals of Emergency Medicine |
| Reviewer | RL, CG, KH |
| Study sponsor | Nil |
| Study type | Retrospective cohort study (August 08–September 14) |
| Location | Seoul, S Korea |
Participants
|
1395 56% male 65 (55–73) Patients aged 18 years or older and who received a diagnosis of severe sepsis or septic shock (defined by SIRS) during their ED stay were included in analysis |
| qSOFA criteria | Systolic blood pressure of less than or equal to 100 mmHg, respiratory rate greater than or equal to 22 breaths/min, and altered mentation (GCS < 15 or <Alert on AVPU) |
| Primary outcome Other outcomes |
28-day mortality In-hospital mortality, use of a vasopressor within 24 h after ED presentation, presence of cryptic shock, increase in a SOFA score of 2 points or more from the baseline, ICU admission, and mechanical ventilation |
| Results | 28-day mortality AUC 0.58 (95% CI 0.55 to 0.62) on ED arrival for qSOFA ≥2 |
| Note | Neutropenic patients included |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Severe sepsis/septic shock. Patients not for active treatments were excluded. |
| Bias in definition and measurement |

|
|
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Missing cases excluded |
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
| First Author (Year) | Innocenti F (2018) [37] |
| Title | SOFA score in septic patients: Incremental prognostic value over age, comorbidities, and parameters of sepsis severity. |
| Journal | Internal & Emergency Medicine |
| Reviewer | RL, CG, LL |
| Study sponsor | Nil |
| Study type | Retrospective review (June 08–April 16) |
| Location | ED-HDU |
Participants
|
742 53% male (mean age 75 ± 14) Diagnosis of sepsis, severe sepsis, or septic shock. |
| qSOFA criteria | GCS < 15 or AVPU, others were not defined |
| Primary outcome Other outcomes |
28-day mortality ICU admission |
| Results | qSOFA 0.625, 95%, CI 0.579–0.671 |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Change of definition through time.Sick population. ED HDU patient |
| Bias in definition and measurement |

|
AMS—determined by deduction from notesSepsis was defined by the 2001 definition |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
|
| Confounding |

|
31% mortality |
| Bias of statistics or presentation of result |

|
Statistics unclearDouble-counting MEWS and SOFA in modelling |
| First Author (Year) | Khwannimit B (2017) [38] |
| Title | Comparison of the performance of SOFA, qSOFA and SIRS for predicting mortality and organ failure among sepsis patients admitted to the intensive care unit in a middle-income country. |
| Journal | Journal of Critical Care |
| Reviewer | RL, CG, KH |
| Study sponsor | Research grant of Faculty of Medicine, Prince of Songkla University |
| Study type | Retrospective cohort study (07–16) |
| Location | Thailand |
Participants
|
2350 56.1% male 62 (45–75) 15 years and older who had been diagnosed with sepsis and admitted to a medical intensive care unit (sepsis was defined by the criteria of the international consensus definition of sepsis) Definitions Conference (Sepsis-2) |
| qSOFA criteria | SBP ≤100 mmHg, respiratory rate ≥22 breath/min, and Glasgow Coma Score (GCS) ≤13 |
| Primary outcome Other outcomes |
All-cause hospital mortality ICU mortality and organ failure |
| Results | All-cause hospital mortality AUC 0.814 for qSOFA |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
MICU patients, 15+ years old |
| Bias in definition and measurement |

|
Sepsis 2 definition of sepsis |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
|
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
| First Author (Year) | Kim MW (2017) [39] |
| Title | Mortality prediction using serum biomarkers and various clinical risk scales in community-acquired pneumonia. |
| Journal | Scandinavian Journal of Clinical & Laboratory Investigation |
| Reviewer | RL, CG, KH |
| Study sponsor | Nil |
| Study type | Retrospective chart review (January–Decemeber 14) |
| Location | Seoul Korea |
Participants
|
125 62.4% male 72 years (59.5–80.0) In-patient adults with a diagnosis of Community Acquired Pneumonia (CAP) |
| qSOFA criteria | Respiratory rate of 22/min or greater, altered mentation (AVPU), or systolic blood pressure of 100 mmHg or less |
| Primary outcome Other outcomes |
Evaluate the performance of various biomarkers and other clinical risk scales for predicting 28-day mortality in CAP patients who were admitted to the ED, and to compare the performance of these predictors. |
| Results | 28-day mortality AUC 0.81 for qSOFA ≥2 |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
CAP |
| Bias in definition and measurement |

|
|
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Not identified or addressed |
| Confounding |

|
CAP patients |
| Bias of statistics or presentation of result |

|
Significant amounts of missing data |
| First Author (Year) | Kolditz M (2016) [40] |
| Title | Comparison of the qSOFA and CRB-65 for risk prediction in patients with community-acquired pneumonia |
| Journal | Intensive Care Medicine |
| Reviewer | RL, KH, LL, MB, CG |
| Study sponsor | CAPNETZ was founded by a BMBF Grant (01KI07145) 2001–2011. |
| Study type | Retrospective cohort (Letter) (2 October–15 June) |
| Location | Germany |
Participants
|
9327 analyzed 56% male 63 ICU patients included in a German community-acquired pneumonia database |
| qSOFA criteria | Respiratory rate ≥22/min, systolic blood pressure ≤100 mmHg, pneumonia-related (new-onset) confusion according to the physician’s discretion |
| Primary outcome Other outcomes |
30-day mortality Requirement for mechanical ventilation and/or vasopressor support during hospital admission, and the combination of 30-day mortality and requirement for mechanical ventilation and/or vasopressor |
| Results | In-hospital mortality AUC 0.70 (0.69–0.71) |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Pneumonia database, inclusion bias |
| Bias in definition and measurement |

|
Subject to individual bias |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Missing data excluded from database |
| Confounding |

|
None found |
| Bias of statistics or presentation of result |

|
| First Author (Year) | LeGuen M (2018) [41] |
| Title | Frequency and significance of qSOFA criteria during adult rapid response team reviews: A prospective cohort study. |
| Journal | Resuscitation |
| Reviewer | RL, CG, KH |
| Study sponsor | Nil |
| Study type | prospective observational audit 6 June, 10 July 16 |
| Location | Victoria, Australia |
Participants
|
258 48% male 72 (57–82) Adults requiring Rapid Response Team response |
| qSOFA criteria | Altered mentation (as measured by a GCS <15); Respiratory Rate ≥22/min; SBP ≤100 mmHg |
| Primary outcome Other outcomes |
In-hospital mortality as per the original qSOFA study ICU length of stay more than three days [6], death, or ICU length of stay greater than three days, intensity of ICU supports, and discharge destination. |
| Results | |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
|
| Bias in definition and measurement |

|
|
| Outcome measurement bias |

|
|
| Handling of missing data |

|
10% excluded |
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
Easily misinterpreted |
| First Author (Year) | Moskowitz A (2017) [42] |
| Title | Quick Sequential Organ Failure Assessment and Systemic Inflammatory Response Syndrome Criteria as Predictors of Critical Care Intervention Among Patients With Suspected Infection. |
| Journal | Critical Care Medicine |
| Reviewer | RL, CG, MB |
| Study sponsor | Drs. Moskowitz, Chase, Berg, and Donnino received support for the article research from the National Institutes of Health (NIH). Dr. Moskowitz is funded by a grant from the NIH (2T32HL007374-37). Dr. Chase is funded by a grant from the National Institute of General Medical Sciences (K23 GM101463). Dr. Shapiro received funding from Thermo Fisher, Cheetah Medical, Rapid Pathogen Screening, and Baxter. Dr. Cocchi is funded by a grant from the American Heart Association (15SDG22420010). Dr. Berg is funded by a grant from the National Institute of Heart, Lung and Blood Institute (NIHLBI) (K23HL128814-01A1). Dr. Donnino is funded by a grant from the NIHLBI (1K24HL127101). |
| Study type | Retrospective cohort |
| Location | United States (January 2010 and December 2014) |
Participants
|
24,164 50.9% male (Mean 63.8 (SD 18.1)) Patients admitted to ED with suspected infection (defined by the collection of any microbial cultures and initiation of antibiotics within 24 h of ED triage time |
| qSOFA criteria | Not defined |
| Primary outcome Other outcomes |
“Received CCI” within 48 h of ED triage Nil |
| Results | AUC 0.71 (0.69–0.72) when used to predict the in-hospital mortality |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
|
| Bias in definition and measurement |

|
Unclear definition |
| Outcome measurement bias |

|
Not objective |
| Handling of missing data |

|
|
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
| First Author (Year) | Muller M (2017) [43] |
| Title | Utility of quick sepsis-related organ failure assessment (qSOFA) to predict outcome in patients with pneumonia. |
| Journal | PLoS ONE |
| Reviewer | RL, CG, MB |
| Study sponsor | Nil |
| Study type | Retrospective analysis (June 11–May 13) |
| Location | Switzerland |
Participants
|
527 64.5% male 66 (50–76) Adults (16 years or older) presenting with a diagnosis of pneumonia |
| qSOFA criteria | Glasgow Coma Scale (GCS) of 14 or less, systolic blood pressure of 100 mmHg or less, respiration rate of 22/min or more. |
| Primary outcome Other outcomes |
In-hospital mortality ICU admission rate and length of hospital stay |
| Results | In-hospital mortality AUC 0.58 for qSOFA |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Pneumonia only |
| Bias in definition and measurement |

|
|
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Patients excluded but not explained |
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
Presentation of wrong results from calculations |
| First Author (Year) | Park HK (2017) [44] |
| Title | Quick sequential organ failure assessment compared to systemic inflammatory response syndrome for predicting sepsis in emergency department. |
| Journal | Journal of Critical Care |
| Reviewer | RL, CG, MB |
| Study sponsor | Nil |
| Study type | Retrospective cohort March 07–February 16 |
| Location | Seoul Korea |
Participants
|
1009 45% male (Mean 67.4 ± 17.6) Patients (≥18 years) with a suspected infection that was identified by using a combination of antibiotics (oral or parenteral) and body fluid cultures (blood, urine, cerebrospinal fluid, etc.) |
| qSOFA criteria | respiratory rate ≥22/min, systolic blood pressure ≤100 mm Hg, and altered mentation (all cases except ‘alert’ were judged to have altered mentation) |
| Primary outcome Other outcomes |
Increase of 2 or more SOFA points within 24 h of ED admission In-hospital mortality |
| Results | In-hospital mortality AUC 0.733 for qSOFA |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
|
| Bias in definition and measurement |

|
Retrospective with antibiotic cultures only |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Identified but not addressed |
| Confounding |

|
Retrospective study, time bias |
| Bias of statistics or presentation of result |

|
Calibration unclear |
| First Author (Year) | Peake (2017) [45] |
| Title | Potential Impact of the 2016 Consensus Definitions of Sepsis and Septic Shock on Future Sepsis Research. |
| Journal | Annals of Emergency Medicine |
| Reviewer | RL, CG, LL |
| Study sponsor | Nil |
| Study type | Post hoc analysis of ARISE database (October 08–April 14) |
| Location | Australasia |
Participants
|
1591 59.7/40.3 (Mean 62.9, SD 16.5) SIRS-positive adults |
| qSOFA criteria | ≥22 breaths/min, systolic blood pressure ≤100 mm Hg, Glasgow Coma Scale [GCS] score <15 |
| Primary outcome Other outcomes |
The proportion of patients enrolled with the SIRS-based criteria that met the new Sepsis-3 definitions for qSOFA, sepsis, and septic shock their baseline characteristics; interventions delivered; and outcomes, including mortality, duration of organ support, and ICU, and the hospital length of stay |
| Results | |
| Note | Second analysis of ARISE database Multiple imputation for Sn, Sp, PPV, and NPV |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Retrospective data that included patients with SIRS-based criteria only |
| Bias in definition and measurement |

|
|
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Unclear |
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
| First Author (Year) | Quinten VM (2017) [46] |
| Title | Sepsis patients in the emergency department—Stratification using the Clinical Impression Score, Predisposition, Infection, Response and Organ dysfunction score |
| Journal | European Journal of Emergency Medicine |
| Reviewer | RL, KH, LL, |
| Study sponsor | Not stated |
| Study type | Prospectively Collected Data Retrospective Cohort (August 12–April 14) |
| Location | Netherlands |
Participants
|
193 analyzed 56% male 60 (48–71) Non-traumatic patients with suspected infection or sepsis in the ED |
| qSOFA criteria | Altered mental status, respiratory frequency, and systolic blood pressure. |
| Primary outcome Other outcomes |
ICU admission In-hospital, 28-day and 6-month mortality, indirect admission to the ICU, and length of stay |
| Results | In-hospital mortality AUC 0.823 (0.707–0.939) |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
|
| Bias in definition and measurement |

|
Not defined |
| Outcome measurement bias |

|
Subject to individual bias |
| Handling of missing data |

|
|
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
Number of missing data (that was excluded) is not stated |
| First Author (Year) | Raith EP (2017) [47] |
| Title | Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit |
| Journal | JAMA |
| Reviewer | RL, KH, LL, |
| Study sponsor | Competitive Research Financing of Tampere University Hospital |
| Study type | Retrospective cohort (2000–2015) |
| Location | Australasia |
Participants
|
1,499,753 identified, 184,875 analyzed 55.4% male 62.9 (17.4) ICU patients with infection-related diagnosis |
| qSOFA criteria | A Glasgow Coma Scale of less than 15 (others not stated) |
| Primary outcome Other outcomes |
In-hospital mortality Combination of in-hospital mortality, or an ICU length of stay of three days or longer |
| Result | In-hospital mortality AUC 0.607 (99% CI 0.603–0.611) |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
|
| Bias in definition and measurement |

|
|
| Outcome measurement bias |

|
|
| Handling of missing data |

|
|
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
| First Author (Year) | Rannikko J (2017) [48] |
| Title | Sepsis-related mortality in 497 cases with blood culture-positive sepsis in an emergency department |
| Journal | International Journal of Infectious Diseases |
| Reviewer | RL, KH, LL, |
| Study sponsor | Competitive Research Financing of Tampere University Hospital |
| Study type | Retrospective cohort (March 12–February 14) |
| Location | Finland |
Participants
|
800 identified, 497 analyzed 53% male 68 (58–78) ED patients with positive blood culture results |
| qSOFA criteria | Respiratory rate > 22/min, altered mentation (GCS < 15), and systolic blood pressure < 100 mmHg |
| Primary outcome Other outcomes |
90-day mortality 28-day mortality |
| Results | Patients with missing data and under 18 years old are excluded, sample size 473. 28-day mortality AUC 0.71 (0.67–0.75), Sensitivity 0.65 (0.53–0.76), Specificity 0.77 (0.73–0.81), PPV 0.33 (0.28–0.39), NPV 0.93(0.9–0.95) +LR 2.9 (2.26–3.72), −LR 0.45 (0.32–0.62) |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Blood culture-positive only |
| Bias in definition and measurement |

|
Altered mentation not defined in the original article, contacted author for clarification |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
|
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
Limited statistics in the original paper. However the original author has supplied our team with de-personalized raw data for further data analysis |
| First Author (Year) | Ranzani (2017) [49] |
| Title | New Sepsis Definition (Sepsis-3) And Community-Acquired Pneumonia Mortality—A Validation and Clinical Decision-Making Study |
| Journal | American Journal of Respiratory and Critical Care Medicine |
| Reviewer | RL, CG, LL |
| Study sponsor | Centro de Investigacio’ n Biomedica En Red-Enfermedades Respiratorias and the European Respiratory Society Research Fellowships |
| Study type | Prospectively Collected Data Retrospective Cohort (1996–2015) |
| Location | Barcelona and Valencia |
Participants
|
6874 62.2 Male Mean (66.1 (19)) Clinical diagnosis of CAP |
| qSOFA criteria | ≥22 breaths/min, systolic blood pressure ≤100 mm Hg, altered mental status |
| Primary outcome Other outcomes |
In-hospital mortality In-hospital mortality and/or need for critical support for three or more days, and 30-day mortality |
| Result | In-hospital mortality AUC 0.697 (0.671–0.722) qSOFA >2 Sn 50(45–55), Sp 81 (80–82), PPV 15 (13–17), NPV 96 (96–97), LR+ 2.70 (2.41–3.03), LR- 0.61 (0.55–0.68) |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
CAP patients. Time bias |
| Bias in definition and measurement |

|
Confusion not clearly defined |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
|
| Confounding |

|
Secondary analysis, time |
| Bias of statistics or presentation of result |

|
| First Author (Year) | Seymour CW (2016) [50] |
| Title | Assessment of clinical criteria for sepsis for the third international consensus definitions for sepsis and septic shock (Sepsis-3) |
| Journal | JAMA |
| Reviewer | RL, KH, LL, |
| Study sponsor | National Institutes of Health, the Department of Veterans, the Permanente Medical Group, German Federal Ministry of Education and Research |
| Study type | Retrospective cohort (January 10–Decemeber 12) |
| Location | US and Germany |
Participants
|
1,309,025 identified, 74,453 analyzed 43% male 61 (19) All patients with suspected infection |
| qSOFA criteria | Systolic hypotension (<100 mmHg), tachypnea (>22/min), or altered mentation GCS < 13 |
| Primary outcome Other outcomes |
In-hospital mortality Combination of in-hospital mortality or ICU stay |
| Result | |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Multiple databases used. Potential bias in individual database |
| Bias in definition and measurement |

|
Altered mentation not defined |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
|
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
| First Author (Year) | Siddiqui S (2017) [51] |
| Title | A comparison of pre ICU admission SIRS, EWS and qSOFA scores for predicting mortality and length of stay in ICU |
| Journal | Journal of Critical Care |
| Reviewer | RL, CG, MB |
| Study sponsor | Nil |
| Study type | Retrospective cohort (January–Decemeber 15) |
| Location | Singapore |
Participants
|
58 60% male (Mean 64.4 ± 12.9) All adult ICU or HDU admissions with a presumed diagnosis of ‘sepsis’ |
| qSOFA criteria | Hypotension b 100 SBP, altered consciousness, GCS b 15, and a respiratory rate N 22 bpm |
| Primary outcome Other outcomes |
In-hospital mortality and ICU length of stay Nil |
| Results | Mortality AUC 0.6875 for qSOFA |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Sepsis not defined and unclear |
| Bias in definition and measurement |

|
Sepsis not defined and unclear |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Not stated. Small number |
| Confounding |

|
Not enough information for assessment |
| Bias of statistics or presentation of result |

|
Small number |
| First Author (Year) | Singer AJ (2017) [52] |
| Title | Quick SOFA Scores Predict Mortality in Adult Emergency Department Patients With and Without Suspected Infection |
| Journal | Annals of Emergency Medicine |
| Reviewer | RL, KH, LL, |
| Study sponsor | Nil |
| Study type | Retrospective cohort (14 January–15 March) |
| Location | NY, USA |
Participants
|
67,475 identified, 22,530 analyzed 47% male 54 (21) All ED patients |
| qSOFA criteria | Respiratory rate ≥22 breaths/min, systolic blood pressure ≤100 mm Hg, and altered mental status |
| Primary outcome Other outcomes |
In-hospital mortality Hospital admission, ICU admission, and total hospital length of stay (ED triage to discharge from the hospital) |
| Results | AUC in-hospital mortality 0.76 (95% CI 0.71–0.78), Sen 29% (95% CI 25% to 34%), and spec 97% (95% CI 97% to 97%), respectively, with a NPV of 99% (95% CI 99% to 99%). |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
|
| Bias in definition and measurement |

|
Not stated explicitly, presumably the level of consciousness |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Large number (61.3%) of missing data excluded |
| Confounding |

|
Not stated |
| Bias of statistics or presentation of result |

|
Not enough to judge |
| First Author (Year) | Sterling (2017) [53] |
| Title | The Impact of the Sepsis-3 Septic Shock Definition on Previously Defined Septic Shock Patients. |
| Journal | Critical Care Medicine |
| Reviewer | RL, CG, LL |
| Study sponsor | Dr. Puskarich received support for article research from the National Institutes of Health (NIH), Dr. Guirgis’ institution received funding from the Society of Critical Care Medicine Vision Grant and from National Center for Advancing Translational Sciences through the University of Florida. Dr. Jones receives support through the National Institutes of General Medical Sciences (R01GM103799-01) |
| Study type | Secondary analysis of two previously completed clinical trials |
| Location | Large academic emergency departments in the United States. |
Participants
|
470 (mean 60 ± 16.7) Patients with suspected infection, more than or equal to two systemic inflammatory response syndrome criteria, and systolic blood pressure of less than 90 mm Hg after fluid resuscitation. |
| qSOFA criteria | (respiratory rate ≥ 22 beats/min, altered mental status, or systolic blood pressure (SBP) of ≤ 100 mm Hg) |
| Primary outcome Other outcomes |
In-hospital mortality |
| Results | |
| Note | 57% of patients meeting old definition for septic shock did not meet Sepsis-3 criteria |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Patient defined altered mentation. Sick population, inclusion by SIRS |
| Bias in definition and measurement |

|
Suspected infection and SIRS patients, and sBP less than 90 mmHg |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
|
| Confounding |

|
Secondary analysis |
| Bias of statistics or presentation of result |

|
| First Author (Year) | Szakmany (2018) [54] |
| Title | Defining sepsis on the wards: Results of a multi-centre point-prevalence study comparing two sepsis definitions |
| Journal | Anaesthesia |
| Reviewer | RL, CG, MB |
| Study sponsor | Fiona Elizabeth Agnew Trust and the Welsh Intensive Care Society |
| Study type | Prospective observational study (19 October 2016) |
| Location | Wales |
Participants
|
380 47% male 74 (61–83) Patients in the ED or in an acute in-patient ward setting with suspected or proven infection |
| qSOFA criteria | Systolic blood pressure ≤ 100 mmHg, respiratory rate ≥ 22 breaths/min, and altered mental status (defined as either a Glasgow Coma Scale score ≤ 13 or an Alert Voice Pain Unresponsive scale (AVPU) other than ‘Alert’) |
| Primary outcome Other outcomes |
Mortality within 30 days Presence of organ dysfunction defined by SOFA score > 2 or the presence of ‘severe sepsis’ |
| Results | AUC for 30-day mortality 0.57 (0.49–0.64) p = 0.07, Sen 0.22 (0.14–0.33), Spec 0.89 (0.85–0.92), PPV 0.34 (0.22–0.49), NPV 0.82 (0.77–0.85) |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
NEWS of 3 or more |
| Bias in definition and measurement |

|
Sepsis = qsofa of 2 or more |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
No indication on how it is handled |
| Confounding |

|
Not stated |
| Bias of statistics or presentation of result |

|
Logistic regression not calibrated |
| First Author (Year) | Tusgul (2017) [55] |
| Title | Low sensitivity of qSOFA, SIRS criteria and sepsis definition to identify infected patients at risk of complication in the prehospital setting and at the emergency department triage |
| Journal | Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine |
| Reviewer | RL, CG, LL |
| Study sponsor | Nil |
| Study type | Retrospective cohort |
| Location | Switzerland |
Participants
|
886 52.1% male 80 (69–87) Patients transported by an ambulance crew with criteria fulfilling diagnosis or suspicion of infection |
| qSOFA criteria | SBP ≤100 mmHg, RR ≥22/min, and GCS<15, or altered mental status from baseline as reported by the family |
| Primary outcome Other outcomes |
Predict ICU admission, ICU stay of ≥3 days and mortality at 48 h. |
| Results | ? |
| Note | Pre-hospital |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
|
| Bias in definition and measurement |

|
|
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Small number, excluded |
| Confounding |

|
Only one reviewer reviewed the charts |
| Bias of statistics or presentation of result |

|
| First Author (Year) | Umemura (2017) [56] |
| Title | Assessment of mortality by qSOFA in patients with sepsis outside ICU: A post hoc subgroup analysis by the Japanese Association for Acute Medicine Sepsis Registry Study Group. |
| Journal | Journal of Infection and Chemotherapy |
| Reviewer | RL, CG, MB |
| Study sponsor | Nil |
| Study type | Prospectively Collected Data Retrospective Cohort |
| Location | Japan |
Participants
|
387 59.7% male ? Adults diagnosed with ‘severe sepsis’ as defined in 2003 |
| qSOFA criteria | Altered mental status (Glasgow Coma Scale score of ≤14), systolic blood pressure of less than or equal to 100 mmHg, and a respiratory rate of at least 22 breaths/min |
| Primary outcome Other outcomes |
All-cause in-hospital mortality ? |
| Results | In-hospital mortality AUC 0.615 for qSOFA |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Old definition, “severe sepsis”, time bias |
| Bias in definition and measurement |

|
|
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Not stated, unclear |
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
Little to interpret, logistic regression not calibrated |
| First Author (Year) | Wang, J.Y. (2016) [57] |
| Title | Predictive performance of quick Sepsis-related Organ Failure Assessment for mortality and ICU admission in patients with infection at the ED |
| Journal | American Journal of Emergency Medicine |
| Reviewer | RL, KH, LL, |
| Study sponsor | Nil |
| Study type | Prospectively collected data retrospective cohort (July 15–Decemeber 15) |
| Location | Beijing, China |
Participants
|
516 identified, 477 analyzed 61.8%male 73 (60–79) ED patients with a “clinical” diagnosis of infection |
| qSOFA criteria | Glasgow Coma Scale score of less than or equal to 13, systolic blood pressure less than or equal to 100 mm Hg, and respiratory rate greater than or equal to 22 per minute |
| Primary outcome Other outcomes |
28-day mortality Admission to ICU |
| Results | 28-day mortality AUC 0.666 (95% CI 0.609–0.723), Sen 42.9%, spec 82.6%, PPV 61.8%, NPV 68.8% |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Restrictive inclusion criteria, low number of patients included in study for a 6-month study at a 2000 bed hospital, gender imbalance |
| Bias in definition and measurement |

|
GCS ≤13 |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
|
| Confounding |

|
|
| Bias of statistics or presentation of result |

|
| First Author (Year) | Williams, J.M. (2017) [59] |
| Title | SIRS, qSOFA and organ dysfunction insights from a prospective database of emergency department patients with infection |
| Journal | Chest |
| Reviewer | RL, KH, LL, |
| Study sponsor | Queensland Emergency Medicine Research Foundation |
| Study type | Prospectively collected data retrospective cohort (October 07–May 11) |
| Location | Australia |
Participants
|
8871 analyzed 51.3% male 49 (30–69) ED patients with suspected infection |
| qSOFA criteria | Respiratory rate ≥22 bpm, systolic blood pressure ≤100 mmHg, and Glasgow Coma Score (GCS) ≤13 |
| Primary outcome Other outcomes |
30-day mortality 1-year mortality |
| Results | 30-day mortality AUC 0.78 (95% CI 0.76–0.81) |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
|
| Bias in definition and measurement |

|
GCS ≤13 |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
|
| Confounding |

|
Not stated |
| Bias of statistics or presentation of result |

|
Primary outcome ROC presented in online supplementary material |
| First Author (Year) | Hu X et al. (2017) [35] |
| Title | A multicenter confirmatory study about the precision and practicability of Sepsis-3. [Chinese] |
| Journal | Chin Crit Care Med (Zhonghua Wei Zhong Bing Ji Jiu Yi Xue) |
| Reviewer | RL, KH, LL |
| Study sponsor | National Natural Science Foundation for Young Scientists of China |
| Study type | Retrospective January 15–June 15 |
| Location | Zhejiang, China |
Participants
|
1420 recruited, 329 analyzed 62.6% ? qSOFA-positive ICU patients |
| qSOFA criteria | Not specified |
| Primary outcome Other outcomes |
28-day mortality |
| Results | AUC 0.597 (95%CI 0.524–0.669) |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Sepsis-3 criteria was used to recruit; high variability from hospital to hospital; ICU patients only |
| Bias in definition and measurement |

|
qSOFA was not defined, particularly for altered mentation; unclear time point of qSOFA |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
|
| Confounding |

|
Retrospective, high male %, patient characteristics not included |
| Bias of statistics or presentation of result |

|
Poor and selective presentation of data |
| First Author (Year) | Wang S et al. (2007) [58] |
| Title | Predictive value of four different scoring systems for septic patient outcomes: A retrospective analysis with 311 patients. [Chinese] |
| Journal | Chin Crit Care Med (Zhonghua Wei Zhong Bing Ji Jiu Yi Xue) |
| Reviewer | RL, KH, LL |
| Study sponsor | National Natural Science Foundation for Young Scientists of China |
| Study type | Retrospective July 12–June 16 |
| Location | Chenzhou, China |
Participants
|
311 69.5% 63 ± 17.3 SIRS and suspected infection |
| qSOFA criteria | Not stated |
| Primary outcome Other outcomes |
28-day mortality Mechanical ventilation, LOS ICU |
| Results | qSOFA AUC 0.604 SN 0.4 SP 0.78 |
| Note |
| Risk of Bias |
Author’s Judgment
 Low Risk
Low Risk
 Unclear
Unclear
 High Risk
High Risk
|
Support for Judgment |
| Selection bias |

|
Inclusion criteria: SIRS and suspected infection; only ICU patients |
| Bias in definition and measurement |

|
Altered mentation defined by GCS, but did not specify at what level |
| Outcome measurement bias |

|
|
| Handling of missing data |

|
Patients with missing value excluded, did not report the number of patients excluded |
| Confounding |

|
Male-to-female ratio of 2:1 |
| Bias of statistics or presentation of result |

|
Logistic regression double counting variables Poor presentation of table margin |
Appendix I. In-Hospital Mortality, All Comers vs. Infection
Figure A1.
In-hospital Mortality, All Comers vs. Infection.
Appendix J. In-Hospital Mortality, Recruitment Location
Figure A2.
In-hospital Mortality, Recruitment Location.
Appendix K. In-Hospital Mortality, Altered Mentation
Figure A3.
In-hospital Mortality, Altered Mentation.
Appendix L. In-Hospital mortality, Timing of qSOFA
Figure A4.
In-hospital mortality, Timing of qSOFA.
Author Contributions
Methodology, R.S.L.L., K.K.C.H. and M.B.; validation, C.A.G.; data extraction, C.Y.Y., S.Y.C. and C.C.Y.L.; formal analysis, L.Y.L. and R.S.L.L.; writing—original draft preparation, R.S.L.L.; writing—review and editing, L.Y.L, K.K.C.H., C.A.G.; supervision, C.A.G.; project administration, R.S.L.L.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Torio C.M., Andrews R.M. National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2011: Statistical Brief# 160. [(accessed on 7 June 2018)];2013 Available online: https://www.ncbi.nlm.nih.gov/books/NBK169005/ [PubMed]
- 2.Angus D.C., Linde-Zwirble W.T., Lidicker J., Clermont G., Carcillo J., Pinsky M.R. Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome, and associated costs of care. Crit. Care Med. 2001;29:1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Pfuntner A., Wier L.M., Steiner C. Costs for Hospital Stays in the United States, 2011: Statistical Brief# 168. [(accessed on 7 June 2018)];2013 Available online: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb168-Hospital-Costs-United-States-2011.jsp.
- 4.Levy M.M., Fink M.P., Marshall J.C., Abraham E., Angus D., Cook D., Cohen J., Opal S.M., Vincent J.L., Ramsay G. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Intens. Care Med. 2003;29:530–538. doi: 10.1007/s00134-003-1662-x. [DOI] [PubMed] [Google Scholar]
- 5.Bone R.C., Balk R.A., Cerra F.B., Dellinger R.P., Fein A.M., Knaus W.A., Schein R.M., Sibbald W.J. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. 1992. Chest. 2009;136:e28. doi: 10.1378/chest.101.6.1644. [DOI] [PubMed] [Google Scholar]
- 6.Singer M., Deutschman C.S., Seymour C.W., Shankar-Hari M., Annane D., Bauer M., Bellomo R., Bernard G.R., Chiche J.D., Coopersmith C.M., et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3) JAMA. 2016;315:801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lo R.S., Brabrand M., Kurland L., Graham C.A. Sepsis—Where are the emergency physicians? Eur. J. Emerg. Med. 2016;23:159. doi: 10.1097/MEJ.0000000000000403. [DOI] [PubMed] [Google Scholar]
- 8.Sprung C.L., Schein R.M., Balk R.A. The new sepsis consensus definitions: The good, the bad and the ugly. Intens. Care Med. 2016;42:2024–2026. doi: 10.1007/s00134-016-4604-0. [DOI] [PubMed] [Google Scholar]
- 9.Singer M. The new sepsis consensus definitions (Sepsis-3): The good, the not-so-bad, and the actually-quite-pretty. Intens. Care Med. 2016;42:2027–2029. doi: 10.1007/s00134-016-4600-4. [DOI] [PubMed] [Google Scholar]
- 10.Ferreira F.L., Bota D.P., Bross A., Mélot C., Vincent J.L. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286:1754–1758. doi: 10.1001/jama.286.14.1754. [DOI] [PubMed] [Google Scholar]
- 11.Moher D., Shamseer L., Clarke M., Ghersi D., Liberati A., Petticrew M., Shekelle P., Stewart L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Higgins J.P., Green S., editors. Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons; Hoboken, NJ, USA: 2011. [Google Scholar]
- 13.MedCalc Software bvba. [(accessed on 7 January 2019)]; Available online: http://www.medcalc.org.
- 14.Hayden J.A., Chou R., Hogg-Johnson S., Bombardier C. Systematic reviews of low back pain prognosis had variable methods and results—Guidance for future prognosis reviews. J. Clin. Epidemiol. 2009;62:781–796. doi: 10.1016/j.jclinepi.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 15.Amland R.C., Sutariya B.B. Quick Sequential [Sepsis-Related] Organ Failure Assessment (qSOFA) and St. John Sepsis Surveillance Agent to Detect Patients at Risk of Sepsis: An Observational Cohort Study. Am. J. Med. Qual. 2018;33:50–57. doi: 10.1177/1062860617692034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.April M.D., Aguirre J., Tannenbaum L.I., Moore T., Pingree A., Thaxton R.E., Sessions D.J., Lantry J.H. Sepsis clinical criteria in emergency department patients admitted to an intensive care unit: An external validation study of quick sequential organ failure assessment. J. Emerg. Med. 2017;52:622–631. doi: 10.1016/j.jemermed.2016.10.012. [DOI] [PubMed] [Google Scholar]
- 17.Askim Å., Moser F., Gustad L.T., Stene H., Gundersen M., Åsvold B.O., Dale J., Bjørnsen L.P., Damås J.K., Solligård E. Poor performance of quick-SOFA (qSOFA) score in predicting severe sepsis and mortality—A prospective study of patients admitted with infection to the emergency department. Scand. J. Trauma Resusc. Emerg. Med. 2017;25:56. doi: 10.1186/s13049-017-0399-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boulos D., Shehabi Y., Moghaddas J.A., Birrell M., Choy A., Giang V., Nguyen J., Hall T., Le S. Predictive value of quick Sepsis-Related Organ Failure Scores following sepsis-related Medical Emergency Team calls: A retrospective cohort study. Anaesth. Intens. Care. 2017;45:688–694. doi: 10.1177/0310057X1704500607. [DOI] [PubMed] [Google Scholar]
- 19.Brabrand M., Havshøj U., Graham C.A. Validation of the qSOFA score for identification of septic patients: A retrospective study. Eur. J. Intern. Med. 2016;36:e35–e36. doi: 10.1016/j.ejim.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 20.Burnham J.P., Kollef M.H. qSOFA score: Predictive validity in Enterobacteriaceae bloodstream infections. J. Crit. Care. 2018;43:143–147. doi: 10.1016/j.jcrc.2017.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen Y.X., Wang J.Y., Guo S.B. Use of CRB-65 and quick Sepsis-related Organ Failure Assessment to predict site of care and mortality in pneumonia patients in the emergency department: A retrospective study. Crit. Care. 2016;20:167. doi: 10.1186/s13054-016-1351-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Churpek M.M., Snyder A., Han X., Sokol S., Pettit N., Howell M.D., Edelson D.P. Quick Sepsis-related Organ Failure Assessment, Systemic Inflammatory Response Syndrome, and Early Warning Scores for Detecting Clinical Deterioration in Infected Patients outside the Intensive Care Unit. Am. J. Respir. Crit. Care Med. 2017;195:906–911. doi: 10.1164/rccm.201604-0854OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.De Groot B., Stolwijk F., Warmerdam M., Lucke J.A., Singh G.K., Abbas M., Mooijaart S.P., Ansems A., Cuevas L.E., Rijpsma D. The most commonly used disease severity scores are inappropriate for risk stratification of older emergency department sepsis patients: An observational multi-centre study. Scand. J. Trauma Resusc. Emerg. Med. 2017;25:91. doi: 10.1186/s13049-017-0436-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Donnelly J.P., Safford M.M., Shapiro N.I., Baddley J.W., Wang H.E. Application of the Third International Consensus Definitions for Sepsis (Sepsis-3) Classification: A retrospective population-based cohort study. Lancet Infect. Dis. 2017;17:661–670. doi: 10.1016/S1473-3099(17)30117-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Du X.M., Hu H., Kurbah O.M. Both qSOFA score and bedside plasma lactate are the predictors of mortality for patients with infections in ED. Am. J. Emerg. Med. 2017;35:1381–1382. doi: 10.1016/j.ajem.2017.03.034. [DOI] [PubMed] [Google Scholar]
- 26.Finkelsztein E.J., Jones D.S., Ma K.C., Pabón M.A., Delgado T., Nakahira K., Arbo J.E., Berlin D.A., Schenck E.J., Choi A.M., et al. Comparison of qSOFA and SIRS for predicting adverse outcomes of patients with suspicion of sepsis outside the intensive care unit. Crit. Care. 2017;21:73. doi: 10.1186/s13054-017-1658-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Forward E., Konecny P., Burston J., Adhikari S., Doolan H., Jensen T. Predictive validity of the qSOFA criteria for sepsis in non-ICU inpatients. Intens. Care Med. 2017;43:945–946. doi: 10.1007/s00134-017-4776-2. [DOI] [PubMed] [Google Scholar]
- 28.Freund Y., Lemachatti N., Krastinova E., Van Laer M., Claessens Y.E., Avondo A., Occelli C., Feral-Pierssens A.L., Truchot J., Ortega M., et al. Prognostic accuracy of Sepsis-3 criteria for in-hospital mortality among patients with suspected infection presenting to the emergency department. JAMA. 2017;317:301–308. doi: 10.1001/jama.2016.20329. [DOI] [PubMed] [Google Scholar]
- 29.Giamarellos-Bourboulis E.J., Tsaganos T., Tsangaris I., Lada M., Routsi C., Sinapidis D., Koupetori M., Bristianou M., Adamis G., Mandragos K., et al. Validation of the new Sepsis-3 definitions: Proposal for improvement in early risk identification. Clin. Microbiol. Infect. 2017;23:104–109. doi: 10.1016/j.cmi.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 30.Del Castillo J.G., Julian-Jiménez A., González-Martínez F., Álvarez-Manzanares J., Piñera P., Navarro-Bustos C., de Zarate M.M., Llopis-Roca F., Fernández M.D., Gamazo-Del Rio J., et al. Prognostic accuracy of SIRS criteria, qSOFA score and GYM score for 30-day-mortality in older non-severely dependent infected patients attended in the emergency department. Eur. J. Clin. Microbiol. 2017;36:2361–2369. doi: 10.1007/s10096-017-3068-7. [DOI] [PubMed] [Google Scholar]
- 31.Guirgis F.W., Puskarich M.A., Smotherman C., Sterling S.A., Gautam S., Moore F.A., Jones A.E. Development of a simple sequential organ failure assessment score for risk assessment of emergency department patients with sepsis. J. Intensive Care Med. 2017 doi: 10.1177/0885066617741284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haydar S., Spanier M., Weems P., Wood S., Strout T. Comparison of qSOFA score and SIRS criteria as screening mechanisms for emergency department sepsis. Am. J. Emerg. Med. 2017;35:1730–1733. doi: 10.1016/j.ajem.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 33.Henning D.J., Puskarich M.A., Self W.H., Howell M.D., Donnino M.W., Yealy D.M., Jones A.E., Shapiro N.I. An emergency department validation of the SEP-3 sepsis and septic shock definitions and comparison with 1992 consensus definitions. Ann. Emerg. Med. 2017;70:544–552. doi: 10.1016/j.annemergmed.2017.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ho K.M., Lan N.S. Combining quick Sequential Organ Failure Assessment with plasma lactate concentration is comparable to standard Sequential Organ Failure Assessment score in predicting mortality of patients with and without suspected infection. J. Crit. Care. 2017;38:1–5. doi: 10.1016/j.jcrc.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 35.Hu X., Wu M., Fang Q. A multicenter confirmatory study about precision and practicability of Sepsis-3. Chin. Crit. Care Med. 2017;29:99–105. doi: 10.3760/cma.j.issn.2095-4352.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 36.Hwang S.Y., Jo I.J., Lee S.U., Lee T.R., Yoon H., Cha W.C., Sim M.S., Shin T.G. Low accuracy of positive qSOFA criteria for predicting 28-day mortality in critically ill septic patients during the early period after emergency department presentation. Ann. Emerg. Med. 2018;71:1–9. doi: 10.1016/j.annemergmed.2017.05.022. [DOI] [PubMed] [Google Scholar]
- 37.Innocenti F., Tozzi C., Donnini C., De Villa E., Conti A., Zanobetti M., Pini R. SOFA score in septic patients: Incremental prognostic value over age, comorbidities, and parameters of sepsis severity. Intern. Emerg. Med. 2018;13:405–412. doi: 10.1007/s11739-017-1629-5. [DOI] [PubMed] [Google Scholar]
- 38.Khwannimit B., Bhurayanontachai R., Vattanavanit V. Comparison of the performance of SOFA, qSOFA and SIRS for predicting mortality and organ failure among sepsis patients admitted to the intensive care unit in a middle-income country. J. Crit. Care. 2018;44:156–160. doi: 10.1016/j.jcrc.2017.10.023. [DOI] [PubMed] [Google Scholar]
- 39.Kim M.W., Lim J.Y., Oh S.H. Mortality prediction using serum biomarkers and various clinical risk scales in community-acquired pneumonia. Scand. J. Clin. Lab. Investig. 2017;77:486–492. doi: 10.1080/00365513.2017.1344298. [DOI] [PubMed] [Google Scholar]
- 40.Kolditz M., Scherag A., Rohde G., Ewig S., Welte T., Pletz M. Comparison of the qSOFA and CRB-65 for risk prediction in patients with community-acquired pneumonia. Intens. Care Med. 2016;42:2108–2110. doi: 10.1007/s00134-016-4517-y. [DOI] [PubMed] [Google Scholar]
- 41.LeGuen M., Ballueer Y., McKay R., Eastwood G., Bellomo R., Jones D. Frequency and significance of qSOFA criteria during adult rapid response team reviews: A prospective cohort study. Resuscitation. 2018;122:13–18. doi: 10.1016/j.resuscitation.2017.11.036. [DOI] [PubMed] [Google Scholar]
- 42.Moskowitz A., Patel P.V., Grossestreuer A.V., Chase M., Shapiro N.I., Berg K., Cocchi M.N., Holmberg M.J., Donnino M.W. Quick sequential organ failure assessment and systemic inflammatory response syndrome criteria as predictors of critical care intervention among patients with suspected infection. Crit. Care Med. 2017;45:1813–1819. doi: 10.1097/CCM.0000000000002622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Müller M., Guignard V., Schefold J.C., Leichtle A.B., Exadaktylos A.K., Pfortmueller C.A. Utility of quick sepsis-related organ failure assessment (qSOFA) to predict outcome in patients with pneumonia. PLoS ONE. 2017;12:e0188913. doi: 10.1371/journal.pone.0188913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Park H.K., Kim W.Y., Kim M.C., Jung W., Ko B.S. Quick sequential organ failure assessment compared to systemic inflammatory response syndrome for predicting sepsis in emergency department. J. Crit. Care. 2017;42:12–17. doi: 10.1016/j.jcrc.2017.06.020. [DOI] [PubMed] [Google Scholar]
- 45.Peake S.L., Delaney A., Bailey M., Bellomo R. Potential impact of the 2016 consensus definitions of sepsis and septic shock on future sepsis research. Ann. Emerg. Med. 2017;70:553–561. doi: 10.1016/j.annemergmed.2017.04.007. [DOI] [PubMed] [Google Scholar]
- 46.Quinten V.M., van Meurs M., Wolffensperger A.E., ter Maaten J.C., Ligtenberg J.J. Sepsis patients in the emergency department: Stratification using the Clinical Impression Score, Predisposition, Infection, Response and Organ dysfunction score or quick Sequential Organ Failure Assessment score? Eur. J. Emerg. Med. 2017 doi: 10.1097/MEJ.0000000000000460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Raith E.P., Udy A.A., Bailey M., McGloughlin S., MacIsaac C., Bellomo R., Pilcher D.V. Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit. JAMA. 2017;317:290–300. doi: 10.1001/jama.2016.20328. [DOI] [PubMed] [Google Scholar]
- 48.Rannikko J., Syrjänen J., Seiskari T., Aittoniemi J., Huttunen R. Sepsis-related mortality in 497 cases with blood culture-positive sepsis in an emergency department. Int. J. Infect. Dis. 2017;58:52–57. doi: 10.1016/j.ijid.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 49.Ranzani O.T., Prina E., Menéndez R., Ceccato A., Cilloniz C., Méndez R., Gabarrus A., Barbeta E., Bassi G.L., Ferrer M., et al. New Sepsis Definition (Sepsis-3) and Community-acquired Pneumonia Mortality. A Validation and Clinical Decision-Making Study. Am. J. Respir. Crit. Care Med. 2017;196:1287–1297. doi: 10.1164/rccm.201611-2262OC. [DOI] [PubMed] [Google Scholar]
- 50.Seymour C.W., Liu V.X., Iwashyna T.J., Brunkhorst F.M., Rea T.D., Scherag A., Rubenfeld G., Kahn J.M., Shankar-Hari M., Singer M., et al. Assessment of clinical criteria for sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315:762–774. doi: 10.1001/jama.2016.0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Siddiqui S., Chua M., Kumaresh V., Choo R. A comparison of pre ICU admission SIRS, EWS and q SOFA scores for predicting mortality and length of stay in ICU. J. Crit. Care. 2017;41:191–193. doi: 10.1016/j.jcrc.2017.05.017. [DOI] [PubMed] [Google Scholar]
- 52.Singer A.J., Ng J., Thode H.C., Spiegel R., Weingart S. Quick SOFA Scores Predict Mortality in Adult Emergency Department Patients with and Without Suspected Infection. Ann. Emerg. Med. 2017;69:475–479. doi: 10.1016/j.annemergmed.2016.10.007. [DOI] [PubMed] [Google Scholar]
- 53.Sterling S.A., Puskarich M.A., Glass A.F., Guirgis F., Jones A.E. The impact of the Sepsis-3 septic shock definition on previously defined septic shock patients. Crit. Care Med. 2017;45:1436–1442. doi: 10.1097/CCM.0000000000002512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Szakmany T., Pugh R., Kopczynska M., Lundin R.M., Sharif B., Morgan P., Ellis G., Abreu J., Kulikouskaya S., Bashir K., et al. Defining sepsis on the wards: Results of a multi-centre point-prevalence study comparing two sepsis definitions. Anaesthesia. 2018;73:195–204. doi: 10.1111/anae.14062. [DOI] [PubMed] [Google Scholar]
- 55.Tusgul S., Carron P.N., Yersin B., Calandra T., Dami F. Low sensitivity of qSOFA, SIRS criteria and sepsis definition to identify infected patients at risk of complication in the prehospital setting and at the emergency department triage. Scand. J. Trauma Resusc. Emerg. Med. 2017;25:108. doi: 10.1186/s13049-017-0449-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Umemura Y., Ogura H., Gando S., Kushimoto S., Saitoh D., Mayumi T., Fujishima S., Abe T., Ikeda H., Kotani J., et al. Assessment of mortality by qSOFA in patients with sepsis outside ICU: A post hoc subgroup analysis by the Japanese Association for Acute Medicine Sepsis Registry Study Group. J. Infect. Chemother. 2017;23:757–762. doi: 10.1016/j.jiac.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 57.Wang J.Y., Chen Y.X., Guo S.B., Mei X., Yang P. Predictive performance of quick Sepsis-related Organ Failure Assessment for mortality and ICU admission in patients with infection at the ED. Am. J. Emerg. Med. 2016;34:1788–1793. doi: 10.1016/j.ajem.2016.06.015. [DOI] [PubMed] [Google Scholar]
- 58.Wang S., Li T., Li Y., Zhang J., Dai X. Predictive value of four different scoring systems for septic patient’s outcome: A retrospective analysis with 311 patients. Chin. Crit. Care Med. 2017;29:133–138. doi: 10.3760/cma.j.issn.2095-4352.2017.02.008. [DOI] [PubMed] [Google Scholar]
- 59.Williams J.M., Greenslade J.H., McKenzie J.V., Chu K., Brown A.F., Lipman J. Systemic Inflammatory Response Syndrome, Quick Sequential Organ Function Assessment, and Organ Dysfunction: Insights from a Prospective Database of ED Patients with Infection. Chest. 2017;151:586–596. doi: 10.1016/j.chest.2016.10.057. [DOI] [PubMed] [Google Scholar]
- 60.Rhee C., Kadri S.S., Danner R.L., Suffredini A.F., Massaro A.F., Kitch B.T., Lee G., Klompas M. Diagnosing sepsis is subjective and highly variable: A survey of intensivists using case vignettes. Crit. Care. 2016;20:89. doi: 10.1186/s13054-016-1266-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vincent J.L. The clinical challenge of sepsis identification and monitoring. PLoS Med. 2016;13:e1002022. doi: 10.1371/journal.pmed.1002022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ramar K., Gajic O. Early recognition and treatment of severe sepsis. Am. J. Respir. Crit. Care Med. 2013;188:7–8. doi: 10.1164/rccm.201304-0801ED. [DOI] [PubMed] [Google Scholar]
- 63.Saito T., Rehmsmeier M. The precision-recall plot is more informative than the ROC plot when evaluating binary classifiers on imbalanced datasets. PLoS ONE. 2015;10:e0118432. doi: 10.1371/journal.pone.0118432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Song J.U., Sin C.K., Park H.K., Shim S.R., Lee J. Performance of the quick Sequential (sepsis-related) Organ Failure Assessment score as a prognostic tool in infected patients outside the intensive care unit: A systematic review and meta-analysis. Crit. Care. 2018;22:28. doi: 10.1186/s13054-018-1952-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fernando S.M., Tran A., Taljaard M., Cheng W., Rochwerg B., Seely A.J., Perry J.J. Prognostic accuracy of the quick sequential organ failure assessment for mortality in patients with suspected infection. Ann. Intern. Med. 2018;168:266–275. doi: 10.7326/M17-2820. [DOI] [PubMed] [Google Scholar]
- 66.Maitra S., Som A., Bhattacharjee S. Accuracy of quick Sequential Organ Failure Assessment (qSOFA) score and systemic inflammatory response syndrome (SIRS) criteria for predicting mortality in hospitalized patients with suspected infection: A meta-analysis of observational studies. Clin. Microbiol. Infect. 2018;24:1123–1129. doi: 10.1016/j.cmi.2018.03.032. [DOI] [PubMed] [Google Scholar]
- 67.Christ M., Geier F., Bertsch T., Singler K. Sepsis in emergency medicine. Dtsch. Med. Wochenschr. 2016;141:1074. doi: 10.1055/s-0042-105597. [DOI] [PubMed] [Google Scholar]
- 68.Dickmann P., Scherag A., Coldewey S.M., Sponholz C., Brunkhorst FM., Bauer M. Epistemology in the intensive care unit—What is the purpose of a definition?: Paradigm shift in sepsis research. Der Anaesth. 2017;66:622–625. doi: 10.1007/s00101-017-0315-3. [DOI] [PubMed] [Google Scholar]
- 69.Leidel B.A. The new Sepsis 3 definition—Flop or top? Notf. Rettungsmed. 2017;20:383. doi: 10.1007/s10049-017-0292-8. [DOI] [Google Scholar]
- 70.Gerlach J. The new Sepsis 3 definition—A courageous approach. Notf. Rettungsmed. 2017;20:385–389. doi: 10.1007/s10049-017-0311-9. [DOI] [Google Scholar]
- 71.Julián-Jiménez A., Yañez M.C., del Castillo J.G., Salido-Mota M., Mora-Ordoñez B., Arranz-Nieto M.J., Chanovas-Borras M.R., Llopis-Roca F., Mòdol-Deltell J.M., Muñoz G. Poder pronóstico de mortalidad a corto plazo de los biomarcadores en los ancianos atendidos en Urgencias por infección. Enferm. Infecci. Microbiol. Clín. 2017 doi: 10.1016/j.eimc.2017.11.017. [DOI] [PubMed] [Google Scholar]
- 72.Lebedev N.V., Klimov A.E., Agrba S.B., Gaidukevich E.K. Combined forecasting system of peritonitis outcome. Khirurgiia. 2017;9:33–37. doi: 10.17116/hirurgia2017933-37. [DOI] [PubMed] [Google Scholar]
- 73.Lemachatti N., Freund Y. Sepsis: Définitions et validations. Ann. Fr. Méd. D’urgence. 2017;7:30–34. doi: 10.1007/s13341-017-0715-7. [DOI] [Google Scholar]