Abstract
Autism Spectrum Disorder (ASD) is a category of neurodevelopmental disturbances seriously affecting social skills, to which the scientific community has paid great attention in last decades. To date, their pathogenesis is still unknown, but several studies highlighted the relevance of gene-environment interactions in the onset of ASD. In addition, an immune involvement was seen in a wide number of ASD subjects, leading several researchers to hypothesize a possible common pathogenesis between ASD and immune disturbances, including Atopic Dermatitis (AD). In general, among potential contributing factors, microRNAs (miRNAs), small molecules capable of controlling gene expression and targeting mRNA transcripts, might represent one of the major circulating link, possibly unraveling the connections between neurodevelopmental and immune conditions. Under such premises, we conducted a systematic literature review, under the PRISMA guidelines, trying to define the panel of common miRNAs involved in both ASD and AD. The review retrieved articles published between January 1, 2005, and December 13, 2018, in PubMed, ScienceDirect, PsycARTICLES, and Google Scholar. We found a handful of works dealing with miRNAs in ASD and AD, with the most overlapping dysregulated miRNAs being miR-146 and miR-155. Two possible compounds are abnormally regulated in both ASD and AD subjects, possibly cross-contributing to the interactions between the two disorders, setting the basis to investigate more precisely the possible link between ASD and AD from another, not just clinical, perspective.
Keywords: Allergy, Autistic Disorder, Dermatitis, Genetics, Immunity, MicroRNAs
1. Introduction
Autism spectrum disorder (ASD) is a heterogeneous group of neurodevelopmental disorders characterized by impairments in social interaction and communication and restricted or stereotyped interests and behaviors [1], typically occurring before the fourth year of life [2]. In the last decades, there has been an increased attention of the scientific community towards this group of conditions, with a consequent improvement in the knowledge about this topic, and contextually, a broadening of the diagnostic criteria [3,4].
Nonetheless, ASD is the most heritable among neuropsychiatric disorders, with genetic contributions accounting for around 80% of ASD risk [5,6,7,8,9], and higher risk is seen in siblings of autistic children [10]. Although epidemiological studies provide information on the genetic contribution to ASD, less is known about the putative genes involved or the frequency of specific polymorphisms and variants (single-nucleotide or copy number variants).
Whole-genome and candidate-gene analyses have shown the complex genetic background of ASD, characterized by high individual differences and variability, with many ASD-risk genes involved in synaptic plasticity and gene products modifying synaptic number and strength. In addition to inherited variants, individuals with ASD often carry de novo genetic variants, defined as variants not present in the parental genome and found for the first time in the proband (see [11] for a related original article or [12] for a review on this argument). Such mutated variants affect biological pathways involved in synaptic plasticity and connectivity at different levels. It has been proposed that the interplay of (mainly) inherited rare and (to a lesser extent) de novo variants could be pivotal in the development of ASD [13,14,15], with some genes (e.g., NLRP2, MOGS) surprisingly found to be concerned with ASD and having an established role in the immune system [13]. Indeed, in general, de novo variants have a reduced impact in ASD, explaining below 5% of the genetic variance in the liability to ASD [16].
The multigenic condition of ASD seems also to be dependent on gene-environment interactions; epigenetic mechanisms involving DNA methylation, transcriptional regulations, and post-translational changes in histone proteins, are all relevant to neurodevelopmental processes that can be affected in-utero by maternal lifestyle factors [17]. Furthermore, chemical or heavy metals exposure appears to strongly contribute to ASD development [18,19,20].
Consistently, recent studies reported the clinical association between ASD and atopic disorders, such as asthma or atopic dermatitis (AD) [21,22,23,24], strengthening the link between neurodevelopmental disorders and immune diseases. Together with this possibly speculative evidence, several works hypothesized a fundamental role for the immune system and neuroinflammation in ASD development (see [25] for a review).
In fact, immunity is thought to play a key role in the neurodevelopment of both central and peripheral nervous systems, as it regulates neuronal proliferation, synaptic formation, and plasticity, removes apoptotic neurons, and actively participates in a number of neurological processes [26,27,28,29].
Furthermore, many studies reported an alteration of immune responses in children and adults with ASD, which are more frequently subject to infections, allergies, asthma, dermatitis, and over-reactions to autoimmune disorders [27,30,31,32,33]. As such, some proteins, named alarmins, featuring multiple functions, including the activation of innate immunity and the recruitment of antigen-presenting cells stimulating an adaptive response, have been hypothesized to be suitable biomarkers of inflammation in ASD and possibly used to interfere with the immune system ameliorating symptoms of ASD [34,35].
Thus, in recent times, a clinical association between ASD and inflammatory diseases, including AD, was hypothesized [22,23], and in this regard, the investigation of a possible common genetic basis is critical for the current scientific knowledge.
As evidenced by Billeci and colleagues, AD, defined as a chronic inflammatory disease, puts patients at higher risk of developing one of more of the other atopic conditions, therefore it is considered as the beginning of the so-called “atopic march” [22].
This condition, also determined by a close gene-environment interaction [36], appears to be correlated with a number of mental health conditions, including, according to recent literature, ASD [22].
Among the compounds which could possibly explain this link, up to now hypothesized from a clinical point of view, microRNAs (miRNAs) were recently seen to play a role in several molecular and cellular mechanisms, including neurodevelopment, brain plasticity, and immunity [37,38].
The miRNAs might participate in the pathological process both in neurological conditions, including autism, and in atopic disorders, including AD [39]. The overlapping microRNAs in ASD and AD could therefore allow exploration of the role of genetics in the hypothetical common pathophysiological pathway of these two conditions.
1.1. General Insight into MicroRNAs
It is known that miRNAs are very short (18–25 nucleotides), single-stranded non-coding RNAs, able to control gene expression and to target mRNA transcripts, possibly bringing on their translational degradation or their repression, with particular degrees of complementarity [40]. The targeting of mRNA transcripts by miRNA occurs since one miRNA is able to target a number of mRNA transcripts; conversely, a single mRNA transcript can be targeted by many miRNAs.
Actually, miRNAs have rapidly induced a great interest in humans, being potential biomarkers for diagnostic and prognostic aims [41,42], with the number of classified miRNA increasing to over 2500 potential molecules in the Homo Sapiens genetic makeup [40]. Despite being small molecules not capable of encoding proteins, miRNAs hold important structural, regulatory, and catalytic functions.
The miRNA genes are located in the introns of protein-coding genes or in independent non-coding DNA loci [43], whereas nearly half of the total miRNAs are pooled on chromosomes with a common promoter [44].
The biogenesis of miRNA is extremely complex, consisting of several phases. These include: (i) in the nucleus, the transcription of miRNA genes into primary miRNA transcripts by RNA polymerase II; (ii) the freeing of pre-miRNA hairpin, through the trim of the primary miRNA transcripts by the RNAse III Drosha endonuclease; (iii) the active exportation of the pre-miRNA hairpin out of the nucleus in a process involving the nucleocytoplasmic shuttler Exportin-5; (iv) the final maturation, in the cytoplasm, processed by Dicer RNase III endonuclease, splitting the pre-miRNA into a single-stranded mature miRNA [45]; (v) the binding of the mature miRNA to proteins of the Ago family, and (vi) the assembly of the RNA-induced silencing complex (RISC) together in order to employ its physiological functions.
The mature miRNA, once incorporated into the RISC, induces post-transcriptional gene silencing by binding RISC to be partially complementary to the target mRNA found mainly within the 3’-untranslated region (UTR) [46,47].
Flaws in miRNA expression deeply affect several pathways related to cell regulation, including apoptosis, stress responses, or cell proliferation throughout the human body [48,49,50]. Indeed, a single miRNA could repress around 100 mRNAs, while around 60% of human protein coding-genes are represented by conserved targets of miRNAs, thus a number of mRNA targets are regulated by miRNAs [51].
1.2. MiRNAs Linked to Brain Function
MiRNAs approximately regulate two-thirds of human mRNAs [51], and are as much as 70% expressed in the central nervous system (CNS), including the brain and spinal cord [52,53]. Their changes during childhood are different depending on the affected brain region [54].
In particular, miRNAs are abundant in neurons and glia, often placed at the synaptic level, and able to regulate the structure of the dendritic spine, as happens with miR-134 which reduces spine growth by targeting spine growth-promoting kinase Limk1 [55].
Indeed, dendritic spines are bulges on a dendritic tree of a neuron, composing the post-synaptic termination of a synapse, reflecting—through their structure—the degree of brain maturation, and, somehow, brain plasticity.
Their density is abnormal in several conditions, including schizophrenia (dendritic spines loss) and ASD, the latter featuring an increase in the quantity of spines in specific brain areas [56,57,58,59].
Several other miRNAs are associated with dendritic spine structure, including miR-125b [60], miR-132 [61], miR-137 [62], and miR-138 [63].
Overall, several miRNAs affect brain functions and development, neuronal plasticity, maturation, and differentiation [37,64]. Dysregulation of miRNA expression is particularly frequent within several neurological disorders, including ASD, therefore the association between some common miRNA families and ASD, despite still largely unknown, is nowadays clearer than in the past.
1.3. MiRNAs and Skin Disorders
Recently, much evidence has been published about the role of miRNAs in several cellular processes, including immune response, DNA repair, apoptosis, proliferation, and differentiation [65], but also in morphogenesis, differentiation, wound healing, psoriasis, and AD [66,67,68]. Specifically, AD pathogenesis is also associated with a complex gene-environment interaction, as well as with an alteration of the skin barrier function, and a deregulation of the immune system [69]. Several miRNAs, including miR-146a, miR-155, miR-203, and miR-483–5p, are also differentially expressed in AD and in other immunologic and inflammatory disorders.
2. Materials and Methods
A literature review of the articles published between 1 January 2005, and 13 December 2018, was conducted in PubMed, ScienceDirect, PsycARTICLES, and Google Scholar following the PRISMA guidelines.
2.1. Studies about ASD
The search strategy for this part was as follows: ((“micrornas” [MeSH Terms] OR “micrornas” [All Fields] OR “microrna” [All Fields]) AND ((“autistic disorder” [MeSH Terms] OR (“autistic” [All Fields] AND “disorder” [All Fields]) OR “autistic disorder” [All Fields] OR “autism” [All Fields]) OR (“autism spectrum disorder” [MeSH Terms] OR (“autism” [All Fields] AND “spectrum” [All Fields] AND “disorder” [All Fields]) OR “autism spectrum disorder” [All Fields]))).
2.2. Studies about AD
In this part, the search strategy was as follows: ((“microRNAs” [MeSH Terms]) AND (“skin” [MeSH Terms] OR “dermatitis” [MeSH Terms] OR “urticaria” [MeSH Terms] OR “eczema” [MeSH Terms] OR “hypersensitivity” [MeSH Terms])).
Overall, the search was limited to articles describing studies conducted on humans published in peer-reviewed journals. After having discarded duplicates, the obtained results were sorted by relevance and the most significant works related to ASD and miRNAs and to AD and miRNAs were selected. We will first present the results from the literature review and then discuss the possible associations between miRNAs in ASD and AD according to such findings.
3. Results
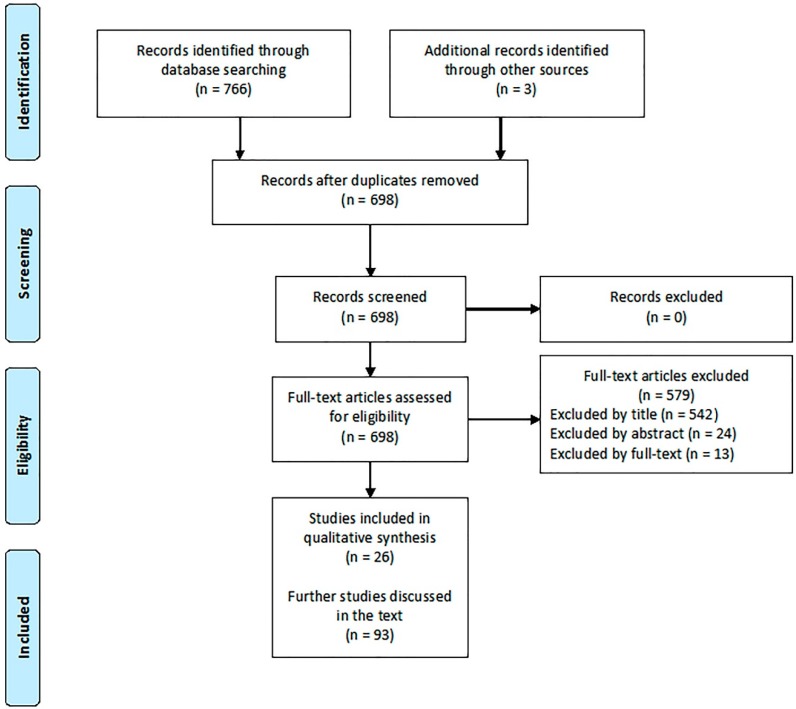
The literature search displayed 26 articles directly related to the relevant topics (Figure 1).
Figure 1.
Study selection.
3.1 Studies about ASD
According to the literature review, a number of miRNAs were found to be associated to ASD (Table 1). Specifically, the most overlapping dysregulated miRNAs appeared to be let-7, miR-19b, miR-23, miR-106, and miR-146.
Table 1.
MicroRNAs directly involved in autism (*: see explanation in the following column).
| Study | N (Case/Control) | Design | Findings | |
|---|---|---|---|---|
| Up-Regulated miRNA | Down-Regulated miRNA | |||
| Abu-Elneel et al. (2008) [70] | 26 (13/13) | Measure of the expression level of 466 human miRNAs from postmortem cerebellar tissue by multiplex real-time PCR, with 377 miRNAs detected and used for further analysis | miR-106a, miR-106b, miR-140, miR-146b, miR-181d, miR-193b, miR-320a, miR-381, miR-432, miR-539, miR-550, miR-652 | miR-7, miR-15a, miR-15b, miR-21, miR-23a, miR-27a, miR-93, miR-95, miR-128, miR-129, miR-132, miR-148b, miR-212, miR-431, miR-484, miR-598 |
| Sarachana et al. (2010) [71] | 14 (5/9) | Lymphoblasts derived from peripheral lymphocytes were obtained; miRNA expression profiling performed by high-throughput miRNA microarray analysis. Differentially expressed miRNAs confirmed by qRT-PCR analysis, putative target genes of two of the confirmed miRNA validated by knockdown and overexpression of the respective miRNAs | miR-16-2, miR-106b, miR-132, miR-133b, miR-136, miR-139, miR-148b, miR-153, miR-182, miR-189, miR-190, miR-199b, miR-211, miR-219, miR-326, miR-367, miR-455, miR-495, miR-518a, miR-520b | miR-23a, miR-23b, miR-25, miR-29b, miR-30e, miR-93, miR-103, miR-107, miR-185, miR-186, miR-191, miR-194, miR-195, miR-205, miR-342, miR-346, miR-376a-AS, miR-451, miR-519c, miR-524 |
| Talebizadeh et al. (2008) [72] | 12 (6/6) | Six subject with Autism Spectrum Disorders (ASD) (3 males, aged 5, 12, and 14 years, and 3 females, aged 6, 11, and 13 years), 6 age- and gender-matched TD controls. Lymphoblastoid cell lines, quantitative PCR, | miR-23a, miR-23b, miR-132, miR-146a, miR-146b, miR-663 | miR-92, miR-320, miR-363 |
| Mundalil Vasu et al. (2014) [73] | 110 (55/55) | 55 ASD (48 males, 6 females, aged 11.29 ± 5.45 years), 55 TD controls (41 males, 14 females, aged 11.3 ± 2.37 years). RNA extracted from serum, mature miRNAs selectively converted into cDNA. The expression of 125 mature miRNAs was compared between pooled control and ASD samples. The differential expression of 14 miRNAs further validated by SYBR Green quantitative PCR of individual samples. Target genes and pathways of miRNAs predicted by DIANA mirPath software | miR-19b-3p, miR-27a-3p, miR-101-3p, miR-106-5p, miR-130a-3p, miR-195b-5p | miR-151a-3p, miR-181b-5p, miR-320a, miR-328, miR-433, miR-489, miR-572, miR-663a |
| Popov et al. (2012) [74] | 55 (30/25) | Thirty ASD (24 males, 6 females, aged 3–20), 25 TD controls (20 males, 5 females, aged 3–20 years). Whole blood collection, analysis of gene expression changes applying LC expression profiling service, using pooled whole blood-derived total RNA samples | miR-486-3p | |
| Seno et al. (2011) [75] | 42 (20/22) | 20 severe ASD (13 males and 7 females), 22 unaffected siblings (19 males and 3 females). Lymphoblastoid cell lines, RNA was extracted and assayed using Illumina gene and miRNA expression arrays. Control quality in BeadStudio (Illumina) | miR-10a, miR-30a, miR-181a, miR-181b, miR-181c, miR-199b-5p, miR-338-3p, miR-486-3p, miR-486-5p, miR-500, miR-502-3p, miR-548 | miR-199a-5p, miR-455-3p, miR-577, miR-656 |
| Mor et al. (2015) [76] | 24 (12/12) | Brain tissue samples taken from postmortem Brodmann’s area 10 | miR-7-5p, miR-19a-3p, miR-19b-3p, miR-21-3p, miR-21-5p, miR-142-3p, miR-142-5p, miR-144-3p, miR-146a-5p, miR-155-5p, miR-219-5p, miR-338-5p, miR-379-5p, miR-451a, miR-494, miR-3168 | miR-34a-5p, miR-92b-3p, miR-211-5p, miR-3960 |
| Ander et al. (2015) [77] | 18 (10/8) | Brain tissue samples taken from postmortem Brodmann’s areas 22, 41, 42 | miR-664-3p, miR-4709-3p, miR-4753-5p | miR-1, miR-297, miR-4742-3p |
| Wu et al. (2016) [78] | 56 (28/28) | Tissue samples taken from postmortem cerebellar cortex, Brodmann area 9 | miR-10a-5p, miR-18b-5p, miR-20b-5p, miR-21-3p, miR-23a-3p, miR-107, miR-129-2-3p, miR-130b-5p, miR-148a-3p, miR-155-5p, miR-218-2-3p, miR-221-3p, miR-223-3p, miR-335-3p, miR-363-3p, miR-424-3p, miR-424-5p, miR-425-3p, miR-449b-5p, miR-450b-5p, miR-484, miR-629-5p, miR-651-5p, miR-708-5p, miR-766-3p, miR-874-3p, miR-887-3p, miR-940, miR-1277-3p, miR-3938, miR-2277-5p, let-7g-3p | miR-204-3p, miR-491-5p, miR-619-5p, miR-3687, miR-5096 |
| Huang et al. (2015) [79] | 40 (20/20) | Peripheral blood sample taken, microarray (5 ASD/5 controls), and quantitative Real-Time PCR (15 ASD/15 controls) | miR-34b-3p, miR-34c-3p, miR-483-5p, miR-494, miR-564, miR-642a-3p, miR-574-5p, miR-575, miR-921, miR-1246, miR-1249, miR-1273c, miR-4270, miR-4299, miR-4436a, miR-4443, miR-4516, miR-4669, miR-4721, miR-4728-5p, miR-4788, miR-5739, miR-6086, miR-6125 | miR-15a-5p, miR-15b-5p, miR-16-5p, miR-19b-3p, miR-20a-5p, miR-92a-3p, miR-103a-3p, miR-195-5p, miR-451a, miR-574-3p, miR-940, miR-1228-3p, miR-3613-3p, miR-3935, miR-4436b-5p, miR-4665-5p, miR-4700-3p, let-7a-5p, let-7d-5p, let-7f-5p |
| Toma et al. (2015) [80] | 1309 (636/673) | Genomic DNA isolated from blood lymphocytes, or from saliva | miR-133b/miR-206 cluster; pooled analysis: miR-133b/miR-206 and miR-17/miR-18a/miR-19a/miR-20a/miR- 19b-1/miR92a-1. |
N/A |
| Hicks et al. (2016) [81] | 45 (24/21) | Salivary samples | miR-7-5p, miR-28-5p, miR-127-3p, miR-140-3p, miR-191-5p, miR-218-5p, miR-335-3p, miR-628-5p, miR-2467-5p, miR-3529-3p | miR-23a-3p, miR-27a-3p, miR-30e-5p, miR-32-5p |
| Nguyen et al. (2016) [82] | 14 (8/6) | Samples taken from olfactory mucosal stem cells and skin fibroblasts or Peripheral Blood Mononuclear Cells. Measured through microarray and quantitative Real-Time PCR validation | miR-146a | miR-221, miR-654-5p, miR-656 |
| Kichukova et al. (2017) [83] | 60 (30/30) | Blood samples. Quantitative Real-Time PCR validation | miR-18b-3p, miR-106b-5p, miR-142-3p, miR-210-5p, miR-365a-3p, miR-374b-5p, miR-619-5p, miR-664a-3p, miR-3620-3p, miR-4489, miR-8052 | hsa-let-7i-3p, miR -15a-5p, miR -20b-3p, miR -29c-5p, miR -96-5p, miR -145-5p, miR -183-5p, miR -193b-3p, miR -197-5p, miR-199a-5p, miR -301a-3p, miR -328-3p, miR -424-5p, miR -486-3p, miR -487b-3p, miR -500a-5p, miR -504-5p, miR -576-5p, miR -587-3p, miR-589-3p, miR -664b-3p, miR -671-3p, miR -3064-5p, miR -3135a, miR -3674, miR -3687, miR-3909, miR -6799-3p, miR -6849-3p |
| Jyonouchi et al. (2017) [84] | 96 (69/27) | Peripheral blood monocytes samples, miRNA expression determined by high-throughput sequencing | hsa-let-7a-1, hsa-let-7a-2, hsa-let-7a-3, hsa-let-7f-1, hsa-let-7f-2, hsa-let-7g, hsa-let-7i, miR-17, miR-26a-2, miR-30b, miR-30c-1, miR-30c-2, miR-98, miR-106b, miR-130a, miR-148a, miR-148b, miR-150, miR-186, miR-301a, miR-374b, miR-494, miR-1248, miR-3607, miR-3609 | hsa-let-7b, miR-15a, miR-15b, miR-16-1, miR-16-2, miR-18a, miR-19a, miR-19b-1, miR-19b-2, miR-20a, miR-21, miR-27a, miR-27b, miR-29a, miR-29b-1, miR-29b-2, miR-29c, miR-30e, miR-93, miR-101-1, miR-101-2, miR-103a-1, miR-103a-2, miR-107, miR-126, miR-142, miR-145, miR-146a, miR-151a, miR-181a-1, miR-181a-2, miR-199b, miR-221, miR-222, miR-320a, miR-376c, miR-409, miR-423, miR-484, miR-625, miR-4433b, miR-5701-1, miR-5701-2 |
| Pagan et al. (2017) [85] | 517 (239/278) * | Post-mortem pineal glands (melatonin) in 9 patients and 22 controls; gut samples (serotonin) in 11 patients and 13 controls; blood platelets from 239 individuals with ASD, their first-degree relatives and 278 controls |
Plasmatic and pineal miR-451 | N/A |
| Nguyen et al. (2018) [86] | 11 (5/6) | Post-mortem analysis of temporal lobe in ASD children and controls, miRNA expression performed using Taqman assay | miR-146a | N/A |
| Yu et al. (2018) [87] | 43 (20/23) | Serum samples, quantitative reverse transcription-PCR to examine miRNAs | miR-486-3p, miR-557 | N/A |
| Williams et al. (2018) [88] | 128 (48/80) * | Blood samples from 48 ASD and 80 parents | miR-873-5p | N/A |
3.2 Studies about AD
A few works studied microRNAs involvement in AD (Table 2). Here, the main dysregulated miRNAs are miR-146, miR-155, and miR-203.
Table 2.
MicroRNAs in atopic dermatitis (*control cohort represented by patients with early-stage mycosis fungoides (MF1)).
| Study | N (Case/Control) | Design | Findings | |
|---|---|---|---|---|
| Up-Regulated miRNA | Down-Regulated miRNA | |||
| Sonkoly et al. (2010) [66] | 47 (18/29) | Skin samples | miR-155 | |
| Lv et al. (2014) [89] | 58 (30/28) | Serum and urine samples | miR-203, miR-483-5p (serum) | miR-203 (urine) |
| Ralfkiaer et al. (2014) [90] | 75 (20/55) * | Skin samples | miR-149, miR-Plus-C1070, miR-205, miR-141, miR-23b, miR-221, miR-27b, miR-203, miR-7b, miR-19b, miR-27a, miR-455-3p, miR-200a, miR-211, miR-23a, miR-214 | miR-181a, miR-342-5p, miR-766, miR-7i, miR-186, miR-342-3p, miR-664, miR-425, miR-9, miR-331-3p, miR-146b-5p, miR-10a, miR-663, miR-937, miR-361-3p, miR-605, miR-146a, miR-940, miR-150, miR-1913, miR-155, miR-302c |
| Rebane et al. (2014) [91] | 18 (9/9) | Skin samples | miR-146a | |
| Ma et al. (2015) [92] | 64 (33/31) | Skin samples | miR-155 | |
| Ding et al. (2016) [93] | 22 (14/8) | Skin samples | miR-148b, miR-152, miR-324 | |
| Yang et al. (2017) [94] | 37 (37/0) | Skin samples | miR-124 | |
Summarizing, the association between ASD and AD revealed a common unbalance for miR-146 and miR-155.
4. Discussion
4.1. The Overlap between Atopy and Autism
Recent data strongly support the clinical association between atopy and ASD [21,22]. It has been widely demonstrated that allergic diseases, especially food allergies, are more frequent among ASD children [95,96].
Notably, a large observational study, comparing 14,812 atopic subjects with 6944 non-atopic subjects, with no lifetime atopic disease, highlighted a strong association between atopy and the risk of developing ASD [97]. Furthermore, autoimmune disorders, including psoriasis (2-fold risk), are also frequently identified in ASD [98].
Beside the robust clinical evidence for the association between atopy and ASD, an intriguing neuroinflammatory hypothesis has been advanced for ASD, involving the disruption of the brain blood barrier induced by inflammatory molecules, brain mast cell activation, and mast cells-microglia interactions [99].
In addition, specific environmental factors, including infectious pathogens, food allergens, toxins, and toxic metals (e.g., aluminum, lead, mercury) may negatively act on neurodevelopment through the alteration of the immune response [100,101,102].
However, the hypothesis that the pro-inflammatory cascade induced by AD could lead to ASD in the presence of genetic susceptibility, is supported by the clinical association and by a shared pattern of cellular damage, with epigenetic changes as a common pathogenic mechanism.
4.2. Role for Overlapping MiRNAs in ASD and AD
The main literature finding concerning miRNAs in AD and ASD is represented by miR-146a. Upregulated in various neurodevelopmental disorders [82], miR-146a was reported to be highly expressed throughout the cortex, hippocampus, and amygdala, key structures for higher cognitive functioning [103]. Furthermore, it was demonstrated that reproducing abnormal miR-146a expression in mouse primary cell cultures leads to impaired neuronal dendritic arborization—producing shriveled dendritic trees with branching points at more proximal levels compared to controls, proving the defective neural connectivity typical of ASD—and to increased astrocyte glutamate uptake capacities [82], in turn modifying fast synaptic transmission at the CNS level. Further, miR-146a, expressed in the developing brain, is enclosed within neurons, with poor expression in the glial lineage in adult mice. However, it generally inhibits the expression of neuron-specific targets, including Nlgn1 and Syt1, preventing glial cells from mistakenly adopting neuron-specific phenotypes.
In addition, the neuron excitation at the cortex is probably affected by miR-146a deregulation through the involvement of potassium two pore domain channel subfamily K member 2 (KCNK2), having a key role in neural excitability and migration at the cortex level of developing mice, a critical issue in ASD.
Furthermore, miR-146a expression contributes to neuroinflammation in the brain of ASD subjects, having a role in immune system regulation.
Its function in the regulation of inflammatory processes could partially fill the gap between ASD (and neurodevelopmental disorders in general) and AD (and atopic conditions in extenso).
It is evident indeed that an increased miR-146a expression is present in the lesional skin of AD patients [104], as it inhibits nuclear factor κ B (NF-κB)-mediated proinflammatory cytokines and chemokines, bringing alleviation of the inflammation directly linked to AD and similar conditions [91].
In AD, during skin inflammation, miR-146a is increased in keratinocytes, controlling chronic inflammatory processes triggered by IFN-γ and the activation of NF-κB. Indeed, the relevance of miR-146a in inflammatory skin disorders is confirmed by evidence from psoriasis research [105]. Furthermore, the expression of miR-146a is strongly dependent on NF-κB, and the miRNA has been shown to suppress the NF-κB signaling pathway through a direct targeting of a number of compounds, including IL-1 receptor–associated kinase 1 (IRAK1), TNF receptor–associated factor 6 [106], v-rel avian reticuloendotheliosis viral oncogene homolog B (RELB) [107], and CARD10 [108].
Moreover, it was discovered that mice with a deficiency of miR-146a develop a late autoimmunity caused by an impaired activation of NF-κB in T cells, and signal transducer and STAT1 activator in regulatory T cells [109].
Of note, previous work demonstrated that both an enhanced opioidergic activity and reduced vitamin D levels could represent shared features of AD [110] and ASD [111], and possibly miR-146a and miR-155 could interact with the genetic milieu in subjects with these disorders. Indeed, both miR-146a and miR-155 have been tested in models of LPS tolerance and miR-146 was able to amplify the severity of morphine-mediated hyper-inflammation [112].
Finally, the regulatory role of miR-146a also occurs at lung alveolar epithelial cells, where the release of IL-8 and CCL5 occurs independently from IL-1β signaling.
Concerning miR-155, its role in ASD is not yet known, whereas in AD it appears to modulate T helper type 17 (Th17) cell differentiation and function [92], and to directly target the suppressor of cytokine signalling-1 (SOCS1) gene, taking part in a negative feedback loop to attenuate cytokine signaling [113]. Interestingly, miR-155 is also linked to inflammation and immunity, thanks to its potent upregulation in immune cell lineages, including lymphocytes, fibroblasts, macrophages, mast cells, and dendritic cells, in turn implicated in the pathogenesis of chronic skin inflammation [114,115,116,117,118,119]. Briefly, miR-155 seems to be also involved in the regulation of T-cell responses through a suppression of cytotoxic T-lymphocyte antigen 4 and by enhancing T-cell proliferation [66]. Its deregulation, seen as increased expression in peripheral CD4 T cells of AD patients, was correlated to disease severity, supporting its role in AD pathogenesis [92].
5. Conclusions
Beyond the clinical evidence [22,23], a possible, yet speculative, role for genetics (miRNAs in particular) can be hypothesized to justify the clinical association between AD and ASD.
However, both miR-146a and 155 appear to be involved in this common pathogenetic pathway, despite the role of the latter still being poorly known. Several other aspects differentiating these diseases remain elusive, including the identification of putative environmental injuries and the complex role of vitamin D in immune and neurologic disorders. Therefore, further studies focusing on the association between vitamin D and opiod receptors in skin and neurologic disorders should investigate the role of target genes for common dysregulated miRNAs, in order to discover specific overlapping features of these conditions.
It remains evident that an inflammatory component is active in both diseases, and the actual data support future applications for miR-146a, both as a biomarker and as a target for therapy.
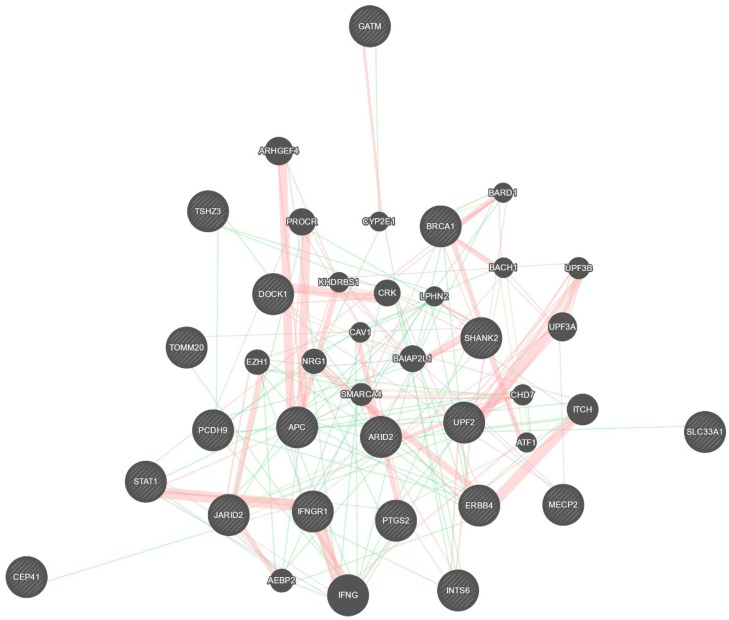
Interestingly, it can be speculated that a deregulation of miR-146a occurs earlier, during embryonic development, thus participating in the development of ASD. Apart from the well-described effect on NF-κB activity and the associated inflammatory pathways strictly linking miR-146a with AD, the deregulation of miR-146a and miR-155 could influence a wide range of their validated targets (Figure 2), essential for brain development and function. However, it remains complex to determine the major source (skin vs brain) of miR-146a and miR-155, and whether they are potentiating each other or having more organ- or disease-specific effects. These aspects warrant future larger longitudinal studies. Finally, a better understanding of the link between ASD and AD might be useful to investigate whether a specific miRNA could act as a biomarker for the risk of developing ASD for patients with AD, and potentially represent a target for ASD prevention.
Figure 2.
Validated targets for miR-146a and miR-155.
Acknowledgment
The authors wish to thank the library management service of the National Research Council of Italy, Pisa Headquarter, for assistance in article retrieval.
Author Contributions
Literature search, A.T., G.B., S.G.; conceptualization, G.B., G.P., S.G.; bias assessment, A.T., L.B., F.S., R.C.; study selection, A.T., G.B., G.P., L.B., S.G.; manuscript drafting, A.T., G.B., G.P., F.S., R.C., S.G.; critical revision and approval of the manuscript, all authors.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; Washington, DC, USA: 2013. [Google Scholar]
- 2.Barger B.D., Campbell J.M., McDonough J.D. Prevalence and onset of regression within autism spectrum disorders: A meta-analytic review. J. Autism Dev. Disord. 2015;43:817–828. doi: 10.1007/s10803-012-1621-x. [DOI] [PubMed] [Google Scholar]
- 3.Chakrabarti S., Fombonne E. Pervasive developmental disorders in preschool children: Confirmation of high prevalence. Am. J. Psychiatry. 2005;162:1133–1141. doi: 10.1176/appi.ajp.162.6.1133. [DOI] [PubMed] [Google Scholar]
- 4.Fombonne E. Editorial: The rising prevalence of autism. J. Child Psychol. Psychiatry. 2018;59:717–720. doi: 10.1111/jcpp.12941. [DOI] [PubMed] [Google Scholar]
- 5.Gaugler T., Klei L., Sanders S.J., Bodea C.A., Goldberg A.P., Lee A.B., Mahajan M., Manaa D., Pawitan Y., Reichert J., et al. Most genetic risk for autism resides with common variation. Nat. Genet. 2014;46:881–885. doi: 10.1038/ng.3039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta A.R., State M.W. Recent advances in the genetics of autism. Biol. Psychiatry. 2007;61:429–437. doi: 10.1016/j.biopsych.2006.06.020. [DOI] [PubMed] [Google Scholar]
- 7.Beaudet A.L. Autism: Highly heritable but not inherited. Nat. Med. 2007;13:534–536. doi: 10.1038/nm0507-534. [DOI] [PubMed] [Google Scholar]
- 8.Colvert E., Tick B., McEwen F., Stewart C., Curran S.R., Woodhouse E., Gillan N., Hallett V., Lietz S., Garnett T., et al. Heritability of Autism Spectrum Disorder in a UK Population-Based Twin Sample. JAMA Psychiatry. 2015;72:415–423. doi: 10.1001/jamapsychiatry.2014.3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sullivan P.F., Daly M.J., O’Donovan M. Genetic architectures of psychiatric disorders: The emerging picture and its implications. Nat. Rev. Genet. 2012;13:537–551. doi: 10.1038/nrg3240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ozonoff S., Young G.S., Carter A., Messinger D., Yirmiya N., Zwaigenbaum L., Bryson S., Carver L.J., Constantino J.N., Dobkins D., et al. Recurrence risk for autism spectrum disorders: A Baby Siblings Research Consortium study. Pediatrics. 2011;128:e488–e495. doi: 10.1542/peds.2010-2825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sanders S.J., He X., Willsey A.J., Ercan-Sencicek A.G., Samocha K.E., Cicek A.E., Murtha M.T., Bal V.H., Bishop S.L., Dong S., et al. Insights into Autism Spectrum Disorder Genomic Architecture and Biology from 71 Risk Loci. Neuron. 2015;87:1215–1233. doi: 10.1016/j.neuron.2015.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vorstman J.A.S., Parr J.R., Moreno-De-Luca D., Anney R.J.L., Nurnberger J.I., Jr., Hallmayer J.F. Autism genetics: Opportunities and challenges for clinical translation. Nat. Rev. Genet. 2017;18:362–376. doi: 10.1038/nrg.2017.4. [DOI] [PubMed] [Google Scholar]
- 13.Al-Mubarak B., Abouelhoda M., Omar A., AlDhalaan H., Aldosari M., Nester M., Alshamrani H.A., El-Kalioby M., Goljan E., Albar R., et al. Whole exome sequencing reveals inherited and de novo variants in autism spectrum disorder: A trio study from Saudi families. Sci Rep. 2017;7:5679. doi: 10.1038/s41598-017-06033-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bourgeron T. From the genetic architecture to synaptic plasticity in autism spectrum disorder. Nat. Rev. Neurosci. 2015;16:551–563. doi: 10.1038/nrn3992. [DOI] [PubMed] [Google Scholar]
- 15.Yuen R.K., Thiruvahindrapuram B., Merico D., Walker S., Tammimies K., Hoang N., Chrysler C., Nalpathamkalam T., Pellecchia G., Liu Y., et al. Whole-genome sequencing of quartet families with autism spectrum disorder. Nat. Med. 2015;21:185–191. doi: 10.1038/nm.3792. [DOI] [PubMed] [Google Scholar]
- 16.Toma C., Torrico B., Hervás A., Valdés-Mas R., Tristán-Noguero A., Padillo V., Maristany M., Salgado M., Arenas C., Puente X.S., et al. Exome sequencing in multiplex autism families suggests a major role for heterozygous truncating mutations. Mol. Psychiatry. 2014;19:784–790. doi: 10.1038/mp.2013.106. [DOI] [PubMed] [Google Scholar]
- 17.Hertz-Picciotto I., Schmidt R.J., Krakowiak P. Understanding environmental contributions to autism: Causal concepts and the state of science. Autism Res. 2018;11:554–586. doi: 10.1002/aur.1938. [DOI] [PubMed] [Google Scholar]
- 18.Meek S.E., Lemery-Chalfant K., Jahromi L.B., Valiente C. A review of gene-environment correlations and their implications for autism: A conceptual model. Psychol. Rev. 2013;120:497–521. doi: 10.1037/a0033139. [DOI] [PubMed] [Google Scholar]
- 19.Gorini F., Muratori F., Morales M.A. The Role of Heavy Metal Pollution in Neurobehavioral Disorders: A Focus on Autism. Rev. J. Autism Dev. Disord. 2014;1:354–372. doi: 10.1007/s40489-014-0028-3. [DOI] [Google Scholar]
- 20.Kalkbrenner A.E., Schmidt R.J., Penlesky A.C. Environmental chemical exposures and autism spectrum disorders: A review of the epidemiological evidence. Curr. Probl. Pediatr. Adolesc. Health Care. 2014;44:277–318. doi: 10.1016/j.cppeds.2014.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tonacci A., Billeci L., Ruta L., Tartarisco G., Pioggia G., Gangemi S. A systematic review of the association between allergic asthma and autism. Minerva Pediatr. 2017;69:538–550. doi: 10.23736/S0026-4946.16.04623-5. [DOI] [PubMed] [Google Scholar]
- 22.Billeci L., Tonacci A., Tartarisco G., Ruta L., Pioggia G., Gangemi S. Association Between Atopic Dermatitis and Autism Spectrum Disorders: A Systematic Review. Am. J. Clin. Dermatol. 2015;16:371–388. doi: 10.1007/s40257-015-0145-5. [DOI] [PubMed] [Google Scholar]
- 23.Billeci L., Tonacci A., Tartarisco G., Ruta L., Pioggia G., Gangemi S. Reply to Fluegge: Association Between Atopic Dermatitis and Autism Spectrum Disorders: A Systematic Review. Am. J. Clin. Dermatol. 2016;17:189–190. doi: 10.1007/s40257-016-0181-9. [DOI] [PubMed] [Google Scholar]
- 24.Heffler E., Allegra A., Pioggia G., Picardi G., Musolino C., Gangemi S. MicroRnas Profiling in Asthma: Potential Biomarkers and Therapeutic Targets. Am. J. Respir. Cell Mol. Biol. 2017;57:642–650. doi: 10.1165/rcmb.2016-0231TR. [DOI] [PubMed] [Google Scholar]
- 25.Bjorklund G., Saad K., Chirumbolo S., Kern J.K., Geier D.A., Geier M.R., Urbina M.A. Immune dysfunction and neuroinflammation in autism spectrum disorder. Acta Neurobiol. Exp. 2016;76:257–268. doi: 10.21307/ane-2017-025. [DOI] [PubMed] [Google Scholar]
- 26.De Jong M., Punt M., De Groot E., Minderaa R.B., Hadders-Algra M. Minor neurological dysfunction in children with autism spectrum disorder. Dev. Med. Child Neurol. 2011;53:641–646. doi: 10.1111/j.1469-8749.2011.03971.x. [DOI] [PubMed] [Google Scholar]
- 27.Wang T.T., Du L., Shan L., Jia F.Y. Research advances in immunological dysfunction in children with autism spectrum disorders. Zhongguo Dang Dai Er Ke Za Zhi. 2014;16:1289–1293. [PubMed] [Google Scholar]
- 28.Jašarević E., Howerton C.L., Howard C.D., Bale T.L. Alterations in the vaginal microbiome by maternal stress are associated with metabolic reprogramming of the offspring gut and brain. Endocrinology. 2015;156:3265–3276. doi: 10.1210/en.2015-1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Young A.M., Chakrabarti B., Roberts D., Lai M.C., Suckling J., Baron-Cohen S. From molecules to neural morphology: Understanding neuroinflammation in autism spectrum condition. Mol. Autism. 2016;7:9. doi: 10.1186/s13229-016-0068-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sakamoto A., Moriuchi H., Matsuzaki J., Motoyama K., Moriuchi M. Retrospective diagnosis of congenital cytomegalovirus infection in children with autism spectrum disorder but no other major neurologic deficit. Brain Dev. 2015;37:200–205. doi: 10.1016/j.braindev.2014.03.016. [DOI] [PubMed] [Google Scholar]
- 31.Li Q., Zhou J.M. The microbiota-gut-brain axis and its potential therapeutic role in autism spectrum disorder. Neuroscience. 2016;324:131–139. doi: 10.1016/j.neuroscience.2016.03.013. [DOI] [PubMed] [Google Scholar]
- 32.Kern J.K., Geier D.A., Sykes L.K., Homme K.G., Geier M.R. Medical conditions in autism and events associated with initial onset of autism. OA Autism. 2014;2:9. [Google Scholar]
- 33.Ruggeri B., Sarkans U., Schumann G., Persico A.M. Biomarkers in autism spectrum disorder: The old and the new. Psychopharmacology. 2014;231:1201–1216. doi: 10.1007/s00213-013-3290-7. [DOI] [PubMed] [Google Scholar]
- 34.Chan J.K., Roth J., Oppenheim J.J., Tracey K.J., Vogl T., Feldmann M., Horwood N., Nanchahal J. Alarmins: Awaiting a clinical response. J. Clin. Investig. 2012;122:2711–2719. doi: 10.1172/JCI62423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Di Salvo E., Casciaro M., Quartuccio S., Genovese L., Gangemi S. Do Alarmins Have a Potential Role in Autism Spectrum Disorders Pathogenesis and Progression? Biomolecules. 2019;9:2. doi: 10.3390/biom9010002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Simpson E.L. Atopic dermatitis: A review of topical treatment options. Curr. Med. Res. Opin. 2010;26:633–640. doi: 10.1185/03007990903512156. [DOI] [PubMed] [Google Scholar]
- 37.Tonelli D.D.P., Pulvers J.N., Haffner C., Murchison E.P., Hannon G.J., Huttner W.B. miRNAs are essential for survival and differentiation of newborn neurons but not for expansion of neural progenitors during early neurogenesis in the mouse embryonic neocortex. Development. 2008;135:3911–3921. doi: 10.1242/dev.025080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dai R., Ahmed S.A. MicroRNA, a new paradigm for understanding immunoregulation, inflammation, and autoimmune diseases. Transl. Res. 2011;157:163–179. doi: 10.1016/j.trsl.2011.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mannucci C., Casciaro M., Minciullo P.L., Calapai G., Navarra M., Gangemi S. Involvement of microRNAs in skin disorders: A literature review. Allergy Asthma Proc. 2017;38:9–15. doi: 10.2500/aap.2017.38.4013. [DOI] [PubMed] [Google Scholar]
- 40.Kozomara A., Griffiths-Jones S. MiRBase: Integrating microRNA annotation and deep-sequencing data. Nucleic Acids Res. 2011;39:D152–D157. doi: 10.1093/nar/gkq1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Radojicic J., Zaravinos A., Vrekoussis T., Kafousi M., Spandidos D.A., Stathopoulos E.N. MicroRNA expression analysis in triple-negative (ER, PR and Her2/neu) breast cancer. Cell Cycle. 2011;10:507–517. doi: 10.4161/cc.10.3.14754. [DOI] [PubMed] [Google Scholar]
- 42.Zaravinos A., Radojicic J., Lambrou G.I., Volanis D., Delakas D., Stathopoulos E.N., Spandidos D.A. Expression of miRNAs involved in angiogenesis, tumor cell proliferation, tumor suppressor inhibition, epithelial-mesenchymal transition and activation of metastasis in bladder cancer. J. Urol. 2012;188:615–623. doi: 10.1016/j.juro.2012.03.122. [DOI] [PubMed] [Google Scholar]
- 43.Krol J., Loedige I., Filipowicz W. The widespread regulation of microRNA biogenesis, function and decay. Nat. Rev. Genet. 2010;11:597–610. doi: 10.1038/nrg2843. [DOI] [PubMed] [Google Scholar]
- 44.Kim V.N., Han J., Siomi M.C. Biogenesis of small RNAs in animals. Nat. Rev. Mol. Cell Biol. 2009;10:126–139. doi: 10.1038/nrm2632. [DOI] [PubMed] [Google Scholar]
- 45.Bartel D.P. MicroRNAs: Genomics, biogenesis, mechanism, and function. Cell. 2004;116:281–297. doi: 10.1016/S0092-8674(04)00045-5. [DOI] [PubMed] [Google Scholar]
- 46.Jansson M.D., Lund A.H. MicroRNA and cancer. Mol. Oncol. 2012;6:590–610. doi: 10.1016/j.molonc.2012.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sabina S., Vecoli C., Borghini A., Guarino R., Andreassi M.G. Analysis of miRNAs Targeting 3’UTR of H2AFX Gene: A General in Silico Approach. Microrna. 2015;4:41–49. doi: 10.2174/2211536604666150227232003. [DOI] [PubMed] [Google Scholar]
- 48.Furdui C. Ionizing radiation: Mechanisms and therapeutics. Antioxid. Redox Signal. 2014;21:218–220. doi: 10.1089/ars.2014.5935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li X.Y., Luo Q.F., Wei C.K., Li D.F., Li J., Fang L. MiRNA-107 inhibits proliferation and migration by targeting CDK8 in breast cancer. Int. J. Clin. Exp. Med. 2014;7:32–40. [PMC free article] [PubMed] [Google Scholar]
- 50.Wojtas B., Ferraz C., Stokowy T., Hauptmann S., Lange D., Dralle H., Musholt T., Jarzab B., Paschke R., Eszlinger M. Differential miRNA expression defines migration and reduced apoptosis in follicular thyroid carcinomas. Mol. Cell. Endocrinol. 2014;388:1–9. doi: 10.1016/j.mce.2014.02.011. [DOI] [PubMed] [Google Scholar]
- 51.Friedman R.C., Farh K.K.H., Burge C.B., Bartel D.P. Most mammalian mRNAs are conserved targets of microRNAs. Genome Res. 2009;19:92–105. doi: 10.1101/gr.082701.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Adlakha Y.K., Saini N. Brain miRNAs and insights into biological functions and therapeutic potential of brain enriched miRNA-128. Mol. Cancer. 2014;13:33. doi: 10.1186/1476-4598-13-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Liu N.K., Xu X.M. MicroRNA in central nervous system trauma and degenerative disorders. Physiol. Genom. 2011;43:571–580. doi: 10.1152/physiolgenomics.00168.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ziats M.N., Rennert O.M. Identification of differentially expressed microRNAs across the developing human brain. Mol. Psychiatry. 2014;19:848–852. doi: 10.1038/mp.2013.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schratt G.M., Tuebing F., Nigh E.A., Kane C.G., Sabatini M.E., Kiebler M., Greenberg M.E. A brain-specific microRNA regulates dendritic spine development. Nature. 2006;439:283–289. doi: 10.1038/nature04367. [DOI] [PubMed] [Google Scholar]
- 56.Hutsler J.J., Zhang H. Increased dendritic spine densities on cortical projection neurons in autism spectrum disorders. Brain Res. 2000;1309:83–94. doi: 10.1016/j.brainres.2009.09.120. [DOI] [PubMed] [Google Scholar]
- 57.Glantz L.A., Lewis D.A. Decreased dendritic spine density on prefrontal cortical pyramidal neurons in schizophrenia. Arch. Gen. Psychiatry. 2000;57:65–73. doi: 10.1001/archpsyc.57.1.65. [DOI] [PubMed] [Google Scholar]
- 58.Kolomeets N.S., Orlovskaya D.D., Rachmanova V.I., Uranova N.A. Ultrastructural alterations in hippocampal mossy fiber synapses in Schizophrenia: A postmortem morphometric study. Synapse. 2005;57:47–55. doi: 10.1002/syn.20153. [DOI] [PubMed] [Google Scholar]
- 59.Sweet R.A., Henteleff R.A., Zhang W., Sampson A.R., Lewis D.A. Reduced dendritic spine density in auditory cortex of subjects with schizophrenia. Neuropsychopharmacology. 2009;34:374–389. doi: 10.1038/npp.2008.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Edbauer D., Neilson J.R., Foster K.A., Wang C.-F., Seeburg D.P., Batterton M.N., Tada T., Dolan B.M., Sharp P.A., Sheng M. Regulation of synaptic structure and function by fmrp-associated micrornas mir-125b and mir-132. Neuron. 2010;68:161. doi: 10.1016/j.neuron.2010.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Impey S., Davare M., Lasiek A., Fortin D., Ando H., Varlamova O., Obrietan K., Soderling T.R., Goodman R.H., Wayman G.A. An activity-induced microRNA controls dendritic spine formation by regulating Rac1-PAK signaling. Mol. Cell. Neurosci. 2010;43:146–156. doi: 10.1016/j.mcn.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Smrt R.D., Szulwach K.E., Pfeiffer R.L., Li X., Guo W., Pathania M., Teng Z.-Q., Luo Y., Peng J., Bordey A., et al. Microrna mir-137 regulates neuronal maturation by targeting ubiquitin ligase mind bomb-1. Stem Cells. 2010;28:1060–1070. doi: 10.1002/stem.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Siegel G., Obernosterer G., Fiore R., Oehmen M., Bicker S., Christensen M., Khudayberdiev S., Leuschner P.F., Busch C.J.L., Kane C., et al. A functional screen implicates microrna-138-dependent regulation of the depalmitoylation enzyme apt1 in dendritic spine morphogenesis. Nat. Cell Biol. 2009;11:705–716. doi: 10.1038/ncb1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Davis T.H., Cuellar T.L., Koch S.M., Barker A.J., Harfe B.D., McManus M.T., Ullian E.M. Conditional loss of dicer disrupts cellular and tissue morphogenesis in the cortex and hippocampus. J. Neurosci. 2008;28:4322–4330. doi: 10.1523/JNEUROSCI.4815-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fiorucci G., Chiantore M.V., Mangino G., Percario Z.A., Affabris E., Romeo G. Cancer regulator microRNA: Potential relevance in diagnosis, prognosis and treatment of cancer. Curr. Med. Chem. 2012;19:461–474. doi: 10.2174/092986712798918798. [DOI] [PubMed] [Google Scholar]
- 66.Sonkoly E., Janson P., Majuri M.-L., Savinko T., Fyhrquist N., Eidsmo L., Xu N., Meisgen F., Wei T., Bradley M., et al. Mir-155 is overexpressed in patients with atopic dermatitis and modulates t-cell proliferative responses by targeting cytotoxic t lymphocyte–associated antigen 4. J. Allergy Clin. Immunol. 2010;126:581–589.e20. doi: 10.1016/j.jaci.2010.05.045. [DOI] [PubMed] [Google Scholar]
- 67.Wei T., Orfanidis K., Xu N., Janson P., Ståhle M., Pivarcsi A., Sonkoly E. The expression of microrna-203 during human skin morphogenesis. Exp. Dermatol. 2010;19:854–856. doi: 10.1111/j.1600-0625.2010.01118.x. [DOI] [PubMed] [Google Scholar]
- 68.Hawkes J.E., Nguyen G.H., Fujita M., Florell S.R., Callis Duffin K., Krueger G.G., O’Connell R.M. microRNAs in psoriasis. J. Investig. Dermatol. 2016;136:365–371. doi: 10.1038/JID.2015.409. [DOI] [PubMed] [Google Scholar]
- 69.Nutten S. Atopic dermatitis: Global epidemiology and risk factors. Ann. Nutr. Metab. 2015;66:8–16. doi: 10.1159/000370220. [DOI] [PubMed] [Google Scholar]
- 70.Abu-Elneel K., Liu T., Gazzaniga F.S., Nishimura Y., Wall D.P., Geschwind D.H., Lao K., Kosik K.S. Heterogeneous dysregulation of microRNAs across the autism spectrum. Neurogenetics. 2008;9:153–161. doi: 10.1007/s10048-008-0133-5. [DOI] [PubMed] [Google Scholar]
- 71.Sarachana T., Zhou R., Chen G., Manji H.K., Hu V.W. Investigation of post-transcriptional gene regulatory networks associated with autism spectrum disorders by microRNA expression profiling of lymphoblastoid cell lines. Genome Med. 2010;2:23. doi: 10.1186/gm144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Talebizadeh Z., Butler M.G., Theodoro M.F. Feasibility and relevance of examining lymphoblastoid cell lines to study role of microRNAs in autism. Autism Res. 2008;1:240–250. doi: 10.1002/aur.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mundalil Vasu M., Anitha A., Thanseem I., Suzuki K., Yamada K., Takahashi T., Wakuda T., Iwata K., Tsujii M., Sugiyama T., et al. Serum microRNA profiles in children with autism. Mol. Autism. 2014;5:40. doi: 10.1186/2040-2392-5-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Popov N.T., Madjirova N.P., Minkov I.N., Vachev T.I. Micro RNA HSA-486-3P Gene Expression Profiling in the Whole Blood of Patients with Autism. Biotechnol. Biotechnol. Equip. 2012;26:3385–3388. doi: 10.5504/BBEQ.2012.0093. [DOI] [Google Scholar]
- 75.Weber F., Teresi R.E., Broelsch C.E., Frilling A., Eng C. A limited set of human microRNA is deregulated in follicular thyroid carcinoma. J. Clin. Endocrinol. Metab. 2006;91:3584–3591. doi: 10.1210/jc.2006-0693. [DOI] [PubMed] [Google Scholar]
- 76.Mor M., Nardone S., Sams D.S., Elliott E. Hypomethylation of miR-142 promoter and upregulation of microRNAs that target the oxytocin receptor gene in the autism prefrontal cortex. Mol. Autism. 2015;6:46. doi: 10.1186/s13229-015-0040-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ander B.P., Barger N., Stamova B., Sharp F.R., Schumann C.M. Atypical miRNA expression in temporal cortex associated with dysregulation of immune, cell cycle, and other pathways in autism spectrum disorders. Mol. Autism. 2015;6:37. doi: 10.1186/s13229-015-0029-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wu Y.E., Parikshak N.N., Belgard T.G., Geschwind D.H. Genome-wide, integrative analysis implicates microRNA dysregulation in autism spectrum disorder. Nat. Neurosci. 2016;19:1463–1476. doi: 10.1038/nn.4373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Huang F., Long Z., Chen Z., Li J., Hu Z., Qiu R., Zhuang W., Tang B., Xia K., Jiang H. Investigation of gene regulatory networks associated with autism spectrum disorder based on mirna expression in china. PLoS ONE. 2015;10:e0129052. doi: 10.1371/journal.pone.0129052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Toma C., Torrico B., Hervás A., Salgado M., Rueda I., Valdés-Mas R., Buitelaar J.K., Rommelse N., Franke B., Freitag C., et al. Common and rare variants of microRNA genes in autism spectrum disorders. World J. Biol. Psychiatry. 2015;16:376–386. doi: 10.3109/15622975.2015.1029518. [DOI] [PubMed] [Google Scholar]
- 81.Hicks S.D., Ignacio C., Gentile K., Middleton F.A. Salivary miRNA profiles identify children with autism spectrum disorder, correlate with adaptive behavior, and implicate ASD candidate genes involved in neurodevelopment. BMC Pediatr. 2016;16:52. doi: 10.1186/s12887-016-0586-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nguyen L.S., Lepleux M., Makhlouf M., Martin C., Fregeac J., Siquier-Pernet K., Philippe A., Feron F., Gepner B., Rougeulle C., et al. Profiling olfactory stem cells from living patients identifies mirnas relevant for autism pathophysiology. Mol. Autism. 2016;7 doi: 10.1186/s13229-015-0064-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kichukova T.M., Popov N.T., Ivanov I.S., Vachev T.I. Profiling of Circulating Serum MicroRNAs in Children with Autism Spectrum Disorder using Stem-loop qRT-PCR Assay. Folia Med. 2017;59:43–52. doi: 10.1515/folmed-2017-0009. [DOI] [PubMed] [Google Scholar]
- 84.Jyonouchi H., Geng L., Streck D.L., Dermody J.J., Toruner G.A. MicroRNA expression changes in association with changes in interleukin-1ß/interleukin10 ratios produced by monocytes in autism spectrum disorders: Their association with neuropsychiatric symptoms and comorbid conditions (observational study) J. Neuroinflamm. 2017;14:229. doi: 10.1186/s12974-017-1003-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pagan C., Goubran-Botros H., Delorme R., Benabou M., Lemière N., Murray K., Amsellem F., Callebert J., Chaste P., Jamain S., et al. Disruption of melatonin synthesis is associated with impaired 14-3-3 and miR-451 levels in patients with autism spectrum disorders. Sci. Rep. 2017;7:2096. doi: 10.1038/s41598-017-02152-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Nguyen L.S., Fregeac J., Bole-Feysot C., Cagnard N., Iyer A., Anink J., Aronica E., Alibeu O., Nitschke P., Colleaux L., et al. Role of miR-146a in neural stem cell differentiation and neural lineage determination: Relevance for neurodevelopmental disorders. Mol. Autism. 2018;9:38. doi: 10.1186/s13229-018-0219-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yu D., Jiao X., Cao T., Huang F. Serum miRNA expression profiling reveals miR-486-3p may play a significant role in the development of autism by targeting ARID1B. Neuroreport. 2018;29:1431–1436. doi: 10.1097/WNR.0000000000001107. [DOI] [PubMed] [Google Scholar]
- 88.Williams S.M., An J.Y., Edson J., Watts M., Murigneux V., Whitehouse A.J.O., Jackson C.J., Bellgrove M.A., Cristino A.S., Claudianos C., et al. An integrative analysis of non-coding regulatory DNA variations associated with autism spectrum disorder. Mol. Psychiatry. 2018 doi: 10.1038/s41380-018-0049-x. [DOI] [PubMed] [Google Scholar]
- 89.Lv Y., Qi R., Xu J., Di Z., Zheng H., Huo W., Zhang L., Chen H., Gao X. Profiling of serum and urinary micrornas in children with atopic dermatitis. PLoS ONE. 2014;9:e115448. doi: 10.1371/journal.pone.0115448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ralfkiaer U., Lindahl L.M., Litman T., Gjerdrum L.M., Ahler C.B., Gniadecki R., Marstrand T., Fredholm S., Iversen L., Wasik M.A., et al. MicroRNA expression in early mycosis fungoides is distinctly different from atopic dermatitis and advanced cutaneous T-cell lymphoma. Anticancer Res. 2014;34:7207–7217. [PubMed] [Google Scholar]
- 91.Rebane A., Runnel T., Aab A., Maslovskaja J., Rückert B., Zimmermann M., Plaas M., Kärner J., Treis A., Pihlap M., et al. Microrna-146a alleviates chronic skin inflammation in atopic dermatitis through suppression of innate immune responses in keratinocytes. J. Allergy Clin. Immunol. 2014;134:836–847.e11. doi: 10.1016/j.jaci.2014.05.022. [DOI] [PubMed] [Google Scholar]
- 92.Ma L., Xue H.B., Wang F., Shu C.M., Zhang J.H. MicroRNA-155 may be involved in the pathogenesis of atopic dermatitis by modulating the differentiation and function of T helper type 17 (Th17) cells. Clin. Exp. Immunol. 2015;181:142–149. doi: 10.1111/cei.12624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ding Y., Shao X., Li X., Zhai Y., Zhang Y., Wang S., Fang H. Identification of candidate genes in atopic dermatitis based on bioinformatic methods. Int. J. Dermatol. 2016;55:791–800. doi: 10.1111/ijd.13291. [DOI] [PubMed] [Google Scholar]
- 94.Yang Z., Zeng B., Wang C., Wang H., Huang P., Pan Y. MicroRNA-124 alleviates chronic skin inflammation in atopic eczema via suppressing innate immune responses in keratinocytes. Cell. Immunol. 2017;319:53–60. doi: 10.1016/j.cellimm.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 95.Jyonouchi H. Autism spectrum disorders and allergy: Observation from a pediatric allergy/immunology clinic. Exp. Rev. Clin. Immunol. 2010;6:397–411. doi: 10.1586/eci.10.18. [DOI] [PubMed] [Google Scholar]
- 96.Bakkaloglu B., Anlar B., Anlar F.Y., Oktem F., Pehlivantürk B., Unal F., Ozbesler C., Gökler B. Atopic features in early childhood autism. Eur. J. Paediatr. Neurol. 2008;12:476–479. doi: 10.1016/j.ejpn.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 97.Chen M.-H., Su T.-P., Chen Y.-S., Hsu J.-W., Huang K.-L., Chang W.-H., Chen T.-J., Pan T.-L., Bai Y.-M. Is atopy in early childhood a risk factor for adhd and asd? a longitudinal study. J. Psychosom. Res. 2014;77:316–321. doi: 10.1016/j.jpsychores.2014.06.006. [DOI] [PubMed] [Google Scholar]
- 98.Zerbo O., Leong A., Barcellos L., Bernal P., Fireman B., Croen L.A. Immune mediated conditions in autism spectrum disorders. Brain Behav. Immun. 2015;46:232–236. doi: 10.1016/j.bbi.2015.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Theoharides T.C. Is a subtype of autism an allergy of the brain? Clin. Ther. 2013;35:584–591. doi: 10.1016/j.clinthera.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 100.Shaw C.A., Seneff S., Kette S.D., Tomljenovic L., Oller J.W., Jr., Davidson R.M. Aluminum-induced entropy in biological systems: Implications for neurological disease. J. Toxicol. 2014;2014:491316. doi: 10.1155/2014/491316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Verlaet A.A., Noriega D.B., Hermans N., Savelkoul H.F. Nutrition, immunological mechanisms and dietary immunomodulation in ADHD. Eur. Child Adolesc. Psychiatry. 2014;23:519–529. doi: 10.1007/s00787-014-0522-2. [DOI] [PubMed] [Google Scholar]
- 102.Adams J.B., Baral M., Geis E., Mitchell J., Ingram J., Hensley A., Zappia I., Newmark S., Gehn E., Rubin R.A., et al. The severity of autism is associated with toxic metal body burden and red blood cell glutathione levels. J. Toxicol. 2009;2009:1–7. doi: 10.1155/2009/532640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lukiw W.J., Zhao Y., Cui J.G. An NF-kappaB-sensitive micro RNA-146a-mediated inflammatory circuit in Alzheimer disease and in stressed human brain cells. J. Biol. Chem. 2008;283:31315–31322. doi: 10.1074/jbc.M805371200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kim J.E., Kim J.S., Cho D.H., Park H.J. Molecular Mechanisms of Cutaneous Inflammatory Disorder: Atopic Dermatitis. Int. J. Mol. Sci. 2016;17:1234. doi: 10.3390/ijms17081234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Srivastava A., Nikamo P., Lohcharoenkal W., Li D., Meisgen F., Xu Landén N., Ståhle M., Pivarcsi A., Sonkoly E. MicroRNA-146a suppresses IL-17-mediated skin inflammation and is genetically associated with psoriasis. J. Allergy Clin. Immunol. 2017;139:550–561. doi: 10.1016/j.jaci.2016.07.025. [DOI] [PubMed] [Google Scholar]
- 106.Taganov K.D., Boldin M.P., Chang K.J., Baltimore D. NF-kappaB-dependent induction of microRNA miR-146, an inhibitor targeted to signaling proteins of innate immune responses. Proc. Natl. Acad. Sci. USA. 2006;103:12481–12486. doi: 10.1073/pnas.0605298103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Etzrodt M., Cortez-Retamozo V., Newton A., Zhao J., Ng A., Wildgruber M., Romero P., Wurdinger T., Xavier R., Geissmann F., et al. Regulation of monocyte functional heterogeneity by mir-146a and relb. Cell Rep. 2012;1:317–324. doi: 10.1016/j.celrep.2012.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Crone S., Jacobsen A., Federspiel B., Bardram L., Krogh A., Lund A.H., Friis-Hansen L. Microrna-146a inhibits g protein-coupled receptor-mediated activation of nf-κb by targeting card10 and cops8 in gastric cancer. Mol. Cancer. 2012;11:71. doi: 10.1186/1476-4598-11-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Zhao J.L., Rao D.S., O’Connell R.M., Garcia-Flores Y., Baltimore D. MicroRNA-146a acts as a guardian of the quality and longevity of hematopoietic stem cells in mice. Elife. 2013;2:e00537. doi: 10.7554/eLife.00537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kanda N., Hau C.S., Tada Y., Sato S., Watanabe S. Decreased serum LL-37 and vitamin D3 levels in atopic dermatitis: Relationship between IL-31 and oncostatin M. Allergy. 2012;67:804–812. doi: 10.1111/j.1398-9995.2012.02824.x. [DOI] [PubMed] [Google Scholar]
- 111.Pioggia G., Tonacci A., Tartarisco G., Billeci L., Muratori F., Ruta L., Gangemi S. Autism and lack of d3 vitamin: A systematic review. Res. Autism Spectr. Disord. 2014;8:1685–1698. doi: 10.1016/j.rasd.2014.09.003. [DOI] [Google Scholar]
- 112.Banerjee S., Meng J., Das S., Krishnan A., Haworth J., Charboneau R., Zeng Y., Ramakrishnan S., Roy S. Morphine induced exacerbation of sepsis is mediated by tempering endotoxin tolerance through modulation of miR-146a. Sci. Rep. 2013;3:1977. doi: 10.1038/srep01977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Lu L.-F., Thai T.-H., Calado D.P., Chaudhry A., Kubo M., Tanaka K., Loeb G.B., Lee H., Yoshimura A., Rajewsky K., et al. Foxp3-dependent microrna155 confers competitive fitness to regulatory t cells by targeting socs1 protein. Immunity. 2009;30:80–91. doi: 10.1016/j.immuni.2008.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Song L., Lin C., Wu Z., Gong H., Zeng Y., Wu J., Li M., Li J. Mir-18a impairs dna damage response through downregulation of ataxia telangiectasia mutated (atm) kinase. PLoS ONE. 2011;6:e25454. doi: 10.1371/journal.pone.0025454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Sand M., Skrygan M., Georgas D., Sand D., Gambichler T., Altmeyer P., Bechara F.G. The miRNA machinery in primary cutaneous malignant melanoma, cutaneous malignant melanoma metastases and benign melanocytic nevi. Cell Tissue Res. 2012;350:119–126. doi: 10.1007/s00441-012-1446-0. [DOI] [PubMed] [Google Scholar]
- 116.Sonkoly E., Ståhle M., Pivarcsi A. MicroRNAs: Novel regulators in skin inflammation. Clin. Exp. Dermatol. 2008;33:312–315. doi: 10.1111/j.1365-2230.2008.02804.x. [DOI] [PubMed] [Google Scholar]
- 117.Xiao C., Rajewsky K. MicroRNA control in the immune system: Basic principles. Cell. 2009;136:26–36. doi: 10.1016/j.cell.2008.12.027. [DOI] [PubMed] [Google Scholar]
- 118.Lu T.X., Rothenberg M.E. Diagnostic, functional, and therapeutic roles of microRNA in allergic diseases. J. Allergy Clin. Immunol. 2013;132:3–13. doi: 10.1016/j.jaci.2013.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Rebane A., Akdis C.A. MicroRNAs: Essential players in the regulation of inflammation. J. Allergy Clin. Immunol. 2013;132:15–26. doi: 10.1016/j.jaci.2013.04.011. [DOI] [PubMed] [Google Scholar]