Abstract
Very few patients with a biochemical failure after radical prostatectomy respond to prostatic bed irradiation. In this setting, 68Ga-PSMA PET/CT seems to be a useful tool for the detection of lesions remaining occult to conventional imaging work-up, changing the treatment strategy in a significant percentage of patients. we report the case of a patient in whom the PSMA PET allowed orientation of the SBRT. To date the patient has no recurrence.
Introduction
Only about 60% of patients with a biochemical failure after radical prostatectomy respond to prostatic bed irradiation.1 In this setting, 68Ga-PSMA PET/CT (Prostate-specific membrane antigen) seems to be a useful tool for the detection of lesions remaining occult to conventional imaging work-up,2 changing the treatment strategy in a significant percentage of patients.3
Case description
A sixty-four year old man with a PSA of 6 μg/L underwent in 2011 a radical prostatectomy for a Gleason 6, pT2cNxR0 prostate adenocarcinoma. PSA became undetectable until January 2014. In December 2014, with a PSA level of 0, 17 μg/L and a negative MRI of the pelvis and the prostatic bed, the patient was referred for classical external beam radiotherapy (EBRT). In 33 sessions, 66Gy were delivered to the prostatic bed. However, PSA levels continued to rise after radiotherapy (RT) with values of 0,21 μg/L and 0,28μg/L at one and four months, respectively. The patient remained totally asymptomatic. The multidisciplinary urological tumor board proposed a 68Ga-PSMA PET/CT (Fig. 1). This revealed a single positive pre-sacral lymphnode, which was confirmed on pelvic MRI. As this lesion was located outside the previous radiation field, a stereotactic body salvage RT (SBRT: 30 Gy/3 fractions) was performed using a tri-modality fusion of PET/CT, MRI and CT for RT Planning (Fig. 2). One month later, the patient was strictly asymptomatic and PSA had gone down to 0,19 μg/L. PSA further decreased to 0,09 μg/L and 0,06 μg/L at 5 and 8 months post-RT, respectively. Finally, PSA became undetectable one year after salvage RT (Fig. 3).
Fig. 1.
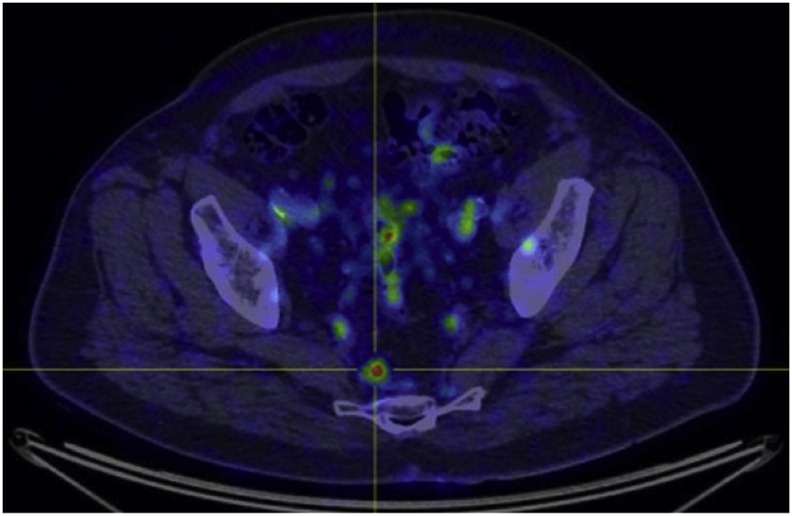
68Ga-PSMA PET/CT axial.
Fig. 2.
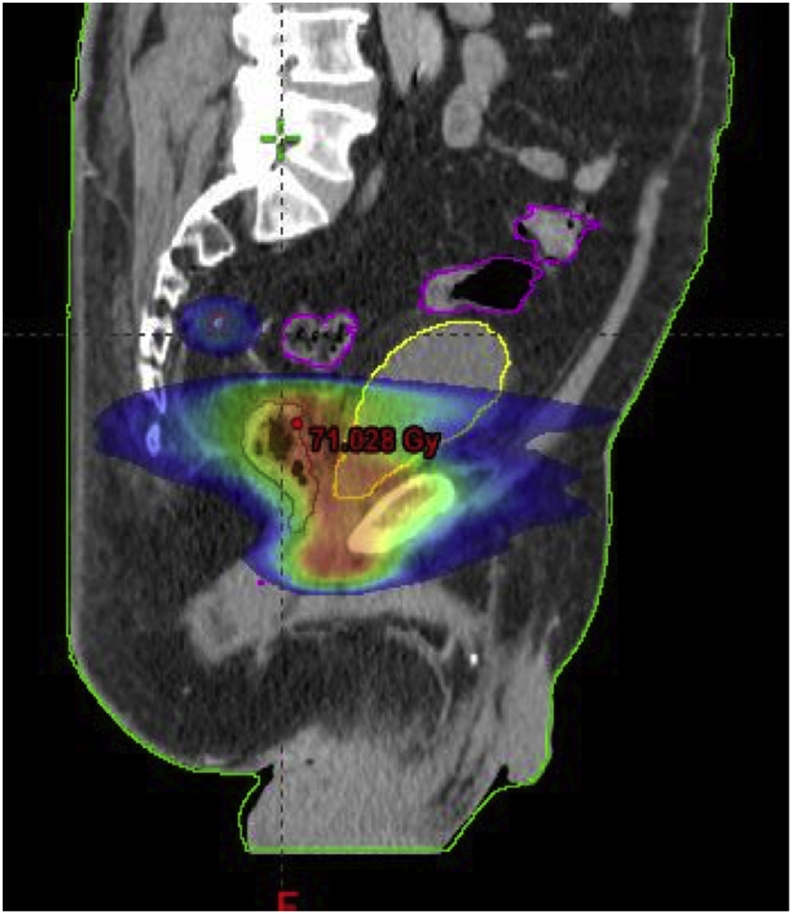
Plan summation of EBRT and SBRT treatment.
Fig. 3.
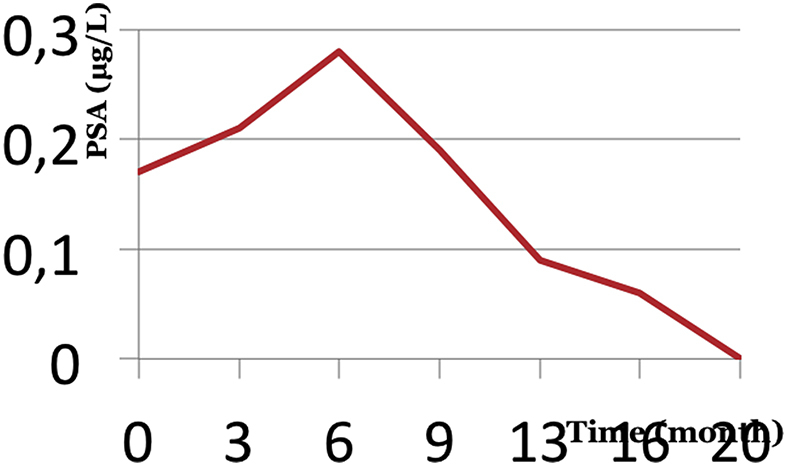
PSA evolution.
Discussion
About 30% of patients will present a biochemical relapse after radical prostatectomy for adenocarcinoma of the prostate.4 Unfortunately, conventional imaging work-up (Thoraco-abdominal CT-Scan, Bone Scan and/or pelvic MRI) is usually negative due to its low sensitivity at low PSA values. Prostatic bed irradiation is considered the standard treatment for those patients. However, about 40% of these recurrences will not be cured by this local radiation. The possibility of a relapse elsewhere, i.e. outside the conventional radiation field, has to be taken into consideration.
In the early 2000s, metabolic imaging appeared. The best known is 18F-fluorodeoxyglucose (18F-FDG). It has been a mainstay of the extension assessment of several cancers however prostate cancer is not hungry for 18F-FDG. Thus, in the context of the biochemical recurrence of prostate cancer, the most used and most studied agent was PET/CT-choline-11C. Compared to standard treatment (CT scan and 99mTc bone scan) it showed increased sensitivity for lymph node and bone metastases. The sensitivity of 11C-choline-CT to PET/CT seems limited in patients with low PSA values. In this context, 68Ga-PSMA PET/CT has shown to be a useful tool in the detection of small bone or lymph node lesions even at very low PSA levels.5 For a PSA between 0.2 and 0.5 ng/ml, the detection rate varies from 15 to 58%. In addition, for Albisinni and Al, PET PSMA changed the therapeutic strategy for nearly 76% of patients.3 This might be of particular interest as we increase the possibilities of detecting 3 or less extra-prostatic lesions (oligo-metastatic disease) where local treatment with SBRT can be delivered, delaying invalidating systemic hormonal treatment up to 38 months. As such, SBRT allows for a less toxic, yet noninvasive approach, with a progression-free survival of about 21 months.
Conclusions
68Ga-PSMA PET/CT might be an interesting tool for early detection and RT guidance of small recurrences after radical prostatectomy for prostate cancer, delaying the use of systemic therapy.
Regulations
All authors have no conflict of interest. We obtained the consent of all patients included in this work. The authors state that they have obtained the approval of the ethics committee.
Author’s contributions
A.S; A. D; R.S: Wrote the paper.
A.M; A.A; A.P: Corrected the article.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.eucr.2019.01.014.
Contributor Information
A. Slaoui, Email: amineslaoui05@gmail.com.
A. Desmet, Email: antoine.desmet@bordet.be.
S. Regragui, Email: souhailr7@gmail.com.
A. Mesfioui, Email: a.mesfioui@yahoo.fr.
A. Ameur, Email: ahmed.ameur@yahoo.fr.
A. Peltier, Email: alexandre.peltier@bordet.be.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Caire Arthur A., Sun Leon, Ode Oludotun. Delayed prostate-specific antigen recurrence after radical prostatectomy: how to identify and what are their clinical outcomes? Urology. 2009 Sep;74(3):643–647. doi: 10.1016/j.urology.2009.02.049. [DOI] [PubMed] [Google Scholar]
- 2.Afshar-Oromieh A., Avtzi E., Giesel F.L. The diagnostic value of PET/CT imaging with the (68)Ga-labelled PSMA ligand HBED-CC in the diagnosis of recurrent prostate cancer. Eur J Nucl Med Mol Imaging. 2015 Feb;42(2):197–209. doi: 10.1007/s00259-014-2949-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Albisinni S., Artigas C., Aoun F. Clinical impact of 68Ga-prostate-specific membrane antigen (PSMA) positron emission tomography/computed tomography (PET/CT) in patients with prostate cancer with rising prostate-specific antigen after treatment with curative intent: preliminary analysis of a multidisciplinary approach. BJU Int. 2017 Aug;120(2):197–203. doi: 10.1111/bju.13739. [DOI] [PubMed] [Google Scholar]
- 4.Boorjian S.A., Karnes R.J., Crispen P.L., Rangel L.J., Bergstralh E.J., Blute M.L. Radiation therapy after radical prostatectomy: impact on metastasis and survival. J Urol. 2009 Dec;182(6):2708–2714. doi: 10.1016/j.juro.2009.08.027. [DOI] [PubMed] [Google Scholar]
- 5.Eiber M., Maurer T., Souvatzoglou M. Evaluation of Hybrid 68Ga-PSMA Ligand PET/CT in 248 Patients with Biochemical Recurrence After Radical Prostatectomy. J Nucl Med. 2015 May;56(5):668–674. doi: 10.2967/jnumed.115.154153. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


