Abstract
Background
Although long working hours have been shown to be associated with the onset of cardiometabolic diseases, the clinical risk factor profile associated with long working hours remains unclear. We compared the clinical risk profile between people who worked long hours and those who reported being never exposed to long hours.
Methods
A cross-sectional study in 22 health screening centres in France was based on a random population-based sample of 75 709 participants aged 18–69 at study inception in 2012–2016 (the CONSTANCES study). The data included survey responses on working hours (never, former or current exposure to long working hours), covariates and standardised biomedical examinations including anthropometry, lung function, blood pressure and standard blood-based biomarkers.
Results
Among men, long working hours were associated with higher anthropometric markers (Body Mass Index, waist circumference and waist:hip ratio), adverse lipid levels, higher glucose, creatinine, white blood cells and higher alanine transaminase (adjusted mean differences in the standardised scale between the exposed and unexposed 0.02–0.12). The largest differences were found for Body Mass Index and waist circumference. A dose–response pattern with increasing years of working long hours was found for anthropometric markers, total cholesterol, glucose and gamma-glutamyltransferase. Among women, long working hours were associated with Body Mass Index and white blood cells.
Conclusion
In this study, men who worked long hours had slightly worse cardiometabolic and inflammatory profile than those who did not work long hours, especially with regard to anthropometric markers. In women, the corresponding associations were weak or absent.
Keywords: blood pressure, diabetes, endocrinology, occupational health, preventive medicine
Introduction
Current guidelines for the prevention of chronic diseases such as myocardial infarction, stroke and diabetes emphasise the importance of maintaining healthy levels of cardiometabolic risk factors such as body weight, blood pressure, cholesterol and glucose.1 2 These guidelines also acknowledge psychosocial factors as potential contributors to cardiometabolic diseases.1 2 One of these, working long hours, is common in the USA, Europe and Asia.3–5
Large collaborative meta-analyses of individual participant data from observational cohort studies have found long working hours to be associated with an increased risk of cardiovascular disease, particularly stroke, and type 2 diabetes (the latter among employees with low socioeconomic position (SEP)).6–8 Studies have also confirmed behavioural risk factors as potential pathways, showing associations between long working hours and smoking,8 risky alcohol use9 and physical inactivity.8 10 In contrast, evidence on the clinical risk profile of people who work long hours is scarce and inconsistent. The Whitehall II study of British civil servants observed no consistent associations between long working hours and cardiometabolic factors such as blood pressure, lipid levels or systemic inflammation.8 Some studies have found an association with self-reported hypertension10–12 while others have reported no association,13 and some further studies have found the risk of hypertension to be lower among individuals who work long hours than among those who work standard 40 hours work weeks.14 15 The evidence is also mixed with regard to metabolic syndrome (an indication of multiple cardiometabolic risk factors) and includes both positive and null findings.16 17 Similarly, studies focusing on overweight and Body Mass Index (BMI) have shown positive associations,8 18–20 no association19–21 and a lower risk of weight gain among individuals who work long hours.15 One limitation in many of these studies is that they rely on self-reported data or data on treated diseases, and many of them have limited statistical power due to small sample sizes, which may lead to imprecise effect estimates, a high likelihood of observing an association by chance and a reduced opportunity to reliably detect small and moderate associations.
To obtain more robust evidence, we examined the association between long working hours and clinically assessed risk markers for chronic diseases, using a large dataset of more than 75 000 French men and women. By carefully assessing exposure, its frequency and duration, we were able to differentiate those never exposed from those formerly or currently exposed and examine potential dose–response patterns in the association. In addition, we assessed associations with several risk factors that have not been examined in relation to long working hours, such as lung function, indicators of liver and kidney function, white and red cell count, and blood clotting (platelets). We also examined whether the association between long working hours and risk markers is similar among men and women and among different socioeconomic groups.
Methods
Participants and procedure
The French CONSTANCES is a population-based cohort study that serves as an open epidemiological research infrastructure.22 The cohort is made up of French adults affiliated with the General Health Insurance Fund in France. This fund covers about 85% of the French population and includes salaried workers (professionally active or retired) aged 18–69 at study inception in 2012–2016. All confidentiality, safety and security procedures were approved by the French legal authorities. The study was carried out in 22 health screening centres across principal regions of France. Of the randomly invited population in the selected catchment areas with stratification according to unequal response probabilities, 7% agreed to participate in the survey and undergo a clinical health examination. Of the 99 924 participants in 2012–2016, 90 607 (91%) provided data on working hours, and of them, 88 009 (97%) also provided data on SEP. A total of 76 486 (87% of those) had data on all other covariates (smoking, alcohol use, physical activity, depressive symptoms and chronic disease), and of those, a maximum of 75 709 (96%) provided data on clinical measurements.
The CONSTANCES Cohort project has been approved by the authorisation of the National Data Protection Authority (Commission nationale de l’informatique et des libertés—CNIL). CNIL verified that before inclusion, clear information is provided to the eligible subjects (presentation of CONSTANCES, type of data to be collected, ability to refuse to participate, informed consent, etc).
Measures
Long working hours were elicited by the following survey question: “Do you have or have you had a daily working time (excluding travel) of more than 10 hours on at least 50 days per year?” with yes/no response options. Of those responding yes, the timing of exposure was requested (starting and ending years of participant’s exposure). We were able to record up to three episodes, and from this information, we determined a total dose of exposure (in years) and whether the participant was formerly (yes/no) or currently (yes/no) exposed.
Risk markers were assessed during a health examination, which was standardised according to standard operating procedures in order to guarantee high-quality physiological data despite unequal conditions (see details23). We calculated BMI from weight and height measurements (weight kg/height m2). We measured waist circumference and hip circumference and calculated waist:hip ratio. Systolic and diastolic blood pressure was measured after 5 min rest with a 2 min break between measurements. The highest value was used for analyses. We calculated pulse pressure as systolic minus diastolic blood pressure. Lung function was assessed by spirometry, which was performed with three measures each of FVC and FEV. For both of these, we used the highest of the three measurements.24
Participants were instructed to fast for 12 hours before the blood test, which was taken between 8:00 and 10:00. Valid lipid and glucose values require a minimum of 8 hours of fasting, which 71 375 (94%) participants with clinical data adhered to. Laboratory tests included blood glucose, lipids (total cholesterol (TC), high-density lipoprotein (HDL) and triglycerides (TG)). Low-density lipoprotein (LDL) was derived from TC, HDL and TG as follows: TC−HDL−(TG/2.2). Gamma-glutamyltransferase (gamma GT) and alanine transaminase (ALT) were indicators of liver function, and blood creatinine was an indicator of kidney function. Other indicators were counts of white blood cells, haemoglobin and platelets.
Covariates included sociodemographic characteristics: self-reported sex, age and SEP. SEP was based on occupational grade, which was further classified into high, intermediate and low; and other/not specified, according to the national socioeconomic nomenclature (‘Professions et catégories sociales’) of the French national statistics office.25 High SEP included executive managers and professionals; intermediate SEP included intermediate professions in education, health, civil service and administration, technicians, foremen and supervisors. Low SEP inlcuded employees (eg, office or commercial employee, child minder, duty officer), farmers, craftsmen and manual workers. The following risk factors were based on survey responses: smoking (never, former, current), physical activity (regular sports activity for 2 hours or more per week vs less) and alcohol consumption, which was based on the 10-item Alcohol Use Disorders Identification Test (AUDIT) survey.26 27 Alcohol use was further categorised into four groups: abstinence; no alcohol abuse or dependence; alcohol abuse (AUDIT score 8–12 for men, 7–11 for women); alcohol dependence (AUDIT score >12 for men, >11 for women). We used the Center for Epidemiological Studies Depression Scale to assess the presence of depressive symptoms.28 Information on chronic somatic disease (yes/no) was based on participants’ self-reported doctor-diagnosed diseases (angina pectoris, myocardial infarction, stroke, lower limb arteritis, other cardiovascular disease, thyroid disease, diabetes, hypercholesterolemia, hypertriglyceridemia, other endocrine disorder, chronic bronchitis, asthma, inflammatory arthritis, other osteoarticular disorder and cancer).
Statistical analyses
We found a skewed distribution of triglycerides, glucose, creatinine, gamma GT, ALT and white blood cell count, and thus logarithmically transformed the values. All values were then standardised (mean 0, SD 1) to allow comparison between the strength of association with long working hours.
We performed multivariable-adjusted analyses, comparing the mean value of each outcome for participants who were formerly or currently exposed to long working hours, setting ‘never exposed’ as the reference group. We further examined the length of exposure among those currently in full-time jobs, exposed to long working hours and aged >35 years (to allow a long exposure to all), again comparing the mean values of each outcome with those among participants never exposed to long working hours. Mean differences and their 95% CIs were computed using the SAS V.9.4 general linear model (genmod) procedure.
We analysed men and women separately and adjusted the models for age, socioeconomic position, smoking, alcohol use, physical activity, depressive symptoms and chronic disease. We performed analyses of spirometry both with and without adjustment for smoking, and analyses of ALT and gamma GT both with and without adjustment for alcohol use. In other sensitivity analyses, we excluded participants with chronic disease and stratified the data by socioeconomic group.
Results
As shown in table 1, participants currently exposed to long working hours were younger, whereas those formerly exposed were older. Both exposure groups included more men and people with a high socioeconomic position. The currently exposed were more often current smokers while the formerly exposed were more often former smokers. The currently exposed also had a higher prevalence of both alcohol abuse and dependence than the other groups, and were more often physically inactive. The formerly exposed had a higher prevalence of chronic somatic disease and depressive symptoms than the never and currently exposed whereas participants who currently worked long hours were less likely to report chronic disease. We conducted a multivariable adjusted binary logistic regression analysis with current versus never exposed to long hours as the outcome and found that the following covariates remained significant after mutual adjustment; younger age, male sex, higher SEP, former and current smoking, alcohol abuse and dependence, lower physical activity, depressive symptoms and lower prevalence of self-reported chronic somatic disease (online supplementary table 1).
Table 1.
Characteristics of the CONSTANCES study participants stratified by exposure to long working hours
| Exposure to long working hours | ||||
| All (n=90 607) | Never (n=66 996) | Former (n=13 359) | Current (n=10 252) | |
| Age (mean, SD) | 48.2 (13.4) | 48.3 (13.5) | 52.4 (12.8) | 42.1 (10.9) |
| Sex (n, %) | ||||
| Male | 42 358 (47) | 28 054 (42) | 8089 (61) | 6215 (61) |
| Female | 48 249 (53) | 38 942 (58) | 5270 (39) | 4037 (39) |
| Socioeconomic position (n, %) | ||||
| Low | 32 527 (37) | 26 032 (40) | 4260 (33) | 2235 (22) |
| Intermediate | 25 296 (29) | 19 705 (30) | 3461 (27) | 2130 (21) |
| High | 25 539 (29) | 15 768 (24) | 4598 (35) | 5173 (51) |
| Other/not specified | 4647 (5) | 3470 (5) | 654 (5) | 523 (5) |
| Smoking (n, %) | ||||
| Never | 40 188 (45) | 30 991 (47) | 4813 (37) | 4384 (43) |
| Former | 27 278 (31) | 19 445 (30) | 5020 (38) | 2813 (28) |
| Current | 21 471 (24) | 15 247 (23) | 3318 (25) | 2906 (29) |
| Alcohol use (n, %) | ||||
| Abstinence | 3940 (5) | 3174 (5) | 469 (4) | 297 (3) |
| No abuse or dependence | 62 216 (74) | 46 635 (75) | 8970 (72) | 6611 (68) |
| Abuse | 13 995 (17) | 9579 (15) | 2234 (18) | 2182 (22) |
| Dependence | 4267 (5) | 2841 (5) | 768 (6) | 658 (7) |
| Physical activity (sports) | ||||
| Less than 2 hours/week | 58 359 (66) | 42 967(65) | 8497 (65) | 6895 (68) |
| 2 hours or more/week | 30 611 (34) | 22 792 (35) | 4598 (35) | 3221 (32) |
| Depressive symptoms | ||||
| No | 65 743 (77) | 48 572 (78) | 9409 (75) | 7762 (79) |
| Yes | 19 132 (23) | 14 026 (22) | 3062 (25) | 2044 (21) |
| Chronic somatic disease | ||||
| No | 55 099 (61) | 40 848 (61) | 7143 (53) | 7108 (69) |
| Yes | 35 508 (39) | 26 148 (39) | 6216 (47) | 3144 (31) |
jech-2018-210943supp001.pdf (110.4KB, pdf)
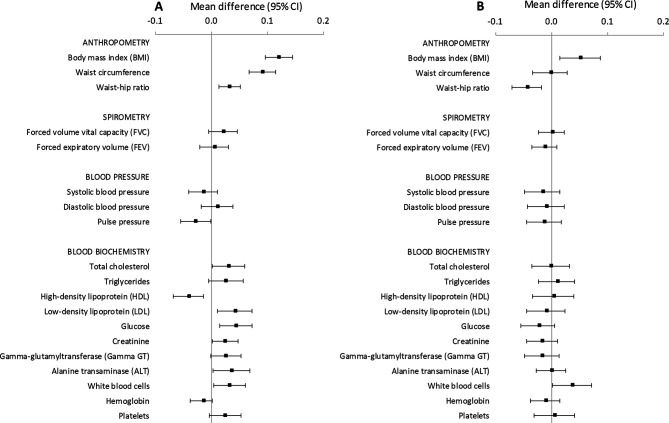
The multivariable adjusted mean differences in the clinical factors of men and women are presented in figure 1 and online supplementary tables 2 and 3. Men who currently worked long hours had higher BMI, larger waist circumference and waist:hip ratio, higher total and LDL cholesterol, lower HDL cholesterol, higher glucose, creatinine, ALT and white blood cell count levels than the never exposed (also illustrated in figure 1A). The strongest association was found for BMI, with a standardised mean difference of 0.12, followed by waist circumference (0.09), whereas all other significant mean differences ranged between 0.02 and 0.04. Among women (online supplementary table 3 and figure 1B), the only significant differences between currently and never exposed were in BMI (mean difference 0.05), white blood cells (mean difference 0.04), and smaller waist:hip ratio (mean difference 0.04). When the analyses were conducted with adjustment for age, sex and SEP only, the estimates were largely similar. The results for spirometry, ALT and gamma GT were almost similar both with and without adjustment for smoking and alcohol use, correspondingly. When we adjusted ALT for BMI among men, the association attenuated to non-significant (p=0.25). Similarly, the associations between current exposure to long working hours and glucose attenuated to non-significant after adjustment for BMI (p=0.40).
Figure 1.
Mean difference in clinical risk markers (standardised values) comparing participants currently exposed with those never exposed to long working hours, adjusted for age, socioeconomic position, smoking, alcohol use, physical activity, depressive symptoms and chronic disease: (A) men; (B) women.
jech-2018-210943supp003.pdf (25.1KB, pdf)
Compared with the never-exposed men, results among the formerly exposed men were to a great extent similar to those obtained among currently exposed men, except for total cholesterol, LDL and creatinine, which were not associated with former long working hours, and triglycerides, which was associated with former but not current long working hours (online supplementary table 2). Among women, former exposure to long hours was associated with higher BMI, waist circumference, waist:hip ratio and triglycerides, lower systolic and diastolic blood pressure, and lower HDL cholesterol when compared with never-exposed women (online supplementary table 3).
jech-2018-210943supp002.pdf (24.7KB, pdf)
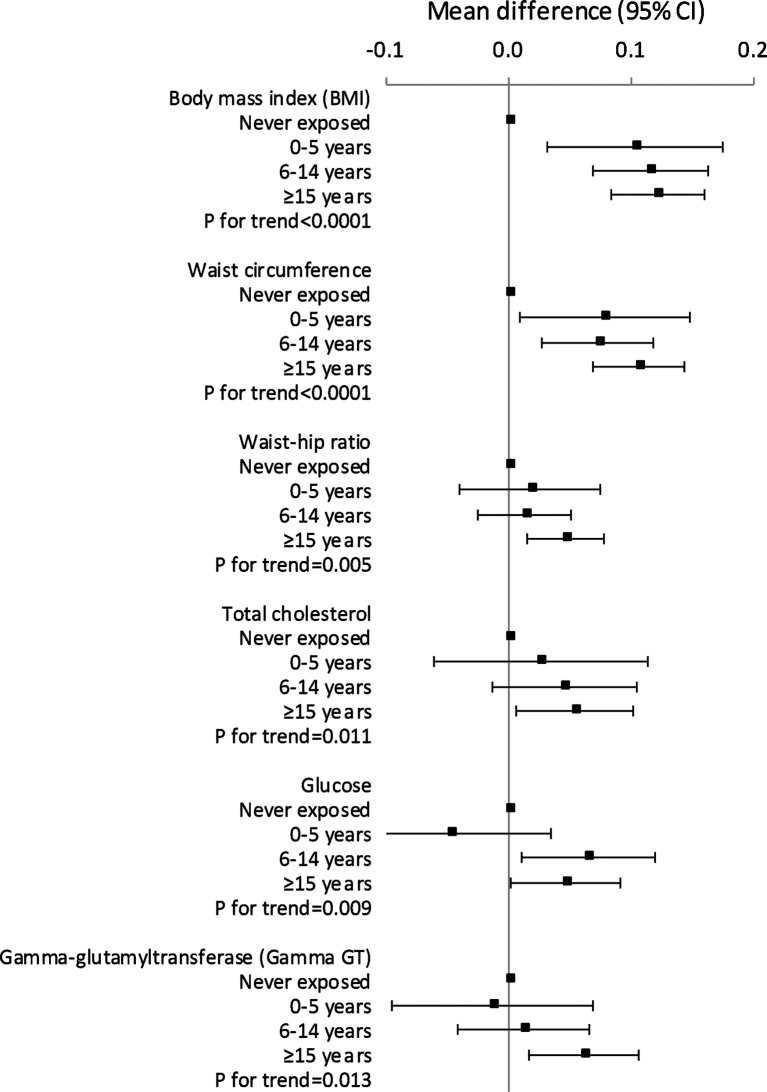
We further analysed the potential dose–response patterns for the number of years exposed to long working hours among those men who currently worked long hours compared with those never exposed, and found a significant dose–response pattern for BMI, waist circumference, waist:hip ratio, total cholesterol, glucose and gamma GT (p values for linear trend 0.013 to <0.0001). These findings are illustrated in figure 2. Among women, no dose–response patterns were found for BMI and white blood cells.
Figure 2.
Mean difference in clinical risk markers (standardised values) among men, comparing participants currently exposed with those never exposed to long working hours, according to the length of exposure and adjusted for age, socioeconomic position, smoking, alcohol use, physical activity, depressive symptoms and chronic disease.
We conducted a sensitivity analysis among men and women free of chronic somatic disease (online supplementary figure 1). The findings are largely similar to those in the original analyses. Another sensitivity analysis was carried out among men and women with low, intermediate and high SEP (online supplementary figures 2 and 3). Given the relatively large CIs, the findings can be considered to a large degree similar in all SEP groups.
jech-2018-210943supp004.pdf (283.7KB, pdf)
Discussion
In this cross-sectional study of a wide range of clinically relevant biomarkers among over 75 000 men and women, current exposure to long working hours was associated with more unfavourable levels in several risk markers among men, in particular in anthropometric risk markers, such as higher BMI, waist circumference and waist:hip ratio, as well as higher glucose and creatinine levels, and poorer scores in lipid parameters. In addition among men, working long hours was associated with higher levels of ALT—an indicator of poorer liver health, and a higher white blood cell count—an indicator of inflammation or infection. Among women, we found associations between long working hours and higher BMI and white blood cell counts. We found no associations between current exposure to long working hours and blood pressure, spirometry, haemoglobin or platelets.
The findings regarding anthropometric markers are in accordance with previous studies on adiposity.8 18–20 However, the Whitehall II study detected no association between long working hours and lipid levels or systemic inflammation.8 In the present study, we observed some indication of a dose–response pattern (a linear trend) for all anthropometric markers, total cholesterol, glucose and gamma GT among men, which may be considered strengthening the evidence of an association between long working hours and these outcomes. However, as the CIs were wide, these findings could be considered suggestive.
A recent meta-analysis including individual participant data reported a prospective association between long working hours and the incidence of hospital-treated diabetes, but only among employees with a low SEP.7 We add to this evidence by an observation of higher clinically measured glucose levels among men who worked long hours, irrespective of socioeconomic position. We also found that the association between long working hours and glucose among men was attenuated after adjustment for BMI, which suggests that increased BMI might be a mechanism that explains the link between long working hours and diabetes. However, previous studies have not found support for the causal link between perceived work stress and obesity,29 30 thus, the missing link—why people who work long hours have higher adiposity—needs to be explored in future studies.
Elevated ALT and gamma GT levels indicate poorer liver health. It is often thought that an adverse changes in ALT is exclusively caused by heavy alcohol use. However, increased ALT may also involve non-alcoholic fatty liver disease, which has emerged as a major liver disease worldwide due to the epidemic of overweight and obesity.31 Although the study participants who worked long hours were more often heavy alcohol users than the other participants, adjustment for alcohol use did not affect the association between long working hours and ALT. In contrast, the association between long working hours and ALT was attenuated after adjustment for BMI. This is consistent with the idea that this working pattern is related to multiple adverse metabolic changes that affect liver health. Furthermore, we may hypothesise that adverse metabolic processes and deteriorating liver health are part of the pathway from long working hours to an increased risk of cardiovascular events found in previous studies.32 A recent study indeed suggested that non-alcoholic fatty liver disease increases coronary artery calcification, independent of traditional risk factors.33 However, as we also observed increased gamma GT among men who had a long history of working overtime, our findings may reflect poorer liver health attributed to risky alcohol use among them.
Our findings also support the idea of systemic inflammation (higher levels of white cell count) as a pathway between long working hours and cardiometabolic diseases. Systemic inflammation is a known risk factor for cardiometabolic diseases and is part of the stress-related pathological changes that contribute to the triggering of cardiovascular and cerebrovascular events.34 Indeed, the peripheral physiological stress response includes the autonomic nervous system response, hypothalamus–pituitary–adrenal (HPA) responses and elevated the levels of inflammatory proteins in the absence of pathogens (known as sterile inflammation).34 However, we adjusted the models for depressive symptoms, a correlate of stress-related HPA activation.
We found no consistent association between working hours and blood pressure outcomes. Many previous studies have relied on self-reported data on hypertension and have reported mixed findings.11–13 Studies that have used clinically measured blood pressure have reported a lower risk of hypertension among those who work long hours.14 15 Thus, it seems that elevated blood pressure or hypertension is not the link between long working hours and cardiovascular events, although this hypothesis needs further confirmation with longitudinal data.
Our sensitivity analysis restricted the sample to healthy participants, that is, those who reported no doctor-diagnosed chronic somatic disease, including cardiovascular disease, thyroid disease, diabetes, dyslipidemia, chronic bronchitis, asthma, inflammatory arthritis, other osteoarticular disorder or cancer. In this way, we were able to characterise the clinical profile among relatively healthy participants, although some of them might have been in a preclinical phase or their disease may have been undetected or undiagnosed. The findings were to a great degree similar to those obtained from the total population (when the models were adjusted for chronic disease).
Working hours were not associated with lung function, haemoglobin or blood platelet concentration. Although participants who worked long hours were more often smokers, adjustment for smoking status did not affect these associations. However, as this was the first study to examine these associations, further research is needed to confirm these results.
Ours is one of the few studies to include an assessment of the duration of exposure to long working hours. With the reference group of ‘never exposed’, we were able to separate the formerly and currently exposed, and control for the misclassification of the formerly to be placed in the ‘not exposed’ group. Indeed, the formerly exposed men had a very similar risk factor profile to that of the currently exposed, which leads us to recommend separating this group from the non-exposed in the future. Interestingly, formerly exposed women had a more adverse risk profile than currently exposed women among whom we found little evidence for the association between long working hours and risk markers. Reasons behind these findings and discrepancies between men and women are unclear but might relate to different selection processes in increasing or decreasing working hours, more excessive working hours among men, as well as women’s resilience towards cardiometabolic risk factors during working age.
A major strength of our study is the large population-based sample, which allowed a precise estimation of the timing of exposure to long working hours, which in turn enabled the assessment of current versus former exposure and dose–response relationships. Such a large study with wide-ranging clinical data has not been carried out in this research field before. The study population included people from across the country, and men and women were equally represented, with a broad range of socioeconomic positions, which supports the generalisability of our findings, although only to the population studied. An important limitation is the low response rate, which raises the question of selection bias. The CONSTANCES participants have been shown to represent a healthier part of the French population. In studies with low participation rates, selection can bias inferences about population prevalence figures of diseases and conditions. However, population prevalence was not the focus of our study; we examined the association between exposures and outcomes and those relationships are less likely to differ between participants and non-participants.35 In addition, people who work long hours may be less likely than people with shorter hours to participate in clinical studies due to lack of time. If the proportionally healthier overtime workers participated, our findings may represent an underestimate of the association between long working hours and risk markers. In addition, statistical robustness does not always mean clinical significance. For example, the adjusted mean in the original BMI scale among never and currently exposed men was 25.3 and 25.8 kg/m2, respectively. The corresponding values among women were 24.1 and 24.3 kg/m2. Neither of these differences are clinically significant. This was a cross-sectional study, which precludes us from making conclusions about the direction of causality but enables an assessment of clinical risk profile. In addition, as former and current exposures to long working hours were differentiated, we were able to evaluate selection effects based on our observations. Even more specific questions on working hours would have been desirable, to capture more detailed hour-based measurements of long working hours. In addition, future studies could examine financial stress as a potential effect modifier in the association between long working hours and health.
In conclusion, our study sheds light on the clinical profile and health of people who work long hours through its large number of anthropometric, functional and blood-based measures. Our findings suggest statistically robust, although modest, associations between exposure to long working hours and greater adiposity, more adverse lipid, glucose, liver and kidney values, and elevated inflammation among men and only few weak associations among women. Future studies should examine long-term effects of overtime work on pathophysiological changes and cardiometabolic diseases.
What is already known on this subject.
Long working hours have been associated with cardiovascular diseases and diabetes, but less is known about the cardiometabolic risk factors associated with long working hours.
What this study adds.
In a large-scale study of working-age population in France, a wide range of cardiometabolic risk factors were examined.
Among men, long working hours were associated with higher body mass index, waist circumference, waist:hip ratio, white blood cell count, glucose, creatinine and alanine transaminase, as well as poorer lipid levels.
Men who work long hours might be in a risk group with an adverse cardiometabolic risk profile.
jech-2018-210943supp005.pdf (257.9KB, pdf)
jech-2018-210943supp006.pdf (257.5KB, pdf)
Footnotes
Contributors: MV, LMH, MG, MZ, SS, JV, HW and MK contributed to conception and design. MV analysed the data and drafted the manuscript. LMH, MG, MZ, SS, JV, HW and MK contributed to interpretation and to critically revising the manuscript. All authors gave final approval and agree to be accountable for all aspects ensuring integrity and accuracy.
Funding: This study was supported by Nordforsk (75021). The CONSTANCES cohort is supported by the French National Research Agency (ANR-11-INBS-0002) and also partly funded by MSD, AstraZeneca and Lundbeck.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: The CONSTANCES Cohort project has been approved by the authorisation of the National Data Protection Authority (Commission nationale de l’informatique et des libertés—CNIL).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The data that support the findings of this study are not publicly available due to legal restrictions, but applications for data access can be submitted in the context of calls for proposals. For more information about how to make use of the CONSTANCES cohort, see http://www.constances.fr/index_EN.php.
References
- 1. Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2016;37:2315–81. 10.1093/eurheartj/ehw106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rydén L, Grant PJ, Anker SD, et al. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the task force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD). Eur Heart J 2013;34:3035–87. 10.1093/eurheartj/eht108 [DOI] [PubMed] [Google Scholar]
- 3. Klein Hesselink J, Goudswaard A. OSHWIKI, 2013. Working time. https://oshwiki.eu/wiki/Working_time
- 4. McCarthy N. A 40 hour work week in the United States actually lasts 47 hours: Forbes, 2014. [Google Scholar]
- 5. OECD. Average annual hours actually worked per worker. OECDstat 2016. [Google Scholar]
- 6. Kivimäki M, Jokela M, Nyberg ST, et al. Long working hours and risk of coronary heart disease and stroke: a systematic review and meta-analysis of published and unpublished data for 603,838 individuals. Lancet 2015;386:1739–46. 10.1016/S0140-6736(15)60295-1 [DOI] [PubMed] [Google Scholar]
- 7. Kivimäki M, Virtanen M, Kawachi I, et al. Long working hours, socioeconomic status, and the risk of incident type 2 diabetes: a meta-analysis of published and unpublished data from 222120 individuals. Lancet Diabetes Endocrinol 2015;3:27–34. 10.1016/S2213-8587(14)70178-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kivimäki M, Nyberg ST, Batty GD, et al. Long working hours as a risk factor for atrial fibrillation: a multi-cohort study. Eur Heart J 2017;38:2621–8. 10.1093/eurheartj/ehx324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Virtanen M, Jokela M, Nyberg ST, et al. Long working hours and alcohol use: systematic review and meta-analysis of published studies and unpublished individual participant data. BMJ 2015;350:g7772 10.1136/bmj.g7772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Artazcoz L, Cortès I, Escribà-Agüir V, et al. Understanding the relationship of long working hours with health status and health-related behaviours. J Epidemiol Community Health 2009;63:521–7. 10.1136/jech.2008.082123 [DOI] [PubMed] [Google Scholar]
- 11. Yang H, Schnall PL, Jauregui M, et al. Work hours and self-reported hypertension among working people in California. Hypertension 2006;48:744–50. 10.1161/01.HYP.0000238327.41911.52 [DOI] [PubMed] [Google Scholar]
- 12. Yoo DH, Kang MY, Paek D, et al. Effect of long working hours on self-reported hypertension among middle-aged and older wage workers. Ann Occup Environ Med 2014;26:25 10.1186/s40557-014-0025-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pimenta AM, Beunza JJ, Bes-Rastrollo M, et al. Work hours and incidence of hypertension among Spanish university graduates: the Seguimiento Universidad de Navarra prospective cohort. J Hypertens 2009;27:34–40. 10.1097/HJH.0b013e3283163c3c [DOI] [PubMed] [Google Scholar]
- 14. Imai T, Kuwahara K, Nishihara A, et al. Association of overtime work and hypertension in a Japanese working population: a cross-sectional study. Chronobiol Int 2014;31:1108–14. 10.3109/07420528.2014.957298 [DOI] [PubMed] [Google Scholar]
- 15. Wada K, Katoh N, Aratake Y, et al. Effects of overtime work on blood pressure and body mass index in Japanese male workers. Occup Med 2006;56:578–80. 10.1093/occmed/kql106 [DOI] [PubMed] [Google Scholar]
- 16. Kobayashi T, Suzuki E, Takao S, et al. Long working hours and metabolic syndrome among Japanese men: a cross-sectional study. BMC Public Health 2012;12:395 10.1186/1471-2458-12-395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pimenta AM, Bes-Rastrollo M, Sayon-Orea C, et al. Working hours and incidence of metabolic syndrome and its components in a Mediterranean cohort: the SUN project. Eur J Public Health 2015;25:683–8. 10.1093/eurpub/cku245 [DOI] [PubMed] [Google Scholar]
- 18. Mercan MA. A research note on the relationship between long working hours and weight gain for older workers in the United States. Res Aging 2014;36:557–67. 10.1177/0164027513510324 [DOI] [PubMed] [Google Scholar]
- 19. Kim BM, Lee BE, Park HS, et al. Long working hours and overweight and obesity in working adults. Ann Occup Environ Med 2016;28:36 10.1186/s40557-016-0110-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jang TW, Kim HR, Lee HE, et al. Long work hours and obesity in Korean adult workers. J Occup Health 2014;55:359–66. 10.1539/joh.13-0043-OA [DOI] [PubMed] [Google Scholar]
- 21. Tsuboya T, Aida J, Osaka K, et al. Working overtime and risk factors for coronary heart disease: a propensity score analysis based in the J-SHINE (Japanese Study of Stratification, Health, Income, and Neighborhood) study. Am J Ind Med 2015;58:229–37. 10.1002/ajim.22409 [DOI] [PubMed] [Google Scholar]
- 22. Goldberg M, Carton M, Descatha A, et al. CONSTANCES: a general prospective population-based cohort for occupational and environmental epidemiology: cohort profile. Occup Environ Med 2017;74:66–71. 10.1136/oemed-2016-103678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ruiz F, Goldberg M, Lemonnier S, et al. High quality standards for a large-scale prospective population-based observational cohort: Constances. BMC Public Health 2016;16:877 10.1186/s12889-016-3439-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J 2005;26:319–38. 10.1183/09031936.05.00034805 [DOI] [PubMed] [Google Scholar]
- 25. Insitut national de la statistique et des études économiques, 2018. Classification of Nomenclatures. http://www.insee.fr/fr/methodes/default.asp?page=nomenclatures/pcs2003/pcs2003.htm (accessed 21 Sep 2018).
- 26. Bohn MJ, Babor TF, Kranzler HR. The Alcohol Use Disorders Identification Test (AUDIT): validation of a screening instrument for use in medical settings. J Stud Alcohol 1995;56:423–32. 10.15288/jsa.1995.56.423 [DOI] [PubMed] [Google Scholar]
- 27. Babor TF, Higgins-Biddle JC, Saunders JB, et al. AUDIT. The alcohol use disorders identification test. Guidelines for use in primary care. Geneva: World Health Organization, 2001. [Google Scholar]
- 28. Radloff L. The CES-D scale: a self report depression scale for research in the general population. Appl Psych Meas 1977:385–401. [Google Scholar]
- 29. Rosengren A, Teo K, Rangarajan S, et al. Psychosocial factors and obesity in 17 high-, middle- and low-income countries: the Prospective Urban Rural Epidemiologic study. Int J Obes 2015;39:1217–23. 10.1038/ijo.2015.48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kivimäki M, Singh-Manoux A, Nyberg S, et al. Job strain and risk of obesity: systematic review and meta-analysis of cohort studies. Int J Obes 2015;39:1597–600. 10.1038/ijo.2015.103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Neuschwander-Tetri BA. Non-alcoholic fatty liver disease. BMC Med 2017;15:45 10.1186/s12916-017-0806-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chung GE, Yim JY, Kim D, et al. Associations between white blood cell count and the development of incidental nonalcoholic fatty liver disease. Gastroenterol Res Pract 2016;2016:1–6. 10.1155/2016/7653689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Park HE, Kwak MS, Kim D, et al. Nonalcoholic fatty liver disease is associated with coronary artery calcification development: a longitudinal study. J Clin Endocrinol Metab 2016;101:3134–43. 10.1210/jc.2016-1525 [DOI] [PubMed] [Google Scholar]
- 34. Kivimäki M, Steptoe A. Effects of stress on the development and progression of cardiovascular disease. Nat Rev Cardiol 2018;15:215–29. 10.1038/nrcardio.2017.189 [DOI] [PubMed] [Google Scholar]
- 35. Rothman KJ, Gallacher JE, Hatch EE. Why representativeness should be avoided. Int J Epidemiol 2013;42:1012–4. 10.1093/ije/dys223 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jech-2018-210943supp001.pdf (110.4KB, pdf)
jech-2018-210943supp003.pdf (25.1KB, pdf)
jech-2018-210943supp002.pdf (24.7KB, pdf)
jech-2018-210943supp004.pdf (283.7KB, pdf)
jech-2018-210943supp005.pdf (257.9KB, pdf)
jech-2018-210943supp006.pdf (257.5KB, pdf)