Abstract
AIM:
This study aims to evaluate the methods of treatment of the thoracic part of oesophagal cancer and to predict the results of treatment depending on the factors of the prognosis.
MATERIALS AND METHODS:
The results of treatment of 366 patients with cancer of the thoracic part of the oesophagus for 10 years (2007-2016) by the department of thoracic oncology of the Karaganda oncological dispensary were studied.
RESULTS:
The overall five-year survival rate, regardless of the method of treatment, was only 8.72% (28 of 321), and in the 6-10 year period 8.41% (27 of 321) lived, p < 0.05. Analysis of the overall survival of patients with cancer of the thoracic part of oesophagus showed that the method of treatment does not have a significant effect on life expectancy. A multivariate analysis of 19 grades that affect the prognosis of the disease was carried out.
CONCLUSION:
Radical type of treatment of the middle and lower thoracic oesophagus is surgical, in which the median of cumulative survival is 19 months. Traditional radiotherapy should be used in a limited way, as it is palliative, with a median survival of no more than 9 months. The leading factor in the prognosis for thoracic part of oesophagal cancer is the presence of regional metastases, on which the choice of method of treatment depends.
Keywords: Esophageal cancer, Radiation therapy, Survival, Regional metastases
Introduction
The incidence of oesophagal cancer in Kazakhstan remains high, amounting to 7.7 per 100 thousand, which is 1.2 times more than in the Russian Federation. Even though the population of the Russian Federation is 10 times more than in Kazakhstan. Mortality from this pathology in Kazakhstan takes the 4th place, accounting for 5.8%. The incidence of oesophagal cancer in the Karaganda region is 8.8 per 100 thousand populations, which is 1.3 higher than in the Republic of Kazakhstan.
The main cause of high mortality up to one year after diagnosis is late detection of oesophagal cancer; mortality is 65% [1]. Many researchers [2], [3] note that the majority of patients at the beginning of treatment have stage III-IV of the tumour process in 65-75% of cases. The presence of common forms of oesophagal cancer at the time of treatment creates certain difficulties in the choice of therapy. Many patients are unresectable due to the high prevalence of the tumour process [4], competing comorbidities. In 20% of cases after radical treatment, local recurrences of a tumour in the anastomosis was detected.
P.A. Herzen (Moscow) [5] has developed the following program for the treatment of oesophagal cancer. At stage I-II and in the absence of metastases, an organ-preserving treatment is proposed: electro- and laser destruction of the tumor with the administration of the “Photochem” and “Photosens” preparations, with locally advanced esophageal cancer, i.e. in stage III, in view of the severity of the initial condition (significant loss in weight, severe dysphagia, and dehydration), at the first stage, gastrostomy is performed according to our own method with revision of paracardial, paraaortal metastasis areas and their removal. According to reports [5], the imposition of gastrostomy allows for adequate rehabilitation of the patient and to prepare for a radical operation. In the presence of a decompensated initial state, simultaneous resection of the oesophagus with esophagoplasty by an isoperistaltic stem from the greater curvature of the stomach is recommended. In doubtful cases, when the initial condition of the patient is assessed as serious, then dobromyslov’s two-stage operation-Toreka is performed. Delayed esophagoplasty is used 6 months after the first. According to L.D. Roman et al., [3], the surgical method of treating cancer of the oesophagus remains the main method, despite the success of chemoradiotherapy. So R.Kube et al., [6] consider the results of 5-year survival during chemoradiation therapy of oesophagal cancer to be doubtful. According to D. Karpov et al., [7], with the common and neglected forms of oesophagal cancer, palliative surgical and endoscopic methods must be supplemented with radiation therapy. At the same time, Chissov V.I., Daryalova S.L. [8] believe that chemotherapy and radiation methods rarely regress a tumour, and the life expectancy after it does not exceed 13 months.
Other researchers [9], on the contrary, note that neoadjuvant radiochemotherapy is a promising method, and in 10–20% of cases complete regression can be achieved. Orringer M.B. et al. used a complex method of treatment of common forms of oesophagal cancer, and in 52% of patients in the postoperative period, no complications were noted [9].
Thus, the prospects for chemoradiation therapy for cancer of the thoracic oesophagus are extremely limited if they are not complemented by surgical intervention.
The purpose of this study is to evaluate the treatment of cancer of the thoracic oesophagus and to predict the results of treatment depending on the prognostic factors.
Material and Methods
The results of treatment of cancer of the ore oesophagus for 10 years (2007-2016) were analysed based on the materials of the Department of Thoracic Oncology of the Karaganda Oncologic Dispensary. The results of treatment of 366 patients with thoracic part of oesophagal cancer were studied. In the analysed material (Figure 1) men prevailed than women, the ratio was 1.6: 1 (p ≤ 0.05).
Figure 1.
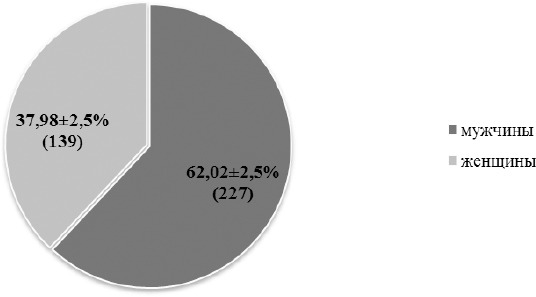
Sex composition of patients
Among the patients, the inhabitants of rural areas prevailed, 70.21 ± 2.4% (257), compared with urban areas, 29.78 ± 2.4% (109) p ≤ 0.05.
According to the ethnic composition (Figure 2) of the patients, it turned out that the majority were (p ≤ 0.05) of the indigenous people of Kazakhs 71.58 ± 2.36% (262), slavs-only 19.39 ± 2.07% (71) while others were identified at 9.03 ± 1.5% (33).
Figure 2.
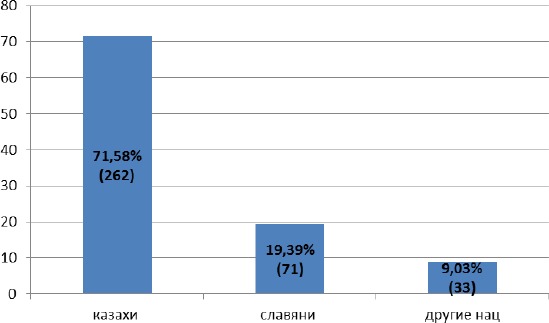
Ethnic composition of patients
Most often, tumours were localised in the middle part of thoracic part of the oesophagus -58.74% (215), then in the lower part, 34.15 (125). According to the prevalence of the tumour process (Table 1), patients were distributed according to the international classification of staging (TNM, 2011) as follows, stage IIa, T3N0M0, 59.56% (218), then stage IIIa, T4aN0M0, 16.93% (62) and Ib stage T2N0M0 was only 10.65% (39) p < 0.05.
Table 1.
Stage cancer of the thoracic part of the oesophagus
| № | Stage | TNM stage | Abs. number | Per cent, % | Mistake, m |
|---|---|---|---|---|---|
| 1 | I a | T1N0M0 | 4 | 1.09 | 0.54 |
| 2 | I b | T2N0M0 | 39 | 10.65 | 1.61 |
| 3 | II a | T3N0M0 | 218 | 59.56 | 2.57 |
| 4 | II b | T1-2N1M0 | 9 | 2.46 | 0.81 |
| 5 | III a | T4aN0M0, T3N1M0, T1-2N2M0 | 62 | 16.94 | 1.96 |
| 6 | III b | T3N2M0 | 30 | 8.20 | 1.43 |
| 7 | III c | T4aN1-2M0, T4bN1-3M0, T1-4N3M0 | 4 | 1.10 | 0.54 |
Among the histological forms, squamous cell carcinoma without keratinisation with keratinisation dominated, respectively -65.30% (239) and 27.05% (99). Rare forms such as adenocarcinoma and undifferentiated cancer did not exceed, respectively, 5.46% (20) and 2.19% (8) p < 0.05.
Regional metastases were detected in paraesophageal lymph nodes in 13.11% (48) cases, paracardial-12.57% (46). Without metastases, there were 35.25% (129) patients, and metastases in 39.07 (143) patients were not verified, which, based on X-ray data and computed tomography, enlarged lymph nodes were detected, and they were subjected to radiation therapy. All patients were distributed according to the treatment plan, taking into account the prognosis factors for 3 groups:
Group 1-surgical treatment of 45.36% (166);
Group 2-radical radiation therapy 41.53% (152);
Group 3-combined method (preoperative course of radiation therapy + surgery) 13.11% (48).
Surgical intervention was carried out in two ways-Subtotal resections of the mid-thoracic part of the oesophagus with bizonal lymph dissection-Lewis operation-46.45% (170), Garlock operation-resection of the lower thoracic part of the oesophagus with resection of the proximal stomach with bizonal lymph dissection-12.02 % (44).
With the traditional method of operation according to the Lewis method, after laparotomy, mobilisation of the stomach with the intersection of the right ligament of the diaphragm with preservation of the right gastroepiploic artery, a turn is made to the left side. The right-sided thoracotomy in the V intercostal space and after revision of the pleural cavity, clarification of the extent of the tumour process, mobilises the oesophagus above the aortic arch with the intersection and ligation of the unpaired vein. At the same time, lymph node dissection is carried out, all mediastinal lymph nodes are removed to the cardiodiaphragmatic angle. After that, the stomach, along with the oesophagus, is pulled into the pleural cavity. After skeletonisation of the lesser curvature of the stomach, we produce a proximal resection of the stomach using UO-60, UO-40 devices. The mechanical suture is covered with grey-serous sutures. After resection of the oesophagus, proximal to a tumour 5 cm impose the oesophagal-gastric submersible anastomosis. In view of the high resection of the esophagus with its significant mobilization, graft tension, extended lymph node dissection, 7 (3.27%) cases of oesophagal anastomosis insolvency were noted for 214 radical operations and 2 (0.93%) for transplant necrosis, in connection with what they decided to improve the method of imposing oesophagal anastomoses.
Starting in 2012, they began to produce esophagoplasty for cancer with a “solid” stomach (patent of the committee for Intellectual property rights of the Ministry of Justice of the Republic of Kazakhstan No. 1449905 dated 04.24.2017, “Method of esophageal plasty for cancer with a “whole” stomach during resection of the thoracic part of esophagus”).
After a right-sided thoracotomy during Lewis type surgery, pulling the oesophagus with the stomach into the pleural cavity, the oesophagus is resected 5 cm above a tumour. Then, only the cardinal part of the stomach is resected, immediately below the cardiac sphincter, a small part of the fundus of the stomach is partially resected, some 5 cm from the extreme short fundal artery. The resection of the stomach is performed using the apparatus of Yo-60, Yo-40. The mechanical suture is covered with grey-serous sutures with the immersion of the nodes of the stomach stump into semi-set sutures, which later, after the imposition of the oesophagal anastomosis, act as a cardiac sphincter. Then an oesophagal-gastric immersion anastomosis of the “end to side” type is formed. In this way, 113 operations were performed, 2 cases with complications (1.76 ± 1.23%), in one case, there was an insufficiency of the oesophagal anastomosis 0.88 ± 0.87%, and 1 graft necrosis 0.88 ± 0.87%, which have been lethal.
The prevailing postoperative complication was congestive pneumonia, which was noted in 6.55% (24) cases. Postoperative mortality was 6.54% (14) for 214 operations, of which in 7 cases (50.00%) there was a failure of the esophageal anastomosis, 5 (35.71%)-cardiovascular disorders, 2 (14.29%), cardiopulmonary insufficiency (p < 0.05).
The long-term results of treating patients with the thoracic part of oesophagal cancer were studied depending on the method of therapy and prognostic factors using survival.
Statistical analysis was performed using Statistica version 10 software. All values are expressed as mean ± mistake or medians and interquartile ranges for continuous factors and frequencies for categorical factors. The one-dimensional analysis was performed using Chi-square and Fisher probability tests for continuous variables. Student t-test was used for continuous factors. Survival 5-year and overall survival were compared between groups using Kaplan-Meier analysis and log-ranking criteria. In a one-dimensional analysis of overall survival, variables with value were statistically rethought to adjust for concomitant factors. The coke model was used for multivariate regression analysis. A p-value less than 0.05 was considered statistically significant.
Results
The overall five-year survival, regardless of the method of treatment, was only 8.72% (28 of 321), and in 6-10 years lived 8.41% (27 of 321), p < 0.05. Analysis of the overall survival of patients with cancer of the thoracic part of oesophagus showed that the method of treatment does not have a significant impact on life expectancy.
From the analysis excluded patients who as of 01/01/2018, after treatment, the follow-up period was less than 2 years, 321 (87.7 ± 1.7) cases were analysed.
Table 2.
The total lifetime of patients with oesophagal cancer after radical treatment
| The number of observed patients | Lifetime in years | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 321 | 1 | 2 | 3 | 5 | >5 | |||||
| Abs. number | % | Abs. number | % | Abs. number | % | Abs. number | % | Abs. number | % | |
| 128 | 39.88 | 86 | 26.79 | 52 | 16.20 | 28 | 8.72 | 27 | 8.41 | |
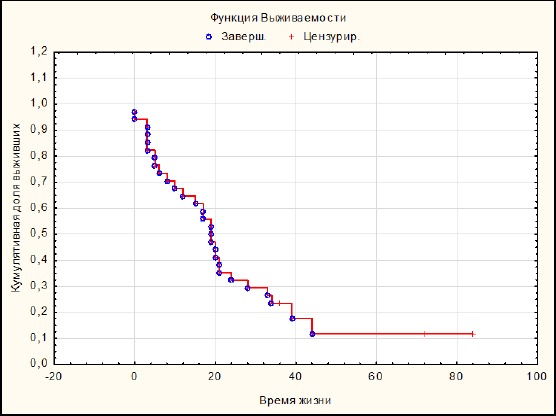
A multifactor analysis of 19 gradations that affect the prognosis of the disease was carried out. Analysis of cumulative survival showed that (Figure 3) the best and 5-year survival was among patients in group 1, which was 26.53% (out of 147 treated, 5 years lived 39). The median survival is 19 months.
Figure 3.
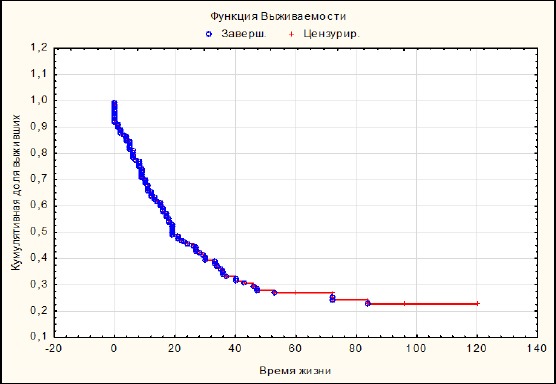
Lifetime with surgical treatment
In the second group (Figure 4), the 5-year survival rate did not significantly exceed 8.57% (out of 140 treated, 5 years survived 12).
Figure 4.
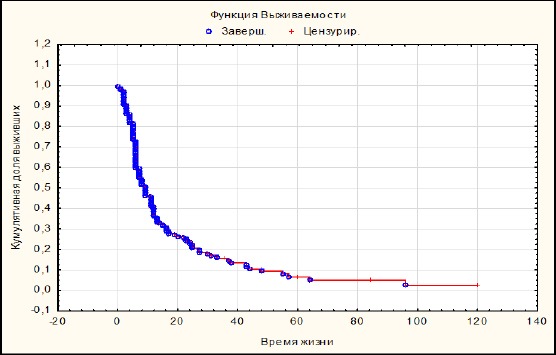
Radical radiation therapy
The patients who underwent combined treatment (Figure 5) lived 5 years in 17.65% (out of 34 treated, 5 years lived 6) cases. At the same time, it should be noted that the median of survival was the same with the surgical treatment group, and was 19 months.
Figure 5.
Lifetime with combined treatment
However, a comparative analysis of cumulative survival by Kaplan-Meier (Figure 6) showed that the best survival was reliably observed with surgical treatment (p < 0.05) than with radiation and combined treatment, the median survival was 13.5 months.
Figure 6.
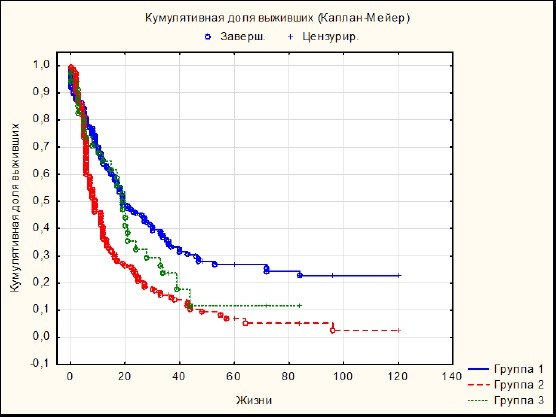
Cumulative survival depending on the method of treatment
Such a low cumulative survival among patients of the 2nd and 3rd groups is because patients with high operational risk were subjected to radiation treatment. The leading cause of failure in surgical treatment was old age (over 70 years of age was 46.7 ± 4.05%) and cardiopulmonary insufficiency was 11.84 ± 2.62. Whereas, in the 1st group, patients aged 51-60 years (46.38 ± 3.87%) with cardiopulmonary pathology prevailed in only 5.42% ± 1.76% of cases. In the group of patients after combined treatment, 33.33 ± 6.8% of cases aged 51-60 years with a cardiopulmonary pathology of 6.25 ± 3.49% (p < 0.05) prevailed.
A mathematical model for assessing the risk of death in cancer of the oesophagus showed (Figure 7), regardless of the method of treatment of cancer of the thoracic oesophagus, the risk of mortality increases in the first 2 years and increased 4 years after treatment.
Figure 7.

The risk of mortality in the treatment of oesophagal cancer
Discussion
According to most researchers [1], [2], [4], [5], [7], the prospects for the use of radiation and chemotherapeutic care for patients with distributed forms of esophageal cancer are limited in view of its resistance, and basically these types of treatment are of an auxiliary nature. The leading treatment for oesophagal cancer is surgical.
According to reports [10], [11], oesophagal cancer has a high potential for lymphogenous metastasis and in case of a lesion of the submucosal layer, i.e. T1 metastases in the lymph nodes are detected in 40%, and during germination of adventitia, 90%.
According to Stilidi I. et al., so-called “jumping metastases” in regional and distant nodes are detected in 20%, and it is extremely difficult to determine the direction of lymphatic drainage. Therefore, a prerequisite, i.e. the standard for the surgical treatment of oesophagal cancer should be considered extended 2-hzonalny lymph node dissection [11].
One of the important prognostic factors affecting life expectancy is the frequency of damage to the lymphatic catch and their number [12]. The 3-and 5-year survival in the presence of N1 was 47.7% and 12.9%, and at the stage of N0, it was 68.6% and 54.8%, respectively (p < 0.05). Equally important for the forecast is the number of affected lymph nodes. The “critical” number is 7 affected lymph nodes [5], [12]. According to Napier K.J. et al., [12], and Stilidi I.S. et al., [11] none of the patients with 7 or more lymph nodes did live up to 3 years.
Japanese surgeons from the 80s [13] used a three-zone lymphadenectomy, arguing that in 40% of patients with squamous cell carcinoma of the oesophagus after radical surgery, metastasis to the cervical lymph nodes is detected in the long term. According to the authors of [14], the 5-year survival rate after the above operations was 65% for squamous cell carcinoma and 46% for adenocarcinoma. The same data confirm Altorki N. et al., [14], who proved that 25% of patients experienced a 5-year follow-up, despite the presence of cervical metastatic lymph nodes.
One of the most promising methods of combined treatment, according to N.V. Dengina [15] is neoadjuvant chemotherapy, in which resectability and patient survival are increased. The effectiveness of neoadjuvant chemotherapy followed by surgery, the author, estimates in 45-70% of cases. With radiation therapy in a total dose of 45-75 Gray in patients with small tumours, the 5-year survival rate does not exceed 10 to 15%. The author notes that radiation and chemotherapy are palliatives in nature. Therefore the use of the above methods as an independent method of treating oesophagal cancer is an alternative solution.
The data obtained confirm the correlation analysis of Spearman, conducted in pairs with each group of patients, depending on the method of treatment and the presence of prognostic factors.
According to the findings, affecting the outcome of treatment of esophageal cancer, factors such as tumour localization (rs = -0.089776), histological form (rs = -0.055125), regional lymph node metastases (rs = -0.0342697) effect , the length of the oesophagus tumour (rs = -0.248513) with a confidence interval of 95%. All of the above factors relate to the concept of the stage of the disease. However, among all the prognostic factors, the presence of regional metastases plays the most important role in the choice of treatment and the prognosis of a long-term outcome. For patients under 60 years of age with regional metastases, the long-term outcome in the combined degree (rs = 0.277693) is determined, as well as the tumour localization in the bronchial and retrocardial segment, it is equal to (rs = 0.243261), the histological type is squamous cell cancer with keratinization (rs = 0.164874), the length of the tumour is not more than 3 cm (rs = 0.311595), invasion of the muscle layer tumour (rs = 0.320403). Also, a lifetime in the long term depends on the factors of cancer recurrence and the progression of the process. Their relationship was, respectively, rs = -0.139073 and rs = 0.144985.
Thus, the prognosis for the long-term outcome of treatment for distributed cancer of the thoracic oesophagus depends on the stage of the disease, the location of the tumour and the presence of regional metastases. When the prehospital diagnosis of cancer localisation in the mid-thoracic oesophagus with a process length of more than 3 cm and the presence of regional metastases before the age of 65, it is necessary to plan a combined treatment (neoadjuvant radiation therapy + surgery). Radiation therapy for advanced cancer of the thoracic oesophagus is palliative in nature and should mainly be used in patients older than 70 years with comorbidities in the decompensation stage.
In conclusion, a radical treatment for cancer of the mid- and lower thoracic oesophagus is surgical, in which the median of cumulative survival is 19 months. Traditional radiation therapy should be applied in a limited way, as it is palliative in nature, the median survival rate does not exceed 9 months.
In the presence of regional metastases in cancer of the thoracic oesophagus, it is advisable to use the combined method (neoadjuvant radiation therapy + Lewis surgery with 2-zonal dissection), the median survival is 19 months.
The leading prognostic factor for cancer of the thoracic region is the presence of regional metastases, on which the choice of treatment depends. With an inadequate choice of treatment method in a long-term period, the frequency of relapses and progression of the tumour process increases. Especially high-risk mortality in the first 2 years after treatment, regardless of the method of treatment of cancer of the thoracic oesophagus.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Axel EM. Statistics of malignant neoplasms of the gastrointestinal tract. Siberian Oncological Journal. 2017;16(3):5–11. https://doi.org/10.21294/1814-4861-2017-3-5-11. [Google Scholar]
- 2.Litvinov RP, Chernykh MV, Nechushkin MI. Brachytherapy of esophageal cancer with localization as a component of radical treatment: advantages and risks. Malignant tumors. 2016;4:109–114. [Google Scholar]
- 3.Roman LD, Shostka KG, Arutyunyan KV. Possibilities of surgical treatment of complicated forms of locally advanced thoracic esophagus cancer. Preventive and Clinical Medicine. 2016;3(60):67–71. [Google Scholar]
- 4.Kanaev SV, Shcherbakov AM, Tiuriaeva EI, Avanesian AA. Conservative treatment of locally advanced and inoperable esophageal cancer: possible methods and future directions. Voprosy onkologii. 2012;58(2):199–202. PMid:22774524. [PubMed] [Google Scholar]
- 5.Mamontov AS. Combined treatment of esophageal cancer. Practical Oncology. 2003;4(2):76–82. [Google Scholar]
- 6.Kube R, Reimer A, Kluge E, et al. Surgical treatment of esophageal malignant neoplasms. Surgery. 2009;9:50–54. [PubMed] [Google Scholar]
- 7.Karpov DV, Kaminsky YuD, Grigoriev AV, Karpova LI. Prognostic factors and their influence on the results of treatment of esophageal cancer. Science of the Young. 2013;4(2):39–51. [Google Scholar]
- 8.Chissov VI, Daryalova SL. Oncology-M: GEOTAR-Media. 2007:560. [Google Scholar]
- 9.Orringer MB, Marshall B, Chang AC, Lee J, Pickens A, Lau CL. Two thousand transhiatal esophagectomies: changing trends, lessons learned. Annals of surgery. 2007;246(3):363. doi: 10.1097/SLA.0b013e31814697f2. https://doi.org/10.1097/SLA.0b013e31814697f2 PMid: 17717440 PMCid: PMC1959358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anil KR, Hashem BE. Esophageal Carcinoma. N Engl J Med. 2014;371:2499–2509. doi: 10.1056/NEJMra1314530. https://doi.org/10.1056/NEJMra1314530 PMid: 25539106. [DOI] [PubMed] [Google Scholar]
- 11.Stilidi I, Davydov M, Bokhyan V, Suleymanov E. Subtotal esophagectomy with extended 2-field lymph node dissection for thoracic esophageal cancer. European journal of cardio-thoracic surgery. 2003;23(3):415–20. doi: 10.1016/s1010-7940(02)00801-1. https://doi.org/10.1016/s1010-7940(02)00801-1. [DOI] [PubMed] [Google Scholar]
- 12.Napier KJ, Scheerer M, Misra S. Esophageal cancer: A Review of epidemiology, pathogenesis, staging workup and treatment modalities. World journal of gastrointestinal oncology. 2014;6(5):112. doi: 10.4251/wjgo.v6.i5.112. https://doi.org/10.4251/wjgo.v6.i5.112 PMid: 24834141 PMCid: PMC4021327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Isono K, Ochiai T, Okuyama K, Onoda S. The treatment of lymph node metastasis from esophageal cancer by extensive lymphadenectomy. The Japanese journal of surgery. 1990;20(2):151–7. doi: 10.1007/BF02470762. https://doi.org/10.1007/BF02470762 PMid: 2342235. [DOI] [PubMed] [Google Scholar]
- 14.Altorki N, Kent M, Ferrara C, Port J. Three-field lymph node dissection for squamous cell and adenocarcinoma of the esophagus. Annals of surgery. 2002;236(2):177. doi: 10.1097/00000658-200208000-00005. https://doi.org/10.1097/00000658-200208000-00005 PMid: 12170022 PMCid: PMC1422563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dengina NV. Modern therapeutic opportunities in cancer of the esophagus. Practical Oncology. 2012;4:276–288. [Google Scholar]


