Abstract
Hyposmia is one of the earliest and the most common symptoms in Parkinson’s disease (PD). The benefits of hydrogen water on motor deficits have been reported in animal PD models and PD patients, but the effects of hydrogen gas on PD patients have not been studied. We evaluated the effect of inhalation of hydrogen gas on olfactory function, non-motor symptoms, activities of daily living, and urinary 8-hydroxy-2′-deoxyguanine (8-OHdG) levels by a randomized, double-blinded, placebo-controlled, crossover trial with an 8-week washout period in 20 patients with PD. Patients inhaled either ~1.2–1.4% hydrogen-air mixture or placebo for 10 minutes twice a day for 4 weeks. Inhalation of low dose hydrogen did not significantly influence the PD clinical parameters, but it did increase urinary 8-OHdG levels by 16%. This increase in 8-OHdG is markedly less than the over 300% increase in diabetes, and is more comparable to the increase after a bout of strenuous exercise. Although increased reactive oxygen species is often associated with toxicity and disease, they also play essential roles in mediating cytoprotective cellular adaptations in a process known as hormesis. Increases of oxidative stress by hydrogen have been previously reported, along with its ability to activate the Nrf2, NF-κB pathways, and heat shock responses. Although we did not observe any beneficial effect of hydrogen in our short trial, we propose that the increased 8-OHdG and other reported stress responses from hydrogen may indicate that its beneficial effects are partly or largely mediated by hormetic mechanisms. The study was approved by the ethics review committee of Nagoya University Graduate School of Medicine (approval number 2015-0295). The clinical trial was registered at the University Hospital Medical Information Network (identifier UMIN000019082).
Keywords: Parkinson's disease, randomized, double-blinded, placebo-controlled, crossover trial, smell test, hydrogen gas, 8-hydroxy-2’- deoxyguanine, 8-OHdG, oxidative stress, hormesis
INTRODUCTION
Hyposmia in Parkinson’s disease (PD) was first reported in 1975 by Ansari and Johnson.1 Subsequent studies revealed that (i) more than 70 to 80% of PD patients have hyposmia; (ii) hyposmia is one of the earliest symptoms of PD; (iii) hyposmia is correlated with severity of cognitive dysfunction.2,3,4,5 Abnormal aggregation of α-synuclein in dopaminergic neurons in the substantia nigra causes neuronal death and is a hallmark of PD. The abnormal aggregate of α-synuclein starts from the olfactory epithelium and/or intestinal neural plexus, and enters the brain.6 The expression level of α-synuclein is normally high in the olfactory epithelium.7 The abnormal aggregate of α-synuclein in the olfactory epithelium is likely due to some environmental toxins and/or genetic factors,8 but the underlying mechanisms remain to be elucidated. Hyposmia is quantitatively evaluated by the University of Pennsylvania Smell Identification Test9 or the Sniffin’ Sticks odor identification test.10 Some substances in these tests, however, are culture-specific and are unfamiliar to Japanese people. To circumvent the cultural barrier, the odor stick identification test for Japanese (OSIT-J) was developed and is comprised of 12 odors embedded in microcapsules.11,12
Neurodegeneration of the substantia nigra in PD is caused by Lewy bodies that are comprised of abnormally aggregated α-synuclein. Braak et al.13 reported in 2002 that Lewy bodies start from the dorsal vagal nucleus, and ascend to the pons, the midbrain, the limbic system, and the cerebral cortex. The anterior olfactory nucleus in the olfactory bulb is also the earliest site where Lewy bodies are observed. The formation of Lewy bodies is causally associated with oxidative stress.14 Urinary excretion of 8-hydroxy-2′-deoxyguanosine (8-OHdG) serves as a marker for oxidative stress, and is increased on average 2.3-fold in PD.15 We later reported that urinary 8-OHdG is elevated only in PD with hallucinations but not with dementia or other clinical features.16
As of 2015, the effects of molecular hydrogen on various diseases have been reported in more than 300 original articles.17 Reactive oxygen species (ROS)-mediated diseases, inflammatory diseases, and metabolic diseases constituted ~70%, 20%, and 6% of original articles, respectively.17 In these studies, hydrogen was administered by ingestion of hydrogen water in ~25% of original articles, inhalation of hydrogen gas in ~20% of original articles, and by other methods in ~55% of original articles (intraperitoneal injection of hydrogen-rich saline, bathing in hydrogen-rich water, etc.).17 We previously reported that drinking hydrogen-rich water almost normalized a rat model of 6-hydroxydopamine-induced hemiparkinsonism.18 Fujita et al.19 similarly reported a marked effect of drinking hydrogen-rich water in a mouse model of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-induced PD. We later reported that intermittent inhalation of 2% hydrogen gas for 15 minutes at a 1-hour interval from 6 p.m. to 6 a.m. for 5 weeks ameliorated a rat model of 6-hydroxydopamine-induced hemiparkinsonism, whereas continuous inhalation of 2% hydrogen gas for 24 hours a day for 5 weeks had no effect.20 A randomized, double-blinded, placebo-controlled, parallel-group clinical pilot study revealed that drinking 1000 mL/d of hydrogen water for 48 weeks significantly ameliorated total Unified Parkinson’s Disease Rating Scale (UPDRS) scores in PD patients.21 The effect of inhalation of hydrogen gas has not been examined in PD patients, but is reported in patients having percutaneous coronary intervention22 and in patients with acute cerebral infarction.23
Here we examined the effect of inhalation of hydrogen gas on hyposmia, non-motor symptoms, activities of daily living (ADLs), and urinary excretion of 8-OHdG. We found that although short-term inhalation of hydrogen gas did not affect any clinical parameters, it significantly increased urinary 8-OHdG.
SUBJECTS AND METHODS
Subjects
The study was approved by the ethics review committee of Nagoya University Graduate School of Medicine (approval number 2015-0295). The clinical trial was registered at the University Hospital Medical Information Network (identifier UMIN000019082). This study follows the Consolidated Standards of Reporting Trials (CONSORT) guidelines. Written informed consent was obtained from 20 PD patients (Additional Table 1). Parkinsonism other than PD was excluded. All PD patients were medicated with levodopa, and no drug was changed during the study.
Additional Table 1.
Demographic features of participants
| Item | Data |
|---|---|
| Number of participants (Male/female) | 20 (8/12) |
| Age (years) | 69.0±6.8 |
| Hoehn and Yahr score | 2.3±0.8 |
| OSIT-J score at baseline | 4.7±2.2 |
| UPDRS1 score at baseline | 2.2±1.7 |
| UPDRS2 score at baseline | 13.7±9.2 |
Note: Date as expressed as the mean ± SD except number of participants. 8-OHdG: 8-Hydroxy- 2’-deoxyguanine; Cr: creatine. UPDRS: Unified Parkinson's Disease Rating Scales.
Procedures
A randomized, double-blinded, placebo-controlled, crossover trial was performed (Figure 1). Twenty PD patients were evenly divided into two groups by one of the authors, AY. At baseline, we examined olfactory function, non-motor symptoms, and ADLs, as stated below. We also collected urine for measuring 8-OHdG. Either a true or placebo hydrogen-producing machine was sent to the patient’s home and then returned after 4 weeks. The treated group received a true machine, whereas the control group received a placebo machine. After 4 weeks of inhalation (10 minutes twice per day), the same clinical and laboratory markers were examined. After an 8-week washout period, the true and placebo machines were switched, and the markers were examined before and after the 4 weeks of inhalation (10 minutes twice per day). The key was open to evaluators after the crossover trial was finished.
Figure 1.
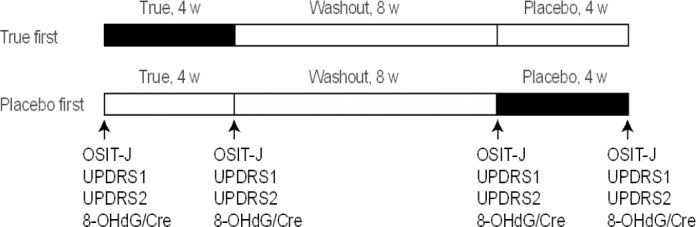
Protocol for randomized, double-blinded, placebo-controlled, crossover trial of inhalation of true and placebo hydrogen gas for 4 weeks.
Note: The odor stick identification test for Japanese (OSIT-J), the Unified Parkinson's Disease Rating Scale scores 1 and 2 (UPDRS1 and UPDRS2), and quantification of urinary 8-hydroxy-2′-deoxyguanine (8-OHdG) normalized for urinary creatinine (Cre) were performed at the indicated time points. w: Weeks.
Hydrogen-producing machine and inhalation of hydrogen gas
The true hydrogen-producing machine generated 3.0–3.5% hydrogen gas in 2 L/min of mixed air by electrolysis. Assuming that the PD patients inhaled 5 L/min of air, 3.0–3.5% hydrogen in 2 L/min of air would equate to 1.2–1.4% hydrogen-air mixture. The placebo machine was made by disconnecting an electrode for electrolysis, but still produced 2 L/min of air using the air pump. The true and placebo machines could not be differentiated without a hydrogen gas-detecting device. We previously reported that intermittent inhalation of 2% hydrogen gas for 15 minutes, 12 times a day, but not continuous inhalation of 2% hydrogen gas, improved motor deficits in a rat model of 6-hydroxydopamine-induced hemiparkinsonism.20 However, the improvement by inhalation of hydrogen gas for 15 minutes, 12 times a day, was not as effective as that by ad libitum administration of hydrogen water.18,20 To simulate a temporal profile of hydrogen concentrations akin to drinking hydrogen water, we instructed participants to inhale the gas produced by the true or placebo machine for 10 minutes in the morning and 10 minutes in the evening using a nasal cannula for 4 weeks. We confirmed after the 4 weeks that all participants complied with the instruction.
Odor examination
In the OSIT-J (Daiichi Yakuhin Sangyo Ltd., Tokyo, Japan), test odorants were microencapsulated and contained within an odorless solid cream dispensed in a lipstick container.12 The odorant was applied to a strip of paraffin paper within a 2-cm diameter circle. The paper strip was folded with the odorant inside, and rubbed together to release the odorant. The total number of correct answers for the 12 odorants made the OSIT-J score. Correct answers were not disclosed to the subjects after the examination.
Measurement of urinary 8-hydroxy-2′-deoxyguanosine
Urinary samples were kept at –20˚C before analysis. Concentrations of urinary 8-OHdG were measured by the New 8-OHdG Check ELISA (Nikken SEIL, Tokyo, Japan), and were normalized by concentrations of urinary creatinine that was measured by the Creatinine (urinary) Colorimetric Assay Kit (Cayman Chemical, Ann Arbor, MI, USA).
Unified Parkinson’s Disease Rating Scale scores
We used UDPRS scores 1 and 2 for quantitative evaluation of clinical severity of PD. UPDRS1 was a rank score for psychomotor functions and mood. UPDRS2 was a rank score for evaluating ADLs.
Statistical analysis
The data were analyzed using JMP Pro 13 (SAS Institute, Cary, NC, USA). P-values less than 0.05 by Student’s paired t-test were designated as having statistical significance. The statistical significance of differences was analyzed using one-way analysis of variance (ANOVA).
RESULTS
A randomized, double-blinded, placebo-controlled, crossover trial of inhalation of ~1.2–1.4% hydrogen-air mixture or placebo for 10 minutes twice a day for 4 weeks in 20 PD patients revealed that OSIT-J (P = 0.77), UPDSR1 (P = 0.84), and UPDRS2 (P = 0.15) were not changed by hydrogen gas (Table 1). In contrast, inhalation of hydrogen gas for 4 weeks increased urinary excretion of 8-OHdG by 16% with statistical significance (P = 0.02) (Table 1 and Figure 2).
Table 1.
Metrics before and after inhalation of true and placebo hydrogen gas for 4 weeks
| Hydrogen | Placebo | |||||
|---|---|---|---|---|---|---|
| Before | After | P | Before | After | P | |
| OSIT-J | 4.7±2.0 | 4.85±1.9 | 0.77 | 4.55±2.4 | 4.6±2.2 | 0.92 |
| UPDRS1 | 2.2±1.6 | 2.3±1.9 | 0.84 | 2.7±2.4 | 2.4±1.9 | 0.41 |
| UPDRS2 | 13.7±9.0 | 15.9±7.0 | 0.15 | 16.6±9.1 | 16.8±6.3 | 0.93 |
| 8-OHdG/Cr (ng/mg Cr) | 9.5±9.7 | 11.0±5.9 | 0.02 | 9.2±6.9 | 9.7±6.8 | 0.59 |
Note: Date are expressed as the mean ± SD. P values are calculated by paired t-test. 8-OHdG: 8-Hydroxy-2′-deoxyguanine; Cr: creatine; UPDRS: Unified Parkinson’s Disease Rating Scale.
Figure 2.
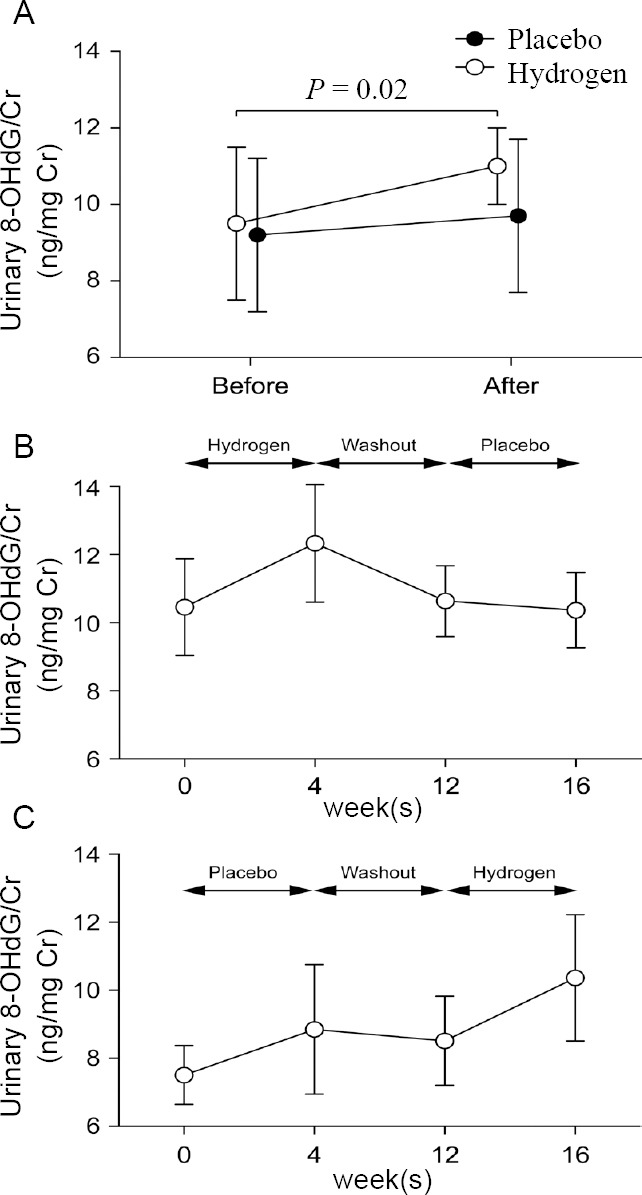
Urinary 8-OHdG/Cr before and after inhalation of true and placebo hydrogen gas for 4 weeks.
Note: (A) Twenty Parkinson's disease (PD) patients. P value by Student's paired t-test is indicated. (B) Ten PD patients who inhaled hydrogen first. (C) Ten PD patients who inhaled placebo first. (B, C) No statistical significance by one-way analysis of variance. Date are expressed as the mean ± SE. 8-OHdG: 8-Hydroxy- 2′-deoxyguanine; Cr: creatine.
DISCUSSION
Molecular hydrogen is the smallest molecule in the universe and has the highest diffusibility.24 Inhaled hydrogen gas readily enters the blood stream through the alveoli.20,25 The 1.2–1.4% hydrogen-air mixture inhaled by PD patients would increase the hydrogen concentrations at the olfactory bulbs and the alveoli by 9.4–10.9 µM according to Henry’s law. Inhalation of hydrogen gas generally elevates hydrogen concentrations more than ingestion of hydrogen water. Drinking 200-mL saturated hydrogen water (0.8 mM)20 and 530-mL hypersaturated hydrogen water (2.5 mM)26 increased the hydrogen concentrations in the organs by ~0.016 µM and ~0.21 µM, respectively. The hydrogen concentration from either inhaling or drinking returns to baseline in ~30 to 60 minutes.20,25,26
Inhalation of hydrogen gas had no effect on olfactory function, non-motor symptoms, and ADLs. Marginal improvement of OSIT-J scores of 0.15 (3.2%) by hydrogen was likely to represent a high variability of OSIT-J scores. The lack of the effect of hydrogen inhalation on olfactory function, non-motor symptoms, and ADLs may be due to a short trial period, short inhalation time (10 minutes twice a day), and/or low hydrogen concentration (1.2–1.4% hydrogen). Alternatively, these clinical features may not be sensitive enough to detect the marginal effects, if any, of hydrogen inhalation. In contrast to the lack of an improvement of clinical features, inhalation of hydrogen gas significantly increased urinary 8-OHdG levels, suggesting that hydrogen increased production of ROS. The 16% increase of 8-OHdG by hydrogen, however, is much less compared to the 53% increase by smoking 15–20 cigarettes per day,27 63% increase in prostate cancer,28 95% increase in bladder cancer,28 335% increase in non-insulin-dependent diabetes mellitus,29 and the 355% increase in insulin-dependent diabetes mellitus.29 Similarly, 30 km/d running for 8 days increases urinary 8-OHdG by 26%,30 and 60-minute exercise at 70% of maximal O2 uptake increases urinary 8-OHdG by 276%.31 In contrast to disease-associated increase in urinary 8-OHdG, the exercise-mediated increase of 8-OHdG is returned to the normal level in 2 days.31 Exercise-induced ROS32 and inflammation33 play important roles in mediating the benefits and cellular adaptations of exercise. Although we did not analyze the temporal profile of the 8-OHdG surge in our patients, rapid dissipation of hydrogen from our body20 implies that patients were temporarily exposed to ROS. Thus, inhalation of hydrogen gas for 10 minutes in our patients might have mimicked a short and mildly strenuous exercise in regard to ROS exposure.
Ohsawa et al.34 reported in 2007 that molecular hydrogen reduces hydroxyl radicals and, to a lesser extent, peroxynitrite. However, significant beneficial effects from a radical-scavenging activity of hydrogen are unlikely to occur in our body, because (i) the concentration of hydrogen is too low compared to those of nucleophilic biomolecules, (ii) hydrogen rapidly dissipates from our body, mostly in the breath, and returns to baseline in ~30 minutes,20,25 (iii) the reaction rate constant between hydrogen and hydroxyl radical is 4.2 × 107 M/s, which is three orders of magnitude slower than most reactions with hydroxyl radicals,35 and (iv) intestinal bacteria produces 12 L of hydrogen in a day by metabolizing only 40 g carbohydrate,36,37 which constantly yields on average 10 ppm (2–12 ppm) of hydrogen in our breath.20,26,38,39
Hydrogen has been reported to decrease urinary 8-OHdG,26 and tissue malondialdehyde, a marker of lipid peroxidation.40 However, in our study, inhalation of hydrogen gas mildly increased ROS production as measured by 8-OHdG. Mild increases in ROS production may provide beneficial effects by evoking hormesis. Hormesis is a physiological process, in which mitochondrial stress activates cytosolic signaling pathways to make the cells less susceptible to oxidative damage.41 Indeed, exercise-induced ROS production plays critical roles in mediating the benefits and cellular adaptations of exercise training. Consequently, ingestion of antioxidants has been reported to blunt/impair exercise training benefits.42,43 Perhaps a mild and transient increase in ROS production from H2 administration may similarly be beneficial. This hypothesis is corroborated by several other studies demonistrating that hydrogen administration increases ROS production, and are accompanied by a beneficial effect. For example, in young athletes, strenuous exercise increased the blood level of derivatives of reactive oxidative metabolites, and administration of hydrogen water mildly potentiated its increase while also suppressing the elevation of blood lactate and improving exercise-induced decline of muscle function.44 Similarly, in a mouse model of a surgically injured brain, hydrogen increased malondialdehyde in the brain while also improving cerebral edema and the neurobehavioral score.45 Likewise, inhalation of 2.9% hydrogen gas for 2 hours increased malondialdehyde in normal mouse brain ~4-fold.46 In Arabidopsis, hydrogen-rich water increased ROS production, which in turn induced drought tolerance.47 Lastly, Murakami et al. recently reported that hydrogen increases the mitochondrial membrane potential, and the production of superoxide radicals in SH-SY5Y cells.48 They also demonstrated that hydrogen-induced oxidative stress activates the Nrf2 anti-oxidative pathway, and proposed that hydrogen is a mitohormetic effector. Hydrogen-mediated activation of the Nrf2 signaling pathway has been repeatedly reported in different disease models,48,49,50,51,52,53,54,55,56 and no effect of hydrogen has been observed in Nrf2-knockout mice.50 Hormesis may also be involved in contributing to the protective effect of hydrogen on a mouse model of ventilator-induced lung injury, where hydrogen enhanced DNA binding of NF-κB in the first hour followed by its suppression in the second hour.57 Similarly, the neuroprotective effect of hydrogen in a model of subarachnoid hemorrhage in rabbits was associated with hydrogen-mediated activation of the NF-κB/Bcl-xL pathway.58 NF-κB activation in the early phase may have been induced by hydrogen-induced increase in ROS production as the hormetic mediator. We also reported by meta-analysis of gene-expression profiles of normal rodent livers that hydrogen induces heat-shock response, and subsequently leads to transient arrest of cell cycles and upregulation of collagen biosynthesis,59 which may also be a form of hormesis. Considering that the primary and long term benefits of hydrogen are unlikely due to it acting as a radical scavenger in our bodies, the mitohormetic response is an attractive and a feasible mechanism to explain the effect of hydrogen.
CONCLUSION
We observed that inhalation of ~1.2–1.4% hydrogen-air mixture for 10 minutes twice a day for 4 weeks increased urinary 8-OHdG levels by 16%, which was markedly less than the over 300% increase in diabetes, and was more comparable to the increase after a bout of strenuous exercise. Increases of oxidative stress by hydrogen have been previously reported, along with its ability to activate the Nrf2, NF-κB pathways, and heat shock responses. Although we did not observe any beneficial effect of hydrogen in our short trial, we propose that the increased 8-OHdG and other reported stress responses from hydrogen indicate that its beneficial effects are partly or largely mediated by hormetic mechanisms.
Additional file
Additional Table 1: Demographic features of participants.
Acknowledgment
We would like to thank Anzu Suzuki, Natsumi Sawada, Emiko Takano, and Momoko Suzuki for their technical assistance.
Footnotes
Funding: The study was supported by Grants-in-Aid from the Ministry of Education, Culture, Sports, Science and Technology, No. 2617K07094 (to MI); the Ministry of Health, Labor and Welfare, No. H29-Nanchi-Ipan-030 (to KO); the Japan Agency for Medical Research and Development, No. JP18gm1010002, JP18ek0109230, JP17ek010002, JP18bm0804005 (to KO); and Smoking Research Foundation and Hori Sciences and Arts Foundation (to MI).
Conflicts of interest
There is no conflict of interest.
Financial support
The study was supported by Grants-in-Aid from the Ministry of Education, Culture, Sports, Science and Technology, No. 2617K07094 (to MI); the Ministry of Health, Labor and Welfare, No. H29-Nanchi-Ipan-030 (to KO); the Japan Agency for Medical Research and Development, No. JP18gm1010002, JP18ek0109230, JP17ek010002, JP18bm0804005 (to KO); and Smoking Research Foundation and Hori Sciences and Arts Foundation (to MI).
Institutional review board statement
The study was approved by the ethics review committee of Nagoya University Graduate School of Medicine (approval number 2015-0295), and was registered at the University Hospital Medical Information Network (identifier UMIN000019082).
Declaration of patient consent
The authors certify that they have obtained patient consent forms. In the form, patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Reporting statement
This study follows the Consolidated Standards of Reporting Trials (CONSORT) guidelines.
Biostatistics statement
The statistical methods of this study were reviewed by the biostatistician of the Department of Pathophysiological Laboratory Sciences, Nagoya University Graduate School of Medicine, Nagoya, Japan.
Copyright license agreement
The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement
Individual participant data that underlie the results reported in this article, after deidentification (text, tables, figures, and appendices). Study protocol and informed consent form will be available immediately following publication, without end date. Results will be disseminated through presentations at scientific meetings and/or by publication in a peer-reviewed journal. Anonymized trial data will be available indefinitely at www.figshare.com.
Plagiarism check
Checked twice by iThenticate.
Peer review
Externally peer reviewed.
REFERENCES
- 1.Ansari KA, Johnson A. Olfactory function in patients with Parkinson’s disease. J Chronic Dis. 1975;28:493–497. doi: 10.1016/0021-9681(75)90058-2. [DOI] [PubMed] [Google Scholar]
- 2.Doty RL, Singh A, Tetrud J, Langston JW. Lack of major olfactory dysfunction in MPTP-induced parkinsonism. Ann Neurol. 1992;32:97–100. doi: 10.1002/ana.410320116. [DOI] [PubMed] [Google Scholar]
- 3.Tissingh G, Berendse HW, Bergmans P, et al. Loss of olfaction in de novo and treated Parkinson’s disease: possible implications for early diagnosis. Mov Disord. 2001;16:41–46. doi: 10.1002/1531-8257(200101)16:1<41::aid-mds1017>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 4.Schapira AHV, Chaudhuri KR, Jenner P. Non-motor features of Parkinson disease. Nat Rev Neurosci. 2017;18:509. doi: 10.1038/nrn.2017.91. [DOI] [PubMed] [Google Scholar]
- 5.Baba T, Takeda A, Kikuchi A, et al. Association of olfactory dysfunction and brain. Metabolism in Parkinson's disease. Mov Disord. 2011;26:621–628. doi: 10.1002/mds.23602. [DOI] [PubMed] [Google Scholar]
- 6.Lerner A, Bagic A. Olfactory pathogenesis of idiopathic Parkinson disease revisited. Mov Disord. 2008;23:1076–1084. doi: 10.1002/mds.22066. [DOI] [PubMed] [Google Scholar]
- 7.Duda JE, Shah U, Arnold SE, Lee VM, Trojanowski JQ. The expression of alpha-, beta-, and gamma-synucleins in olfactory mucosa from patients with and without neurodegenerative diseases. Exp Neurol. 1999;160:515–522. doi: 10.1006/exnr.1999.7228. [DOI] [PubMed] [Google Scholar]
- 8.Tofaris GK, Garcia Reitbock P, Humby T, et al. Pathological changes in dopaminergic nerve cells of the substantia nigra and olfactory bulb in mice transgenic for truncated human alpha-synuclein(1-120): implications for Lewy body disorders. J Neurosci. 2006;26:3942–3950. doi: 10.1523/JNEUROSCI.4965-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Doty RL, Shaman P, Kimmelman CP, Dann MS. University of Pennsylvania Smell Identification Test: a rapid quantitative olfactory function test for the clinic. Laryngoscope. 1984;94:176–178. doi: 10.1288/00005537-198402000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Hummel T, Sekinger B, Wolf SR, Pauli E, Kobal G. ‘Sniffin’ sticks’: olfactory performance assessed by the combined testing of odor identification, odor discrimination and olfactory threshold. Chem Senses. 1997;22:39–52. doi: 10.1093/chemse/22.1.39. [DOI] [PubMed] [Google Scholar]
- 11.Saito S, Ayabe-Kanamura S, Takashima Y, et al. Development of a smell identification test using a novel stick-type odor presentation kit. Chem Senses. 2006;31:379–391. doi: 10.1093/chemse/bjj042. [DOI] [PubMed] [Google Scholar]
- 12.Iijima M, Kobayakawa T, Saito S, et al. Smell identification in Japanese Parkinson’s disease patients: using the odor stick identification test for Japanese subjects. Intern Med. 2008;47:1887–1892. doi: 10.2169/internalmedicine.47.1345. [DOI] [PubMed] [Google Scholar]
- 13.Braak H, Del Tredici K, Bratzke H, Hamm-Clement J, Sandmann-Keil D, Rub U. Staging of the intracerebral inclusion body pathology associated with idiopathic Parkinson’s disease (preclinical and clinical stages) J Neurol. 2002;249:1–5. doi: 10.1007/s00415-002-1301-4. [DOI] [PubMed] [Google Scholar]
- 14.Dias V, Junn E, Mouradian MM. The role of oxidative stress in Parkinson’s disease. J Parkinsons Dis. 2013;3:461–491. doi: 10.3233/JPD-130230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sato S, Mizuno Y, Hattori N. Urinary 8-hydroxydeoxyguanosine levels as a biomarker for progression of Parkinson disease. Neurology. 2005;64:1081–1083. doi: 10.1212/01.WNL.0000154597.24838.6B. [DOI] [PubMed] [Google Scholar]
- 16.Hirayama M, Nakamura T, Watanabe H, et al. Urinary 8-hydroxydeoxyguanosine correlate with hallucinations rather than motor symptoms in Parkinson’s disease. Parkinsonism Relat Disord. 2011;17:46–49. doi: 10.1016/j.parkreldis.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 17.Ilida A, Nosaka N, Yumoto T, et al. The clinical application of hydrogen as a medical treatment. Acta Med Okayama. 2016;70:331–337. doi: 10.18926/AMO/54590. [DOI] [PubMed] [Google Scholar]
- 18.Fu Y, Ito M, Fujita Y, et al. Molecular hydrogen is protective against 6-hydroxydopamine-induced nigrostriatal degeneration in a rat model of Parkinson’s disease. Neurosci Lett. 2009;453:81–85. doi: 10.1016/j.neulet.2009.02.016. [DOI] [PubMed] [Google Scholar]
- 19.Fujita K, Seike T, Yutsudo N, et al. Hydrogen in drinking water reduces dopaminergic neuronal loss in the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine mouse model of Parkinson’s disease. PLoS One. 2009;4:e7247. doi: 10.1371/journal.pone.0007247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ito M, Hirayama M, Yamai K, et al. Drinking hydrogen water and intermittent hydrogen gas exposure, but not lactulose or continuous hydrogen gas exposure, prevent 6-hydorxydopamine-induced Parkinson’s disease in rats. Med Gas Res. 2012;2:15. doi: 10.1186/2045-9912-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yoritaka A, Takanashi M, Hirayama M, Nakahara T, Ohta S, Hattori N. Pilot study of H2 therapy in Parkinson’s disease: a randomized double-blind placebo-controlled trial. Mov Disord. 2013;28:836–839. doi: 10.1002/mds.25375. [DOI] [PubMed] [Google Scholar]
- 22.Katsumata Y, Sano F, Abe T, et al. The effects of hydrogen gas inhalation on adverse left ventricular remodeling after percutaneous coronary intervention for ST-elevated myocardial infarction-first pilot study in humans. Circ J. 2017;81:940–947. doi: 10.1253/circj.CJ-17-0105. [DOI] [PubMed] [Google Scholar]
- 23.Ono H, Nishijima Y, Ohta S, et al. Hydrogen gas inhalation treatment in acute cerebral infarction: a randomized controlled clinical study on safety and neuroprotection. J Stroke Cerebrovasc Dis. 2017;26:2587–2594. doi: 10.1016/j.jstrokecerebrovasdis.2017.06.012. [DOI] [PubMed] [Google Scholar]
- 24.Venetsanos AG, Huld T, Adams P, Bartzis JG. Source, dispersion and combustion modelling of an accidental release of hydrogen in an urban environment. J Hazard Mater. 2003;105:1–25. doi: 10.1016/j.jhazmat.2003.05.001. [DOI] [PubMed] [Google Scholar]
- 25.Sobue S, Yamai K, Ito M, et al. Simultaneous oral and inhalational intake of molecular hydrogen additively suppresses signaling pathways in rodents. Mol Cell Biochem. 2015;403:231–241. doi: 10.1007/s11010-015-2353-y. [DOI] [PubMed] [Google Scholar]
- 26.Ishibashi T, Sato B, Rikitake M, et al. Consumption of water containing a high concentration of molecular hydrogen reduces oxidative stress and disease activity in patients with rheumatoid arthritis: an open-label pilot study. Med Gas Res. 2012;2:27. doi: 10.1186/2045-9912-2-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yamaguchi Y, Haginaka J, Morimoto S, Fujioka Y, Kunitomo M. Facilitated nitration and oxidation of LDL in cigarette smokers. Eur J Clin Invest. 2005;35:186–193. doi: 10.1111/j.1365-2362.2005.01472.x. [DOI] [PubMed] [Google Scholar]
- 28.Wu LL, Chiou CC, Chang PY, Wu JT. Urinary 8-OHdG: a marker of oxidative stress to DNA and a risk factor for cancer, atherosclerosis and diabetics. Clin Chim Acta. 2004;339:1–9. doi: 10.1016/j.cccn.2003.09.010. [DOI] [PubMed] [Google Scholar]
- 29.Dandona P, Thusu K, Cook S, et al. Oxidative damage to DNA in diabetes mellitus. Lancet. 1996;347:444–445. doi: 10.1016/s0140-6736(96)90013-6. [DOI] [PubMed] [Google Scholar]
- 30.Okamura K, Doi T, Hamada K, et al. Effect of repeated exercise on urinary 8-hydroxy-deoxyguanosine excretion in humans. Free Radic Res. 1997;26:507–514. doi: 10.3109/10715769709097821. [DOI] [PubMed] [Google Scholar]
- 31.Orhan H, van Holland B, Krab B, et al. Evaluation of a multi-parameter biomarker set for oxidative damage in man: increased urinary excretion of lipid, protein and DNA oxidation products after one hour of exercise. Free Radic Res. 2004;38:1269–1279. doi: 10.1080/10715760400013763. [DOI] [PubMed] [Google Scholar]
- 32.Gomes EC, Silva AN, de Oliveira MR. Oxidants, antioxidants, and the beneficial roles of exercise-induced production of reactive species. Oxid Med Cell Longev. 2012;2012:756132. doi: 10.1155/2012/756132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pedersen BK, Akerstrom TC, Nielsen AR, Fischer CP. Role of myokines in exercise and metabolism. J Appl Physiol (1985) 2007;103:1093–1098. doi: 10.1152/japplphysiol.00080.2007. [DOI] [PubMed] [Google Scholar]
- 34.Ohsawa I, Ishikawa M, Takahashi K, et al. Hydrogen acts as a therapeutic antioxidant by selectively reducing cytotoxic oxygen radicals. Nat Med. 2007;13:688–694. doi: 10.1038/nm1577. [DOI] [PubMed] [Google Scholar]
- 35.Buxton GV, Greenstock CL, Helman WP, Ross AB. Critical view of rate constants for reactions of hydrated electrons, hydrogen atoms and hydroxyl radicals (•OH/•OH–) in aqueous solution. J Phys Chem Ref Data. 1988;17:513–886. [Google Scholar]
- 36.Christl SU, Murgatroyd PR, Gibson GR, Cummings JH. Production, metabolism, and excretion of hydrogen in the large intestine. Gastroenterology. 1992;102:1269–1277. [PubMed] [Google Scholar]
- 37.Strocchi A, Levitt MD. Maintaining intestinal H2 balance: credit the colonic bacteria. Gastroenterology. 1992;102:1424–1426. doi: 10.1016/0016-5085(92)90790-6. [DOI] [PubMed] [Google Scholar]
- 38.Perman JA, Modler S, Barr RG, Rosenthal P. Fasting breath hydrogen concentration: normal values and clinical application. Gastroenterology. 1984;87(6):1358–1363. [PubMed] [Google Scholar]
- 39.Sone Y, Tanida S, Matsubara K, et al. Everyday breath hydrogen excretion profile in Japanese young female students. J Physiol Anthropol Appl Human Sci. 2000;19:229–237. doi: 10.2114/jpa.19.229. [DOI] [PubMed] [Google Scholar]
- 40.Nakao A, Kaczorowski DJ, Wang Y, et al. Amelioration of rat cardiac cold ischemia/reperfusion injury with inhaled hydrogen or carbon monoxide, or both. J Heart Lung Transplant. 2010;29:544–553. doi: 10.1016/j.healun.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 41.Yun J, Finkel T. Mitohormesis. Cell Metab. 2014;19:757–766. doi: 10.1016/j.cmet.2014.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ristow M, Zarse K, Oberbach A, et al. Antioxidants prevent health-promoting effects of physical exercise in humans. Proc Natl Acad Sci U S A. 2009;106:8665–8670. doi: 10.1073/pnas.0903485106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gomez-Cabrera MC, Salvador-Pascual A, Cabo H, Ferrando B, Vina J. Redox modulation of mitochondriogenesis in exercise. Does antioxidant supplementation blunt the benefits of exercise training? Free Radic Biol Med. 2015;86:37–46. doi: 10.1016/j.freeradbiomed.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 44.Aoki K, Nakao A, Adachi T, Matsui Y, Miyakawa S. Pilot study: Effects of drinking hydrogen-rich water on muscle fatigue caused by acute exercise in elite athletes. Med Gas Res. 2012;2:12. doi: 10.1186/2045-9912-2-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Han L, Tian R, Yan H, et al. Hydrogen-rich water protects against ischemic brain injury in rats by regulating calcium buffering proteins. Brain Res. 2015;1615:129–138. doi: 10.1016/j.brainres.2015.04.038. [DOI] [PubMed] [Google Scholar]
- 46.Matchett GA, Fathali N, Hasegawa Y, et al. Hydrogen gas is ineffective in moderate and severe neonatal hypoxia-ischemia rat models. Brain Res. 2009;1259:90–97. doi: 10.1016/j.brainres.2008.12.066. [DOI] [PubMed] [Google Scholar]
- 47.Xie Y, Mao Y, Zhang W, Lai D, Wang Q, Shen W. Reactive oxygen species-dependent nitric oxide production contributes to hydrogen-promoted stomatal closure in Arabidopsis. Plant Physiol. 2014;165:759–773. doi: 10.1104/pp.114.237925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Murakami Y, Ito M, Ohsawa I. Molecular hydrogen protects against oxidative stress-induced SH-SY5Y neuroblastoma cell death through the process of mitohormesis. PLoS One. 2017;12:e0176992. doi: 10.1371/journal.pone.0176992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Spulber S, Edoff K, Hong L, Morisawa S, Shirahata S, Ceccatelli S. Molecular hydrogen reduces LPS-induced neuroinflammation and promotes recovery from sickness behaviour in mice. PLoS One. 2012;7(7):e42078. doi: 10.1371/journal.pone.0042078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kawamura T, Wakabayashi N, Shigemura N, et al. Hydrogen gas reduces hyperoxic lung injury via the Nrf2 pathway in vivo. Am J Physiol Lung Cell Mol Physiol. 2013;304:646–656. doi: 10.1152/ajplung.00164.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhai X, Chen X, Shi J, et al. Lactulose ameliorates cerebral ischemia-reperfusion injury in rats by inducing hydrogen by activating Nrf2 expression. Free Radic Biol Med. 2013;65:731–741. doi: 10.1016/j.freeradbiomed.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 52.Li DZ, Zhang QX, Dong XX, Li HD, Ma X. Treatment with hydrogen molecules prevents RANKL-induced osteoclast differentiation associated with inhibition of ROS formation and inactivation of MAPK, AKT and NF-kappa B pathways in murine RAW264.7 cells. J Bone Miner Metab. 2014;32:494–504. doi: 10.1007/s00774-013-0530-1. [DOI] [PubMed] [Google Scholar]
- 53.Xie Q, Li XX, Zhang P, et al. Hydrogen gas protects against serum and glucose deprivationinduced myocardial injury in H9c2 cells through activation of the NFE2related factor 2/heme oxygenase 1 signaling pathway. Mol Med Rep. 2014;10:1143–1149. doi: 10.3892/mmr.2014.2283. [DOI] [PubMed] [Google Scholar]
- 54.Song G, Zong C, Zhang Z, et al. Molecular hydrogen stabilizes atherosclerotic plaque in low-density lipoprotein receptor-knockout mice. Free Radic Biol Med. 2015;87:58–68. doi: 10.1016/j.freeradbiomed.2015.06.018. [DOI] [PubMed] [Google Scholar]
- 55.Li Y, Li Q, Chen H, et al. Hydrogen gas alleviates the intestinal injury caused by severe sepsis in mice by increasing the expression of heme oxygenase-1. Shock. 2015;44:90–98. doi: 10.1097/SHK.0000000000000382. [DOI] [PubMed] [Google Scholar]
- 56.Li Y, Xie K, Chen H, Wang G, Yu Y. Hydrogen gas inhibits high-mobility group box 1 release in septic mice by upregulation of heme oxygenase 1. J Surg Res. 2015;196:136–148. doi: 10.1016/j.jss.2015.02.042. [DOI] [PubMed] [Google Scholar]
- 57.Huang CS, Kawamura T, Peng X, et al. Hydrogen inhalation reduced epithelial apoptosis in ventilator-induced lung injury via a mechanism involving nuclear factor-kappa B activation. Biochem Biophys Res Commun. 2011;408:253–258. doi: 10.1016/j.bbrc.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 58.Zhuang Z, Sun XJ, Zhang X, et al. Nuclear factor-kappaB/Bcl-XL pathway is involved in the protective effect of hydrogen-rich saline on the brain following experimental subarachnoid hemorrhage in rabbits. J Neurosci Res. 2013;91:1599–1608. doi: 10.1002/jnr.23281. [DOI] [PubMed] [Google Scholar]
- 59.Nishiwaki H, Ito M, Negishi S, Sobue S, Ichihara M, Ohno K. Molecular hydrogen upregulates heat shock response and collagen biosynthesis, and downregulates cell cycles: meta-analyses of gene expression profiles. Free Radic Res. 2018;52:434–445. doi: 10.1080/10715762.2018.1439166. [DOI] [PubMed] [Google Scholar]


