Abstract
This study reported the frequency of anesthetic overdose measured with the bispectral index in a high altitude city (Bogotá-Colombia, 2600 meters above sea level). We assembled a prospective cohort of patients. Preoperative variables were described, and 10 minutes after the surgical incision, bispectral index, mean alveolar concentration, mean arterial pressure, and oxygen saturation were recorded. Bispectral index was classified as superficial (60), adequate (40–60), and deep (> 40). Mean alveolar concentration was classified as low (< 0.8), normal (0.8–1.2), and high (> 1.2). We included 50 patients. The mean age of the patients was 36.3 ± 13.5 years; 48% were male and 78% were categorized as ASA I. Mean values of mean alveolar concentration and bispectral index were 1.14 ± 0.18 and 38.66 ± 6.9, respectively. Frequency of anesthetic overdose measured with bispectral index was 54% and only 20% with mean alveolar concentration. In total, 78% of patients received normal mean alveolar concentration values, and among these patients, 49% had deep bispectral index levels and 51% were adequate. There was no correlation between mean alveolar concentration and bispectral index (Pearson r = 0.161, P = 0.246) or between bispectral index and mean arterial pressure (Pearson r = 0.367, P = 0.08). All patients older than 60 years exhibited deep bispectral index levels, and although we did not identify a correlation between age and bispectral index, a tendency was observed (Pearson r = –0.087, P = 0.538). Safe and effective anesthesia overdose could be a common phenomenon. Bispectral index-guided anesthesia could be a helpful and reliable tool in the assessment and prevention of anesthesia overdose at high altitude. The study was approved by the ethics committee of the Fundación Cardioinfantil-Instituto de cardiología, Bogota, Colombia (approved number: 312017).
Keywords: general anesthesia, drug overdose, biespectral index, mean alveolar concentration, altitude, inhalation, intraoperative awareness
INTRODUCTION
Mean alveolar concentration (MAC) has been used as an indicator of the hypnotic component of anesthesia. Its reliability has been questioned due to its changes with physiological variables, pathologies, and barometric pressure.1 In addition, MAC describes the inhibition of movement response to noxious stimulation.2 Anesthetic overdose with MAC-guided anesthesia is not uncommon and can result in increased risk of complications such as prolonged recovery time, upper respiratory obstruction, post-operative delirium, length of stay, and nausea or vomiting, especially in patients with fragility.3 Under dosage can increase the risk of intraoperative awareness.4
Anesthesia overdose is not related to hemodynamic parameters. Hence, in order to assess the level of consciousness and prevent anesthesia overdose bispectral index (BIS) was introduced. BIS is an analysis of the patient’s electroencephalogram during general anesthesia that evaluates anesthetic depth and has shown a high level of accuracy.3
The consequences of altitude on the partial pressure and density of anesthetic gases have been described. The behaviors of flowmeters and vaporizers are not constant in hypobaric conditions, and MAC is not as reliable as it is at sea level due to Dalton’s law (as atmospheric pressure decreases with elevation, the partial oxygen pressure declines).5 Thus, at high altitudes, anesthesiologists try to compensate for the hypobaric environment with a higher MAC, which in turn could increase the risk of anesthetic overdose. Safe and effective anesthesia at high altitude is a challenge for anesthesiologists and approximately 140 million people worldwide live at altitudes above 2500 m (8000 ft).5
Therefore, this study reports the frequency of anesthetic overdose measured with the BIS in a high altitude city (Bogotá-Colombia, 2600 m [8661 ft] above sea level) when inhalation anesthesia is guided by MAC. This study seeks to improve anesthesia at high-altitude, document and diminish the rate of anesthesia overdose, and promote the use BIS-guided anesthesia.
SUBJECTS AND METHODS
Subjects
We assembled a prospective cohort of patients who underwent low-risk surgeries at Fundacion Cardioinfantil-Instituto de Cardiologia, with an American Society of Anesthesiologists (ASA) physical status examination of I or II. All patients received inhalation anesthesia with sevoflurane.
Exclusion criteria were the presence of a neurological disease, use of anticonvulsive medication, alcohol abuse, and previous intraoperative recall. To avoid bias, the anesthesiologists in charge of the cases did not know the patient was selected for the study. All patients provided written consent to participate in the study, and the study was approved by the ethics committee of the Fundación Cardioinfantil-Instituto de Cardiología (approval number: 312017). This study follows the Consolidated Standards of Reporting Trials (CONSORT) guidelines.
Variables
Before the procedure, preoperative variables were collected. Ten minutes after the surgical incision BIS, MAC, mean arterial pressure (MAP), and oxygen saturation variables were measured and documented for the study. BIS values were classified as superficial (> 60), adequate (40–60), and deep (> 40). MAC was classified as low (< 0.8), normal (0.8–1.2), and high (> 1.2).
Bispectral index
All patients received MAC guided anesthesia and BIS was measured separately 10 minutes after the surgical incision. For BIS measurements, we used the BIS QUATROTM sensors (Coviden Ireland Limited, IDA Business & Technology Park, Tullamore). Previous to sensor positioning, we wiped the skin of the patients with dry alcohol. Then we position the sensor diagonally on the forehead, the edges of the sensors were pressed to assure correct adhesion. Finally, the sensor was tab into patients interface cable.
The sensor was connected to a BIS VISTA TM MONITORING SYSTEM (Aspect Medical System Inc., One Upland Road, Norwood, MA, USA).
Statistical analysis
Baseline demographics and clinical characteristics were summarized using descriptive statistics. For continuous variables, data are presented as the mean or median, and standard deviations or interquartile range. The frequency of anesthetic overdose was described. We performed a Pearson correlation coefficient between MAP and BIS, age and BIS, and MAC and BIS. Statistical analysis was performed with the Stata SE 14 program (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX, USA: StataCorp LP). A significance level of 0.05 was used throughout the analysis.
RESULTS
Overall, 50 patients were included in the study, with a mean age of 36.3 ± 13.5 years, 48% were male, and 78% were categorized as ASA I. The mean values of MAC and BIS were 1.14 ± 0.18 and 38.66 ± 6.9, respectively (Table 1). Twenty-six (42%) patients underwent a general surgery procedure, 14 (28%) orthopedic, 6 (3%) gynecologic, 3 (1.5%) urologic, and one (0.5%) thoracic.
Table 1.
Preoperative variables
| Variables | n (StD) |
|---|---|
| Male (%) | 24 (48) |
| Age (years) | 36.3 (13.5) |
| Weight (kg) | 69.8 (12.3) |
| Height (cm) | 167 (9.1) |
| BMI (kg/m2) | 24.9 (3.8) |
| BIS | 38.6 (6.9) |
| ASA I | 39 (78) |
| Heart rate (beats/min) | 65 (10.9) |
| MAC | 1.14 (0.1) |
Note: ASA: American Society of Anesthesiologists physical status examination; BMI: body mass index; BIS: bispectral index; MAC: mean alveolar concentration.
The frequency of anesthetic overdose measured with BIS was 54% (Figure 1). Seventy-eight percent of the patients received normal MAC values, and among these patients, 49% exhibited deep and 51% adequate BIS values. Ten patients received high MAC values. Amongst them, 70% had deep and 30% adequate BIS levels. Only one patient received a low MAC value, that patient had a deep BIS level (Figure 2). We did not find any correlation between MAC and BIS (Pearson r = 0.161, P = 0.246) or between BIS and MAP (Pearson r = 0.367, P = 0.08).
Figure 1.
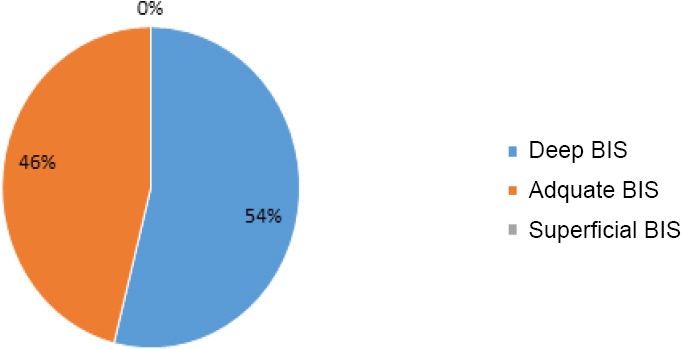
The frequency of anesthetic overdose with MAC-guided anesthesia.
Note: Forty-six percent of the patients had adequate BIS levels and 54% had deep BIS levels. MAC: Mean alveolar concentration; BIS: bispectral index.
Figure 2.
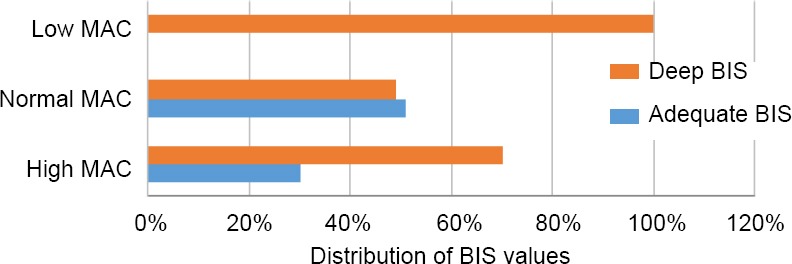
Distribution of BIS values according to MAC categories.
Note: Twenty percent of patients received high MAC values. Amongst them, 70% had deep and 30% adequate BIS levels. Seventy-eight percent of the patients received normal MAC values, and among these patients, 49% exhibited deep and 51% adequate BIS values. All patients that received low MAC values had deep BIS levels. MAC: Mean alveolar concentration; BIS: bispectral index.
The distribution of BIS values in MAP categories is described in Figure 3. Overall, 70% of the patients with MAP > 90 mmHg had adequate BIS levels, and 66% of the patients with MAP < 60 mmHg had adequate BIS levels. All patients older than 60 years and 65% of the patients between 36–59 years had deep BIS levels. Although no correlation was found between age and BIS, a tendency was observed between the variables (Pearson r = –0.087, P = 0.538) (Figure 4). The overdose frequency measured with BIS was 54% and 20% with MAC.
Figure 3.
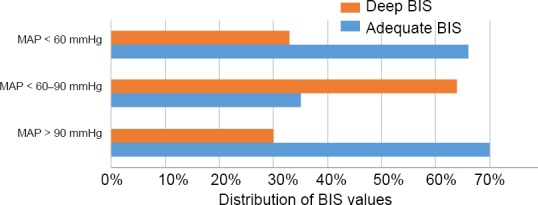
Distribution of BIS values according to MAP categories (< 60 mmHg, 60–90 mmHg, > 90 mmHg).
Note: Seventy percent of the patients with MAP > 90 mmHg had adequate BIS levels, and 66% of the patients with MAP < 60 mmHg had adequate BIS levels. All patients older than 60 years and 65% of the patients between 36–59 years had deep BIS levels. MAP: Mean arterial pressure; BIS: bispectral index.
Figure 4.
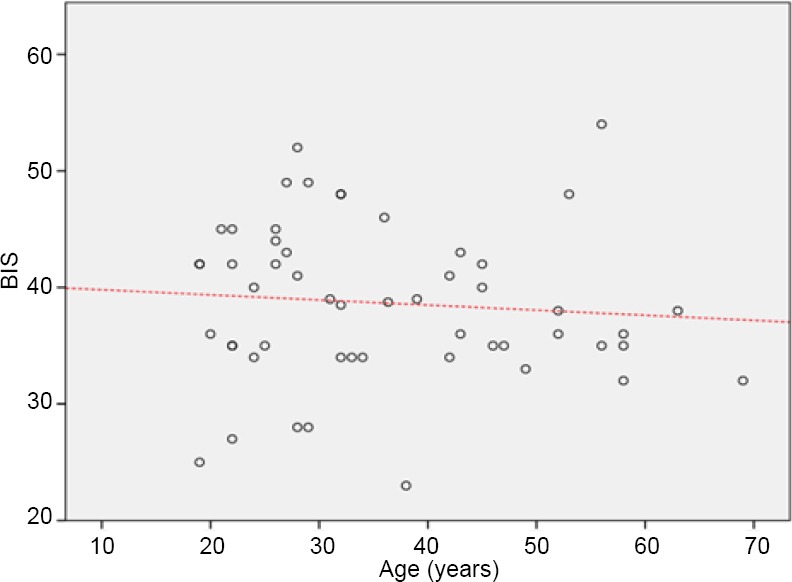
Correlation between age and BIS levels.
Note: No correlation was found between age and BIS (Pearson r = –0.087, P = 0.538). BIS: Bispectral index.
DISCUSSION
Achieving and maintaining optimal anesthetic depth is challenging for anesthesiologists. It requires creating a balance between the administration of the anesthetic agent and the response inhibition to surgical stimuli.6,7 Achieving adequate anesthetic depth can prevent intraoperative awareness, upper respiratory obstruction, and post-operatory delirium, provide optimal conditions for surgery, and shorten recovery time, especially in patients with fragility.8 The present study evaluated the level of anesthetic depth using BIS, to establish whether the administration of MAC-guided anesthesia is associated with anesthetic overdose at high altitude.
Tracking anesthetic depth is essential to achieve an adequate dosage of anesthetic agents.6,9,10 BIS monitors process a cortical electroencephalographic signal, which provides an indirect measurement of the conscious level. BIS values range from 0–100, where 0 corresponds to the absence of brain activity and 100 corresponds to the awake state. Values from 40–60 reflect an adequate hypnotic plane in patients undergoing surgery.9,11,12 Punjasawadwong et al.9 concluded that BIS values ranging from 40–60 could decrease the anesthetic consumption and the postoperative recovery time (eye opening, response to orders, extubation, and length of stay).
More than 50% of our patients and all patients older than 60 years had BIS values < 40 with MAC-guided anesthesia. Monk et al.13 described an association between low BIS values and worse survival, due to the possible toxic effects of volatile anesthesia on brain cells. Other studies have described an association between BIS values less than 45 and mortality.7,14
In the long-term follow-up of the B-Aware trial,15 patients with BIS values < 40 for more than 5 minutes had a higher risk of death. In the subgroup of cardiac surgery, a greater cumulative duration of BIS < 45 was associated with worse long-term survival, acute myocardial infarction, and stroke. One limitation of this study was the lack of availability of covariates, such as information on intraoperative hypotension, which has been independently associated with poor results.3
Currently, MAC-guided anesthesia has some flaws. MAC describes the inhibition of movement response to noxious stimulation and is modified by several factors, including age, obesity, temperature, sodium concentration, anemia, genetic mutations, diseases, and barometric pressure.6,8 The immobilizing potency of the anesthetic reflects its effects on the spinal cord rather than the state of consciousness. This could explain why 49% of patients with adequate MAC had deep BIS values. In clinical practice, a number of factors encourage anesthesiologists to use high MAC values, such as intraoperative recall, good surgical conditions, and fewer dose adjustments.2
We did not find a relationship between anesthetic depth (measured with BIS) and hemodynamic variables (MAP and heart rate).16 These results are consistent with the literature. A patient’s movements in response to noxious stimulation, hypertension, tachycardia, and lacrimation, despite being important signs, are unreliable, and are not related to the state of consciousness.16
The use of BIS-guided anesthesia has been shown to diminish anesthetic dosage, reduce secondary effects, and achieve a faster recovery.9 Oversee of cortical functions with BIS provides a more accurate measurement and helps determine the correct dose of hypnotics. The frequency of anesthetic overdose was higher than expected in a group of low-risk patients; this raises concern, as MAC-guided anesthesia may not be a reliable method at high altitude. Anesthesiologists may try to compensate for the hypobaric environment using a higher MAC, which could lead to an increased risk of anesthetic overdose. Therefore, BIS is an important tool that could help the anesthesiologist prevent hypnotic overdosage and improve the length of stay and post-operatory outcomes in low-risk patients. However, larger studies are needed, so the physiological effects of anesthesia gases at high altitude can be analyzed, and the MAC level can be standardized based on altitude.
There are still some limitations. The first limitation is the sample size. Larger studies with higher potency are needed, so stronger conclusions can be made. Additionally, this study reflects a single center experience.
To conclude, safe and effective anesthesia at high altitude is a challenge for the anesthesiologist and anesthesia overdose could be a common phenomenon. The frequency of anesthetic overdose with adequate MAC was higher than expected and we did not find a clear relationship between BIS and MAC, or vital signs and anesthesia overdose. MAC-guided anesthesia is not as reliable as previously believed. BIS-guided anesthesia can be a helpful tool for the anesthesiologist at high altitude to prevent overdose.
Acknowledgment
We would like to thank the research department for the advisory and corrections given for this manuscript.
Footnotes
Conflicts of interest
There is no conflict of interest.
Financial support
None.
Institutional review board statement
The study was approved by the ethics committee of the Fundación Cardioinfantil-Instituto de cardiología, Bogota, Colombia (approved number: 312017).
Declaration of patient consent
The authors certify that they have obtained patient consent forms. In the form, patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Reporting statement
This study follows the Consolidated Standards of Reporting Trials (CONSORT) guidelines.
Biostatistics statement
The statistical methods of this study were reviewed by the biostatistician of the Universidad del Rosario.
Copyright license agreement
The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement
Individual participant data that underlie the results reported in this article, after deidentification (text, tables, figures, and appendices). Study protocol and informed consent form will be available immediately following publication, without end date. Results will be disseminated through presentations at scientific meetings and/or by publication in a peer-reviewed journal. Anonymized trial data will be available indefinitely at www.figshare.com.
Plagiarism check
Checked twice by iThenticate.
Peer review
Externally peer reviewed.
REFERENCES
- 1.James MF, White JF. Anesthetic considerations at moderate altitude. Anesth Analg. 1984;63:1097–1105. [PubMed] [Google Scholar]
- 2.Duarte LTD, Saraiva, RA Immobility: essential inhalational anesthetics action. Rev Bras Anestesiol. 2005;55:100–117. doi: 10.1590/s0034-70942005000100013. [DOI] [PubMed] [Google Scholar]
- 3.Short TG, Leslie K, Campbell D, et al. A pilot study for a prospective, randomized, double-blind trial of the influence of anesthetic depth on long-term outcome. Anesth Analg. 2014;118:981–986. doi: 10.1213/ANE.0000000000000209. [DOI] [PubMed] [Google Scholar]
- 4.Sanders RD, Tononi G, Laureys S, Sleigh JW. Unresponsiveness ≠ unconsciousness. Anesthesiology. 2012;116:946–959. doi: 10.1097/ALN.0b013e318249d0a7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leissner KB, Mahmood FU. Physiology and pathophysiology at high altitude: Considerations for the anesthesiologist. J Anesth. 2009;23:543–553. doi: 10.1007/s00540-009-0787-7. [DOI] [PubMed] [Google Scholar]
- 6.Aranake A, Mashour GA, Avidan MS. Minimum alveolar concentration: ongoing relevance and clinical utility. Anaesthesia. 2013;68:512–522. doi: 10.1111/anae.12168. [DOI] [PubMed] [Google Scholar]
- 7.Eger EI. Age, minimum alveolar anesthetic concentration, and minimum alveolar anesthetic concentration-awake. Anesth Analg. 2001;93:947–953. doi: 10.1097/00000539-200110000-00029. [DOI] [PubMed] [Google Scholar]
- 8.Kim JK, Kim DK, Lee MJ. Relationship of bispectral index to minimum alveolar concentration during isoflurane, sevoflurane or desflurane anaesthesia. J Int Med Res. 2014;42:130–137. doi: 10.1177/0300060513505525. [DOI] [PubMed] [Google Scholar]
- 9.Punjasawadwong Y, Phongchiewboon A, Bunchungmongkol N. Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database Syst Rev. 2014;17:38–43. doi: 10.1002/14651858.CD003843.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Noreika V, Jylhänkangas L, Móró L, et al. Consciousness lost and found: subjective experiences in an unresponsive state. Brain Cogn. 2011;77:327–334. doi: 10.1016/j.bandc.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 11.Cook TM. Anesthesia awareness and the bispectral index. N Engl J Med. 2008;359:430–431. [PubMed] [Google Scholar]
- 12.Recart A, Gasanova I, White PF, et al. The effect of cerebral monitoring on recovery after general anesthesia: a comparison of the auditory evoked potential and bispectral index devices with standard clinical practice. Anesth Analg. 2003;97:1667–1674. doi: 10.1213/01.ANE.0000087041.63034.8C. [DOI] [PubMed] [Google Scholar]
- 13.Monk TG, Saini V, Weldon BC, Sigl JC. Anesthetic management and one-year mortality after noncardiac surgery. Anesth Analg. 2005;100:4–10. doi: 10.1213/01.ANE.0000147519.82841.5E. [DOI] [PubMed] [Google Scholar]
- 14.Davidson AJ, Czarnecki C. The bispectral index in children: comparing isoflurane and halothane. Br J Anaesth. 2004;92:14–17. doi: 10.1093/bja/aeh011. [DOI] [PubMed] [Google Scholar]
- 15.Leslie K, Myles PS, Forbes A, Chan MTV. The effect of bispectral index monitoring on long-term survival in the B-aware trial. Anesth Analg. 2010;110:816–822. doi: 10.1213/ANE.0b013e3181c3bfb2. [DOI] [PubMed] [Google Scholar]
- 16.Musizza B, Ribaric S. Monitoring the depth of anaesthesia. Sensors. 2010;10:10896–10935. doi: 10.3390/s101210896. [DOI] [PMC free article] [PubMed] [Google Scholar]


