Abstract
Adenoid cystic carcinoma of the buccal mucosa has an increased propensity for recurrence and distant metastases. Due to the poor prognosis at late detection of distant metastases, it is advisable to keep a close follow-up. In the present case, 18F-fluorodeoxyglucose positron emission tomography/computed tomography proved invaluable in the comprehensive workup of the patient, including detection of local recurrence, distant metastases, and in assessing treatment response.
Keywords: 18F-fluorodeoxyglucose positron emission tomography/computed tomography, adenoid cystic carcinoma, lung metastasis, positron emission tomography/computed tomography-guided biopsy, response evaluation
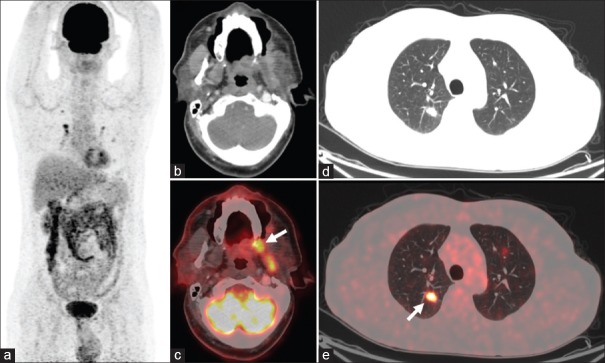
A 54-year-old male presented with pain in the left cheek for 2 months. Five years back, he had undergone wide local excision with left segmental mandibulectomy and lymph nodal dissection, followed by radiotherapy for carcinoma of the left buccal mucosa, which revealed adenoid cystic carcinoma (ACC) in postoperative histopathology. In view of this past history, 18F-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) was performed for recurrence evaluation. Maximum-intensity projection [Figure 1a], transaxial CT, and fused PET/CT images revealed FDG-avid lesion in the region of left retromolar trigone [arrow; Figure 1b and c; SUVmax 9.3] and buccal mucosa, eroding the adjoining alveolar plate and involving the left lateral pterygoid muscle. Multiple FDG-avid parenchymal nodules [arrow; Figure 1d and e; SUVmax 11.6] were also noted in bilateral lung fields.
Figure 1.
18F-fluorodeoxyglucose positron emission tomography/computed tomography maximum-intensity projection (a), transaxial computed tomography, and fused positron emission tomography/computed tomography images showing fluorodeoxyglucose-avid lesion in the region of left retromolar trigone (arrow; b and c) and buccal mucosa, eroding the adjoining alveolar plate and involving the left lateral pterygoid muscle. Multiple fluorodeoxyglucose-avid parenchymal nodules (arrow; d and e) noted in the bilateral lung fields
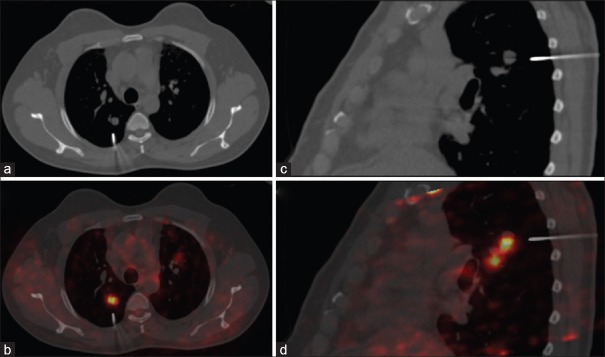
With suspicion of pulmonary metastasis, the patient was scheduled for 18F-FDG PET/CT-guided biopsy from the parenchymal nodule in the right lung. With the patient in prone position, the nodule with the maximum FDG uptake was selected for performing needle biopsy. Transaxial [Figure 2a and b] and sagittal [Figure 2c and d] CT and fused PET/CT images confirmed the correct positioning of the needle. Histopathology of the biopsy specimen confirmed metastatic ACC.
Figure 2.
18F-fluorodeoxyglucose positron emission tomography/computed tomography for guided biopsy: transaxial (a and b) and sagittal (c and d) computed tomography and fused positron emission tomography/computed tomography images confirming the correct positioning of the biopsy needle
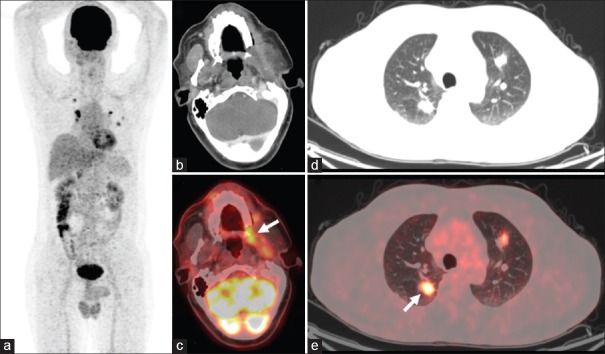
The patient was treated with chemoradiation for 6 months and scheduled for 18F-FDG PET/CT, 4 months later for response evaluation. Maximum-intensity projection [Figure 3a], transaxial CT, and fused PET/CT images revealed FDG-avid lesion in the region of left retromolar trigone [arrow; Figure 3b and c; SUVmax 9.5] and buccal mucosa with no significant change from the previous study. Multiple FDG-avid parenchymal- and pleural-based nodules [arrow; Figure 3d and e; SUVmax 42.1] were noted in the bilateral lung fields with increase in FDG avidity, size, and number compared to the previous study, suggesting disease progression. The patient refused further treatment and was lost to follow-up.
Figure 3.
18F-fluorodeoxyglucose positron emission tomography/computed tomography maximum-intensity projection (a), transaxial computed tomography, and fused positron emission tomography/computed tomography images showing fluorodeoxyglucose-avid lesion in the region of left retromolar trigone (arrow; b and c) and buccal mucosa. Multiple fluorodeoxyglucose-avid parenchymal- and pleural-based nodules (arrow; d and e) noted in the bilateral lung fields
ACC is a malignant neoplasm developing more commonly in minor (~60%) than major salivary glands (~40%).[1] The disease often has an indolent course with multiple episodes of recurrence and distant metastases, commonly to the lung and bones, as a late occurrence.[1] ACCs have been typically characterized as low grade-to-non-FDG avid tumors, reported as false negative on 18F-FDG PET/CT.[2,3] Later, various reports demonstrated the role of 18F-FDG PET/CT in evaluating disease recurrence and identification of distant metastases in ACC, thus affecting patient management.[4,5] In comparison with magnetic resonance imaging, 18F-FDG PET/CT showed superior sensitivity for detection of local tumor recurrence and regional and distant metastases.[6] Due to the inherent aggressive nature of the primary neoplasm, distant metastases in most patients is inevitable, even after being treated with curative intent, leading to poor prognosis.[7,8] The present case illustrates the holistic role of 18F-FDG PET/CT in the entire workup of the patient including identification of local tumor recurrence and distant lung metastases, in their histopathological confirmation by guided biopsy, and in assessing treatment response evaluation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Stell PM. Adenoid cystic carcinoma. Clin Otolaryngol Allied Sci. 1986;11:267–91. doi: 10.1111/j.1365-2273.1986.tb01928.x. [DOI] [PubMed] [Google Scholar]
- 2.Purohit BS, Ailianou A, Dulguerov N, Becker CD, Ratib O, Becker M, et al. FDG-PET/CT pitfalls in oncological head and neck imaging. Insights Imaging. 2014;5:585–602. doi: 10.1007/s13244-014-0349-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roh JL, Ryu CH, Choi SH, Kim JS, Lee JH, Cho KJ, et al. Clinical utility of 18F-FDG PET for patients with salivary gland malignancies. J Nucl Med. 2007;48:240–6. [PubMed] [Google Scholar]
- 4.Bhagat N, Zuckier LS, Hameed M, Cathcart C, Baredes S, Ghesani NV, et al. Detection of recurrent adenoid cystic carcinoma with PET-CT. Clin Nucl Med. 2007;32:574–7. doi: 10.1097/RLU.0b013e3180646b0f. [DOI] [PubMed] [Google Scholar]
- 5.Otsuka H, Graham MM, Kogame M, Nishitani H. The impact of FDG-PET in the management of patients with salivary gland malignancy. Ann Nucl Med. 2005;19:691–4. doi: 10.1007/BF02985118. [DOI] [PubMed] [Google Scholar]
- 6.Ruhlmann V, Poeppel TD, Veit J, Nagarajah J, Umutlu L, Hoffmann TK, et al. Diagnostic accuracy of 18F-FDG PET/CT and MR imaging in patients with adenoid cystic carcinoma. BMC Cancer. 2017;17:887. doi: 10.1186/s12885-017-3890-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ko YH, Lee MA, Hong YS, Lee KS, Jung CK, Kim YS, et al. Prognostic factors affecting the clinical outcome of adenoid cystic carcinoma of the head and neck. Jpn J Clin Oncol. 2007;37:805–11. doi: 10.1093/jjco/hym119. [DOI] [PubMed] [Google Scholar]
- 8.Bobbio A, Copelli C, Ampollini L, Bianchi B, Carbognani P, Bettati S, et al. Lung metastasis resection of adenoid cystic carcinoma of salivary glands. Eur J Cardiothorac Surg. 2008;33:790–3. doi: 10.1016/j.ejcts.2007.12.057. [DOI] [PubMed] [Google Scholar]