Abstract
Background:
In situ decompression (ISD), subcutaneous transposition (SQT), and submuscular transposition (SMT) for cubital tunnel syndrome (CuTS) have historically yielded similar outcomes. Our null hypothesis is that no differences exist in surgical encounter total direct costs (SETDC) for ISD, SQT, and SMT.
Methods:
Adult patients treated surgically for CuTS by four fellowship-trained hand surgeons between August 2011 and December 2016 were identified by CPT code (64718) at our tertiary academic institution. Retrospective chart review was performed to determine whether ISD, SQT, or SMT was performed, and to exclude those with prior elbow surgery or fracture/dislocation and those undergoing revision or additional simultaneous procedures. Using our institution’s information technology value tools, we extracted prospectively-collected SETDC data for each surgical encounter. SETDC were compared between groups, and univariate and multivariable gamma regression were used to model SETDC.
Results:
ISD, SQT, and SMT were performed on 45, 62, and 14 unique surgical encounters, respectively, with mean surgical times of 28.0, 46.5, and 50.0 minutes, respectively. SETDC differed significantly between each surgical method. Surgical method and provider significantly affected SETDC in the univariate model, with non-significance of age, sex, BMI, and ASA class. Multivariable modelling demonstrated that SQT was 1.18-fold more costly than ISD, and SMT was 1.55-fold more costly than ISD, while controlling for age, sex, and provider.
Conclusions:
Surgical costs differed significantly between ISD, SQT, and SMT. Given historically-similar outcomes reported for these techniques, cost differences should be considered in addition to clinical factors to inform surgical decision-making for CuTS patients.
Introduction:
The cost of health care delivered in the United States has received increasing attention over the past decade, in part due to policy changes that have included value-based payment models.1,2 Cubital tunnel syndrome (CuTS) is the second most common compressive peripheral neuropathy,3 and the rate of surgical treatment has increased in both the United States and United Kingdom over the last two decades.4,5 Surgical options include in situ decompression (ISD), subcutaneous transposition (SQT), submuscular transposition (SMT), and medial epicondylectomy. Multiple randomized trials,6–9 and a meta-analysis of randomized controlled trials,10 have failed to show a difference in clinical outcomes between these methods even in the setting of severe neurological impairment. Additional meta-analyses failed to demonstrate differences in clinical outcome scores or improvements in motor conduction velocities for patients undergoing ISD and anterior transposition of the ulnar nerve,11 or differences in outcomes between open and endoscopic techniques.12,13 Therefore, none of these procedures have demonstrated superiority, and it remains unclear whether revision rates differ between these techniques.
Although substantial efforts have been made to compare the clinical outcomes for various CuTS surgical treatments,6–9,11,14–18 there is a paucity of studies attempting to understand cost differences between these methods. In 2007, Brauer and Graham published a decision analysis to compare ISD, SQT, SMT, and medial epicondylectomy.19 ISD demonstrated the highest expected utility, and the authors supported this as the preferred surgical strategy for CuTS based upon their results. Subsequently in 2012, Song et al. published a cost-utility analysis using Medicare estimated payment data to compare four treatment strategies: 1) ISD followed by salvage SMT, 2) SQT followed by salvage SMT, 3) medial epicondylectomy followed by salvage SMT, and 4) SMT as the index procedure.20 The authors concluded that ISD was a cost-effective treatment for CuTS, with effectiveness ratios of less than $2027 per quality-adjusted life year. Despite these informative studies, surgical encounter total direct costs associated with surgical treatments for CuTS still currently lack transparency. Given similar clinical outcomes reported in the peer-reviewed literature for ISD, SQT, and SMT, the discussion related to what constitutes appropriate treatment should also focus on improving value through cost reduction, in addition the prior focus upon clinical factors when choosing the treatment technique.18,21–23
Our institution has developed a “Value Driven Outcomes” (VDO) database containing detailed patient- and item-level total direct cost and payment data for a variety of health care services. This validated tool has successfully identified areas of high variability in cost, leading to improved value of care delivered.1,24,25 In the current study, the VDO tool was utilized to test the primary null hypothesis that surgical encounter total direct surgical costs (SETDC) were no different for ISD, SQT, and SMT.
Methods:
This IRB-approved retrospective study considered for inclusion all adult (≥ 18 years of age) patients undergoing surgical treatment for CuTS between August 2011 and December 2016 performed by four fellowship-trained orthopaedic hand surgeons at a single tertiary academic institution. Patients were identified by CPT code (64718). Manual chart review was performed to determine whether open ISD, SQT, or SMT was performed, and to collect and corresponding basic demographic and surgical data. Manual chart review of all operative, anesthesia, and orthopaedic clinic notes was performed to confirm that the diagnosis of CuTS had been established, to record the anesthesia type, and to exclude patients undergoing additional simultaneous procedures including other surgeries or injections, those with prior injury (fracture and/or dislocation) or surgery to the elbow, and those undergoing revision decompression. Also excluded were patients treated surgically prior to August 2011 (corresponding with initiation of the VDO database at our institution).
ISD, SQT, and SMT were performed as previously described.26 Based upon surgeon preferences, SQT was performed using a flexor-pronator fascial sling, or by suturing subcutaneous tissue from the anterior skin flap to the medial epicondyle, to prevent posterior translation of the ulnar nerve. SMT was performed using a Z-cut in the flexor-pronator fascia and excision of muscular steptae, which was repaired following transposition. Nerve tubes, nerve wraps, or other similar adjuncts were not used in any case. Surgeries were performed under monitored anesthesia care (MAC) with local, general anesthesia, or under a surgical block with MAC based on surgeon preference.
Surgical encounter total direct cost (SETDC) data were collected from the Value Driven Outcomes (VDO) database for each individual surgery performed. The VDO information technology tool draws prospectively-collected payment data and patient- and item-level total direct cost data from our institution’s data warehouse for specific patient encounters. VDO costing methods have been previously described, yielding total direct costs for materials used for patient care, facility utilization direct costs (including sterile processing costs), and time-based cost allocations including procedure/operative time and cost of staff involved in care (nursing, surgical technicians, medical assistants).1,24,25 Specific cost categories are further elucidated in Appendix I, Supplemental Digital Content 1, which shows the Breakdown of Value-Driven Outcomes database categories for total direct costs, INSERT HYPER LINK. All reported cost data were normalized using each individual’s cost divided by the median cost in the data set, to comply with institutional guidelines prohibiting the public reporting of raw financial data related to the details of non-publically disclosed contractual agreements.
Continuous variables were summarized as mean and standard deviation (SD), and categorical variables were summarized as count and percentage (%). Raw cost data were converted to January 2016 US dollars using the consumer price index, based upon the month and year of the surgery.27 Relative costs were then calculated by normalizing each distinct group mean by the lowest group median. SETDC were compared among ISD, SQT, and SMT using the Kruskal-Wallis test with Tukey pairwise comparisons. Univariate and multivariable gamma regression with a log link was used to model SETDC. Based upon clinical practice patterns, ISD is more likely to be performed under MAC than transpositions at our institution, and transpositions were are more likely to be performed under general or surgical block than ISD – due to this direct clinical association between anesthesia type and surgical method, the primary multivariable regression analysis did not include anesthesia type as a predictor. However, due to potential influences of anesthesia type on SETDC, a secondary multivariable regression analysis was performed that included anesthesia type as a predictor to determine whether costs of ISD differed from transposition (SQT and SMT).
Age was compared among ISD, SQT, and SMT groups using one-way ANOVA with Tukey’s honest significant difference (HSD) test for multiple comparisons. Surgical times were compared using a Kruskal-Wallis test followed by pairwise Wilcox rank sum tests with a Bonferroni correction for multiple comparisons. Categorical variables were compared using the Fisher Exact test or chi-squared test with pairwise tests using a Bonferroni correction. Statistical significance was assessed at the 0.05 level, and all applicable tests were two-tailed.
An a priori power analysis was performed. To detect a medium effect size of 0.5 in standard deviation units between ISD and SQT groups, 80% power would be achieved to detect statistical significance at a two-tailed 0.05 alpha level with 64 patients/group. With 45 patients in the ISD group and 62 patients in the SQT group, we had 80% power to detect an effect size of 0.55 between these two groups.
Results:
Of 158 surgical encounters identified by CPT code, 37 were excluded (24 revisions, 9 with prior elbow surgery, 4 with additional simultaneous procedures). Two patients underwent staged bilateral ISD, 7 underwent staged bilateral SQT, and one underwent staged ISD followed by contralateral SQT. Therefore in total, 45, 62, and 14 unique surgical encounters for ISD, SQT, and SMT, respectively, were included.
Baseline patient characteristics and surgical details are reported in Table 1. Mean age was 52.2, 41.3, and 48.1 years, respectively (p < 0.05 between ISD and SQT). There were no differences in sex or BMI between groups. Mean surgical times were 28.0, 46.5, and 50.0 minutes, respectively. Surgical time for ISD was significantly less than for SQT or SMT (p < 0.05), with no difference between SQT and SMT (p > 0.05 per pairwise Wilcox rank sum tests with a Bonferroni correction for multiple comparisons).
Table 1 -.
Baseline Patient Characteristics and Surgical Details
| Factor | ISD (n = 45) |
SQT (n = 62) |
SMT (n = 14) |
p-value |
|---|---|---|---|---|
| Age (years ± SD) | 52.2 ± 15.5 | 41.3 ± 14.8 | 48.0 ± 15.3 | < 0.05a |
| Sex (female) | 17 (38%) | 32 (52%) | 5 (36%) | 0.28 |
| BMI | 31.2 ±7.2 | 28.9 ± 6.8 | 29.8 ± 8.7 | 0.30 |
| Race | 0.55 | |||
| Native American | 1 ( 2 %) | 1 ( 2 %) | 0 ( 0 %) | - |
| Asian | 0 ( 0 %) | 1 ( 2 %) | 0 ( 0 %) | - |
| Black | 4 ( 9 %) | 1 ( 2 %) | 0 ( 0 %) | - |
| Other | 4 ( 9 %) | 3 ( 5 %) | 1 ( 7 %) | - |
| White | 34 ( 79 %) | 56 ( 90 %) | 13 ( 93 %) | - |
| ASA Class | ||||
| 1 | 10 ( 27 %) | 20 ( 42 %) | 2 ( 17 %) | < 0.05b |
| 2 | 13 ( 35 %) | 22 ( 46 %) | 4 ( 33 %) | - |
| 3 | 14 ( 38 %) | 6 ( 12 %) | 6 ( 50 %) | - |
| 4 | 0 (0%) | 0 (0%) | 0 (0%) | - |
| Anesthesia Type | ||||
| Monitored anesthesia care (MAC) | 6 ( 13 %) | 0 ( 0 %) | 1 ( 7 %) | < 0.05 |
| General | 26 ( 58 %) | 55 ( 90 %) | 11 ( 79 %) | - |
| Surgical block with MAC | 13 ( 29 %) | 6 ( 10 %) | 2 ( 14 %) | - |
| Surgeon | ||||
| A | 17 ( 38 %) | 10 ( 16 %) | 5 ( 36 %) | < 0.05 |
| B | 5 ( 11 %) | 20 ( 32 %) | 5 ( 36 %) | |
| C | 19 ( 42 %) | 6 ( 10 %) | 2 ( 14 %) | |
| D | 4 ( 9 %) | 26 ( 42 %) | 2 ( 14 %) | |
| Surgical Time (minutes) | 28 (23, 35) | 46.5 (38.5, 61.2) | 50 (42.8, 57.5) | < 0.05c |
Continuous data presented as mean ± standard deviation, with the exception of Surgical Time (mean and interquartile range in parentheses). Categorical data presented as number of patients and (percentage).
Pairwise comparisons reveal significant differences between ISD and SQT, ISD and SMT, but not between SQT and SMT.
Pairwise comparisons reveal a significantly different rate of use of general anesthesia between ISD and SQT, but no differences between ISD and SMT, or between SQT and SMT.
Pairwise comparisons reveal significant differences between ISD and SQT, and ISD and SMT, with no difference between SQT and SMT.
SETDC differed significantly between each surgical method (p < 0.05; Figure 1). Facility utilization costs comprised the majority of SETDC for ISD, SQT, and SMT (71%, 74%, and 67%, respectively), and were significantly greater (1.4- and 1.6-fold) for SQT and SMT respectively, as compared to ISD. Facility costs were greater for SQT than ISD (p < 0.05), greater for SMT than ISD (p < 0.05), but not different between SQT and SMT (p > 0.05 per pairwise Wilcox rank sum tests with a Bonferroni adjustment for the multiple comparisons). Recovery room costs were the second largest contributor to SETDC for ISD, SQT, and SMT (15%, 16%, and 15%, respectively), and were significantly greater by 1.3- and 1.6-fold for SQT and SMT, respectively, as compared to ISD. Recovery room costs for ISD was significantly less than SMT (p < 0.05) with no other differences between groups (p > 0.05). Pharmacy costs were the third largest contributor to SETDC for ISD, SQT, and SMT (9%, 10%, and 6%, respectively), and were significantly greater by 1.5- and 1.2-fold for SQT and SMT, respectively, as compared to ISD. Pharmacy costs for ISD were significantly less than for SQT (p < 0.05), with no other differences between groups (p > 0.05).
Figure 1-.
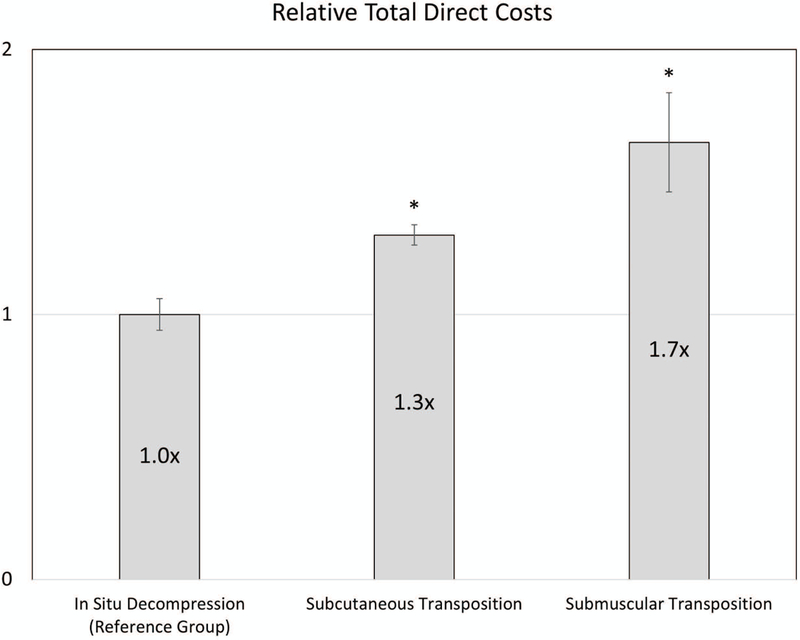
Comparison of surgical total direct costs for three methods of cubital tunnel decompression. Data represents normalized mean costs relative to in situ decompression. Error bars represent standard error of the mean (SEM). * p < 0.05 as compared to the reference group (in situ decompression).
Univariate gamma regression revealed that surgical method and provider contributed significantly to SETDC, and suggested non-significance of factors including age, sex, BMI, and ASA class (Table 2). The primary multivariable gamma regression analysis found that SQT was 1.18-fold more costly than ISD (p < 0.05), and SMT was 1.55-fold more costly than ISD (p < 0.05) while controlling for age, sex, and provider (Table 3). The secondary multivariable gamma regression analysis found that transposition was 1.18-fold more costly than ISD (p < 0.05) when adding anesthesia type to the primary multivariable regression model, and suggested that general anesthesia is 31% more expensive than MAC (p < 0.05), while controlling for age, sex, and provider (Table 4).
Table 2 -.
Univariate Analysis to Elucidate Factors Affecting Surgical Encounter Total Direct Costs
| Factor | Relative Costa | P - Value | |
|---|---|---|---|
| Coefficient | 95% Confidence Interval |
||
| Age (years)b | 1.00 | (0.99 • 1.00) | 0.20 |
| Anesthesia Typec | |||
| Monitored anesthesia care (MAC) | Reference Category | - | - |
| General | 1.49 | (1.18 • 1.89) | < 0.05 |
| Surgical block + MAC | 0.93 | (0.71 • 1.21) | 0.57 |
| Provider | |||
| A | Reference Category | - | - |
| B | 1.61 | (1.37 • 1.89) | < 0.05 |
| C | 1.26 | (1.07 • 1.48) | < 0.05 |
| D | 1.21 | (1.04 • 1.42) | < 0.05 |
| Sex | |||
| Female | Reference Category | - | - |
| Male | 0.91 | (0.80 • 1.04) | 0.16 |
| Surgical Method | |||
| In situ decompression (ISD) | Reference Category | - | - |
| Subcutaneous transposition (SQT) | 1.24 | (1.10 • 1.41) | < 0.05 |
| Submuscular transposition (SMT) | 1.62 | (1.34 • 1.97) | < 0.05 |
Relative Cost (RC): Gamma univariate regression coefficients (eβ). For example, a value of 1.6 is interpereted as a 60% increase in total direct costs as compared to the reference category. Bolded p-values were determined to be statistically-significant.
Per additional 1 year of age.
Note that anesthesia type and surgical method are confounded; due to clinical practice patterns, ISD is more likely to be performed under MAC, and transpositions performed under general anesthesia.
Table 3 -.
Primary Analysis: Multivariable Regression Analysis to Elucidate Factors Affecting Surgical Encounter Total Direct Costs
| Factor | Relative Costa–b | P - Value | |
|---|---|---|---|
| Coefficient | 95% Confidence Interval | ||
| Age (years)b | 1.00 | (1.00 • 1.00) | > 0.99 |
| Provider | |||
| A | Reference Category | - | - |
| B | 1.50 | (1.29 • 1.74) | < 0.05 |
| C | 1.28 | (1.11 • 1.48) | < 0.05 |
| D | 1.15 | (0.99 • 1.34) | 0.72 |
| Sex | |||
| Female | Reference Category | - | - |
| Male | 0.96 | (0.86 • 1.06) | 0.40 |
| Surgical Method | |||
| In situ decompression (ISD) | Reference Category | - | - |
| Subcutaneous transposition (SQT) | 1.18 | (1.03 • 1.34) | < 0.05 |
| Submuscular transposition (SMT) | 1.55 | (1.30 • 1.85) | < 0.05 |
Relative Cost (RC): Gamma univariate regression coefficients (eβ). For example, a value of 1.6 is interpereted as a 60% increase in total direct costs as compared to the reference category. Bolded p-values were determined to be statistically-significant.
Note that anesthesia type and surgical method are associated due to clinical practice patterns in which ISD is more likely to be performed under MAC, and transpositions performed under general anesthesia. Therefore, anesthesia type was not included in the primary multivariable regression analysis as a predictor.
Per additional 1 year of age.
Table 4 -.
Secondary Analysis: Multivariable Regression Analysis to Elucidate Factors Affecting Surgical Encounter Total Direct Costs
| Factor | Relative Costa–b | P - Value | |
|---|---|---|---|
| Coefficient | 95% Confidence Interval | ||
| Age (years)b | 1.00 | (1.00 • 1.01) | 0.36 |
| Anesthesia Type | |||
| Monitored Anesthesia Care (MAC) | Reference Category | - | - |
| General | 1.31 | (1.04 • 1.65) | < 0.05 |
| Surgical block + MAC | 0.92 | (0.72 • 1.17) | 0.49 |
| Provider | |||
| A | Reference Category | - | - |
| B | 1.61 | (1.37 • 1.89) | < 0.05 |
| C | 1.26 | (1.07 • 1.48) | 0.33 |
| D | 1.21 | (1.04 • 1.42) | 0.65 |
| Sex | |||
| Female | Reference Category | - | - |
| Male | 0.96 | (0.86 • 1.06) | 0.43 |
| Surgical Method | |||
| In situ decompression (ISD) | Reference Category | - | - |
| Transposition (SQT and SMT) | 1.18 | (1.04 • 1.35) | < 0.05 |
Relative Cost (RC): Gamma univariate regression coefficients (eβ). For example, a value of 1.6 is interpereted as a 60% increase in total direct costs as compared to the reference category. Bolded p-values were determined to be statistically-significant.
Note that anesthesia type and surgical methods are associated due to clinical practice patterns in which ISD is more likely to be performed under MAC, and transpositions performed under general anesthesia. By including both predictors, the effect of surgical method may be falsely lowered.
Per additional 1 year of age.
Power analysis revealed that with 45 patients in the ISD group and 62 patients in the SQT group, 80% power was achieved at a two-tailed 0.05 alpha level to detect an effect size of 0.55 between these two groups.
Discussion:
Our main finding was that surgical encounter total direct costs for subcutaneous transposition (SQT) and submuscular transposition (SMT) were significantly greater than for in situ decompression (ISD) by 1.18- and 1.55-fold, respectively. These differences were associated with discrepancies in facility costs, recovery room costs, and pharmacy costs. Therefore, we rejected our null hypothesis.
Although we were unable to identify study reporting actual direct costs for these surgical procedures, our findings add strength to the current literature. Song et al. performed a cost-utility analysis evaluating four treatment strategies for CuTS surgical treatment: 1) ISD followed by salvage SMT, 2) SQT followed by salvage SMT, 3) medial epicondylectomy followed by salvage SMT, and 4) SMT as the index procedure.20 Estimated costs derived from Medicare reimbursement rates, rather than actual direct costs, were used as a surrogate for cost. Given the database study design and identical CPT coding for ISD, SQT, and SMT (CPT 64718), the study was limited in the ability to accurately estimate surgical direct costs for these three procedures: direct costs related to surgical services, anesthesia services, and facility fees were assumed to be identical for ISD, SQT, and SMT in their study. This contrasts with our observed significant differences in surgical costs between the three procedures. However, strengths of their study include estimation of indirect and opportunity costs related to missed work and recovery, and by performing a full cost-utility analysis from a societal perspective based upon a comprehensive review of complication rates in the literature. Nonetheless, the authors concluded that initial surgical treatment with ISD was more cost-effective than proceeding first with SQT, SMT, or medial epicondylectomy. These conclusions mirror those of the decision analysis study published by Brauer and Graham.19 We speculate that the calculated cost-effectiveness of ISD would be even more favorable if the model were run using the actual SETDC of the current study.
Limitations of the current study deserve mention. Although each surgical procedure was verified with chart review, the initial identification of patients by procedure code, the retrospective study design, and evaluation of patients from a single center introduce potential for selection bias. Due to the nonrandomized study design, significant differences in age, ASA class, and anesthesia type were observed between some of the groups. However, it is unclear if these differences would affect surgical costs. Generalizability of our results may be limited by our unique pricing agreements between our institution and suppliers, which may affect total direct costs of time-allocated costs of operating room time, perioperative services, and other products used during the surgical encounter. We acknowledge that medial epicondylectomy and endoscopic ISD are described options for CuTS,28,29 and our study is limited given that none of the surgeons at our institution perform these procedures. We did not quantify the opportunity cost for ISD versus transpositions in which the latter required more surgical time, nor does the VDO database include indirect cost data such as that related to housekeeping, electricity, or property rent/depreciation. Our study is not a true cost-effectiveness analysis as we did not combine our cost findings with outcomes, however historically no CuTS surgical procedure has been shown to lead to superior outcomes.7–9,11,14,30 Additionally, anesthesia type and surgical method are associated. Due to clinical practice patterns at our institution, ISD is more likely to be performed under MAC, and transpositions are more likely to be performed under general anesthesia. Although it is impossible to statistically dissect one from the other, and it is likely our secondary multivariable analysis underestimates the impact of surgical technique on cost due to association of surgical method and anesthesia type, our reporting methods for primary and secondary multivariable regression analyses both suggest that surgical method affects SETDC.
One additional limitation that deserves specific mention pertains to generalizability of our findings. Although the VDO database has previously been validated and has successfully been used to improve value of care,1,24,25 our results should be generalized with caution, as operating room staffing and recovery room protocols, as well as the insurance payer mix and negotiated rates for medications and surgical supplies may differ by region. We acknowledge that facility costs, recovery room costs, and costs of medications and supplies for cubital tunnel release surgical encounters likely differ at other institutions. Nonetheless, our observed differences in SETDC between ISD and transpositions were driven mostly by facility costs, which are in turn driven by surgical time. At other institutions, surgical times may differ based upon surgeon experience and whether trainees are involved, which could affect SETDC. Since costs likely differ for other institutions, our observed differences in relative costs between ISD, SQT, and SMT may be more generalizable than the actual costs.
In conclusion, we found that surgical encounter total direct costs for SQT and SMT were 1.18- and 1.55-fold greater than ISD. These differences were associated with differences in facility costs, recovery room costs, and pharmacy costs. In light of similar outcomes in the current literature for ISD, SQT, and SMT,11,30 cost differences between these procedures should be considered when indicating CuTS patients for surgery in addition to clinical factors such as prior elbow trauma, nerve mobility, symptom severity22,23 and greater morbidity associated with transposition18. Awareness of cost implications for these surgical techniques may result in substantial savings over time.
Supplementary Material
See Appendix 1, which shows the Breakdown of Value-Driven Outcomes database categories for total direct costs, INSERT HYPER LINK.
Acknowledgments
Financial Disclosure Statement:
This investigation was supported by the University of Utah Study Design and Biostatistics Center, with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant 5UL1TR001067–02 (formerly 8UL1TR000105 and UL1RR025764). None of the authors has a financial interest in any of the products, devices, or drugs mentioned in this manuscript.
References:
- 1.Lee VS, Kawamoto K, Hess R, et al. Implementation of a value-driven outcomes program to identify high variability in clinical costs and outcomes and association with reduced cost and improved quality. JAMA. 2016;316:1061–1072. [DOI] [PubMed] [Google Scholar]
- 2.Kawamoto K, Martin CJ, Williams K, et al. Value driven outcomes (vdo): A pragmatic, modular, and extensible software framework for understanding and improving health care costs and outcomes. J Am Med Inform Assoc. 2015;22:223–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bozentka DJ. Cubital tunnel syndrome pathophysiology. Clin Orthop Relat Res. 1998;90–94. [PubMed] [Google Scholar]
- 4.Soltani AM, Best MJ, Francis CS, Allan BJ, Panthaki ZJ. Trends in the surgical treatment of cubital tunnel syndrome: An analysis of the national survey of ambulatory surgery database. J Hand Surg Am. 2013;38:1551–1556. [DOI] [PubMed] [Google Scholar]
- 5.Bebbington E, Furniss D. Linear regression analysis of hospital episode statistics predicts a large increase in demand for elective hand surgery in england. J Plast Reconstr Aesthet Surg. 2015;68:243–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Geutjens GG, Langstaff RJ, Smith NJ, Jefferson D, Howell CJ, Barton NJ. Medial epicondylectomy or ulnar-nerve transposition for ulnar neuropathy at the elbow? J Bone Joint Surg Br. 1996;78:777–779. [PubMed] [Google Scholar]
- 7.Bartels RH, Verhagen WI, van der Wilt GJ, Meulstee J, van Rossum LG, Grotenhuis JA. Prospective randomized controlled study comparing simple decompression versus anterior subcutaneous transposition for idiopathic neuropathy of the ulnar nerve at the elbow: Part 1. Neurosurgery. 2005;56:522–530; discussion 522–530. [DOI] [PubMed] [Google Scholar]
- 8.Gervasio O, Gambardella G, Zaccone C, Branca D. Simple decompression versus anterior submuscular transposition of the ulnar nerve in severe cubital tunnel syndrome: A prospective randomized study. Neurosurgery. 2005;56:108–117; discussion 117. [DOI] [PubMed] [Google Scholar]
- 9.Biggs M, Curtis JA. Randomized, prospective study comparing ulnar neurolysis in situ with submuscular transposition. Neurosurgery. 2006;58:296–304; discussion 296–304. [DOI] [PubMed] [Google Scholar]
- 10.Caliandro P, La Torre G, Padua R, Giannini F, Padua L. Treatment for ulnar neuropathy at the elbow. Cochrane Database Syst Rev. 2016;11:CD006839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zlowodzki M, Chan S, Bhandari M, Kalliainen L, Schubert W. Anterior transposition compared with simple decompression for treatment of cubital tunnel syndrome. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am. 2007;89:2591–2598. [DOI] [PubMed] [Google Scholar]
- 12.Aldekhayel S, Govshievich A, Lee J, Tahiri Y, Luc M. Endoscopic versus open cubital tunnel release: A systematic review and meta-analysis. Hand (N Y). 2016;11:36–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buchanan PJ, Chieng LO, Hubbard ZS, Law TY, Chim H. Endoscopic versus open in situ cubital tunnel release: A systematic review of the literature and meta-analysis of 655 patients. Plast Reconstr Surg. 2018;141:679–684. [DOI] [PubMed] [Google Scholar]
- 14.Nabhan A, Ahlhelm F, Kelm J, Reith W, Schwerdtfeger K, Steudel WI. Simple decompression or subcutaneous anterior transposition of the ulnar nerve for cubital tunnel syndrome. J Hand Surg Br. 2005;30:521–524. [DOI] [PubMed] [Google Scholar]
- 15.Caliandro P, La Torre G, Padua R, Giannini F, Padua L. Treatment for ulnar neuropathy at the elbow. Cochrane Database Syst Rev. 2011;CD006839. [DOI] [PubMed] [Google Scholar]
- 16.Shi Q, MacDermid J, Grewal R, King GJ, Faber K, Miller TA. Predictors of functional outcome change 18 months after anterior ulnar nerve transposition. Arch Phys Med Rehabil. 2012;93:307–312. [DOI] [PubMed] [Google Scholar]
- 17.Caliandro P, La Torre G, Padua R, Giannini F, Padua L. Treatment for ulnar neuropathy at the elbow. Cochrane Database Syst Rev. 2012;CD006839. [DOI] [PubMed] [Google Scholar]
- 18.Staples R, London DA, Dardas AZ, Goldfarb CA, Calfee RP. Comparative morbidity of cubital tunnel surgeries: A prospective cohort study. J Hand Surg Am. 2018;43:207–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brauer CA, Graham B. The surgical treatment of cubital tunnel syndrome: A decision analysis. J Hand Surg Eur Vol. 2007;32:654–662. [DOI] [PubMed] [Google Scholar]
- 20.Song JW, Chung KC, Prosser LA. Treatment of ulnar neuropathy at the elbow: Cost-utility analysis. J Hand Surg Am. 2012;37:1617–1629 e1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goldfarb CA, Sutter MM, Martens EJ, Manske PR. Incidence of re-operation and subjective outcome following in situ decompression of the ulnar nerve at the cubital tunnel. J Hand Surg Eur Vol. 2009;34:379–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krogue JD, Aleem AW, Osei DA, Goldfarb CA, Calfee RP. Predictors of surgical revision after in situ decompression of the ulnar nerve. J Shoulder Elbow Surg. 2015;24:634–639. [DOI] [PubMed] [Google Scholar]
- 23.Henn CM, Patel A, Wall LB, Goldfarb CA. Outcomes following cubital tunnel surgery in young patients: The importance of nerve mobility. J Hand Surg Am. 2016;41:e1–7. [DOI] [PubMed] [Google Scholar]
- 24.Chalmers PN, Granger E, Nelson R, Yoo M, Tashjian RZ. Factors affecting cost, outcomes, and tendon healing after arthroscopic rotator cuff repair. Arthroscopy. 2018; [DOI] [PubMed] [Google Scholar]
- 25.Tashjian RZ, Belisle J, Baran S, et al. Factors influencing direct clinical costs of outpatient arthroscopic rotator cuff repair surgery. J Shoulder Elbow Surg. 2018;27:237–241. [DOI] [PubMed] [Google Scholar]
- 26.Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH. Green’s operative hand surgery; sixth edition Philadelphia, PA: Elsevier Churchill Livingstone; 2010. [Google Scholar]
- 27.Bureau of labor statistics - data tools. [12/6/2017]; Available from: https://data.bls.gov/cgi-bin/surveymost
- 28.Osei DA, Padegimas EM, Calfee RP, Gelberman RH. Outcomes following modified oblique medial epicondylectomy for treatment of cubital tunnel syndrome. J Hand Surg Am. 2013;38:336–343. [DOI] [PubMed] [Google Scholar]
- 29.Bacle G, Marteau E, Freslon M, et al. Cubital tunnel syndrome: Comparative results of a multicenter study of 4 surgical techniques with a mean follow-up of 92 months. Orthop Traumatol Surg Res. 2014;100:S205–208. [DOI] [PubMed] [Google Scholar]
- 30.Mowlavi A, Andrews K, Lille S, Verhulst S, Zook EG, Milner S. The management of cubital tunnel syndrome: A meta-analysis of clinical studies. Plast Reconstr Surg. 2000;106:327–334. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Bureau of labor statistics - data tools. [12/6/2017]; Available from: https://data.bls.gov/cgi-bin/surveymost
Supplementary Materials
See Appendix 1, which shows the Breakdown of Value-Driven Outcomes database categories for total direct costs, INSERT HYPER LINK.


