Abstract
Plating of distal radius fractures is a common procedure. Especially in busy practices the procedure is mostly performed by a single surgeon. By the use of a distance holder screw in the most proximal hole of the shaft of an angular stable distal radius plate a lever arm can be created that allows indirect reduction of a dorsally displaced distal radius fracture. The method described here may facilitate the operation in that the articular block can be securely fixed while the plate is stable centered on the shaft of the radius. Especially for single surgeon operations this may save time. In contrast the costs of an extra angular stable screw must be accepted.
Keywords: Distale radius fracture, Angular stable plating, Reduction
1. Introduction
Angular stable plating has become a standard technique in a large variety of AO-23 fractures, distal radius and distal forearm. The modern anatomic plate design is of great help for anatomic reconstruction. The introduction of the popular volar approach that can be used for many indications has reduced complications like tendon adherence and subsequent decrease in range of motion. The key point of this technique is angular stable screw fixation because the zone of greatest comminution and displacement is located posteriorly. While the reduction can be achieved by manipulation of the hand and Kirschner-wires from all directions, stable fixation must be provided by volar implant positioning. Current operation principles do mainly have a reduction and temporary fixation in common. After primary reduction there are two main options of plate fixation. The plate can either be fixed at the shaft, preferably through an oval hole, the articular block is then reduced against the distal portion of the plate and the joint-bearing fragments can be fixed by angular stable screws. An alternative is to begin with the fixation of the articular block. If the long lever of the plate shaft is left unfixed the plate can be elevated along the shaft axis. After fixation of the distal fragments an increase in volar inclination can be achieved by reducing the elevated plate shaft to the radial shaft.
The Criteria that can be used to evaluate the reduction and which have prognostic value are volar inclination, radial length, fracture gap, radio-ulnar inclination.1, 2, 3, 4, 5, 6, 7, 8, 9 Retrospective analysis of numerous cases has shown that the restoration of the palmar inclination is of major interest regarding the range of volarflection/extention.10 With respect to the current literature a reduction of at least zero degrees volar inclination is a requirement for full range of motion after bony consolidation.
2. Methods
The study was performed after ethics approval was obtained by the ehtics committee of the University of Schleswig-Holstein (No D 451/13). Written consent was obtained by all patients included.
3. Study Population
26 patients (12 male, 14 female) were operated by the author from January 2015 to January 2016 using the method described. The mean age was 67 ± 7.9 yrs. All patients had no concomitant injures apart from minor bruises that were not treated. Open fractures were excluded. Initial x-rays were obtained for diagnosis and in case of a suspected or obvious intraarticular injury a CT scan was obtained. All patients were treated surgically within 7 days of presentation (5 ± 3,1 days). Primary treatment was closed reduction under oral analgesia and application of a split cast. Most fractures treated were AO Type A2 and A3 fractures (11). There were 5 B1 and B2 fractures and 10 C-type injuries (5-C3, 2 C-2, 3 C-3).
4. Results/Surgical technique
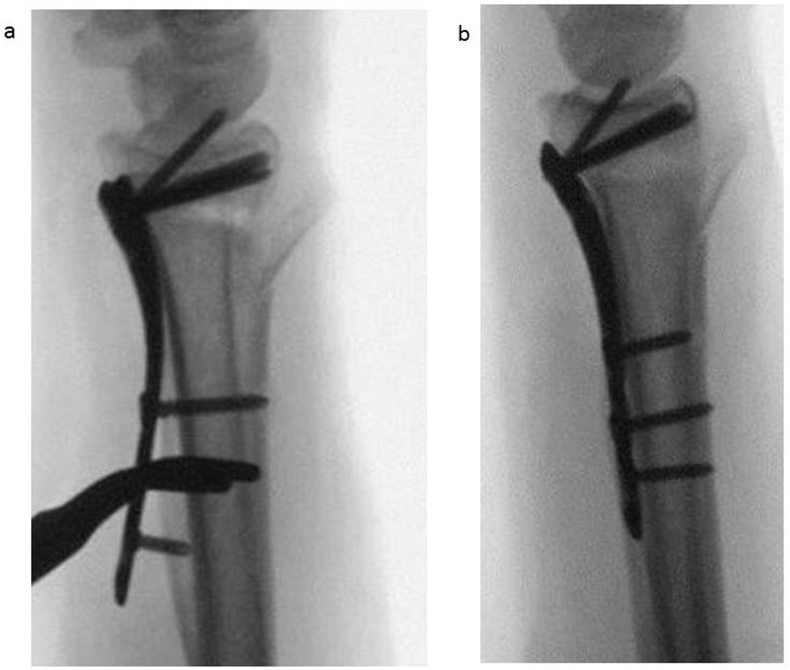
A standard volar approach to the distal radius is made and a retractor inserted. The fracture is cleaned and provisional reduction is achieved by placing the thumb onto the volar aspect of the fracture and a standard reduction maneuver with distraction-dorsal angulation-volar inclincation. Usually imaging at this stage reveals slight dorsal angulation of the articular surface and the anatomic shape of the plate does not match the volar aspect of the articular block. To address this the screw through the oval hole is untightened and a 10 mm locking screw is inserted into the most proximal hole of the shaft levering the plate up and thereby achieving full contact of the distal end of the plate with the articular block (Fig. 1, Fig. 2a). A crocodile clamp is used to temporary center the plate on the radial shaft. By tightening the cortical screw through the oval hole the plate is fixed again. Four to six screws are then used to fix the articular block to the plate, good contact is ensured by placing the thumb onto the plate and applying counter pressure with the index finger at the dorsal aspect. The distance holder screw is then removed and the plate is fully reduced down to the volar aspect of the radius thereby creating volar angulation of the articular surface (Fig. 2b). Two cortical screws are used to secure the plate in line with the radial shaft. After thorough irrigation wound closure is performed in layers as ususal. During the procedure no complications occurred. All intraoperative fluoroscopic controls showed proper alignment of the plate and well- positioned screws. During the process of levering no screws pulled out or cut out. Compared to the usual technique no greater bone loss was seen posteriorly where the comminution zone was unfolded.
Fig. 1.
Schematic drawing of the effect of a 1cm distance holder screw on volar inclination.
Fig. 2.
a) ap and lateral x-ray of reduction and fixation with distance holder screw in place b) ap and lateral x-ray of completed reduction.
5. Postoperative outcome
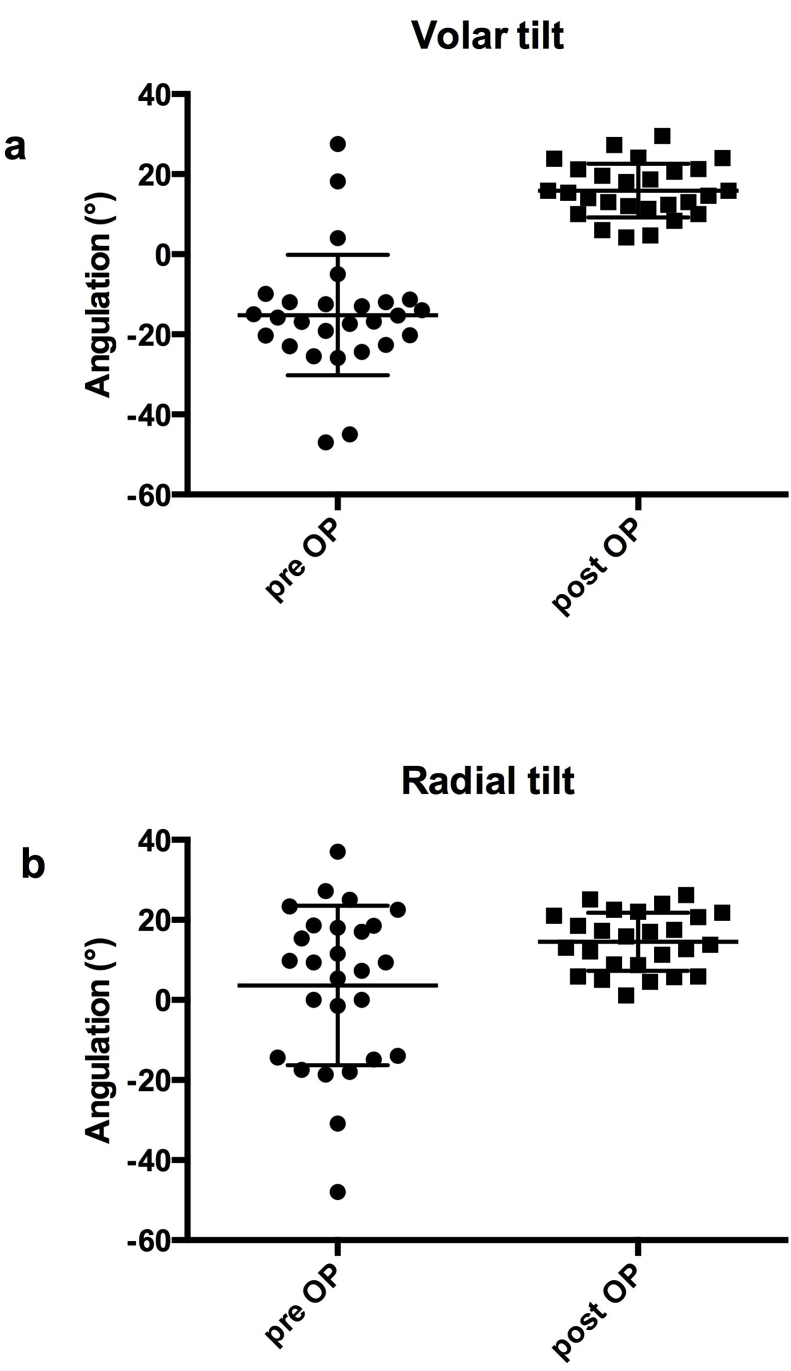
Reduction was assessed in standard radiographs of the wrist. The postoperative palmar / volar inclination was 15.89 ± 6.7 as opposed to -15.19 ± 15.0 preoperatively. The radial inclination was 14,54 ± 7.26 compared to 3,6 ± 19.9 preOP (Fig. 3). Six weeks postoperatively the Mayo wrist score was 42.37 ±22-2. The DASH score was 46.4 ± 22.8. Radiographically all fractures were consolidated to an extent that allowed full mobilization. All patients were seen one year after surgery. Non of the patients did report substantial restrictions in any activities of daily life. Apart from occasional pain no complaints were noted.
Fig. 3.
a) volar tilt pre- and postoperatively b) radial inclination pre- and postoperatively.
6. Discussion
Volar angular stable plating has become a standard method for the treatment of distal radius fractures. Although recent research has brought up evidence that the ultimate clinical outcome may not be generally improved as closed reduction and percutaneous wire fixation can lead to equally good function it is well accepted that there are advantages to this method. These include the ability to accurately reduce the fracture, release the median nerve if necessary and allow early functional treatment. This in turn may reduce the risk of CRPS and is often perceived as more comfortable by the patient. Typing and even writing may become possible after two to three weeks of rest.
The technique described here provides a very well controllable correction of palmar inclination. Especially when the operation is performed by a single surgeon there might be a desired further increase in inclination that cannot be achieved without an assistant holding and flexing the wrist. In other words it can be difficult to hold the plate in alignment with the shaft, levered to a certain extent and reduce and fix the articular block at the same time. With this technique fixation of the articular block and restoration of palmar tilt can be performed step by step while the plate is securely held in place. This is the main difference to well known methods by which the plate shaft is held with some distance to the radial shaft but not held in place by a screw. The angle (α) gained can be calculated by the simple equation α = arc tan (length of screw/length of plate) as shown in Fig. 1. With a distance holder screws of 8mm length and an assumed lever arm of 40mm the increase in volar tilt is 11.3°. In practice distance holder screws up to 10mm can easily be used without the need for extra soft tissue dissection. Our results demonstrate that with controlled levering of the plate palmar tilt and radial inclination can be restored sufficiently. The DASH and Mayo Score that were used to assess the early outcome were within the range of the usually expected, large, variance. After one year the outcomes were favourable in all cases with full range of motion. With respect to age and possible differences amongst age groups it is worth stating that neither with young patients nor with elder patients complications seemed more likely at any age. In younger patients that most probably did not suffer from osteopenia no associated soft tissue problems that could have related to pain or disability were documented. In the elderly, who represented the major group of patients, no pull-out or secondary loss of reduction could be detected. Hence the technique is safe for use in any age group, probably because modern plate designs with four or more distal angular stable screws provides enough subcortical anchorage to prevent screw migration or joint penetration.
Despite advantages in reduction and fixation that ultimately lead to shorter operating time, an extra screw gives rise to extra costs. Therefore the costs of one 8–10mm angular stable have to be outweighed by the technical advantages. To overcome this problem one company has implemented the technique into their set of instruments. To my knowledge this is the only company that provides reusable distance holder screws in their distal radius plate set.
Conflict of interest
The author declares that no conflict of interest exists.
Ethical approval
Informed consent was obtained from all individual participants included in the study. FIg 1 a, b reprinted with permission of Icotec ag, Altstaetten, Switzerland.
Funding
There is no funding source.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jor.2019.01.001.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Benson L.S., Minihane K.P., Stern L.D., Eller E., Seshadri R. The outcome of intra-articular distal radius fractures treated with fragment-specific fixation. J Hand Surg. 2006;31:1333–1339. doi: 10.1016/j.jhsa.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 2.Bradway J.K., Amadio P.C., Cooney W.P. Open reduction and internal fixation of displaced, comminuted intra-articular fractures of the distal end of the radius. J Bone Joint Surg Am Vol. 1989;71:839–847. [PubMed] [Google Scholar]
- 3.Cole R.J., Bindra R.R., Evanoff B.A., Gilula L.A., Yamaguchi K. Radiographic evaluation of osseous displacement following intra-articular fractures of the distal radius: reliability of plain radiography versus computed tomography. J Hand Surg. 1997;22:792–800. doi: 10.1016/s0363-5023(97)80071-8. [DOI] [PubMed] [Google Scholar]
- 4.Doi K., Hattori Y., Otsuka K., Abe Y., Yamamoto H. Intra-articular fractures of the distal aspect of the radius: arthroscopically assisted reduction compared with open reduction and internal fixation. J Bone Joint Surg Am Vol. 1999;81:1093–1110. doi: 10.2106/00004623-199908000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Drobetz H., Bryant A.L., Pokorny T., Spitaler R., Leixnering M. Volar fixed-angle plating of distal radius extension fractures: influence of plate position on secondary loss of reduction--a biomechanic study in a cadaveric model. J Hand Surg. 2006;31:615–622. doi: 10.1016/j.jhsa.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 6.Fernandez D.L., Geissler W.B. Treatment of displaced articular fractures of the radius. J Hand Surg. 1991;16:375–384. doi: 10.1016/0363-5023(91)90001-r. [DOI] [PubMed] [Google Scholar]
- 7.Gasse N., Lepage D., Pem R., Bernard C., Lerais J.M. Anatomical and radiological study applied to distal radius surgery. Surg Radiol Anat: SRA. 2011;33:485–490. doi: 10.1007/s00276-010-0754-x. [DOI] [PubMed] [Google Scholar]
- 8.Grewal R., Perey B., Wilmink M., Stothers K. A randomized prospective study on the treatment of intra-articular distal radius fractures: open reduction and internal fixation with dorsal plating versus mini open reduction, percutaneous fixation, and external fixation. J Hand Surg. 2005;30:764–772. doi: 10.1016/j.jhsa.2005.04.019. [DOI] [PubMed] [Google Scholar]
- 9.Pace A., Cresswell T. Use of articular wrist views to assess intra-articular screw penetration in surgical fixation of distal radius fractures. J Hand Surg. 2010;35:1015–1018. doi: 10.1016/j.jhsa.2010.03.041. [DOI] [PubMed] [Google Scholar]
- 10.Dario P., Matteo G., Carolina C., Marco G., Cristina D. Is it really necessary to restore radial anatomic parameters after distal radius fractures? Injury. 2014;45(Suppl 6):S21–S26. doi: 10.1016/j.injury.2014.10.018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.