Abstract
Objective.
To examine sociodemographic and military characteristics of U.S. veterans who do and do not utilize Veterans Affairs (VA) healthcare services as their primary source of healthcare, and examine the relationship between VA utilization and medical and psychosocial characteristics.
Methods.
Participants were a nationally representative sample of 3,152 military veterans (89.8% male, 83.5% Caucasian, 6.0%, Mage = 62.0, SD = 13.1) who completed a survey assessing healthcare utilization, sociodemographic, military service, medical and psychosocial characteristics. Receiver operator characteristic analyses and logistic and linear regressions were conducted to provide a comprehensive and multivariate examination of factors associated with VA utilization.
Results.
Veterans who used VA were more likely to be Black, younger, female, unmarried, less educated, and have lower household incomes. They were also more likely to have served longer in the military and in combat. VA users were more likely to screen positive for lifetime psychopathology, endorse current suicidality, and report enduring more traumas. VA users were also more likely to report more medical conditions, endorse a disability, and score lower on measures of functioning. The primary factor differentiating VA users from those that did not use VA was presence of lifetime psychopathology.
Conclusion.
Results provide a comprehensive profile of veterans who do and do not utilize VA and suggest that veterans who use VA have a substantially elevated health burden compared to other veterans. Results may help inform outreach and engagement initiatives targeting the unique healthcare needs of veterans who do and do not utilize VA services.
Keywords: Veterans, Healthcare
Prior research shows utilization of Veterans Affairs (VA) healthcare services increased from 20% in 2001 to 48% in 20161,2. From 2007 to 2016, the percent of female and male veterans utilizing VA services increased from 35% to 47% and 39% to 48% respectively2. Despite significant increases in service utilization, little is known about the sociodemographic and health characteristics of veterans who do not use VA services1. It is critical to gain a better understanding of these characteristics so that VA can better engage and serve veterans.
Veterans represent a vulnerable population, and are at higher risk for mental and physical health struggles such as posttraumatic stress disorder (PTSD) and hepatitis C3. PTSD among veterans can be particularly problematic as it is characterized by additional physical and mental health comorbidities4,5. According to the Institute of Medicine6, up to 24% of all returning service members have PTSD with percentages increasing every year from 2006–2012. Further, Jakupcak and colleagues4 found that veterans who screened positive for PTSD were 4 times more likely to report suicidal ideation than veterans who did not. Rates of suicide are disproportionately elevated among veterans, as veterans account for 18% of all deaths from suicide among U.S. adults, but constitute only 8.5% of the population7. With the older average age of veterans compared to the general population8, as well as the increased risk for mental and physical health problems, access to healthcare and integration of services is critical. Several independent studies have demonstrated that VA performs better than or similar to other medical systems on measures of safety, effectiveness, mortality and morbidity, as well as quality of care.9,10 The VA has also taken innovative steps to improve integration of care within and outside of VA systems. For instance, the Computerized Patient Record System (CPRS) provides a fully-integrated patient record system accessible at any VA, and the VA Continuity of Care Document allows veterans to electronically share their health information with non-VA providers. Despite these encouraging findings and developments, many veterans do not use VA healthcare services for a wide range of reasons (e.g., excessive wait times, difficulties navigating services)11,12.
The 2016 Congressional report from the Commission on Care13 stated that the VA healthcare system struggles with staffing, funding, information systems, and gender and minority health care disparities. Many of these obstacles are administrative in nature, rather than related to quality of care. Meanwhile, despite a strong record of performance on key clinical outcomes within VA, patient satisfaction scores have been varied. Average VA satisfaction scores are comparable or worse than other facilities14. However, 92% of veterans would rather improve the VA system than dismantle it15.
At present, much of the literature on veteran healthcare utilization focuses on specific groups (e.g., LGBTQ community, racial minorities) and conditions (e.g., PTSD), leaving a significant gap in research on utilization of healthcare in the broader veteran population. Gaining a better understanding of differences between VA and non-VA users may help inform service planning, increasing accessibility and engagement in VA healthcare. Thus, the aims of the current study were to analyze data from a nationally representative sample of U.S. veterans to: (1) characterize sociodemographic and military characteristics of veterans who do and do not utilize VA as their primary source of healthcare, and (2) employ a novel, multivariable approach of identifying patient-level correlates of VA utilization.
Method
Participants
Data were drawn from the National Health and Resilience in Veterans Study (NHRVS), a nationally representative study of 3,157 U.S military veterans aged 21 and older conducted in the fall of 2011 (see Klingensmith et al.16 for detailed information on sampling procedures). In the current study, data were analyzed from 3,152 participants who completed a single-item about VA healthcare utilization. Study procedures were approved by the U.S. Department of Veterans Affairs and Yale University Institutional Review Boards, and all participants provided written informed consent.
Measures
Demographics and military service history.
Participants completed a demographic questionnaire that assessed gender, age, education, race/ethnicity, marital status, household income, employment status, and metropolitan status. VA healthcare utilization was assessed with a single-item, “Is the VA your primary source of healthcare?”. Assessment of military service history included military branch, conflict served, years of service, combat status, level of combat exposure (Combat Exposure Scale17), and whether drafted or enlisted.
Psychiatric and substance use disorder (SUD) history.
Psychopathology was operationalized as endorsement of major depression disorder (MDD), social phobia, PTSD, or suicide attempt. Substance use disorder (SUD) was characterized as endorsement of alcohol use disorder (AUD) or drug use disorder (DUD). Lifetime MDD, social phobia, AUD, and DUD were assessed with the Mini-International Neuropsychiatric Interview18. Current AUD was assessed using the Alcohol Use Disorders Identification Test19 (AUDIT-C), where a score of >5 indicated a positive screen for current (past year) AUD. A score ≥3 on the MDD and generalized anxiety disorder (GAD) questions of the Patient Health Questionnaire-420 (PHQ-4) indicated a positive screen for current (past 2 weeks) MDD and GAD. Participants were screened for current suicidal ideation (endorsement of at least 1 of 2 items of the PHQ-9), history of suicide attempts, and prior use of mental health treatment (i.e., prescription medication or psychotherapy for a psychiatric or emotional problem). The PTSD Checklist21 for DSM-IV-TR (4th ed., text revision) was used to assess lifetime and past-month PTSD symptoms, with a positive screen for lifetime or past-month PTSD indicated by total score ≥4422. A sum of total lifetime traumas was assessed using a 15-item version of the Trauma History Screen23. All psychiatric and substance use disorder variables were dichotomous, except for total number of lifetime traumas which was continuous.
Medical history and Functioning.
A Medical Conditions Checklist was used to assess previous medical diagnoses. All medical history variables were dichotomous, except for total number of medical conditions which was continuous. In addition, the Short Form-8 Health Survey24 (SF-8) was used to assess physical and mental functioning. SF-8 component summary scores range from 0 to 100 with higher scores reflecting better functioning. The MOS Cognitive Functioning Scale25 assessed cognitive functioning in the past month. High scores reflect better functioning. Disability was assessed using an Activities of Daily Living Checklist26, a physical disability was dichotomously categorized as endorsement of difficulty with any daily living activity.
Data Analysis
First, descriptive statistics were computed on demographic characteristics of the sample (N = 3,152). Second, independent-samples t tests (Spearman Rho correlations in instances of a non-normal distribution) and Pearson chi-square analyses were conducted to assess differences between veterans who did and did not utilize VA as their primary source of healthcare. Third, a series of independent, multivariable logistic and linear regression analyses, adjusted for sociodemographic and military characteristics that differed by VA utilization, were conducted to evaluate the relationship between VA utilization, and mental and physical health and functioning measures. Effect sizes were expressed using odds ratios and 95% confidence intervals (95% CIs) for dichotomous outcomes and Cohen’s d for continuous outcomes. Alphas were adjusted to 0.01 to help control against both Type I and Type II errors. Fourth, two receiver operating characteristic (ROC) analyses were conducted to identify patient-level correlates of VA utilization, and to characterize unique associations of individual psychiatric and medical diagnoses with VA utilization. The primary ROC analysis included significant predictor variables as determined by regression analyses.
ROC analyses were conducted using publicly available ROC software (ROC Version 5.07; http://web.stanford.edu/~yesavage/ROC.html). ROC analysis is a non-parametric test which allows for examination of multiple predictor variables, identifying homogeneous subgroups of a population with differential likelihood for a specific binary outcome. Although regression analyses identify similar relations, ROC analyses are uniquely able to identify systematic interactions among many categorical and continuous variables. The ROC model uses signal detection analyses to iteratively partition the sample based on the predictors and cut points that best discriminate on the outcome, yielding a hierarchical decision tree. Signal detection has been especially useful in analyses where predictors are likely to be highly collinear and interactions between independent variables exist27. For the current study, efficiency was optimized by setting sensitivity (avoiding false negatives) and specificity (avoiding false positives) to 50%. The ROC software searched for a cut points that maximized efficiency, balancing sensitivity and specificity in the prediction of VA utilization. The strongest predictor was identified and compared against a stopping rule of p < .05. If the test does not pass the stopping rule, the analysis at that level is complete. If the stopping rule is passed, the sample is divided into subgroups based on that variable. Analyses are rerun on all subgroups until stopping rules are met. Variables associated with a p > 0.05 are excluded from the decision tree. Analyses were rerun on all subgroups until stopping rules were met. Through this systematic iterative approach higher order interactions and subgroups with differential likelihood of utilizing VA healthcare were yielded27.
To permit generalizability of study results to the entire population of U.S. veterans, raw numbers of participants and weighted prevalences and means (SDs) were computed and applied in all analyses involving inferential statistics based on demographic distributions from the contemporaneous U.S. Census Bureau Current Population Survey28. These weights adjust for any survey nonresponse, as well as any noncoverage, under sampling, or oversampling. Demographic characteristics of the NHRVS sample were consistent with those observed in prior population-based surveys of veterans29.
Results
Descriptive Statistics
Of the full sample (N = 3,152), 16.9% of participants utilized VA as their primary source of healthcare. Participants were 89.8% male, 83.5% Caucasian, 6.0% Black, 4.8% Hispanic, 5.7% other, and mean age was 62.0 (SD = 13.1, range = 21–96). 42.4% percent of the sample had obtained a bachelor’s degree or higher, 52.1% reported a household income of $60,000 or higher, 74.4% were married, and 84.3% lived in a metropolitan area.
Group Differences Analyses
Table 1 shows sociodemographic and military characteristics of the full sample and by VA utilization status. Compared with veterans who did not utilize VA as their primary source of healthcare, VA utilizers were more likely to be Black, younger, female, unmarried, less educated, and have a lower income. Employed veterans were less likely to utilize VA healthcare. There were no differences based on living in a metropolitan or rural area (i.e., urbanicity). In terms of military experience, veterans utilizing VA were more likely to have served longer in the military, to have served in the Vietnam, Iraq/Afghanistan, or Persian Gulf conflicts. VA utilizers were more likely to have served in a combat zone and had higher levels of combat exposure. Furthermore, veterans that did not utilize VA as their main source of healthcare were more likely to be drafted and in the Air Force.
Table 1.
Demographic and Military Characteristics by Primary Use of VA Healthcare Service Status
| Test of Difference | |||||
|---|---|---|---|---|---|
| Characteristic | Total (N = 3,152) |
Non-VA user (n = 2,547)a |
VA-user (n = 608)a |
t or χ2 | p |
| Sociodemographic characteristics | |||||
| Age, mean (SD), y | 62.0 (13.1) | 60.9 (14.9) | 57.5 (15.2) | 4.96 | <0.01 |
| Gender, n (%) | 4.16 | <0.05 | |||
| Male | 2832 (89.8) | 2322 (91.2) | 538 (88.5) | ||
| Female, n (%) | 320 (10.2) | 225 (8.8) | 70 (11.5) | ||
| Race/ethnicity, n (%) | −3.35 | <0.01 | |||
| White, non-Hispanic | 2633 (83.5) | 1989 (78.1) | 414 (68.1) | 27.04 | <0.01 |
| Black, non-Hispanic | 189 (6.0) | 212 (8.3) | 91 (15.0) | 24.95 | <0.01 |
| Hispanic | 152 (4.8) | 207 (8.1) | 53 (8.7) | 0.23 | 0.62 |
| Non-metropolitan | 496 (15.7) | 445 (17.5) | 118 (19.4) | 1.26 | 0.26 |
| Education, n (%) | 2.46 | < 0.05 | |||
| Less than high school | 52 (1.6) | 99 (3.9) | 19 (3.1) | 0.79 | 0.41 |
| High school graduate or equivalent | 431 (13.7) | 741 (29.1) | 191 (31.4) | 1.27 | 0.28 |
| Some college | 1331 (42.2) | 930 (36.5) | 263 (43.3) | 9.49 | < 0.01 |
| Bachelor’s degree or higher | 1338 (42.4) | 741 (29.1) | 191 (31.4) | 1.27 | 0.28 |
| Married, n (%) | 2345 (74.4) | 1884 (74.0) | 346 (66.9) | 68.95 | <0.01 |
| Employed, n (%) | 1284 (40.7) | 1084 (43.7) | 202 (34.5) | 16.20 | <0.01 |
| Household income ≥60k, n (%) | 1643 (52.1) | 1229 (48.3) | 157 (25.9) | 99.74 | <0.01 |
| Military characteristics | |||||
| Drafted, n (%) | 428 (13.6) | 340 (13.4) | 48 (7.9) | 13.47 | < 0.01 |
| Combat veteran, n (%) | 1104 (35.0) | 795 (31.3) | 312 (51.7) | 61.88 | < 0.01 |
| Branch of service, n (%) | −0.15 | 0.88 | |||
| Army | 1269 (40.3) | 959 (37.7) | 252 (41.4) | 2.99 | 0.08 |
| Navy | 720 (24.1) | 618 (24.3) | 142 (23.4) | 0.22 | 0.67 |
| Air Force | 711 (22.8) | 601 (23.6) | 110 (18.1) | 8.52 | < 0.01 |
| Marine Corps | 256 (8.1) | 277 (10.9) | 74 (12.2) | 0.83 | 0.35 |
| National Guard | 45 (1.4) | 41 (1.6) | 14 (2.3) | 1.38 | 0.23 |
| Coast Guard | 36 (1.1) | 32 (1.3) | 12 (2.0) | 1.84 | 0.18 |
| Other | 20 (0.6) | 17 (0.7) | 4 (0.7) | 0.001 | 1.00 |
| War era, n (%)* | −4.31 | < 0.01 | |||
| World War II | 45 (1.4) | 49 (1.9) | 8 (1.3) | 1.02 | 0.40 |
| Korean | 104 (3.3) | 99 (3.9) | 27 (4.4) | 0.40 | 0.30 |
| Vietnam | 656 (20.8) | 396 (15.5) | 125 (20.6) | 8.94 | < 0.01 |
| Persian Gulf | 106 (3.4) | 88 (3.5) | 35 (5.8) | 6.94 | < 0.05 |
| Iraq/Afghanistan | 115 (3.6) | 109 (4.3) | 73 (12.0) | 54.10 | < 0.01 |
| Other War/Era | 67 (2.1) | 46 (1.8) | 22 (13.1) | 7.65 | < 0.05 |
| Years in military, mean (SD) | 7.4 (7.7) | 6.8 (7.2) | 7.8 (7.7) | 3.10 | < 0.01 |
values are weighted. Total weighted n = 3155.
assessed only among combat veterans.
Abbreviations: VA = Department of Veterans affairs.
Regression Analyses
Table 2 compares psychiatric, medical, and functioning variable by VA user status. The column labeled “Bivariate Test of Difference” displays a series of independent-samples t and chi-square tests that were conducted to compare each characteristic by VA utilization status. The column labeled “Multivariable Tests” shows the results of the 13 linear and 36 logistic multivariable regression analyses. This column reports the relation between VA user status and psychiatric, medical, and functioning variables after adjustment for sociodemographic and military variables that differed bivariately (p < 0.05) by VA user status. Importantly, alpha was adjusted to 0.01 to help control against both Type I and Type II errors. Given that predictors for the ROC analysis were determined by the results of these regressions, it was important to we identify all variables that could potentially influence prediction of VA utilization. demonstrated that veterans that utilized VA as their primary source of healthcare were more likely than those who did not to experience lifetime psychopathology. Specifically, they were more likely to screen positive for lifetime PTSD, social phobia, drug use disorder, suicide attempt and current depression, anxiety, and suicidal ideation. They also were more likely to report a history of trauma and a greater number of traumas. VA utilizers were more likely to report receiving prior mental health treatment. In terms of medical conditions, veterans who utilize VA were more likely to have a history of a medical condition and a greater number of medical conditions. Specifically, veterans utilizing VA were more likely to have lung conditions (e.g., asthma, bronchitis, COPD), chronic pain, liver disease, heart disease, high cholesterol and blood pressure, sleep disorder, migraine, osteoporosis/osteopenia, and rheumatoid arthritis. Additionally, VA utilizers were more likely to report a disability and greater difficulties with cognitive, physical, and mental functioning.
Table 2.
Differences in Psychiatric, Medical, and Functioning by Primary Use of VA Healthcare Service Status
| Bivariate Test of Difference | Multivariable Tests | |||||||
|---|---|---|---|---|---|---|---|---|
| Measure | Total (N = 3,152) |
Non-VA user (n = 2,547)a |
VA-user (n = 608)a |
t/p^ or χ2 | P | Wald x2 or F | P | Adjusted OR (95% CI) or Cohen db |
| Psychiatric measures, n (%) | ||||||||
| Lifetime | ||||||||
| Mental health treatment | 676 (21.4) | 444 (17.5) | 242 (40.2) | 147.05 | < 0.01 | 77.41 | < 0.01 | 2.56 (2.09–3.20) |
| Psychopathology | 716 (22.7) | 497 (19.7) | 230 (38.3) | 93.21 | < 0.01 | 35.36 | < 0.01 | 1.93 (1.56–2.40) |
| Psychopathology + SUD | 454 (14.4) | 319 (12.7) | 150 (24.9) | 57.13 | < 0.01 | 17.97 | < 0.01 | 1.69 (1.32–2.15) |
| Posttraumatic stress disorder | 306 (9.7) | 217 (8.6) | 131 (21.8) | 84.76 | < 0.01 | 18.92 | < 0.01 | 1.81 (1.39–2.37) |
| Depression | 517 (16.4) | 352 (13.8) | 183 (30.1) | 92.37 | < 0.01 | 40.29 | < 0.01 | 2.12 (1.68–2.67) |
| Social phobia | 271 (8.6) | 196 (7.7) | 105 (17.3) | 52.14 | < 0.01 | 16.44 | < 0.01 | 1.80 (1.35–2.38) |
| Alcohol use disorder | 1282 (40.7) | 1064 (41.8) | 266 (43.8) | 0.79 | .385 | 0.00 | 0.97 | 1.00 (0.82–1.21) |
| Drug use disorder | 386 (12.2) | 297 (11.7) | 126 (20.7) | 34.73 | < 0.01 | 19.20 | < 0.01 | 1.78 (1.37–2.30) |
| Substance use disorder | 1342 (42.6) | 1108 (43.5) | 284 (46.8) | 2.15 | 0.15 | 0.18 | 0.67 | 1.04 (0.86–1.26) |
| Suicide attempt | 165 (5.2) | 129 (5.1) | 88 (14.5) | 67.41 | < 0.01 | 20.26 | < 0.01 | 2.08 (1.51–2.85) |
| Current | ||||||||
| Depression | 212 (6.7) | 153 (6.1) | 93 (15.3) | 57.59 | < 0.01 | 10.91 | < 0.01 | 1.66 (1.23–2.24) |
| Anxiety | 202 (6.4) | 157 (6.2) | 92 (15.2) | 53.10 | < 0.01 | 11.77 | < 0.01 | 1.69 (1.25–2.27) |
| Suicidal ideation | 222 (7.0) | 178 (7.1) | 107 (17.7) | 65.98 | < 0.01 | 19.02 | < 0.01 | 1.87 (1.41–2.48) |
| Alcohol use disorder | 264 (8.4) | 219 (12.3) | 75 (19.3) | 13.36 | < 0.01 | 3.08 | 0.08 | 1.33 (0.97–1.83) |
| Traumatic event | 2730 (86.6) | 2184 (86.1) | 552 (91.5) | 12.94 | < 0.01 | 9.06 | < 0.01 | 1.64 (1.19–2.27) |
| Total traumas, mean (SD) | 3.30 (2.7) | 3.07 (2.5) | 4.70 (3.4) | 0.20^ | < 0.01 | 40.70 | < 0.01 | 0.15 |
| Medical conditions, n % | ||||||||
| Any medical diagnosis | 2746 (87.1) | 2161 (84.8) | 548 (90.3) | 11.95 | < 0.01 | 15.31 | < 0.01 | 1.90 (1.38–2.63) |
| Arthritis | 983 (31.2) | 723 (28.4) | 209 (34.4) | 8.42 | < 0.01 | 11.73 | < 0.01 | 1.44 (1.17–1.78) |
| Lung conditions | 341 (10.8) | 259 (10.2) | 89 (14.6) | 9.99 | < 0.01 | 4.69 | < 0.05 | 1.36 (1.03–1.79) |
| Cancer | 492 (15.6) | 408 (16.0) | 70 (11.5) | 7.75 | < 0.01 | 0.01 | 0.91 | 0.98 (0.73–1.33) |
| Chronic pain | 595 (18.9) | 438 (17.2) | 188 (31.0) | 58.47 | < 0.01 | 34.94 | < 0.01 | 1.91 (1.54–2.37) |
| Liver disease | 54 (1.7) | 35 (1.4) | 24 (3.9) | 17.71 | < 0.01 | 7.98 | < 0.01 | 2.28 (1.29–4.05) |
| Diabetes | 597 (18.9) | 427 (16.8) | 120 (19.7) | 3.03 | 0.08 | 3.58 | 0.06 | 1.27 (0.99–1.61) |
| Heart disease | 443 (14.1) | 347 (13.6) | 95 (15.6) | 1.63 | 0.22 | 5.63 | < 0.05 | 1.40 (1.06–1.85) |
| Heart attack | 254 (8.1) | 209 (8.2) | 56 (9.2) | 0.64 | 0.42 | 2.57 | 0.11 | 1.32 (0.94–1.86) |
| High cholesterol | 1563 (49.6) | 1166 (45.8) | 292 (48.0) | 0.10 | 0.32 | 9.45 | < 0.01 | 1.36 (1.12–1.66) |
| High blood pressure | 1600 (50.8) | 1195 (46.9) | 330 (54.3) | 10.64 | < 0.01 | 17.62 | < 0.01 | 1.55 (1.26–1.90) |
| Kidney disease | 84 (2.7) | 71 (2.8) | 15 (2.5) | 0.19 | 0.78 | 0.19 | 0.66 | 0.87 (0.47–1.61) |
| Sleep disorders | 600 (19.0) | 434 (17.0) | 183 (30.1) | 53.21 | < 0.01 | 23.40 | < 0.01 | 1.70 (1.37–2.11) |
| Migraine | 198 (6.3) | 137 (5.4) | 58 (9.5) | 14.65 | < 0.01 | 4.90 | < 0.05 | 1.49 (1.05–2.11) |
| Multiple sclerosis | 5 (0.2) | 3 (0.1) | 2 (0.3) | 1.38 | 0.25 | 0.55 | 0.46 | 2.34 (0.25–21.83) |
| Osteoporosis | 100 (3.2) | 59 (2.3) | 25 (4.1) | 6.11 | < 0.05 | 5.92 | < 0.05 | 1.93 (1.14–3.29) |
| Rheumatoid arthritis | 110 (3.5) | 78 (3.1) | 40 (6.6) | 13.84 | < 0.01 | 9.12 | < 0.01 | 1.92 (1.26–2.93) |
| Stroke | 67 (2.1) | 51 (2.0) | 8 (1.3) | 1.26 | 0.32 | 1.21 | 0.27 | 0.64 (0.29–1.42) |
| Traumatic brain injury | 16 (0.5) | 14 (0.5) | 4 (0.7) | 0.10 | 0.76 | 1.50 | 0.22 | 2.08 (0.39–10.98) |
| HIV/AIDS | 11 (0.3) | 4 (0.2) | 3 (0.5) | 2.51 | 0.14 | 42.81 | 0.39 | 2.24 (1.76–2.85) |
| Sum medical conditions, mean (SD) | 2.7 (2.0) | 2.5 (1.9) | 3.1 (2.2) | 4.96 | < 0.01 | 61.21 | < 0.01 | 0.14 |
| Functioning | ||||||||
| Any disability | 385 (12.2) | 255 (10.0) | 153 (25.2) | 100.00 | < 0.01 | 42.81 | < 0.01 | 2.24 (1.76–2.85) |
| Cognitive functioning, mean (SD) | 90.1 (14.1) | 91.1 (12.9) | 81.2 (22.1) | −0.21^ | < 0.01 | 35.58 | < 0.01 | −0.18 |
| SF-8 mental summary, mean (SD) | 63.7 (8.0) | 64.1 (7.6) | 59.0 (12.1) | −0.19^ | < 0.01 | 46.22 | < 0.01 | −0.16 |
| Vitality | 50.8 (7.4) | 50.9 (7.2) | 47.9 (8.8) | 7.58 | < 0.01 | 17.96 | < 0.01 | −0.11 |
| Social functioning | 50.7 (7.5) | 51.5 (7.0) | 46.3 (10.2) | −0.23^ | < 0.01 | 30.12 | < 0.01 | −0.19 |
| Mental health | 52.4 (7.2) | 52.9 (6.9) | 48.3 (10.5) | −0.22^ | < 0.01 | 41.57 | < 0.01 | −0.16 |
| Role-emotional | 49.8 (5.8) | 50.1 (5.5) | 46.9 (8.6) | −0.20^ | < 0.01 | 26.28 | < 0.01 | −0.14 |
| SF-8 physical summary, mean (SD) | 57.0 (9.7) | 57.5 (9.2) | 53.1 (11.4) | −0.15^ | < 0.01 | 27.36 | < 0.01 | −0.16 |
| General health | 49.0 (7.7) | 49.2 (7.4) | 45.1 (8.7) | 10.60 | < 0.01 | 28.04 | < 0.01 | −0.16 |
| Physical functioning | 47.5 (8.3) | 48.0 (8.1) | 44.5 (10.0) | −0.14^ | < 0.01 | 20.77 | < 0.01 | −0.14 |
| Role-physical | 48.2 (8.6) | 48.6 (7.8) | 44.4 (10.2) | −0.18^ | < 0.01 | 27.90 | < 0.01 | −0.16 |
| Bodily Pain | 48.8 (8.4) | 49.4 (8.2) | 45.5 (9.8) | 8.94 | < 0.01 | 16.49 | < 0.01 | −0.16 |
values are weighted
ORs (95% CIs) and Cohen d estimates are adjusted for age, gender, race/ethnicity, income, education, marital status, branch of service, combat status, and years in the military.
Lifetime psychopathology = major depression disorder, social phobia, posttraumatic stress disorder, or suicide attempt.
Lifetime substance use disorder = was categorized as lifetime alcohol use disorder or drug use disorder.
Spearman rho correlation (p) is provided because of non-normal [skewed, kurtotic] distribution.
Abbreviations: VA = Department of Veterans Affairs; HIV = human immunodeficiency virus; AIDS = acquired immunodeficiency syndrome; SF-8 = Short form-8 Health Survey.
ROC Analyses
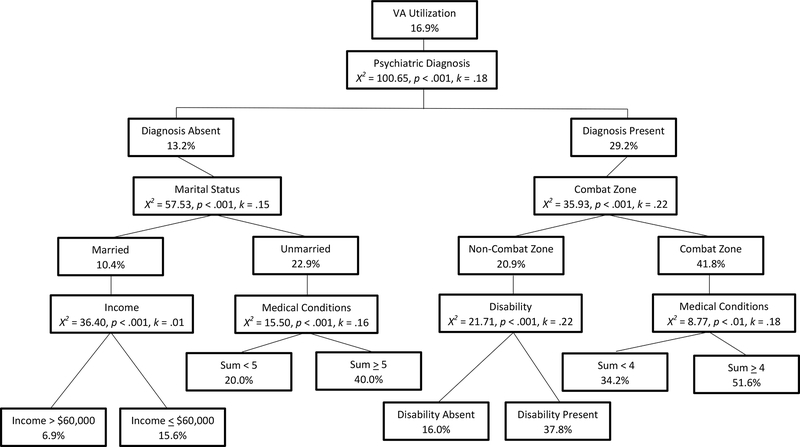
Figure 1 displays the results from the primary ROC analyses. This model included significant sociodemographic and military covariates, any disability, lifetime SUD, lifetime psychopathology, sum of medical conditions, lifetime mental health treatment, and suicide attempt. The primary factor that differentiated those who utilize VA services was lifetime psychopathology. Lifetime psychopathology was used to divide the sample into two subsamples, and the next predicting variable divides the higher-risk subsample. Specifically, 29.2% of those with a lifetime psychopathology endorsed VA utilization compared to 13.2% of those without. Individuals with lifetime psychopathology were further differentiated by service in a combat zone whereas 41.8% of those who served in a combat zone utilized VA compared to 20.9% of those who did not. Among those who served in a combat zone, 51.6% of veterans with four or more medical conditions reported VA utilization compared to 34.2% of those with less than four medical conditions. Among those who served in a non-combat zone, 37.8% of veterans who had a physical disability reported VA utilization compared to 16.0% of those who did not.
Figure 1.
Graphical depiction of primary ROC analysis
Among veterans without lifetime psychopathology, 22.9% of unmarried veterans endorsed VA utilization compared to 10.4% of married veterans. Sum of medical conditions further differentiated unmarried veterans, as 40.0% of those who endorsed five or more medical conditions utilized VA compared to 20.0% of those who endorsed less than five medical conditions. Among those who were married, 15.6% of veterans with a gross income of less than $60,000 per year reported VA utilization compared to 6.9% of veterans with a gross income of $60,000 or more per year.
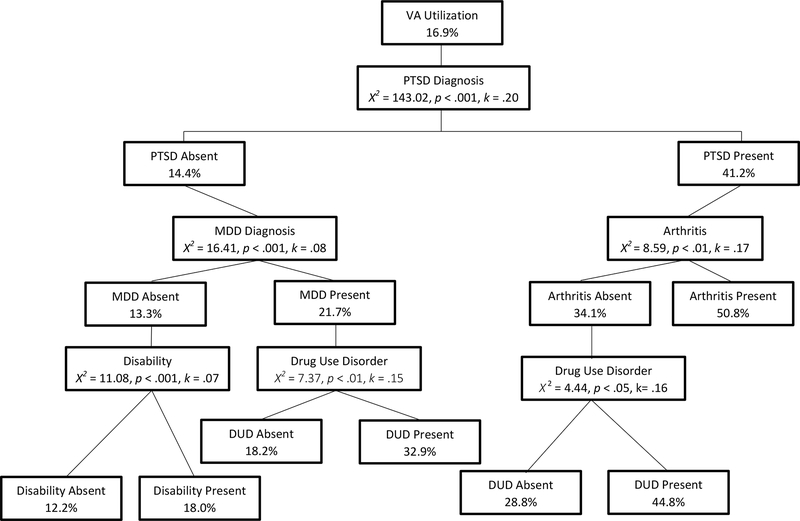
After determining that lifetime psychopathology and sum of medical conditions differentiated those who utilize VA, we ran a specificity analysis including all lifetime psychiatric and medical conditions (see Figure 2). The primary factor that differentiated those who utilize VA services was lifetime PTSD diagnosis. Specifically, 41.2% of those with a lifetime PTSD diagnosis endorsed VA utilization compared to 14.4% of those without a PTSD diagnosis. Individuals with a lifetime PTSD diagnosis were further differentiated by arthritis diagnosis whereas 50.8% of those who were diagnosed with arthritis utilized VA compared to 34.1% of those who were not. Among those without an arthritis diagnosis, 44.8% of veterans with a drug use disorder reported VA utilization compared to 28.8% of those without a drug use disorder.
Figure 2.
Graphical depiction of specificity ROC analysis
Among those without a lifetime PTSD diagnosis, 21.7% of veterans who had a lifetime MDD diagnosis endorsed VA utilization compared to 13.3% of Veterans who did not. Veterans with MDD were further differentiated by lifetime drug use disorder whereas 32.9% of those who endorsed a drug use disorder utilized VA compared to 18.2% of those who did not. Among those without lifetime MDD, 18.0% of veterans with a disability reported VA utilization compared to 12.2% of those without a disability.
Discussion
To our knowledge, the present study is among the first to identify characteristics associated with a greater likelihood of using the VA as the primary source of healthcare in the U.S. veteran population. Additionally, this study uses a novel statistical analysis approach to determine significant differences between veterans who do and do not utilize VA services. The use of ROC analyses and logistic and linear regressions provides a comprehensive and multivariate examination of factors associated with VA utilization. ROC analyses are uniquely able to identify systematic interactions among many categorical and continuous variables and are especially useful in analyses where predictors are likely to be highly collinear and interactions between independent variables exist27.
The study findings are consistent with prior research demonstrating that beliefs about psychiatric problems vary across cultural groups and genders which may lead to differences in help-seeking attitudes and behaviors30. For instance, men, especially younger men, are more likely than women to avoid or delay seeking help for medical and mental health concerns31,32. However, women may be deterred from using the VA due to perceptions that the VA lacks care that is sensitive to issues of women’s health33.
Findings from the current study may help inform resource allocation and program development within the VA. Specifically, results highlight the increased need for specialty services targeting PTSD, depression, anxiety, social phobia, DUD, and suicidality, as these mental health disorders were significantly more prevalent in VA users. Meanwhile, the findings that nearly 1 in 5 VA users (17.7%) are contemplating suicide and 14.5% of VA users have attempted suicide demonstrates the continued need for suicide prevention programs and emergency psychiatric services.
Consistent with prior research, VA users were more likely to have lifetime psychopathology. Importantly, researchers have highlighted the concern that veterans exhibit a gap in rates of mental illness versus help-seeking compared to civilians34. Approximately 25% of recently returning veterans experience mental health challenges35. Veterans with mental health challenges will often not seek out treatment despite their being eligible for VA care35, potentially due to low satisfaction with services, poor perceptions of care quality, and difficulty navigating the VA system12, 33, 36. Further, combat veterans may need more services, as combat exposure increases the likelihood of experiencing traumatic events, such as an attack or ambush, which are in turn linked to elevated risk of PTSD, depression, substance use and other problems37. Findings also highlight the importance of targeted services for physical health conditions, as VA users endorsed a greater number of medical conditions. Older veterans, specifically, are more likely to experience co-occurring mental and physical health challenges38.
There are limitations to this study that are worth noting. First, the survey for this study was conducted in 2011. As the VA continues to undergo changes to better meet the evolving demographics and needs of veterans, it is important to re-evaluate utilization. Second, women make up about ten percent of the sample in this study. Future research should oversample female veterans to better-understand their healthcare utilization patterns. Third, VA utilization status was assessed using a single-item that asked if the VA was the primary source of healthcare. Therefore, it was not possible to differentiate between those who do not utilize VA healthcare at all and those who utilize VA as a secondary source of healthcare. Additionally, it is unknown whether the 83% of veterans that said they did not use VA as their primary source of healthcare are receiving healthcare elsewhere. The current study also did not gauge utilization of specific services.
Notwithstanding these limitations, results of this study have several implications for clinical practice. First, outreach strategies tailored to specific groups of veterans identified as not using the VA could help to improve access. For example, this study found that veterans who did not use VA as their primary healthcare were more likely to be older and outreach efforts that target older individuals may be beneficial. Rickwood and colleagues32 note that efforts to improve help-seeking must improve both the population’s awareness of the available services, and the willingness or motivation to reach out and communicate their needs. Further, Pietrzak and colleagues12 recommend use of education to increase access to information about mental health care, decrease stigma, and to help veterans navigate barriers to care. Future research could focus on development and evaluation of programs to raise awareness and educate veterans on the procedures required to access VA services. Education efforts may also target cultural and/or social norms that interfere with help-seeking behavior in veterans. Additionally, given the importance of social support in help-seeking among veterans, support for families caring for veterans represents a potentially high yield target12. Future research should evaluate currently offered services, such as VA Program of Comprehensive Assistance for Family Caregivers, to develop improved efforts for educating and supporting veterans and their families39.
In summary, this study highlights that there are many veterans who do not utilize VA services as their primary source of healthcare. Through better understanding the factors that predict use of VA services, research can identify strategies to ensure that more veterans get the care they need. Employment of qualitative methods to gather information from non-VA utilizers could help elucidate the needs of these veterans and deterring factors. Finally, other factors that have been barriers to care for veterans in the past, such as sexual minority status, should be examined to better understand the full picture of VA utilization for more marginalized groups.
Clinical Points.
Veterans who use VA healthcare services have a substantially elevated health burden compared to other veterans.
There is an increased need for specialty VA services targeting posttraumatic stress disorder, depression, anxiety, social phobia, drug use disorder, and suicidality in veterans.
Research can inform outreach and engagement initiatives targeting the unique healthcare needs of veterans who do and do not utilize VA services.
Acknowledgments
Funding/Support: The National Health and Resilience in Veterans Study was funded by the U.S. Department of Veterans Affairs National Center for Posttraumatic Stress Disorder. Preparation of this report was supported in part by a VA Rehabilitation Research and Development Career Development Award – 2 (1IK2RX001492–01A1) granted to Dr. Heinz. The expressed views do not necessarily represent those of the Department of Veterans Affairs.
Role of sponsor: The funding sources had no role in the design, analysis, interpretation, or publication of this study.
Footnotes
Previous Presentation: Poster presentation at the annual convention of APA in San Francisco, California, May 26, 2018. Paper presented at the annual Health Services Research Conference in Menlo Park, California, May 15, 2018.
Potential Conflicts of Interest: None.
Contributor Information
Catherine Hausman, Pacific Graduate School of Psychology, Palo Alto University, Palo Alto, CA
Adrienne J. Heinz, Dissemination and Training Division, National Center for PTSD, and Center for Innovation to Implementation, Veterans Affairs Palo Alto Healthcare System, Menlo Park, CA
References
- 1.Bagalman E The number of veterans that use VA health care services: a fact sheet In: Congressional Research Service; June 3, 2014. https://fas.org/sgp/crs/misc/R43579.pdf. Accessed April 24, 2018. [Google Scholar]
- 2.VA utilization profile FY 2016 National Center for Veterans Analysis and Statistics. https://www.va.gov/vetdata/docs/Quickfacts/VA_Utilization_Profile.pdf Published November 2017 Nov. Accessed April 24th, 2018 Apr 24 [Google Scholar]
- 3.Gaziano JM, Concato J, Galea S, Smith NL, Provenzale D. Epidemiologic approaches to veterans’ health. Epidemiol Rev. 2015;37(1):1–6. 10.1093/epirev/mxu013 [DOI] [PubMed] [Google Scholar]
- 4.Jakupcak M, Cook J, Imel Z, Fontana A, Rosenheck R, McFall M. Posttraumatic stress disorder as a risk factor for suicidal ideation in Iraq and Afghanistan war veterans. J Trauma Stress. 2009;22(4):303–6. 10.1002/jts.20423 [DOI] [PubMed] [Google Scholar]
- 5.Qureshi SU, Pyne JM, Magruder KM, Schulz PE, Kunik ME. The link between post-traumatic stress disorder and physical comorbidities: a systematic review. Psychiatr Q. 2009;80(2):87–97. 10.1007/s11126-009-9096-4 [DOI] [PubMed] [Google Scholar]
- 6.Galea S, Basham K, Culpepper L, et al. Treatment for posttraumatic stress disorder in military and veteran populations: initial assessment. The National Academies, July 2012. http://www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2012/PTSD-Initial-Assessment/PTSD_I_RB.pdf. Accessed April 24, 2018 Apr 24. [PubMed] [Google Scholar]
- 7.Suicide among veterans and other Americans, 2001–2014. Office of Mental Health and Suicide Prevention. August 3, 2016. https://www.mentalhealth.va.gov/docs/2016suicidedatareport.pdf. Updated August 2017. Accessed April 24, 2018.
- 8.Profile of veterans: 2016. Data from the American Community Survey. National Center for Veterans Analysis and Statistics, Department of Veterans Affairs. February 2018. https://www.va.gov/vetdata/docs/SpecialReports/Profile_of_Veterans_2016.pdf. Accessed April 26, 2018. [Google Scholar]
- 9.RAND corporation. VA health care system faces significant challenges, but meets the needs of most eligible veterans. February 8, 2016. https://www.rand.org/news/press/2016/02/08/index1.html. Accessed April 24, 2018.
- 10.O’Hanlon C, Huang C, Sloss E, et al. Comparing VA and non-VA quality of care: a systematic review. J Gen Intern Med. 2017;32(1):105–21. 10.1007/s11606-016-3775-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Returning Home from Iraq and Afghanistan: Assessment of Readjustment Needs of Veterans, Service Members, and Their Families. The National Academies Press, Institute of Medicine, March 12, 2013. 10.17226/13499. Accessed April 24, 2018. [DOI] [PubMed] [Google Scholar]
- 12.Pietrzak RH, Johnson DC, Goldstein MB, Malley JC, Southwick SM. Perceived stigma and barriers to mental health care utilization among OEF-OIF veterans. Psychiatr Serv. 2009;60(8):1118–22. 10.1176/ps.2009.60.8.1118 [DOI] [PubMed] [Google Scholar]
- 13.Final report of the commission on care. Commission on Care. June 30, 2016 https://s3.amazonaws.com/sitesusa/wp-content/uploads/sites/912/2016/07/Commission-on-Care_Final-Report_063016_FOR-WEB.pdf. Accessed April 24, 2018. [Google Scholar]
- 14.The VA healthcare system: a broken system with superior quality. Definitive Healthcare. April 24, 2017. https://blog.definitivehc.com/the-va-healthcare-system-a-broken-system-with-superior-quality. Accessed May 1, 2018. [Google Scholar]
- 15.Our care 2017: a report evaluating veteran’s health care. Veterans of Foreign Wars. March 2017. https://vfw-cdn.azureedge.net/-/media/VFWSite/Files/Advocacy/VFW-Our-Care-2017--Executive-Summary.pdf?la=en Accessed April 24, 2018. [Google Scholar]
- 16.Klingensmith K, Tsai J, Mota N, Southwick SM, Pietrzak RH. Military sexual trauma in US veterans: results from the National Health and Resilience in Veterans Study. J Clin Psychiatry. 2014;75(10), e1133–e1139. 10.4088/JCP.14m09244 [DOI] [PubMed] [Google Scholar]
- 17.Keane TM, Fairbank JA, Caddell JM, Zimering RT, Taylor KL, Mora CA. Clinical evaluation of a measure to assess combat exposure. Psychol Assess. 1989;1(1):53 10.1037/1040-3590.1.1.53 [DOI] [Google Scholar]
- 18.Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):2233. [PubMed] [Google Scholar]
- 19.Rumpf HJ, Hapke U, Meyer C, John U. Screening for alcohol use disorders and at-risk drinking in the general population: psychometric performance of three questionnaires. Alcohol Alcohol. 2002;37(3):261–8. 10.1093/alcalc/37.3.261 [DOI] [PubMed] [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics. 2009;50(6):613–21. 10.1016/S0033-3182(09)70864-3 [DOI] [PubMed] [Google Scholar]
- 21.Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD checklist (PCL): reliability, validity, and diagnostic utility In annual convention of the international society for traumatic stress studies, San Antonio, TX, vol. 462; 1993. https://www.researchgate.net/profile/Frank_Weathers/publication/291448760_The_PTSD_Checklist_PCL_Reliability_validity_and_diagnostic_utility/links/57c7125408ae28c01d4f7e70/The-PTSD-Checklist-PCL-Reliability-validity-and-diagnostic-utility [Google Scholar]
- 22.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD checklist (PCL). Behav Res Ther. 1996;34(8):669–73. 10.1016/0005-7967(96)00033-2 [DOI] [PubMed] [Google Scholar]
- 23.Carlson EB, Smith SR, Palmieri PA, et al. Development and validation of a brief self-report measure of trauma exposure: The Trauma History Screen. Psychol Assess. 2011;23(2):463 10.1037/a0022294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.QualityMetric. SF-8 Health Survey. Boston MA, Qualitymetric, 2014. [Google Scholar]
- 25.Stewart A, Ware JE, Sherbourne CD, Wells KB. Psychological distress/well-being and cognitive functioning measures In: Stewart AL, Ware JE, eds. Measuring Functioning and Well-Being: The Medical Outcomes Study Approach. Durham, NC: Duke University; 1992;102–142. [Google Scholar]
- 26.Hardy SE, Gill TM. Recovery from disability among community-dwelling older persons. JAMA. 2004. April;291(13):1596–602. doi: 10.1001/jama.291.13.1596 [DOI] [PubMed] [Google Scholar]
- 27.Kiernan M, Kraemer HC, Winkleby MA, King AC, Taylor CB. Do logistic regression and signal detection identify different subgroups at risk? Implications for the design of tailored interventions. Psychol Methods. 2001;6(1):35. [DOI] [PubMed] [Google Scholar]
- 28.Current population survey. US Census Bureau website. https://www.census.gov/programs-surveys/cps/data-detail.html Updated March 6, 2018. Accessed April 26, 2018. [Google Scholar]
- 29.Profile of veterans: 2014. Data from the American Community Survey. National Center for Veterans Analysis and Statistics, Department of Veterans Affairs. March 2016. https://www.va.gov/vetdata/docs/SpecialReports/Profile_of_Veterans_2014.pdf Accessed April 26, 2018. [Google Scholar]
- 30.Sheikh S, Furnham A. A cross-cultural study of mental health beliefs and attitudes towards seeking professional help. Soc Psychiatry Psychiatr Epidemiol. 2000;35(7):326–34. 10.1007/s001270050246 [DOI] [PubMed] [Google Scholar]
- 31.Galdas PM, Cheater F, Marshall P. Men and health help‐seeking behaviour: literature review. J Adv Nurs. 2005;49(6):616–23. 10.1111/j.1365-2648.2004.03331.x [DOI] [PubMed] [Google Scholar]
- 32.Rickwood D, Deane FP, Wilson CJ, Ciarrochi J. Young people’s help-seeking for mental health problems. Australian e-journal for the Advancement of Mental health. 2005;4(3):218–51. DOI: 10.5172/jamh.4.3.218 [DOI] [Google Scholar]
- 33.Washington DL, Kleimann S, Michelini AN, Kleimann KM, Canning M. Women veterans’ perceptions and decision-making about Veterans Affairs health care. Mil Med. 2007;172(8):812–7. 10.7205/MILMED.172.8.812 [DOI] [PubMed] [Google Scholar]
- 34.Fortney JC, Curran GM, Hunt JB, et al. Prevalence of probable mental disorders and help-seeking behaviors among veteran and non-veteran community college students. Gen Hosp Psychiatry. 2016;38:99–104. 10.1016/j.genhosppsych.2015.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stecker T, Fortney JC, Hamilton F, Ajzen I. An assessment of beliefs about mental health care among veterans who served in Iraq. Psychiatr Serv. 2007;58(10):1358–61. https://ps.psychiatryonline.org/doi/full/10.1176/ps.2007.58.10.1358 [DOI] [PubMed] [Google Scholar]
- 36.Blay E, DeLancey JO, Hewitt DB, Chung JW, Bilimoria KY. Initial public reporting of quality at Veterans Affairs vs non–Veterans Affairs hospitals. JAMA Intern Med. 2017;177(6):882–5. doi: 10.1001/jamainternmed.2017.0605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Farmer CM, Vaughan CA, Garnett J, Weinick RM. Pre-deployment stress, mental health, and help-seeking behaviors among marines. Rand Health Q. 2015;5(1). [PMC free article] [PubMed] [Google Scholar]
- 38.Qureshi SU, Kimbrell T, Pyne JM, et al. Greater prevalence and incidence of dementia in older veterans with posttraumatic stress disorder. [See editorial comments by Dr. Soo Borson, pp 1797–1798]. J Am Geriatr Soc. 2010;58(9):1627–33. DOI: 10.1111/j.1532-5415.2010.02977.x [DOI] [PubMed] [Google Scholar]
- 39.Shepherd-Banigan M, Smith VA, Maciejewski ML, et al. The effect of support and training for family members on access to outpatient services for veterans with posttraumatic stress disorder (PTSD). Adm Policy Ment Health. 2018;January:1–5. 10.1007/s10488-017-0844-8 [DOI] [PMC free article] [PubMed] [Google Scholar]