Abstract
Anaemia prevalence in pregnant women of India declined from 57.9% to 50.3% from National Family Health Survey (NFHS)-3 to NFHS-4. However, over the course of that decade, the uptake of iron and folic acid (IFA) supplementation for 100 days of pregnancy improved by only 15%. To understand demand side risk factors of anaemia specifically related to IFA intake, an in-depth survey was conducted on pregnant women (n = 436) in 50 villages and wards of Sirohi district of Rajasthan, India. At the demand side, consistent IFA consumption in the previous trimester was inversely and strongly associated with anaemia (OR: 0.26, 95% CI: 0.12, 0.55). Reasons for inconsistent consumption included not registering to antenatal clinic, not receiving IFA tablets from the health worker and perceived lack of need. At the supply side, an analysis of IFA stock data at various levels of the health care (n = 168) providers from primary to tertiary levels showed that 14 out of 52 villages surveyed did not have access to IFA tablets. The closest availability of an IFA tablet for 16 villages, was more than 5 km away. To improve the uptake of IFA supplementation and thereby reduce iron deficiency anaemia in pregnant women, a constant supply of IFA at the village or sub-centre level, where frontline workers can promote uptake, should be ensured.
Introduction
Anaemia is characterised by low haemoglobin concentrations and could lead to adverse health outcomes such as maternal and peri-natal mortality and low birth weight [1,2]. In India, particularly among pregnant women, anaemia is a major public health problem, with the recently concluded nationally representative NFHS-4 [3] reporting a prevalence of 50.3%, with not much variation between rural (54.3%) and urban (50.9%) populations.
Iron deficiency is probably the most common cause of anaemia in India [4]. For this reason, under the National Iron Plus Initiative (NIPI, [5]), the government of India provides daily doses of IFA to pregnant women for a period of 100 days during their pregnancy. However, despite revisions to the NIPI programme with an increase in provision of elemental iron from 60 mg to 100 mg, the prevalence of anaemia in pregnant women has not come down significantly in the last 10 years between the nationally representative surveys, NFHS-3 conducted in 2005–2006 and NFHS-4 conducted between 2015–2016 among women aged 15–49 years. (Fig 1).
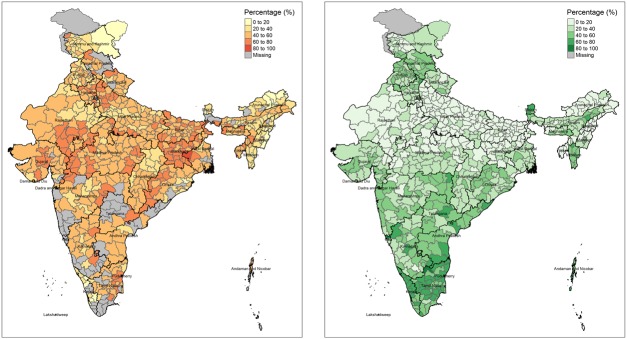
Fig 1. Findings from National Family Health Survey-4 related to anaemia in pregnant women.
(A) Anaemia among Pregnant women and (B) percentage of women consuming 100 or more IFA tablets in India by district (NFHS-4). The maps were created from shapefiles available freely from datameet.org using tmap package (https://cran.r-project.org/web/packages/tmap/index.html) in R.
Plausible explanations for this continuing burden of anaemia, in spite of an apparently improved, but still not satisfactory compliance to the NIPI program as reported by NFHS surveys, are attributed to dietary and environmental reasons. The dietary reasons include an even lower than estimated iron density of diet, inhibition of iron supplement absorption due to diet components such as phytate and polyphenols [6,7] and a predominantly vegetarian diet leading to low intake compared to highly bioavailable heme iron [8–10]. The presence of the “leaky gut” syndrome [11,12] or environmental enteric dysfunction (EED) driven by water, sanitation and hygiene (WASH), hookworm infestation [13], and genetic causes [14,15] are other possible reasons.
An equally plausible set of reasons for the continuing prevalence of anaemia relates to the poor coverage of the IFA supplementation. This is expected to reach the pregnant women either through the antenatal services (ANC) or through frontline health workers. Although, the NFHS [3] surveys report an improvement in the uptake of IFA from 15.2% to 30.3% at a national level from round 3 to 4, it is far from being sufficient. There are both demand-side and supply-side problems contributing to the situation. There are important demand-side considerations, such as side effects, poor antenatal care utilization and forgetfulness, which are well known [16–18] and are held responsible for low compliance. However, there are little data on the supply-side deficiencies in an uncontrolled setting, such as relationship between antenatal care provision, health worker motivation [19] and availability of IFA stocks across different public health facilities [20,21], though periodical surveys such as the National Family Health Surveys tend to report some, but not all of these issues. An important logistic component relates to the distance to health facilities [22–24], that in turn determines health seeking behaviour. This has not been studied in any systematic way, to determine its impact. This paper studies the risk factors associated with anaemia and the coverage of the flagship IFA supplementation program (NIPI), among pregnant women in Sirohi district, Rajasthan, and maps the distance to the nearest iron supplements for women in the villages surveyed.
Methods
An in-depth district level survey was conducted to collect data pertaining to both the demand-side from the perspective of the individual and the supply-side by examining facility level data. To study associated risk factors of anaemia at an individual level resulting from inadequate dietary intake and low compliance towards IFA tablets, data from survey, conducted in pregnant women in Sirohi District in Rajasthan state between March to June 2016, were used. This survey had collected detailed information on 5,324 households from 52 villages and wards, on maternal and child health in Sirohi, and aimed to identify the major risk factors of anaemia in children (0 to 59 months), adolescent girls (10 to 19 years), pregnant and lactating women, and stunting in children and adolescent girls. The survey also included a supply-side component which aimed to understand the functioning of the health system (from village to district level) in addressing malnutrition. All data other than the biomarkers were collected using questionnaires which were developed in consultation with experts and referring to literature on the current evidence available on nutrition specific and nutrition sensitive factors associated with malnutrition, anaemia and stunting, surveys conducted in India and elsewhere, and health system guidelines. The questionnaires were pre-tested and translated to local language before being used in the field.
Ethical approval
Ethical approval was obtained from the institutional ethics committee of the St John’s Medical College and informed written consent was obtained from each of the survey respondents both from the demand and the supply side. Permission from the state health department and the office of the district collector were procured prior to commencement of the survey.
Survey design
A multi-stage cluster sampling of Primary Sampling Units (PSU) which were villages (for rural areas) and wards (for urban areas) as per the Census of India [25] was employed. The sampling was stratified by block, rural-urban status and the PSUs were selected by probability proportional to size sampling. The definition of a village in rural areas corresponded to geographically defined villages, that relate to meaningful social and administrative divisions; in urban areas, communities are based on well-defined wards and are considered to be demographically homogeneous [26]. The eligible households were randomly sampled in the next stage of sampling for the demand survey. For the supply side component of the survey, the facilities catering to the sampled villages were surveyed. Geographical Information System (GIS) mapping of each village/ward was done. A village representative provided information on distance of village from different health facilities such as Sub Centre, Primary Health Centre (PHC), Community Health Centre (CHC), Sub Divisional Hospital, District Hospital and Private Clinics, and health workers such as Accredited Social Health Activists (ASHA) and Anganwadi Workers (AWW). ASHA workers report to an Auxiliary Nurse Midwife (AN) located at the Sub Centre. In Sirohi, six Sub Centres report administratively to either a PHC or a CHC, which then report to the District Hospital. Village level information on items such as local agricultural production, waste disposal, industrial emissions etc. were also collected from the Panchayat head or any senior literate and knowledgeable member of a village or ward.
Household information (Demand)
Household information on possessions, food security and details on education, age, occupation and marital status of members were collected from the head or a responsible adult member in the household. Data pertaining to medical information and diet of pregnant women collected in the survey was considered for this analysis. Trained field staff conducted interviews and anthropometric measurements of height and weight in all eligible individuals. Haemoglobin (Hb) was measured from capillary blood samples using Hemocue 301 analyzer in all sampled pregnant women. Pregnant women with Hb levels below 110g/l [27] were classified as anaemic for this analysis. The survey covered 454 pregnant women in Sirohi district, Rajasthan. Out of these, data on 436 subjects who had Hb measurements were considered for this analysis. There was no altitude adjustment of Hb required. Reported symptoms related to anaemia such as fatigue, were collected. IFA demand was measured in terms of receipt and consumption of IFA tablets for each trimester up to the trimester when a pregnant woman was recruited. Diet diversity was measured in terms of the food group consumed and had 11 categories of food groups. Additionally, frequency of consumption of vitamin A and vitamin C rich foods on a monthly basis was also collected. GIS data (Latitude, Longitude and Altitude) for households was measured using Samsung Tab 4—T231 (Samsung Electronics), an Android device commonly used in surveys.
Facility information (Supply)
To get the perspective from the supply side, health care personnel from 168 facilities (70 Accredited Social Health Activists or ASHAs, 52 Anganwadi workers, 30 Sub Centres, 20 Primary Health Centres, 6 Community Health Centres) in Sirohi catering to the villages/wards that were sampled were interviewed. In addition, specific questions on IFA supply was recorded at these centres, both by recording responses from health care providers as well as through observations by field workers of drug kits provided for ASHAs and AWW, and through stock checks in the pharmacy for Sub Centres and Primary Health Centres. GIS data for frontline workers (FLWs) in a village was assumed to be centroid of surveyed households in the village. GIS data for facilities was assumed to be location of village/town where the facility was housed, as this information for facilities was not collected. The distance to the nearest IFA tablet was the distance to the closest health facility which had IFA stocks had the sampled village in its catchment area.
Statistical analysis
Descriptive statistics were reported as numbers and percentage for categorical data and mean ± standard deviation for continuous normally distributed data. In the individual dataset, the factors associated with anaemia were analysed using chi square test, independent sample t test and Mann-Whitney U Test as appropriate. The significant factors from these analyses were used in bivariate and multiple variable logistic regression of anaemia. The factors considered for analysis in individual data sets were dietary diversity, health service utilization, morbidity, usage of intoxicant substances like paan (betel leaf, arecanut) and tobacco, water, sanitation and hygiene practices. Mobile usage was considered as a proxy for woman’s economic status. The factors were considered in the multiple variable analysis with a cut off value of p < 0.2 in bivariate logistic regression. The final model in the multiple variable analysis was identified using a hierarchical iterative process. Confounding and interaction effects were also explored. All analyses were performed using R software (https://cran.r-project.org/bin/windows/base/old/3.3.3/) and survey weighted logistic regression was carried with R survey package [28].
Results and discussion
Results
The survey covered a sample of 454 pregnant women of which haemoglobin was measured for 436 (4% non-respondents). There were 110, 187 and 139 pregnant women in their first, second and third trimesters respectively out of the 436, at the time of survey. A detailed description of the study population is provided in Table 1.
Table 1. Socio-demographic and economic characteristics of pregnant women in Sirohi district, India.
| N (%) | |
|---|---|
| Number of Pregnant women interviewed | 454 |
| Rural | 346 (76) |
| Urban | 108 (24) |
| Number of Pregnant women for whom Hb was measured | 436 (96) |
| Rural | 334 (97) |
| Urban | 102 (94) |
| Trimester | |
| First | 110 (25) |
| Second | 187 (43) |
| Third | 139 (32) |
| Age of household head# | 39.6 ± 13.9 |
| Educational level of household head (%) | |
| Illiterate | 47.9 |
| Primary (1st to 5th grade) | 16.5 |
| Type of family | |
| Nuclear | 258 (59) |
| Extended | 47 (11) |
| Joint | 131 (30) |
| Main source of income | |
| Agriculture | 55 (13) |
| Non-agriculture | 265 (61) |
| Both | 116 (27) |
| Household size# | 5.6 ± 2.2 |
| Socio-demographic characteristics of pregnant women | |
| Age (yrs.) # | 24.9 ± 4.6 |
| Literate | 169 (39) |
| Work for income | 111 (25) |
| Read state language | 140 (32) |
| Write state language | 133 (31) |
| Currently married | 429 (98) |
| Age at marriage > = 18 years | 274 (63) |
| Multiparous | 203 (47) |
| Use mosquito net | 228 (52) |
| Suffer from malaria in last three months | 16 (4) |
| Use mobile phone | 266 (61) |
#- Mean ± SD
While 66% of the women were anaemic, 35% were moderately or severely anaemic. General fatigue was the most reported anaemia related symptom among the anaemic women (59%) followed by giddiness, dizziness or headache. Among 299 anaemic women, 37 (12%) did not report any symptom and out of these 17 (6%) were mildly anaemic. Among 436 pregnant women, 303 (69%) reported registering for antenatal care, although the ANC card was available with only 209 (48%) of the respondents. Of the 227 with whom the card was not available, 66 (29%) were in their third trimester and 88 (39%) in the second trimester. About 59% of pregnant women chose to register at a government facility. Those who registered elsewhere (10%) cited quality of care, higher trust of non-government facilities and distance to government health centre as major reasons for not registering at a government centre. More information on utilization is available in Table 2.
Table 2. Antenatal care and morbidity of pregnant women in Sirohi district, India (N = 436).
| Antenatal services received by pregnant women | N (%) |
|---|---|
| Received antenatal check-up | 208 (48) |
| Physical Examination | 65 (15) |
| Measurement of weight | 62 (14) |
| BP measured | 59 (13) |
| Received TT vaccination | 48 (11) |
| Consumed IFA in previous month’s trimester^ | 155 (36) |
| Folic Acid received in 1st trimester as per ANC card# | 4 (4) |
| Folic Acid consumed in 1st trimester (previous month's trimester = 1)^# | 30 (20) |
| IFA received in 2nd or 3rd trimester* as per ANC card | 47 (14) |
| IFA consumed in 2nd/3rd trimester* (previous month's trimester = 2 or 3; N = 270) | 125 (46) |
| Ever Received deworming tablet as per ANC card during pregnancy | 11 (2) |
| Received professional breastfeeding counselling as per ANC card | 14 (4) |
| Hb examined at health centre as per ANC card | 71 (29) |
| Prevalence of Anaemia | 299 (69) |
| Mild anaemia | 146 (34) |
| Moderate anaemia | 140 (32) |
| Severe anaemia | 13 (3) |
| Morbidity (last one month) | |
| Diarrhoea | 64 (15) |
| Vomiting | 204 (47) |
| Fever | 117 (27) |
| Symptoms related to anaemia | |
| General fatigue | 259 (59) |
| Breathlessness on routine and somewhat strenuous work | 156 (36) |
| Giddiness, dizziness, headache | 197 (45) |
| Appetite loss | 125 (29) |
| Weight loss | 57 (13) |
| Blurring of vision | 149 (34) |
| Sudden swelling of feet | 68 (16) |
^—calculation does not include those women (N = 13) in their first month of pregnancy;
#—Folic Acid is provided in Trimester 1;
*—IFA is provided in Trimester 2 and 3
Factors associated with anaemia in pregnant women
The factors associated with anaemia in pregnancy in the bivariate and multiple variable logistic regression analyses are presented in Table 3. The final logistic regression model showed IFA supplementation to be negatively associated with anaemia such that there was 74% lower odds of anaemia with consistent consumption of IFA or folic acid supplement in previous trimester (OR: 0.26, 95% CI: 0.12 to 0.55, p = 0.001). In addition, month of pregnancy (OR: 1.21, p = 0.012), mobile usage (OR: 0.41, p = 0.010), usage of intoxicant substances (OR: 2.27, p = 0.075), number of women in household (OR: 0.72, p = 0.079) were also significantly associated with anaemia (Table 3).
Table 3. Individual and household characteristics associated with anaemia outcome in pregnant women of Sirohi district, India.
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Individual characteristics | Odds Ratio | P-value | Odds Ratio | P-value |
| Month of Pregnancy | 1.13 | 0.07 | 1.211 | 0.012 |
| Previous month's trimester | 1.58 | 0.05 | ||
| Writing state language | 0.49 | 0.09 | ||
| Mobile usage | 0.29 | <0.001 | 0.409 | 0.010 |
| Low BMI | 2.04 | 0.04 | ||
| Usage of tobacco | 3.20 | 0.03 | 2.268 | 0.075 |
| Past history of seizures | 2.45 | 0.06 | ||
| Awareness of health and nutrition programs | 0.95 | 0.08 | ||
| Receipt of blood transfusion in last 1 year | 9.74 | 0.03 | ||
| Dietary consumption | ||||
| vegetables and pulses | 0.62 | 0.02 | ||
| Guava | 1.33 | 0.09 | ||
| Jackfruit | 0.63 | 0.02 | ||
| Papaya | 1.69 | 0.05 | ||
| Pumpkin | 0.02 | 0.04 | ||
| Avoid meat | 9.10 | 0.03 | ||
| Avoid poultry | 23.31 | 0.01 | ||
| Avoid fish | 4.55 | 0.09 | ||
| Avoid eggs | 4.61 | 0.10 | ||
| ICDSa | ||||
| Consuming ICDS Supplementary Nutrition alone | 2.82 | 0.05 | ||
| Consuming ICDS Supplementary Nutrition completely | 2.49 | 0.10 | ||
| Antenatal Care | ||||
| Consistent IFA/FA consumed (every day in last month's trimester) | 0.29 | <0.001 | 0.258 | 0.001 |
| Never Received IFA tablets | 1.64 | 0.06 | ||
| ANC Check-up in 3rd Trimester | 0.89 | 0.04 | ||
| Mobile Registration for ANC- Registered vs Not registered | 4.17 | 0.01 | ||
| WASH | ||||
| General use of soap | 0.19 | 0.05 | ||
| Brushing teeth at least once a day | 0.35 | 0.06 | ||
| Health seeking behaviour index | 0.86 | 0.07 | ||
| Household Characteristics | ||||
| Altitude | 0.99 | 0.07 | ||
| Total Household Members | 0.91 | 0.05 | ||
| Number of women in household | 0.70 | 0.04 | 0.724 | 0.079 |
| Relationship to head of household | 6.01 | 0.06 | ||
| Non-Hindu religion | 6.13 | 0.05 | ||
| Wealth Index | 0.88 | 0.02 | ||
| Wealth Quintile | 0.83 | <0.001 | ||
| NREGA beneficiary | 2.42 | 0.05 | ||
| Expected number of pregnant women in village | 0.994 | 0.575 | ||
aICDS- Integrated Child Development Services scheme. Odds ratio from survey weighted logistic regression analysis. Adjusted odds ratio after including all variables listed in the table.
Factors associated with IFA consumption in pregnant women
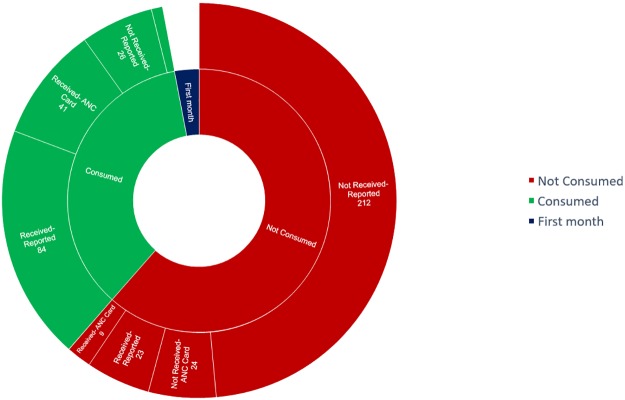
Since consistent consumption of iron and folic acid or folic acid tablets is associated with anaemia, the timely receipt of IFA supplements by pregnant women in Sirohi is critical and is examined in Fig 2. Among those who did not receive IFA, ‘no provision’ from the health worker was the most common reason. Among those who received supplements and did not consume them, low palatability, unrealized need, constipation and forgetfulness were the major reasons.
Fig 2. Reporting of consumption and receipt of iron and folic acid supplements.
Values are number of subjects.
ANC registration was significantly associated with consumption of IFA or folic acid supplements by pregnant women in the previous month’s trimester (χ2 = 69.7, p<0.01, N = 423). Majority of those who did not consume did not receive IFA (88%). Table 4 provides a summary of ANC registration, IFA supplementation status and health worker visit. There was no association between health worker visit and receiving IFA (χ 2 = 2.8, p>0.05, N = 326) in Trimester 2 and 3. A health worker was more likely to visit those pregnant women who were registered under ANC (χ 2 = 29.7, p<0.01, N = 436).
Table 4. Antenatal care registration and health worker visits in surveyed population (N = 436).
| Health worker visits regularly | Health worker does not visit | |
|---|---|---|
| ANC Registered | 135 | 168 |
| Did not receive IFA (Trimester 1*) | 19 (14%) | 20 (12%) |
| Received IFA (Trimester 2 and 3) | 24 (18%) | 23 (14%) |
| Did not receive IFA (Trimester 2 and 3) | 92 (68%) | 125 (74%) |
| ANC Not Registered | 23 | 110 |
| Did not receive IFA (Trimester 1*) | 12 (52%) | 59 (54%) |
| Received IFA (Trimester 2 and 3) | 0 (0%) | 0 (0%) |
| Did not receive IFA (Trimester 2 and 3) | 11 (48%) | 51 (46%) |
*Eligible for folic acid; IFA- Iron and Folic Acid
Availability of IFA to pregnant women
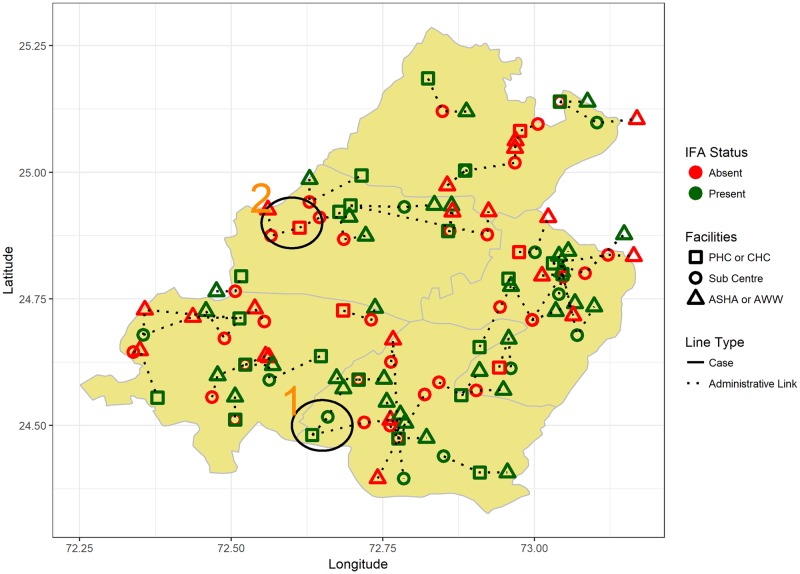
Fourteen of 52 surveyed villages in Sirohi did not have access to an IFA tablet except at the CHC or District Hospital level. Nineteen villages had access at the ASHA or Anganwadi level, while 9 and 10 villages had access at the sub-centre and PHC level respectively. Distance between two geographic locations, also known as the geodesic, was calculated as the shortest distance between two points on an ellipsoid, namely WGS84 [29]. Reported distance to each type of facility, per information from the village representative, was also recorded.
There are 4 villages which had IFA availability only at the District Hospital level (as per referral structure) which was 31.5 km (median reported distance) from the villages. On the other end, among the remaining villages 17 had IFA tablet available with either the ASHA or Anganwadi worker within the village at geodesic distance 0.6 km [IQR: 0,5.5], while the reported median distance was 0 km [IQR: 0, 7.2]. Excluding the farthest and nearest availability of IFA, for the remaining villages the nearest tablet was at geodesic distance of 3.6 km [IQR: 1.2, 8.5] while the reported distance was 5 km [IQR: 0.5, 10]. For 15 villages, the nearest IFA tablets were more than 5 km away (geodesic) from the source. Fig 3 represents the location of different facilities, administrative relationships between the facilities and the status of their IFA stock spatially. Table 5 contains information on health facilities with IFA supplements and their proximity to villages.
Fig 3. Geographical distribution of health facilities, inter-facility relationships and availability of IFA supplementation.
The polygon was filtered from the shape file and modified using ggplot2 package (https://cran.r-project.org/web/packages/ggplot2/index.html) in R.
Table 5. Distance from different levels of public health facilities where IFA is available to surveyed villages.
| IFA Available with | N | Geodesic distance (km) | Reported distance (km) |
|---|---|---|---|
| Asha | 10 | 0 (Within village) | 0 (Within village) |
| Anganwadi | 7 | 0 (Within village) | 0 (Within village) |
| Sub Centre | 8 | 1.06 (IQR: 0.5 to 2.5) | 0.5 (IQR: 0 to 3.5) |
| PHC | 10 | 7.9 (IQR: 4.4 to 8.9) | 10 (IQR: 7.3 to 11.8) |
| CHC | 9 | 2.2 (IQR: 1.2 to 8.7) | 2.5 (IQR: 0 to 10) |
| District Hospital | 4 | 22.6 (IQR: 16.2 to 24.3) | 31.5 (IQR: 22.25 to 38.75) |
IQR: Inter Quartile Range
Fig 3 provides administrative linkages between different health facilities and the status of their IFA stocks. We randomly shifted the location of the village to North, South, East or West by 5km for confidentiality purposes. “1” refers to an ideal case where all facilities from village level onwards have IFA stocks. “2” refers to a non-ideal case where none of the facilities, except at the district level have IFA stocks. Approximately 50% of villages do not have IFA stocks below or at Sub-Centre level.
Both geodesic (r = -0.21, p = 0.15) and reported distance (r = -0.18, p = 0.23) to the health facility with IFA supplements were negatively (but not significantly) correlated with the proportion of women receiving IFA supplementation in the village.
Discussion
The burden of anaemia was high at 66% in pregnant women of Sirohi district and consistent consumption of IFA/folic acid supplements during the previous trimester of pregnancy was the single most strongly inversely associated factor for anaemia. In addition low mobile usage, low number of women in household, use of tobacco and paan, late month of pregnancy increased the odds of anaemia. Of these, mobile usage (possibly a proxy for latent unmeasured variables such as woman’s empowerment and access to information in addition to woman’s economic status), substance use and IFA/folic acid intake are factors amenable to intervention.
Poor consumption of IFA supplements is a key risk factor contributing to anaemia among pregnant women in Sirohi. Though anaemia is a complex and multi-faceted problem which involves interaction of various nutrients, iron supplementation could alleviate a considerable proportion [30] of anaemia in India. As observed in Sirohi, a low intake of IFA supplements resulting from a combined effect of low stocks and poor demand drives anaemia among pregnant women. There was no significant difference of IFA receipt between women those who were visited by a health worker and those who were not. A possible explanation for this could be low stocks of IFA with frontline workers and IFA supply only from centralized locations such as Sub-centres or Anganwadi centres and not at homes. It could also mean that the health worker responsible for distributing IFA tablets was not the one who visited pregnant women at their homes. However, other studies have shown that antenatal care utilization can be improved from health worker visits [31]. The present study also shows that health worker visits are more likely for those women who are registered for antenatal care.
It is important to note that more than one-fourth of the villages surveyed did not have access to IFA supplements within a 5 km radius. As per Fig 2, most women did not consume IFA supplements not because of perceived side-effects but because they were not provided the same. NFHS-4 reports only 25.9% of pregnant women in rural areas consume 100 IFA tablets during pregnancy. Other studies in South Asia have reported that geographic proximity to health service is important in its utilization, especially for antenatal care, chronic diseases and infectious diseases [22,23]. To ensure stocks are in place in all health facilities, the local government could re-evaluate the supply chain management information system in place as well as provide for other measures such as buffer stocks and pharmacy budgets for health facilities. If so, health workers could plan the effective generation of demand in the community. For this, at least two actions are required; that the supply of IFA should be proactive and constant at the village level or the sub-centre, and that the distance to the nearest tablet should be at least at the Sub Centre level if not at the village level ensuring that visiting health workers (ANMs, ASHAs) have stock and would be able to supply pregnant women with IFA tablets.
Anaemia as a result of use of substances such as paan (betel leaf and/or betel nut) or tobacco is well-known [32,33]. Almost 40 (9%) pregnant women consumed paan masala or chewable tobacco on a routine basis. Smokeless tobacco [32] during pregnancy is observed to decrease haemoglobin levels, similar to cigarette smoking. In addition to reducing maternal red blood cell count, the habit can also lead to decreased serum Vitamin B12 and maternal red blood cell folate. The increasing odds of anaemia with month of pregnancy is a well-known phenomenon, often referred to as the physiological anaemia of pregnancy [34].
This analysis is not without limitations. Firstly, we surveyed only 52 PSUs (villages and wards) of which, reported distance to health facilities were available only for 48. However, the PSUs were sampled based on a probability proportional to size (PPS) design and ought to be representative of the district. Secondly, access to different health facilities were not considered when estimating the distance to the nearest IFA supplement. It is possible [35,36] that a health facility is close to a village, but not accessible due to socio-cultural reasons. Thirdly, distance and receipt of IFA supplementation were not significantly associated at a village level. As a result, the optimal location of the health facility for optimal provision of IFA cannot be defined. Fourth, since the road networks in the rural part of the district is poor, geodesic might not convey the true picture of distance. We tried to overcome this limitation by using the reported distance to the health facility as reported by the village representative along with the geodesic. Finally, it is possible that the stock-out of IFA which our team observed (we did not assess folic acid stocks) prevailed only for the duration of the survey period. This limitation is common to all cross-sectional studies.
Conclusion
The prevalence of anaemia among pregnant women in Sirohi was higher than the national prevalence. Anaemia in pregnant women was associated with inconsistent consumption of IFA/FA. IFA not supplied by health worker was identified as demand side factor associated with inconsistent IFA consumption. With more than half the sample of pregnant women not being visited by health worker during pregnancy, it is critical that IFA is available at the nearest health facility. However, it was observed that about 50% of the villages did not have IFA available at the nearest health facility. While anaemia among pregnant Indian women continues to be a priority issue for the government, focussed interventions such as regular haemoglobin testing and ensuring successful implementation of the National Iron Plus Initiative nuanced for the local context and access to IFA can go a long way in meeting anaemia reduction targets in India.
Acknowledgments
The authors would like to acknowledge Divya Mishra, Dr. Nidhi Jaikrishna, Shruthi Cyriac, Sumedha Minocha, Dr. Swetha Rajeswari, Dr. Khushbu Gandhi and Vijay Singh for assisting in field coordination and data pre-processing support. The authors would also like to acknowledge Dr. Prabal V. Singh, Dr. Navin Kumar. Dr. Nayan Kumar and Pooja Singh of Oxford Policy Management Ltd. for assisting in the data collection process.
Data Availability
Data are available from GitHub: https://github.com/jvargh7/how-far-is-the-ifa.
Funding Statement
This work was supported by Tata Trusts (RAPID MCN Study), www.tatatrusts.org.
References
- 1.World Health Organization. The global prevalence of anaemia in 2011. Geneva: World Health Organization; 2015 [Google Scholar]
- 2.Stevens GA, Finucane MM, Paciorek CJ, Flaxman SR, White RA, Donner AJ, et al. Trends in mild, moderate, and severe stunting and underweight, and progress towards MDG 1 in 141 developing countries: A systematic analysis of population representative data. Lancet. 2012;380(9844):824–34. 10.1016/S0140-6736(12)60647-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.International Institute for Population Sciences. National Family Health Survey-4, 2015–16: India Fact Sheet. IIPS; 2017
- 4.Anand T, Rahi M, Sharma P, Ingle GK. Issues in prevention of iron deficiency anemia in India. Nutrition. 2014. July;30(7–8):764–70. 10.1016/j.nut.2013.11.022 [DOI] [PubMed] [Google Scholar]
- 5.Kapil U, Bhadoria AS. National Iron-plus Initiative guidelines for control of iron deficiency anaemia in India, 2013. Natl Med J India. 2014;27(1):27–9. [PubMed] [Google Scholar]
- 6.Al Hasan SM, Hassan M, Saha S, Islam M, Billah M, Islam S. Dietary phytate intake inhibits the bioavailability of iron and calcium in the diets of pregnant women in rural Bangladesh: a cross-sectional study. BMC Nutr. 2016;2(1):24. [Google Scholar]
- 7.Thankachan P, Walczyk T, Muthayya S, Kurpad AV., Hurrell RF. Iron absorption in young Indian women: The interaction of iron status with the influence of tea and ascorbic acid1-3. Am J Clin Nutr. 2008;87(4):881–6. 10.1093/ajcn/87.4.881 [DOI] [PubMed] [Google Scholar]
- 8.Rammohan A, Awofeso N, Robitaille M-C. Addressing Female Iron-Deficiency Anaemia in India: Is Vegetarianism the Major Obstacle? ISRN Public Health. 2012;2012:1–8. [Google Scholar]
- 9.Hunt JR. Biaoavailability of iron, zinc, and other trace minerals from vegetarian diets. Am J Clin Nutr. 2003;78(3 Suppl):633S–639S. 10.1093/ajcn/78.3.633S [DOI] [PubMed] [Google Scholar]
- 10.Thankachan P, Muthayya S, Walczyk T, Kurpad AV., Hurrell RF. An analysis of the etiology of anemia and iron deficiency in young women of low socioeconomic status in Bangalore, India. Food Nutr Bull. 2007;28(3):328–36. 10.1177/156482650702800309 [DOI] [PubMed] [Google Scholar]
- 11.Prendergast AJ, Humphrey JH, Mutasa K, Majo FD, Rukobo S, Govha M, et al. Assessment of environmental enteric dysfunction in the SHINE Trial: Methods and challenges. Clin Infect Dis. 2015;61(October):S726–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mbuya MNN, Humphrey JH. Preventing environmental enteric dysfunction through improved water, sanitation and hygiene: an opportunity for stunting reduction in developing countries. Matern Child Nutr. 2016. May;12(S1):106–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brooker S, Hotez PJ, Bundy DAP. Hookworm-related anaemia among pregnant women: A systematic review. PLoS Negl Trop Dis. 2008;2(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mukherjee MB, Lu CY, Ducrocq R, Gangakhedkar RR, Colah RB, Kadam MD, et al. Effect of alpha-thalassemia on sickle-cell anemia linked to the Arab- Indian haplotype in India. Am J Hematol. 1997;55(2):104–9. [DOI] [PubMed] [Google Scholar]
- 15.Mariani R, Trombini P, Pozzi M, Piperno A. Iron metabolism in thalassemia and sickle cell disease. Mediterr J Hematol Infect Dis. 2009; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seck BC, Jackson RT. Determinants of compliance with iron supplementation among pregnant women in Senegal. Public Health Nutr. 2008;11(6):596–605. [DOI] [PubMed] [Google Scholar]
- 17.Mithra P, Unnikrishnan B, Rekha T, Nithin K, Mohan K, Kulkarni V, et al. Compliance with iron-folic acid (IFA) therapy among pregnant women in an urban area of south India. Afr Health Sci. 2013;13(4):880–5. 10.4314/ahs.v13i4.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pappagallo S, Bull DL. Operational problems of an iron supplementation programme for pregnant women: An assessment of UNRWA experience. Bull World Health Organ. 1996;74(1):25–33. [PMC free article] [PubMed] [Google Scholar]
- 19.Schultink W. Iron-supplementation programmes: Compliance of target groups and frequency of tablet intake. Food Nutr Bull. 1996;17(1). [Google Scholar]
- 20.Galloway R, McGuire J. Determinants of compliance with iron supplementation: Supplies, side effects, or psychology? Soc Sci Med. 1994;39(3):381–90. [DOI] [PubMed] [Google Scholar]
- 21.Stuart Gillespie JK and JM. Controlling Iron Deficiency − Nutrition policy discussion paper No. 9. Nutr policy Discuss Pap No 9. 1991;(9):7, 21.
- 22.Musoke D, Boynton P, Butler C, Musoke MB. Health seeking behaviour and challenges in utilising health facilities in Wakiso district, Uganda. Afr Health Sci. 2014;14(4):1046–55. 10.4314/ahs.v14i4.36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shaikh BT, Hatcher J. Health seeking behaviour and health service utilization in Pakistan: Challenging the policy makers. J Public Health (Bangkok). 2005;27(1):49–54. [DOI] [PubMed] [Google Scholar]
- 24.Puthuchira Ravi R, Athimulam Kulasekaran R. Care Seeking Behaviour and Barriers to Accessing Services for Sexual Health Problems among Women in Rural Areas of Tamilnadu State in India. J Sex Transm Dis. 2014;2014:292157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Government of India O of the RG& CC. Census of India 2011 Meta Data. 2011.
- 26.Mejía-Guevara I, Krishna A, Corsi DJ, Subramanian S V. Individual and Ecological Variation in Child Undernutrition in India: A Multilevel Analysis. J South Asian Dev. 2015;10(2):168–98. [Google Scholar]
- 27.World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System, Geneva, World Health Organization, 2011 (WHO/NMH/NHD/MNM/11.1) 2011.
- 28.Lumley T. survey: analysis of complex survey samples. R package version 3.32–1. 2017;
- 29.National Imagery and Mapping Agency G and GD. Department of Defense World Geodetic System 1984-Technical Report. 2000.
- 30.Petry N, Olofin I, Hurrell R, Boy E, Wirth J, Moursi M, et al. The Proportion of Anemia Associated with Iron Deficiency in Low, Medium, and High Human Development Index Countries: A Systematic Analysis of National Surveys. Nutrients. 2016. November;8(11):693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Navaneetham K, Dharmalingam A. Utilization of maternal health care services in southern India. Soc Sci Med. 2002;55(10):1849–69. [DOI] [PubMed] [Google Scholar]
- 32.Subramoney S, Gupta P. Anemia in pregnant women who use smokeless tobacco. Nicotine Tob Res. 2008;10(5):917–20. 10.1080/14622200802027206 [DOI] [PubMed] [Google Scholar]
- 33.Nordenberg D, Yip R, Binkin NJ. The effect of cigarette smoking on hemoglobin levels and anemia screening. JAMA. 1990;264(12):1556–9. [PubMed] [Google Scholar]
- 34.Costantine MM. Physiologic and pharmacokinetic changes in pregnancy. Front Pharmacol. 2014; April 5(April):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sen G, Östlin P. Gender inequity in health: Why it exists and how we can change it. Glob Public Health. 2008;3(SUPPL. 1):1–12. [DOI] [PubMed] [Google Scholar]
- 36.Baru R, Acharya A, Acharya S, Kumar AS, Nagaraj K. Inequities in Access to Health Services in India: Caste, Class and Region. Econ Polit Wkly. 2010;45(38):49–58. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from GitHub: https://github.com/jvargh7/how-far-is-the-ifa.