Abstract
Background
This is the second update of a Cochrane Review originally published in 2009. Millions of workers worldwide are exposed to noise levels that increase their risk of hearing disorders. There is uncertainty about the effectiveness of hearing loss prevention interventions.
Objectives
To assess the effectiveness of non‐pharmaceutical interventions for preventing occupational noise exposure or occupational hearing loss compared to no intervention or alternative interventions.
Search methods
We searched the CENTRAL; PubMed; Embase; CINAHL; Web of Science; BIOSIS Previews; Cambridge Scientific Abstracts; and OSH UPDATE to 3 October 2016.
Selection criteria
We included randomised controlled trials (RCT), controlled before‐after studies (CBA) and interrupted time‐series (ITS) of non‐clinical interventions under field conditions among workers to prevent or reduce noise exposure and hearing loss. We also collected uncontrolled case studies of engineering controls about the effect on noise exposure.
Data collection and analysis
Two authors independently assessed study eligibility and risk of bias and extracted data. We categorised interventions as engineering controls, administrative controls, personal hearing protection devices, and hearing surveillance.
Main results
We included 29 studies. One study evaluated legislation to reduce noise exposure in a 12‐year time‐series analysis but there were no controlled studies on engineering controls for noise exposure. Eleven studies with 3725 participants evaluated effects of personal hearing protection devices and 17 studies with 84,028 participants evaluated effects of hearing loss prevention programmes (HLPPs).
Effects on noise exposure
Engineering interventions following legislation
One ITS study found that new legislation in the mining industry reduced the median personal noise exposure dose in underground coal mining by 27.7 percentage points (95% confidence interval (CI) −36.1 to −19.3 percentage points) immediately after the implementation of stricter legislation. This roughly translates to a 4.5 dB(A) decrease in noise level. The intervention was associated with a favourable but statistically non‐significant downward trend in time of the noise dose of −2.1 percentage points per year (95% CI −4.9 to 0.7, 4 year follow‐up, very low‐quality evidence).
Engineering intervention case studies
We found 12 studies that described 107 uncontrolled case studies of immediate reductions in noise levels of machinery ranging from 11.1 to 19.7 dB(A) as a result of purchasing new equipment, segregating noise sources or installing panels or curtains around sources. However, the studies lacked long‐term follow‐up and dose measurements of workers, and we did not use these studies for our conclusions.
Hearing protection devices
In general hearing protection devices reduced noise exposure on average by about 20 dB(A) in one RCT and three CBAs (57 participants, low‐quality evidence). Two RCTs showed that, with instructions for insertion, the attenuation of noise by earplugs was 8.59 dB better (95% CI 6.92 dB to 10.25 dB) compared to no instruction (2 RCTs, 140 participants, moderate‐quality evidence).
Administrative controls: information and noise exposure feedback
On‐site training sessions did not have an effect on personal noise‐exposure levels compared to information only in one cluster‐RCT after four months' follow‐up (mean difference (MD) 0.14 dB; 95% CI −2.66 to 2.38). Another arm of the same study found that personal noise exposure information had no effect on noise levels (MD 0.30 dB(A), 95% CI −2.31 to 2.91) compared to no such information (176 participants, low‐quality evidence).
Effects on hearing loss
Hearing protection devices
In two studies the authors compared the effect of different devices on temporary threshold shifts at short‐term follow‐up but reported insufficient data for analysis. In two CBA studies the authors found no difference in hearing loss from noise exposure above 89 dB(A) between muffs and earplugs at long‐term follow‐up (OR 0.8, 95% CI 0.63 to 1.03 ), very low‐quality evidence). Authors of another CBA study found that wearing hearing protection more often resulted in less hearing loss at very long‐term follow‐up (very low‐quality evidence).
Combination of interventions: hearing loss prevention programmes
One cluster‐RCT found no difference in hearing loss at three‐ or 16‐year follow‐up between an intensive HLPP for agricultural students and audiometry only. One CBA study found no reduction of the rate of hearing loss (MD −0.82 dB per year (95% CI −1.86 to 0.22) for a HLPP that provided regular personal noise exposure information compared to a programme without this information.
There was very‐low‐quality evidence in four very long‐term studies, that better use of hearing protection devices as part of a HLPP decreased the risk of hearing loss compared to less well used hearing protection in HLPPs (OR 0.40, 95% CI 0.23 to 0.69). Other aspects of the HLPP such as training and education of workers or engineering controls did not show a similar effect.
In three long‐term CBA studies, workers in a HLPP had a statistically non‐significant 1.8 dB (95% CI −0.6 to 4.2) greater hearing loss at 4 kHz than non‐exposed workers and the confidence interval includes the 4.2 dB which is the level of hearing loss resulting from 5 years of exposure to 85 dB(A). In addition, of three other CBA studies that could not be included in the meta‐analysis, two showed an increased risk of hearing loss in spite of the protection of a HLPP compared to non‐exposed workers and one CBA did not.
Authors' conclusions
There is very low‐quality evidence that implementation of stricter legislation can reduce noise levels in workplaces. Controlled studies of other engineering control interventions in the field have not been conducted. There is moderate‐quality evidence that training of proper insertion of earplugs significantly reduces noise exposure at short‐term follow‐up but long‐term follow‐up is still needed.
There is very low‐quality evidence that the better use of hearing protection devices as part of HLPPs reduces the risk of hearing loss, whereas for other programme components of HLPPs we did not find such an effect. The absence of conclusive evidence should not be interpreted as evidence of lack of effectiveness. Rather, it means that further research is very likely to have an important impact.
Plain language summary
Interventions to prevent hearing loss caused by noise at work
What is the aim of this review?
The aim of this Cochrane Review was to find out if hearing loss caused by noise at work can be prevented. Cochrane researchers collected and analysed all relevant studies to answer this question. They found 29 studies that studied the effect of preventive measures.
Key messages
Stricter legislation might reduce noise levels. At the personal level, earmuffs and earplugs can reduce noise exposure to safe levels. However, instruction on how to put plugs into the ears is needed. Without instruction earplugs probably do not protect enough. Providing feedback to workers on noise exposure probably does not decrease noise. Engineering solutions such as better maintenance might lead to similar noise reduction as hearing protection. Better evaluation of these engineering solutions is needed.
The effects of hearing loss prevention programmes (HLPP) are unclear. Better use of hearing protection as part of a programme probably helps but does not fully protect against hearing loss. Improved implementation might provide better protection.
What was studied in the review?
Millions of workers are exposed to noise that can lead to hearing loss. The review authors were interested in the effect of any intervention to reduce noise or hearing loss at workplaces, such as engineering solutions, hearing protection or hearing loss prevention programmes.
What are the results of the review?
Effects on noise exposure
Engineering solutions
We found one study that showed that noise levels decreased by about 5 decibels (dB) after the implementation of stricter legislation in the mining industry. Even though many case studies show that technical improvements can reduce noise levels at workplaces by as much as 20 dB, there were no controlled studies outside the laboratory that would show this with more confidence.
Hearing protection
In eight studies with 358 workers, hearing protection reduced noise exposure of workers by about 20 dB(A). However, for earplugs there was moderate‐quality evidence in two randomised studies that if workers lack proper instructions in the use of earplugs, the attenuation offered is reduced by on average 9 dB.
Feedback on noise exposure
Providing feedback on noise exposure did not change noise levels in the construction industry in one study.
Effects on hearing loss
We found 16 studies with 81,220 participants on the long‐term effects of hearing protection on hearing loss.
Hearing protection
The use of hearing protection devices in a well‐implemented HLPP was associated with less hearing loss. For other elements of programmes such as worker training, audiometry alone, noise monitoring, or providing feedback on personal noise exposure, there was no clear effect. Two studies with 3242 workers found that there was no difference in the long‐term effect of earmuffs versus earplugs on hearing loss.
Hearing loss prevention programmes
Four studies provided very low‐quality evidence that, compared to non‐exposed workers, average HLPPs do not reduce the risk of hearing loss to below a level at least equivalent to that of workers who are exposed to 85 dB(A). Two comparable additional studies showed that the risk of hearing loss is still substantial despite being covered by a HLPP. However, one low‐quality study showed that a stricter HLPP can protect workers from hearing loss.
The absence of conclusive evidence should not be interpreted as evidence of lack of effectiveness. Rather, it means that further research is very likely to affect the conclusions we reached. Higher‐quality prevention programmes, better quality of studies, especially in the field of engineering controls, and better implementation of legislation are needed to prevent noise‐induced hearing loss.
How up to date is this review?
The review authors searched for studies that had been published up to October 2016
Summary of findings
Summary of findings for the main comparison. Stricter legislation for noise exposure.
| Stricter legislation compared with existing legislation for noise exposure | |||||
|
Patient or population: workers with noise exposure Settings: coal mines Intervention: stricter legislation Comparison: existing legislation | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | No of observations (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | ||||
| Existing legislation | Stricter legislation | ||||
|
Immediate change in level in year 2000 (noise level at work as PEL dose in dB(A); range 0 to 6400, log scale) 1 year |
The mean noise levels during pre‐intervention years were 56.9 PEL dose | The mean noise exposure level after introduction was 27.70 PEL dose lower (36.1 lower to 19.3 lower PEL dose) | 14 years pre‐intervention and 4 years post‐intervention (1 ITS) |
⊕⊝⊝⊝ very low1 | The reduction of 27.7 PEL dose translates to about 4.5 dB(A) |
|
Change in slope after introduction (noise level at work as PEL dose in dB(A); range 0 to 6400, log scale) 4 years |
The mean noise levels during pre‐intervention years were 56.9 PEL dose | The mean change in level of noise exposure per year after introduction was 2.10 PEL dose lower (4.90 lower to 0.70 PEL dose higher) | 14 years pre‐intervention and 4 years post‐intervention (1 ITS) |
⊕⊝⊝⊝ very low1 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the absolute effect of the intervention (and its 95% CI). CI: Confidence interval; PEL: permissible exposure level | |||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | |||||
1We downgraded by one level from low to very low because there is only one study and it has a high risk of bias.
Summary of findings 2. Earplugs with instruction versus without instruction (noise exposure).
| Earplugs with instruction compared with no instruction for noise reduction | |||||
|
Patient or population: workers with exposure to noise Settings: industrial Intervention: instruction on how to insert earplugs Comparison: no instruction | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | ||||
| Without instruction | With instruction | ||||
|
Mean noise attenuation over 0.5, 1, 2, 3, 4, 6, 8 kHz (dB) Immediate follow‐up |
The mean noise attenuation ranged across frequencies from 5.5 to 25.9 dB | The mean noise attenuation in the intervention groups was 8.59 dB higher (6.92 dB higher to 10.25 dB higher) | 140 participants (2 RCTs) | ⊕⊕⊕⊝ moderate1 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval | |||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | |||||
1We downgraded from high quality by one level because of imprecision due to small number of participants.
Summary of findings 3. Training plus exposure information compared to training (noise exposure).
| Exposure information compared with training as usual for noise exposure | |||||
|
Patient or population: workers exposed to noise Settings: construction industry Intervention: provision of noise level indicator Comparison: safety training as usual | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | ||||
| Training as usual | Plus noise level indicator | ||||
| Change in noise levels at 4 months' follow‐up (dB(A)) | The mean noise level in the control group ranged from 87.1 to 89 dB(A) | The mean noise level in the intervention groups was 0.3 dB(A) higher (2.31 dB(A) lower to 2.91 dB(A) higher | 176 (1 study, RCT) | ⊕⊕⊝⊝ low1 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval | |||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | |||||
1We downgraded by two levels from high to low because of high risk of bias and imprecision.
Summary of findings 4. Earmuffs versus earplugs (hearing loss).
| Earmuffs compared with earplugs for noise‐induced hearing loss | ||||||
|
Patient or population: workers exposed to 88‐94 dB(A) Settings: shipyard Intervention: most wearing earmuffs Comparison: most wearing earplugs | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Earplugs | Earmuffs | |||||
|
Hearing loss change over 3 years (4 kHz/STS) 2 to 3 years' follow‐up |
High risk population | OR 0.8 (0.63 to 1.03 ) | 3242 (2 CBA studies) | ⊕⊝⊝⊝ very low1 | At lower exposures the results were too heterogeneous to be combined | |
| 42 per 1000 | 34 per 1000 (26 to 43) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds Ratio; STS: standard threshold shift | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
1We downgraded from low quality to very low quality because of high risk of bias in both studies.
Summary of findings 5. Hearing loss prevention programme compared to audiometric testing (hearing loss).
| Hearing loss prevention programme (HLPP) compared to audiometric testing | ||||||
|
Patient or population: agricultural students without hearing loss Settings: agricultural schools Intervention: HLPP with information Comparison: audiometric testing only | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Audiometric testing only | HLPP with information | |||||
| Hearing loss STS ≥ 10 dB loss average over 2, 3, 4 kHz in either ear Follow‐up: mean three years | 21 per 1000 | 18 per 1000 (6 to 49) | OR 0.85 (0.29 to 2.44) | 687 (1 study, RCT) | ⊕⊕⊕⊝ moderate1 | |
| Hearing loss STS ≥ 10 dB hearing loss average over 2, 3, 4 kHz in either ear Follow‐up: mean 16 years | 149 per 1000 | 141 per 1000 (74 to 250) | OR 0.94 (0.46 to 1.91) | 355 (1 study, RCT) | ⊕⊕⊕⊝ moderate1 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; HLPP; hearing loss prevention programme; OR: Odds ratio; STS: standard threshold shift | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
1We downgraded one level from high to moderate due to lack of information on randomisation and allocation concealment.
Summary of findings 6. Hearing loss prevention programme (HLPP) with exposure information compared to HLPP without exposure information (hearing loss).
| HLPP with exposure information compared with HLPP without exposure information for noise‐induced hearing loss | |||||
|
Patient or population: workers exposed to noise Settings: aluminium smelter Intervention: exposure information as part of HLPP Comparison: no such information | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | ||||
| Without exposure info | With exposure info | ||||
|
Annual increase in hearing threshold (dB/year at 2,3 and 4 kHz) 4‐year follow‐up |
The mean hearing loss rate in the control group was 1.0 dB per year | The mean hearing loss rate in the intervention groups was 0.82 dB/year lower (1.86 lower to 0.22 higher) | 312 (1 CBA study) | ⊕⊝⊝⊝ very low1 | Matched for age, gender, baseline hearing loss and baseline hearing |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; HLPP: hearing loss prevention programme | |||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | |||||
1We downgraded by one level from low to very low because of high risk of bias.
Summary of findings 7. Well‐implemented hearing loss prevention programme (HLPP) compared to less well‐implemented HLPP (hearing loss).
| Well‐implemented hearing loss prevention programme (HLPP) compared to less well‐implemented HLPP for hearing loss | ||||||
| Patient or population: workers Settings: exposure to noise Intervention: well‐implemented HLPP Comparison: less well‐implemented HLPP | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Less well‐implemented HLPP | Well‐implemented HLPP | |||||
| Hearing loss STS > 10 dB change average over 2, 3 and 4 kHz1 Follow‐up: mean 9.3 years | 86 per 1000 | 36 per 1000 (21 to 61)2 | OR 0.40 (0.23 to 0.69)3 | 16,301 (3 studies4) | ⊕⊝⊝⊝ very low5 | SMD 0.26 (0.14 to 0.47) |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; HLPP: hearing loss prevention programme; OR: Odds ratio; STS: standard threshold shift | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
1STS used in two studies, change of mean 4 kHz threshold in one study. 2Number of events based on median event rate in included studies. 3Result from the meta‐analysis of three studies. 4One extra study provided similar evidence but could not be combined in the meta‐analysis. 5We downgraded by one level from low to very low because of risk of bias due to lack of adjustment for age and hearing loss.
Summary of findings 8. Hearing loss prevention programme (HLPP) compared to non‐exposed workers (hearing loss).
| Hearing loss prevention programme (HLPP) compared to non‐exposed workers | ||||||
| Patient or population: workers Settings: exposure to noise Intervention: HLPP Comparison: non‐exposed workers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Non‐exposed workers | HLPP | |||||
| Hearing loss Change in hearing threshold at 4 kHz in dB Follow‐up: mean five years | The mean hearing loss in the control groups was 3.6 dB at 4 kHz1 | The mean hearing loss in the intervention groups was 1.8 dB higher (0.6 lower to 4.2 higher) | 1846 (3 studies2) | ⊕⊝⊝⊝ very low3,4 | pooled effect size 0.17 (95% CI ‐0.06 to 0.40) recalculated into dBs | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; HLPP: hearing loss prevention programme; SMD: standardised mean difference | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
1Assumed increase of hearing threshold: median of three studies with respectively 3.4, 3.6 and 5.2 dB increase in hearing threshold at 4 kHz after five years' follow‐up. 2Results from three of five studies included in sensitivity analysis because one study was at serious risk of bias and one other study showed that in spite of hearing protection workers were still more at risk than non‐exposed workers. 3We downgraded by one level from low to very low because three studies did not adjust for age and hearing loss at baseline. 4We would have downgraded by one more level because the confidence interval does not exclude a risk of hearing loss similar to exposure to 85 dB(A) but we had already reached a rating of very low quality evidence.
Background
Description of the condition
Noise is a prevalent exposure in many workplaces. Approximately nine million workers in the USA alone are exposed to time‐weighted average (TWA) sound levels of 85 dB(A) and above (WHO 2002). The first signs of noise‐induced hearing loss (NIHL) can be detected in the typical 4 kHz 'notch' observed on audiograms (Nelson 2005). Worldwide, 16% of disabling hearing loss in adults is attributed to occupational noise. Leigh 1999 calculated a global annual incidence of NIHL of 1,628,000 cases, which means an annual incidence rate of almost two new cases per 1000 older workers. Noise‐induced hearing loss is the second most common self‐reported occupational illness or injury, despite decades of study, workplace interventions, and regulations (Nelson 2005). Information is also available for self‐reported hearing difficulty and tinnitus among workers and non‐workers (Masterson 2016a), incidence and prevalence data from audiometric data sets (Masterson 2015), and disability‐adjusted life years (Masterson 2016b). Self‐reported rates of hearing difficulty and tinnitus were higher among noise‐exposed workers when compared to non‐workers (Masterson 2016a). The mining sector had the highest prevalence of workers with any hearing impairment (hearing loss that impacts day‐to‐day activities), and with moderate or worse impairment, followed by the construction and manufacturing sectors (Masterson 2016b); rates were also high among workers in the healthcare and social assistance sector (Masterson 2015). Two‐and‐a‐half healthy life years were lost each year for every 1000 noise‐exposed US workers because of hearing impairment. Mining, construction and manufacturing workers lost more healthy years than workers in other industry sectors, respectively 3.5, 3.1 and 2.7 healthy years were lost each year for every 1000 workers due to hearing impairment.
Construction workers are still considered as an underserved population where it comes to hearing loss prevention, with one in twenty construction workers estimated to have occupational hearing loss (Suter 2009; Tak 2009). An analysis of the noise exposure on construction sites shows the difficulties for preventive interventions in this industrial sector. Due to the setting and nature of the job, noise exposure varies over time and there are often combined exposures such as chemicals and vibration. Various trades work in the same environment, which also puts quiet trades at risk. Communication and sound localisation are of vital importance for the workers but personal hearing protection devices can degrade those abilities. The use of personal hearing protection also causes other problems such as hygiene problems or occlusion effects (Suter 2002). Interventions to reduce noise at the source such as efficient design, retrofit, and maintenance of equipment or special marks for extra quiet equipment are presented in the literature but these have not been evaluated nor sufficiently implemented (Seixas 2001; Suter 2002; Trabeau 2008). Overall there is a lack of information about noise exposure and hearing ability of construction workers even though methods are available (Haron 2009; Neitzel 2011; Seixas 2001; Suter 2002). One reason is that it is difficult to keep records and organise follow‐up of workers in the construction industry. Mobility among the workers is high, employment periods are often short and seasonal, and self‐employed workers might not even be part of a hearing conservation programme (Suter 2002).
Long‐term exposure to noise levels beyond 80 dB(A) carries an increased risk of hearing loss, which increases with the noise level and can ultimately lead to hearing impairment (ISO 1990). The risk of hearing impairment also increases substantially with age. There are various definitions of hearing impairment in use. The most commonly used definition for hearing impairment is a weighted average hearing loss at 1 kHz, 2 kHz, 3 kHz and 4 kHz greater than 25 dB (John 2012). Such a hearing loss decreases the capacity to engage in conversation in meetings or social activities thus creating a significant barrier in establishing or maintaining emotional relationships. Measured this way, the probability of hearing impairment occurring in persons not exposed to noise at the ages of 35 and 65 is estimated to be 10% and 55% respectively, because it increases naturally with age. Ten years of noise exposure at the level of 100 dB(A) will raise the probability of hearing impairment for the same individuals to 94.5% and 99.5%. Thus, 10 years of noise exposure entails a relative risk of hearing impairment of 9.9 for a 35 year‐old worker and 1.8 for a 65 year‐old worker compared to their non‐exposed peers (Prince 1997). Concurrent exposure to ototoxic substances (that is, damaging to the cochlea or auditory nerve), such as solvents and heavy metals, may increase the damaging potential of noise (EU 2003; Johnson 2010). The condition is permanent and there is no effective treatment for permanent hearing loss resulting from excessive noise exposure. However, the risk of noise‐induced hearing loss can be greatly minimised if noise is reduced to below 80 dB(A) (ISO 1990).
Description of the intervention
The preventive potential of reducing noise exposure has led to mandatory HLPPs in many countries. However, the reportedly continuing high rate of occupational noise‐induced hearing loss casts doubt upon the effectiveness of these standards and workers' compliance with them. Moreover, the broad range of interventions included in HLPPs makes it difficult to appraise the most effective strategy for reducing risk.
How the intervention might work
There is a general belief that it is most effective to apply control measures in a hierarchical order. This means first using measures that eliminate the source of the noise and, at the other end of the spectrum, implementing measures that protect the individual worker only. In occupational hygiene terms this is called the hierarchy of controls (Ellenbecker 1996). Despite the general consensus that this should be the leading principle for noise reduction strategies at the workplace, the first attempt to reduce noise often is limited to the provision of hearing protectors. Also clinical interventions such as the use of magnesium or anti‐oxidants such as N‐acetylcysteine for preventing noise‐induced hearing loss have been studied (Le Prell 2012; Lynch 2005). These will not be included in this review.
Why it is important to do this review
A more general and non‐systematic review on the effectiveness of hearing conservation programmes concluded in 1995 that there was no convincing evidence that HLPPs are effective (Dobie 1995). A systematic review of studies that have evaluated interventions to reduce occupational exposure to noise or to decrease occupationally‐induced hearing loss is therefore warranted. This is the second update of a Cochrane Review originally published in 2009.
Objectives
To assess the effectiveness of non‐pharmaceutical interventions for preventing occupational noise exposure and occupational hearing loss compared to no or alternative interventions.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCT), cluster‐randomised trials, controlled before‐after studies (CBA) and interrupted time‐series (ITS).
Evaluations of hearing loss prevention interventions can be biased by factors that also cause hearing loss other than noise, such as ageing or exposure to ototoxic substances (Kirchner 2012). Randomisation is the best protection against such bias. However, noise reduction is an intervention that is almost never carried out only at the individual level. Noise reduction in enterprises usually entails replacing noisy machinery or shielding off noisy machinery or tools. Cluster‐randomisation, in which whole companies or departments are randomly assigned to the intervention and control group, is a way to replace randomisation at the individual level and is a relatively new trial design.
As randomisation is difficult to perform for the interventions of interest in this review, we therefore also included CBA studies. There is no uniform nomenclature for non‐randomised studies. In the literature CBA studies are also known as cohort studies, quasi‐experimental studies, non‐randomised pre‐post‐intervention or controlled clinical trials. For studies that measured an immediate effect of hearing protection it was difficult to assess what the control group should be. We included only studies that measured an immediate effect of two types of hearing protectors if this was measured in the same study participants. For studies that measured hearing loss in the long‐term we excluded those that did not collect data on a proper control group but used only data from available databases.
In addition, hearing loss is often registered in medical databases. These can form a reliable source in which changes can be observed in trends over time as a result of interventions. These type of data are also called ITS. Cochrane Effective Practice and Organisation of Care (EPOC) has defined these as studies in which the outcome has been measured at least three times before and three times after the intervention (EPOC 2012; Ramsay 2003).
We also included uncontrolled before‐and‐after studies that evaluated the effectiveness of engineering controls in reducing noise levels to compare studies and review results in the discussion part of this review. We only included studies if they compared noise readings in the same location during similar work operations before and after engineering controls were implemented.
For the effect of hearing protection devices on noise attenuation, we only included studies that compared different devices worn by the same workers in real work conditions. This is because hearing attenuation depends both on the skills of the worker to fit a device and the properties of the device itself. A comparison between devices worn by different groups of workers would be a comparison between skills of workers and the attenuation of devices at the same time and the effects would be impossible to disentangle.
For the effect of training workers in the fitting of hearing protection devices on noise attenuation, we included studies with a comparison group including different workers but for the same device.
We excluded laboratory studies because it has been repeatedly reported that the results in the laboratory are often overly positive due to the lack of real‐world conditions, such as change of working tasks, differences in training in the fitting of devices, and wearing of glasses.
Types of participants
We included studies with male and female workers at workplaces exposed to noise levels of more than 80 dB(A) as a TWA over a period of an entire work shift or working day or part of the work shift.
Types of interventions
We included studies where the interventions intended to prevent noise‐induced hearing loss, or which formed part of a noise‐induced hearing loss prevention programme (HLPP). We included interventions consisting of one or more of the following elements.
Engineering controls: reducing or eliminating the source of the noise, changing materials, processes or workplace layout (NIOSH 1997)
Administrative controls: changing work practices, management policies or worker behaviour (NIOSH 1997)
Personal hearing protection devices (NIOSH 1998)
Hearing surveillance: monitoring the hearing levels of exposed workers (NIOSH 1998)
We excluded all clinical interventions such as the use of anti‐oxidants, magnesium or other compounds.
Types of outcome measures
We included two main outcomes: noise exposure and hearing loss. We included studies that reported the effects of the intervention on either noise exposure or hearing loss. For both outcomes we took the change in the outcome between before and after the implementation of the intervention. We did so because we included mostly non‐randomised studies where workers could already have had hearing loss before the intervention.
We included noise exposure as a primary outcome because the relation between exposure to noise at work and hearing loss has been well established (ISO 1990; Prince 1997). It can be safely assumed that interventions that reduce noise exposure will in turn lead to a decrease in participants with hearing loss. Noise exposure is therefore a good predictor of the eventual health outcome, hearing loss. We also made a distinction between short‐term and long‐term effects. We considered three follow‐up times as important: less than one year, one to five years and more than five years. Short‐term effects were considered if a change in outcome was possible in less than one year. Long‐term effects were considered to occur only after at least one year.
An alternative technique to evaluate immediate or long‐term effects on hearing ability is the measurement of otoacoustic emissions (OAEs). OAEs provide a measurement of outer hair cell integrity with two most prominent types of measurement: transient evoked otoacoustic emissions (TEOAEs), and dual‐tone evoked distortion product otoacoustic emissions (DPOAEs). Both can be used for example to check the attenuation effect of hearing protection devices in real wearing conditions (Bockstael 2008). Nevertheless there is an ongoing discussion in the literature about the use of TEOAEs and DPOAEs as diagnostic tools in occupational health examinations of noise‐exposed workers (EU‐OSHA 2009; Helleman 2010). Because of considerable uncertainties regarding the use of OAEs we decided not to use OAE test results as outcome measurements. References of studies qualifying for inclusion but measuring noise‐induced hearing loss only as OAEs were listed as references pending classification. In cases where study results were measured additionally as OAEs the studies were included with the outcome measurements mentioned above.
Noise exposure
We included studies that directly measured the change in noise exposure level either as the difference in noise levels (dB) or the difference in exposure doses (%). We also included noise levels measured as noise attenuation effects from hearing protection devices assessed as the difference in hearing threshold with and without the hearing protection device. We included studies regardless of the frequencies measured (Hz). All outcomes can either be measured as long‐term or short‐term effects, depending on the follow‐up time of the study.
We included studies reporting noise exposure measurements for either a specific area or a specific worker. Measurement instruments could be fixed in one location, attached on a person (e.g. on the collar), or installed in the ear behind the hearing protection device (e.g. microphone in real ear (MIRE)). We included outcome measures of the exposure for one point in time and measures over longer time periods (e.g. average exposure over one working day).
We intended to include all noise outcomes that were measured with a measurement instrument that was calibrated before use. Although we intended to include only measurements executed according to a written national or international standard, in which information on measurement method and measurement settings (e.g. time weighting) was given, this turned out to be an excessively strict criterion. We therefore included all reported noise measurements.
Noise level
We included studies that reported sound pressure levels, either as absolute measures or as averages over time in dB.
TWA noise levels are used to convey a worker's daily exposure to noise (normalised to an eight‐hour day), taking into account the average levels of noise and time spent in each area. Decisions have to be made on which parameters to use in these calculations. The Equivalent Continuous Sound Level ‐ (Leq) is based on the equal energy hypothesis, which states that equal amounts of sound energy produce equal amounts of damage regardless of their distribution over time. Leq calculations are based on an 85 dB limit and an exchange rate of 3 dB. However, in the USA, noise levels are often reported as TWA, or averaged sound level (Lavg) with an exchange rate of 5 dB and threshold level of 90 dB, as these are the levels set by the Occupational Safety and Health Administration (OSHA). This results in one hour of exposure to 90 dB(A) in US studies being equal to half an hour of exposure to 95 dB(A) whereas in European studies this would equal half an hour of 93 dB(A). As a consequence, the US time‐weighted figure would be an underestimate of the same noise levels measured according to the European methodology. Because we had no method to correct for this, we used the outcome measurements as described by the study authors.
Exposure dose
The calculation of a dose is based on the permissible exposure limit. For example a day‐long exposure to 90 dB(A) would lead to a dose of 100% for that day. With each 5 dB increase or decrease the dose would be doubled or halved. However different standards recommend different exposure limits (e.g. 90 dB(A), 85 dB(A) or 80 dB(A)) as well as different exchange rates (e.g. 3 dB, 4 dB, 5 dB) and different threshold levels. As a consequence, the same exposure would be expressed as a smaller dose for the higher exposure limits. We again used the outcome measurements as described by the study authors.
Immediate hearing threshold changes
We included measures of differences between hearing thresholds with and without hearing protection. This method is called real ear attenuation at threshold (REAT) and is equivalent to the noise attenuation effect of the hearing protection device.
Hearing loss
Short‐term effects
We also included measures of temporary threshold shifts (TTS), a temporary decrease in hearing acuity after some hours of exposure. We included studies that used TTS as an effect measure of the noise attenuation of hearing protection devices.
Long‐term effects
We included studies that measured permanent threshold shifts (PTS). Those threshold shifts are non‐reversible and only occur after several years. We also included studies that used standard thresholds shifts (STS), which is a measure of a minimum relevant shift of the PTS by, for example, 15 dB.
We intended to include only hearing loss measured with a calibrated audiometer and defined by means of a written protocol, which was the case for most studies. However, in some cases this was found to be an excessively strict criterion so we also included audiometric measurements when there was no written protocol reported.
Search methods for identification of studies
We conducted systematic searches for RCTs, CBA studies, ITS studies and noise reduction case studies. We used no restrictions on language, publication year or publication status. The date of the last search was 26 September 2016 for Pubmed, Embase, Web of Science and OSHupdate. The database Central and CINAHL were last searched on 3 October 2016.
Electronic searches
We searched:
the Cochrane Central Register of Controlled Trials (CENTRAL, 2008, Issue 4) in the Cochrane Library (until 3 October 2016) (including Cochrane Ear, Nose and Throat Disorders Group's Trials Register and Cochrane Work's Trials Register);
PubMed (until 26 September 2016);
Embase (using Embase) (until 26 September 2016);
CINAHL (until 3 October 2016);
Web of Science (until 26 September 2016);
OSHupdate (until 26 September 2016) (including the databases from the US National Institute of Occupational Safety and Health (NIOSHTIC, NIOSHTIC‐2), International Occupational Safety and Health Information Centre of The International Labour Organisation (CISDOC), International bibliographic, UK Health and Safety executive (HSELINE), Institut de recherche Robert‐Sauvé en santé et en sécurité du travail, Canada (IRRST), Ryerson Technical University Library, Toronto, Canada (RILOSH)
The following databases were included in the original review (2008) but were not included in the update, as we did not locate additional relevant studies:
LILACS;
KoreaMed;
IndMed;
PakMediNet;
CAB Abstracts;
BIOSIS Previews;
mR CT (Current Controlled Trials); and
Google.
We modelled subject strategies for databases on the search strategy designed for CENTRAL. We did not combine subject strategies with a methodological filter because we wanted to identify all occupational health studies, both randomised and non‐randomised (Verbeek 2005).
The search strategy for CENTRAL is shown in Appendix 1.
The search strategies for other key databases including PubMed are shown in Appendix 2.
Searching other resources
We scanned reference lists of identified studies for further papers. We also searched PubMed, TRIPdatabase, NHS Evidence ‐ Ear, Nose, Throat and Audiology (formerly NLH ENT & Audiology Specialist Library) and Google to retrieve existing systematic reviews possibly relevant to this systematic review, so that we could scan their reference lists for additional studies.
We contacted Dr E Berger who keeps an up‐to‐date archive on hearing protector effectiveness and obtained copies from the grey literature studies that he included in his review of real field effectiveness studies of hearing protection. Of the 22 studies in his review we were unable to retrieve two because they were personal communications (Berger 1996).
Data collection and analysis
Selection of studies
To determine which studies to assess further, pairs of the review authors (EK, JV, TM, WD, CM, SF) independently scanned the titles and abstracts of every record retrieved. Full articles were retrieved for further assessment if the information given suggested that the study could meet all of the following criteria:
included workers exposed to noise levels greater than 80 dB(A);
concerned interventions aimed at reduction of noise exposure to prevent noise‐induced hearing loss;
used noise exposure or noise‐induced hearing loss as an outcome; and
used RCT, CBA studies, or ITS as the study design.
Data extraction and management
For each study included, pairs of the review authors (EK, JV, TM, WD, CM, SF) extracted data independently. Where possible, we resolved discrepancies in the results by discussion or we involved a third review author. Studies with unclear information were often over 20 years old and we refrained from trying to contact the authors. We contacted eight authors of recent studies and obtained additional data from three (Davies 2008; Joy 2007; Rabinowitz 2011).
We used a standard form to extract the following information: characteristics of the study (design, methods of randomisation); setting; participants; interventions and outcomes (types of outcome measures, timing of outcomes, adverse events).
Assessment of risk of bias in included studies
We conducted the evaluation of the risk of bias of RCTs and cohort studies included in the review by means of the checklist developed by Downs and Black (Downs 1998). We only used the items on internal validity of the checklist and not those on reporting quality or external validity. We slightly adapted the way answers to the items of the checklist were formulated to make it fit the Cochrane 'Risk of bias' tool (Higgins 2011a) as implemented in Review Manager 5 (RevMan 5) (RevMan 2014) and thus used the judgements high, low or unclear risk of bias instead of using scores 1 or 0 as proposed by the checklist authors.
For non‐randomised studies, for item allocation concealment, we judged all studies to have an unclear risk of bias because this item is not applicable to non‐randomised studies and the effect of unconcealed allocation on the outcome hearing loss and noise is unknown.
We assessed risk of bias due to confounding separately for noise and hearing loss outcomes. We judged studies based on the assessment and adjustment for confounders. If confounders were similar at baseline or confounders were adjusted for adequately in the analysis, we judged studies to be at low risk of bias for confounding. We judged none of the engineering control studies to be at high risk of bias for confounding, as we don't know of factors that have been shown to be significant predictors of noise exposure. For behavioural interventions, we considered age, gender, and hearing loss to be possible confounders of noise exposure outcomes as those participant characteristics could lead to different behaviours (e.g. distance to noisy equipment) and could therefore alter the effect of an intervention. We judged studies adjusting for at least two of those possible confounders to have a low risk of bias and studies not fulfilling that criteria to have an unknown risk of bias. We considered age, hearing levels, recreational noise exposure, ototoxic medication and previous ear infections as possible confounders for studies measuring hearing loss outcomes. We considered age to be the most important confounder and judged studies that did not adjust for age to have a high risk of bias irrespective of adjustment to other factors. We considered age to be similar between intervention and control group as long as the mean age difference was smaller than five years. We judged studies that adjusted for age and at least one additional possible confounder to have a low risk of bias. Studies that did not report sufficient information about baseline differences or necessary statistical adjustments, we judged to have an unknown risk of bias.
Pairs of the review authors independently examined the risk of bias of the studies. We resolved disagreements by discussion. We defined low risk of bias overall as a score of more than 50% on the internal validity scale of the checklist.
For ITS we used the quality criteria as presented by Ramsay 2003.
Measures of treatment effect
The included studies measured noise exposure on a continuous scale in decibels (dB) with A or C weighting. The A weighting takes into account the sensitivity of the human ear to certain frequencies whereas the C weighting is used for peak sound level measurements. The studies calculated the effect of an intervention, either as attenuation of noise level or as change in noise level over time, by subtracting the level after the intervention from the level measured before the intervention. In one study (Joy 2007) the authors used the medians of all noise measurements in a year as the measure of effect in an ITS analysis to show the long‐term effect. We used a PEL of 90 dB(A) as 100% and a 5 dB exchange rate to convert the change in the exposure dose into the change in dB(A).
For immediate effects of noise attenuation, authors used the MIRE to measure the difference in noise levels inside and outside hearing protection (Pääkkönen 1998; Pääkkönen 2001). They also used REAT, which measures hearing thresholds with and without protection (Park 1991b protection). The MIRE and REAT methods yield slightly different results at different frequencies. For studies that reported noise attenuation in dB for each frequency measured we calculated the mean noise attenuation over all measured frequencies. We calculated the mean noise attenuation as the average of the reported means with a standard deviation calculated from the variances, as square root of the average variance (Salmani 2014). We applied the same formula for calculating the mean noise exposure from machinery if studies reported mean noise level measurements separately for multiple machines of the same type (Küpper 2013). Two studies included participants with different times of follow‐up between control and intervention group. We recalculated the effect as RR per 100 person years to adjust for the differences in the length of follow‐up (Muhr 2006; Muhr 2016). We have reported the original study data that we used to recalculate the outcomes in Table 9.
1. Recalculation of study data for review results and meta‐analysis.
| Küpper 2013 (Outcome: Leq 8 h (dB)a) ‐ noise exposure of rescue helicopter personnel ‐ case study | ||||||||||
| Study data | Recalculation ‐ group mean, SD | |||||||||
| Helicopter type | Helicopter name | mean | SD | dB min | dB max | variance | mean | SD | ||
| with advanced technology | EC 135b | 85.80 | 4.00 | 73.00 | 97.00 | 16.00 | 87.9 | 4.16 | ||
| BK 117b | 87.20 | 4.60 | 74.00 | 101.00 | 21.16 | |||||
| Bell 206 B Jetrangerc | 88.80 | 4.00 | 76.00 | 100.00 | 16.00 | |||||
| Bell 206 Longranger IIc | 89.80 | 4.00 | 77.00 | 101.00 | 16.00 | |||||
| without advanced technology | UH 1Db | 86.80 | 4.00 | 74.00 | 98.00 | 16.00 | 98.41 | 4.49 | ||
| BO 105c | 91.80 | 4.00 | 79.00 | 103.00 | 16.00 | |||||
| Sea Kingc | 92.60 | 7.50 | 78.00 | 114.00 | 56.25 | |||||
| Ecureuil AS350Bb | 92.80 | 4.00 | 80.00 | 104.00 | 16.00 | |||||
| Alouette IIIbb | 98.40 | 4.80 | 85.00 | 113.00 | 23.04 | |||||
| Sikorsky H‐23/UH12c | 99.70 | 3.90 | 87.00 | 111.00 | 15.21 | |||||
| Alouette IIb | 100.10 | 4.40 | 87.00 | 113.00 | 19.36 | |||||
| Sikorsky H‐34c | 101.8 | 4.00 | 89.00 | 113.00 | 16.00 | |||||
| Mi‐4c | 109.10 | 3.50 | 97.00 | 117.00 | 12.25 | |||||
| Sikorsky H‐37 Mojavec | 111 | 3.40 | 99.00 | 119.00 | 11.56 | |||||
| Muhr 2016 (Outcome: STS) ‐ hearing loss Swedish military ‐ CBA | ||||||||||
| Study data | Recalculation | |||||||||
| group | follow up mean (month) | # Events | N | follow up (month/year) | per 100 person‐years | |||||
| event rate | lnRR | SE | ||||||||
| HLPP | 8 | 9 | 395 | 0.67 | 3.4 | 0.002 | 0.379 | |||
| non‐exposed | 13 | 31 | 839 | 1.08 | 3.4 | |||||
| Muhr 2006 (Outcome: STS) ‐ hearing loss Swedish military ‐ CBA | ||||||||||
| Study data | Recalculation | |||||||||
| group | follow up mean (month) |
# Events | N | group | follow up (year) |
# Events | N | per 100 person‐years | ||
| event rate | lnRR | SE | ||||||||
| HLPP (low‐exposed) | 9.25 | 11 | 291 | HLPP (low‐exposed) | 0.77 | 11 | 291 | 4.9 | 0.73 | 1.04 |
| HLPP (medium‐exposed) | 13 | 252 | non‐exposed (split 1) | 0.92 | 1 | 46 | 2.37 | |||
| HLPP (high‐exposed) | 35 | 204 | HLPP (medium‐exposed) | 0.77 | 13 | 252 | 6.69 | 1.04 | 1.04 | |
| non‐exposed | 11 | 4 | 138 | non‐exposed (split 2) | 0.92 | 1 | 46 | 2.37 | ||
| HLPP (high‐exposed) | 0.77 | 35 | 204 | 22.26 | 1.55 | 0.73 | ||||
| non‐exposed (split 3) | 0.92 | 2 | 46 | 4.74 | ||||||
| non‐exposed (all) | 0.92 | 4 | 138 | 3.16 | ||||||
| low‐exposed vs non‐exposed (all) | 0.439 | 0.584 | ||||||||
| medium‐exposed vs non‐exposed (all) | 0.750 | 0.572 | ||||||||
| high‐exposed vs non‐exposed (all) | 1.951 | 0.528 | ||||||||
aBased on task analysis and helicopter noise data, task analysis is based on measurements of type and duration of tasks per rescue operation of four bases over 1 year (total, 2726 rescue operations). bStudy authors obtained helicopter noise data from own measurements (n = 3 per helicopter). cStudy authors obtained helicopter noise data from other studies.
For hearing loss, the included studies measured effects both as permanent loss of hearing acuity (dB units) on a continuous scale expressed as differences in means, and as the rate of workers with a certain amount of hearing loss, which was expressed using odds ratios (OR). Usually these amounts were defined as a STS and measured as a change or shift in hearing loss of at least 10 dB averaged over 2 kHz, 3 kHz and 4 kHz in either ear, which is also the criterion used by OSHA to maintain a safe and healthy work environment (Rabinowitz 2007). In one study this was defined as the better ear (Davies 2008) and in one study as the worst ear (Lee‐Feldstein 1993). In one study the STS was considered for all frequencies tested (Nilsson 1980). In another study it was defined as greater than 15 dB at the best ear at any test frequency (Muhr 2006). We considered STS to be the event and were recalculated rates per 100 person‐years for all studies that used the STS as an outcome measure.
We used the change in hearing level at 4 kHz as the effect measure because this frequency is generally considered to be the most susceptible to the detrimental effects of noise (May 2000). We took the last minus the first measurement in all cases, thus a positive number indicates an increase in hearing loss.
For TTS, all outcomes were recalculated in order to reflect hearing thresholds before noise exposure minus hearing thresholds after noise exposure. TTS is highly dependent on the amount of time between exposure and measurement. All authors indicated this time interval. We presented the results according to this time interval.
For time‐series, were extracted data from the original papers (Joy 2007) or obtained additional data from the authors (Rabinowitz 2011) and re‐analysed them according to the recommended methods for analysis of ITS designs for inclusion in systematic reviews (Ramsay 2003). These methods utilise a segmented time‐series regression analysis to estimate the effect of an intervention while taking into account secular time trends and any autocorrelation between individual observations. For the included studies, we fitted a first order auto regressive time‐series model to the data using a modification of the parameters of Ramsay 2003. Details of the mode specification are as follows:
Y = ß0+ ß1time+ ß2 (time‐p) I(time > p) +ß3 I(time > p)+ E, E˜ N(0, s2)
For time = 1,...,T, where p is the time of the start of the intervention, I (time ≥ p) is a function that takes the value 1 if time is p or later and zero otherwise, and where the errors E are assumed to follow a first order auto regressive process (AR1). The parameters ß have the following interpretation:
ß1 is the pre‐intervention slope; ß2 is the difference between post and pre‐intervention slopes; ß3 is the change in level at the beginning of the intervention period, meaning that it is the difference between the observed level at the first intervention time point and that predicted by the pre‐intervention time trend.
Unit of analysis issues
There were no cluster‐randomised trials for which we had to assess a unit of analysis error. However, there were three studies (Adera 2000; Lee‐Feldstein 1993; Simpson 1994) that used a cluster of companies as a control group but did not correct for the clustering effect and thus had artificially high precision. We assumed an intra‐class correlation coefficient of 0.06, based on analogy of the study on workplace health promotion by Martinson 1999. We adjusted the size of the control groups for the design effect according to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b). For studies that used a cluster‐randomised design and adjusted statistically for the design effect (Berg 2009), we used the adjusted OR to be entered into RevMan 5 (RevMan 2014). One other study (Seixas 2011) used a combined cluster‐ and individually‐randomised design but did not provide enough information about the clustering to be able to adjust for clustering effects.
One study had multiple intervention arms (Hager 1982). To include it in a meta‐analysis, we chose to include the arm with the most active intervention and the control group with the least noise exposure, thus avoiding the inclusion of the same control group twice.
Dealing with missing data
We asked seven study authors to provide missing data and we obtained data from six of them (Davies 2008; Huttunen 2011; Joy 2007; Moshammer 2015; Rabinowitz 2011; Seixas 2011). In two cases we calculated standard deviations (SDs) from P values (Hager 1982) and standard errors (SE) from OR and 95% confidence interval (CI) values (Berg 2009) according to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b).
We also contacted the author of one study to categorise the evaluated helicopters to the two different types of intervention compared in the study (with or without advanced technology) and we received the additional information (Küpper 2013).
Assessment of heterogeneity
First we assessed whether studies were sufficiently homogeneous to be included in one comparison, based on the similarity of the timing of the outcome measurement (immediate or long‐term) and the type of intervention, what the control condition was (poor‐quality HLPP, non‐exposed workers) and when the outcome was measured (one year, one to five years, more than five years).
Next, we tested for statistical heterogeneity by means of the I² statistic as presented in the meta‐analysis graphs generated by the RevMan software (Higgins 2003; RevMan 2014). If this test statistic was greater than 50% we considered there to be substantial heterogeneity between studies (Deeks 2011).
Assessment of reporting biases
Since there were no comparisons for which we could include more than five studies we did not attempt to assess publication bias.
Data synthesis
We included studies that we deemed sufficiently homogeneous with regard to interventions, participants, settings and the outcomes measured in a meta‐analysis.
For HLPPs, we deemed both the change in hearing loss at 4 kHz and the STS sufficiently similar to combine them as similar outcomes in the meta‐analysis. Because the former is a continuous measure and the latter a dichotomous measure we had to use effect sizes to combine these two. We used the mean change in hearing threshold at 4 kHz to calculate effect size as follows: (effect size = mean change difference/standard deviation). For the rate of occurrence of standard threshold shifts we calculated the ORs, took their natural logarithm and divided them by 1.8 to transform them also into effect sizes (Chinn 2000). We entered these effect sizes and their standard errors into the meta‐analysis using the Generic Inverse Variance method as implemented in RevMan 2014.
When the results were statistically heterogeneous according to the I² statistic we used a random‐effects model for the meta‐analysis.
After meta‐analysis we recalculated a mean change difference from the pooled effect size using the median standard deviation of the included studies in the formula: (pooled mean change = pooled effect size * median standard deviation).
Some study authors reported the results according to hearing thresholds at the start of the study (Pell 1973). We included these categories as subgroups and combined them in the meta‐analysis as subcategories. Other study authors presented the data according to gender (Adera 2000) and we combined these data following the instructions of the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2011). In two studies, we used the same control group as a comparison in multiple subgroups. To avoid using the same control group data more than once, we split the control group into three (Muhr 2006) or two (Seixas 2011) equal subgroups that were subsequently combined in the meta‐analysis.
In our protocol we planned to conduct a qualitative synthesis. However the GRADE approach is now the recommended method. We therefore used the GRADE approach to rate the quality of evidence as follows. The quality of the evidence on a specific outcome is based on the study design, risk of bias, consistency, directness (generalisability) and precision (sufficient or precise data) of results and publication bias across all studies that measure that particular outcome. The overall quality is considered to be high when RCTs with low risk of bias, with consistent, precise and directly applicable results and without evidence of reporting bias, measure the results for the outcome, and is reduced by a level for each of the factors not met. For observational studies, the overall quality is considered low at the start of the rating process and this can be further downgraded in the same way as for RCTs but upgraded if the studies have special strengths (large effect size, dose response and findings contrary to confounding). For non‐randomised studies, the judgement of the quality of the evidence is more difficult than for RCTs because of the wider variation and the lesser likelihood of being able to combine studies in a meta‐analysis. Therefore we presented our GRADE rating in a separate table that includes all comparisons (Table 10).
2. Assessment of quality of evidence (GRADE).
| Comparison | N Studies | 1. RoB? | 2. Inconsistent? | 3. Indirect? | 4. Imprecise? | 5. Pub bias? | 6. Large ES? | 7. DR? | 8. Opp Conf | Qualitya |
| Outcome noise | ||||||||||
| Legislation vs no legislation | 1 ITS | yes | 1 study | no | no | 1 study | yes | no | no | very low (1) |
| One HPD vs another HPD | 1 RCT 4 CBA | 2 yes | no | no | no | not shown | no | no | no | low (1) |
| HPD+Instruction vs HPD‐instruction | 2 RCT | 2 no | no | no | yes | not shown | na | na | na | moderate (4) |
| Information vs no information | 1 RCT (2 arms) | 1 yes | 1 study | no | yes | 1 study | na | na | na | low (1, 4) |
| Outcome hearing loss | ||||||||||
| One HPD vs another HPD (TTS) | 2 CBA | no data | ||||||||
| Muffs vs plugs | 2 CBA | 2 yes | no | no | yes | not shown | no | no | no | very low (1,4) |
| Frequent HPD vs less frequent use | 1 CBA | 1 yes | 1 study | no | yes | 1 study | no | no | no | very low (1) |
| HLPP vs audiometry | 1 RCT | 1 yes | 1 study | no | no | 1 study | na | na | na | moderate (1) |
| HLPP+exposure information vs HLPP‐information | 1 CBA | 1 yes | 1 study | no | yes | 1 study | no | no | no | very low (1,4) |
| Frequent HPD in HLPP vs less | 5 CBA | 5 yes | no | no | yes | not shown | no | no | no | very low (1,4) |
| HLPP vs no exposure | 7 CBA | 7 yes | no | no | yes | not shown | no | no | no | very low (1,4) |
| Follow‐up vs no follow‐up | 1 CBA | 1 yes | 1 study | no | yes | 1 study | no | no | no | very low (1,4) |
| HLPP+long shifts vs HLPP normal | 1 CBA | 1 yes | 1 study | no | yes | 1 study | no | no | no | very low (1,4) |
1‐5 Reasons for downgrading: 1. Risk of bias/Limitations in study design 2. Inconsistency between studies. 3. Indirectness of PICO 4. Imprecision of the results 5. Publication bias. 6‐8 Reasons for upgrading: 6. Large effect size. 7. Dose‐repsonse relationship 8. Confounding opposes the direction of the effect; na= not applicable; 1 study = only one study available and impossible to assess consistency or publication bias
aFinal grading of quality of evidence, between brackets domain that led to down/upgrading the quality.
The interpretation of the quality of evidence is as follows. With high‐quality evidence, it is unlikely that further research will change our confidence in the estimate of effect. With moderate‐quality evidence, further research is likely to have an impact and may change the estimates. With low‐quality evidence, further research is very likely to have an important impact and with very low‐quality evidence any estimate of effect is very uncertain.
We entered the results for the most important comparisons into eight 'Summary of findings' tables (Table 1). To keep the amount of information manageable we left out the comparison of the effects of various hearing protection devices on noise exposure and temporary hearing loss, the comparison of frequent versus less frequent use, the comparison of follow‐up of STS and the comparison of HLPP for long versus normal shifts.
Sensitivity analysis
We conducted a sensitivity analysis, which involved leaving out one study (Pell 1973) that had the highest risk of bias, due to differences in age between the intervention and the control group.
Results
Description of studies
Results of the search
Our search yielded 3899 references in total (1360 in 2009, plus 1129 in 2012, plus 1410 in 2016). The search in 2009 yielded 1198 references from a combined search of MEDLINE and Embase using Ovid, 86 from CINAHL, 76 from CENTRAL and 9 from the Cochrane Work's Trials Register up until 2005. An additional search from 2005 to December 2008 yielded an additional 256 references. The update in January and February 2012 for references from 2009 to 2012 brought 54 new references from PubMed, 299 from Embase, 601 from Web of Science, 168 from NIOSHTIC and 7 references from reference lists of articles. The update in September 2016 was based on two searches, one in 2015 and one in 2016. The combined retrieval for references from 2012 to 2016 yielded 987 references from PubMed and Embase, 385 from Web of Science, and 204 from OSHupdate. We searched CENTRAL and CINAHL for references from 2009 to September 2016 and found 294 references from CENTRAL (excluding reviews) and 263 from CINAHL.
The screening of references for eligibility resulted in 265 studies (104 in 2009, 50 in 2012, 111 in 2016), which we then retrieved in full text.
Following further screening using our eligibility checklist, 29 articles ultimately fulfilled our inclusion criteria. One article described two trials (Park 1991a instructions; Park 1991b protection) and two articles described the same study. This resulted in 29 included studies (21 in 2009, 4 in 2012, and 4 in 2016).
See also Figure 1.
1.
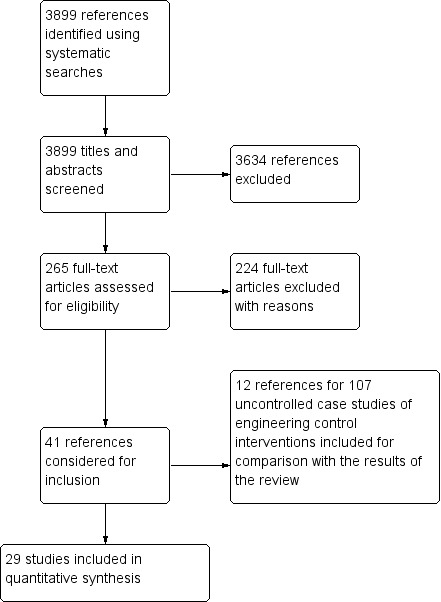
PRISMA Study flow diagram
Included studies
See also the 'Characteristics of included studies' table.
Design
We had considerable difficulty in establishing the types of study design used. In many articles, studies reported technical measurements that would apparently not be prone to bias and would not require a control group or long‐term follow‐up. Four studies used a randomised design (Berg 2009; Park 1991a instructions; Salmani 2014; Seixas 2011) and one study used a quasi‐randomised design with alternation (Royster 1980). Another two studies used an interrupted time‐series (ITS) design (Joy 2007; Rabinowitz 2011). All remaining studies used a form of controlled before‐after (CBA) design.
To measure the long‐term effects of hearing loss prevention, only two studies used a randomised design (Berg 2009; Seixas 2011) and another study used a CBA design but reported data for an ITS analysis, and we used these data for the analysis (Rabinowitz 2011). Seven studies implicitly used an equivalence design in which they tried to prove that the intervention (a hearing loss prevention programme (HLPP)) led to the same amount of hearing loss as in a non‐exposed control group (Davies 2008;Gosztonyi 1975; Hager 1982; Lee‐Feldstein 1993; Muhr 2006; Muhr 2016; Pell 1973). In another five studies, the authors tried to show that better implementation of a HLPP led to a better outcome. Adera 1993, Adera 2000 and Simpson 1994 compared study companies with companies from a database called ANSI S12.13, which were rated as having a very high‐quality HLPP, and Brink 2002 compared workers who wore hearing protection less than 33% of the time to those who wore hearing protection more often. A similar comparison of more versus less use of hearing protection devices was used in Moshammer 2015. Heyer 2011 used a retrospective study design and combined historical data of noise exposure, working tasks and audiometric results of the workforce of three plants. The authors compared the effect on the rate of hearing change during the time individuals were in a well‐implemented hearing conservation programme, with the rate observed among individuals who were in less well‐implemented programmes, by programme component.
All but three of the long‐term equivalence and implementation studies were retrospective by design meaning that the data were already gathered before the study was planned. The first of these three studies reported to be prospective (Pell 1973), whereas the second study (Seixas 2011) collected noise exposure measurement data pre‐intervention and at two‐ and four month follow‐up times. The third study (Berg 2009) collected hearing loss data of students enrolled in a HLPP prospectively over a three‐ and 16‐year follow‐up and used retrospectively collected data to assess exposure for the 16‐year follow‐up. Many studies reported only the change, which made it difficult to assess baseline comparability of age and hearing loss.
To measure the immediate effects of hearing protection, studies essentially used before‐after measurements in which it was not always clearly stated what the comparison was. In this case, before and after the intervention should be interpreted as 'outside' versus 'inside' the hearing protector (Pääkkönen 1998; Pääkkönen 2001; Park 1991a instructions) or 'before exposure with protection' versus 'after exposure with protection' (Horie 2002; Royster 1980).
For assessing the immediate effect, all studies used a prospective design in which data were gathered after the study had been planned. One study used a Latin square design in which participants were randomised to four different types of hearing protection with and without instructions for use (Park 1991a instructions; Park 1991b protection). Another study randomised participants to the same type of hearing protections either with or without training (Salmani 2014). In five studies the same workers used sequentially different types of hearing protection (Horie 2002; Huttunen 2011; Pääkkönen 1998; Pääkkönen 2001; Royster 1980).
Sample sizes
Although large numbers of workers were examined, this number was reduced substantially in many cases because workers had to be followed over a long period of time in the same noise levels, thus reducing the number of eligible subjects.
The sample size of the first ITS noise exposure study was 142,735 workplaces, measured during 18 years of follow‐up, four years post‐intervention and 14 years pre‐intervention with the intervention implemented in the year 2000 (Joy 2007). The other ITS study included 312 workers followed during nine years from 2000 to 2009 with the year of intervention being 2005 (Rabinowitz 2011).
In the 19 hearing loss evaluation studies, sample sizes ranged from 43 to 22,376 workers, amounting to a total of 84,153 with an average of 4429 participants per study. We adjusted for the cluster effect by reducing the sample size according to the number of clusters and the design effect. After adjustment the sample sizes totaled 55,908 with an average of 2943 participants per study.
Numbers in the eight immediate effect studies ranged from 4 to 150, amounting to a total of 358, with an average of 45 workers per study.
Setting
The legislation evaluation study (Joy 2007) was carried out in coal mines and the administrative control intervention study (Seixas 2011) in construction sites in the USA.
Eight studies evaluated immediate effects (noise attenuation) and three studies evaluated the preventive effect on hearing loss of personal hearing protection devices. One of the immediate studies was carried out in Japan, one in Iran, three in Finland and three in the USA. Four of the immediate effect studies were carried out after 2000, three in the 1990s and one in 1980. All of the hearing loss studies were based on data from the 1980s, two were carried out in Sweden and one in Austria. In one study we found a potential conflict of interest as the company that produced the earplugs that were tested also participated in the study (Royster 1980).
Nine long‐term hearing loss evaluation studies were published after 2000, five in the 1990s, one in the 1980s, and two in the 1970s. Since most studies were retrospective, they were based on data gathered in the decade(s) preceding their publication.
Thirteen of the long‐term HLPP evaluation studies were carried out in the USA, one in Canada (Davies 2008) and two in Sweden (Muhr 2006; Muhr 2016), which is of importance because of the different weighting used for summarising noise levels over time.
Two older studies were carried out by in‐house occupational health professionals (Gosztonyi 1975; Pell 1973) and four by in‐house military officials (Adera 1993; Meyer 1993; Muhr 2006; Muhr 2016). They were thus actually financed by the companies that were supposed to benefit from the HLPP. This created, in our view, a potential conflict of interest in the sense that the employers of the authors could potentially benefit from a positive result of their studies.
Participants
The participants in all studies were described as being exposed to noise at work. However, these descriptions were often based on measurement methods that were not clearly described.
Noise‐exposed participants worked on construction sites (one study), in mines (one study), in the automobile industry (three studies), in the steel industry (two studies), in an aluminium smelter (one study), in agriculture (one study), in the lumber industry (one study), in an orchestra (one study), at a shipyard (two studies), in the military (four studies), in one unspecified company (three studies) or were gathered from various workplaces (eight studies). One study did not specify the type of industry nor the type of jobs included in the study (Salmani 2014).
In most studies only men were included or there were mostly male workers at the workplaces that were studied.
Interventions
We found one study that evaluated technical noise reduction measures over time based on the change of legislation that forced coal mines to take measures to decrease noise levels (Joy 2007). The new legislation established the primacy of engineering and administrative controls and an Action Level of 85 dB(A), at which enrolment for hearing conservation programmes should be started. The legislation officially came into effect in the year 2000 but many employers had already prepared themselves to address it in 1999. Nevertheless we chose the year 2000 as the intervention year but we also present results for the year 1999. The intervention was supposed to be equally effective for the above ground and underground workplaces. We present the outcomes for both situations.
Another study intended to change workers' behaviour (Seixas 2011). The intervention consisted of two types of information and the distribution of personal noise level indicators. The control group received information at baseline only. It was a one‐time information session consisting of two hours of instructions for hearing protection device use and fitting as well as noise control techniques (sound barriers and distance). The three intervention groups each received a different combination of the interventions: both types of information (extensive information), noise level indicator with extensive information, or noise level indicator with one‐time information only. The extensive information consisted of a one month long weekly on‐site training session focusing on areas of hearing protection device use and noise control. Workers receiving the noise level indicator clipped it to their shoulder or chest. The noise level indicators were implemented for two months and gave a light signal when the noise level exceeded 85 dB(A), 95 dB(A), 105 dB(A) and in addition vibrated at 115 dB(A).
Studies that evaluated hearing protection devices evaluated active noise cancellation devices (Horie 2002; Pääkkönen 2001), special communication earmuffs (Pääkkönen 1998), the effect of fitting instructions (Park 1991a instructions; Salmani 2014), alternative hearing protection (Erlandsson 1980; Huttunen 2011; Nilsson 1980; Park 1991b protection; Royster 1980) or the percentage of working time with hearing protection devices (more versus less use) (Moshammer 2015).
In sixteen studies a hearing surveillance, hearing conservation or HLPP was evaluated as the intervention of interest. We have described the contents of the interventions extensively in Table 11. For example, in one study the intervention consisted of annual audiometry and instruction once but with yearly reminders delivered to the home address and free hearing protection whereas the control group received only audiometry (Berg 2009). In another study the intervention was daily monitoring of at‐ear noise exposure with regular feedback from a supervisor in addition to the ongoing mandatory hearing conservation programme (Rabinowitz 2011). In Meyer 1993 the intervention was frequent follow‐up for one year after a standard threshold shift (STS) had been found in a person exposed to noise, with the aim of detecting susceptible people with increasing hearing loss. Reynolds 1990a evaluated the effectiveness of a HLPP for workers on 12‐hour work shifts.
3. Contents of hearing loss prevention programmes.
| Study | Described as HLPP | HPD provided | Noise measurements | Technical measures | Administrative measures | Audiometry |
| Adera 1993 | ? | Enforced mandatory wearing of hearing protection | Personal dosimeter twice a year | ? | ? | Audiometric booth ANSI‐OSHA |
| Adera 2000 | HLPP | ? based on Aldera 1993 we assumed that excellent implementation meant better use of hearing protection | ? | ? | ? | Audiogram taken |
| Berg 2009 | HCP | Beside educational intervention, hearing protection devices were provided free to students and replaced regularly | Students were given opportunity to use sound level meter unaffiliated | Not part of the programme | Not part of the programme | Yearly audiometric testing, calibrated per ANSI standard with Hughson‐Westlake modification of the ascending threshold technique |
| Brink 2002 | HCP | ? | Area‐wide sound level surveys | ? | ? | Annual audiometric evaluation calibrated Bekesy audiometer ANSI |
| Davies 2008 | HCP | Hearing protection was one element | Noise monitoring was one element | Engineering controls were one element | Administrative controls were one element | Audiometric evaluation by certified audiometric technicians |
| Erlandsson 1980 | ? | ? | Personal noise dosimeters | ? | ? | Calibrated ISO r389 |
| Gosztonyi 1975 | HCP | Earmuffs mandatory in noise areas | Calibrated personal dosimeters sound level meter in all shop areas | ? | ? | Soundproof booth ANSI s3.1‐1960 |
| Hager 1982 | Walsh‐Healy standard; OSHA | Yes, mandatory use of approved protection | ? | Gradual continuous engineering control wherever, whenever economically feasible | ? | Audiometric surveys |
| Heyer 2011 | HCP | ? Percent use of hearing protection used as a quality indicator | Used as a quality indicator of the programmes: high quality if any monitoring and worker input reported by focus group | Stated as part of the programme but not possible to evaluate with the study data | Training and education stated as part of the programme but not possible to evaluate with study data | Audiometric testing, quality varies, evaluated as days between two tests, audiometry method not reported |
| Lee‐Feldstein 1993 | ? | ? | Annual sound surveys | ? | ? | Automatic audiometer according to ANSI s3.6‐1996 |
| Meyer 1993 | HCP | Must be provided with effective HP devices | Identify hazardous noise | ? | Detailed follow‐up 3 and 6 months after a STS | ? |
| Muhr 2006 | HCP | Earmuffs and or earplugs with level‐dependent function limited to 82 dB(A) with SNR 27 dB | Standardised noise measurements | Risk areas around weapon use | ? | Screening audiometry |
| Muhr 2016 | HCP, stated to be stricter than to the one evaluated in Muhr 2006 | Mandatory use of HPDs, earmuffs and or earplugs with or without level‐dependent function (enable speech communication), (stated to be stricter recommendations and better devices) | ? | safety distances (stated to be stricter) | Mandatory training in HPD use and education in NIHL and noise induced tinnitus, stricter audiometry inclusion criteria for acceptance to military service (≤ 25 dB average HL for the frequencies 0.5 to 8 kHz in both ears, 30 dB HL at one or more frequencies, and 35–40 dB HL at one single frequency) (to exclude mild hearing loss cases presumed to be more vulnerable to HL) | Screening audiometry at begin and end of military service |
| Nilsson 1980 | Routine HCP | ? | Individual noise dosimetry over long periods | ? | ? | Calibrated ISO 389 isolated booth |
| Pell 1973 | ? | Mandatory hearing protection | Routine noise level surveys | Noise abatement | ? | Automatic Bekesy‐type ANSI calibrated |
| Reynolds 1990a | HCP | 3 specific types of earplugs | Sound survey, noise dosimeters | ? | ? | Audiometric database |
| Simpson 1994 | Demonstrate excellent HCP practices | ? | ? | ? | ? | ? |
ANSI = American National Standards Institute HCP = hearing conservation programme HL = hearing loss HLPP = hearing loss prevention programme HPD = hearing protection device ISO = International Organization for Standardization OSHA =Occupational Safety and Health Administration SNR = Single Number Rating ? = not reported
Outcomes and measures
In one ITS and all but one long‐term evaluation study, the authors measured hearing thresholds as an outcome measure for hearing loss. Three studies measured the difference in hearing thresholds with and without hearing protection as the effect measure for noise attenuation. One ITS and three short‐term evaluation studies measured sound pressure levels as the outcome measure for noise exposure.
In some studies the authors also reported the percentage of workers whose hearing got worse or the percentage of workers whose hearing got better. Others used the increase in standard deviations of hearing levels to show the effect of the programme or summarised audiometric results in low and high frequencies. However we did not use these percentages of workers nor increases in standard deviation because they did not add anything to the outcomes that we already included.
Authors used varying definitions of hearing loss. In seven studies they used STS, defined as an increase in hearing threshold of at least 10 dB averaged over 2 kHz, 3 kHz or 4 kHz compared to a baseline measurement or the previous measurement (Adera 1993; Adera 2000; Berg 2009; Davies 2008; Lee‐Feldstein 1993; Meyer 1993; Simpson 1994 ). In one study STS was defined as an increase of more than 10 dB in any frequency. In another study STS was defined as an increase of 15 dB in one or both ears at one or more frequencies (0.25 kHz to 8 kHz) between the first and second audiometry (Muhr 2016). In other studies hearing loss was measured as the average over the frequencies 0.5 kHz, 1 kHz, 2 kHz, 3 kHz, 4 kHz and 6 kHz. One study used the frequencies 3 kHz, 4 kHz and 6 kHz (Heyer 2011). Two studies also included the frequency of 8 kHz (Muhr 2006; Park 1991a instructions). One study used the rate of hearing loss in the binaural average hearing level at 2 kHz, 3 kHz, and 4 kHz (Rabinowitz 2011). One study did not clearly define hearing loss but used the baseline hearing minus age‐related hearing loss at the last observation as the outcome measurement (Moshammer 2015).
The authors of two studies measured temporary threshold shifts (TTS) as the effect measure of noise attenuation (difference in hearing levels before and after exposure to noise) (Horie 2002; Royster 1980). Four other studies used REAT (the differences in hearing thresholds with and without hearing protection) (Huttunen 2011; Park 1991a instructions; Park 1991b protection; Salmani 2014). Two studies reported the mean (SD) noise attenuation over the frequencies 0.125 kHz to 8 kHz (Huttunen 2011) or over the frequencies 0.5 kHz, 1 kHz, 2 kHz, 3 kHz, 4 kHz, 6 kHz, and 8 kHz (Salmani 2014). In Salmani 2014 the SDs reported were unrealistically small and did not match with the box‐plots in the figure. We contacted the study authors but they did not reply. We then extracted the interquartile ranges from the box‐plots and multiplied them by 1.35 to obtain a more realistic estimate of the SDs, according to the advice in the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2011). One study reported the noise attenuation per frequency (0.5 kHz, 1 kHz, 2 kHz, 3 kHz, 4 kHz, 6 kHz, and 8 kHz) and we calculated the mean (SD) noise attenuation over all measured frequencies (Park 1991a instructions).
In one study, authors used personal noise dosimeters with a 3 dB exchange rate, 80 dB(A) threshold level, 85 dB(A) criterion level, and slow response to measure the full‐shift Equivalent Continuous Sound Level (Leq) (Seixas 2011). In one study authors used the eight‐hour time‐weighted average (TWA) as a measure for noise exposure transformed to a permissible exposure level (PEL) dose (Joy 2007). The PEL dose transforms the noise levels to an equivalent of a 90 dB(A) noise exposure by using an exchange rate of 5 dB for doubling the dose. This translates 90 dB(A) into a 100% PEL dose, and for example 85 dB(A) into 50% and 95 dB(A) into 150% PEL dose. Two studies used MIRE (microphone in real ear) to measure the difference in noise levels inside and outside the hearing protectors (Pääkkönen 1998; Pääkkönen 2001).
Case studies
In this 2017 update, we collected 12 additional references that reported effects of engineering control interventions of 107 cases (Azman 2012; Caillet 2012; Cockrell 2015; Golmohammadi 2014; HSE 2013; HSE 2015; Küpper 2013; Maling 2016; Morata 2015; Pan 2016; Thompson 2015; Wilson 2016). Table 12 provides an overview of study characteristics. We have presented the results under the heading Effects of interventions and in additional tables (Table 13; Table 14; Table 15; Table 16; Table 17; Table 18; Table 19).
4. List of included case studies.
| Reference ID | Case studies included in review | |||||
| Number of cases | Type of industry | Country | Interventiona | Measureb | Additional information (number of cases) | |
| Azman 2012 | 1 | mining (1) | USA | retro‐fit | noise level, noise dose | description of noise measurement (1), follow‐up (1) |
| Caillet 2012 | 1 | offshore helicopter (1) | France | all retro‐fit | noise level | description of noise measurement (1), funding (1), conflict of interest (1) |
| Cockrell 2015 | 2 | manufacturing (2) | USA | all retro‐fit | noise level, dose | description of noise measurement (2) |
| Golmohammadi 2014 | 3 | steel industry (3) | Iran | all retro‐fit | noise level, dose | description of noise measurement (3), funding (3), conflict of interest (3) |
| HSE 2013a | 57 | manufacturing (57) | not reported | new 6 retro‐fit 51 |
noise level | ‐ |
| HSE 2015 | 2 | manufacturing (2) | not reported | all retro‐fit | noise level | ‐ |
| Küpper 2013 | 1 | alpine rescue operation (helicopter) (1) | Austria, Switzerland | new | noise level | description of noise measurement, follow‐up, statistical tests used |
| Maling 2016 | 8 | textile (1), paper shredding (1), manufacturing (6) | USA | new 4, retro‐fit 2, both 2 |
noise level | ‐ |
| Morata 2015 | 18 | manufacturing (15), drilling industry (2), mining (1) | not reported | new 5, retro‐fit 11, both 2 |
noise level, dose | description of noise measurement (3) |
| Pan 2016 | 3 | mining (3) | Australia | all retro‐fit | dose | description of noise measurement (2), funding (3), follow‐up (immediate) (3) |
| Thompson 2015 | 5 | mining(5) | USA | all retro‐fit | noise level, dose | description of noise measurement (1), adverse effects: engine over‐heating (1), time of intervention: 2014/2015 (1) |
| Wilson 2016 | 6 | manufacturing (6) | not reported | all retro‐fit | noise level | ‐ |
| Total | 107 | manufacturing (88), mining (10), steel (3), drilling (2), helicopter (2), textile (1), paper shredding (1) | Australia (3), Iran (3), France (1), USA (16), Austria and Switzerland (1), nr (26) | retro‐fit (86), new (16), both (4) | noise level, dose | description of noise measurement (14), funding (7), follow‐up (5), conflict of interest (4), adverse effects (1), time of intervention (1), statistical tests used (1) |
aTypes of intervention: installation of completely new equipment (new), intervention to improve existing equipment (e.g. new parts, additional damping material layers) (retro‐fit), or a combination of new and retro‐fit interventions (both). bNoise level (including time‐weighted averages or sound pressure levels), dose (including calculations according to OSHA, NIOSH, or MSHA PEL specifications).
5. Results case studies ‐ new equipment.
| New equipment | |||||||
| Noise source | Intervention | follow‐up | Initial noise level | Noise level after | 8 h TWA before | 8 h TWA after | Reference ID |
| Helicopter | Modern helicopter with advanced technology (compared to older helicopters without advanced technology) | short term (1 year) | mean 98.41 (SD 4.49) (n = 10) | mean 87.9 (SD 4.16) (n = 4) | Küpper 2013 | ||
| Pumps | New high‐pressure coolant pumps have been installed at various metal cutting operations. These new pumps produce more pressure and more volume directly at the cutting tools. | not reported | 110 dB | 87 dB | Maling 2016 | ||
| Drill | New injector drill with a sound enclosure for a deep drilling operation | not reported | 110 dB | 95 dB | |||
| Roof fans | Old roof fans were replaced with new high‐efficiency fans | not reported | lowered the noise below the fan | ||||
| Air gun | Air gun substitution | not reported | 94 dB | 85 dB | Morata 2015 | ||
| Fork lifts | Use of tugs instead of fork lifts | not reported | 92 dB | 72 dB | |||
| Alarm system | Change from audible alarm to visual warning and pressure sensor | not reported | 95 dB | 0 dB | |||
| Air wand | Replacement of 45 air wands | not reported | 112.8 dB | 90.1 dB | |||
| Bottling line ‐ rinser‐filler‐capper machine | Purchase of a new bottling line | not reported | 89 dB | below 80 dB | HSE 2013 | ||
| Bottle‐blowers | New bottle‐blowers and segregation | not reported | 86‐87 dB | below 83 dB | |||
| Glass bottles on transport conveyer | Purchasing new design of bottle transport conveyor | not reported | 101 dB | 83 dB | |||
| Packing machinery ‐ Compressors and compressed‐air exhausts | Purchasing policy and fitted silencers | not reported | above 90 dB | below 85 dB | |||
| Bakery machinery | Not purchasing equipment that produced noise level above 85 dB, company’s health and safety adviser would visit the makers of new machinery during its manufacture and conduct a noise assessment to make sure the machinery did not exceed 85 dB | not reported | 94 dB | 85 dB | |||
| Bottle‐laner ‐ bottles banging together on laner conveyor | New machine with guide‐rails | not reported | 93‐96 dB | 87 dB | |||
| Number of cases: 14 | mean before | mean after | mean reduction | ||||
| Noise level dB | 97.4 dB | 77.7 dB | 19.7 | ||||
| TWA dB | 98.41 (SD 4.49) | 87.9 (SD 4.16) | 10.51 (95% CI 15.45 to 5.57) | ||||
TWA = time weighted average
6. Results case studies ‐ acoustic panels and curtains.
| Acoustic panels and curtains | |||||||
| Noise source | Intervention | Follow‐up | Initial noise level | Noise level after | Dose before | Dose after | Reference ID |
| Production noise | Door | not reported | 85 dB | 79 dB | Morata 2015 | ||
| Blast furnace | Control rooms were redesigned in order to improve acoustical condition: installation of a UPVC window with vacuumed double‐layered glass 80 x 80 cm and double wall for entrance by 90° rotate plus a 2.0 × 1.2 m steel door without glass | not reported | 80 dB | 52.6 dB | Golmohammadi 2014 | ||
| Blast furnace | In rest room wall facing to the furnace was made from the armed concrete with a thickness of 20 cm, length of 9 m, and height of 3 m and was located in the entrance by 90° rotate | not reported | 86.1 dB | 58.4 dB | |||
| Blast furnace | Control room and rest room redesigned to improve acoustical condition | not reported | 236% (unspecified) | 130% (unspecified) | |||
| Product impact on multi‐head weigher | Fitted flexible PVC curtains | not reported | 92 dB | 88 dB | HSE 2013 | ||
| Packaging lines | Fitted acoustic baffles to ceiling | not reported | Above 90 dB | below 90 dB | |||
| Noise from hearing protection zones affecting quieter areas | Erected acoustic panels and automatic doors between hearing protection zones and quieter areas | not reported | Above 90 dB | below 85 dB | |||
| Filler pump | Improved efficiency of pump and added acoustic hood | not reported | 96 dB | 86 dB | |||
| Compressed air in bottle transportation | Acoustic side panels fitted | not reported | 85–86 dB | 73 dB | |||
| Product impact on hoppers | Flexible PVC curtains fitted | not reported | Above 90 dB | 83 dB | |||
| Number of cases: 10 | mean before | mean after | mean reduction | ||||
| noise level dB | 88.3 | 77.2 | 11.1 | ||||
| Dose % (unspecified) | 236 | 130 | 106 | ||||
7. Results case studies ‐ damping material and silencers.
| Damping material and silencers | |||||||||
| Noise source | Intervention | Follow‐up | Initialnoise level | Noise level after | 8 h TWA before | 8 h TWA after | Dose before | Dose after | Reference ID |
| Confetti machine | Damped machine surfaces: Replaced vacuums with small cyclones that were quieter and had fewer clogs, Installed conveyors to carry the paper into the disintegrators | not reported | 95 dB | 85 dB | Maling 2016 | ||||
| Production noise | Installation of sound absorbing panels, shields, covers, insulation, sheeting, installation of mufflers for fans and solenoids, reduction of compressed‐air pressure and volume in vents, use of vibrating personal alarms instead of audible alarms | not reported | 2 to 11 dB noise reduction | ||||||
| Helicopter | Cover of structural leaks with lightweight materials (e.g. new door seals) and damping of the structure (patches of constrained visco‐elastic materials that are bonded to the structure), optimised sound‐proofing panels (sandwich panels with “soft core”) and windows (thickened laminated windows with damping layer and double glazing), and Main Gear Box suspension devices (laminated ball joints at MGB support strut foot) | not reported | 7 dB noise reduction | Caillet 2012 | |||||
| Pump | Suppressor on palletizer hydraulic pump to minimize hydraulic banging, pump whine contained in sound‐insulated box | not reported | 88 dB | 83 dB | Morata 2015 | ||||
| Air‐rotary drill rig | Installation of hydraulic noise suppressors and a lead‐fiberglass blanket covering Ihe gap between the inside door and the cab frame | not reported | 98 dB | 95 dB | MSHA PEL 280%; NIOSH 3222% | MSHA PEL 210%: NIOSH 2585% | |||
| Air‐rotary drill rig | Installation of hydraulic noise suppressors | not reported | 98 dB | 97 dB | MSHA PEL 280%; NIOSH 3222% | MSHA PEL 249%; NIOSH 2951% | |||
| Pumps | Installing mufflers on pumps | not reported | 98.1 dB | 81.3 dB | |||||
| Haul trucks in underground metal/non‐metal mines | Improving the engine compartment noise barrier: the usual barrier material has been replaced with a barrier material part number Duracote 5356, manufactured by Durasonic | not reported | MSHA PEL 495% | MSHA PEL 416% | Thompson 2015 | ||||
| Chiller | Reduce noise from a chiller with a combination of acoustic absorbent and retro‐fit constrained layer damping | not reported | 8 dB noise reduction | Wilson 2016 | |||||
| High‐speed strip‐fed press | Normally the press legs are welded boxes, the press frame was isolated from the fabricated legs by inserting 6 mm composite pads between frame and legs | not reported | 101 dB | 92 dB | |||||
| Product impact on hoppers and chutes | Coated internally with food‐grade, sound‐deadening material | not reported | 96–98 dB | Noise reduced by 2‐8 dB | HSE 2013 | ||||
| Gas cylinder impact on metal table | Rubber matting on table | not reported | 110 dB peaks | removal of peak noises | |||||
| Product impact on ducting | Lagged ductwork with noise‐absorbent padding | not reported | 92 dB | 84 dB | |||||
| Product impact on vibrating components | Coated externally with sound‐deadening material | not reported | 92 dB | 84 dB | |||||
| Bread‐basket stacking machine | Fitted hydraulic dampers | not reported | 92 dB | 83 dB | |||||
| Hand‐crimping metal foil packages | Mounted on layers of rubber | not reported | 86–89 dB | 85–86 dB | |||||
| Keg impact on concrete floor | Fitted rubber matting on to floor | not reported | High noise levels | Noise levels reduced | |||||
| Gas cylinder impact on metal ‘A’ frame trolleys | Fitted rubber matting on to trolleys | not reported | 110 dB peaks | Peak noise levels reduced | |||||
| Road tanker degassing | Fitted silencers | not reported | 92 dB | 83 dB | |||||
| Evaporative condensers and refrigeration plant | Fitted silencers | not reported | 94 dB | 83–87 dB | |||||
| Number of cases: 20 | mean before | mean after | mean reduction | ||||||
| noise level dB | 93.6 | 86.5 | 7 | ||||||
| TWA dB | 101 | 92 | 9 | ||||||
| Dose % (MSHA PEL) [dosimeter settings: 90 dB Lt, 90 dB Lc, 5‐dB exchange rate] | 351.7 | 291.7 | 60 | ||||||
| Dose % (NIOSH) [dosimeter settings: 80 dB Lt, 85 dB Lc, 3‐dB exchange rate] | 3222 | 2768 | 454 | ||||||
MSHA = Mine safety and health administration
NIOSH = National Institute for Occupational Safety and Health
PEL = permissible exposure limit
8. Results case studies ‐ design changes.
| Design changes | |||||||||
| Noise source | Intervention | Follow‐up | Initial noise level | Noise level after | 8 h TWA before | 8 h TWA after | Dose before | Dose after | Reference ID |
| Roof bolting machine at underground coal mines | New drill bit isolator | immediate | reduced by 3.2 dB | MSHA PEL per hole 0.85% | MSHA PEL per hole 0.57% | Azman 2012 | |||
| short term (after 253 holes and 628 m) | reduced by 2.2 dB | MSHA PEL per hole 0.9% | MSHA PEL per hole 0.66% | ||||||
| 4‐roll calender in a tire manufacturing facility "calender operator" | Replacing the piercer brackets, optimising alignment and improving preventative maintenance (increased and more frequent lubrication of the piercer and other areas of the equipment with high friction or pressure) | not reported | 87.7 dB | 86.3 dB | OSHA dose 72.8% | OSHA dose 59.6% | Cockrell 2015 | ||
| 4‐roll calender in a tire manufacturing facility "wind up operator" | Replacing the piercer brackets, optimising alignment and improving preventative maintenance (increased and more frequent lubrication of the piercer and other areas of the equipment with high friction or pressure) | not reported | 93.1 dB | 89 dB | OSHA dose 153% | OSHA dose 87.3% | |||
| Heavy metal arms which drove the reciprocating blade on the machines | Alternative linkage using flexible nylon straps | not reported | 95 dB | 75 dB | HSE 2015 | ||||
| Tobacco filter making machine | Machine design improvements on a tobacco filter making machine and room improvements | not reported | 9 dB reduction | Maling 2016 | |||||
| Weaving machines | Use of different spindle | not reported | 100 dB | 90 dB | |||||
| Locomotive for mining | Active noise control | immediate | Pan 2016 | ||||||
| Mining truck | Active noise control | immediate | |||||||
| Mining truck | active noise control and damping material | immediate | |||||||
| Filler | Filler outfeed: line shaft removed, individual drives installed | not reported | 107 dB | 81 dB | Morata 2015 | ||||
| Con‐air dryer | Machine set on vibration mounts, quieter blower | not reported | 94 dB | 85 dB | |||||
| Transfer cart | not reported | not reported | 94 dB | 79 dB | |||||
| Trimmer | rReplacing nozzles from trimmer with in feed decline drive belt | not reported | 98 to 113 dB | 86 to 104 dB | |||||
| Continuous mining machine | Exchange of a single sprocket chain for a dual sprocket chain on a continuous mining machine (CMM, Joy Mining Machine 14CM‐15) | not reported | 93.4 to 93.3 dB | 92 dB | MSHA PEL 159 % | MSHA PEL 132.5% | |||
| Moen case former | Exchange of pneumatic cylinder for servo‐mandrel | not reported | 97 dB | 87 dB | |||||
| Cart | Exchange of cart wheels | not reported | 88 dB | 72 dB | |||||
| Standard longwall cutting drums (mining) | Modified set of longwall cutting drums instead of a set of standard (baseline) drums | not reported | 98 dB | 92 dB | 95.7 dB | 93.1 dB | MSHA PEL 220.5% | MSHA PEL 158.6% | Thompson 2015 |
| Haul trucks in underground metal/non‐metal mines | Improving the engine compartment noise barrier and changing the fan type, size, and rotation speed (larger fan of different design and different fan pulley to reduce the fan rotation speed to 90%) | not reported | 102 dB | 93 dB | MSHA PEL 495% | MSHA PEL 158% | |||
| Load‐haul‐dumps (LHDs) in underground metal/non‐metal mines | Improving the engine compartment noise barrier and changing the fan type, size, and rotation speed (larger fan of a different design and a different fan hub to reduce the fan rotation speed to roughly 87% and new noise barrier material (Duracote Durasonic 5356)) | not reported | 98 dB | 96 dB | MSHA PEL 289% | MSHA PEL 231% | |||
| Load‐haul‐dumps (LHDs) in underground metal/non‐metal mines | Improving the engine compartment noise barrier and changing the fan type, size, and rotation speed (a larger fan of a different design was installed as well as a different fan hub to reduce the fan rotation speed to roughly 95%) | not reported | 98 dB | 93 dB | MSHA PEL 289% | MSHA PEL 142% | |||
| Standard camshaft washer drying nozzles (pneumatic) | Pneumatic nozzles replaced with suitable entraining units | not reported | 12 dB reduction | Wilson 2016 | |||||
| Drier fan | Retro‐fitting aerodynamic and acoustic elements inside fan casings and the associated ductwork | not reported | 9 dB reduction | ||||||
| Aluminium can extract and chopper fans | Fitting aerodynamic inserts inside the fan casing | not reported | 22 dB reduction | ||||||
| Separator (large thin sheet distribution dome) | alteration to a vibratory separator: forming this component in stainless sound deadened steel | not reported | 105 dB | 89 dB | |||||
| Metal trays | Replacing metal trays with plastic trays | not reported | 89 dB | 84‐85 dB | HSE 2013 | ||||
| Metal wheels on baking racks | Replacing baking rack wheels with resin wheels | not reported | above 100 dB | 86‐92 dB | |||||
| Loosening product from baking tins with air knives | Air knives modified to operate with a diffuse air jet | not reported | above 90 dB | below 85 dB | |||||
| Bottles and cans banging together on conveyors | Fitted a pressureless combiner conveyor system | not reported | above 90 dB | below 90 dB | |||||
| Baking tins banging together on chain or slat conveyors | Installing ‘tin‐friendly’ conveyors | not reported | above 90 dB | below 85 dB | |||||
| Manual changeover of baking tins on conveyor | Installed robots to handle pans | not reported | 94‐96 dB | below 90 dB | |||||
| Water pumps on filling machines | Replaced with air pumps and fitted silencers | not reported | 90 dB | 84 dB | |||||
| Filling sachets and cups | New design of horizontal powder‐feeder and enclosed machine | not reported | 83‐84 dB | 80 dB | |||||
| Bottle manufacture, filling and packing lines | Acoustic panels fitted to walls, high ceiling installed | not reported | Above 90 dB | 83 dB | |||||
| Contact between metal trays and metal tracking | Replaced with plastic tracking | not reported | 94 dB | 87 dB | |||||
| Product impact on metal chutes | Replaced with plastic chutes | not reported | 96‐98 dB | 90 dB | |||||
| Electrically powered sausage‐spooling machines | Replaced with compressed‐air spooler | not reported | 86‐90 dB | below 80 dB | |||||
| Tray‐indexing arm | Plastic caps on fingers of indexing arm | not reported | 94 dB | 87‐89 dB | |||||
| Vibratory conveyor | Ensured conveyor only used at least noisy speed | not reported | above 90 dB | below 85 | |||||
| Glass bottles on conveyor | New design of conveyor with different chain speeds | not reported | 101 dB | 84 dB | |||||
| Lidding and de‐lidding tins | Installed robots to lid and de‐lid baking tins | not reported | 90‐93 dB | 88 dB | |||||
| Number of cases: 41 | mean before | mean after | mean reduction | ||||||
| Noise level dB | 94.5 dB | 85.3 dB | 9.6 dB | ||||||
| TWA dB | 95.4 | 91.8 | 3.4 dB | ||||||
| Dose % (OSHA) | 112.9 | 73.5 | 39.5 | ||||||
| Dose % (MSHA PEL) | 207.8 | 117.6 | 90.1 | ||||||
MSHA = Mine Safety and Health Administration
OSHA = Occupational Safety and Health Administration
PEL = permissible exposure limit
9. Results case studies ‐ enclosure.
| Enclosure | |||||
| Noise source | Intervention | Follow‐up | Initial noise level | Noise level after | Reference ID |
| Conveyor | An enclosure was put over the conveyor at a cost of GBP 2000 and the conveyor speed was changed to reduce jar clashing | not reported | 96 dB | 86 dB | HSE 2015 |
| Grinder | Enclosure over the grinder | not reported | 93 dB | 85 dB | Morata 2015 |
| Not reported | Use of an enclosure with acoustical foam to deburring area | not reported | 104 dB | 82 dB | |
| Feeder | Enclosing the bowl feeder | not reported | 116 dB | 86 dB | Maling 2016 |
| Compressed‐air knives | Enclosed machine | not reported | 91–92 dB | Below 85 dB | HSE 2013 |
| Glass‐bottle conveyor | Enclosed the conveyor noise levels | not reported | Above 90 dB | reduced by 2‐8 dB | |
| Blower machine | Enclosed machine using sound‐absorbent panels | not reported | above 90 | Below 90 dB | |
| Bottle‐blowing machines | Machine enclosed and segregated | not reported | 94 dB | 89 dB | |
| Hammer mill | Enclosed in an acoustic booth | not reported | 102 dB | 87 dB | |
| Rinser‐filler‐capper machine | Enclosed machine | not reported | 85 dB | 73 dB | |
| Glass jars clashing together on conveyor | Fitted enclosure and changed conveyor speed | not reported | 96 dB | 86 dB | |
| Bottles banging together on filler infeed conveyor | Fitted covers over conveyor | not reported | 96‐100 dB | 92 dB | |
| Number of cases: 12 | mean before | mean after | mean reduction | ||
| Noise level (dB) | 96.3 dB | 85.5 dB | 11.8 dB | ||
10. Results case studies ‐ maintenance.
| Maintenance | |||||
| Noise source | Intervention | Follow‐up | Initial noise level | Noise level after | Reference ID |
| Dough mixer | Maintenance modifications to a mixing machine | not reported | 94 dB | 91 dB | HSE 2013 |
| Compressed air in soft drinks factory machines | Regular maintenance of machines to reduce noise from air leaks | not reported | High noise levels | Noise levels reduced by 3 to 4 dB | |
| Gearboxes on mixing machine | Lubricating gearboxes | not reported | 80–85 dB | Noise levels reduced by 1.5 dB | |
| Compressed‐air exhausts on vacuum‐wrapping machines | Fitting and maintaining silencers on wrapping machines | not reported | 88–90 dB | Below 85 dB | |
| Number of cases: 4 | mean before | mean after | mean reduction | ||
| Noise level dB | 88.5 dB | 85.7 dB | 3 dB | ||
11. Results case studies ‐ segregation.
| Segregation | |||||
| Noise source | Intervention | Follow‐up | Initial noise level | Noise level after | Reference ID |
| Main production area of bakery | Re‐routing pedestrian traffic, signage and training | not reported | 94 dB | below 85 dB | HSE 2013 |
| Bowl chopper and mincers | Moved from main production area to an isolated area | not reported | 88–94 dB | below 85 dB | |
| Basket‐washing machine in main bakery | Moved to a separate building | not reported | 88 dB | Noise source removed | |
| High‐pressure air‐compressor | Located in a separate room | not reported | 110–112 dB | 60–70 dB outside room | |
| Vibrating cap‐hoppers | Located in separate enclosure | not reported | Above 90 dB | Noise source removed | |
| Air‐compressor | Located in separate, unmanned room | not reported | 94–95 dB | 80 dB | |
| Pet food processing area | Solid block wall with acoustic panelling between processing and packaging area | not reported | 95 dB | Below 85 dB | |
| Number of cases: 7 | mean before | mean after | mean reduction | ||
| Noise level dB | 97.1 dB | 80.0 dB | 17.1 dB | ||
For most cases the country location of the intervention was not reported (78 of 107 cases). Eighteen cases were implemented and evaluated in the USA, three in Australia, three in Iran and one in France.
Study authors reported funding sources for only seven out of 107 cases. Funds came from ALCOA, Strategic Marine, and SVT Engineering Consultants (no grant numbers reported) (Pan 2016), Hamadan University (Golmohammadi 2014), and Eurocopter Ltd (Caillet 2012). Study authors did not report conflict of interest, except for three cases where they declared no conflict of interest (Golmohammadi 2014). Nevertheless study authors reported for 14 cases that the outcome was evaluated by an acoustical consultant or an employee at the firm where the intervention was evaluated and a conflict of interest was apparent (Caillet 2012; Maling 2016; Wilson 2016).
For most cases (n = 87) the effect of the intervention was measured as change in absolute noise levels. For other cases the personal noise exposure for workers was measured, either as TWA (12) or as PEL exposure dose (OSHA 2, MSHA PEL 10, NIOSH 2, other 1).
Study authors reported information on the collection of the noise data only for 16 of the cases and on the measurement device settings only for eight of the cases. Study authors reported that noise data for those eight cases was collected A‐weighted with a slow response with four of those cases using a 5 dB exchange rate.
Most cases evaluated design changes (n = 41), followed by installing damping material and silencers (n = 20), purchasing new equipment (n = 14), the use of enclosures (n = 12), acoustic panels and curtains (n = 10), and maintenance only (n = 4).
None of the study authors reported the time of the intervention. Only for a few case studies authors reported the time of follow up (7 of 107 cases). Five cases had an immediate follow‐up (Azman 2012; Caillet 2012; Pan 2016) and two cases a short‐term follow‐up, with one study collecting data for one year (Küpper 2013) and another study reporting that the device was used to drill a total of 253 holes (Azman 2012).
Interventions were mostly evaluated in the manufacturing industry, followed by mining, steel, drilling, helicopter, textile, and paper‐shredding industry. Types of jobs, when reported, included operating machines and driving vehicles.
Excluded studies
See also the 'Characteristics of excluded studies' table.
We excluded one study (Pääkkönen 2005) because most of the data had already been reported in another article (Pääkkönen 1998) and the remainder did not meet the inclusion criteria. Most studies were excluded because they were either not empirical studies or because the authors did not use a control group. We excluded one controlled study on noise reduction in an MRI scanner because only the patients were exposed to the noise and not the healthcare workers (Mechfske 2002). In another study the participants were excluded if they were routinely exposed to occupational noise (Byrne 2011). Other identified studies of noise reduction in occupational settings were either case studies (Jelinic 2005; Knothe 1999; Pingle 2006; Scannell 1998; Stone 1971) or had a cross‐sectional design without pre‐intervention measurements (Chou 2009), consisted of descriptions of a noise abatement strategy but without a control group (as for example Groothoff 1999), or recommended noise reductions without evaluating them (such as Bowes 1990; Golmohammadi 2010; Kardous 2003). For long‐term hearing evaluation we excluded studies that used data from existing databases as control group material (Brühl 1994).
We excluded hearing protection studies that evaluated immediate effects on volunteers or that were not field studies such as Franks 2000; Merry 1992; Toivonen 2002; Williams 2004. We also excluded studies that evaluated the immediate effects of hearing protection but did not use the same workers for the evaluation (Giardino 1996; Neitzel 2005; Reynolds 1990b).
Risk of bias in included studies
The overview of risk of bias, based on the Downs and Black checklist (Downs 1998), is shown in Figure 2 and Figure 3.
2.
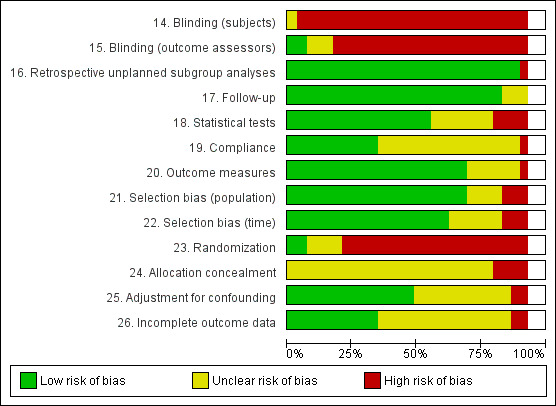
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies. Please note that the blank space corresponds to the studies that have an ITS study design.
3.
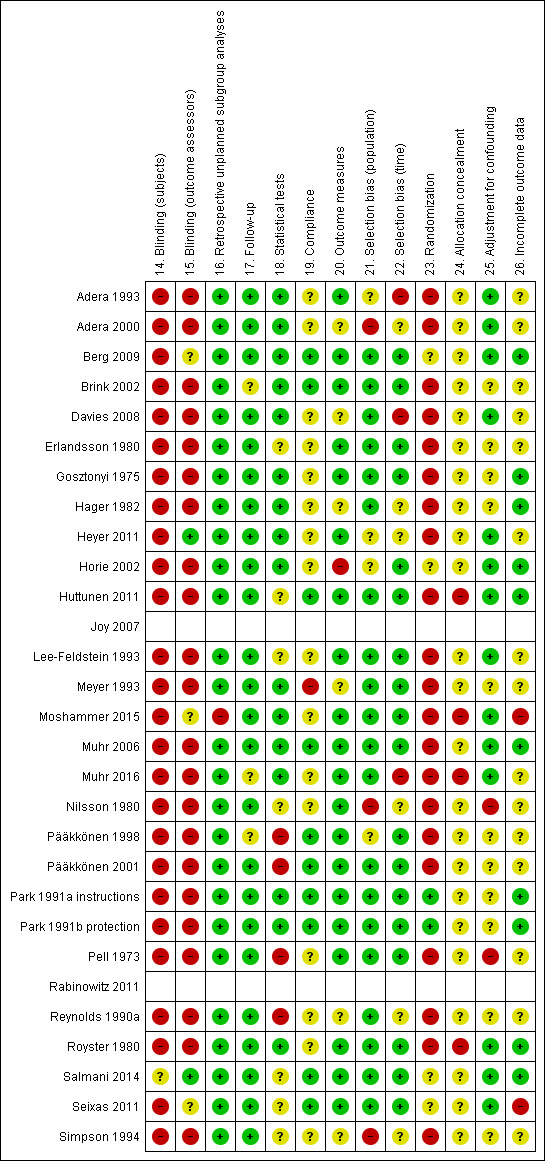
Risk of bias summary: review authors' judgements about each risk of bias item for each included study. Please note that the blank spaces correspond to the studies that have an ITS study design.
Allocation
Four studies randomised participants to intervention and control groups (Berg 2009; Park 1991a instructions; Salmani 2014; Seixas 2011). Of these only one study properly described the randomisation process (Park 1991a instructions). Salmani 2014 indicated using random number tables but not how these were used and the authors did not provide an explanation. None of the included studies reported allocation concealment.
Confounding and selection bias
For studies measuring hearing loss, the age and hearing loss of the intervention and control group participants should be comparable at baseline. Comparability of both age and hearing loss at baseline could be ascertained in six studies (Davies 2008; Heyer 2011; Lee‐Feldstein 1993; Moshammer 2015; Muhr 2006; Muhr 2016), age only in two studies (Berg 2009; Gosztonyi 1975) and hearing loss only in one study (Pell 1973), and neither age nor hearing loss in one study (Hager 1982). In Pell 1973 there was a difference of 10 years between the protected and the non‐exposed group, artificially increasing the risk in the non‐exposed group. In Hager 1982 there was a 7.8 dB difference in hearing level at entry to the study between the protected and non‐exposed group, thus artificially increasing the risk in the protected group. In Lee‐Feldstein 1993 and Pell 1973 the non‐exposed group still had considerable exposure and could thus have confounded an effect of the intervention programme. One study recruited participants from different time periods for control and intervention groups (Muhr 2016). Thus, according to our judgment, only three long‐term evaluation studies had a low risk of confounding and selection bias.
Blinding
Only two studies reported blinded outcome assessment leading to our assessment of a low risk of bias (Heyer 2011; Salmani 2014).
Incomplete outcome data
Most study authors did not report the loss of follow‐up or had a loss of more than 20%. Only nine studies had a low risk of bias in this domain (Berg 2009; Gosztonyi 1975; Hager 1982; Huttunen 2011; Muhr 2006; Park 1991a instructions; Park 1991b protection; Royster 1980; Salmani 2014).
Selective reporting
We did not formally test for reporting bias. However as many studies were funded or carried out by professionals that were part of the company where the intervention took place it can be assumed that they had an interest in reporting favourable results. We considered it conceivable that the results of the studies were biased towards a positive outcome. Horie 2002 and Royster 1980 did not provide SDs and were thus at risk for outcome reporting bias.
Other potential sources of bias
One of the two ITS studies met three of the seven risk of bias criteria, which means that there was considerable risk of bias in the study (Joy 2007). The most serious risk of bias was that the intervention and the outcome measurements were not independent. The number of inspections on which the noise measurement data are based increased after the intervention and might also have included workplaces with lower noise levels that were not previously included (Table 20). The other ITS study met five of the seven criteria and thus we judged it to have a low risk of bias overall (Rabinowitz 2011).
12. Risk of bias of interrupted time‐series.
| Study | Independence other changes | Sufficient data points | Formal test for trend | Intervention does not affect data | Blinded assessment of outcome | Complete data set | Reliable outcome measure |
| Joy 2007 | Not done | Done | Done | Not done | Not done | Not clear | Done |
| Rabinowitz 2011 | Not done | Done | Done | Done | Not Done | Done | Done |
Overall risk of bias per study
Most studies scored poorly on all aspects of the checklist. Six studies (four well‐designed CBA studies and two well‐designed RCTs) achieved more than 50% of the maximum score of 13 on the internal validity scale of the checklist and we considered them to be at low risk of bias overall (Berg 2009; Horie 2002; Huttunen 2011; Muhr 2006; Park 1991a instructions; Salmani 2014).
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8
1 Effect on noise exposure
1.1 Immediate and short‐term follow‐up (noise reduction)
1.1.1 Engineering controls following legislation
Legislation in the mining industry (ITS)
We found one study that indirectly measured the effect of legislation on the decrease of noise levels. We assumed that the effect was mediated by better engineering controls. The content of legislation was directed at better compliance with the law with primacy for engineering and administrative controls.
Outcome: noise exposure (dB)
In the Joy 2007 study, in which legislation was introduced to reduce noise levels in the mining industry, the immediate effect of introducing changes in surface mining locations in the year 2000 was a 27.7 percentage points reduction in the median noise dose level (95% confidence interval (CI) −36.10 to −19.30 percentage points) compared to that predicted by extrapolation of the pre‐intervention slope (Analysis 1.1). The noise dose was measured as a permissible exposure level (PEL) dose percentage. Given a predicted post‐intervention level of 58.7 PEL dose and a measured level of 31 PEL dose, this means a change from 86.1 dB(A) to 81.6 dB(A) or a 4.5 dB(A) decrease.
1.1. Analysis.
Comparison 1 Legislation to decrease noise exposure (long‐term) ‐ ITS, Outcome 1 Immediate change in level.
For the underground mining noise levels the immediate effect was −16.8 noise dose percentage points (95% CI −23.5 to −10.1 percentage points). Given a predicted post‐intervention level of 79.8 PEL dose and a measured level of 63 PEL dose, this means a change from 88.3 dB(A) to 86.7 dB(A).
Taking 1999 as the year in which the change of legislation was implemented, the immediate effect is smaller but the change of slope larger and significant. We rated the overall quality of evidence as very low (see Table 1).
1.1.2 Personal hearing protection devices
a) Hearing protection devices with instructions versus without instructions
Earmuffs with instruction versus without instruction (RCT, immediate)
Outcome: noise attenuation (REAT, dB(A) at one frequency)
The use of earmuffs with instructions compared to no instructions increased noise attenuation, measured as REAT, at 0.5 kHz, 1 kHz, 2 kHz, 3 kHz, 4 kHz, 6 kHz, and 8 kHz but the effect was non‐significant (Park 1991a instructions, Analysis 2.1; Analysis 2.2; Analysis 2.3; Analysis 2.4; Analysis 2.5; Analysis 2.6; Analysis 2.7). Noise attenuation at 4 kHz increased slightly but non‐significantly after instruction with 0.83 dB (95% CI −3.28 dB to 4.95 dB) for two different types of earmuffs (Analysis 2.5). We rated the quality of evidence as moderate.
2.1. Analysis.
Comparison 2 HPD (muffs) with instructions vs without instructions (immediate) ‐ RCT, Outcome 1 Noise attenuation at 0.5 kHz (REAT).
2.2. Analysis.
Comparison 2 HPD (muffs) with instructions vs without instructions (immediate) ‐ RCT, Outcome 2 Noise attenuation at 1 kHz (REAT).
2.3. Analysis.
Comparison 2 HPD (muffs) with instructions vs without instructions (immediate) ‐ RCT, Outcome 3 Noise attenuation at 2 kHz (REAT).
2.4. Analysis.
Comparison 2 HPD (muffs) with instructions vs without instructions (immediate) ‐ RCT, Outcome 4 Noise attenuation at 3 kHz (REAT).
2.5. Analysis.
Comparison 2 HPD (muffs) with instructions vs without instructions (immediate) ‐ RCT, Outcome 5 Noise attenuation at 4 kHz (REAT).
2.6. Analysis.
Comparison 2 HPD (muffs) with instructions vs without instructions (immediate) ‐ RCT, Outcome 6 Noise attenuation at 6 kHz (REAT).
2.7. Analysis.
Comparison 2 HPD (muffs) with instructions vs without instructions (immediate) ‐ RCT, Outcome 7 Noise attenuation at 8 kHz (REAT).
Earplugs with instruction versus without instruction (RCT, immediate)
Outcome: noise attenuation (REAT, dB(A) at one frequency)
The use of earplugs with instructions compared to no instructions significantly increased noise attenuation at 0.5 kHz, 1 kHz, 2 kHz, 3 kHz, 4 kHz, 6 kHz, and 8 kHz, measured as REAT (Park 1991a instructions; Analysis 3.1; Analysis 3.2; Analysis 3.3; Analysis 3.4; Analysis 3.5; Analysis 3.6; Analysis 3.7). Noise attenuation at 4 kHz significantly increased with 7.97 dB (95% CI 3.60 dB to 12.34 dB) for two different types of earplugs (Analysis 3.5). We rated the quality of evidence as moderate.
3.1. Analysis.
Comparison 3 HPD (plugs) with instructions vs without instructions (immediate) ‐ RCT, Outcome 1 Noise attenuation at 0.5 kHz (REAT).
3.2. Analysis.
Comparison 3 HPD (plugs) with instructions vs without instructions (immediate) ‐ RCT, Outcome 2 Noise attenuation at 1 kHz (REAT).
3.3. Analysis.
Comparison 3 HPD (plugs) with instructions vs without instructions (immediate) ‐ RCT, Outcome 3 Noise attenuation at 2 kHz (REAT).
3.4. Analysis.
Comparison 3 HPD (plugs) with instructions vs without instructions (immediate) ‐ RCT, Outcome 4 Noise attenuation at 3 kHz (REAT).
3.5. Analysis.
Comparison 3 HPD (plugs) with instructions vs without instructions (immediate) ‐ RCT, Outcome 5 Noise attenuation at 4 kHz (REAT).
3.6. Analysis.
Comparison 3 HPD (plugs) with instructions vs without instructions (immediate) ‐ RCT, Outcome 6 Noise attenuation at 6 kHz (REAT).
3.7. Analysis.
Comparison 3 HPD (plugs) with instructions vs without instructions (immediate) ‐ RCT, Outcome 7 Noise attenuation at 8 kHz (REAT).
Outcome: noise attenuation (REAT, mean dB(A) over frequencies 0.5 kHz, 1 kHz, 2 kHz, 3 kHz, 4 kHz, 6 kHz, 7 kHz, and 8 kHz)
The use of earplugs with instructions compared to no instructions significantly increased the mean noise attenuation over 0.5 kHz, 1 kHz, 2 kHz, 3 kHz, 4 kHz, 6 kHz, 7 kHz, and 8 kHz by 8.59 dB (95% CI 6.92 to 10.25; I² = 0%) (Park 1991a instructions; Salmani 2014; Analysis 3.8).
3.8. Analysis.
Comparison 3 HPD (plugs) with instructions vs without instructions (immediate) ‐ RCT, Outcome 8 Mean noise attenuation over 0.5, 1, 2, 3, 4, 6, 8 kHz (REAT).
Earplugs with instructions versus earplugs without instructions but a higher noise reduction rate
Outcome: noise attenuation (REAT, mean dB(A) over frequencies 0.5 kHz, 1 kHz, 2 kHz, 3 kHz, 4 kHz, 6 kHz, 7 kHz, and 8 kHz)
The use of earplugs with instructions compared to earplugs with a higher noise reduction rate but without instructions significantly increased the mean noise attenuation over 0.5 kHz, 1 kHz, 2 kHz, 3 kHz, 4 kHz, 6 kHz, 7 kHz, and 8 kHz by 2.62 dB (95% CI 1.75 to 3.49) (Salmani 2014; Analysis 4.1).
4.1. Analysis.
Comparison 4 HPD (plugs) lower noise reduction rate (NRR) with instructions vs higher NRR without instructions (immediate) ‐ RCT, Outcome 1 Mean attenuation at 0.5, 1, 2, 3, 4, 6, 8 kHz.
b) Hearing protection versus alternative hearing protection
Hearing protection with noise cancelling devices versus hearing protection without noise cancelling devices (CBA, immediate)
Outcome: noise attenuation (MIRE, dB(A))
The installation of active noise cancellation in the same hearing protector increased the total noise reduction (measured with MIRE) from 17 dB(A) to 25 dB(A) in one helmet and from 20 dB(A) to 24 dB(A) in another helmet (Pääkkönen 2001, Analysis 5.1).
5.1. Analysis.
Comparison 5 HPD with ANC vs without ANC (immediate), Outcome 1 Noise attenuation (dB).
Earplugs with higher noise reduction rates versus earplugs with lower noise reduction rates (CBA, immediate)
Outcome: mean noise attenuation (REAT, dB over frequencies 0.125 kHz to 8 kHz)
Earplugs with a higher noise reduction rate compared to earplugs with a lower noise reduction rate increased noise attenuation by 3.1 dB(A) (95% CI 1.12 to 5.08) (Huttunen 2011; Analysis 6.1).
6.1. Analysis.
Comparison 6 Custom‐moulded musician HPD (plugs) with higher versus HPD (plugs) with lower noise attenuation, Outcome 1 Noise attenuation dB(A).
Noise attenuation of various hearing protection devices (RCT, CBA)
Outcome: noise attenuation (dB)
In the RCT and with fitting instructions, the EAR plug had a 17 dB higher noise attenuation than the Bilsom muff at 0.5 kHz and 16 dB at 1 kHz, and outperformed the other plug and muff at all other frequencies (Park 1991b protection).
For peak noise, the noise attenuation ranged between 22 dB (SD 14) and 27 dB (SD 16) for six different types of hearing protectors but none of the differences were significant (Pääkkönen 1998, Analysis 7.1).
7.1. Analysis.
Comparison 7 HPD (various) noise attenuation (immediate), Outcome 1 Noise attenuation (dB).
1.1.3 Hearing loss prevention programmes (HLPP)
Hearing loss prevention training with noise level indicators versus training only (RCT, four‐month follow‐up)
Outcome: noise level (Leq dB(A))
In Seixas 2011, we compared the change in noise level of two intervention groups to one control group. The comparison was basic information plus extensive information in so called tool‐box sessions plus personal noise‐level indicators or basic information plus personal noise level indicators versus basic information only. We entered the two interventions as subgroups in one comparison. Noise level indicators with or without information did not show a significant effect in lowering the sound pressure level compared to the group receiving information only. At two months, the noise level decreased 0.32 dB more in the control group (95% CI −2.44, 3.08) but at four months' follow‐up the noise levels in the intervention group decreased 0.14 dB more than in the control group (95% CI −2.66 to 2.38) but neither were statistically significant (Analysis 8.1; Analysis 8.2).
8.1. Analysis.
Comparison 8 HLPP with noise level indicator vs no noise level indicator, Outcome 1 Change in noise levels at 2 months' follow‐up.
8.2. Analysis.
Comparison 8 HLPP with noise level indicator vs no noise level indicator, Outcome 2 Change in noise levels at 4 months' follow‐up.
Extensive information versus information only (RCT, four‐month follow‐up)
Outcome: noise level (Leq dB(A))
In the same study (Seixas 2011), noise levels of workers who received additional extensive information in four tool‐box sessions were compared to those of workers who received one baseline information session only but there were no significant differences. The noise level decreased 1.7 dB more in the information‐only control group at two months (95% CI −1.24 to 4.64) but 0.3 dB less at four months (95% CI −2.31 to 2.91) compared to the intervention group (Analysis 9.1; Analysis 9.2).
9.1. Analysis.
Comparison 9 HLPP with extensive information vs information only, Outcome 1 Change in noise levels at 2 months' follow‐up.
9.2. Analysis.
Comparison 9 HLPP with extensive information vs information only, Outcome 2 Change in noise levels at 4 months' follow‐up.
1.2 Long‐term follow‐up (noise reduction)
1.2.1 Engineering controls, legislation
Legislation in the mining industry (ITS)
The same study that measured immediate effects of legislation change also measured the impact of the intervention on the trend over time.
Outcome: noise exposure (dB)
In the Joy 2007 study, in which legislation was introduced to reduce noise levels in the mining industry, the long‐term effect in the change of trend in time as measured by the change in slope before and after the intervention was −2.1 PEL dose percentage points per year but this was not statistically significant (95% CI −4.9 to 0.7 points) (Analysis 1.2). For the underground mining noise levels the long‐term effect was −3.8 PEL dose points per year (95% CI −6.2 to −1.4 dB). Taking 1999 as the year in which the change of legislation was implemented, the immediate effect is smaller but the change of slope larger and significant. We rated the overall quality of evidence as very low (see Table 1).
1.2. Analysis.
Comparison 1 Legislation to decrease noise exposure (long‐term) ‐ ITS, Outcome 2 Change in slope.
2 Effect on hearing loss
2.1 Short‐term follow‐up (temporary hearing loss)
2.1.1 Personal hearing protection devices
a) Hearing protection versus alternative hearing protection
Hearing protection with noise cancelling devices versus hearing protection without noise cancelling devices (CBA)
Outcome: TTS (dB at single frequencies 1 kHz, 2 kHz, 4 kHz, 6 kHz and 8 kHz)
Protectors with noise cancellation compared to protectors without noise cancellation resulted in less temporary hearing loss at the frequencies 1 kHz, 2 kHz, 4 kHz, 6 kHz and 8 kHz (Horie 2002, Analysis 5.2; Analysis 5.3; Analysis 5.4; Analysis 5.5; Analysis 5.6 ). The average temporary hearing loss at 4 kHz was 11.2 dB for conventional protectors without cancellation devices and 5.8 dB for different protectors with noise cancellation (Analysis 5.4). The study did not provide SDs and the statistical significance is unclear.
5.2. Analysis.
Comparison 5 HPD with ANC vs without ANC (immediate), Outcome 2 TTS at 1 kHz (before exposure ‐ after exposure ).
5.3. Analysis.
Comparison 5 HPD with ANC vs without ANC (immediate), Outcome 3 TTS at 2 kHz (before exposure ‐ after exposure ).
5.4. Analysis.
Comparison 5 HPD with ANC vs without ANC (immediate), Outcome 4 TTS at 4 kHz (before exposure ‐ after exposure ).
5.5. Analysis.
Comparison 5 HPD with ANC vs without ANC (immediate), Outcome 5 TTS at 6 kHz (before exposure ‐ after exposure ).
5.6. Analysis.
Comparison 5 HPD with ANC vs without ANC (immediate), Outcome 6 TTS at 8 kHz (before exposure ‐ after exposure ).
Earplug versus alternative earplug (RCT, CBA)
Outcome: TTS (dB at single frequencies 0.5 kHz, 1 kHz, 2 kHz, 3 kHz, 4 kHz and 6 kHz)
In one study, the EAR plug users had less TTS than those wearing another plug (V‐51‐R) which, according to the study authors, was significant but we could not check it due to missing standard deviations (Royster 1980, Analysis 10.1; Analysis 10.2; Analysis 10.3; Analysis 10.4; Analysis 10.5; Analysis 10.6).
10.1. Analysis.
Comparison 10 V‐51‐R plug versus EAR plug (immediate), Outcome 1 TTS at 0.5 kHz (Hearing loss before exposure ‐ after exposure ).
10.2. Analysis.
Comparison 10 V‐51‐R plug versus EAR plug (immediate), Outcome 2 TTS at 1 kHz (before exposure ‐ after exposure ).
10.3. Analysis.
Comparison 10 V‐51‐R plug versus EAR plug (immediate), Outcome 3 TTS at 2 kHz (before exposure ‐ after exposure ).
10.4. Analysis.
Comparison 10 V‐51‐R plug versus EAR plug (immediate), Outcome 4 TTS at 3 kHz (before exposure ‐ after exposure ).
10.5. Analysis.
Comparison 10 V‐51‐R plug versus EAR plug (immediate), Outcome 5 TTS at 4 kHz (before exposure ‐ after exposure).
10.6. Analysis.
Comparison 10 V‐51‐R plug versus EAR plug (immediate), Outcome 6 TTS at 6 kHz (before exposure ‐ after exposure).
All hearing protectors performed worse than the official attenuation ratings provided by the manufacturers.
2.2 Long‐term follow‐up (permanent hearing loss)
2.2.1 Personal hearing protection devices
a) Hearing protection versus alternative hearing protection
Earmuffs versus earplugs (CBA, three‐year follow‐up)
Outcome: standard threshold shift (STS)
Studies divided workers into high and low noise exposure groups. We did not combine study results in a meta‐analysis because of considerable inconsistency in the results due to one study. Most studies show no difference in preventing permanent hearing loss between earmuffs and earplugs (Erlandsson 1980; Nilsson 1980; Analysis 11.1). We rated the overall quality of evidence as very low.
11.1. Analysis.
Comparison 11 Earmuffs vs earplugs (long‐term), Outcome 1 Hearing loss change over 3 years (4 kHz / STS).
b) More versus less hearing protection device use
Outcome: hearing loss (dB) (CBA, more than two‐year follow‐up)
In one study the authors reported that an increase in the use of hearing protection devices at work in noisy areas from 80% to 90% of the time showed a decrease in hearing loss of 3 dB to 5 dB (Moshammer 2015). The study authors also reported a regression coefficient of −5.342 (95% CI −9.116 to −1.568) from a different and unpublished analysis, which they calculated to be a 0.2 dB to 1.6 dB reduction in hearing loss (additional email conversation). We were not able to recalculate the reported results ourselves from the available data. The difference between the two analyses is unclear.
2.2.2 Hearing Loss Prevention Programmes (HLPPs)
a) Components of HLPPs
HLPP versus audiometric testing only (RCT, more than five‐year follow‐up)
Outcome: standard threshold shift (STS)
Berg 2009 calculated the likelihood of developing a STS. The three‐year and 16‐year follow‐up showed no difference between intervention and control group with an odds ratio (OR) of 0.85 (95% CI 0.29 to 2.44) after three years' follow‐up and 0.94 (95% CI 0.46 to 1.91) after 16 years' follow‐up (Analysis 12.1, Table 5).
12.1. Analysis.
Comparison 12 HLPP vs audiometric testing (agriculture students, long‐term, 3‐year and 16‐year follow‐up) ‐ RCT, Outcome 1 STS.
HLPP with daily noise exposure monitoring and feedback versus audiometric testing only (ITS, five‐year follow‐up)
Outcome: change in mean hearing threshold (dB) at 2 kHz, 3 kHz, and 4 kHz
In Rabinowitz 2011 there was no effect of the programme immediately after introduction (Analysis 13.1). The trend over time showed a significant yearly decrease of the rate of hearing loss, measured as the mean hearing threshold at 2 kHz, 3 kHz, and 4 kHz controlled for differences in age, gender, and baseline hearing, of −1.57 dB (95% CI −2.37 to −0.77) in the intervention group (Analysis 13.2). Similar but smaller improvements over time also occurred in the control group (−0.23 dB per year with 95% CI −0.39 to −0.07). The trend of the difference between the intervention and control group remained significant with −1.35 dB per year for the intervention group (95% CI −2.09 to −0.61).
13.1. Analysis.
Comparison 13 HLPP with daily noise‐exposure monitoring with feedback vs annual audiometry (long‐term) ‐ ITS, Outcome 1 HL (dB/year at 2, 3 and 4 kHz) Δ level.
13.2. Analysis.
Comparison 13 HLPP with daily noise‐exposure monitoring with feedback vs annual audiometry (long‐term) ‐ ITS, Outcome 2 HL (dB/year at 2, 3 and 4 kHz) slope.
The study authors could also control for the initial rate of hearing loss as a potential confounder. The results were similar to the previous comparison but the trend over time for the intervention group minus the control group was no longer significant (−0.82 with 95% CI −1.86 to 0.22) (Analysis 13.2).
The study authors also analysed the data as the mean yearly change in rate of hearing loss before and after the introduction of the intervention but their results were similar to our findings.
Follow‐up examinations after STS versus no follow‐up in one year (CBA, one‐year follow‐up)
Outcome: standard threshold shift (STS)
In one study the OR for sustaining a STS was 0.87 (95% CI 0.56 to 1.36) after having a year of follow‐up examinations versus no examinations (Meyer 1993) (Analysis 14.1).
14.1. Analysis.
Comparison 14 Follow‐up exam after initial STS vs no exam (long‐term), Outcome 1 Hearing loss change (STS).
b) HLPPs compared to other HLPPs
Well‐implemented HLPP versus less well‐implemented HLPP (CBA, one‐year follow‐up)
Outcome: standard threshold shift (STS)
In Simpson 1994, employees in companies with a well‐implemented HLPP ran a lower risk of STS than those in companies with less well‐implemented programmes, with a relative risk of 0.36, which was not significant (95% CI 0.09 to 1.42) (Analysis 15.1).
15.1. Analysis.
Comparison 15 Well‐implemented HLPP vs less well‐implemented (long‐term, 1‐year follow‐up), Outcome 1 STS.
Well‐implemented HLPP versus less well‐implemented HLPP (CBA, more than five‐year follow‐up)
Outcome: standard threshold shift (STS at 4 kHz)
In a meta‐analysis of three studies we estimated the effect as the OR of sustaining a STS during the follow‐up period in workers in companies with a well‐implemented HLPP versus those in companies with less well‐implemented programmes (Adera 1993; Adera 2000; Brink 2002). The OR for the risk of sustaining a STS was 0.40 (95% CI 0.23 to 0.69) (Analysis 16.1) for workers covered by well‐implemented programmes. The results were statistically heterogeneous, with an I² of 66%. We rated the overall quality of evidence as very low (Table 7).
16.1. Analysis.
Comparison 16 Well‐implemented HLPP vs less well‐implemented (long‐term > 5‐year follow‐up), Outcome 1 Hearing loss change STS/at 4 kHz.
Outcome: changes in binaural hearing thresholds at 3 kHz, 4 kHz, and 6 kHz
In Heyer 2011, only one out of three quality aspects of the HLPP was associated with hearing loss. We could not include the data in a meta‐analysis because they were reported as the results of a regression analysis. Years with more than 50% use of hearing protection devices (better quality) caused less hearing loss than years in a HLPP with less than 50% compliance of using hearing protection devices, for men with a beta of −0.31 dB(A) (95% CI −0.37 to −0.24) ) and for women −0.14 dB(A) (95% CI −0.27 to −0.01). The other quality aspect, noise monitoring (men: beta −0.13 dB(A) (95% CI −0.20 to −0.07); women: beta −0.15 dB(A) 95% CI −0.44 to 0.14) showed varying results but was, according to the study authors likely to be confounded by plant. The quality aspects of audiometric testing (men: beta 0.13 dB(A) (95% CI 0.06 to 0.19); women: beta 0.33 dB(A) 95% CI 0.19 to 0.47) and worker training (men: beta −0.04 dB(A) (95% CI −0.10 to 0.02); women: beta −0.05 dB(A) 95% CI −0.18 to 0.07), did not show a significant association with hearing loss.
c) HLPPs compared to less or no exposure
HLPP for 12‐hour shifts versus eight‐hour shifts (CBA, one‐year follow‐up)
Outcome: change in hearing level (dB) at 4 kHz
In one study the mean difference in change in hearing level over one year at 4 kHz for the same HLPP between the 12‐hour shift and 8‐hour shift was −0.68 dB (95% CI ‐1.85 to 0.49) (Reynolds 1990a) (Analysis 17.1).
17.1. Analysis.
Comparison 17 HLPP 12‐hour shift vs HLPP 8‐hour shift (long‐term 1‐year follow‐up), Outcome 1 Hearing loss change over 1 year at 4 kHz.
HLPP versus non‐exposed workers (CBA, one‐year follow‐up)
Outcome: standard threshold shifts (STS), per 100 person‐years
In Muhr 2006 the rate ratio per 100 person‐years of sustaining a STS in the total cohort of recruits was 3.38 (95% CI 1.23 to 9.32) compared to recruits waiting for their training and not exposed. Meta‐analysis results for the subgroups have to be interpreted with caution as the control group in the analysis was split into three parts and the total number of events was small (n = 4) (Analysis 18.1). Results show that the risk of sustaining a STS compared to non‐exposed recruits increased for exposed recruits with the level of exposure from low to high. Separate calculations of the rate ratio for low, medium, and high exposed recruits versus all controls show a rate ratio of 1.55 (95% CI 0.49 to 4.87), 2.12 (95% CI 0.69 to 6.5), and 7.04 (95% CI 2.5 to 19.8) (Table 9).
18.1. Analysis.
Comparison 18 HLPP vs non‐exposed workers (long‐term 1‐year follow‐up), Outcome 1 hearing loss STS.
In Muhr 2016 the rate ratio per 100 person‐years of sustaining a STS in a cohort of high exposed recruits (artillery and armoured vehicle crew members) compared to recruits waiting for their training did not show a difference between the exposed enrolled in the HLPP and the unexposed (RR 1.00, 95% CI 0.48 to 2.11) (Analysis 19.1).
19.1. Analysis.
Comparison 19 Improved HLPP vs non‐exposed workers (long‐term 1‐year follow‐up), Outcome 1 hearing loss STS.
HLPP or hearing protection versus non‐exposed workers (CBA, more than five‐year follow‐up)
Outcome: change in hearing levels (dB) at 4 kHz
In the meta‐analysis of four studies the summary effect size estimate was 0.05 (95% CI −0.05 to 0.16) (Analysis 20.1). When calculated back to a difference in mean changes in hearing level at 4 kHz the result was 0.53 dB (95% CI −0.53 to 1.68) (Gosztonyi 1975; Hager 1982; Lee‐Feldstein 1993; Pell 1973). The results were statistically homogeneous.
20.1. Analysis.
Comparison 20 HLPP vs non‐exposed workers (long‐term > 5‐year follow‐up), Outcome 1 Hearing loss change at 4 kHz/STS (5‐year follow‐up).
We performed a sensitivity analysis by leaving out the Pell 1973 study because of the 10‐year age difference between the intervention and the non‐exposed group, which could explain a difference of 7 dB hearing thresholds (calculated based on ISO 1990). This yielded an effect size of 0.17 (95% CI −0.06 to 0.40) (Analysis 21.1). When calculated back to a difference in mean changes in hearing level at 4 kHz, this resulted in 1.8 dB (95% CI −0.6 to 4.2).
21.1. Analysis.
Comparison 21 HLPP vs non‐exposed sensitivity analysis (long‐term, 5‐year follow‐up), Outcome 1 Hearing loss change at 4kHz / STS.
These results indicate that the workers in a HLPP have equivalent hearing thresholds to the non‐exposed workers. However, the 95% CI includes the possibility of a hearing loss as great as 4.2 dB. This threshold is equivalent to thresholds resulting from five years of exposure to 85 dB(A). Consequently these results do not rule out the risk of hearing loss in protected workers.
Outcome: time to a standard threshold shift (STS)
Davies 2008 measured the time to a STS and compared the hazard ratio (HR) to a non‐exposed group with a result of 2.1 (95% CI 1.26 to 3.49) for workers with exposure of 80 to 85 dB‐years. The HR gradually increased to 6.6 (95% CI 5.56 to 7.84) for workers with an exposure of more than 100 dB‐years. Combined in the meta‐analysis, this yielded a HR of 3.78 (95% CI 2.69 to 5.31) (Analysis 20.2).
20.2. Analysis.
Comparison 20 HLPP vs non‐exposed workers (long‐term > 5‐year follow‐up), Outcome 2 Hazard of STS.
We rated the overall quality of evidence as very low (Table 8).
3. Effects from uncontrolled before after case studies of engineering control interventions
New equipment
A reduction in noise levels with new equipment was reported for fourteen cases.
Outcome: personal noise exposure (Leq eight hours dB(A))
One study reported a decrease in personal daily noise exposure at work based on a case of renovating helicopters. The use of helicopters for rescue operations with advanced technology decreases daily personal noise exposure by 10.51 dB(A) (95% CI 15.45 to 5.57 dB(A), Leq 8 hours) compared to helicopters without this technology (Küpper 2013; Table 9; Table 13).
Outcome: noise level (dB(A))
Study authors reported for the other thirteen cases a mean noise reduction with new equipment of 19.7 dB(A) (HSE 2013; Maling 2016; Morata 2015; Table 13).
Acoustic panels and curtains
Outcome: noise level (dB(A))
In nine cases of application of panels and curtains, study authors reported a mean reduction in noise levels of 11.1 dB (Golmohammadi 2014; HSE 2013; Morata 2015; Table 14).
Damping material and silencers
Outcome: personal noise exposure (eight‐hour TWA dB)
In two cases, damping material and application of silencers reduced the personal noise exposure of workers by 5.5 dB (Thompson 2015; Wilson 2016; Table 15).
Outcome: Mine Safety and Health Administration (MSHA) PEL dose (%)
In three cases the effect was measured as exposure dose (MSHA PEL) and the intervention reduced the dose on average by 60 percentage points.
Outcome: noise level (dB(A))
In another 15 cases, damping material and silencers reduced noise on average by 7 dB (Caillet 2012, HSE 2013; Maling 2016; Morata 2015; Wilson 2016; Table 15).
Design changes
Outcome: personal noise exposure (eight‐hour TWA dB)
Design changes led to a mean decrease in the TWA noise exposure for workers of 3.4 dB in nine cases (Azman 2012; Cockrell 2015; Maling 2016; Thompson 2015; Table 16).
Outcome: Occupational Safety and Health Administration (OSHA) PEL dose (%)
Design changes reduced the noise OSHA PEL dose by 39.5 percentage points in two cases (Cockrell 2015; Table 13).
Outcome: MSHA PEL dose (%)
The design changes decreased MSHA PEL noise dose by 90.1 percentage points in seven cases (Azman 2012; Morata 2015; Thompson 2015; Table 16).
Outcome: noise level (dB(A))
In another 31 cases, authors reported a mean decrease in noise levels of 9.6 dB(A) (HSE 2013; HSE 2015; Maling 2016; Morata 2015; Pan 2016; Thompson 2015; Wilson 2016).
Enclosure
Outcome: noise level (dB(A))
Studies reported a mean noise level reduction of 11.8 dB in 12 cases (HSE 2013; HSE 2015; Maling 2016; Morata 2015; Table 17).
Maintenance
Outcome: noise level (dB(A))
A mean noise level reduction of 3 dB was reported in four cases studies (HSE 2013; Table 18).
Segregation
Outcome: noise level (dB(A))
Studies reported a mean noise level reduction of 17.1 dB in five cases (HSE 2013; Table 19).
Discussion
Summary of main results
Effects on noise exposure
We found 12 studies describing 107 cases of engineering interventions to reduce noise exposures but we could not draw conclusions about the long‐term effects due to the lack of controls and long‐term follow‐up. There was very low‐quality evidence from one study showing that legislation can probably induce technical improvements in the working environment that lead to a relevant reduction in noise exposure levels.
For hearing protection we found an average noise reduction of approximately 20 dB with variation among brands. Noise attenuations achieved under field conditions, however, are lower than indicated ratings provided by the manufacturers. Noise cancellation devices provide some additional noise attenuation in the low frequencies. For peak noise, there were no significant differences in the noise attenuation of several types of hearing protection. There was moderate‐quality evidence that instructions for inserting earplugs into the ear canal have a considerable effect on the noise attenuation of the devices with a 8.6 dB (95% CI 6.9 to 10.3) higher protection averaged across frequencies.
Providing feedback on daily noise exposure or providing on‐site training sessions on noise reduction behaviour did not lead to lower noise‐exposure levels in one cluster RCT.
Effects on hearing loss
The long‐term evaluation of the effect of earmuffs versus earplugs on hearing loss showed that, in high noise levels, earmuffs might perform better than earplugs but in low noise levels the effects were better for plugs (very low‐quality evidence).
One cluster‐RCT did not find an effect of an extensive HLPP in agricultural students at three‐ or 16‐year follow‐up (moderate‐quality evidence).
Very low‐quality evidence of long‐term evaluation studies of components of HLPPs showed that the use of hearing protection devices in a well‐implemented HLPP was associated with less hearing loss. This could not be shown for other elements such as worker training, audiometry alone or noise monitoring by very low‐ and moderate‐quality evidence. More individual information on daily noise exposure as part of a HLPP showed favourable but non‐significant effects on hearing loss in one study.
There was also very low‐quality evidence that, compared to non‐exposed workers in long‐term follow‐up, average HLPPs do not reduce the risk of hearing loss to below a level at least equivalent to that of workers who are exposed to 85 dB(A). We were able to combine some studies in a meta‐analysis and found a hearing loss at 4 kHz of 0.5 dB with an upper confidence limit of 1.7 dB for studies with a five‐year follow‐up. After sensitivity analysis hearing loss was 1.8 dB with an upper limit of 4.2 dB. To be able to asses whether HLPPs are as good as not being exposed to noise we had to make an assumption about the minimal clinically relevant hearing loss. For this we took the hearing loss that is caused by exposure to 85 dB(A) as the minimum amount of damage that should be avoided by protection. Based on ISO 1990 we calculated that the amount of hearing loss after five years of exposure to 85 dB(A) for the median, 10th and 90th percentile would be 4.2 dB, 2.1 dB and 6.1 dB, respectively. Based on Hozo 2005, this is equivalent to a mean of 4.2 dB hearing loss and represents clinically relevant hearing loss. The 95% CI of our meta‐analysis should therefore include zero but not 4.2 to be sure that the hearing losses from the protected and the non‐exposed group are equivalent (Piaggio 2006). After sensitivity analysis, the 95% CI includes 4.2 dB hearing loss, which means that even though there is no significant difference between the protected and the non‐exposed workers, we still cannot be sure that the protected workers are not at risk of a clinically relevant hearing loss. In addition, two other studies that could not be combined in the meta‐analysis still found considerable risks of hearing loss in spite of participants being covered by a HLPP. Another more recent study found no difference between exposed and unexposed workers and concluded that the HLPP was sufficiently improved over time.
Overall completeness and applicability of evidence
It is striking that only one controlled study evaluated measures to reduce noise exposure at the macro‐level. We could not find any controlled studies in which technical measures to reduce noise levels were evaluated at the company level. In a previous version of this review we had already noted that case reports of engineering interventions showed considerable reductions in noise level; for example, 7 dB(A) to 9 dB(A) in Jelinic 2005, 30 dB(A) in Knothe 1999, 3 dB(A) to 22 dB(A) in Pingle 2006, 10 dB(A) to 20 dB(A) in Scannell 1998, 13 dB in Stone 1971, 4 dB(A) to 15 dB(A) in Kavraz 2009, 3 dB(A) in Smith 2006 and Smith 2009. We then concluded that our criterion for controlled studies was too strict in the light of the reductions in sound level that are possible by technical interventions alone. Glasziou 2007 argues that in such cases no control group is necessary. On the other hand, the measurement of noise levels in real working life is not simple and can be biased by many factors such as the worker, the task and the environment, where it is impossible to control all operational and environmental variables. Therefore, in our 2017 update of this review, we systematically searched for uncontrolled studies and extracted data from those that we located. All 107 engineering control intervention cases showed reductions in noise levels or personal noise exposure. Engineering solutions such as new equipment, segregation of noisy equipment, installation of enclosures, and panels or curtains can substantially reduce noise levels, with mean reductions of 19.7 dB, 17.1 dB, 11.8 dB and 11.1 dB respectively. These effects are similar to those of hearing protection devices. This means that engineering interventions can potentially make the use of hearing protection devices in workplaces unnecessary, along with the other components of hearing conservation programmes. As engineering interventions do not depend on training, personal preferences or ear canal anatomy, this is a significant advantage.
However, in most case studies, authors measured environmental noise levels in the immediate surroundings of machinery without reporting a measurement protocol. It is therefore unclear if the measured reductions also represent reductions in personal level noise exposure. Even studies that measured the personal noise exposure of workers as TWA or exposure dose did not report measurement protocols including items such as the place of measurement, the exchange rate and permissible exposure levels used to calculate the outcome. Also here we are uncertain what the exact reductions in personal level noise exposure dose are.
Moreover, a long‐term follow‐up was missing from all but one of the case studies that had a one‐year follow‐up. We believe that for many of the engineering interventions such as panelling or maintenance, the effects could wear off over time and it is necessary to show that these are lasting solutions. We also believe that publication bias as well as conflict of interest issues can have distorted the results. To us, it seems probable that a case study with negative results, not showing a reduction in noise levels, would not so easily make it into a publication as a study with positive results. In many cases, the evaluators had a direct interest in showing that the situation improved and we believe that this creates a conflict of interest. Because there are still so many potential biases in the uncontrolled studies that at least partly would be remediated by a control group and long‐term follow‐up we did not include the case‐studies in our conclusions.
However, the case studies do show that engineering controls are feasible across a range of noise problems and can have a considerable immediate effect on noise exposure. Better reporting of the noise measurements and longer‐term follow‐up would be needed to make them more reliable evidence.
No studies evaluated the effectiveness of the practice of recommendations from occupational health services, national agencies or occupational health professionals to reduce noise levels. A possible but speculative reason for the low number of studies could be the tight regulation regarding noise at work, which makes it difficult to challenge current practice in experiments.
For immediate effects of hearing protection, we restricted our inclusion criteria to field studies among workers and excluded studies that made use of volunteers (Franks 2000; Merry 1992;Williams 2004) or were carried out in a laboratory environment (Toivonen 2002). All of these excluded studies showed a benefit of extra instruction compared to less or no instruction. The increase in attenuation was similar to that found in our review (Park 1991a instructions; Salmani 2014). We only included studies that compared different devices worn by the same workers because the evaluation depends to such a great extent on the wearer. That criterion excluded a great number of studies that evaluated different devices worn by different workers. However this provides us with more reliable results of the effect.
Authors of studies that intended to evaluate a HLPP did not clearly define the programmes. It is unclear if the results are applicable in other settings and if measures to reduce noise levels were taken or if workers got training and education in addition to being provided with hearing protection devices. Only two studies that evaluated a HLPP (or components thereof) used a randomised design. Even though randomised studies are more robust to bias, they did not show beneficial effects of HLPPs. One study was conducted in the construction industry, the other RCT (Berg 2009) managed to follow the participants for many years. It shows that, even though it has often been argued that it is difficult to randomise workers, this is feasible even in difficult sectors such as the construction industry (Seixas 2011).
There were two studies that offered a novel component of a HLPP: monitoring personal noise exposure in a way that the individual worker was made aware of his exposure levels (Rabinowitz 2011; Seixas 2011). Possibly due to small sample sizes neither of them found a significant outcome but given the problems in construction industry with varying noise sources that at least partly can be controlled by the worker, this could be a promising intervention to be tested further in this branch of industry.
Quality of the evidence
The risk of bias was high (especially for the long‐term evaluation studies) because it is difficult to control for the confounding effect of aging and prior hearing loss and most studies were set up retrospectively. Consquently there is a need for better quality studies, which is possible, as demonstrated by the one RCT with long‐term follow‐up that we found. Also the ITS design has potential for evaluating HLPPs because much data is collected routinely. We believe that these studies would provide better‐quality evidence than comparing HLPPs to non‐exposed workers or using a retrospective design.
For the immediate effect evaluation, only two studies used a randomised design, even though it is not too demanding to randomise hearing protection in studies of its immediate effects. Since individual factors, such as the skills necessary to use hearing protection, have an important effect on the outcome, it is important that there are no baseline differences. Randomisation is the only way to ensure this equivalence. Some study authors consider effectiveness to be such a technical matter that they do not even describe the participants in their study.
There was also a lack of information on the implementation level of the prevention measures. This is especially important in the studies that compared well‐implemented HLPPs with those of poorer quality. It is possible to compare different HLPPs or single programme components, or different levels of implementation in a cluster‐randomised design. This would eventually yield much higher‐quality information on the effectiveness of hearing loss prevention. Given the enormous numbers of hearing‐impaired workers, this effort seems justified.
Potential biases in the review process
Even though we made significant efforts to search databases that would contain grey literature, such as NIOSHTIC, we did not have the opportunity to go through all conference proceedings. It is therefore possible that we missed retrospective cohort studies or controlled noise‐reduction studies.
Publication bias could play a role in the results of the evaluation studies of HLPPs, with four of the studies being funded or carried out by people employed by the company responsible for the intervention, who could possibly have an interest in publishing studies demonstrating a preventative effect of HLPPs (Muhr 2006; Muhr 2016).
Agreements and disagreements with other studies or reviews
Berger 1996 reviewed 22 studies that evaluated the field performance of many different types of hearing protection devices (also partly reported in Berger 1998). The main purpose of the included studies was to evaluate the noise attenuation of hearing protection when worn by different workers in field conditions. All these studies concluded that there was great variation among workers leading to large standard deviations in the average attenuation values. This was mainly due to the problem of a lack of fitting instructions and training in fitting the devices (Royster 1996). The inclusion criteria of these studies were therefore essentially different from ours because different workers wore different devices, whereas we only included studies that compared devices among the same subjects. However, the conclusions from all these studies are in agreement: under field conditions the noise attenuation of hearing protection devices is much less than is possible to achieve in the lab and what is indicated by the manufacturer. The inherent lack of precision of the methods used since the late 1970s for determining noise attenuation (used in the labelling of these products) is widely recognised. To address this issue, de‐rating procedures for the reported attenuation values in the labels have been proposed (Franks 2000), and standards have been developed with new strategies for a more accurate determination of the noise attenuation provided in the field (ANSI/ASA 2007; ANSI/ASA 2008; ISO 1999b; ISO 2006). The latest standards incorporate the variance of both the fit of the protector across a population of test subjects and the variance of the protector's performance in a wide range of noise spectra. In the USA, new regulation has been proposed that provides guidance for passive hearing protection devices, active noise reduction devices and also for impulse noise reduction devices such as sound restoration or nonlinear acoustic protectors (Murphy 2008).
One other review concluded that the available evidence from long‐term evaluation studies does not support the effectiveness of HLPPs (Dobie 1995). The author acknowledges that he did not perform a systematic search. He included and commented upon the same two evaluation studies that compared hearing protection users versus non‐users and those that compared protected workers to non‐exposed workers as we included in this review. He included three long‐term evaluation studies, of which two were also included in this review. His conclusions are similar to ours in that the evidence for the effectiveness of HLPPs is not very convincing.
Borchgrevink 2003 reviewed only occupational noise‐induced hearing loss data and because hearing loss still occurred he concluded that HLPPs were ineffective. Daniell 2006 evaluated the quality of HLPPs in companies and concluded that they were commonly incomplete and that consideration of noise control was low in all industries. This concurs with the conclusions of our review. Another narrative review was directed at one sector only (mining) (McBride 2004), but drew similar conclusions.
Authors' conclusions
Implications for practice.
There is one study that shows that legislation can reduce noise‐exposure levels at the branch level. Technical measures can yield similar reductions in noise levels to hearing protection devices but there are, however, no controlled long‐term evaluation studies on implemented technical measures to reduce noise levels in companies, nor on advice to take such measures. Technical measures, therefore, should be the first choice in the management of noise problems at work, especially if the noise reductions lead to a reduction in personal noise doses received by workers. Better implementation and reinforcement of the law could be effective in better implementing technical measures for reducing noise levels.
Hearing protection from various manufacturers showed an immediate effect of noise attenuation of around 20 dB at frequencies 0.5 kHz to 8 kHz under field conditions. This is significantly lower than the attenuation advertised by manufacturers. There was moderate‐quality evidence that personal instructions for the insertion of earplugs are needed to guarantee sufficient noise reduction. If properly inserted, earplugs can provide protection equivalent to earmuffs. There is a great variation in noise attenuation between various hearing protection devices. Active noise cancellation devices and devices with a higher noise‐reduction rate can lead to a moderate additional reduction of noise levels. For noise cancellation devices this has been shown to take place in the lower frequency range.
There was very low‐quality evidence that the use of hearing protection devices in well‐implemented hearing loss prevention programmes (HLPP) was associated with less hearing loss but this could not be shown for other elements, such as worker training or audiometry alone or noise monitoring. More individual information on noise exposure as part of a HLPP showed a favourable but non‐significant effect. There was also very low‐quality evidence that, compared to non‐exposed workers, average HLPPs do not reduce the risk of hearing loss to below a level at least equivalent to that of workers who are exposed to 85 dB(A). It might be that a better‐implemented HLPP could prevent hearing loss in workers at a level comparable to not being exposed at all.
Implications for research.
Research on the long‐term effects of engineering interventions to reduce noise is needed. Even field case studies with valid measurements of personal noise doses of workers with long‐term follow‐up would provide better evidence than what is currently available. The effects of recommendations of measures should preferably be evaluated using a cluster‐randomised design in which companies or departments are randomised to either the intervention or the control group.
Future evaluation studies of the immediate effects of hearing protection should use randomisation and take into account the effects of instruction and field conditions. Also studies that evaluate the effects of engineering control interventions should make use of control conditions or use an interrupted time‐series approach with at least three measurements before and three after the intervention. Noise measurements can be improved by taking into account the known variability in noise levels (ISO 9612:2009) and by adapting the number of measurements accordingly. Studies need to better report the measurement criteria used, especially when calculating time‐weighted averages or exposure doses.
HLPPs should also be evaluated in a cluster‐randomised design, in which programmes with specific components can be compared to programmes without these components. A follow‐up time of five years has been shown to be feasible and should be sufficient to show effects on hearing given the observation that hearing threshold changes at 4 kHz can already occur in the first year of exposure and can be more than 25 dB after two to five years (Sulkowski 2007). A detailed process evaluation could reveal how well the measures were implemented. Studies evaluating HLPPs with innovative content are especially needed in branches of industry where noise exposure is prevalent and difficult to eliminate such as the construction industry or military.
What's new
| Date | Event | Description |
|---|---|---|
| 9 January 2019 | Amended | Missing reference added from study that has been screened and excluded in the 2017 update, Date of assessed as up‐to‐date changed from June to April 2017 (within 6 month of date of search) |
History
Protocol first published: Issue 1, 2007 Review first published: Issue 3, 2009
| Date | Event | Description |
|---|---|---|
| 26 June 2017 | New search has been performed | New citations, conclusions not changed: Search updated. Four new studies included. Overview of uncontrolled engineering control studies added. Methods section improved. |
| 8 May 2012 | New citation required and conclusions have changed | New search and study selection conducted. Four new studies included. Methods improved. Conclusions changed. |
Notes
Disclaimer: The findings and conclusions in this report are those of the author(s) and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
Acknowledgements
We would like to thank the Dutch Ministry of Social Affairs and Employment and the Cochrane Editorial Unit for the grants received to complete and update this review. In addition, we would like to thank Jani Ruotsalainen from Cochrane Work and Jenny Bellorini from Cochrane ENT for their support. We also thank Bas Sorgdrager who contributed to an earlier version of this review.
Appendices
Appendix 1. Search strategy for CENTRAL
#1 MeSH descriptor Noise, Occupational explode all trees with qualifier: PC #2 noise AND (reduction OR abatement OR diminishment OR elimination OR "engineering controls" OR "administrative controls") #3 "hearing loss prevention" OR "hearing conservation" OR "hearing surveillance" #4 "ear protective device" OR "ear protective devices" OR "hearing protective device" OR "hearing protective devices" OR "hearing protector" OR "hearing protectors" OR "hearing protection" OR "ear muffs" OR "ear plugs" OR "ear defenders" #5 ("noise reduction" AND "protective equipment") #6 MeSH descriptor Noise, Occupational explode all trees #7 "protective equipment" #8 (#6 AND #7) #9 (#1 OR #2 OR #3 OR #4 OR #5 OR #8)
2016
#10 (#9) limited to publication year from 2008
Appendix 2. Search strategies for other databases
| PubMed | Embase | CINAHL |
|
2009 #1 noise [tiab] AND (reduction [tiab] OR abatement [tiab] OR diminishment [tiab] OR elimination [tiab] OR "engineering controls" [tiab] OR "administrative controls"[tiab]) #2 "hearing loss prevention" [tiab] OR "hearing conservation" [tiab] OR "hearing surveillance" [tiab] #3 "ear protective device" [tiab] OR "ear protective devices" [tiab] OR "hearing protective device" [tiab] OR "hearing protective devices" [tiab] OR "hearing protector" [tiab] OR "hearing protectors" [tiab] OR "hearing protection" [tiab] OR "ear muffs" [tiab] OR "ear plugs" [tiab] OR "ear defenders" [tiab] #4 ("noise reduction" [tiab] AND "protective equipment" [tiab]) #5 "Noise, Occupational/prevention and control"[Mesh] #6 "Noise, Occupational"[Mesh] #7 "protective equipment" [tiab] #8 #6 AND #7 #9 #1 OR #2 OR #3 OR #4 OR #5 OR #8 #10 (effect*[tiab] OR control*[tiab] OR evaluation*[tiab] OR program*[tiab]) AND (work*[tiab] OR worker*[tiab] OR workplace*[tiab] OR occupation*[tiab] OR prevention*[tiab] OR protect*[tiab]) #11 #9 AND #10 2012 #12 2008:2012[dp] #13 #11 AND #12 2015 #12 "2012"[Date ‐ Publication] : "3000"[Date ‐ Publication] #13 #11 AND #12 2016 #12 "2015/08/21"[Date ‐ Publication] : "3000"[Date ‐ Publication] #13 #11 AND #12 |
2009 1 industrial noise/ 2 (protective adj equipment).tw. 3 1 and 2 4 (noise and (reduction or abatement or diminishment or elimination or (engineering adj controls) or (administrative adj controls))).tw. 5 ((hearing adj loss adj prevention) or (hearing adj conservation) or (hearing adj surveillance)).tw. 6 ((ear adj protective adj device) or (ear adj protective adj devices) or (hearing adj protective adj device) or (hearing adj protective adj devices) or (hearing adj protecto) or (hearing adj protectors) or (hearing adj protection) or (ear adj muffs) or (ear adj plugs) or (ear adj defenders)).tw. 7 ((noise adj reduction) and (protective adj equipment)).tw 8 6 or 4 or 3 or 7 or 5 9 ((effect* or control* or evaluation* or program*) and (work or worker* or workplace* or working or occupation* or prevention* or protect*)).tw. 10 8 and 9 11 10 2012 #1 'industrial noise':de AND [2008‐2012]/py #2 protective NEAR/3 equipment AND [2008‐2012]/py #3 #1 AND #2 AND [2008‐2012]/py #4 noise AND (reduction OR abatement OR diminishment OR elimination OR 'engineering controls' OR 'administrative controls') AND [2008‐2012]/py #5 noise:ab,ti AND (reduction:ab,ti OR abatement:ab,ti OR diminishment:ab,ti OR elimination:ab,ti OR 'engineering controls':ab,ti OR 'administrative controls':ab,ti) AND [2008‐2012]/py #6 'hearing loss' NEAR/5 preventionAND [2008‐2012]/py #7 hearing NEAR/5 conservation AND [2008‐2012]/py #8 'hearing surveillance' AND [2008‐2012]/py #9 #6 OR #7 OR #8 AND [2008‐2012]/py #10 ear NEAR/5 protective AND device* AND [2008‐2012]/py #11 hearing NEAR/3 protect* AND [2008‐2012]/py #12 ear NEAR/1 muff* AND [2008‐2012]/py #13 ear NEAR/1 plug* AND [2008‐2012]/py #14 ear NEAR/1 defender* AND [2008‐2012]/py #15 #10 OR #11 OR #12 OR #13 OR #14 AND [2008‐2012]/py #16 noise NEAR/1 reduct* AND protect* NEAR/1 equipm* AND [2008‐2012]/py #17 #3 OR #4 OR #9 OR #15 OR #16 AND [2008‐2012]/py #18 effect* OR control* OR evaluation* OR program* AND (work OR worker* OR workplace* OR working OR occupation* OR prevention* OR protect*) AND [2008‐2012]/py #19 #17 AND #18 AND [2008‐2012]/py #20 #19 AND [embase]/lim AND [2008‐2012]/py #21 #20 NOT [medline]/lim AND [2008‐2012]/py 2015 same search as in 2012 except change of time span [2008‐2012]/py to [2012‐2015]/py 2016 same search as in 2012 except change of time span [2012‐2015]/py to [2015‐2016]/py |
2009 #1 (noise AND (reduction OR abatement OR diminishment OR elimination OR "engineering controls" OR "administrative controls")) OR "hearing loss prevention" OR "hearing conservation" OR "hearing surveillance" #2 "ear protective device" OR "ear protective devices" OR "hearing protective device" OR "hearing protective devices" OR "hearing protector" OR "hearing protectors" OR "hearing protection" OR "ear muffs" OR "ear plugs" OR "ear defenders" #3 (noise(mh) AND "protective equipment") OR ("noise reduction" AND "protective equipment") #4 (effect* OR control* OR evaluation* OR program*) AND (work* OR worker* OR workplace* OR working OR occupation* OR prevention* OR protect*) #5 (#1 OR #2 OR #3) #6 (#4 AND #5) 2015 same strategy, #7 (#6) results limited to date of publication Jan 2012 ‐ October 2016 |
| BIOSIS/CAB Abstracts | Web of Science | NIOSHTIC/OSH UPDATE |
|
2009 1 (noise and (reduction or abatement or diminishment or elimination or (engineering adj controls) or (administrative adj controls))).tw. 2 ((hearing adj loss adj prevention) or (hearing adj conservation) or (hearing adj surveillance)).tw. 3 ((ear adj protective adj device) or (ear adj protective adj devices) or (hearing adj protective adj device) or (hearing adj protective adj devices) or (hearing adj protecto) or (hearing adj protectors) or (hearing adj protection) or (ear adj muffs) or (ear adj plugs) or (ear adj defenders)).tw. 4 ((noise adj reduction) and (protective adj equipment)).tw 5 ((effect* or control* or evaluation* or program*) and (work or worker* or workplace* or working or occupation* or prevention* or protect*)).tw. 6 4 or 1 or 3 or 2 7 6 and 5 |
2009 #1 TS=(noise AND (reduction OR abatement OR diminishment OR elimination OR "engineering controls" OR "administrative controls")) #2 TS=("hearing loss prevention" OR "hearing conservation" OR "hearing surveillance") #3 TS=("ear protective device" OR "ear protective devices" OR "hearing protective device" OR "hearing protective devices" OR "hearing protector" OR "hearing protectors" OR "hearing protection" OR "ear muffs" OR "ear plugs" OR "ear defenders") #4 #3 OR #2 OR #1 #5 TS=((effect* OR control* OR evaluation* OR program*) AND (work* OR worker* OR workplace* OR working OR occupation* OR prevention* OR protect*)) #6 #5 AND #4 2012 same as search in 2009, added time span 2008‐2012 2016 same as search in 2009, added time span 2012‐2016 #7 (#6) refined by: WEB OF SCIENCE CATEGORIES: ( PUBLIC ENVIRONMENTAL OCCUPATIONAL HEALTH OR ACOUSTICS OR ENGINEERING MECHANICAL OR METALLURGY METALLURGICAL ENGINEERING OR ENGINEERING ENVIRONMENTAL OR MECHANICS OR ENGINEERING MANUFACTURING OR CONSTRUCTION BUILDING TECHNOLOGY OR ENGINEERING MULTIDISCIPLINARY OR TRANSPORTATION OR GEOSCIENCES MULTIDISCIPLINARY OR MEDICINE GENERAL INTERNAL OR OPERATIONS RESEARCH MANAGEMENT SCIENCE OR BEHAVIORAL SCIENCES OR ENGINEERING INDUSTRIAL OR ENGINEERING AEROSPACE OR MEDICINE RESEARCH EXPERIMENTAL OR AGRICULTURE MULTIDISCIPLINARY) |
2009 NIOSHTIC (noise AND (induced OR hearing)) 2012 OSH UPDATE time span 01‐2008 to 01‐2012 Searched in bibliographic databases: International bibliographic, CISDOC, HSELINE, IRRST, NIOSHTIC, NIOSHTIC‐2, RILOSH #1 DC{OUBIB OR OUCISD OR OUHSEL OR OUISST OR OUNIOC OR OUNIOS OR OURILO} #2 GW{noise} #3 GW{induced OR hearing} #4 #2 AND #3 #5 #1 AND #4 #6 PY{2008 OR 2009 OR 2010 OR 2011 OR 2012} #7 #5 AND #6 2015 OSHupdate strategy same as in 2012, change of time span: # 6 PY{2012 OR 2013 OR 2014 OR 2015} 2016 OSHupdate all databases, strategy same as 2012, change of time span: #6 PY{2015 OR 2016} |
Data and analyses
Comparison 1. Legislation to decrease noise exposure (long‐term) ‐ ITS.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Immediate change in level | 1 | immediate change in level (Random, 95% CI) | Totals not selected | |
| 1.1 Surface noise Intervention (Int) Year 1999 | 1 | immediate change in level (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Underground noise Int Year 1999 | 1 | immediate change in level (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Surface noise Int Year 2000 | 1 | immediate change in level (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Underground noise Int Year 2000 | 1 | immediate change in level (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Change in slope | 1 | change in slope (Random, 95% CI) | Totals not selected | |
| 2.1 Surface noise Int Year 1999 | 1 | change in slope (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Underground noise Int Year 1999 | 1 | change in slope (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Surface noise Int Year 2000 | 1 | change in slope (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Underground noise Int Year 2000 | 1 | change in slope (Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 2. HPD (muffs) with instructions vs without instructions (immediate) ‐ RCT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Noise attenuation at 0.5 kHz (REAT) | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 2.34 [‐0.85, 5.54] |
| 1.1 Wilson Sound Ban cap | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 4.1 [‐2.47, 10.67] |
| 1.2 Bilsom UF‐1 muff | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 1.80 [‐1.86, 5.46] |
| 2 Noise attenuation at 1 kHz (REAT) | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 0.89 [‐3.02, 4.80] |
| 2.1 Wilson Sound Ban Cap | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 3.80 [‐3.70, 11.30] |
| 2.2 Bilsom UF‐1 Muff | 1 | 20 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐4.78, 4.38] |
| 3 Noise attenuation at 2 kHz (REAT) | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 2.57 [‐0.23, 5.38] |
| 3.1 Wilson Sound Ban Cap | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 2.70 [‐1.89, 7.29] |
| 3.2 Bilsom UF‐1 Muff | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 2.5 [‐1.05, 6.05] |
| 4 Noise attenuation at 3 kHz (REAT) | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 2.23 [0.09, 4.36] |
| 4.1 Wilson Sound Ban Cap | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 1.60 [‐3.01, 6.21] |
| 4.2 Bilsom UF‐1 Muff | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 2.40 [‐0.01, 4.81] |
| 5 Noise attenuation at 4 kHz (REAT) | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 0.83 [‐3.28, 4.95] |
| 5.1 Wilson Sound Ban Cap | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 0.90 [‐6.18, 7.98] |
| 5.2 Bilsom UF‐1 Muff | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 0.80 [‐4.26, 5.86] |
| 6 Noise attenuation at 6 kHz (REAT) | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 0.64 [‐3.76, 5.04] |
| 6.1 Wilson Sound Ban Cap | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 2.30 [‐7.31, 11.91] |
| 6.2 Bilsom UF‐1 Muff | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐4.75, 5.15] |
| 7 Noise attenuation at 8 kHz (REAT) | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 1.14 [‐3.59, 5.87] |
| 7.1 Wilson Sound Ban Cap | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 2.0 [‐8.13, 12.13] |
| 7.2 Bilsom UF‐1 Muff | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 0.90 [‐4.45, 6.25] |
Comparison 3. HPD (plugs) with instructions vs without instructions (immediate) ‐ RCT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Noise attenuation at 0.5 kHz (REAT) | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 12.69 [7.69, 17.69] |
| 1.1 EAR foam plugs | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 16.30 [5.93, 26.67] |
| 1.2 UltraFit plugs | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 11.6 [5.89, 17.31] |
| 2 Noise attenuation at 1 kHz (REAT) | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 13.31 [8.13, 18.50] |
| 2.1 EAR foam plugs | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 15.40 [5.62, 25.18] |
| 2.2 UltraFit plugs | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 12.5 [6.39, 18.61] |
| 3 Noise attenuation at 2 kHz (REAT) | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 9.62 [4.52, 14.72] |
| 3.1 EAR foam plugs | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 7.90 [‐1.21, 17.01] |
| 3.2 UltraFit plugs | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 10.40 [4.25, 16.55] |
| 4 Noise attenuation at 3 kHz (REAT) | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 6.71 [2.66, 10.76] |
| 4.1 EAR foam plugs | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 6.20 [‐1.54, 13.94] |
| 4.2 UltraFit plugs | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 6.90 [2.15, 11.65] |
| 5 Noise attenuation at 4 kHz (REAT) | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 7.97 [3.60, 12.34] |
| 5.1 EAR foam plugs | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 6.00 [‐1.23, 13.23] |
| 5.2 UltraFit plugs | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 9.10 [3.62, 14.58] |
| 6 Noise attenuation at 6 kHz (REAT) | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 12.13 [6.21, 18.05] |
| 6.1 EAR foam plugs | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 9.2 [‐1.87, 20.27] |
| 6.2 UltraFit plugs | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 13.3 [6.30, 20.30] |
| 7 Noise attenuation at 8 kHz (REAT) | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 11.07 [4.51, 17.64] |
| 7.1 EAR foam plugs | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 7.60 [‐0.97, 16.17] |
| 7.2 UltraFit plugs | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 14.3 [6.11, 22.49] |
| 8 Mean noise attenuation over 0.5, 1, 2, 3, 4, 6, 8 kHz (REAT) | 2 | 140 | Mean Difference (IV, Fixed, 95% CI) | 8.59 [6.92, 10.25] |
| 8.1 Moldex Comets, EN352, USA | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | 8.34 [6.58, 10.10] |
| 8.2 EAR foam plugs | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | 9.8 [0.60, 19.00] |
| 8.3 UltraFit plugs | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | 11.16 [4.87, 17.45] |
Comparison 4. HPD (plugs) lower noise reduction rate (NRR) with instructions vs higher NRR without instructions (immediate) ‐ RCT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean attenuation at 0.5, 1, 2, 3, 4, 6, 8 kHz | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 NRR 20 vs NRR 30 | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | 2.62 [1.75, 3.49] |
Comparison 5. HPD with ANC vs without ANC (immediate).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Noise attenuation (dB) | 1 | 4 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.1 Alpha‐200 series with Active Noise Cancelling | 1 | 2 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Gentex/Bose Active Noise Cancelling | 1 | 2 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 TTS at 1 kHz (before exposure ‐ after exposure ) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3 TTS at 2 kHz (before exposure ‐ after exposure ) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4 TTS at 4 kHz (before exposure ‐ after exposure ) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5 TTS at 6 kHz (before exposure ‐ after exposure ) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6 TTS at 8 kHz (before exposure ‐ after exposure ) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only |
Comparison 6. Custom‐moulded musician HPD (plugs) with higher versus HPD (plugs) with lower noise attenuation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Noise attenuation dB(A) | 1 | 20 | Mean Difference (IV, Random, 95% CI) | 3.10 [1.12, 5.08] |
Comparison 7. HPD (various) noise attenuation (immediate).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Noise attenuation (dB) | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.1 Peltor H61 Muff Elec | 1 | 6 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Peltor H7 Muff Elec | 1 | 6 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 Peltor H6 Muff Elec | 1 | 6 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.4 Bilsom Marksman Muff Elec | 1 | 6 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.5 Silenta Hunter Muff Elec | 1 | 6 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.6 EAR Ultra 9000 Plug | 1 | 6 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 8. HLPP with noise level indicator vs no noise level indicator.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in noise levels at 2 months' follow‐up | 1 | 132 | Mean Difference (IV, Random, 95% CI) | 0.32 [‐2.44, 3.08] |
| 1.1 Extensive information plus NLI vs information only | 1 | 64 | Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐4.37, 3.57] |
| 1.2 Information plus NLI vs Information only | 1 | 68 | Mean Difference (IV, Random, 95% CI) | 1.0 [‐2.84, 4.84] |
| 2 Change in noise levels at 4 months' follow‐up | 1 | 132 | Mean Difference (IV, Fixed, 95% CI) | ‐0.14 [‐2.66, 2.38] |
| 2.1 Extensive information plus NLI vs information only | 1 | 64 | Mean Difference (IV, Fixed, 95% CI) | ‐0.30 [‐3.95, 3.35] |
| 2.2 Information plus NLI vs information only | 1 | 68 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐3.48, 3.48] |
Comparison 9. HLPP with extensive information vs information only.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in noise levels at 2 months' follow‐up | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Change in noise levels at 4 months' follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 10. V‐51‐R plug versus EAR plug (immediate).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 TTS at 0.5 kHz (Hearing loss before exposure ‐ after exposure ) | 1 | 70 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.1 After 8 minutes out of noise | 1 | 18 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 After 14.6 minutes out of noise | 1 | 18 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 After 20 minutes out of noise | 1 | 17 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.4 After 27.2 minutes out of noise | 1 | 17 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 TTS at 1 kHz (before exposure ‐ after exposure ) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 After 8 minutes out of noise | 1 | 18 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 After 14.6 minutes out of noise | 1 | 18 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 After 20 minutes out of noise | 1 | 17 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.4 After 27.2 minutes out of noise | 1 | 17 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 TTS at 2 kHz (before exposure ‐ after exposure ) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 After 8 minutes out of noise | 1 | 18 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 After 14.6 minutes out of noise | 1 | 18 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.3 After 20 minutes out of noise | 1 | 17 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.4 After 27.2 minutes out of noise | 1 | 17 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 TTS at 3 kHz (before exposure ‐ after exposure ) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 After 8 minutes out of noise | 1 | 18 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 After 14.6 minutes out of noise | 1 | 18 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.3 After 20 minutes out of noise | 1 | 17 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.4 After 27.2 minutes out of noise | 1 | 17 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 TTS at 4 kHz (before exposure ‐ after exposure) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 After 8 minutes out of noise | 1 | 18 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 After 14.6 minutes out of noise | 1 | 18 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.3 After 20 minutes out of noise | 1 | 17 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.4 After 27.2 minutes out of noise | 1 | 17 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 TTS at 6 kHz (before exposure ‐ after exposure) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 After 8 minutes out of noise | 1 | 18 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 After 14.6 minutes out of noise | 1 | 18 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 After 20 minutes out of noise | 1 | 17 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.4 After 27.2 minutes out of noise | 1 | 17 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 11. Earmuffs vs earplugs (long‐term).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Hearing loss change over 3 years (4 kHz / STS) | 2 | OR (Random, 95% CI) | Subtotals only | |
| 1.1 High noise exposure > 89 dB(A) | 2 | OR (Random, 95% CI) | 0.80 [0.63, 1.03] | |
| 1.2 Low noise exposure < 89 dB(A) | 2 | OR (Random, 95% CI) | 2.65 [0.40, 17.52] |
Comparison 12. HLPP vs audiometric testing (agriculture students, long‐term, 3‐year and 16‐year follow‐up) ‐ RCT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 STS | 1 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| 1.1 3‐year follow‐up | 1 | Odds Ratio (Fixed, 95% CI) | 0.85 [0.29, 2.44] | |
| 1.2 16‐year follow‐up | 1 | Odds Ratio (Fixed, 95% CI) | 0.94 [0.46, 1.91] |
Comparison 13. HLPP with daily noise‐exposure monitoring with feedback vs annual audiometry (long‐term) ‐ ITS.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 HL (dB/year at 2, 3 and 4 kHz) Δ level | 1 | rate of hearing loss (Random, 95% CI) | Totals not selected | |
| 1.1 intervention ‐ controlled for age, gender, baseline hearing | 1 | rate of hearing loss (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 control ‐ controlled for age, gender, baseline hearing | 1 | rate of hearing loss (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 intervention minus control ‐ controlled for age, gender, baseline hearing | 1 | rate of hearing loss (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 intervention ‐ controlled for age, gender, baseline hearing and initial rate of HL | 1 | rate of hearing loss (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.5 control ‐ controlled for age, gender, baseline hearing and initial rate of HL | 1 | rate of hearing loss (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.6 intervention minus control ‐ controlled for age, gender, baseline hearing and initial rate of HL | 1 | rate of hearing loss (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 HL (dB/year at 2, 3 and 4 kHz) slope | 1 | rate of hearing loss (Fixed, 95% CI) | Totals not selected | |
| 2.1 intervention ‐ controlled for age, gender, baseline hearing | 1 | rate of hearing loss (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 control ‐ controlled for age, gender, baseline hearing | 1 | rate of hearing loss (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 intervention minus control ‐ controlled for age, gender, baseline hearing | 1 | rate of hearing loss (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 intervention ‐ controlled for age, gender, baseline hearing and initial rate of HL | 1 | rate of hearing loss (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.5 control ‐ controlled for age, gender, baseline hearing and initial rate of HL | 1 | rate of hearing loss (Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.6 intervention minus control ‐ controlled for age, gender, baseline hearing and initial rate of HL | 1 | rate of hearing loss (Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 14. Follow‐up exam after initial STS vs no exam (long‐term).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Hearing loss change (STS) | 1 | 1317 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.56, 1.36] |
Comparison 15. Well‐implemented HLPP vs less well‐implemented (long‐term, 1‐year follow‐up).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 STS | 1 | 341 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.36 [0.09, 1.42] |
Comparison 16. Well‐implemented HLPP vs less well‐implemented (long‐term > 5‐year follow‐up).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Hearing loss change STS/at 4 kHz | 3 | 16301 | OR (Random, 95% CI) | 0.40 [0.23, 0.69] |
| 1.1 Adera 2000 | 1 | 15345 | OR (Random, 95% CI) | 0.26 [0.14, 0.47] |
| 1.2 Adera 1993 | 1 | 692 | OR (Random, 95% CI) | 0.35 [0.19, 0.65] |
| 1.3 Brink 2000 | 1 | 264 | OR (Random, 95% CI) | 0.62 [0.40, 0.97] |
Comparison 17. HLPP 12‐hour shift vs HLPP 8‐hour shift (long‐term 1‐year follow‐up).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Hearing loss change over 1 year at 4 kHz | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 18. HLPP vs non‐exposed workers (long‐term 1‐year follow‐up).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 hearing loss STS | 1 | Risk Ratio (Random, 95% CI) | 3.38 [1.23, 9.32] | |
| 1.1 low‐exposed engineers | 1 | Risk Ratio (Random, 95% CI) | 2.07 [0.27, 15.99] | |
| 1.2 medium‐exposed infantry | 1 | Risk Ratio (Random, 95% CI) | 2.82 [0.37, 21.57] | |
| 1.3 high‐exposed artillery | 1 | Risk Ratio (Random, 95% CI) | 4.69 [1.13, 19.51] |
Comparison 19. Improved HLPP vs non‐exposed workers (long‐term 1‐year follow‐up).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 hearing loss STS | 1 | Risk Ratio (Fixed, 95% CI) | Totals not selected | |
| 1.1 high‐exposed artillery | 1 | Risk Ratio (Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 20. HLPP vs non‐exposed workers (long‐term > 5‐year follow‐up).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Hearing loss change at 4 kHz/STS (5‐year follow‐up) | 4 | 2231 | effect size (Fixed, 95% CI) | 0.05 [‐0.05, 0.16] |
| 1.1 Pell hearing loss 10 dB | 1 | 628 | effect size (Fixed, 95% CI) | ‐0.1 [‐0.27, 0.07] |
| 1.2 Pell hearing loss 15 to 35 dB | 1 | 559 | effect size (Fixed, 95% CI) | 0.09 [‐0.11, 0.29] |
| 1.3 Pell hearing loss 40 dB | 1 | 385 | effect size (Fixed, 95% CI) | 0.18 [‐0.06, 0.42] |
| 1.4 Lee‐Feldstein | 1 | 474 | effect size (Fixed, 95% CI) | 0.29 [‐0.07, 0.66] |
| 1.5 Hager | 1 | 43 | effect size (Fixed, 95% CI) | ‐0.1 [‐0.72, 0.52] |
| 1.6 Gosztonyi | 1 | 142 | effect size (Fixed, 95% CI) | 0.15 [‐0.18, 0.48] |
| 2 Hazard of STS | 1 | Hazard Ratio (Random, 95% CI) | 3.78 [2.69, 5.31] | |
| 2.1 80 to 85 dB‐years | 1 | Hazard Ratio (Random, 95% CI) | 2.10 [1.26, 3.49] | |
| 2.2 85 to 90 dB‐years | 1 | Hazard Ratio (Random, 95% CI) | 3.00 [2.27, 3.96] | |
| 2.3 90 to 95 dB‐years | 1 | Hazard Ratio (Random, 95% CI) | 3.30 [2.76, 3.94] | |
| 2.4 95 to 100 dB‐years | 1 | Hazard Ratio (Random, 95% CI) | 4.60 [3.86, 5.48] | |
| 2.5 More than 100 dB‐years | 1 | Hazard Ratio (Random, 95% CI) | 6.60 [5.56, 7.84] |
Comparison 21. HLPP vs non‐exposed sensitivity analysis (long‐term, 5‐year follow‐up).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Hearing loss change at 4kHz / STS | 3 | effect size (Fixed, 95% CI) | 0.17 [‐0.06, 0.40] | |
| 1.1 Lee‐Feldstein | 1 | effect size (Fixed, 95% CI) | 0.29 [‐0.07, 0.66] | |
| 1.2 Hager | 1 | effect size (Fixed, 95% CI) | ‐0.1 [‐0.72, 0.52] | |
| 1.3 Gosztonyi | 1 | effect size (Fixed, 95% CI) | 0.15 [‐0.18, 0.48] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Adera 1993.
| Methods | CBA study | |
| Participants | Various occupations n = 692 USA Military | |
| Interventions | Intervention: HLPP in company with apparently good programme (1972‐1981); n = 93 Comparison: HLPP in study company (1980‐1989) with poor programme; n = 599 | |
| Outcomes | STS/100 person‐years ≥ 10 dB in either ear as the mean change at 2, 3 and 4 kHz 9‐year follow‐up | |
| Notes | Long term Comparability ‐ intervention/control: age: adjusted hearing level: ? |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | not blinded |
| 15. Blinding (outcome assessors) | High risk | not blinded |
| 16. Retrospective unplanned subgroup analyses | Low risk | no additional analyses |
| 17. Follow‐up | Low risk | same time period |
| 18. Statistical tests | Low risk | RR (95%CI) |
| 19. Compliance | Unclear risk | not reported |
| 20. Outcome measures | Low risk | audiometry quality reported (STS) |
| 21. Selection bias (population) | Unclear risk | not reported |
| 22. Selection bias (time) | High risk | recruited over different time periods |
| 23. Randomization | High risk | no randomisation |
| 24. Allocation concealment | Unclear risk | no randomisation, not applicable |
| 25. Adjustment for confounding | Low risk | adjusted for age and gender |
| 26. Incomplete outcome data | Unclear risk | not reported |
Adera 2000.
| Methods | CBA study | |
| Participants | Various occupations n = 19,640 USA 1 company | |
| Interventions | Intervention: well‐implemented HLPP in 5 companies; n = 4317, after adjustment for design n = 22 Comparison: HLPP in 1 company with poor quality HLPP; n = 15,323 | |
| Outcomes | STS/100 person‐years ≥ 10 dB in either ear as the mean change at 2, 3 and 4 kHz 5‐year follow‐up | |
| Notes | Long‐term Comparability ‐ intervention/control: age: adjusted hearing: adjusted |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | no blinding |
| 15. Blinding (outcome assessors) | High risk | no blinding |
| 16. Retrospective unplanned subgroup analyses | Low risk | no additional analyses |
| 17. Follow‐up | Low risk | same time period |
| 18. Statistical tests | Low risk | HR model, 95%CI |
| 19. Compliance | Unclear risk | not reported |
| 20. Outcome measures | Unclear risk | STS, audiometry quality not reported |
| 21. Selection bias (population) | High risk | different companies |
| 22. Selection bias (time) | Unclear risk | not reported |
| 23. Randomization | High risk | not randomised |
| 24. Allocation concealment | Unclear risk | not randomised, not applicable |
| 25. Adjustment for confounding | Low risk | adjusted for age, race, hearing loss |
| 26. Incomplete outcome data | Unclear risk | not reported |
Berg 2009.
| Methods | Cluster‐randomised controlled study | |
| Participants | Agricultural students involved in farm work n = 753 USA 34 schools |
|
| Interventions | Intervention: hearing test yearly, instruction once, 11 mailings at home, free hearing protection plus replacements, use of sound meter Control: yearly hearing tests plus questionnaires |
|
| Outcomes | STS with ≥ 10 dB loss at 2, 3, 4 kHz in either ear Median and mean thresholds at 0.5, 1, 2, 3, 4, 5, 6 kHz High‐frequency average (3, 4, 6 kHz) and low‐frequency average (0.5, 1, 2 kHz) thresholds Bulge depth 3‐year and 16‐year follow‐up |
|
| Notes | Long‐term Comparability ‐ intervention/control: mean age: intervention 14.5 years, control 14.6 years hearing: max. threshold (R or L) at 0.5 kHz intervention md 10 dB/control md 5 dB, at 1, 2, 3, 4 kHz intervention/control md 5 dB, at 6 kHz intervention md 15 dB/control md 10 dB |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | no blinding |
| 15. Blinding (outcome assessors) | Unclear risk | not reported |
| 16. Retrospective unplanned subgroup analyses | Low risk | no subgroup analysis |
| 17. Follow‐up | Low risk | RCT |
| 18. Statistical tests | Low risk | multilevel analysis |
| 19. Compliance | Low risk | increase in hearing protector use |
| 20. Outcome measures | Low risk | hearing thresholds, STS |
| 21. Selection bias (population) | Low risk | RCT |
| 22. Selection bias (time) | Low risk | RCT |
| 23. Randomization | Unclear risk | randomisation stated but no method reported |
| 24. Allocation concealment | Unclear risk | no information provided |
| 25. Adjustment for confounding | Low risk | adjustment for baseline differences |
| 26. Incomplete outcome data | Low risk | < 20% |
Brink 2002.
| Methods | CBA study | |
| Participants | Automobile workers n = 264 USA 1 automobile company | |
| Interventions | Intervention: wearing hearing protection > 33% of the time; n = 132 Control: wearing hearing protection < 33% of the time; n = 132 | |
| Outcomes | Hearing thresholds at 0.5, 1, 2, 3, 4 kHz 14‐year follow‐up | |
| Notes | Long‐term Comparability ‐ intervention/control: age: ? hearing: ? |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | no blinding |
| 15. Blinding (outcome assessors) | High risk | no blinding |
| 16. Retrospective unplanned subgroup analyses | Low risk | no additional analyses |
| 17. Follow‐up | Unclear risk | not reported |
| 18. Statistical tests | Low risk | ANOVA |
| 19. Compliance | Low risk | HPD use measured |
| 20. Outcome measures | Low risk | audiometry quality reported (STS) |
| 21. Selection bias (population) | Low risk | same population |
| 22. Selection bias (time) | Low risk | same time |
| 23. Randomization | High risk | no randomisation |
| 24. Allocation concealment | Unclear risk | no randomisation, not applicable |
| 25. Adjustment for confounding | Unclear risk | no difference in age |
| 26. Incomplete outcome data | Unclear risk | not reported |
Davies 2008.
| Methods | CBA study | |
| Participants | Workers in lumber mills during 1979‐1996 who had at least 2 hearing tests n = 22,376 Canada, British Columbia | |
| Interventions | Intervention: hearing conservation programme; n = 16,347 Control: those exposed to < 80 dB‐years plus those at their first hearing test following baseline; n = 6002 estimated from the number of person‐years of 41,357 with 6.8‐year follow‐up | |
| Outcomes | STS: ≥ 10 dB at 2, 3 or 4 kHz in the better ear | |
| Notes | Long‐term Comparability ‐ intervention/control: proportional hazards model to adjust for age and hearing ability at baseline |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | not blinded |
| 15. Blinding (outcome assessors) | High risk | not blinded |
| 16. Retrospective unplanned subgroup analyses | Low risk | no subgroup analyses |
| 17. Follow‐up | Low risk | same time period for cases and controls (dB‐years) |
| 18. Statistical tests | Low risk | multivariable (Cox) regression analyses, HR (95% CI) |
| 19. Compliance | Unclear risk | no information provided |
| 20. Outcome measures | Unclear risk | audiometry quality not reported (hearing thresholds, STS) |
| 21. Selection bias (population) | Low risk | same industry |
| 22. Selection bias (time) | High risk | different time period |
| 23. Randomization | High risk | no randomisation |
| 24. Allocation concealment | Unclear risk | no randomisation, not applicable |
| 25. Adjustment for confounding | Low risk | adjusted for age and hearing loss |
| 26. Incomplete outcome data | Unclear risk | not reported |
Erlandsson 1980.
| Methods | CBA study | |
| Participants | Shipyard workers n = 40 Assembly department n = 26 < 89 dB(A) exposure n = 26 Boiler department n = 24 > 89 dB(A) exposure n = 24 Sweden One shipyard | |
| Interventions | Intervention: those wearing earmuffs; n = 20 Control: those wearing earplugs; n = 30 | |
| Outcomes | Average change in hearing thresholds over 3 years at 2, 3, 4, 6, 8 kHz 3‐year follow‐up | |
| Notes | Long‐term Comparability ‐ intervention/control: age: matched hearing: ? |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | not blinded |
| 15. Blinding (outcome assessors) | High risk | not blinded |
| 16. Retrospective unplanned subgroup analyses | Low risk | no additional analyses |
| 17. Follow‐up | Low risk | same time period |
| 18. Statistical tests | Unclear risk | statistical methods not reported |
| 19. Compliance | Unclear risk | not reported |
| 20. Outcome measures | Low risk | audiometric quality reported (hearing thresholds) |
| 21. Selection bias (population) | Low risk | same population |
| 22. Selection bias (time) | Low risk | same time |
| 23. Randomization | High risk | no randomisation |
| 24. Allocation concealment | Unclear risk | no randomisation, not applicable |
| 25. Adjustment for confounding | Unclear risk | only adjusted for age |
| 26. Incomplete outcome data | Unclear risk | not reported |
Gosztonyi 1975.
| Methods | CBA study | |
| Participants | Various occupations in 1 company n = 142 USA | |
| Interventions | Intervention: HLPP; n = 71 Control: non‐exposed workers; n = 71 | |
| Outcomes | Average change in hearing thresholds over 3 years at 0.5, 1, 2, 3, 4, 6 kHz 5‐year follow‐up | |
| Notes | Long‐term Comparability ‐ intervention/control: age: intervention ‐ md 42.8 years; control ‐ md 43.2 years hearing: ? |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | not blinded |
| 15. Blinding (outcome assessors) | High risk | not blinded |
| 16. Retrospective unplanned subgroup analyses | Low risk | no additional analyses |
| 17. Follow‐up | Low risk | similar time (either 4 or 5 years) |
| 18. Statistical tests | Low risk | only analyses of variance |
| 19. Compliance | Unclear risk | mandatory programme, no measurement |
| 20. Outcome measures | Low risk | audiometry quality reported |
| 21. Selection bias (population) | Low risk | same factory |
| 22. Selection bias (time) | Low risk | same time period |
| 23. Randomization | High risk | no randomisation |
| 24. Allocation concealment | Unclear risk | no randomisation, not applicable |
| 25. Adjustment for confounding | Unclear risk | only adjusted for age |
| 26. Incomplete outcome data | Low risk | no loss |
Hager 1982.
| Methods | CBA study | |
| Participants | Various workers n = 43 USA 1 company | |
| Interventions | Intervention: hearing protection as part of HLPP in company; n = 27 Control: non‐exposed colleagues; n = 16 | |
| Outcomes | Hearing thresholds at entrance minus HT at follow‐up at 0.5, 1, 2, 3, 4, 6 kHz Follow‐up average 5 and 10 years | |
| Notes | Long‐term Comparability ‐ intervention/control: age: ? hearing: intervention 8.1 dB 4 kHz; control 0.3 dB 4 kHz |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | no blinding |
| 15. Blinding (outcome assessors) | High risk | no blinding |
| 16. Retrospective unplanned subgroup analyses | Low risk | no additional analyses |
| 17. Follow‐up | Low risk | same time (5years) |
| 18. Statistical tests | Low risk | t‐test |
| 19. Compliance | Unclear risk | not reported |
| 20. Outcome measures | Unclear risk | audiometry quality not reported |
| 21. Selection bias (population) | Low risk | same factory |
| 22. Selection bias (time) | Unclear risk | control subjects not grouped according to period of time |
| 23. Randomization | High risk | not randomised |
| 24. Allocation concealment | Unclear risk | not randomised, not applicable |
| 25. Adjustment for confounding | Unclear risk | age corrected control group |
| 26. Incomplete outcome data | Low risk | not reported |
Heyer 2011.
| Methods | CBA study (retrospective) | |
| Participants | Workers of 2 automotive plants, 1 food‐processing plant n = 6483 USA |
|
| Interventions | HLPP quality data available
Intervention: years in better‐implemented programme based on (based on more HPD use, better training, better noise monitoring, better audiometry) Control: years in less well‐implemented programme based on same criteria |
|
| Outcomes | Rate of hearing loss increase over 3, 4, 6 kHz both ears between the first and subsequent audiograms | |
| Notes | Long‐term Comparability ‐ intervention/control: age and hearing: adjusted noise exposure: adjusted, based on retrospective noise level assessment |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | not blinded |
| 15. Blinding (outcome assessors) | Low risk | blinded, those evaluating quality of interventions were not aware of audiometric data |
| 16. Retrospective unplanned subgroup analyses | Low risk | no data dredging |
| 17. Follow‐up | Low risk | adjustment for exposure and exposure to intervention |
| 18. Statistical tests | Low risk | GEE analysis |
| 19. Compliance | Unclear risk | measurements very crude |
| 20. Outcome measures | Low risk | audiometry programme |
| 21. Selection bias (population) | Unclear risk | comparison was between rate of change in hearing according to stratified years of employment within estimated component of the programme of a certain quality level for each of the five defined components |
| 22. Selection bias (time) | Unclear risk | plants were followed for different time periods |
| 23. Randomization | High risk | no randomisation |
| 24. Allocation concealment | Unclear risk | no randomisation, not applicable |
| 25. Adjustment for confounding | Low risk | initial hearing loss and age |
| 26. Incomplete outcome data | Unclear risk | not reported |
Horie 2002.
| Methods | CBA study | |
| Participants | Steel industry quality check workers n = 12 Japan 1 company | |
| Interventions | Intervention: hearing protection with active noise cancellation: proactive PA‐3100; n = 12 Control: hearing protection without active noise cancellation; n = 12 | |
| Outcomes | TTS after 4 hours of exposure at 1, 2, 4, 6, 8 kHz (HT after ‐ HT before) (immediate) | |
| Notes | Immediate | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | no blinding |
| 15. Blinding (outcome assessors) | High risk | no blinding |
| 16. Retrospective unplanned subgroup analyses | Low risk | no additional analyses |
| 17. Follow‐up | Low risk | same time |
| 18. Statistical tests | Low risk | MANOVA |
| 19. Compliance | Unclear risk | not reported |
| 20. Outcome measures | High risk | audiometry quality reported but no SDs provided |
| 21. Selection bias (population) | Unclear risk | same company |
| 22. Selection bias (time) | Low risk | same time |
| 23. Randomization | Unclear risk | not randomised |
| 24. Allocation concealment | Unclear risk | not randomised, not applicable |
| 25. Adjustment for confounding | Low risk | same workers |
| 26. Incomplete outcome data | Low risk | no loss |
Huttunen 2011.
| Methods | CBA immediate follow‐up (REAT) Finland Music industry (orchestra) |
|
| Participants | Age, gender, hearing ability not reported n = 10 |
|
| Interventions | Intervention: custom‐moulded musician's ear‐plug ER‐15 by Etymotic Research Inc., Elk Grove Village, IL, USA Control group: custom‐moulded musician's ear‐plug ER‐9 by Etymotic Research Inc., Elk Grove Village, IL, USA |
|
| Outcomes | Noise attenuation: REAT | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | no blinding |
| 15. Blinding (outcome assessors) | High risk | no blinding |
| 16. Retrospective unplanned subgroup analyses | Low risk | no subgroup analysis |
| 17. Follow‐up | Low risk | same time period |
| 18. Statistical tests | Unclear risk | not reported |
| 19. Compliance | Low risk | immediate follow‐up |
| 20. Outcome measures | Low risk | REAT audiometry |
| 21. Selection bias (population) | Low risk | participants as their own controls (REAT) |
| 22. Selection bias (time) | Low risk | same time |
| 23. Randomization | High risk | no randomisation |
| 24. Allocation concealment | High risk | no randomisation |
| 25. Adjustment for confounding | Low risk | participants as their own controls |
| 26. Incomplete outcome data | Low risk | no loss |
Joy 2007.
| Methods | ITS | |
| Participants | Coal mines Workplace measurements n = 142,735 USA Whole mining branch | |
| Interventions | Introduction of new legislation in 1999 becoming effective in 2000: primacy of engineering and administrative controls, establishment of an Action Level of 85 dB(A), hearing conservation programme enrolment starting from 85 dB(A), introduction of statutory hearing loss of 25 dB average over 2, 3 and 4 kHz in either ear | |
| Outcomes | Median of measurements of compliance with PEL, which includes all sound pressure levels from 90 dB(A) to 140 dB(A) with a doubling rate of 5 dB as an 8‐hour TWA | |
| Notes | Outcomes for general noise levels and underground noise levels respectively: 1987: 61 and 65.8 dB, 1988: 55 and 65 dB, 1989: 62 and 63 dB, 1990: 63 and 65.4 dB, 1991: 59 and 69.4 dB, 1992: 54.2 and 73.4 dB, 1993: 63 and 74.9 dB, 1994: 67 and 76 dB, 1995: 58.9 and 68 dB, 1996: 60 and 69.3 dB, 1997: 56.5 and 73 dB, 1998: 48.8 and 74 dB, 1999: 57.1 and 78.2 dB, 2000: 31 and 63 dB, 2001: 23 and 54 dB, 2002: 22 and 50 dB, 2003: 20 and 52 dB, 2004: 20 and 50 dB | |
Lee‐Feldstein 1993.
| Methods | CBA study | |
| Participants | Automobile workers n = 11,435 USA 1 company | |
| Interventions | Intervention: HLPP; n = 11,104, after cluster adjustment n = 97 Control: non‐exposed colleagues; n = 331 | |
| Outcomes | Rate of STS, average change in mean hearing threshold at 2, 3 and 4 kHz in the worst ear follow‐up average 5 years | |
| Notes | Long‐term Comparability ‐ intervention/control: age: adjusted hearing: adjusted |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | not blinded |
| 15. Blinding (outcome assessors) | High risk | not blinded |
| 16. Retrospective unplanned subgroup analyses | Low risk | no additional analyses |
| 17. Follow‐up | Low risk | similar |
| 18. Statistical tests | Unclear risk | not reported |
| 19. Compliance | Unclear risk | not reported |
| 20. Outcome measures | Low risk | audiometry quality reported |
| 21. Selection bias (population) | Low risk | same factory |
| 22. Selection bias (time) | Low risk | same period |
| 23. Randomization | High risk | not randomised |
| 24. Allocation concealment | Unclear risk | not randomised, not applicable |
| 25. Adjustment for confounding | Low risk | adjusted for age and hearing loss |
| 26. Incomplete outcome data | Unclear risk | not reported |
Meyer 1993.
| Methods | CBA study | |
| Participants | Various occupations n = 1377 USA Military | |
| Interventions | Intervention: detailed follow‐up examination after STS; n = 496 Control: no detailed follow‐up; n = 821 | |
| Outcomes | Rate of new STS; before 1990 defined as a change of 20 dB or more at 1, 2, 3 or 4 kHz, after 1990 an average change of 10 dB or more at 2, 3 and 4 kHz in either ear 1‐year follow‐up | |
| Notes | Long‐term Comparability ‐ intervention/control: age: ? hearing: ? |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | not blinded |
| 15. Blinding (outcome assessors) | High risk | not blinded |
| 16. Retrospective unplanned subgroup analyses | Low risk | no additional analyses |
| 17. Follow‐up | Low risk | same follow‐up |
| 18. Statistical tests | Low risk | RR (95% CI) |
| 19. Compliance | High risk | only few got detailed follow‐up |
| 20. Outcome measures | Unclear risk | no audiometry quality reported |
| 21. Selection bias (population) | Low risk | all subjects from the army |
| 22. Selection bias (time) | Low risk | all subjects selected between 1989‐1991 |
| 23. Randomization | High risk | no randomisation |
| 24. Allocation concealment | Unclear risk | no randomisation, not applicable |
| 25. Adjustment for confounding | Unclear risk | not reported |
| 26. Incomplete outcome data | Unclear risk | not reported |
Moshammer 2015.
| Methods | CBA (arc sin transformed linear regression analysis of HPD use on NIHL) Austria Type of industry: steel factory |
|
| Participants | Fitters and welders at a steel factory Age mean 16.4 years, range 14‐19 years Gender, hearing ability not reported Average noise exposure: 90.8 dB(A) (range 85.4‐107.4 dB(A) over 13.3 years (range 2‐23 years) n = 125 |
|
| Interventions | Use of hearing protection, self‐reported percentage of use, geometric mean of responses on questionnaire at 3 annual health examinations when hearing level was measured | |
| Outcomes | Noise‐induced hearing loss at 4 kHz, measured as hearing level at baseline adjusted for age minus hearing level at end of follow‐up adjusted for age (information from the study authors); also the average hearing loss at 2, 3 and 4 kHz was measured | |
| Notes | The study was set up to predict hearing loss based on TTS at start of the study. Participants were selected from a cohort of workers that started as apprentices at the firm between 1982 and 1989, who had at least 2 years of noise exposure and who worked at places that were noisy | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | No blinding; participants chose themselves about wearing or not wearing HPD |
| 15. Blinding (outcome assessors) | Unclear risk | Not clear if audiometrists were aware of HPD use |
| 16. Retrospective unplanned subgroup analyses | High risk | different data analysis and results because of comments on journal article |
| 17. Follow‐up | Low risk | regression analysis includes adjustment for different time of follow‐up (noise years) |
| 18. Statistical tests | Low risk | multivariate analysis |
| 19. Compliance | Unclear risk | self‐reports of use of hearing protectors in noisy areas, unclear how valid |
| 20. Outcome measures | Low risk | NIHL was calculated from thresholds measured with audiogram minus age related HL |
| 21. Selection bias (population) | Low risk | same workplaces, type of work (closed cohort in 1 steel plant) |
| 22. Selection bias (time) | Low risk | workers in I and C started between 1982‐1989 |
| 23. Randomization | High risk | no randomisation, participants chose themselves how often they used HPDs in noisy areas |
| 24. Allocation concealment | High risk | no randomisation |
| 25. Adjustment for confounding | Low risk | adjusted confounders |
| 26. Incomplete outcome data | High risk | > 60% lost to follow‐up |
Muhr 2006.
| Methods | CBA study | |
| Participants | Army conscripts n = 885 conscripted between 1 June 1999 and 1 June 2000 with hearing loss < 20 dB average over 2 and 3 kHz and < 32.5 dB over 4 and 6 kHz or < 25 dB over 2 and 3 kHz and < 20 dB over 4 and 6 kHz Exposure to impulse noise from shooting Sweden Military |
|
| Interventions | Intervention: regular hearing protection; n = 747 Control: non‐exposed waiting for training period; n = 138 |
|
| Outcomes | STS ≥ 15 dB at the best ear at any of 0.25, 0.5, 1, 2, 3, 4, 6 or 8 kHz between baseline and follow‐up hearing test with average follow‐up of 7.5‐11 months | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | no blinding |
| 15. Blinding (outcome assessors) | High risk | no blinding |
| 16. Retrospective unplanned subgroup analyses | Low risk | no additional analyses |
| 17. Follow‐up | Low risk | similar time for controls and study subjects |
| 18. Statistical tests | Low risk | RR (95% CI) |
| 19. Compliance | Low risk | not reported |
| 20. Outcome measures | Low risk | audiometry quality reported |
| 21. Selection bias (population) | Low risk | all subjects recruits of the army |
| 22. Selection bias (time) | Low risk | all from 1999‐2000 |
| 23. Randomization | High risk | no randomisation |
| 24. Allocation concealment | Unclear risk | no randomisation, not applicable |
| 25. Adjustment for confounding | Low risk | age, all male |
| 26. Incomplete outcome data | Low risk | < 20% |
Muhr 2016.
| Methods | CBA study | |
| Participants | Army conscripts (n= 1234) Control group: before military service in 2002‐2004 (n = 839), Intervention group: in military service 2004‐2005 (n = 395), 40 servicemen from the armoured regiment included in the control‐group are also included in the intervention group. Mean age: intervention, 19 years, control, 18 years at enrolment Gender: male Hearing ability: most participants had maximum hearing thresholds of 25 dB for frequencies 0.5 to 8 kHz in both ears at enrolment to study (I 88.4%, C 85.5%) Exposure: intervention group exposed to impulse noise from shooting Sweden Military |
|
| Interventions | Intervention: HLPP including HPDs and administrative controls (n = 395) Control: non‐exposed to military noise, waiting for training period (n = 839) |
|
| Outcomes | STS ≥ 15 dB at 1 or both ears at any of 0.25, 0.5, 1, 2, 3, 4, 6 or 8 kHz between baseline and follow‐up, hearing test with average follow‐up of 8 months (intervention group) and 13 months (control group) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | no blinding |
| 15. Blinding (outcome assessors) | High risk | no blinding |
| 16. Retrospective unplanned subgroup analyses | Low risk | no subgroup analysis, data dredging unlikely |
| 17. Follow‐up | Unclear risk | approximate difference of 5 months in follow‐up between intervention and control, 1.5 times longer for control |
| 18. Statistical tests | Low risk | RR (95%CI) |
| 19. Compliance | Unclear risk | not reported |
| 20. Outcome measures | Low risk | audiometry quality reported |
| 21. Selection bias (population) | Low risk | all subjects recruits to the army |
| 22. Selection bias (time) | High risk | different time periods, 2004/2005 vs 2002‐2004 |
| 23. Randomization | High risk | no randomisation |
| 24. Allocation concealment | High risk | no randomisation |
| 25. Adjustment for confounding | Low risk | Control and intervention groups of similar age and hearing, baseline for other confounders not reported |
| 26. Incomplete outcome data | Unclear risk | loss of follow‐up not reported |
Nilsson 1980.
| Methods | CBA study | |
| Participants | Ship builders; n = 231 Highly exposed group with > 94 dB(A); n = 1838 Low exposed group with < 88 dB(A); n = 1354 Sweden 1 shipyard | |
| Interventions | Intervention: workers wearing earmuffs; n = 1883 Control: workers wearing earplugs; n = 1309 | |
| Outcomes | STS > 10 dB any frequency in either ear per 100 person‐years; frequencies tested: 0.25, 0.5, 1, 2, 3, 4, 6, 8 kHz | |
| Notes | Long‐term Comparability ‐ intervention/control: age: ? hearing: both groups < 35 dB all frequencies |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | not blinded |
| 15. Blinding (outcome assessors) | High risk | not blinded |
| 16. Retrospective unplanned subgroup analyses | Low risk | no subgroup analyses |
| 17. Follow‐up | Low risk | all about 3.3 years' follow‐up |
| 18. Statistical tests | Unclear risk | one sided Chi2 test |
| 19. Compliance | Unclear risk | not reported |
| 20. Outcome measures | Low risk | audiometry quality reported |
| 21. Selection bias (population) | High risk | same factory but different departments with different noise exposure |
| 22. Selection bias (time) | Unclear risk | same time |
| 23. Randomization | High risk | not randomised |
| 24. Allocation concealment | Unclear risk | not randomised, not applicable |
| 25. Adjustment for confounding | High risk | 5 years' difference in average age |
| 26. Incomplete outcome data | Unclear risk | not reported |
Park 1991a instructions.
| Methods | RCT | |
| Participants | Various workers n = 40 USA Several companies | |
| Interventions | Intervention: fitting instructions for earplugs and earmuffs in step‐by‐step procedure; n = 20 Control: instructions on paper as provided by the manufacturer n = 20 | |
| Outcomes | Hearing thresholds with and without protection at 0.5, 1, 2, 3, 4, 6, 8 kHz | |
| Notes | Immediate | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | no blinding |
| 15. Blinding (outcome assessors) | High risk | no blinding |
| 16. Retrospective unplanned subgroup analyses | Low risk | no additional analyses |
| 17. Follow‐up | Low risk | all 3 weeks |
| 18. Statistical tests | Low risk | ANOVA |
| 19. Compliance | Low risk | wearing of HPD checked |
| 20. Outcome measures | Low risk | audiometry quality reported |
| 21. Selection bias (population) | Low risk | same population |
| 22. Selection bias (time) | Low risk | same time |
| 23. Randomization | Low risk | subjects were randomly assigned |
| 24. Allocation concealment | Unclear risk | not reported, not applicable |
| 25. Adjustment for confounding | Unclear risk | not reported |
| 26. Incomplete outcome data | Low risk | no loss |
Park 1991b protection.
| Methods | RCT | |
| Participants | Various workers n = 40 USA Several companies | |
| Interventions | Intervention: 4 different types of hearing protectors: EAR foam plug, Bilsom UF1 earmuff, Ultrafit plug, Wilson Sound Ban Muff; n = 20 Control: earmuffs versus earplugs; n = 20 | |
| Outcomes | Hearing thresholds with and without protection at 0.5, 1, 2, 3, 4, 6, 8 kHz | |
| Notes | Immediate | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | no blinding |
| 15. Blinding (outcome assessors) | High risk | no blinding |
| 16. Retrospective unplanned subgroup analyses | Low risk | no additional analyses |
| 17. Follow‐up | Low risk | all three weeks |
| 18. Statistical tests | Low risk | ANOVA |
| 19. Compliance | Low risk | wearing of HPD checked |
| 20. Outcome measures | Low risk | audiometry quality reported |
| 21. Selection bias (population) | Low risk | same population |
| 22. Selection bias (time) | Low risk | same time |
| 23. Randomization | Low risk | subjects were randomly assigned |
| 24. Allocation concealment | Unclear risk | not reported |
| 25. Adjustment for confounding | Unclear risk | not reported |
| 26. Incomplete outcome data | Low risk | no loss |
Pell 1973.
| Methods | CBA study Prospective | |
| Participants | Various workers n = 1572 n = 628 < 20 dB hearing loss at entrance n = 559 15‐35 dB hearing loss at entrance n = 385 > 40 dB hearing loss at entrance USA 1 company | |
| Interventions | Intervention: HLPP mainly hearing protection; n = 399 Control: non‐exposed colleagues; n = 1173 | |
| Outcomes | Average change in hearing thresholds last‐entrance measurement at 0.5, 1, 2, 3, 4, 6 kHz 5‐year follow‐up | |
| Notes | Long‐term Comparability ‐ intervention/control: average age: intervention ‐ 34 years; control ‐ 43 years hearing: stratified according to HL at start |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | not blinded |
| 15. Blinding (outcome assessors) | High risk | not blinded |
| 16. Retrospective unplanned subgroup analyses | Low risk | no unplanned analyses |
| 17. Follow‐up | Low risk | 5‐year follow‐up |
| 18. Statistical tests | High risk | ANOVA |
| 19. Compliance | Unclear risk | not reported |
| 20. Outcome measures | Low risk | audiometry quality reported |
| 21. Selection bias (population) | Low risk | same factory |
| 22. Selection bias (time) | Low risk | same time |
| 23. Randomization | High risk | not randomised |
| 24. Allocation concealment | Unclear risk | not randomised, not applicable |
| 25. Adjustment for confounding | High risk | difference in mean age was 10 years |
| 26. Incomplete outcome data | Unclear risk | not reported |
Pääkkönen 1998.
| Methods | CBA study | |
| Participants | Shots with 762 Rk 62 rifle n = 5 shots Finland Military | |
| Interventions | Intervention: Hearing Protector Earmuffs: Peltor H61, Peltor H7, Peltor H6, Bilsom Marksman, Silenta Hunter at 156 Lcpeak dB(C); n = 5 | |
| Outcomes | Difference in noise level outside versus inside the protectors | |
| Notes | Immediate | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | not blinded |
| 15. Blinding (outcome assessors) | High risk | not blinded |
| 16. Retrospective unplanned subgroup analyses | Low risk | no additional analysis |
| 17. Follow‐up | Unclear risk | immediate outcome measurement (inside/outside HPD) |
| 18. Statistical tests | High risk | no test used |
| 19. Compliance | Low risk | closely observed use of HPD |
| 20. Outcome measures | Low risk | calibrated measurements |
| 21. Selection bias (population) | Unclear risk | all subjects were military staff |
| 22. Selection bias (time) | Low risk | same day in 1995 |
| 23. Randomization | High risk | not randomised |
| 24. Allocation concealment | Unclear risk | not randomised, not applicable |
| 25. Adjustment for confounding | Unclear risk | not reported |
| 26. Incomplete outcome data | Unclear risk | not reported |
Pääkkönen 2001.
| Methods | CBA study | |
| Participants | Air combat plane n = 2 Finland Military | |
| Interventions | Intervention: noise cancellation on in helmet: Alpha 200 series, Gentex/Bose Control: noise cancellation off Exposure time 8 minutes Leq 104‐106 dB(A) | |
| Outcomes | Difference in noise level outside versus inside the helmets | |
| Notes | Immediate | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | not blinded |
| 15. Blinding (outcome assessors) | High risk | not blinded |
| 16. Retrospective unplanned subgroup analyses | Low risk | no additional analysis |
| 17. Follow‐up | Low risk | immediate outcome (inside outside measurement) |
| 18. Statistical tests | High risk | no statistical tests used |
| 19. Compliance | Low risk | took proper adjustment of helmet into account |
| 20. Outcome measures | Low risk | A‐weighted equivalent sound pressure levels |
| 21. Selection bias (population) | Low risk | same military staff |
| 22. Selection bias (time) | Low risk | probably same time period (compare Pääkönen 1998) but not clearly reported |
| 23. Randomization | High risk | not randomised |
| 24. Allocation concealment | Unclear risk | not randomised, not applicable |
| 25. Adjustment for confounding | Unclear risk | not reported |
| 26. Incomplete outcome data | Unclear risk | not reported |
Rabinowitz 2011.
| Methods | CBA study/ITS (authors provided additional data for ITS analysis) | |
| Participants | Various workers of an aluminium smelter n = 312 |
|
| Interventions | Intervention: daily monitoring of at‐ear noise exposure and regular feedback from supervisors Control: ongoing hearing conservation programme (regulation‐mandated hearing tests, noise measurements, training) |
|
| Outcomes | Median TWA ambient noise exposures Median and range of noise exposures inside hearing protection (intervention group) High frequency hearing threshold levels (2, 3, 4 kHz) Annual rate of hearing loss (dB/year) |
|
| Notes | Long‐term Comparability ‐ intervention/control (matched on age, gender and hearing): age: similar age (within 5 years); intervention mean 48.7 years, control mean 48,6 years hearing: controls matched (control group 1) and highly matched (control group 2): Control group 1: baseline hearing = similar high frequency hearing threshold levels (binaural average of 2, 3 and 4 kHz) (within 5 dB) (intervention, n = I 78; control n = 234) Control group 2: baseline hearing and initial rate of hearing loss during pre‐intervention period (intervention, n = 46; control, n = 138) For risk of bias see Table 20 |
|
Reynolds 1990a.
| Methods | CBA study | |
| Participants | Various workers n = 852 USA 1 company in the chemical industry | |
| Interventions | Intervention: HLPP at 12‐h shifts; n = 272, adjusted for design effect n = 218 Control: HLPP at 8‐h shifts; n = 580 | |
| Outcomes | Average change in hearing thresholds at 0.5, 1, 2, 3, 4, 6 kHz 1‐year follow‐up | |
| Notes | Long‐term Comparability ‐ intervention/control: age: ? hearing: similar loss |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | not blinded |
| 15. Blinding (outcome assessors) | High risk | not blinded |
| 16. Retrospective unplanned subgroup analyses | Low risk | no additional analysis |
| 17. Follow‐up | Low risk | same time length (annual hearing test differences) |
| 18. Statistical tests | High risk | ANOVA, no RR, no CI |
| 19. Compliance | Unclear risk | not reported |
| 20. Outcome measures | Unclear risk | audiometry quality not reported |
| 21. Selection bias (population) | Low risk | same company |
| 22. Selection bias (time) | Unclear risk | each employee's last audiometry test in the same year |
| 23. Randomization | High risk | not randomised |
| 24. Allocation concealment | Unclear risk | not randomised, not applicable |
| 25. Adjustment for confounding | Unclear risk | not reported |
| 26. Incomplete outcome data | Unclear risk | not reported |
Royster 1980.
| Methods | CBA study | |
| Participants | Various occupations n = 70 USA | |
| Interventions | Intervention: V‐51R plug Control: EAR plug | |
| Outcomes | Temporary threshold shift at 0.5, 1, 2, 3, 4, 6 kHz. In 3 subgroups after leaving noise after 8, 14, 6, 20 and 27.2 minutes | |
| Notes | Immediate | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | no blinding |
| 15. Blinding (outcome assessors) | High risk | no blinding |
| 16. Retrospective unplanned subgroup analyses | Low risk | no additional analyses |
| 17. Follow‐up | Low risk | immediate outcomes |
| 18. Statistical tests | Low risk | t‐test |
| 19. Compliance | Unclear risk | not reported |
| 20. Outcome measures | Low risk | audiometry quality reported |
| 21. Selection bias (population) | Low risk | same company |
| 22. Selection bias (time) | Low risk | prospective study |
| 23. Randomization | High risk | alternation |
| 24. Allocation concealment | High risk | not properly randomised |
| 25. Adjustment for confounding | Low risk | similar in age, race, sex |
| 26. Incomplete outcome data | Low risk | 2/72 lost to follow‐up |
Salmani 2014.
| Methods | RCT | |
| Participants | Occupations not reported n = 150 Age: mean ± SD 28.3 ± 5.4 (range: 19–39) years Gender: 42% male Iran |
|
| Interventions | Intervention: earplugs with training in correct methods of wearing and inserting plugs Control group1: earplugs without training Control group 2: earplug with higher noise attenuation without training |
|
| Outcomes | Noise attenuation (REAT) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | Unclear risk | participants knew if they were in the control or intervention group (type of earplug and training) |
| 15. Blinding (outcome assessors) | Low risk | blinding of audiometrist |
| 16. Retrospective unplanned subgroup analyses | Low risk | no subgroup analysis |
| 17. Follow‐up | Low risk | immediate follow‐up |
| 18. Statistical tests | Unclear risk | not reported |
| 19. Compliance | Low risk | immediate follow‐up |
| 20. Outcome measures | Low risk | ANSI |
| 21. Selection bias (population) | Low risk | randomised to intervention or control |
| 22. Selection bias (time) | Low risk | recruited over similar time period (over 1 year) |
| 23. Randomization | Unclear risk | random digit table, procedure not described |
| 24. Allocation concealment | Unclear risk | unconcealed |
| 25. Adjustment for confounding | Low risk | outcome was measured as difference in hearing threshold between with and without earplugs, no baseline differences in age and sex |
| 26. Incomplete outcome data | Low risk | no loss |
Seixas 2011.
| Methods | Both cluster and individually randomised RCT, first 4 work sites got baseline training, then these were cluster‐randomised to tool‐box or no tool‐box training and then individuals were randomised to noise level indicators or no indicators | |
| Participants | Construction workers; various trades n = 176 USA |
|
| Interventions | Many comparisons possible, we choose to compare two interventions considered to be most relevant for practice Intervention 1: baseline training plus noise 'tool box' on‐site training (n = 44) Intervention 2: baseline training plus noise 'tool box' on‐site training plus personal noise level indicator (n = 41) Control: baseline training (n = 46) |
|
| Outcomes | Noise level measured as Leq at 2 and 4 months' follow‐up | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | different interventions at the same site visible |
| 15. Blinding (outcome assessors) | Unclear risk | not reported |
| 16. Retrospective unplanned subgroup analyses | Low risk | no subgroup analyses |
| 17. Follow‐up | Low risk | similar follow‐up |
| 18. Statistical tests | Unclear risk | differences in outcome not tested |
| 19. Compliance | Low risk | NLI checked every week, participating in training course or excluded |
| 20. Outcome measures | Low risk | Leq according to NIOSH criteria |
| 21. Selection bias (population) | Low risk | different intervention groups |
| 22. Selection bias (time) | Low risk | same time |
| 23. Randomization | Unclear risk | methods not reported |
| 24. Allocation concealment | Unclear risk | not reported |
| 25. Adjustment for confounding | Low risk | intention to treat |
| 26. Incomplete outcome data | High risk | reported, no differences between groups, but loss to follow‐up ranged from 20%‐33% |
Simpson 1994.
| Methods | CBA study | |
| Participants | Various occupations in 21 companies n = 13283 USA | |
| Interventions | Intervention: well‐implemented HLPP Control: poor quality HLPP | |
| Outcomes | Rate of STS defined as on average ≥ 10 dB at 2, 3 and 4 kHz in either ear Follow‐up average 1 year | |
| Notes | Long‐term Comparability ‐ intervention/control: age: ? hearing: ? |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 14. Blinding (subjects) | High risk | no blinding |
| 15. Blinding (outcome assessors) | High risk | no blinding |
| 16. Retrospective unplanned subgroup analyses | Low risk | no additional analyses |
| 17. Follow‐up | Low risk | same period (second audiogram fell within time window of 6‐18 months) |
| 18. Statistical tests | Unclear risk | no tests mentioned |
| 19. Compliance | Unclear risk | not reported |
| 20. Outcome measures | Unclear risk | audiometry quality not reported |
| 21. Selection bias (population) | High risk | different companies |
| 22. Selection bias (time) | Unclear risk | not reported |
| 23. Randomization | High risk | not randomised |
| 24. Allocation concealment | Unclear risk | not randomised, not applicable |
| 25. Adjustment for confounding | Unclear risk | not reported |
| 26. Incomplete outcome data | Unclear risk | not reported |
ANOVA = analysis of variance ANSI = American National Standards Institute CBA = controlled before and after (study) CI = confidence interval ? = no information available HL = hearing loss HLPP = hearing loss protection programme HPD = hearing protection device HR = hazard ratio HT = hearing threshold ITS = interrupted time series L = left Leq = equivalent continuous sound level MANOVA = multivariate analysis of variance md = median NIHL = noise‐induced hearing loss NLI = Noise level indicator PEL = permissible exposure level R = right REAT = real ear attenuation at threshold RR = risk ratio STS = standard threshold shift TTS = temporary threshold shift TWA = time‐weighted average
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aybek 2010 | Study design: one measurement per intervention, no before measurement, groups not comparable |
| Bealko 2009 | Study design: cross‐sectional design |
| Bockstael 2008 | Participants: HPD not tested on same participants |
| Bowes 1990 | Intervention and study design: only noise measurements and recommendations, no evaluation of measures taken |
| Brueck 2009 | Study design, intervention, outcome measurement: no work place intervention, laboratory tests and observations |
| Brühl 1994 | Study design: control group taken from database |
| Byrne 2011 | Participants: subjects were excluded if they were routinely exposed to occupational noise |
| Casali 2009 | Outcome: operational performance, no noise or hearing tests |
| Chou 2009 | Study design: cross‐sectional study, no pre‐intervention measurements |
| Franks 2000 | Participants: not a field study with workers |
| Giardino 1996 | Study design: not the same workers using different hearing protection |
| Golmohammadi 2010 | Study design: effect of intervention not evaluated |
| Griest 2008 | Participants and outcome: school‐age children, behaviour change, attitudes and knowledge |
| Groothoff 1999 | Study design: several case studies on noise reduction but no control group |
| Jelinic 2005 | Study design: case study only |
| Kardous 2003 | Study design: case study on noise reduction |
| Karlsmose 2001 | Participants: no noise‐exposed workers included |
| Kavraz 2009 | Study design and exposure: quasi‐experimental, attenuation not measured for the workers over a typical work day/situation (noise duration?, TWA?, high frequencies?, shift dose?) |
| Knothe 1999 | Study design: case study on noise reduction |
| Kotarbinska 2009 | Study design: immediate effect of HPD, but no control group and no comparison of 2 types of HPD on the same workers |
| Lempert 1983 | Study design: no control group, only one measurement before intervention |
| Lutz 2015 | study design: before – after comparison of HPDs on different persons |
| Mechfske 2002 | Participants: noise reduction for patients not for healthcare personnel |
| Merry 1992 | Participants: not a field study with workers |
| Monazzam 2011 | Study design: no measurement after the intervention |
| Mrena 2008 | Study design: two cross‐sectional studies |
| Murphy 2011 | Study design: laboratory results |
| Nair 2009 | Study design: no before measurement |
| Neitzel 2005 | Study design: not the same workers using different hearing protection |
| Neitzel 2008 | Study design and outcome measurement: one measurement before and after intervention, no control group, self reported HPD use |
| Niskanen 2001 | Study design: no control group, not an ITS |
| Oestenstad 2008 | Study design and exposure: retrospective study, control group built from database/recalculation of exposure data |
| Pearlman 2009 | Study design: experimental study in a laboratory |
| Pingle 2006 | Study design: case study only |
| Pääkkönen 2005 | Similar results as in Pääkkönen 1998 Study design: not the same workers using different hearing protection |
| Randolph 2008 | Study design, participants: no control group/ITS, no real workers/workplaces |
| Reeves 2009 | Study design: examples of before‐after measurements but not as time series or with some sort of control |
| Reynolds 1990b | Study design: not the same workers using hearing protection |
| Sataloff 2010 | Study design and participants: cross‐sectional study, no occupational noise exposure |
| Scannell 1998 | Study design: case study on technical noise reducing measures |
| Schaefer 1992 | Study design: case study on technical noise reducing measures |
| Smith 2006 | Study design: no ITS, no control group |
| Smith 2009 | Study design: no CBA measurements, no ITS |
| Smith 2011 | Study design: only one measurement before and one after intervention, no ITS, no control group |
| Stone 1971 | Study design: case study on technical noise reducing measures |
| Toivonen 2002 | Participants: not a field study with workers |
| Tsukada 2008 | Study design: no control group, no ITS |
| Walter 2009 | Study design: no control group, no ITS |
| Waugh 1990 | Outcome: no audiometric measurements, noise measurements before but not after the intervention |
| Williams 2004 | Participants: not a field study with workers |
| Wu 2009 | Study design: no data of controls before intervention |
CBA = controlled before and after HPD = hearing protection device ITS = interrupted time series TWA = time‐weighted average
Differences between protocol and review
For noise measurements, we intended to include only measurements executed according to a written national or international standard in which information on measurement method, time weighting etc. was given. However, this transpired to be an excessively strict criterion. We therefore included all reported noise measurements, with the permission of the editorial base.
For hearing loss measurements, we intended to include only hearing loss measured with a calibrated audiometer and defined by means of a written protocol, which was the case for most studies. However, in some cases this was found to be an excessively strict criterion so we also included audiometric measurements when there was no written protocol reported, with the consent of the editorial base.
We intended to use a qualitative analysis if the data could not be combined in a quantitative way. Instead of the proposed synthesis we used the GRADE approach to rate the quality of the evidence.
Contributions of authors
All: Comment on drafts of protocol and review.
Christina Tikka: Searching, eligibility screening, quality assessment, data extraction, data analysis, update of the text. Christina Tikka is the guarantor of this review.
Jos Verbeek: Protocol development, searching, eligibility screening, quality assessment, data extraction, data analysis, writing and update of the text.
Erik Kateman: Protocol development, searching for trials, eligibility screening, quality assessment of studies, data extraction, review development.
Thais Morata: Searching for studies, eligibility screening, data extraction, and update of the text.
Wouter Dreschler: Eligibility screening and data extraction.
Silvia Ferrite: Eligibility screening and data extraction.
Sources of support
Internal sources
No sources of support supplied
External sources
-
Dutch Ministry of Social Affairs and Employment as part of the KIS programme, Netherlands.
Erik Kateman received a grant of EUR 5000 for the original (2009) version of this review.
-
Cochrane Work formerly known as Cochrane Occupational Safety and Health Review Group, Finland.
Provided support in kind.
-
Stichting Arbouw, Netherlands.
Provided EUR 5000 for Cochrane Work for the 2012 update of the review.
-
Cochrane Editorial Unit, UK.
Provided GBP 5000 to Christina Tikka for the 2017 update.
Declarations of interest
Christina Tikka: None known.
Jos Verbeek: None known.
Erik Kateman: None known.
Thais Morata: None known.
Wouter Dreschler: None known.
Silvia Ferrite: None known.
Edited (no change to conclusions)
References
References to studies included in this review
Adera 1993 {published data only}
- Adera T, Donahue AM, Malit BD, Gaydos JC. An epidemiologic method for assessing the effectiveness of hearing conservation programs using audiometric data. Military Medicine 1993;158(11):698‐701. [PubMed] [Google Scholar]
Adera 2000 {published data only}
- Adera T, Amir C, Anderson L. Use of comparison populations for evaluating the effectiveness of hearing loss prevention programs. American Industrial Hygiene Association Journal 2000;61(1):11‐5. [PubMed] [Google Scholar]
Berg 2009 {published data only}
- Berg RL, Pickett W, Fitz‐Randolph M, Broste SK, Knobloch MJ, Wood DJ, et al. Hearing conservation program for agricultural students: short‐term outcomes from a cluster‐randomised trial with planned long‐term follow‐up. Preventive Medicine 2009;49(6):546‐52. [DOI] [PubMed] [Google Scholar]
- Marlenga B, Linneman JG, Pickett W, Wood DJ, Kirkhorn SR, Broste SK, et al. Randomized trial of a hearing conservation intervention for rural students: long‐term outcomes. Pediatrics 2011;128(5):e1139‐46. [DOI] [PubMed] [Google Scholar]
Brink 2002 {published data only}
- Brink LL, Talbott EO, Burks JA, Palmer CV. Changes over time in audiometric thresholds in a group of automobile stamping and assembly workers with a hearing conservation program. American Industrial Hygiene Association Journal 2002;63(4):482‐7. [DOI] [PubMed] [Google Scholar]
Davies 2008 {published data only}
- Davies H, Marion S, Teschke K. The impact of hearing conservation programs on incidence of noise‐induced hearing loss in Canadian workers. American Journal of Industrial Medicine 2008;51:923‐31. [DOI] [PubMed] [Google Scholar]
Erlandsson 1980 {published data only}
- Erlandsson B, Hakanson H, Ivarsson A, Nilsson P. The difference in protection efficiency between earplugs and earmuffs. An investigation performed at a workplace. Scandinavian Audiology 1980;9(4):215‐21. [DOI] [PubMed] [Google Scholar]
Gosztonyi 1975 {published data only}
- Gosztonyi RE. The effectiveness of hearing protective devices. Journal of Occupational Medicine 1975;17(9):569‐80. [PubMed] [Google Scholar]
Hager 1982 {published data only}
- Hager WL, Hoyle ER, Hermann ER. Efficacy of enforcement in an industrial hearing conservation program. American Industrial Hygiene Association Journal 1982;43(6):455‐65. [DOI] [PubMed] [Google Scholar]
Heyer 2011 {published data only}
- Heyer N, Morata TC, Pinkerton LE, Brueck SE, Stancescu D, Panaccio MP, et al. Use of historical data and a novel metric in the evaluation of the effectiveness of hearing conservation program components. Occupational and Environmental Medicine 2011;68(7):510‐7. [DOI: 10.1136/oem.2009.053801] [DOI] [PubMed] [Google Scholar]
Horie 2002 {published data only}
- Horie S. Improvement of occupational noise‐induced temporary threshold shift by active noise control earmuff and bone conduction microphone. Journal of Occupational Health 2002;44(6):414‐20. [Google Scholar]
Huttunen 2011 {published data only}
- Huttunen KH, Sivonen VP, Poykko VT. Symphony orchestra musicians' use of hearing protection and attenuation of custom‐made hearing protectors as measured with two different real‐ear attenuation at threshold methods. Noise & Health 2011;13(51):176‐88. [DOI] [PubMed] [Google Scholar]
Joy 2007 {published data only}
- Joy G, Middendorf PJ. Noise exposure and hearing conservation in US coal mines, a surveillance report. Journal of Occupational and Environmental Hygiene 2007;4:26‐35. [DOI] [PubMed] [Google Scholar]
Lee‐Feldstein 1993 {published data only}
- Lee‐Feldstein A. Five‐year follow‐up study of hearing loss at several locations within a large automobile company. American Journal of Industrial Medicine 1993;24(1):41‐54. [DOI] [PubMed] [Google Scholar]
Meyer 1993 {published data only}
- Meyer GD, Wirth DB. An evaluation of the U.S. Air Force's detailed follow‐up audiometric examination program. Military Medicine 1993;158(9):603‐5. [PubMed] [Google Scholar]
Moshammer 2015 {published and unpublished data}
- Moshammer H, Kundi M, Wallner P, Herbst A, Feuerstein A, Hutter HP. Author response: comments on TTS as a predictor of noise‐induced hearing loss. Occupational and Environmental Medicine 2015;72(2):160‐1. [DOI] [PubMed] [Google Scholar]
- Moshammer H, Kundi M, Wallner P, Herbst A, Feuerstein A, Hutter HP. Early prognosis of noise‐induced hearing loss. Occupational & Environmental Medicine 2015;72(2):85‐9. [DOI] [PubMed] [Google Scholar]
Muhr 2006 {published data only}
- Muhr P, Månsson B, Hellström PA. A study of hearing changes among military conscripts in the Swedish army. International Journal of Audiology 2006;45:247‐51. [DOI] [PubMed] [Google Scholar]
Muhr 2016 {published and unpublished data}
- Muhr P, Johnson A‐C, Skoog B, Rosenhall U. A demonstrated positive effect of a hearing conservation program in the Swedish armed forces. International Journal of Audiology 2016;55(3):168‐72. [DOI] [PubMed] [Google Scholar]
Nilsson 1980 {published data only}
- Nilsson R, Lindgren F. The effect of long term use of hearing protectors in industrial noise. Scandinavian Audiology 1980;Suppl 12:204‐11. [PubMed] [Google Scholar]
Pääkkönen 1998 {published data only}
- Pääkkönen R, Lehtomaki K, Savolainen S. Noise attenuation of communication hearing protectors against impulses from assault rifle. Military Medicine 1998;163(1):40‐3. [PubMed] [Google Scholar]
Pääkkönen 2001 {published data only}
- Pääkkönen R, Kuronen P, Korteoja M. Active noise reduction in aviation helmets during a military jet trainer test flight. Scandinavian Audiology Supplementum 2001;52:177‐9. [DOI] [PubMed] [Google Scholar]
Park 1991a instructions {published data only}
- Park MY, Casali JG. A controlled investigation of in‐field attenuation performance of selected insert, earmuff, and canal cap hearing protectors. Human Factors 1991;33(6):693‐714. [DOI] [PubMed] [Google Scholar]
Park 1991b protection {published data only}
- Park MY, Casali JG. A controlled investigation of in‐field attenuation performance of selected insert, earmuff, and canal cap hearing protectors. Human Factors 1991;33(6):693‐714. [DOI] [PubMed] [Google Scholar]
Pell 1973 {published data only}
- Pell S. An evaluation of hearing conservation program ‐ a five‐year longitudinal study. American Industrial Hygiene Association Journal 1973;34(2):82‐91. [DOI] [PubMed] [Google Scholar]
Rabinowitz 2011 {published data only}
- Rabinowitz PM, Galusha D, Kirsche SR, Cullen MR, Slade MD, Dixon‐Ernst C. Effect of daily noise exposure monitoring on annual rates of hearing loss in industrial workers. Occupational and Environmental Medicine 2011;68(6):414‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reynolds 1990a {published data only}
- Reynolds JL, Royster LH, Pearson RG. Hearing conservation programs (HCPs): the effectiveness of one company's HCP in a 12‐hr work shift environment. American Industrial Hygiene Association Journal 1990;51(8):437‐46. [DOI] [PubMed] [Google Scholar]
Royster 1980 {published data only}
- Royster LH. An evaluation of the effectiveness of two different insert types of ear protection in preventing TTS in an industrial environment. American Industrial Hygiene Association Journal 1980;41(3):161‐9. [DOI] [PubMed] [Google Scholar]
Salmani 2014 {published data only}
- Salmani Nodoushan M, Mehrparvar AH, Torab Jahromi M, Safaei S, Mollasadeghi A. Training in using earplugs or using earplugs with a higher than necessary noise reduction rating? A randomized clinical trial. International Journal of Occupational and Environmental Medicine 2014;5:187‐93. [PMC free article] [PubMed] [Google Scholar]
Seixas 2011 {published data only}
- Seixas NS, Neitzel R, Stover B, Sheppard L, Daniell B, Edelson J. A multi‐component intervention to promote hearing protector use among construction workers. International Journal of Audiology 2011; Vol. 50:s46‐s56. [DOI] [PMC free article] [PubMed]
Simpson 1994 {published data only}
- Simpson TH, Stewart M, Kaltenbach JA. Early indicators of hearing conservation program performance. Journal of the American Academy of Audiology 1994;5:300‐6. [PubMed] [Google Scholar]
References to studies excluded from this review
Aybek 2010 {published data only}
- Aybek A, Kamer HA, Arslan S. Personal noise exposures of operators of agricultural tractors. Applied Ergonomics 2010;41:274‐81. [DOI] [PubMed] [Google Scholar]
Bealko 2009 {published data only}
- Bealko SB. Mining haul truck cab noise: an evaluation of three acoustical environments. Mining Engineering 2009;61(10):36‐42. [Google Scholar]
Bockstael 2008 {published data only}
- Bockstael A, Keppler H, Dhooge I, D'haenens W, Maes L, Philips B, et al. Effectiveness of hearing protector devices in impulse noise verified with transiently evoked and distortion product otoacoustic emissions. International Journal of Audiology 2008;47:119‐33. [DOI] [PubMed] [Google Scholar]
Bowes 1990 {published data only}
- Bowes SM, Corn M. Noise exposure reduction aboard an oceangoing hopper dredge. American Industrial Hygiene Association Journal 1990;51(9):469‐4. [DOI] [PubMed] [Google Scholar]
Brueck 2009 {published data only}
- Brueck L. Real world use and performance of hearing protection. Health and Safety Executive, 2009. [Google Scholar]
Brühl 1994 {published data only}
- Bruhl P, Ivarsson A. Noise‐exposed male sheet‐metal workers using hearing protectors. A longitudinal study of hearing threshold shifts covering fifteen years. Scandinavian Audiology 1994;23(2):123‐8. [DOI] [PubMed] [Google Scholar]
Byrne 2011 {published data only}
- Byrne DC, Davis RR, Shaw PB, Specht BM, Holl AN. Relationship between comfort and attenuation measurements for two types of earplugs. Noise & Health 2011;13(51):86‐92. [DOI] [PubMed] [Google Scholar]
Casali 2009 {published data only}
- Casali JG, Ahroon WA, Lancaster JA. A field investigation of hearing protection and hearing enhancement in one device: for soldiers whose ears and lives depend upon it. Noise & Health 2009;11(42):69‐90. [DOI] [PubMed] [Google Scholar]
Chou 2009 {published data only}
- Chou YF, Lai JS, Kuo HW. Effects of shift work on noise‐induced hearing loss. Noise & Health 2009;11(45):185‐8. [DOI] [PubMed] [Google Scholar]
Franks 2000 {published data only}
- Franks JR, Murphy WJ, Johnson JL, Harris DA. Four earplugs in search of a rating system. Ear and Hearing 2000;21(3):218‐26. [DOI] [PubMed] [Google Scholar]
Giardino 1996 {published data only}
- Giardino DA, Durkt G. Evaluation of muff‐type hearing protectors as used in a working environment. American Industrial Hygiene Association Journal 1996;57(3):264‐71. [DOI] [PubMed] [Google Scholar]
Golmohammadi 2010 {published data only}
- Golmohammadi R, Monazzam MR, Nourollahi M, Nezafat A, Fard SMB. Evaluation of noise propagation characteristics of compressors in Tehran oil refinery centre and presenting control methods. Journal of Research in Health Sciences 2010;10(1):22‐30. [PubMed] [Google Scholar]
Griest 2008 {published data only}
- Griest S. Evaluation of a hearing‐loss prevention program. Seminars in Hearing 2008;29(1):122‐36. [Google Scholar]
Groothoff 1999 {published data only}
- Groothoff B. Incorporating effective noise control in music entertainment venues? Yes, it can be done. Journal of Occupational Health & Safety ‐ Australia & New Zealand 1999;15(6):543‐50. [Google Scholar]
Jelinic 2005 {published data only}
- Jelinic JD, Mustajbegovic J, Zuskin E, Lukic J, Cavar V, Ivankovic A. Managing occupational safety and health in aluminium production: case study of aluminium production factory, Mostar, Bosnia and Herzegovina. Croatian Medical Journal 2005;46(5):838‐47. [PubMed] [Google Scholar]
Kardous 2003 {published data only}
- Kardous CA, Willson RD, Hayden CS, Szlapa P, Murphy WJ, Reeves EF. Noise exposure assessment and abatement strategies at an indoor firing range. Applied Occupational and Environmental Hygiene 2003;18:629‐36. [DOI] [PubMed] [Google Scholar]
Karlsmose 2001 {published data only}
- Karlsmose B, Lauritzen T, Engberg M, Parving A. A randomised controlled trial of screening for adult hearing loss during preventive health checks. British Journal of General Practice 2001;51(466):351‐5. [PMC free article] [PubMed] [Google Scholar]
Kavraz 2009 {published data only}
- Kavraz M, Abdulrahimov R. A study comparing the noise reduction behavior of variously shaped barriers of limited size in indoor spaces. Indoor and Built Environment 2009;18(6):541‐52. [Google Scholar]
Knothe 1999 {published data only}
- Knothe E, Busche H‐J. Noise reduction in scrap treatment facilities. Zeitschrift fur Larmbekampfung 1999;46(6):210‐3. [Google Scholar]
Kotarbinska 2009 {published data only}
- Kotarbinska E, Kozlowski E. Measurement of Effective Noise Exposure of Workers Wearing Ear‐Muffs. International Journal of Occupational Safety and Ergonomics 2009;15(2):193‐200. [DOI] [PubMed] [Google Scholar]
Lempert 1983 {published data only}
- Lempert B, Edwards R. Field investigations of noise reduction afforded by insert‐type hearing protectors. American Industrial Hygiene Association Journal 1983;44(12):894‐902. [DOI] [PubMed] [Google Scholar]
Lutz 2015 {published data only}
- Lutz EA, Reed RJ, Turner D, Littau SR, Lee V, Hu CC. Effectiveness evaluation of existing noise controls in a deep shaft underground mine. Journal of occupational and environmental hygiene 2015;12(5):287‐93. [DOI] [PubMed] [Google Scholar]
Mechfske 2002 {published data only}
- Mechefske CK, Geris R, Gati JS, Rutt BK. Acoustic noise reduction in a 4 T MRI scanner. MAGMA 2002;13(3):172‐6. [DOI] [PubMed] [Google Scholar]
Merry 1992 {published data only}
- Merry CJ, Sizemore CW, Franks JR. The effect of fitting procedure on hearing protector attenuation. Ear & Hearing 1992;13(1):11‐8. [DOI] [PubMed] [Google Scholar]
Monazzam 2011 {published data only}
- Monazzam MR, Golmohammadi R, Nourollahi M, Fard SMB. Assessment and control design for steam vent noise in an oil refinery. Journal of Research in Health Sciences 2011;1(1):14‐9. [PubMed] [Google Scholar]
Mrena 2008 {published data only}
- Mrena R, Ylikoski J, Kiukaanniemi H, Makitie AA, Savolainen S. The effect of improved hearing protection regulations in the prevention of military noise‐induced hearing loss. Acta Oto‐Laryngologica 2008;128(9):997‐1003. [DOI] [PubMed] [Google Scholar]
Murphy 2011 {published data only}
- Murphy WJ, Stephenson MR, Byrne DC, Witt B, Duran J. Effects of training on hearing protector attenuation. Noise & Health 2011;13(51):132‐41. [DOI] [PubMed] [Google Scholar]
Nair 2009 {published data only}
- Nair S, Kashyap RC. Prevalence of noise induced hearing loss in Indian Air Force personnel. Medical Journal Armed Forces India 2009;65(3):247‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Neitzel 2005 {published data only}
- Neitzel R, Seixas N. The effectiveness of hearing protection among construction workers. Journal of Occupational & Environmental Hygiene 2005;2(4):227‐38. [DOI] [PubMed] [Google Scholar]
Neitzel 2008 {published data only}
- Neitzel R, Meischke H, Daniell W, Trabeau M, Somers S, Seixas NS. Development and pilot test of hearing conservation training for construction workers. American Journal of Industrial Medicine 2008;51(2):120‐9. [DOI] [PubMed] [Google Scholar]
Niskanen 2001 {published data only}
- Niskanen J, Anttonen H. Ways to promote a noise control programme. Scandinavian Audiology 2001;30(52):174‐6. [DOI] [PubMed] [Google Scholar]
Oestenstad 2008 {published data only}
- Oestenstad RK, Norman MW, Borton TE. Efficacy of the US Army Policy on Hearing Conservation Programs. Military Medicine 2008;173(10):992‐8. [DOI] [PubMed] [Google Scholar]
Pääkkönen 2005 {published data only}
- Paakkonen R, Lehtomaki K. Protection efficiency of hearing protectors against military noise from handheld weapons and vehicles. Noise & Health 2005;7(26):11‐20. [DOI] [PubMed] [Google Scholar]
Pearlman 2009 {published data only}
- Pearlman RT, Sandidge O. Noise characteristics of surgical space suits. Orthopedics 2009;32(11):825. [DOI] [PubMed] [Google Scholar]
Pingle 2006 {published data only}
- Pingle S, Shanbag S. CASH ‐ an innovative approach to sustainable OSH improvement at workplace. Medicina del Lavoro 2006;97(2):358‐67. [PubMed] [Google Scholar]
Randolph 2008 {published data only}
- Randolph RF, Kissell FN, NIOSH. The effect of an insertion lubricant on the noise attenuation of foam earplugs. NOISE‐CON. Institute of Noise Control Engineering 2008:1‐4.
Reeves 2009 {published data only}
- Reeves ER, Randolph RF, Yantek DS, Peterson JS, NIOSH. Noise control in underground metal mining. Information circular 2009; Vol. IC 9518:1‐62.
Reynolds 1990b {published data only}
- Reynolds JL, Royster LH, Pearson RG. Hearing conservation programs (HCPs): the effectiveness of one company's HCP in a 12‐hr work shift environment. American Industrial Hygiene Association Journal 1990;51(8):437‐46. [DOI] [PubMed] [Google Scholar]
Sataloff 2010 {published data only}
- Sataloff J, Hawkshaw MJ, Sataloff RT. "Gun‐shooting hearing loss": A pilot study. Ear, Nose and Throat Journal 2010;89(1):E15‐E19. [PubMed] [Google Scholar]
Scannell 1998 {published data only}
- Scannell K. Low‐cost methods of noise control at source which increase production and reduce the risk of hearing damage. Journal of Occupational Health & Safety ‐ Australia & New Zealand 1998;14(5):493‐503. [Google Scholar]
Schaefer 1992 {published data only}
- Schaefer PD. Successful noise abatement program relies on engineering controls. Occupational Health & Safety 1992;61(10):82‐6. [PubMed] [Google Scholar]
Smith 2006 {published data only}
- Smith AK, Spencer ER, Alcorn LA, Kovalchik PG. Underground evaluation of coated flight bars for a continuous mining machine [The 35th International Congress and Exposition on Noise Control Engineering, 3‐6 December 2006]. International Institute of Noise Control Engineering. Honolulu, Hawaii. West Lafayette, 2006 Dec:1‐8.
Smith 2009 {published data only}
- Smith AK, Kovalchik PG, Alcorn LA, Matetic RJ. A dual sprocket chain as a noise control for a continuous mining machine. Noise Control Engineering Journal 2009;57(5):413‐9. [Google Scholar]
Smith 2011 {published data only}
- Smith AK, Zimmerman JJ, Michael R, Kovalchik PG. Modified tail section reduces noise on a continuous mining machine. Mining Engineering 2011;63(7):83‐5. [Google Scholar]
Stone 1971 {published data only}
- Stone GF, Freman TW, Craig RL. Noise control and hearing conservation in large steam‐electric generating stations. American Industrial Hygiene Association Journal 1971;32(2):123‐30. [DOI] [PubMed] [Google Scholar]
Toivonen 2002 {published data only}
- Toivonen M, Pääkkönen R, Savolainen S, Lehtomäki K. Noise attenuation and proper insertion of earplugs into ear canals. Annals of Occupational Hygiene 2002;46(6):527‐30. [DOI] [PubMed] [Google Scholar]
Tsukada 2008 {published data only}
- Tsukada T, Sakakibara H. A trail of individual education for hearing protection with an instrument that measures the noise attenuation effect of wearing earplugs. Industrial Health 2008;46(4):393‐6. [DOI] [PubMed] [Google Scholar]
Walter 2009 {published data only}
- Walter JS. Sound exposure levels experienced by university wind band members. Medical Problems of Performing Artists 2009;24(2):63‐70. [Google Scholar]
Waugh 1990 {published data only}
- Waugh R, Forcier L. Research workshop paper: sense of sound. Australian Deafness Council project. Journal of Occupational Health and Safety 1990;6(5):399‐401. [Google Scholar]
Williams 2004 {published data only}
- Williams W. Instruction and the improvement of hearing protector performance. Noise & Health 2004;7(25):41‐7. [PubMed] [Google Scholar]
Wu 2009 {published data only}
- Wu CC, Young YH. Ten‐year longitudinal study of the effect of impulse noise exposure from gunshot on inner ear function. International Journal of Audiology 2009;48(9):655‐60. [DOI] [PubMed] [Google Scholar]
Additional references
ANSI/ASA 2007
- ANSI/ASA. American national standard methods of estimating effective A‐weighted sound pressure levels when hearing protectors are worn. ANSI S12.68‐2007. Melville, NY: Acoustical Society of America 2007.
ANSI/ASA 2008
- ANSI/ASA. American national standard methods for measuring the real‐ear attenuation of hearing protectors. ANSI S12.6‐2008 (Revision of ANSI S12.6‐1997). Melville, NY: Acoustical Society of America 2008.
Azman 2012
- Azman AS, Yantek DS, Alcorn LA. Evaluations of a noise control for roof bolting machines. Mining Engineering 2012;64(12):64‐70. [PMC free article] [PubMed] [Google Scholar]
Berger 1996
- Berger EH, Franks JR, Lindgren F. International Review of Feld Studies of Hearing Protector Attenuation. In: Axlesson A, Borchgrevink H, Hamernik RP, Hellstrom P, Henderson D, Salvi RJ editor(s). Scientific Basis of Noise‐induced Hearing Loss. New York: Thieme Medical Publishing, 1996:361‐77. [Google Scholar]
Berger 1998
- Berger EH, Franks JR, Behar A, Casali JG, Dixon‐Ernst C, Kieper RW, et al. Development of a new standard laboratory protocol for estimating the field attenuation of hearing protection devices. Part III. The validity of subject‐fit data. Journal of the Acoustic Society of America 1998;103:665‐72. [DOI] [PubMed] [Google Scholar]
Borchgrevink 2003
- Borchgrevink HM. Does health promotion work in relation to noise?. Noise & Health 2003;5(18):25‐30. [PubMed] [Google Scholar]
Caillet 2012
- Caillet J, Marrot F, Unia Y, Aubourg PA. Comprehensive approach for noise reduction in helicopter cabins. Aerospace Science and Technology 2012;23(1):17‐25. [Google Scholar]
Chinn 2000
- Chinn S. A simple method for converting an odds ratio to effect size for use in meta‐analysis. Statistics in Medicine 2000;19:3127‐31. [DOI] [PubMed] [Google Scholar]
Cockrell 2015
- Cockrell TW, Balanay JAG, Dawkins W. Engineering control of noise from 4‐roll calender operations in tire manufacturing. Journal of Occupational & Environmental Hygiene 2015;12(9):D193‐200. [DOI] [PubMed] [Google Scholar]
Daniell 2006
- Daniell WE, Swan SS, McDaniel MM, Camp JE, Cohen MA, Stebbins JG. Noise exposure and hearing loss prevention programmes after 20 years of regulations in the United States. Occupational & Environmental Medicine 2006;63(5):343‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG (editors). Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Dobie 1995
- Dobie RA. Prevention of noise‐induced hearing loss. Archives of Otolaryngology ‐ Head and Neck Surgery 1995;121(4):385‐91. [DOI] [PubMed] [Google Scholar]
Downs 1998
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non‐randomised studies of health care interventions. Journal of Epidemiology and Community Health 1998;52(6):377‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ellenbecker 1996
- Ellenbecker MJ. Engineering controls as an intervention to reduce worker exposure. American Journal of Industrial Medicine 1996;29(4):303‐7. [DOI] [PubMed] [Google Scholar]
EPOC 2012
- Cochrane Effective Practice and Organisation of Care (EPOC) Review Group. The data collection checklist. www.epoc.cochrane.org (accessed 10 March 2012).
EU 2003
- EU. Directive 2003/10/EC on the minimum health and safety requirements regarding exposure of workers to the risks arising from physical agents (noise). EU 2003.
EU‐OSHA 2009
- European Agency for Safety and Health at Work. Combined exposure to noise and ototoxic substances. European Risk Observatory Literature Review 2009:1‐62.
Glasziou 2007
- Glasziou P, Chalmers I, Rawlins M, McCulloch P. When are randomised trials unnecessary? Picking signal from noise. BMJ 2007;334:349‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Golmohammadi 2014
- Golmohammadi R, Giahi O, Aliabadi M, Darvishi E. An intervention for noise control of blast furnace in steel industry. Journal of Research in Health Sciences 2014;14(4):287‐90. [PubMed] [Google Scholar]
Haron 2009
- Haron Z, Yahya K, Mohamad MI. Probability approach for prediction of construction site noise. Journal of Asian Architecture and Building Engineering 2009;8(2):571‐7. [Google Scholar]
Helleman 2010
- Helleman HW, Jansen EJM, Dreschler WA. Otoacoustic emissions in a hearing conservation program: general applicability in longitudinal monitoring and the relation to changes in pure‐tone thresholds. International Journal of Audiology 2010;49(6):410‐19. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2011b
- Higgins JPT, Deeks JJ, Altman DG (editors). Chapter 16: Special topics in statistics. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hozo 2005
- Hozo S Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range and the size of a sample. BMC Medical Research Methodology 2005;5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
HSE 2013
- HSE. Sound solutions for the food and drink industries: reducing noise in food and drink manufacture. HSG232. 2nd Edition. Health and safety executive, 2013:77. [Google Scholar]
HSE 2015
- HSE. A recipe for safety: health and safety in food and drink manufacture. HSG252. 2nd Edition. Health and safety executive, 2015. [Google Scholar]
ISO 1990
- ISO ‐ International Standard Organisation. ISO 1999: Acoustics ‐ Determination of occupational noise exposure and estimation of noise‐induced hearing impairment. Geneva: ISO, 1990. [Google Scholar]
ISO 1999b
- ISO International Standard Organisation. ISO 4869‐1: Acoustics ‐ Hearing Protectors ‐ Part 1: Subjective method for the measurement of sound attenuation. Geneva: ISO 1990.
ISO 2006
- ISO, International Standard Organisation. ISO 4869‐5: Acoustics ‐ Hearing Protectors ‐ Part 5: Method for estimation of noise reduction using fitting by inexperienced test subjects. Geneva: ISO 2006.
John 2012
- John AB, Kreisman BM, Pallett S. Validity of hearing impairment calculation methods for prediction of self‐reported hearing handicap. Noise Health 2012;14:13‐20. [DOI] [PubMed] [Google Scholar]
Johnson 2010
- Johnson AC, Morata TC. Occupational exposure to chemicals and hearing impairment. Arbete och Halsa 2010;44:1‐177. [https://gupea.ub.gu.se/bitstream/2077/23240/1/gupea_2077_23240_1.pdf] [Google Scholar]
Kirchner 2012
- Kirchner DB, Evenson E, Dobie RA, Rabinowitz P, Crawford J, Kopke R, et al. Occupational noise‐induced hearing loss: ACOEM Task Force on Occupational Hearing Loss. Journal of Occupational and Environmental Medicine 2012;54(1):106‐8. [DOI] [PubMed] [Google Scholar]
Küpper 2013
- Küpper T, Jansing P, Schöffl V, Giet S. Does modern helicopter construction reduce noise exposure in helicopter rescue operations?. Annals of Occupational Hygiene 2013;57(1):34‐42. [DOI] [PubMed] [Google Scholar]
Le Prell 2012
- Prell CG, Bao J. Prevention of Noise‐induced Hearing Loss: Potential Therapeutic Agents. In: Prell CG, Henderson D, Fay RR, Popper AN editor(s). Noise‐Induced Hearing Loss: Scientific Advances. New York: Springer Science+Business Media, LLC, 2012:285‐338. [Google Scholar]
Leigh 1999
- Leigh J, Macaskill P, Kuosma E, Mandryk J. Global burden of disease and injury due to occupational factors. Epidemiology 1999;10(5):626‐31. [PubMed] [Google Scholar]
Lynch 2005
- Lynch ED, Kil J. Compounds for the prevention and treatment of noise‐induced hearing loss. Drugs Discovery Today 2005;10:1291‐8. [DOI] [PubMed] [Google Scholar]
Maling 2016
- Maling GC Jr, Wood EW, Lotz G, Lang WW. Reducing employee noise exposure in manufacturing: best practices, innovative techniques, and the workplace of the future. Institute of Noise Control Engineering of the USA 2016.
Martinson 1999
- Martinson BC, Murray DM, Jeffery RW, Hennrikus DJ. Intraclass correlations for measures from a work site health promotion study: estimates, correlates and applications. American Journal of Health Promotion 1999;13(6):347‐57. [DOI] [PubMed] [Google Scholar]
Masterson 2015
- Masterson EA, Deddens JA, Themann CL, Bertke S, Calvert GM. Trends in worker hearing loss by industry sector, 1981‐2010. American Journal of Industrial Medicine 2015;58(4):392‐401. [DOI: 10.1002/ajim.22429] [DOI] [PMC free article] [PubMed] [Google Scholar]
Masterson 2016a
- Masterson EA, Themann CL, Luckhaupt SE, Li J, Calvert GM. Hearing difficulty and tinnitus among U.S. workers and non‐workers in 2007. American Journal of Industrial Medicine 2016;59(4):290‐300. [DOI: 10.1002/ajim.22565] [DOI] [PubMed] [Google Scholar]
Masterson 2016b
- Masterson EA, Bushnell PT, Themann CL, Morata TC. Hearing impairment among noise‐exposed workers ‐ United States, 2003‐2012. MMWR. Morbidity and Mortality Weekly Report 2016;65(15):389‐94. [DOI: 10.15585/mmwr.mm6515a2] [DOI] [PubMed] [Google Scholar]
May 2000
- May JJ. Occupational hearing loss. American Journal of Occupational Medicine 2000;37:112‐20. [DOI] [PubMed] [Google Scholar]
McBride 2004
- McBride DI. Noise‐induced hearing loss and hearing conservation in mining. Occupational Medicine 2004;54(5):290‐6. [DOI] [PubMed] [Google Scholar]
Morata 2015
- Morata T, Hayden C, Driscoll D, Stephenson CM, Clegg PM, Afanuh S. Preventing hazardous noise and hearing loss during project design and operation. Workplace design solutions, National Institute for Occupational Safety and Health 2015.
Murphy 2008
- Murphy WJ. How to assess hearing protection evaluation effectiveness: what is new in ANSI/ASA S12.68. Acoustics Today 2008;4:40‐2. [Google Scholar]
Neitzel 2011
- Neitzel RL, Stover B, Seixas NS. Longitudinal assessment of noise exposure in a cohort of construction workers. Annals of Occupational Hygiene 2011;55(8):906‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nelson 2005
- Nelson DI, Nelson RY, Concha‐Barrientos M, Fingerhut M. The global burden of occupational noise‐induced hearing loss. American Journal of Industrial Medicine 2005;48(6):446‐58. [DOI] [PubMed] [Google Scholar]
NIOSH 1997
- Cohen AL, Gjessing CC, Fine LJ, Bernard BP, McGlothin JD. Elements of ergonomics programs, a primer based on workplace evaluations of musculoskeletal disorders. Publication No. 97–117. Cincinnati OH: Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health (NIOSH), 1997. [Google Scholar]
NIOSH 1998
- NIOSH. Criteria for a recommended standard: occupational noise exposure, revised criteria 1998. Publication no 98‐126. Cincinnati OH: NIOSH 1998.
Pan 2016
- Pan J, Paurobally R, Qiu XJ. Active noise control in workplaces. Acoustics Australia 2016;44(1):45‐50. [Google Scholar]
Piaggio 2006
- Piaggio G, Elbourne DR, Altman DG, Pocock SJ, Evans SJW. Reporting of non‐inferiority and equivalence randomised trials. JAMA 2006;295:1152‐60. [DOI] [PubMed] [Google Scholar]
Prince 1997
- Prince MM, Stayner LT, Smith RJ, Gilbert SJ. A re‐examination of risk estimates from the NIOSH Occupational Noise and Hearing Survey (ONHS). Journal of the Acoustical Society of America 1997;101(2):950‐63. [DOI] [PubMed] [Google Scholar]
Rabinowitz 2007
- Rabinowitz PM, Galusha D, Dixon‐Ernst, Slade MD. Audiometric early flags for occupational hearing loss. Journal of Occupational and Environmental Medicine 2007;12:1310‐6. [DOI] [PubMed] [Google Scholar]
Ramsay 2003
- Ramsay CR, Matowe L, Grilli R, Grimshaw JM, Thomas RE. Interrupted time series designs in health technology assessment: lessons from two systematic reviews of behavior change strategies. International Journal of Technology Assessment in Health Care 2003;19(4):613‐23. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Nordic Cochrane Centre. The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre. The Cochrane Collaboration, 2014.
Royster 1996
- Royster JD, Berger EH, Merry CJ, Nixon CW, Franks JR, Behar A, et al. Development of a new standard laboratory protocol for estimating the field attenuation of hearing protection devices. Part I. Research of Working Group 11, Accredited Standards Committee S12, Noise. Journal of the Acoustical Society of America 1996;99:1506‐26. [DOI] [PubMed] [Google Scholar]
Seixas 2001
- Seixas NS, Ren K, Neitzel R, Camp J, Yost M. Noise exposure among construction electricians. American Industrial Hygiene Association Journal 2001;62(5):615‐21. [DOI] [PubMed] [Google Scholar]
Sulkowski 2007
- Sulkowski WJ. Occupational Noise. In: Luxon LM, Prasher D editor(s). Noise and its effects. West Sussex, England: Whurr Publisher Limited, 2007:397‐434. [Google Scholar]
Suter 2002
- Suter AH. Construction noise: exposure, effects, and the potential for remediation; a review and analysis. American Industrial Hygiene Association Journal 2002;63(6):768‐89. [DOI] [PubMed] [Google Scholar]
Suter 2009
- Suter AH. The hearing conservation amendment: 25 years later. Noise & Health 2009;11(42):2‐7. [DOI] [PubMed] [Google Scholar]
Tak 2009
- Tak SW. Noise, hearing protector use, and hearing loss in American workers. The Newsletter of the Council for Accreditation in Occupational Hearing Conservation 2009;21(2):5‐6. [Google Scholar]
Thompson 2015
- Thompson J K. Noise control of large mining machines. inter.noise The 44th International Congress and Exposition on Noise Control Engineering, August 9‐12, 2015, San Francisco, California. 2015.
Trabeau 2008
- Trabeau M, Neitzel R, Meischke H, Daniel WE, Seixas NS. A comparison of "Train‐the‐Trainer" and expert training modalities for hearing protection use in construction. American Journal of Industrial Medicine 2008;51(2):130‐7. [DOI] [PubMed] [Google Scholar]
Verbeek 2005
- Verbeek J, Salmi J, Pasternack I, Jauhiainen M, Laamanen I, Schaafsma F, et al. A search strategy for occupational health intervention studies. Occupational and Environmental Medicine 2005;62(10):682‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2002
- WHO ‐ World Health Organization. The World Health Report (Chapter 4) Selected occupational risks. www.who.int/wht/2002/chapter 4/en/index8.html. WHO, 2002. [Google Scholar]
Wilson 2016
- Wilson P. Top 10 Noise Control Techniques: 2015. Acoustics Australia 2016;44:33‐43. [Google Scholar]
References to other published versions of this review
Verbeek 2014
- Verbeek JH, Kateman E, Morata TC, Dreschler WA, Mischke C. Interventions to prevent occupational noise‐induced hearing loss: a Cochrane systematic review. International Journal of Audiology 2014;53(Suppl 2):84‐96. [DOI: 10.3109/14992027.857436] [DOI] [PMC free article] [PubMed] [Google Scholar]
Verbeek 2015
- Verbeek JH, Kateman E, Morata TC, Dreschler WA, Mischke C. The effectiveness of interventions to prevent occupational noise‐induced hearing loss: a Cochrane systematic review [Efetividade das intervenções para prevenção de perda auditiva ocupacional induzida por ruído: uma Revisão Sistemática Cochrane]. In: Boéchat E, Menezes PL, Couto CM, Frizzo ACF, Scharlach RC, Anastacio ART editor(s). Tratado de Audiologia. 2nd Edition. Rio de Janeiro: Guanabara Coogan Ltda, 2015:211‐224. [ISBN 978‐85‐277‐2732‐7] [Google Scholar]


