Abstract
Background
Restless legs syndrome (RLS) is a common neurologic disorder that is associated with peripheral iron deficiency in a subgroup of patients. It is unclear whether iron therapy is effective treatment for RLS.
Objectives
To evaluate the efficacy and safety of oral or parenteral iron for the treatment of restless legs syndrome (RLS) when compared with placebo or other therapies.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, Embase, PsycNFO, and CINAHL for the time period January 1995 to September 2017. We searched reference lists for additional published studies. We searched Clinicaltrials.gov and other clinical trial registries (September 2017) for ongoing or unpublished studies.
Selection criteria
Controlled trials comparing any formulation of iron with placebo, other medications, or no treatment, in adults diagnosed with RLS according to expert clinical interview or explicit diagnostic criteria.
Data collection and analysis
Two review authors independently extracted data and assessed trial quality, with discussion to reach consensus in the case of any disagreement. The primary outcome considered in this review was restlessness or unpleasant sensations, as experienced subjectively by the patient. We combined treatment/control differences in the outcomes across studies using random‐effects meta‐analyses. We analysed continuous data using mean differences (MDs) where possible and performed standardised mean difference (SMD) analyses when different measurements were used across studies. We calculated risk ratios (RRs) for dichotomous data using the Mantel‐Haenszel method and 95% confidence intervals (CIs). We analysed study heterogeneity using the I2 statistic. We used standard methodological procedures expected by Cochrane. We performed GRADE analysis using GRADEpro.
Main results
We identified and included 10 studies (428 total participants, followed for 2‐16 weeks) in this review. Our primary outcome was restlessness or uncomfortable leg sensations, which was quantified using the International Restless Legs Scale (IRLS) (range, 0 to 40) in eight trials and a different RLS symptom scale in a ninth trial. Nine studies compared iron to placebo and one study compared iron to a dopamine agonist (pramipexole). The possibility for bias among the trials was variable. Three studies had a single element with high risk of bias, which was lack of blinding in two and incomplete outcome data in one. All studies had at least one feature resulting in unclear risk of bias.
Combining data from the seven trials using the IRLS to compare iron and placebo, use of iron resulted in greater improvement in IRLS scores (MD ‐3.78, 95% CI ‐6.25 to ‐1.31; I2= 66%, 7 studies, 345 participants) measured 2 to 12 weeks after treatment. Including an eighth study, which measured restlessness using a different scale, use of iron remained beneficial compared to placebo (SMD ‐0.74, 95% CI ‐1.26 to ‐0.23; I2 = 80%, 8 studies, 370 participants). The GRADE assessment of certainty for this outcome was moderate.
The single study comparing iron to a dopamine agonist (pramipexole) found a similar reduction in RLS severity in the two groups (MD ‐0.40, 95% CI ‐5.93 to 5.13, 30 participants).
Assessment of secondary outcomes was limited by small numbers of trials assessing each outcome. Iron did not improve quality of life as a dichotomous measure (RR 2.01, 95% CI 0.54 to 7.45; I2=54%, 2 studies, 39 participants), but did improve quality of life measured on continuous scales (SMD 0.51, 95% CI 0.15 to 0.87; I2= 0%, 3 studies, 128 participants), compared to placebo. Subjective sleep quality was no different between iron and placebo groups (SMD 0.19, 95% CI ‐0.18 to 0.56; I2 = 9%, 3 studies, 128 participants), nor was objective sleep quality, as measured by change in sleep efficiency in a single study (‐35.5 +/‐ 92.0 versus ‐41.4 +/‐ 98.2, 18 participants). Periodic limb movements of sleep were not significantly reduced with iron compared to placebo ( SMD ‐0.19, 95% CI ‐0.70 to 0.32; I2 = 0%, 2 studies, 60 participants). Iron did not improve sleepiness compared to placebo, as measured on the Epworth Sleepiness Scale (data not provided, 1 study, 60 participants) but did improve the daytime tiredness item of the RLS‐6 compared to placebo (least squares mean difference ‐1.5, 95% CI ‐2.5 to ‐0.6; 1 study, 110 participants). The GRADE rating for secondary outcomes ranged from low to very low.
Prespecified subgroup analyses showed more improvement with iron in those trials studying participants on dialysis. The use of low serum ferritin levels as an inclusion criteria and the use or oral versus intravenous iron did not show significant subgroup differences.
Iron did not result in significantly more adverse events than placebo (RR 1.48, 95% CI 0.97 to 2.25; I2=45%, 6 studies, 298 participants). A single study reported that people treated with iron therapy experienced fewer adverse events than the active comparator pramipexole.
Authors' conclusions
Iron therapy probably improves restlessness and RLS severity in comparison to placebo. Iron therapy may not increase the risk of side effects in comparison to placebo. We are uncertain whether iron therapy improves quality of life in comparison to placebo. Iron therapy may make little or no difference to pramipexole in restlessness and RLS severity, as well as in the risk of adverse events. The effect on secondary outcomes such as quality of life, daytime functioning, and sleep quality, the optimal timing and formulation of administration, and patient characteristics predicting response require additional study.
Keywords: Humans; Dopamine Agonists; Dopamine Agonists/adverse effects; Dopamine Agonists/therapeutic use; Ferric Compounds; Ferric Compounds/adverse effects; Ferric Compounds/therapeutic use; Ferric Oxide, Saccharated; Ferric Oxide, Saccharated/adverse effects; Ferric Oxide, Saccharated/therapeutic use; Ferrous Compounds; Ferrous Compounds/adverse effects; Ferrous Compounds/therapeutic use; Iron; Iron/adverse effects; Iron/therapeutic use; Maltose; Maltose/adverse effects; Maltose/analogs & derivatives; Maltose/therapeutic use; Patient Dropouts; Patient Dropouts/statistics & numerical data; Pramipexole; Pramipexole/adverse effects; Pramipexole/therapeutic use; Quality of Life; Randomized Controlled Trials as Topic; Restless Legs Syndrome; Restless Legs Syndrome/therapy; Trace Elements; Trace Elements/adverse effects; Trace Elements/therapeutic use; Treatment Outcome
Plain language summary
Iron for the treatment of restless legs syndrome
Background
Restless legs syndrome is a common medical condition that causes uncomfortable urges to move the legs. These urges happen in the evening and at night and can keep people from sleeping well. Low blood levels of iron are often seen in people who have restless legs syndrome. Low blood iron levels may be part of the cause of restless legs syndrome. Iron can be taken as a pill or given as an injection into the bloodstream. We performed this review to see if iron treatment reduces the symptoms of restless legs syndrome.
Study characteristics
We included 10 studies of iron. These 10 studies included 428 people with restless legs syndrome. Not all participants had low blood levels of iron. All participants were adults. Most of the studies used injections of iron, while three studies used iron in pill form. Iron treatment was compared to a non‐active treatment (i.e. a placebo) in nine studies. In one study, iron was compared to another restless legs syndrome treatment called a dopamine agonist. The main measure of interest in our review was the severity of restlessness. This was usually measured using a 10‐question survey regarding severity and effects of urges to move the legs, called the International Restless Legs Syndrome Severity Rating Scale (IRLS). This was measured 2‐4 weeks after injections of iron and 12‐14 weeks after iron in pill form.
Four trials were funded by the drug manufacturer. Two trials were funded by the USA National Institutes of Health. Two trials were funded by the workplaces of the study investigators. Two studies did not report who funded the study. The four studies funded by drug manufacturers were the largest. The studies funded by drug companies contributed over half of the total number of participants.
Key results and quality of evidence
Overall, the studies showed that iron is better than a placebo for reducing the severity of restless legs syndrome symptoms, although the benefit was low to moderate. This is mostly based on studies using injections of iron, rather than iron pills. Iron was helpful even if blood iron levels were normal at the start of the study. The quality of the evidence was moderate, because not all completed studies have been published, not all important outcomes have been measured, and not enough people have been studied. Side effects were not more common with iron than with placebo. Based on one study, side effects were less common with iron than with another commonly used restless legs syndrome treatment, although the certainty in this result is very low. More studies are needed to allow people with RLS and doctors to make decisions about who should take iron for restless legs syndrome treatment, using what type of iron, and for how long. The evidence is current to September 2017.
Summary of findings
Summary of findings for the main comparison. Iron compared to placebo for the treatment of restless legs syndrome.
| Iron compared to placebo for the treatment of restless legs syndrome | |||||
| Patient or population: people with restless legs syndrome Settings: outpatient clinics Intervention: iron Comparison: placebo | |||||
| Outcomes | № of participants (studies) Follow up | Certainty of the evidence (GRADE) | Relative effect (95% CI) | Anticipated absolute effects* (95% CI) | |
| Placebo | Difference with iron compared to placebo | ||||
| Change in IRLS severity scale score | 345 (7 RCTs) | ⊕⊕⊕⊝ Moderate a | ‐ | The average reduction in IRLS severity scores in the placebo group ranged from 0.8 points to 12 points | The reduction in IRLS severity scores was 3.78 points (1.31 to 6.25) lower in the iron group than in the placebo group |
| Change in any measure of restlessness | 370 (8 RCTs) | ⊕⊕⊕⊝ Moderate a | ‐ | The amount of restlessness in the iron group was on average 0.74 SDs (0.23 to 1.26) less than in the placebo group | |
| Quality of life (dichotomous measure) | 39 (2 RCTs) | ⊕⊝⊝⊝ Very low a b c | RR 2.01 (0.54 to 7.45) | Study population | |
| 450 per 1000 reported an improvement in quality of life | 454 more per 1000 (207 fewer to 2903 more) | ||||
| Change in quality of life (continuous measure) | 128 (3 RCTs) | ⊕⊝⊝⊝ Very low a b c | ‐ | The improvement in quality of life in the iron group was on average 0.51 SDs (0.15 to 0.87) higher than in the placebo group | |
| Withdrew to use other RLS medication or because of inadequate RLS symptom control | 391 (9 RCTs) | ⊕⊕⊝⊝ Low a c | RR 0.77 (0.41 to 1.47) | Study population | |
| 195 per 1000 | 45 fewer per 1000 (115 fewer to 92 more) | ||||
| Adverse events | 298 (6 RCTs) | ⊕⊕⊕⊝ Moderate a | RR 1.48 (0.97 to 2.25) | Study population | |
| 260 per 1000 | 125 more per 1000 (8 fewer to 325 more) | ||||
| Drop out due to adverse event | 398 (9 RCTs) | ⊕⊕⊝⊝ Low a c | RR 1.91 (0.50 to 7.26) | Study population | |
| 16 per 1000 | 14 more per 1000 (8 fewer to 98 more) | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; IRLS: International Restless Legs Scale; RCT: randomised controlled trial; RR: risk ratio; SD: standard deviation | |||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | |||||
a We downgraded one level for publication bias for several reasons: 1) one study completed in 2012 (NCT00685815) for which published results could not be found in the search; 2) generally small sample sizes; and 3) the majority of participants were in trials funded by pharmaceutical companies. bWe downgraded one level for the possibility of selective outcome reporting, as this outcome was infrequently reported across studies. cWe downgraded one level because the Optimal Information Size (OIS) calculation suggests insufficient power for this outcome.
Background
Description of the condition
Restless legs syndrome (RLS, also known as Willis‐Ekbom Disease) is a common neurologic condition consisting of four cardinal features: an urge to move the legs (which is usually but not invariably associated with unpleasant leg sensations); at least transient relief with movement; worsening with rest; and a predilection to occur during the evening and night. These symptoms must not be better accounted for by another disorder that mimics RLS (Allen 2014). The diagnosis is one of clinical judgment, with no definitive confirmatory testing presently available. However, the presence of periodic limb movements, a response to dopaminergic medications, and a positive family history can all provide supportive evidence for the diagnosis (Allen 2003). Periodic limb movements are repetitive movements of the limb, most often flexion of the great toe and ankle, that occur with a periodicity between 5 and 90 seconds. Periodic limb movements are seen in 80% to 90% of people with RLS (Montplaisir 1997; Trotti 2009), but they are not specific to RLS (Hornyak 2006).
RLS is more common in women than in men (Berger 2004), and the prevalence of RLS increases with age (Bliwise 2006). RLS has a prevalence of 5% to 15% in populations of western European descent but lower prevalence in other investigated populations, such as subsets of Asia (0.1% to 5%) (Stefansson 2007). RLS has long been suspected to have a genetic basis because of the high proportion of sufferers who have a positive family history. Familial linkage studies have identified numerous potentially causative regions (Trotti 2008). Genome‐wide association studies have found single nucleotide polymorphisms in six different genes that confer increased risk for RLS, periodic limb movements of sleep, or both, including BTBD9, MEIS1, MAP2K5, SKOR1, PTPRD, and TOX3 (Schormair 2008; Stefansson 2007; Winkelmann 2007; Winkelmann 2011). Collectively, the population attributable risk for these variants is approximately 80% (Rye 2015).
Despite these genetic advances, the pathophysiology of RLS has yet to be fully elaborated. What is known about the functions of the recently implicated genes does not yet explain RLS pathology, although both BTBD9 and MEIS1 are now known to interact with iron and dopamine homeostasis, both implicated in RLS (Rye 2015). From a clinical standpoint, a state of dopaminergic dysfunction is suspected to cause RLS because people with RLS frequently improve when given low doses of dopaminergic medications (Allen 2004). More recently, hypotheses have moved from postulating a state of dopamine deficiency to one of dopamine dysregulation, potentially mediated through deficiencies in central nervous system iron (Earley 2014).
Description of the intervention
Iron therapy has been used for people with RLS, both those with and those without documented peripheral iron deficiency. Iron supplementation can be provided orally or intravenously, with several formulations available for each method of delivery. Intravenous iron provides the advantage of replenishing iron stores more quickly than oral therapy, which can take weeks to months, and a lower rate of gastrointestinal side effects (Avni 2015). In meta‐analysis, intravenous iron is associated with severe infusion reactions (with a number needed to treat for an additional harmful outcome of 255; i.e. one severe infusion reaction is expected to happen for every 255 participants receiving intravenous iron compared with placebo). However, the overall risk of serious adverse events is not increased with the use of intravenous iron (Avni 2015).
How the intervention might work
Iron deficiency has been implicated in the pathophysiology of RLS based on the clinical findings that people with iron deficiency anaemia have a high frequency of RLS (32%, with clinically significant disease in 24%; Allen 2013), and that severity of iron deficiency correlates with the severity of RLS symptoms (Earley 2000). Treatment with dopamine agonists is sometimes complicated by a phenomenon known as augmentation, in which symptoms return with earlier time of onset, greater severity, and more extensive bodily involvement (Allen 2003); this treatment complication appears more likely to occur in those people who have iron deficiency (Trenkwalder 2008). Iron exhibits a circadian pattern similar to RLS symptoms; serum iron nadirs occur between 8 pm and midnight, in line with the peak time of RLS symptom severity (Earley 2000). Studies of iron in people with RLS have demonstrated low cerebrospinal fluid iron levels (Earley 2000), low iron concentrations in the substantia nigra on magnetic resonance imaging (Allen 2004), and decreased substantia nigra iron stores on autopsy specimens (Connor 2003). Additionally, iron has known interactions with dopamine, acting as a cofactor for tyrosine hydroxylase, the rate‐limiting enzyme in dopamine production. Iron deficient rodents have been shown to have altered dopamine functioning, with increases in presynaptic dopamine, decreased dopamine transporter functioning and dopamine clearance, and elevated levels of extracellular dopamine in the caudate nucleus and putamen (Earley 2000; Earley 2014; Nelson 1997).
Why it is important to do this review
Current consensus guidelines put forth by the RLS Foundation's Medical Advisory Board recommend iron replacement therapy for people with a low ferritin level (less than 20 micrograms per litre) and consideration of iron therapy, on a case‐by‐case basis, for those with a ferritin level below 75 micrograms per litre (Silber 2013). However, previous meta‐analyses have found insufficient evidence to determine whether iron is beneficial (Trotti 2012).
Objectives
To evaluate the efficacy and safety of oral or parenteral iron for the treatment of restless legs syndrome (RLS) when compared with placebo or other therapies. The PICO question formulation was, "In people with RLS, does iron improve RLS‐related symptoms and signs, compared to placebo or other interventions."
Methods
Criteria for considering studies for this review
Types of studies
We searched for all controlled trials investigating the treatment of restless legs syndrome (RLS) with oral or parenteral iron versus placebo, versus another drug, or with a no‐intervention control group. We planned to include controlled trials regardless of whether or not they were randomised or blinded. We planned to include parallel and cross‐over trials, but not the second phase of cross‐over trials because washout periods are not universally used or may not be long enough. Trials that allowed concurrent use of other medications, such as dopamine agonists, anticonvulsants or others were considered suitable for inclusion if they allowed equal access to such medications for participants in the iron and control groups.
Types of participants
We sought trials on adult participants (18 years or over) of either sex, in whom RLS was diagnosed according to expert clinical interview or to explicit diagnostic criteria, such as those defined by the International Restless Legs Syndrome Study Group (IRLSSG; Allen 2003). We planned to include trials on pregnant women or people with renal disease (including those with end‐stage renal disease who are on dialysis) and use these in the investigation of study heterogeneity.
Types of interventions
Therapy with any dose or regimen of oral or parenteral iron‐containing compounds compared with placebo, other drugs, or no intervention.
Types of outcome measures
Primary outcomes
The primary outcome considered in this review was restlessness or unpleasant sensations, as experienced subjectively by the participant. We did not prespecify a rating scale or other measure of restlessness, although the majority of studies employed the International Restless Legs Syndrome Study Group severity scale (IRLS; Walters 2003). This 10‐question, 40‐point scale addresses the severity and impact of RLS symptoms, with higher scores indicating more severe symptoms.
Secondary outcomes
Efficacy‐related outcomes
Quality of life measures
Patient satisfaction with treatment
PLM index (number of periodic limb movements per hour of sleep)
Sleep quality (subjective and objective)
Daytime functioning
Decreased occurrence of augmentation (according to the definition in Allen 2003)
Safety‐related outcomes
Adverse events during treatment
Discontinuation rate due to adverse events
Search methods for identification of studies
Electronic searches
We searched the following databases: MEDLINE, Embase, CINAHL, PsychINFO (all for the period January 1995 through to September 2017); and the Cochrane Central Register of Controlled Trials (CENTRAL, in the Cochrane Library, most recently available issue at the time of the search). The lower time period limit was set to 1995 because generally accepted diagnostic criteria did not exist until that date (see Walters 1995).
Our MEDLINE search used the Cochrane Highly Sensitive Search Strategy for identifying randomised trials (2008 revision) along with MESH headings and free‐text searches designed to identify studies of iron administration and of participants with restless legs syndrome with high sensitivity (Appendix 1). We adapted the MEDLINE search as necessary for use in the other databases searched.
Searching other resources
We checked the reference lists of included studies for other potentially relevant publications in any language. We contacted the corresponding authors of RCTs and selected members of the International Restless Legs Syndrome Study Group to attempt to find additional published and unpublished trials during the initial search. We searched for unpublished, or ongoing trials, or both, in the following registries: US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov), Australia New Zealand Clinical Trials Registry (www.anzctr.org.au), CenterWatch Clinical Trials Listing Service (https://www.centerwatch.com/clinical‐trials/listings/), Chinese Clinical Trial Registry (http://www.chictr.org.cn/searchprojen.aspx), EU Community Research & Development Information Service (https://cordis.europa.eu/search/advanced_en), EU Clinical Trials Register (https://www.clinicaltrialsregister.eu/ctr‐search/search), International Clinical Trials Registry Platform (WHO, http://apps.who.int/trialsearch/), Hong Kong Clinical Trials Register (http://www.hkuctr.com/search), Clinical Trials Registry‐India (http://www.ctri.nic.in/Clinicaltrials/advancesearchmain.php), South African National Clinical Trial Register (http://www.sanctr.gov.za/SAClinicalTrials/tabid/169/Default.aspx), and the UK Clinical Trials Gateway(https://ukctg.nihr.ac.uk/clinical‐trials/search‐for‐a‐clinical‐trial/).
Data collection and analysis
Selection of studies
Two review authors independently used the titles and abstracts of the identified citations to exclude publications that clearly did not meet the inclusion criteria of the review. If either reviewer thought that the publication might possibly meet the criteria, the full paper was obtained for further examination. The same two review authors then reviewed articles that passed this initial screen to determine their fit with the review inclusion criteria. Authorship and results were not blinded. We resolved all types of disagreement by discussion and consensus. A PRISMA flowchart (http://www.prisma‐statement.org/PRISMAStatement/FlowDiagram.aspx) was created to detail the inclusion/exclusion process.
Data extraction and management
We developed a data extraction form to aid in the collection of relevant data from included studies. As described above in Criteria for considering studies for this review, we abstracted data on participants, interventions, and outcomes. We also abstracted on to this form the trial characteristics to be used in our assessment of methodological quality. In addition, we collected data on potential effect modifiers, including comorbidities such as end‐stage renal disease, baseline iron status, and pregnancy. Two review authors independently extracted and cross‐checked the data; we handles disagreements by consensus. We contacted study authors to obtain unpublished information when necessary, including outcome data not explicitly stated in the published papers. In cases where data were not presented as means and standard deviations (SDs), we performed additional calculations to allow inclusion in meta‐analyses. Specifically, if only medians and interquartile ranges were provided, we estimated means and SDs as described in Wan 2014.
Assessment of risk of bias in included studies
Two review authors assessed the methodological quality of each trial, using the domain‐based evaluation outlined in the chapter 'Assessing risk of bias in included studies' in the Cochrane Handbook for Systematic Reviews of Interventions (see sections 8.3‐8.15; Higgins 2011). We used the kappa statistic to assess agreement among the review authors regarding quality of the retrieved articles, resolving disagreements by discussion and consensus. In keeping with current Cochrane Handbook guidance (section 8.15), funding by pharmaceutical company was not included in the risk of bias unless there was any suggestion that study design, analysis, or conclusion was influenced by that funding. Information about study funding is included in Characteristics of included studies tables.
Measures of treatment effect
We analysed continuous data using mean differences (MDs) where possible, and performed standardised mean difference (SMD) analyses when different measurements were used across studies. SMD was calculated as (SMD = difference in mean outcome between groups/SD of outcome among participants). We calculated risk ratios (RRs) for dichotomous data using the Mantel‐Haenszel method and 95% confidence intervals (CIs). Where possible, we performed intention‐to‐treat analyses to control attrition bias.
Unit of analysis issues
We planned to include only the first period of cross‐over trials. In studies in which multiple timepoints of outcome measurement were used, we selected the timepoint that was most similar to timepoints measured in other included studies.
Dealing with missing data
Missing outcome data from individual studies are discussed in the risk of bias assessments.
Assessment of heterogeneity
We analysed study heterogeneity using the I2 statistic.
We planned to investigate the following as potential sources of heterogeneity when sufficient data were available.
Different formulations of oral or parenteral iron.
Comparator.
Duration of treatment.
Patient characteristics, including pregnancy or end‐stage renal disease.
Baseline levels of ferritin or other documentation of iron deficiency.
Assessment of reporting biases
We planned to construct a funnel plot to identify possible publication bias if we identified sufficient numbers of trials (i.e. 10 or more assessing the same outcome).
Data synthesis
We generated effect estimates using random‐effects meta‐analyses included in Review Manager version 5.3, which uses the DerSimonian‐Laird meta‐analytic method.
We considered risk of bias, inconsistency, indirectness, imprecision, publication bias, magnitude of effect, dose‐response gradient, and influence of plausible residual confounding to generate an assessment of certainty, using the GRADE framework (Guyatt 2011; tools at https://gradepro.org/). Imprecision was assessed by calculating Optimal Information Size (OIS) to evaluate if included sample sizes were sufficiently powered for each outcome included in the Summary of Findings table.
Subgroup analysis and investigation of heterogeneity
We prespecified subgroup analyses to examine the effects of different types of participants (e.g. pregnant women or people with end‐stage renal disease) and different formulations of iron (oral versus parenteral).
Sensitivity analysis
We planned to conduct sensitivity analyses for high‐ versus low‐quality trials and for parallel group versus cross‐over trial designs, if we identified sufficient numbers of trials.
Results
Description of studies
Results of the search
The searches yielded 1361 potentially relevant articles; 1040 after removal of duplicates (see Figure 1). Of these, we excluded 1009 after review of title, abstract, or www.clinicaltrials.gov posting because they did not meet the inclusion criteria. We reviewed the full text of 31 studies. Four studies were ongoing or were completed but had released insufficient data to allow inclusion at the time of this review (e.g. unpublished, no data could be obtained); these are included in the Characteristics of ongoing studies section below. Of the 27 remaining studies, 10 met the criteria for inclusion (Allen 2011; Cho 2016; Davis 2000; Deng 2016; Earley 2009; Grote 2009; Lee 2014; Sloand 2004; Trenkwalder 2017; Wang 2009), for a total of 428 participants. Nine studies used a placebo comparator and we included them in a quantitative meta‐analysis. We included the study using pramipexole as a comparator only in the qualitative review.
1.
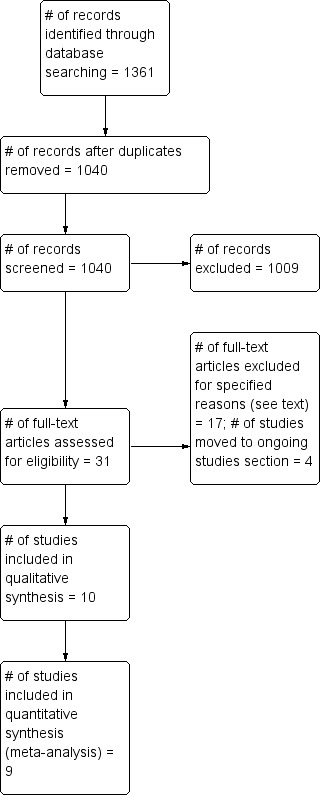
Study flow diagram.
Included studies
All 10 included studies were randomised, parallel group trials. For a comparison of key differences in study design, see Table 2. Nine compared iron to placebo and one compared iron to a dopamine agonist (Lee 2014). Resless legs syndrome (RLS) was defined using the 1995 International Restless Legs Syndrome Study Group criteria (IRLSSG) in three studies (Deng 2016; Sloand 2004; Walters 1995), the 2003 IRLSSG criteria in six studies (Allen 2003; Allen 2011; Grote 2009; Lee 2014; Trenkwalder 2017; Wang 2009), the Hopkins telephone diagnostic interview for RLS in three studies (Hening 2003; Cho 2016; Earley 2009), and by clinical interview by a neurologist in one study (Davis 2000). In this latter study, 24 of 28 participants met all four diagnostic criteria for RLS using the 1995 criteria. Four studies included only participants with low or low‐normal iron stores, defined as: serum ferritin < 45 ng/mL (Grote 2009); serum ferritin 15‐50 ng/mL (Lee 2014); serum ferritin 15‐75 ng/mL (Wang 2009); or serum ferritin < 75 ng/mL or the combination of serum ferritin 75‐300 ng/mL and a transferrin saturation < 20% (Trenkwalder 2017). Two studies included only participants on dialysis (haemodialysis or peritoneal dialysis) (Deng 2016; Sloand 2004), while renal disease was an exclusion criterion for most other studies. No study reported inclusion of pregnant women. Three studies administered oral iron as ferrous sulfate 325 mg twice a day (Davis 2000; Lee 2014; Wang 2009). Seven studies used intravenous iron preparations, three of which were iron sucrose (Deng 2016; Earley 2009; Grote 2009), one of which was iron dextran (Sloand 2004), and three of which were ferric carboxymaltose (Allen 2011; Cho 2016; Trenkwalder 2017). In all cases, total dosage of intravenous iron was 1000 mg, but this was usually divided into multiple doses. Our primary endpoint of restlessness or unpleasant sensations was evaluated in nine of the included studies, using the IRLS in eight (Allen 2011; Cho 2016; Deng 2016; Earley 2009; Grote 2009; Lee 2014; Trenkwalder 2017; Wang 2009), and a scale developed at the University of Rochester in one (Sloand 2004). The remaining study (Davis 2000), the earliest of the included studies, assessed the effect of treatment on sleep and quality of life, but did not explicitly assess restlessness. Four studies were funded by the pharmaceutical companies selling the iron formulations tested in the studies (Allen 2011; Cho 2016; Grote 2009; Trenkwalder 2017).
1. Key study characteristics.
| Study | Measure of restlessness | Comparator | IV or oral iron | Type of iron | Baseline iron status |
Study population (if RLS plus another condition) |
Time of assessment used |
| Allen 2011 | IRLS | Placebo | IV | Ferric carboxymaltose | Not an inclusion/exclusion criterion (unless > 300 ng/mL); mean ferritin 40.6 ng/mL |
23 days | |
| Cho 2016 | IRLS | Placebo | IV | Ferric carboxymaltose | Not an inclusion/exclusion criterion (unless > 300 ng/mL); mean ferritin 61.4 ng/mL |
4 weeks | |
| Davis 2000 | Not measured | Placebo | Oral | Ferrous sulfate | Excluded if haemoglobin < 10 g/dL; mean ferritin 117.7 ng/mL | 12‐14 weeks | |
| Deng 2016 | IRLS | Placebo | IV | Iron sucrose | For inclusion, serum ferritin < 200 ng/mL and transferrin saturation < 20% | Uremia on haemodialysis at least 1 year | 2 weeks |
| Earley 2009 | IRLS | Placebo | IV | Iron sucrose | Excluded if haemoglobin < 12 d/dL; mean ferritin 75.2 ng/mL | 2 weeks | |
| Grote 2009 | IRLS | Placebo | IV | Iron sucrose | For inclusion, serum ferritin < 45 ng/mL | 3 weeks | |
| Lee 2014 | IRLS | Pramipexole | Oral | Ferrous sulfate | For inclusion, serum ferritin 15‐50 ng/mL | 12 weeks | |
| Sloand 2004 | University of Rochester | Placebo | IV | Iron dextrose | Not an inclusion/exclusion criterion; median ferritin 136.3 ng/mL | End‐stage renal disease on dialysis |
2 weeks |
| Trenkwalder 2017 | IRLS | Placebo | IV | Ferric carboxymaltose | For inclusion, serum ferritin < 75 ng/mL or both ferritin 75‐300 ng/mL and transferrin saturation < 20% | 4 weeks | |
| Wang 2009 | IRLS | Placebo | Oral | Ferrous sulfate | For inclusion, serum ferritin 15‐75 ng/mL | 12 weeks |
IRLS: International Restless Legs Scale IV: intravenous
In the earliest trial (Davis 2000), 28 participants were randomised to receive either placebo or oral ferrous sulfate liquid, 325 mg twice a day for 16 weeks, at which point participants who wished to continue the study drug as monotherapy were followed for an additional 10 weeks. Iron status and renal function at baseline were not part of the inclusion or exclusion criteria. RLS symptoms were measured with two visual analogue scales, the first which quantified the extent to which RLS symptoms interfered with sleep and the second which quantified how RLS symptoms affected each participant's life, recorded over two weeks at baseline and after 12 weeks. This study was supported by a grant from the National Institutes of Health.
In the second trial (Sloand 2004), 25 participants with end‐stage renal disease on dialysis (22 on haemodialysis, 3 on peritoneal dialysis) were randomised to receive either intravenous iron dextran or placebo. Both interventions were given as a 15 mL test dose (30 mg of iron dextran) over three minutes followed by one hour of observation for adverse reactions; if no adverse reactions were noted, the remaining 485 mL (970 mg of iron dextran) was infused over three hours. RLS symptoms were measured at baseline, one week, two weeks, and four weeks after infusion using the University of Rochester RLS severity scale developed for this study. This three‐question scale assesses frequency of RLS symptoms within the last two days, the amount of distress caused by RLS symptoms, and the duration of symptoms to generate a score from 0 to 10‐point scale (with higher numbers corresponding to increased RLS severity). The funding source for this study was not reported.
In the Earley 2009 trial, 21 participants were randomised to receive either intravenous iron or placebo. A prespecified interim analysis was performed after 18 participants had been enrolled, at which point the study was discontinued because of lack of effect of the intervention, so three of the randomised participants did not complete the protocol. Intravenous iron was given as iron sucrose, 500 mL (containing 500 mg iron sucrose) over 10 hours, followed by a second infusion over 12 hours the following day. The same infusion schedule of saline was given to the placebo group. IRLS scores were measured at baseline and approximately two weeks following the intervention. Other outcome measures included a global rating scale of RLS severity, periodic limb movements during wake and sleep, changes in cerebrospinal fluid ferritin and transferrin levels, objective sleep quality (total sleep time and sleep efficiency during polysomnography), and changes in iron index within the substantia nigra on magnetic resonance imaging (MRI). This study was funded by grants from the National Institutes of Health.
Grote 2009 randomised 60 participants, all of whom were iron deficient (based on a serum ferritin less than or equal to 45 ng/mL), to receive either intravenous iron or placebo. Iron was delivered as 200 mg of iron sucrose (10 mL of 20 mg/mL Venofer), given five times over a three‐week period. The placebo group received the dosing schedule of 0.9% NaCl. The IRLS scale was measured at baseline, week 3, week 7, week 11, five months, eight months, and 12 months. Serum ferritin and the Epworth Sleepiness Scale (Johns 1991) were both measured as well. This study was supported by Renapharma (manufacturer of Venofer).
Wang 2009 randomised 18 participants with low or low‐normal ferritin levels (serum ferritin 15‐75 ng/mL) to receive either oral iron (ferrous sulfate 325 mg bid) or matched placebo for 12 weeks. IRLS scores were measured at baseline, six weeks, and 12 weeks after the intervention. Serum ferritin was also measured at 12 weeks, as was a single question regarding change in quality of life compared to prior to beginning the study medication (rated as improved, stayed the same, or worsened). Compliance (based on manual pill count) was measured at six and 12 weeks. The funding source for this study was not reported.
Allen 2011 enrolled 46 participants, of whom 43 received all doses of study medication. Participants were randomised to receive either intravenous ferric carboxymaltose or placebo. Iron was delivered as 500 mg of ferric carboxymaltose in 100 mL of normal saline, given on day 0 and day 5. Normal saline was given using the same volume and schedule to participants in the placebo group. Following day 28, participants were assigned to receive ferric carboxymaltose or normal saline based on their serum ferritin and IRLS scores at day 28. Because the treatment assignation at day 28 was not randomised (although it remained blinded), we only considered data gathered before the treatment given on day 28. IRLS scores were measured at baseline, day 14, and day 28. Other outcome measures included the RLS Quality of Life (RLS‐QoL) scale (Abetz 2005), the Medical Outcomes Study sleep scale (a subjective measure of sleep quality, Hays 1992), periodic limb movements (measured via leg actigraphy), the Clinical Global Impression of Change (Guy 1976), a patient global rating of change (the PGI‐C, Guy 1976), and the Fatigue Severity Scale (Krupp 1989). This study was supported by Luitpold Pharmaceuticals (manufacturer of ferric carboxymaltose).
Lee 2014 randomised 30 participants with low‐normal ferritin levels (15‐50 ng/mL) to either oral iron (ferrous sulfate, 325 mg twice a day) or the dopamine agonist pramipexole (beginning dose 0.25 mg (salt) at bedtime, with titration during the study period based on effect and tolerability). Participants and study personnel were not blinded to treatment allocation. IRLS scores were measured at baseline and at weeks 2, 4, 8, and 12. Serum ferritin, subjective sleep quality, daytime sleepiness, and depressive symptoms were also measured. This study was funded by a grant through the Seoul National University Bundang Hospital.
Cho 2016 randomised 64 participants to receive either a single dose of intravenous ferric carboxymaltose (1000 mg in 100 mL normal saline, infused over 15 minutes) or normal saline placebo infused in the same manner. IRLS scores were completed at baseline and at four and six weeks after infusion. Other outcome measures included the Pittsburgh Sleep Quality Index (Buysse 1989), a visual analogue scale of RLS severity, the RLS‐QoL, and the Short Form‐36 Health Survey (SF‐36, Ware 1992). Following collection of data six weeks post‐infusion, participants who received placebo were offered ferric carboxymaltose and all participants were followed in an unblinded fashion through week 30. For these analyses, only data from the initial, randomised, blinded six weeks of the study were included. Grant support for this work was provided by JW Pharmaceutical, and drug support for this work was provided by Vifor Pharma (manufacturer of ferric carboxymaltose).
Trenkwalder 2017 randomised 110 participants with moderate to severe RLS, who were iron‐deficient but non‐anaemic, to either a single dose of intravenous ferric carboxymaltose (1000 mg) or placebo, infused over 15 +/‐ 2 minutes. IRLS scores were collected at baseline, and weeks 1, 4, 8, and 12. Other collected outcome measures included the Clinical Global Impression of Severity (CGI‐S, Guy 1976), the PGI‐C, the RLS‐6 rating scale (Kohnen 2004), the RLS‐QoL, the Medical Outcomes Study sleep scale (items assessing satisfaction with sleep and degree of daytime tiredness). This study was supported by Vifor Pharma (manufacturer of ferric carboxymaltose).
Deng 2016 randomised 32 participants, all of whom had renal disease on stable haemodialysis treatment for at least 12 months and a diagnosis of RLS. Participants were required to have a baseline serum ferritin < 200 ng/mL and a transferrin saturation < 20%. Participants received either 100 mg of intravenous iron sucrose three days per week for a total of 10 doses, or placebo normal saline of the same volume (50 mL). IRLS was assessed at baseline and two weeks following the final infusion. This study was supported by departmental sources.
Excluded studies
We excluded the remaining trials because of one or more of: 1) lack of any control group or use of a different formulation or dose of iron as the control group (Birgegard 2010; Cho 2011; Earley 2004; Earley 2005; Ekermo 2013; Macher 2015; Mohri 2008; NCT00895232; O'Keeffe 1994; Ondo 2010; Simakajornboon 2003; Zhang 2014; Zilberman 2010), or 2) participant age younger than 18 (Konofal 2008; Mohri 2008; Simakajornboon 2003), or 3) study performed prior to standard RLS criteria definition in 1995 (O'Keeffe 1994),or 4) duplicate publication of same trial (Halterman 2007), 5) absence of original trial data (Auerbach 2014), or 6) use of a combined iron/folate intervention compared to a control group receiving neither folate nor iron (Vishwakarma 2013).
Risk of bias in included studies
Several of the studies had incomplete reporting, which limited our assessment of potential bias (Figure 2). The Kappa for agreement between two reviewers about risk of bias was 0.55. We resolved all disagreements by discussion and consensus.
2.
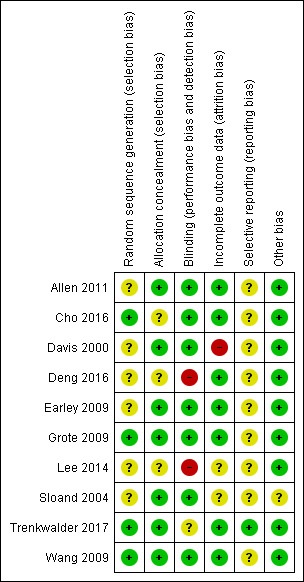
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Sequence generation was not clearly described in six of the studies (Allen 2011; Davis 2000; Deng 2016; Earley 2009; Lee 2014; Sloand 2004), and allocation concealment was unclear in three (Cho 2016; Deng 2016; Lee 2014).
Blinding
Two studies were unblinded by design (Deng 2016; Lee 2014), and one study was reported to be blinded but did not clearly state how the appearance of the intravenous injection was obscured or matched (Trenkwalder 2017).
Incomplete outcome data
Incomplete outcome data were a potential problem in three studies (Davis 2000; Lee 2014; Sloand 2004). In the study by Davis et al, six of 14 iron‐treated participants but only one of 14 placebo‐treated participants withdrew before analysis at 14 weeks (the time of primary outcome measurement) and no imputation of missing values was performed. In the Lee study, four of 15 participants in the pramipexole group dropped out due to medication side effects, but no participants dropped out of the iron group for this reason. Sloand et al reported two dropouts in the placebo group but reported outcome data for the entire group, without a clear discussion of how outcome data were imputed for the participants who dropped out.
Selective reporting
It is difficult to fully rule out the possibility of selective outcome reporting in any of the trials for which we were unable to find published protocols (Cho 2016; Davis 2000; Deng 2016; Earley 2009; Lee 2014; Sloand 2004; Wang 2009). Two additional trials had publicly accessible trial protocols (at ClinicalTrials.gov and www.controlled‐trials.com, respectively; Allen 2011; Grote 2009), but the date of registration appeared to be after the end date of the trials.
Other potential sources of bias
The intervention groups were imbalanced with respect to important potential confounders in one study (Sloand 2004), with mean baseline RLS severity scores being two points higher (out of a possible 10) in the placebo group and with duration of dialysis being longer in the placebo group (3.3 versus 2.5 years). Both of these could potentially indicate more severe disease in the placebo group, which might be more refractory to therapy.
Effects of interventions
See: Table 1
The included studies did not all report the same outcome measures. For our primary outcome measure, subjective restlessness or leg discomfort experienced by the patient, data were available from nine studies. Eight of these studies used the IRLS (Allen 2011; Cho 2016; Deng 2016; Earley 2009; Grote 2009; Lee 2014; Trenkwalder 2017; Wang 2009), and the ninth used a severity scale developed specifically for use in the trial (Sloand 2004). Several studies measured our primary outcome at multiple time points. For the purpose of comparing changes in restlessness across studies, we attempted to pick a time of assessment that was as consistent as possible across studies. As a result, we analysed changes in scores between two to four weeks after the intervention for intravenous iron, with the two‐week measurement determined by the Earley 2009 and Deng 2016 studies, in which this was the only time point available, and the four‐week measurement determined by the Cho 2016 study, as this was the earliest available time point after the intervention. Time points between two to four weeks were then chosen for the intravenous iron studies of Sloand 2004 (2 weeks), Grote 2009 (3 weeks), Allen 2011 (23 days after infusion completion), and Trenkwalder 2017 (4 weeks). For oral iron studies, we compared change as measured at 12 weeks, reported in both the Wang 2009 and Lee 2014 studies, and as measured from 12 to 14 weeks in the Davis 2000 study. We considered secondary outcome measures for these same time points, if reported, or for the closest alternate time point when not available.
Iron versus placebo
Nine studies compared iron to placebo. Eight of these studies assessed our primary outcome, i.e. severity of restlessness. Of these eight studies, seven could be combined with random effects meta‐analysis of change in IRLS scores from baseline. Iron decreased IRLS severity scores significantly more so than did placebo, with a MD in change in IRLS of ‐3.78 (95% CI ‐6.25 to ‐1.31; I2 = 66%, 7 studies, 345 participants, Analysis 1.1). Data from the Sloand 2004 study were presented as medians and interquartile ranges for the University of Rochester severity scale, from which we estimated means and standard deviations (SDs), using methodology described by Wan 2014. For all these eight studies together, the standardised mean difference (SMD) in change in severity was ‐0.74 (95% CI ‐1.26 to ‐0.23; I2 = 80%, 8 studies, 370 participants, Analysis 1.2) for iron compared to placebo. We rated the certainty regarding these effects of iron versus placebo as moderate (Table 1).
1.1. Analysis.
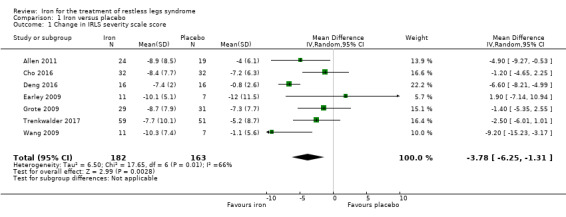
Comparison 1 Iron versus placebo, Outcome 1 Change in IRLS severity scale score.
1.2. Analysis.
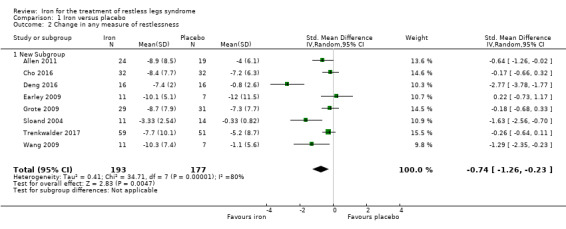
Comparison 1 Iron versus placebo, Outcome 2 Change in any measure of restlessness.
Considering secondary outcomes, changes in quality of life with treatment were assessed in five studies (Allen 2011; Cho 2016; Davis 2000; Trenkwalder 2017; Wang 2009). There was no difference in change in quality of life between the treatment and placebo groups in studies using a dichotomised measure of improved versus unchanged or worsened (risk ratio (RR) 2.01, 95% CI 0.54 to 7.45; I2 = 54%, 2 studies, 39 participants, Analysis 1.8; Davis 2000; Wang 2009), but there was an improvement in quality of life measured as a continuous variable (SMD 0.51, 95% CI 0.15 to 0.87; I2 = 0%, 3 studies, 128 participants, Analysis 1.9; Allen 2011; Cho 2016; Davis 2000). Trenkwalder 2017 also reported significant improvements in several individual quality of life measures contained in the RLS‐QoL. We rated the certainty regarding these effects of iron versus placebo as very low.
1.8. Analysis.
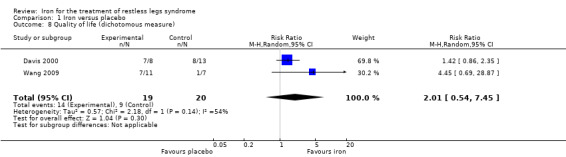
Comparison 1 Iron versus placebo, Outcome 8 Quality of life (dichotomous measure).
1.9. Analysis.
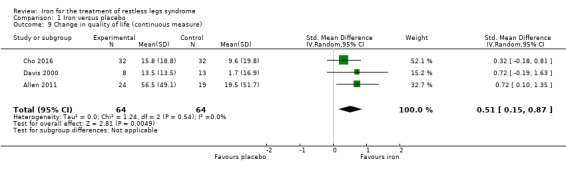
Comparison 1 Iron versus placebo, Outcome 9 Change in quality of life (continuous measure).
All nine studies comparing iron to placebo assessed patient satisfaction, either directly or indirectly. In two of the studies, satisfaction was measured directly at a certain time point, when participants were asked if they would prefer to remain in the study or leave the study to start different therapy for RLS (Davis 2000; Earley 2009). In the remaining seven studies, participant dropouts due to lack of efficacy of therapy were reported. Combining these two measures to determine the proportion of participants who chose to leave the study due to lack of efficacy, there was no difference between the iron and placebo groups (RR 0.77, 95% CI 0.41 to 1.47; I2 = 43%, 9 studies, 391 participants, Analysis 1.10). The Allen 2011, Deng 2016, and Wang 2009 studies had no dropouts due to lack of efficacy in either group. We rated the certainty regarding these effects of iron versus placebo as low.
1.10. Analysis.
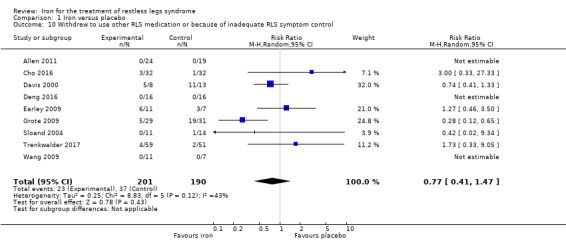
Comparison 1 Iron versus placebo, Outcome 10 Withdrew to use other RLS medication or because of inadequate RLS symptom control.
Patient impression of change using the PGI‐C was reported by two studies. In the Allen 2011 study, significantly more participants receiving iron rated themselves as much improved or very much improved (45.8% versus 9.5% with placebo, P = 0.03). In the Trenkwalder 2017 study, the PGI‐C was combined with item 2 of the CGI‐I, and significantly more participants receiving iron rated themselves as very much improved and had a CGI of much improved (43.4% versus 14.9%, P = 0.002).
Subjective sleep quality was no different between iron and placebo in the studies that reported it (SMD 0.19, 95% CI ‐0.18 to 0.56; I2 = 9%, 3 studies, 128 participants, Analysis 1.11; Allen 2011; Cho 2016; Davis 2000). Objective sleep quality, measured as sleep efficiency during polysomnography, was not significantly different between the iron and placebo groups (‐35.5 +/‐ 92.0 versus ‐41.4 +/‐ 98.2) in the single study that measured it (Earley 2009). Periodic limb movements of sleep were measured in two studies (Allen 2011; Earley 2009), by actigraphy or polysomnography. The decrease after treatment was not significantly different between the iron and placebo groups (SMD ‐0.19, 95% CI ‐0.70 to 0.32; I2 = 0%, 2 studies, 60 participants, Analysis 1.12). Daytime functioning was assessed in one study using the Epworth Sleepiness Scale, a subjective measure of propensity to fall asleep during routine activities (Grote 2009). Epworth scores were not given for the treatment groups, but were noted not to be significantly different from placebo at any time point. However, when measured in a single study by the RLS‐6, daytime tiredness was reduced by iron compared to placebo (least squares MD ‐1.5, 95% CI ‐2.5 to ‐0.6; Trenkwalder 2017). Changes in the rate of augmentation were not addressed in any of the included studies.
1.11. Analysis.
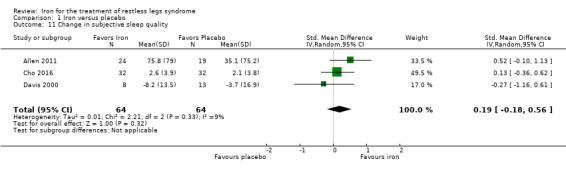
Comparison 1 Iron versus placebo, Outcome 11 Change in subjective sleep quality.
1.12. Analysis.
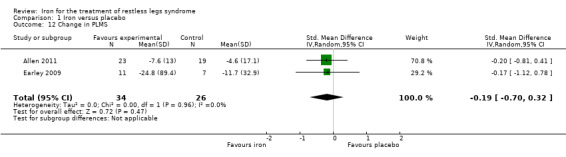
Comparison 1 Iron versus placebo, Outcome 12 Change in PLMS.
Adverse events were reported for eight of the nine studies comparing iron to placebo. In one study, no adverse events occurred in either group (Deng 2016). In five of the studies, data were reported (Davis 2000; Sloand 2004; Trenkwalder 2017), or available from the authors (L. Grote, R. Allen) by number of participants in each group to experience any adverse event. In others (Cho 2016; Earley 2009), adverse events were listed but it was not clear which adverse events were unique occurrences or when an individual participant may have had more than one adverse event. For the purpose of our meta‐analysis, therefore, we included only data from the first six studies. The risk of any adverse event was not different between the iron and placebo groups (RR 1.48, 95% CI 0.97 to 2.25; I2 = 45%, 6 studies, 298 participants, Analysis 1.13). We rated the certainty regarding these effects of iron versus placebo as moderate. Gastrointestinal side effects (nausea/vomiting, constipation, diarrhoea, and abdominal pain) were considered as unique events (i.e. counted as separate occurrences even if they occurred in the same patient) and were no more common in the iron than placebo groups (1.47, 95% CI 0.77 to 2.80; I2 = 0%, 8 studies, 380 participants, Analysis 1.14). Participants were no more likely to drop out of the study due to adverse events in the iron than the placebo group (RR 1.91, 95% CI 0.50 to 7.26; I2 = 0%, 8 studies, 380 participants, Analysis 1.15). No dropouts due to adverse events occurred in five of the studies (Allen 2011; Cho 2016; Deng 2016; Earley 2009; Wang 2009). We rated the certainty regarding this effect of iron versus placebo as low.
1.13. Analysis.
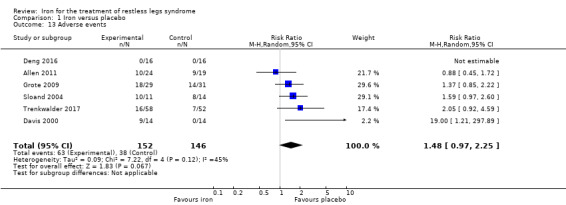
Comparison 1 Iron versus placebo, Outcome 13 Adverse events.
1.14. Analysis.
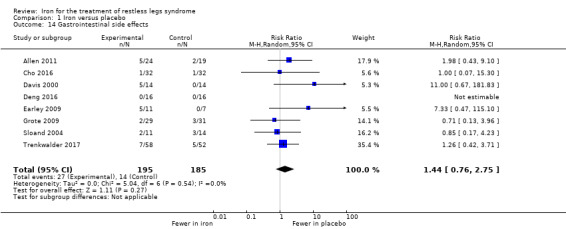
Comparison 1 Iron versus placebo, Outcome 14 Gastrointestinal side effects.
1.15. Analysis.
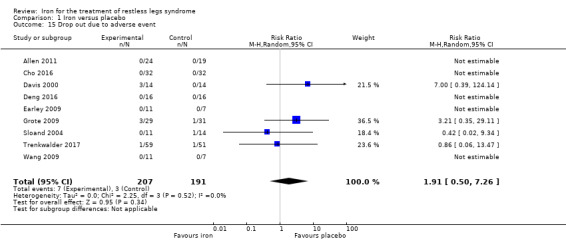
Comparison 1 Iron versus placebo, Outcome 15 Drop out due to adverse event.
Iron versus placebo ‐ subgroup analyses
Subgroup analyses were performed for those studies with participants who were on dialysis versus not on dialysis, those studies selecting for only participants with low or low‐normal baseline iron stores versus studies that did not select for iron deficiency, and for studies administering oral versus intravenous iron. We then further subdivided the intravenous iron studies by performing subgroup analysis on studies administering iron sucrose versus ferric carboxymaltose.
Two studies evaluated change in restlessness in participants on dialysis and six studies evaluated this in participants not on dialysis. While the benefit of iron over placebo was apparent for both groups, the benefit was significantly greater in studies of participants on dialysis (Chi2 = 10.16, P = 0.001, Analysis 1.3).
1.3. Analysis.
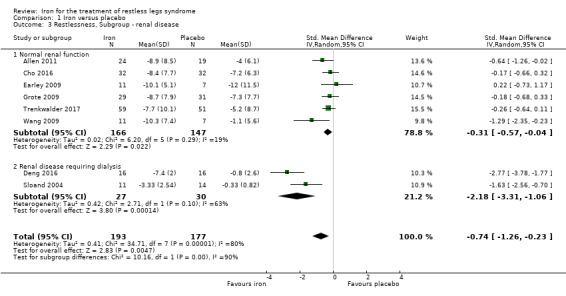
Comparison 1 Iron versus placebo, Outcome 3 Restlessness, Subgroup ‐ renal disease.
Three studies included only participants selected for low or low‐normal iron stores. There was no significant difference between change in restlessness among those selected for or not selected for iron deficiency at baseline (Chi2 1.29, P = 0.26, Analysis 1.4). Three studies additionally reported that baseline ferritin levels were not different between participants whose restlessness responded to iron therapy and those whose did not (Allen 2011; Cho 2011; Davis 2000).
1.4. Analysis.
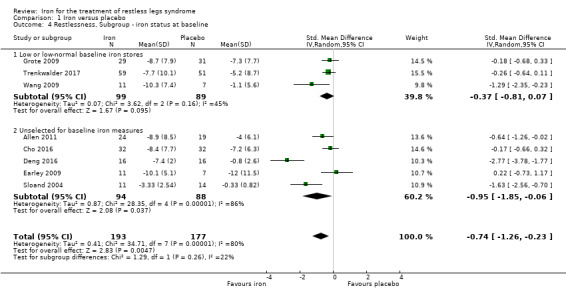
Comparison 1 Iron versus placebo, Outcome 4 Restlessness, Subgroup ‐ iron status at baseline.
Considering type of iron delivery (oral versus intravenous), there was no significant difference between decrease in restlessness in the single study using oral iron versus the seven studies using intravenous iron (Chi2 = 1.00, P = 0.32, Analysis 1.5). As a post hoc analysis, we considered iron sucrose (3 studies) versus ferric carboxymaltose (3 studies). There was no significant difference in reduction in restlessness with these two formulations of intravenous iron (Chi² = 0.48, P = 0.49, Analysis 1.6).
1.5. Analysis.
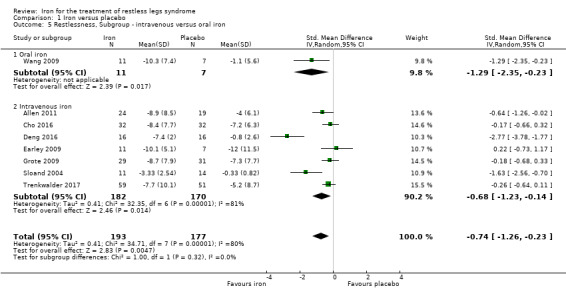
Comparison 1 Iron versus placebo, Outcome 5 Restlessness, Subgroup ‐ intravenous versus oral iron.
1.6. Analysis.
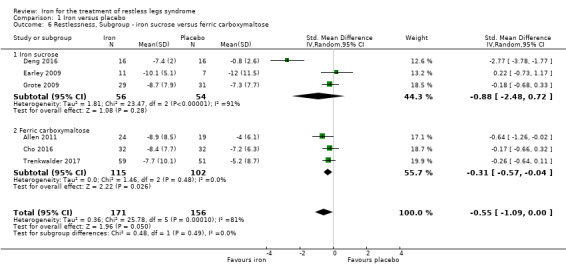
Comparison 1 Iron versus placebo, Outcome 6 Restlessness, Subgroup ‐ iron sucrose versus ferric carboxymaltose.
Iron versus placebo ‐ sources of heterogeneity
There was high heterogeneity for our primary outcome measure of restlessness for the comparison of iron versus placebo (I2 = 80%). Heterogenity decreased only modestly when considering those studies measuring restlessness with the IRLS (I2 = 66%). Heterogeneity was considerably lower among studies of participants without renal disease (I2 = 19%) than those on dialysis (I2 = 63%). Heterogeneity was somewhat lower when considering only those who were iron deficient at baseline (I2 = 45%) than those unselected for iron deficiency (I2 = 86%). Hetereogeneity remained high when considering only studies using intravenous iron (I2 = 81%), although was very low among those studies using intravenous ferric carboxymaltose (I2 = 0%).
Iron versus placebo ‐ sensitivity analysis
As a sensitivity analysis for quality of trials, we repeated our analysis of restlessness excluding trials with a high risk of bias. This demonstrated a somewhat smaller but still statistically significant benefit of iron over placebo (SMD ‐0.46, 95% CI ‐0.82 to ‐0.10; I2 = 56%, 7 trials, 338 participants, Analysis 1.7).
1.7. Analysis.
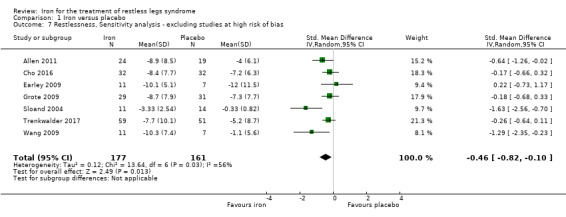
Comparison 1 Iron versus placebo, Outcome 7 Restlessness, Sensitivity analysis ‐ excluding studies at high risk of bias.
Iron versus dopamine agonist
For the single study comparing iron to a dopamine agonist (Lee 2014), change in IRLS score from baseline was no different between the iron and pramipexole groups (MD ‐0.40, 95% CI ‐5.93 to 5.13; 1 study, 30 participants). Several secondary outcomes were also not different between treatments, including change in subjective sleep quality, measured by the Pittsburgh Sleep Quality Index and daytime sleepiness measured by the Epworth Sleepiness Scale. Adverse events were reported as being significantly more frequent in the dopamine agonist group, without additional detail provided (Lee 2014). Four participants in the pramipexole group dropped out due to adverse events, while no participants in the iron group dropped out for this reason.
Discussion
Summary of main results
Iron is more effective than placebo at decreasing restlessness and restless legs syndrome (RLS) severity as measured by the International Restless Legs Scale (IRLS). The average improvement in IRLS score above that seen by placebo was 3.78 points, which is above the proposed minimal clinically important change of 2.9 to 3.2 points (Allen 2013b). However, it is lower than the change seen in meta‐analysis of dopamine agonists versus placebo for RLS (4.2 points with ropinirole, 5.2 points with pramipexole, and 7.0 points with rotigotine (Scholz 2011)). Assessment of the effect of iron on secondary outcomes was limited by small numbers of studies collecting each secondary outcome, and we rated the certainty level for most secondary outcomes as low or very low. However, available data indicate that iron might be superior to placebo for improving some, but not all, measures of RLS‐related quality of life and are conflicting as to whether iron is superior to placebo in improving daytime sleepiness in participants with RLS. Subjective and objective sleep quality were no more improved by iron than by placebo in included studies.
Subgroup analyses indicated that participants on dialysis may be more likely to benefit from iron therapy than participants without renal disease, but there were no significant subgroup effects by baseline iron measures or type of iron administered. However, subgroup analyses are based on relatively small numbers of small studies, e.g. the subgroup of participants included in intravenous iron trials totaled 352, versus only 18 participants with oral iron. Thus, subgroup analyses should be considered exploratory only.
Although current practice guidelines recommend replacing iron in people with RLS when serum ferritin levels are < 75 ng/mL (Silber 2013), most of the included studies were not limited to participants with serum ferritin values in this range and three studies reported that iron responders and non‐responders did not differ by baseline iron status. Further data are needed to determine the role of baseline iron deficiency in selecting people for RLS treatment with iron.
One included study compared iron with an established active treatment (Lee 2014), i.e. the dopamine agonist pramipexole, rather than to placebo. This study found no difference between iron and pramipexole in reduction of RLS severity. This indirectly supports a clinical benefit of iron for RLS treatment, as dopamine agonists are known to significantly reduce RLS severity compared to placebo. However, the width of the confidence interval (CI) around the mean difference (MD) between these two therapies in the included study was quite wide, such that one of these two treatments may have clinical superiority.
Adverse events were no more common with iron therapy than placebo, but may be less common with iron than with a dopamine agonist (as reported by the single study of Lee 2014). Although it could not be fully assessed in our review, there may be differences in tolerability between oral and intravenous iron for the treatment of RLS. Tolerability may also be influenced by factors other than route of administration (e.g. formulation of iron).
Overall completeness and applicability of evidence
The total number of participants included in all studies included in this review was relatively low at 428, and half of the included studies had 30 participants or fewer. Secondary outcomes were each included in only a few trials, limiting assessment of these clinically‐important secondary outcomes. Insufficient power and concern about possible publication bias based on the presence of mostly small, often industry‐sponsored trials, resulted in downgrading of confidence levels in results. Larger, well‐designed studies are clearly needed to allow confidence in the estimate of treatment benefit from iron, to understand the effect of iron on secondary outcomes, and to evaluate the role of group differences (e.g. baseline iron status).
Quality of the evidence
Assessment of trial quality was hampered by incomplete reporting of study design, in part likely reflecting evolving guidelines for clinical trial reporting since the earliest included studies were published. Using available data, several studies had potentially high risks of bias, related to high dropout rates without use of last observation carried forward and lack of blinding. Even in studies where dropouts were appropriately handled using intention‐to‐treat with last observation carried forward analyses, high dropout rates may have contributed to a bias toward the null, partially obscuring a true treatment effect (e.g. in Trenkwalder 2017).
Potential biases in the review process
Given the small numbers of participants involved in each trial, this review does not allow for the detection of serious but rare adverse events (e.g. severe infusion reactions with intravenous iron). Because outcomes were not assessed at the same time in each study, we chose to use the time points that were most similar for each route of iron assessment, i.e. two to four weeks for intravenous iron and 12 weeks for oral iron. In several studies (e.g. Cho 2016; Grote 2009; Trenkwalder 2017), there was no significant benefit of iron at the time point we selected for analysis, but a significant benefit was identified at other studied time points; this may have led to an underestimation of a transient or delayed benefit of iron. In other cases (e.g. Allen 2011; Sloand 2004), the time point that we selected for analysis showed a significant benefit, while other reported time points did not, which could have overestimated a benefit of iron. Optimal timing to measure the effect of oral or intravenous iron is not well characterised (Trenkwalder 2017).
Agreements and disagreements with other studies or reviews
Evidence‐based treatment guidelines for RLS are available from the American Academy of Sleep Medicine (Aurora 2012), the International Restless Legs Syndrome Study Group (specifically addressing long‐term, rather than short‐term, treatment; Garcia‐Borreguero 2013), a combined group of European neurologic and sleep societies (Garcia‐Borreguero 2012), and the American Academy of Neurology (Winkelman 2016). The American Academy of Sleep Medicine and the International Restless Legs Syndrome Study Group concluded, similar to our initial review (Trotti 2012), that iron supplementation has not been shown to be effective for RLS (Aurora 2012; Garcia‐Borreguero 2013). In contrast, the European societies considered each iron formulation separately to conclude that intravenous iron sucrose is not effective but that oral ferrous sulfate and intravenous ferric carboxymaltose are probably effective for short‐term treatment (Garcia‐Borreguero 2012). The American Academy of Neurology found moderately strong evidence in support of intravenous ferric carboxymaltose (Level B) and oral ferrous sulfate with vitamin C in those with serum ferritin < 75 ng/mL (Level B) (Winkelman 2016). A systematic review from the Agency for Healthcare Research and Quality reported moderate evidence for ferric carboxymaltose (Wilt 2013).
Authors' conclusions
Implications for practice.
Iron probably improves restlessness in people with restless legs syndrome (RLS), compared to placebo, based largely on trials of intravenous iron of moderate quality. However, insufficient data are available to directly determine whether iron or dopamine agonists are more effective or better tolerated, and no data address the question of whether iron or alpha‐2‐delta ligands are more effective or better tolerated. Thus, the decision of whether to use iron as first‐line treatment, as combination therapy with a dopamine agonist or alpha‐2‐delta ligand, or only as a second‐line medication after first‐line agents fail, cannot be fully guided by currently available evidence.
Implications for research.
Larger, high‐quality studies are needed to evaluate several key questions that are unanswered by available studies, including: 1) confirmation of the benefit of iron, currently based on small studies of relatively few participants, followed for a short period of time; 2) effect of iron therapy on important secondary outcomes in participants with RLS, such as quality of life and sleep quality; 3) effect of oral iron therapy on RLS symptoms; 4) relative efficacy of different formulations of intravenous iron, e.g. ferric carboxymaltose versus iron sucrose; 5) optimal timing of iron administration and monitoring of treatment response; and 6) specific patient characteristics (e.g. baseline iron stores, renal function) that predict response to treatment. Further work is needed to evaluate both the relative efficacy of iron versus standard RLS treatments and the potential benefit of combination therapy using iron and standard treatment.
What's new
| Date | Event | Description |
|---|---|---|
| 3 May 2018 | New citation required and conclusions have changed | Updated search, addition of four new studies. Conclusion changed to support a benefit of iron for restless legs syndrome (RLS). |
Acknowledgements
We wish to thank the investigators of the studies included or evaluated for this review, especially Richard Allen, Bradley Davis, Ludger Grote, Claudia Trenkwalder, and Kirti Vishwakarma, who provided us with unpublished data or manuscript clarifications. We also wish to thank Jan Ulfberg and his co‐authors for providing us access with their then‐unpublished manuscript comparing oral and intravenous iron in blood donors. We thank Srinivas Bhadriraju for his authorship of the initial publication of this review in 2012. We are grateful to Andrew Becker for his assistance with Excel and Robert Lyles for statistical consultation.
Appendices
Appendix 1. Search Strategy
Our MEDLINE search used the following strategy:
1 RANDOMIZED CONTROLLED TRIAL
2 CONTROLLED CLINICAL TRIAL
3 RANDOMIZED
4 PLACEBO
5 DRUG THERAPY
6 RANDOMLY
7 TRIAL
8 GROUPS
9 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8
10 animals not (humans and animals)
11 #9 not #10
12 IRON
13 IRON COMPOUNDS
14 IRON‐DEXTRAN COMPLEX
15 FERROUS COMPOUNDS
16 IRON, DIETARY
17 FERROUS SULFATE
18 FERROUS GLUCONATE
19 FERROUS FUMARATE
20 IRON SUCROSE
21 FERRIC GLUCONATE
22 IRON DEXTRAN
23 FERRIC CARBOXYMALTOSE
24 #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23
25 RESTLESS LEGS SYNDROME
26 NOCTURNAL MYOCLONUS SYNDROME
27 PERIODIC LIMB MOVEMENT*
28 PERIODIC LEG MOVEMENT*
29 EKBOM* and SYNDROME
30 PARASITOSIS
31 #29 not #30
32 RESTLESS LEG*
33 NOCTURNAL MYOCLONUS
34 PSYCHOMOTOR AGITATION
35 AKATH*
36 WILLIS‐EKBOM DISEASE
37 #25 or #26 or #27 or #28 or #31 or #32 or #33 or #34 or #35 or #36
38 #11 and #24 and #37
Data and analyses
Comparison 1. Iron versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in IRLS severity scale score | 7 | 345 | Mean Difference (IV, Random, 95% CI) | ‐3.78 [‐6.25, ‐1.31] |
| 2 Change in any measure of restlessness | 8 | 370 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.74 [‐1.26, ‐0.23] |
| 2.1 New Subgroup | 8 | 370 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.74 [‐1.26, ‐0.23] |
| 3 Restlessness, Subgroup ‐ renal disease | 8 | 370 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.74 [‐1.26, ‐0.23] |
| 3.1 Normal renal function | 6 | 313 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.57, ‐0.04] |
| 3.2 Renal disease requiring dialysis | 2 | 57 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.18 [‐3.31, ‐1.06] |
| 4 Restlessness, Subgroup ‐ iron status at baseline | 8 | 370 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.74 [‐1.26, ‐0.23] |
| 4.1 Low or low‐normal baseline iron stores | 3 | 188 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.81, 0.07] |
| 4.2 Unselected for baseline iron measures | 5 | 182 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.95 [‐1.85, ‐0.06] |
| 5 Restlessness, Subgroup ‐ intravenous versus oral iron | 8 | 370 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.74 [‐1.26, ‐0.23] |
| 5.1 Oral iron | 1 | 18 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.29 [‐2.35, ‐0.23] |
| 5.2 Intravenous iron | 7 | 352 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.68 [‐1.23, ‐0.14] |
| 6 Restlessness, Subgroup ‐ iron sucrose versus ferric carboxymaltose | 6 | 327 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐1.09, 0.00] |
| 6.1 Iron sucrose | 3 | 110 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.88 [‐2.48, 0.72] |
| 6.2 Ferric carboxymaltose | 3 | 217 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.57, ‐0.04] |
| 7 Restlessness, Sensitivity analysis ‐ excluding studies at high risk of bias | 7 | 338 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.82, ‐0.10] |
| 8 Quality of life (dichotomous measure) | 2 | 39 | Risk Ratio (M‐H, Random, 95% CI) | 2.01 [0.54, 7.45] |
| 9 Change in quality of life (continuous measure) | 3 | 128 | Std. Mean Difference (IV, Random, 95% CI) | 0.51 [0.15, 0.87] |
| 10 Withdrew to use other RLS medication or because of inadequate RLS symptom control | 9 | 391 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.41, 1.47] |
| 11 Change in subjective sleep quality | 3 | 128 | Std. Mean Difference (IV, Random, 95% CI) | 0.19 [‐0.18, 0.56] |
| 12 Change in PLMS | 2 | 60 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.70, 0.32] |
| 13 Adverse events | 6 | 298 | Risk Ratio (M‐H, Random, 95% CI) | 1.48 [0.97, 2.25] |
| 14 Gastrointestinal side effects | 8 | 380 | Risk Ratio (M‐H, Random, 95% CI) | 1.44 [0.76, 2.75] |
| 15 Drop out due to adverse event | 9 | 398 | Risk Ratio (M‐H, Random, 95% CI) | 1.91 [0.50, 7.26] |
Comparison 2. Iron versus dopamine agonist.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Change in IRLS severity scale score | 1 | 30 | Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐5.93, 5.13] |
| 2 Change in subjective sleep quality | 1 | 30 | Mean Difference (IV, Random, 95% CI) | ‐1.80 [‐3.89, 0.29] |
2.1. Analysis.
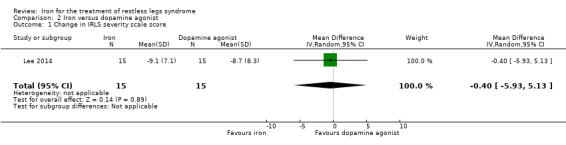
Comparison 2 Iron versus dopamine agonist, Outcome 1 Change in IRLS severity scale score.
2.2. Analysis.
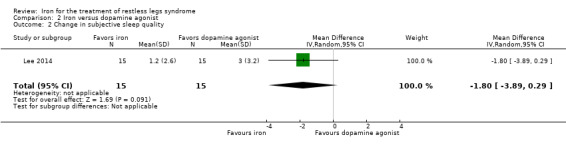
Comparison 2 Iron versus dopamine agonist, Outcome 2 Change in subjective sleep quality.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Allen 2011.
| Methods | Randomised, placebo‐controlled trial | |
| Participants | 46 adult men and women with at least moderately severe RLS (IRLS >= 15), RLS symptoms at least five nights per week, and at least 15 PLMS/hour, enrolled from multiple sites | |
| Interventions | Intervention: ferric carboxymaltose 500 mg in 100 mL normal saline, infused over 15 minutes, on days 0 and 5 Placebo: 100 mL normal saline with same dosing schedule |
|
| Outcomes | IRLS, RLS‐QoL, CGI‐I, PGI‐C, MOS scale, FSS, PLMS measured by actigraphy, ferritin | |
| Notes | Funded by pharmaceutical company | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Study randomised, but method of sequence generation not specified |
| Allocation concealment (selection bias) | Low risk | Central allocation using interactive voice recognition system |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Study nurse not blinded and interacted with participants, but was not an outcome assessor. IV bag and tubing concealed for study drug administration |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Three dropouts were not included in final analysis, all three from placebo group, all withdrew before receiving full dose of placebo (i.e. after 0 or 1 doses), none reported side effects |
| Selective reporting (reporting bias) | Unclear risk | Study protocol available but clinicaltrials.gov reports the protocol was first received 2/23/11, after the study was completed |
| Other bias | Low risk | No other risks identified |
Cho 2016.
| Methods | Randomised, placebo‐controlled trial | |
| Participants | 64 adult men and women with at least moderately severe RLS (IRLS >= 15) and symptoms at least 5 nights/week, enrolled from a single centre (Republic of Korea) | |
| Interventions | Intervention: 1000 mg of ferric carboxymaltose, given intravenously in 100 mL normal saline over 15 minutes, as a single dose Placebo: 100 mL normal saline over 15 minutes, as a single dose |
|
| Outcomes | IRLS, VAS of symptom severity, PSQI, RLS‐QoL, SF‐36, ferritin | |
| Notes | Funded by pharmaceutical company | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer random number generator |
| Allocation concealment (selection bias) | Unclear risk | May have used an open random allocation scheduled, i.e. "random number sequence" |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Nurse who administered intervention was unblinded but did not assess outcomes. IV bottles and lines were covered with foil to prevent identification of FCM versus placebo |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | One participant dropped out prior to receiving medications (not analysed). Two participants dropped out after receiving only one dose (included in safety set but not efficacy analyses). Three dropouts from ferric carboxymaltose and one from placebo group, all because of RLS severity. Included in analyses using last observation carried forward |
| Selective reporting (reporting bias) | Unclear risk | No mention of protocol registration |
| Other bias | Low risk | No other risks identified |
Davis 2000.
| Methods | Randomised, placebo‐controlled trial | |
| Participants | 28 adult men and women with symptomatic RLS currently on treatment, enrolled from a single neurology clinic (USA) | |
| Interventions | Intervention: ferrous sulfate liquid 325 mg twice a day Placebo: a 50:50 mixture of water and 2% carboxymethlycellulose with a "slightly disagreeable taste, similar to liquid ferrous sulfate". Study drug continued through week 16, then extended an additional 10 weeks if participants preferred study drug to their previous RLS medication |
|
| Outcomes | VAS of the extent that RLS interferes with sleep; VAS of how RLS affects life, ferritin, gastrointestinal side effects | |
| Notes | Power for primary outcome was 25% | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Block randomisation, but method not specified |
| Allocation concealment (selection bias) | Low risk | Randomisation controlled by nurse not involved in the study; randomisation key in locked cabinet |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Investigators and participants blinded; placebo and iron both liquids with slightly disagreeable taste |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 6 of 14 iron‐treated participants left before primary and secondary outcomes measured at week 14 (versus 1 of 14 placebo‐treated participants). Study data only reported for the people who remained |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available |
| Other bias | Low risk | No other risks identified |
Deng 2016.
| Methods | Randomised, placebo‐controlled trial | |
| Participants | 32 people with RLS, renal disease on dialysis at least 1 year, with serum ferritin < 200 ng/mL and transferrin saturation < 20%. Age > 18 was not specified as an inclusion criteria, but mean age was 63.9 (standard deviation 6.5) years | |
| Interventions | Intervention: Iron sucrose, given as a 50 mL injection (containing 100 mg iron sucrose) three times per week for a total of 10 doses Placebo: sodium chloride, given as the same volume and with the same schedule |
|
| Outcomes | IRLS, serum iron measurements | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Study was randomised in pairs but method of sequence generation not specified |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment; study unblinded |
| Blinding (performance bias and detection bias) All outcomes | High risk | Unblinded study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Unclear risk | No mention of study protocol registration |
| Other bias | Low risk | Unclear if participants were allowed to use other RLS medications during the study and whether such use was balanced between groups; note made that dialysis prescription had to remain unchanged |
Earley 2009.
| Methods | Randomised, placebo‐controlled trial | |
| Participants | 18 adult men and women with RLS and PLMS > 15/hr, enrolled from a single medical centre (USA) | |
| Interventions | Intervention: iron sucrose, given as a 500 mL infusion (containing 500 mg iron sucrose) over 10 hours, then another 500 mL over 12 hours the following day Placebo: sodium chloride, given in the same infusion volume and with the same dosing schedule |
|
| Outcomes | IRLS (a secondary outcome), PLMS/hr by second night PSG, ferritin, global rating scale (7‐point scale of symptom severity completed by the participant), sleep diary, periodic limb movements during wake on the suggested immobilisation test, change in cerebrospinal fluid ferritin levels, change in MRI iron index in substantia nigra | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised 2:1 but does not specify method of sequence generation |
| Allocation concealment (selection bias) | Low risk | Randomisation performed by pharmacy |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Nurse and one investigator (CJE) knew treatment status at times but were not outcome assessors. IV solution and tubing wrapped with black opaque plastic to conceal solution |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All subjects who received interventions were analysed |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available |
| Other bias | Low risk | No other risks identified; prior review rated high risk of bias for early stopping based on stopping rule, but this has been removed per current Cochrane guidance |
Grote 2009.
| Methods | Randomised, placebo‐controlled trial | |
| Participants | 60 adult men and women meeting all 4 RLS diagnostic criteria who had IRLS scores >= 10 and s‐ferritin < 45 ng/mL, recruited from three separate hospitals (Sweden) | |
| Interventions | Intervention: 200 mg iron sucrose IV (10 mL of 20 mg/mL iron (III) as iron (III)‐hydroxide sucrose complex) given 5 times over 3 weeks Placebo: sodium chloride given with same timing as intervention |
|
| Outcomes | IRLS (baseline (BL), week 3, week 7, week 11, month 5, month 8, month 12, with difference at week 11 set as primary outcome), ferritin, ESS | |
| Notes | Funded by pharmaceutical company | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Minimisation method |
| Allocation concealment (selection bias) | Low risk | Central randomisation |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Non‐transparent infusion bags and disposables used to obscure treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat analysis with last observation carried forward |
| Selective reporting (reporting bias) | Unclear risk | Study protocol registered but registration date appears to be after study completion |
| Other bias | Low risk | No other risks identified |
Lee 2014.
| Methods | Randomised, active‐comparator controlled trial | |
| Participants | 30 participants with RLS, ages 20‐80, with serum ferritin 15‐50 ng/mL, enrolled at a single site (Korea) | |
| Interventions | Intervention: oral ferrous sulfate, 325 mg bid, for 12 weeks Control: oral pramipexole at bedtime, starting dose 0.25 mg with dose increase as needed and tolerated |
|
| Outcomes | IRLS measured at baseline, weeks 2, 4, 8, and 12, ferritin, ESS score, Beck Depression Inventory, PSQI | |
| Notes | The authors calculated that > 20 subjects would be needed per group for 80% power to detect an effect size of 0.8 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Block randomisation used |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment; study unblinded |
| Blinding (performance bias and detection bias) All outcomes | High risk | Study was unblinded to participants and study personnel |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Although last observation carried forward was used, there was a high dropout rate for treatment‐related reasons that differed between conditions (4/15 dropped out of pramipexole group because of side effects versus 1/15 from iron group for lack of efficacy; an additional 2/15 left the iron group for study inconvenience) |
| Selective reporting (reporting bias) | Unclear risk | No mention of protocol registration |
| Other bias | Low risk | No other risks identified |
Sloand 2004.
| Methods | Randomised, placebo‐controlled trial | |
| Participants | 25 adult men and women with ESRD (on either haemodialysis or peritoneal dialysis) who also had RLS by IRLSSG criteria, recruited from the dialysis units of a single medical centre (USA) | |
| Interventions | Active: IV iron dextran given as: 30 mg test dose over 3 min, followed by 970 mg (in 485 mL volume) over 3 hrs if no reaction to the test dose Placebo: sodium chloride given in the same volume and with the same timing as the intervention group |
|
| Outcomes | ferritin, hematocrit, gastrointestinal side effects, University of Rochester severity score (10‐point scale, where 0 = none, 10 = bad) at 0, 1, 2, 4 weeks | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomisation not specified |
| Allocation concealment (selection bias) | Low risk | Randomisation appears to have been performed by pharmacy |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Medication and tubing covered with opaque sleeve to conceal treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Two placebo participants dropped out after infusion; Figure 1 reports data on all 14 placebo participants although use of last observation carried forward not explicitly stated |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available |
| Other bias | Unclear risk | Baseline imbalance of 2 points in RLS severity score; there was also a broader range of scores in the treated group; imbalance in duration of dialysis |
Trenkwalder 2017.
| Methods | Randomised, placebo‐controlled trial | |
| Participants | 110 participants with at least moderately severe RLS (IRLS >= 15) and serum ferritin less than 75 ng/mL (or serum ferritin 75‐300 ng/mL and transferrin saturation < 20%) | |
| Interventions | Intervention: intravenous ferric carboxymaltose, 1000 mg infusion over 15 minutes Control: placebo with matched infusion rate |
|
| Outcomes | IRLS, CGI‐severity, PGI‐C, RLS‐6 quality of life scale, MOS sleep | |
| Notes | Funded by pharmaceutical company | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised by statistician |
| Allocation concealment (selection bias) | Low risk | Central allocation |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Nurse administering treatment was not blinded but did not assess outcomes. Unclear how treatment was concealed during IV administration |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Relatively high dropout rate (21%), but for similar reasons and used last observation carried forward |
| Selective reporting (reporting bias) | Low risk | Protocol registered on EudraCT prior to start of enrolment; protocol consistent with reported outcomes |
| Other bias | Low risk | No other risks identified |
Wang 2009.
| Methods | Randomised, placebo‐controlled | |
| Participants | 18 adult men and women with RLS who had ferritin 15‐75 ng/mL and IRLS scores >= 11 | |
| Interventions | Intervention: ferrous sulfate 325 mg bid in non‐descript capsules Placebo: lactose, appearance‐matched Study drug continued for 12 weeks |
|
| Outcomes | IRLS (BL, 6 weeks, 12 weeks), ferritin (BL, 6 weeks, 12 weeks), single question on change in quality of life at 12 weeks (improved, same, worsened), compliance at 6 and 12 weeks (by manual pill count) | |
| Notes | Authors raise issue of iron causing stool discolouration and therefore inadvertent unblinding, although this is speculative | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used randomly generated sequenced number programme |
| Allocation concealment (selection bias) | Low risk | Independent investigative pharmacist performed randomisation and kept randomisation code in locked cabinet |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Matched capsules of placebo and iron; investigators and participants blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants who were randomised completed the study |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available |
| Other bias | Low risk | No other risks identified |
BL: baseline CGI‐I: Clinical Global Impression of Improvement ESRD: end‐stage renal disease ESS: Epworth Sleepiness Scale FSS: fatigue severity scale IRLS: International RLS Study Group severity scale IRLSSG: International Restless Legs Syndrome Study Group IV: intravenous MOS: medical outcomes of sleep MRI: magnetic resonance imaging PGI‐C: Patient Global Impression of Change
PLMS: periodic limb movements of sleep PSG: polysomnography PSQI: Pittsburgh Sleep Quality Index RLS: restless legs syndrome RLS‐QoL: RLS quality of life scale SF‐36: Short‐form‐36 VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Auerbach 2014 | Not a report of original data |
| Birgegard 2010 | No non‐iron control group |
| Cho 2011 | No non‐iron control group |
| Earley 2004 | No control group |
| Earley 2005 | No control group |
| Ekermo 2013 | No non‐iron control group |
| Halterman 2007 | Duplicate publication of Sloand 2004 (included) |
| Konofal 2008 | Included children |
| Macher 2015 | No non‐iron control group |
| Mohri 2008 | No control group; included children |
| NCT00895232 | No non‐iron control group |
| O'Keeffe 1994 | Performed prior to 1995 (non‐standard diagnostic criteria for RLS used); no control group |
| Ondo 2010 | No control group |
| Simakajornboon 2003 | No control group; included children |
| Vishwakarma 2013 | Iron group also given folate, while other treatment groups were not given folate |
| Zhang 2014 | No non‐iron control group |
| Zilberman 2010 | No control group |
RLS: restless legs syndrome
Characteristics of ongoing studies [ordered by study ID]
ISRCTN01222004.
| Trial name or title | A single blind, randomised controlled study of iron supplementation in iron deficient, but otherwise healthy, patients on hypoxic pulmonary vascular responses |
| Methods | Single‐blind, randomised controlled trial |
| Participants | Iron deficient subjects |
| Interventions | Up to 1000 mg of ferric carboxymaltose |
| Outcomes | RLS and nocturnal limb movements measured by actigraphy are secondary outcomes |
| Starting date | November 2009. Completed in 2013 per UK Clinical Trials Gateway but outcome data for RLS appear to be as‐yet unpublished |
| Contact information | Dr Annabel Nickol, Oxford Centre for Respiratory Medicine |
| Notes | Available on UK Clinical Trials Gateway |
NCT00685815.
| Trial name or title | Intravenous iron metabolism in restless legs syndrome |
| Methods | Double‐blind, randomised controlled trial |
| Participants | 36 adults with RLS |
| Interventions | 500 mg of IV ferric carboxymaltose given on two consecutive days |
| Outcomes | RLS symptoms |
| Starting date | November 2006. Completed in 2012 per clinical trials.gov but appears to be as‐yet unpublished |
| Contact information | Christopher J Earley, MD, PhD, Johns Hopkins University |
| Notes | Registered at www.clinicaltrials.gov |
NCT01895231.
| Trial name or title | A Study of intravenous iron isomaltoside 1000 (Monofer®) administered by infusions to iron‐deficient blood donors |
| Methods | Double‐blind, randomised controlled trial |
| Participants | 100 female, adult, first‐time blood donors (some of whom are anticipated to have RLS) with serum ferritin < 30 ng/mL |
| Interventions | Iron isomaltoside 1000 mg IV infusion over 15 minutes |
| Outcomes | RLS symptoms |
| Starting date | June 2013 |
| Contact information | Lars Lykke Thomsen |
| Notes | Registered at www.clinicaltrials.gov |
NCT02826681.
| Trial name or title | Randomized, placebo‐controlled trial of ferric carboxymaltose in RLS patients with iron‐deficiency anemia |
| Methods | Randomised, controlled trial |
| Participants | Participants with RLS and iron deficiency anaemia |
| Interventions | Intervention: ferric carboxymaltose Control: placebo |
| Outcomes | IRLS, CGI |
| Starting date | anticipated March 2017 |
| Contact information | Angelia D Butcher |
| Notes | Registered at www.clinicaltrials.gov |
CGI: Change in Glogal Impression IRLS: International Restless Legs Scale RLS: restless legs syndrome
Differences between protocol and review
We did not construct a funnel plot because we identified fewer than 10 studies for inclusion. We did not prespecify GRADE analyses, but we added them at the suggestion of the reviewers. The title of the original protocol and first version of this review was "Iron for restless legs syndrome," which was updated for this review.
Contributions of authors
Lynn Marie Trotti (LMT) conceived and co‐ordinated the review; performed the search; screened the search results for acceptable trials; graded and extracted data from trials; entered and analysed data; wrote the initial draft of the review; and incorporated feedback into the final draft.
Lorne A Becker (LAB) designed the review; screened the search results for acceptable trials; graded and extracted data from trials; entered and analysed data; and co‐wrote the review.
Sources of support
Internal sources
No sources of support supplied
External sources
-
National Center for Advancing Translational Sciences of the National Institutes of Health, USA.
Award Number UL1TR000454 for statistical consultation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Declarations of interest
Dr. Trotti reports no declarations of interest. Dr. Becker reports no declarations of interest.
Edited (conclusions changed)
References
References to studies included in this review
Allen 2011 {published and unpublished data}
- Allen RP, Adler CH, Du W, Butcher A, Bregman DB, Earley CJ. Clinical efficacy and safety of IV ferric carboxymaltose (FCM) treatment of RLS: a multi‐centred, placebo‐controlled preliminary clinical trial. Sleep Medicine 2011;12(9):906‐13. [DOI] [PubMed] [Google Scholar]
Cho 2016 {published data only}
- Cho YW, Allen RP, Earley CJ. Clinical efficacy of ferric carboxymaltose treatment in patients with restless legs syndrome. Sleep Medicine 2016;25:16‐23. [DOI] [PubMed] [Google Scholar]
Davis 2000 {published data only}
- Davis BJ, Rajput A, Rajput ML, Aul EA, Eichhorn GR. A randomized, double‐blind, placebo‐controlled trial of iron in restless legs syndrome. European Neurology 2000;43:70‐5. [DOI] [PubMed] [Google Scholar]
Deng 2016 {published data only (unpublished sought but not used)}
- Deng Y, Wu J, Jia Q. Efficacy of intravenous iron sucrose in hemodialysis patients with restless legs syndrome (RLS): a randomized, placebo‐controlled study. Medical Science Monitor 2016;23:1254‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Earley 2009 {published data only (unpublished sought but not used)}
- Earley CJ, Horska A, Mohamed MA, Barker PB, Beard JL, Allen RP. A randomized, double‐blind, placebo‐controlled trial of intravenous iron sucrose in restless legs syndrome. Sleep Medicine 2009;10:206‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Grote 2009 {published and unpublished data}
- Grote L, Leissner L, Hedner J, Ulfberg J. A randomized, double‐blind, placebo‐controlled, multi‐center study of intravenous iron sucrose and placebo in the treatment of restless legs syndrome. Movement Disorders 2009;24(10):1445‐52. [DOI] [PubMed] [Google Scholar]
Lee 2014 {published data only}
- Lee CS, Lee SD, Kang SH, Park HY, Yoon IY. Comparison of the efficacies of oral iron and pramipexole for the treatment of restless legs syndromre patients with low serum ferritin. European Journal of Neurology 2014;21:260‐6. [DOI] [PubMed] [Google Scholar]
Sloand 2004 {published data only (unpublished sought but not used)}
- Sloand JA, Shelly MA, Feigin A, Bernstein P, Monk RD. A double‐blind, placebo‐controlled trial of intravenous iron dextran therapy in patients with ESRD and restless legs syndrome. American Journal of Kidney Diseases 2004;43(4):663‐70. [DOI] [PubMed] [Google Scholar]
Trenkwalder 2017 {published and unpublished data}
- Trenkwalder C, Winkelmann J, Oertel W, Virgin G, Roubert B, Mezzacasa A, FCM‐RLS Study Investigators. Ferric carboxymaltose in patients with restless legs syndrome and nonanemic iron deficiency: A randomized trial. Movement Disorders 2017;32(10):1478‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2009 {published data only (unpublished sought but not used)}
- Wang J, O'Reilly B, Venkataraman R, Mysliwiec V, Mysliwiec A. Efficacy of oral iron in patients with restless legs syndrome and a low‐normal ferritin: A randomized, double‐blind, placebo‐controlled study. Sleep Medicine 2009;10(9):973‐5. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Auerbach 2014 {published data only}
- Auerbach M. The role of intravenous iron in the treatment of restless legs. American Journal of Hematology 2014;89(10):1016. [DOI] [PubMed] [Google Scholar]
Birgegard 2010 {published data only}
- Birgegard G, Schneider K, Ulfberg J. High incidence of iron depletion and restless legs syndrome (RLS) in regular blood donors: intravenous iron sucrose substitution more effective than oral iron. Vox Sang 2010;99(4):354‐61. [DOI] [PubMed] [Google Scholar]
Cho 2011 {published data only}
- Cho Y, Kim D, Shin W, Earley CJ, Allen RP. Lower molecular weight intravenous iron dextran for restless legs syndrome. Sleep 2011;34 Suppl 1:A204. [DOI] [PubMed] [Google Scholar]
Earley 2004 {published data only}
- Earley CJ, Heckler D, Allen RP. The treatment of restless legs syndrome with intravenous iron dextran. Sleep Medicine 2004;5:231‐5. [DOI] [PubMed] [Google Scholar]
Earley 2005 {published data only}
- Earley CJ, Hecker D, Allen RP. Repeated IV doses of iron provides effective supplemental treatment of restless legs syndrome. Sleep Medicine 2005;6:301‐5. [DOI] [PubMed] [Google Scholar]
Ekermo 2013 {published data only}
- Ekermo BE, Forsberg P, Schedvin G, Berlin G. An open, randomised, clinical study of oral versus intravenous iron for iron substitution in blood donors. Transfusion 2013;53(Suppl 2):36A. [Google Scholar]
Halterman 2007 {published data only}
- Halterman MW, Sloand JA. An update on the use of intravenous iron for the treatment of restless legs syndrome in end stage renal disease. Salud (i) Ciencia 2007;15:860‐5. [Google Scholar]
Konofal 2008 {published data only}
- Konofal E, Lecendreux M, Deron J, Marchand M, Cortese S, Zaim M, et al. Effects of iron supplementation on attention deficit hyperactivity disorder in children. Pediatric Neurology 2008;38:20‐6. [DOI] [PubMed] [Google Scholar]
Macher 2015 {published and unpublished data}
- Macher S, Drexler C, Stojakovic T, Lindenau I, Schrock M, Reinprecht C, et al. Intravenous high‐dose iron supplementation for blood donors with iron deficiency. Haematologica 2015;100(Suppl 1):140. [Google Scholar]
Mohri 2008 {published data only}
- Mohri I, Kato‐Nishimura K, Tachibana N, Ozono K, Taniike M. Restless legs syndrome (RLS): an unrecognized cause for bedtime problems and insomnia in children. Sleep Medicine 2008;9:701‐2. [DOI] [PubMed] [Google Scholar]
NCT00895232 {published data only}
- NCT00895232. Iron Sucrose In The Treatment of Restless Legs Syndrome: Safety of Three Dose Regimens as Evaluated by Clinical Assessments. clinicaltrials.gov/ct2/show/NCT00895232 (first received 5/7/09).
O'Keeffe 1994 {published data only}
- O'Keeffe ST, Gavin K, Lavan JN. Iron status and restless legs syndrome in the elderly. Age and Aging 1994;23:200‐3. [DOI] [PubMed] [Google Scholar]
Ondo 2010 {published data only}
- Ondo WG. Intravenous iron dextran for severe refractory restless legs syndrome. Sleep Medicine 2010;11(5):494‐6. [DOI] [PubMed] [Google Scholar]
Simakajornboon 2003 {published data only}
- Simakajornboon N, Gozal D, Vlasic V, Mack C, Sharon D, McGinley BM. Periodic limb movements in sleep and iron status in children. Sleep 2003;26(6):735‐8. [DOI] [PubMed] [Google Scholar]
Vishwakarma 2013 {published and unpublished data}
- Vishwakarma K, Kalra J, Gupta R, Sharma M, Sharma T. A double‐blind, randomized, controlled trial to compare the efficacy and tolerability of fixed doses of ropinirole, bupropion, and iron in treatment of restless legs syndrome (Willis‐Ekbom disease). Annals of Indian Academy of Neurology 2016;19(4):472‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhang 2014 {published data only}
- Zhang X, Chen WW, Huang WJ. Efficacy of the low‐dose Saccharum iron treatment of idiopathic restless legs syndrome. Panminerva Medica 2015;57(3):109‐13. [PubMed] [Google Scholar]
Zilberman 2010 {published data only}
- Zilberman M, Silverberg DS, Schwartz D, Oksenberg A. Restless legs syndrome (RLS) in anemic patients with congestive heart failure and chronic renal failure: lack of effect of anemia treatment. International Journal of Cardiology 2010;143(2):205‐7. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
ISRCTN01222004 {unpublished data only}
- ISRCTN01222004. Iron supplementation in iron deficiency. http://www.isrctn.com/ISRCTN01222004 (date applied 10/22/2009).
NCT00685815 {unpublished data only}
- NCT00685815. Intravenous Iron Metabolism in Restless Legs Syndrome. https://clinicaltrials.gov/ct2/show/NCT00685815 (first submitted 5/23/08).
NCT01895231 {unpublished data only}
- NCT01895231. A Study of Intravenous Iron Isomaltoside 1000 (Monofer®) Administered by Infusions to Iron‐deficient Blood Donors. https://clinicaltrials.gov/ct2/show/NCT01895231 (first submitted 6/26/13).
NCT02826681 {unpublished data only}
- NCT02826681. Randomized, Placebo‐controlled Trial of Ferric Carboxymaltose in RLS Patients With Iron‐deficiency Anemia. https://clinicaltrials.gov/ct2/show/NCT02826681 (first submitted 6/30/16).
Additional references
Abetz 2005
- Abetz L, Vallow SM, Kirsch J, Allen RP, Washburn T, Earley CJ. Validation of the Restless Legs Syndrome Quality of Life questionnaire. Value Health 2005;8(2):157‐67. [DOI] [PubMed] [Google Scholar]
Allen 2003
- Allen RP, Picchietti D, Hening WA, Trenkwalder C, Walters AS, Montplaisir J. Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Medicine 2003;4:101‐19. [DOI] [PubMed] [Google Scholar]
Allen 2004
- Allen R. Dopamine and iron in the pathophysiology of restless legs syndrome. Sleep Medicine 2004;5:385‐91. [DOI] [PubMed] [Google Scholar]
Allen 2013
- Allen RP, Auerbach S, Bahrain H, Auerbach M, Earley CJ. The prevalence and impact of restless legs syndrome on patients with iron deficiency anemia. American Journal of Hematology 2013;88:261‐4. [DOI] [PubMed] [Google Scholar]
Allen 2013b
- Allen RP. Minimal clinically significant change for the International Restless Legs Syndrome Study Group rating scale in clinical trials is a score of 3. Sleep Medicine 2013;14(11):1229. [DOI] [PubMed] [Google Scholar]
Allen 2014
- Allen RP, Picchietti DL, Garcia‐Borreguero D, Ondo WG, Walters AS, Winkelman JW, et al. International Restless Legs Syndrome Study Group. Restless legs syndrome/Willis‐Ekbom disease diagnostic criteria: updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria‐history, rationale, description, and significance. Sleep Medicine 2014;15(8):860‐73. [DOI] [PubMed] [Google Scholar]
Aurora 2012
- Aurora RN, Kristo DA, Bista SR, Rowley JA, Zak RS, Casey KR, et al. The treatment of restless legs syndrome and periodic limb movement disorder in adults ‐ an update for 2012: practice parameters with an evidence‐based systematic review and meta‐analysis. Sleep 2012;35(8):1039‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Avni 2015
- Avni T, Bieber A, Grossman A, Green H, Leibovici L, Gafter‐Gvili A. The safety of intravenous iron preparations: systematic review and meta‐analysis. Mayo Clinic Proceedings 2015;90(1):12‐23. [DOI] [PubMed] [Google Scholar]
Berger 2004
- Berger K, Luedemann J, Trenkwalder C, John U, Kessler C. Sex and the risk of restless legs syndrome in the general population. Archives of Internal Medicine 2004;164:196‐202. [DOI] [PubMed] [Google Scholar]
Bliwise 2006
- Bliwise DL. Periodic leg movements in sleep and restless legs syndrome: Considerations in geriatrics. Sleep Medicine Clinics 2006;1:263‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Buysse 1989
- Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research.. Psychiatry Research 1989;28(2):193‐213. [DOI] [PubMed] [Google Scholar]
Connor 2003
- Connor JR, Boyer PJ, Menzies SL, Dellinger B, Allen RP, Ondo WG, et al. Neuropathological examination suggests impaired brain iron acquisition in restless legs syndrome. Neurology 2003;61:304‐9. [DOI] [PubMed] [Google Scholar]
Earley 2000
- Earley CJ, Allen RP, Beard JL, Connor JR. Insight into the pathophysiology of restless legs syndrome. Journal of Neuroscience Research 2000;62:623‐8. [DOI] [PubMed] [Google Scholar]
Earley 2014
- Earley CJ, Connor J, Garcia‐Borreguero D, Jenner P, Winkelman J, Zee PC, et al. Altered brain iron homeostasis and dopaminergic function in Restless Legs Syndrome (Willis‐Ekbom Disease). Sleep Medicine 2014;15(11):1288‐301. [DOI] [PubMed] [Google Scholar]
Garcia‐Borreguero 2012
- Garcia‐Borreguero D, Ferini‐Strambi L, Kohnen R, O'Keeffe S, Trenkwalder C, Hogl B, et al. European guidelines on management of restless legs syndrome: report of a joint task force by the European Federation of Neurological Societies, the European Neurological Society, and the European Sleep Research Society. European Journal of Neurology 2012;19:1385‐96. [DOI] [PubMed] [Google Scholar]
Garcia‐Borreguero 2013
- Garcia‐Borreguero D, Kohnen R, Silber MH, Winkelman JW, Earley CJ, Hogl B, et al. The long‐term treatment of restless legs syndrome/Willis‐Ekbom disease: evidence‐based guidelines and clinical consensus best practice guidance: a report from the International Restless Legs Syndrome Study Group. Sleep Medicine 2013;14:675‐84. [DOI] [PubMed] [Google Scholar]
Guy 1976
- Guy W. ECDEU Assessment Manual for Psychopharmacology. US Department of Health, Education, and Welfare, 1976. [Google Scholar]
Guyatt 2011
- Guyatt GH, Oxman AD, Montori V, Vist G, Kunz R, Brozek J, et al. GRADE guidelines: 5. Rating the quality of evidence ‐ publication bias. Journal of Clinical Epidemiology 2011;64:1277‐82. [DOI] [PubMed] [Google Scholar]
Hays 1992
- Hays RD, Stewart AL. Sleep measures. Measuring functioning and well being: the Medical Outcomes Study approach. Durham, NC: Duke University Press, 1992. [Google Scholar]
Hening 2003
- Hening WA, Allen RP, Thanner S, Washburn T, Heckler D, Walter AS, et al. The Johns Hopkins telephone diagnostic interview for the restless legs syndrome: preliminary investigation for validation in a multi‐center patient and control population. Sleep Medicine 2003;4(2):137‐41. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org. Wiley‐Blackwell.
Hornyak 2006
- Hornyak M, Feige B, Riemann D, Voderholzer U. Periodic leg movements in sleep and periodic limb movement disorder: prevalence, clinical significance and treatment. Sleep Medicine Reviews 2006;10(3):169‐77. [DOI] [PubMed] [Google Scholar]
Johns 1991
- Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale.. Sleep 1991;14(6):540‐5. [DOI] [PubMed] [Google Scholar]
Kohnen 2004
- Kohnen R, Stiasny‐Kolster K, Oertel WH, Benes H, Trenkwalder C. Severity rating of restless legs syndrome: Validation of the RLS‐6 scale. Sleep 2004;27(Suppl 1):A342. [Google Scholar]
Krupp 1989
- Krupp LB, LaRocca NG, Muir‐Nash J, Steinberg AD. The fatigue severity scale. Archives of Neurology 1989;46:1121‐3. [DOI] [PubMed] [Google Scholar]
Montplaisir 1997
- Montplaisir J, Boucher S, Poirier G, Lavigne G, Lapierre O, Lesperance P. Clinical, polysomnographic, and genetic characteristics of restless legs syndrome. Movement Disorders 1997;12:61‐5. [DOI] [PubMed] [Google Scholar]
Nelson 1997
- Nelson C, Erikson K, Piñero DJ, Beard JL. In vivo dopamine metabolism is altered in iron‐deficient anemic rats. Journal of Nutrition 1997;127:2282‐8. [DOI] [PubMed] [Google Scholar]
Rye 2015
- Rye DB. The molecular genetics of restless legs syndrome. Sleep Medicine Clinics 2015;10(3):227‐33. [DOI] [PubMed] [Google Scholar]
Scholz 2011
- Scholz H, Trenkwalder C, Kohnen R, Riemann D, Kriston L, Hornyak M. Dopamine agonists for restless legs syndrome. Cochrane Database of Systematic Reviews 2011, Issue 3. [DOI: 10.1002/14651858.CD006009.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schormair 2008
- Schormair B, Kemlink D, Roeske D, Eckstein G, Xiong L, Lichtner P, et al. PTPRD (protein tyrosine phosphatase receptor type delta) is associated with restless legs syndrome. Nature Genetics 2008;40(8):946‐8. [DOI] [PubMed] [Google Scholar]
Silber 2013
- Silber MH, Becker PM, Earley C, Garcia‐Borreguero D, Ondo WG. Willis‐Ekbom Disease Foundation revised consensus statement on the management of restless legs syndrome. Mayo Clinic Proceedings 2013;88(9):977‐86. [DOI] [PubMed] [Google Scholar]
Stefansson 2007
- Stefansson H, Rye DB, Hicks A, Petursson H, Ingason A, Thorgeirsson TE, et al. A genetic risk factor for periodic limb movements in sleep. New England Journal of Medicine 2007;357(7):639‐47. [DOI] [PubMed] [Google Scholar]
Trenkwalder 2008
- Trenkwalder C, Hogl B, Benes H, Kohnen R. Augmentation in restless legs syndrome is associated with low ferritin. Sleep Medicine 2008;9(5):572‐4. [DOI] [PubMed] [Google Scholar]
Trotti 2008
- Trotti LM, Bhadriraju S, Rye DB. An update on the pathophysiology and genetics of restless legs syndrome. Current Neurology and Neuroscience Reports 2008;8:281‐7. [DOI] [PubMed] [Google Scholar]
Trotti 2009
- Trotti LM, Bliwise DL, Greer SA, Sigurdsson AP, Gudmundsdottir GB, Wessel T, et al. Correlates of PLMS variability over multiple nights and impact upon RLS diagnosis. Sleep Medicine 2009;10(6):668‐71. [DOI] [PubMed] [Google Scholar]
Walters 1995
- Walters AS. Toward a better definition of the restless legs syndrome. The International Restless Legs Syndrome Study Group. Movement Disorders 1995;10(5):634‐42. [DOI] [PubMed] [Google Scholar]
Walters 2003
- Walters AS, LeBrocq C, Dhar A, Hening W, Rosen R, Allen RP, et al. Validation of the International Restless Legs Syndrome Study Group rating scale for restless legs syndrome. Sleep Medicine 2003;4(2):121‐32. [DOI] [PubMed] [Google Scholar]
Wan 2014
- Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Medical Research Methodology 2014;14:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ware 1992
- Ware JE Jr, Sherbourne CD. The MOS 36‐item short‐form health survey (SF‐36). I. Conceptual framework and item selection. Med Care 1992;30(6):473‐83. [PubMed] [Google Scholar]
Wilt 2013
- Wilt TJ, MacDonald R, Ouellette J, Khawaja IS, Rutks I, Butler M, et al. Pharmacologic therapy for primary restless legs syndrome: a systematic review and meta‐analysis. JAMA Internal Medicine 2013;173(7):496‐505. [DOI] [PubMed] [Google Scholar]
Winkelman 2016
- Winkelman JW, Armstrong MJ, Allen RP, Chaudhuri KR, Ondo W, Trenkwalder C, et al. Practice guideline summary: Treatment of restless legs syndrome in adults: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology 2016;87(24):2585‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Winkelmann 2007
- Winkelmann J, Schormair B, Lichtner P, Ripke S, Xiong L, Jalilzadeh S, et al. Genome‐wide association study of restless legs syndrome identifies common variants in three genomic regions. Nature Genetics 2007;39(8):1000‐6. [DOI] [PubMed] [Google Scholar]
Winkelmann 2011
- Winkelmann J, Czamara D, Schormair B, Knauf F, Schulte EC, Trenkwalder C, et al. Genome‐wide association study identifies novel restless legs syndrome susceptibility loci on 2p14 and 16q12.1. PLoS Genetic 2011;7(7):e1002171. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Trotti 2009b
- Trotti LM, Bhadriraju S, Becker LA. Iron for Restless Legs. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Trotti 2012
- Trotti LM, Bhadriraju S, Becker LA. Iron for restless legs syndrome. Cochrane Database of Systematic Reviews 2012, Issue 5. [doi: 10.1002/14651858.CD007834.pub2.] [DOI] [PMC free article] [PubMed] [Google Scholar]


