Fahr's disease (FD) is a rare autosomal‐dominant disease characterized by intracranial calcifications involving basal ganglia and other brain regions, such as dentate nuclei, in the cerebellum. Clinically, patients manifest with various combinations of dementia, psychiatric symptoms, and movement disorders that most frequently include tremulous or akinetic‐rigid parkinsonism, but also ataxia, dystonia, and chorea have been reported.
Recently, three causative genes (SLC20A2, PDGFRB, and PDGF) have been discovered in sporadic and familial cases,1, 2, 3 with highly heterogeneous phenotypes even within the same family.
Here, we report on a 65‐year‐old man who came to our attention for a left frontal lacunar stroke in the periventricular white matter presenting with mild right upper‐limb paresis, right central facial palsy, and dysarthria. His past medical history included blood hypertension, diabetes, and obesity. No previous exposure to neuroleptics was reported. There was no family history of movement disorders, dementia, or psychiatric disturbances. His mother died at age 77 from stroke, his father died from a laryngeal malignancy, and his sister, age 71, is reported to be in good health. The patient's daughter's examination at age 37 was unremarkable.
Patient's neurological examination showed continuous, patternless, involuntary hyperkinetic movements focally involving the first three digits of the left hand, which were not distractible or entrainable nor associated with an urge to perform the movements. The observed phenomenology was consistent with chorea, which was present at rest, on posture, and while walking and could only be abolished by sleep. Bradykinesia was not detectable on finger tapping whereas mild myoclonic jerks were present at the same site (see Video 1). No involuntary movements were observed in the left foot. Chorea had been present since age 53, with a gradual onset and no spreading or worsening and did not cause major functional limitations to the patient. A CT brain scan showed extensive bilateral basal ganglia and dentate nuclei calcifications, consistent with FD (Fig. 1A,B). A brain MRI demonstrated a hyperintense focal lesion on diffusion‐weighted imaging sequences in the periventricular white matter of the left frontal lobe, consistent with a recent lacunar stroke (Fig. 1C,D). Blood calcium, phosphates, vitamin D, and parathyroid hormone were all in the normal range. Blood glocose was within normal limits on admission (95 mg/dL). Despite the unusual presentation, rarer genetic or autoimmune causes of chorea, such as Huntington's disease and antiphospholipid syndrome, were not investigated in view of the absence of family history, normal cognition (Mini–Mental State Examination: 29/30), duration and lack of spreading of the movement disorder (that had been present for the past 12 years), and the patient's age and multiple cardiovascular risk factors.
Figure 1.
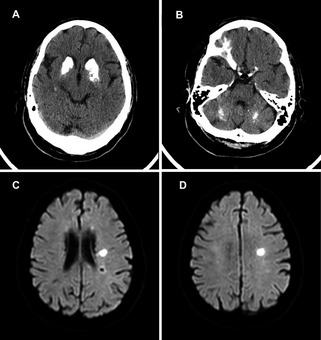
(A and B) Patient's brain CT scan at age 65, showing extensive bilateral calcification of basal ganglia and dentate nuclei in the cerebellum. (C and D) Patient's brain MRI on admission, demonstrating a left frontal lacunar stroke in the periventricular white matter.
Genetic analysis revealed a missense mutation in the SLC20A2 gene (c.338C>G), which creates a premature stop codon in the coding protein (p.Ser113*), and was previously reported in association with an atypical parkinsonian phenotype.4 Other family members were not available for genetic testing.
Isolated hyperkinetic movement disorders have only rarely been described as a manifestation of FD since the identification of the first three causative genes. Nicolas et al. found 10 SLC20A2‐positive patients, of whom 1 had dystonia and 1 orofacial dyskinesias.5 Among 15 PDGFRB‐positive subjects, only 1 was reported to have chorea, but no details on the distribution of movement disorders were available. Interestingly, also, paroxysmal dystonia has been reported in FD with and without SLC20A2 mutations.6, 7, 8
Recently published genetic screenings9 demonstrated poor correlation between the site and extension of brain calcifications and clinical symptoms in FD, with patients showing no or minor abnormalities on examination despite extensive calcium deposition. Here, we report on an unusual clinical phenotype of FD, with adult‐onset focal unilateral chorea despite extensive bilateral calcifications in the striatum and dentate nuclei. This case confirms the clinical heterogeneity of FD, broadening the spectrum of hyperkinetic movement disorders associated with SLC20A2 mutations. To the best of our knowledge, a similar phenotype has not been previously reported on in SLC20A2‐positive patients.
Author Roles
(1) Research Project: A. Conception, B. Organization, C. Execution; (2) Statistical Analysis: A. Design, B. Execution, C. Review and Critique; (3) Manuscript: A. Writing of the First Draft, B. Review and Critique.
M.C.: 1A, 1B, 1C, 3A
C.B.: 1B, 1C
C.V.: 1A, 1B
R.C.: 3B
B.G.: 1A, 1C, 3B
Disclosures
Funding Sources and Conflicts of Interest: The authors report no sources of funding and no conflicts of interest.
Financial Disclosures for previous 12 months: M.C. has received honoraria from Lundbeck and has received a grant from the International Parkinson and Movement Disorder Society. B.G. has received grants from Fondazione Telethon and Fondazione Pierfranco e Luisa Mariani.
Supporting information
A video accompanying this article is available in the supporting information here.
Video 1. The video shows the patient's clinical picture during admission for a lacunar stroke (note central right facial nerve palsy). Focal chorea involving the first three digits of the left hand is visible at rest, on posture, and during walking. Mild superimposed myoclonic jerks are also visible at the same site.
Relevant disclosures and conflicts of interest are listed at the end of this article.
References
- 1. Wang C, Li Y, Shi L, et al. Mutations in SLC20A2 link familial idiopathic basal ganglia calcification with phosphate homeostasis. Nat Genet 2012;44:254–256. [DOI] [PubMed] [Google Scholar]
- 2. Nicolas G, Pottier C, Maltête D, et al. Mutation of the PDGFRB gene as a cause of idiopathic basal ganglia calcification. Neurology 2013;80:181–187. [DOI] [PubMed] [Google Scholar]
- 3. Keller A, Westenberger A, Sobrido MJ, et al. Mutations in the gene encoding PDGF‐B cause brain calcifications in humans and mice. Nat Genet 2013;45:1077–1082. [DOI] [PubMed] [Google Scholar]
- 4. Baker M, Strongosky AJ, Sanchez‐Contreras MY, et al. SLC20A2 and THAP1 deletion in familial basal ganglia calcification with dystonia. Neurogenetics 2014;15:23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nicolas G, Pottier C, Charbonnier C, et al; French IBGC Study Group . Phenotypic spectrum of probable and genetically‐confirmed idiopathic basal ganglia calcification. Brain 2013;136:3395–3407. [DOI] [PubMed] [Google Scholar]
- 6. Zhu M, Zhu X, Wan H, Hong D. Familial IBGC caused by SLC20A2 mutation presenting as paroxysmal kinesigenic dyskinesia. Parkinsonism Relat Disord 2014;20:353–354. [DOI] [PubMed] [Google Scholar]
- 7. Chung EJ, Cho GN, Kim SJ. A case of paroxysmal kinesigenic dyskinesia in idiopathic bilateral striopallidodentate calcinosis. Seizure 2012;21:802–804. [DOI] [PubMed] [Google Scholar]
- 8. Hsu SC, Sears RL, Lemos RR, et al. Mutations in SLC20A2 are a major cause of familial idiopathic basal ganglia calcification. Neurogenetics 2013;14:11–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chen WJ, Yao XP, Zhang QJ, et al. Novel SLC20A2 mutations identified in southern Chinese patients with idiopathic basal ganglia calcification. Gene 2013;529:159–162. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A video accompanying this article is available in the supporting information here.
Video 1. The video shows the patient's clinical picture during admission for a lacunar stroke (note central right facial nerve palsy). Focal chorea involving the first three digits of the left hand is visible at rest, on posture, and during walking. Mild superimposed myoclonic jerks are also visible at the same site.


