Abstract
Background
Reported risk factors for the development of a psychogenic movement disorder (PMD) include young age, female gender, history of abuse, current or past psychiatric disorder, lower levels of education and socioeconomic status, and employment as a healthcare worker. Although employment in healthcare is included in several diagnostic criteria for PMD, as well as in many case series, this association has never been validated.
Methods
Using the University of Maryland Movement Disorder Database (UMMDD), we identified PMD cases, as well as patients with isolated focal dystonia as controls. An experienced movement disorder specialist diagnosed all patients, and all cases met criteria for clinically established PMD. Demographic and occupational histories were obtained from medical records and were supplemented by telephone interviews. PMD cases and controls were compared using t tests/χ2 tests.
Results
Controls (n = 148) were older than PMD cases (n = 132), with an average age of 61.4 and 52.1 years, respectively (P < 0.001); there were no significant differences between groups with respect to gender, education level, and ethnicity. The proportion of healthcare workers was not significantly different between PMD cases and controls (25% of PMD cases vs. 20% of controls; P = 0.28).
Conclusions
In contrast to traditional teaching, this investigation demonstrates that in our patient population, patients with a PMD were no more likely to be employed as healthcare workers than patients with isolated focal dystonia. This study calls into question the use of employment in healthcare as a reliable criterion to support the diagnosis of PMD.
Keywords: psychogenic movement disorder, healthcare worker, functional movement disorder, conversion disorder
Psychogenic movement disorders (PMDs), also called functional movement disorders, are common and often present a diagnostic challenge.1 The prevalence of PMD in the general population is unknown; most estimates suggest PMDs comprise about 2% to 3% of patients seen in movement disorder clinics2, 3, 4, 5, 6, 7 with some estimates as high as 25%.8 All types of organic movement disorders [note: we acknowledge that PMDs are also organic and we use the term here only for the sake of differentiation without implying etiology] can be mimicked by a psychogenic disorder, the most common being tremor, dystonia, and myoclonus.4, 6, 7, 9, 10, 11, 12, 13, 14
Criteria for establishing the diagnosis of a PMD was proposed by Williams et al. in 199510 and have since been modified.15, 16, 17 The diagnosis is based primarily on recognizing clinical features that are incongruous and inconsistent with an organic movement disorder. Features from the history suggesting a PMD include abrupt onset, multiple exacerbations and remissions, and other medically unexplained symptoms.18 Reported risk factors for the development of a PMD include young age, female gender, history of abuse, current or past psychiatric disorder, lower levels of education and socioeconomic status, and employment as a healthcare worker.5, 7, 8, 16, 19, 20, 21, 22, 23, 24, 25, 26 That healthcare workers are at greater risk for development of a PMD comes from the idea that disorders observed in the workplace are assumed by the vulnerable patient.15 Yet, despite its repeated mention in the PMD literature, based largely on anecdotal evidence,7, 8, 16, 18, 19, 21, 22, 25, 26 employment in healthcare has not been validated as occurring more frequently in patients with a PMD compared to organic movement disorders.
In a study by Kenney et al.,27 no significant difference in healthcare employment status was observed between patients with essential tremor (n = 33) compared to patients with psychogenic tremor (n = 12). This study, limited by its small sample size, provided preliminary data disputing the association between PMD and healthcare employment, yet subsequent studies by this same group have continued to suggest that working in healthcare is a diagnostic clue for a PMD.18
The objective of this case‐control study was to investigate whether employment as a healthcare worker occurs more commonly in PMD compared to patients with an organic movement disorder, for which we chose to use patients with isolated focal dystonia as the control group.
Methods
Participant Selection
The Institutional Review Board (IRB) at the University of Maryland, Baltimore, approved study protocols. Participants were selected from the IRB‐approved University of Maryland Movement Disorders Database (UMMDD). The UMMDD records diagnostic, demographic, medical, and quality‐of‐life measures for all patients seen at the University of Maryland Movement Disorder Clinic. Additionally, approximately 80% of these patients also consented to be included in the research component of the UMMDD, agreeing to have their information used for research and to be contacted for future research purposes.
At the time of this study, the UMMDD included patients who had been seen at the University of Maryland Movement Disorder Clinic between January 2003 and July 2011. Using the UMMDD, potential PMD cases and controls were identified and medical records were examined to obtain contact information, date of birth, date of initial clinic visit, and diagnosis. PMD cases were eligible for participation if they were coded in the database as “psychogenic” and had a diagnosis of a PMD in their medical record. Patients with isolated focal dystonia were chosen as controls because this population is most similar to the PMD population with respect to age and sex, compared to other organic movement disorders in our database. Furthermore, isolated focal dystonia usually develops independently of a patient's occupation. Patients whose focal dystonia was possibly related to their occupation (e.g, musician's dystonia) were excluded.
Collection of Occupational History
After PMD cases and controls were identified, available demographic, educational, and occupational data were collected using the UMMDD and patient medical records. Our clinic questionnaire, completed by the patient at the initial visit, includes a question about occupation. To obtain a more detailed account of occupational history, we attempted to contact all living PMD cases and controls.
Participants were sent a letter explaining the purpose of the study and were given the opportunity to opt out by returning a de‐identified, prestamped, preaddressed postcard. Two weeks after sending the initial letter, we attempted to contact participants who had not returned the opt‐out postcard. Participants who were contacted by telephone were reminded about the objective of the study and were asked to provide verbal consent. If consent was given, the participants were asked the following questions:
Where you employed at the time of your visit to the University of Maryland Movement Disorder Clinic?
What is your current and/or past occupation?
Have you ever worked as a healthcare professional or in a healthcare setting?
Participants were considered to be or to have been a healthcare worker if they answered “Yes” to question 3 and could provide a description of an occupation agreed on by the research staff to be in the healthcare field. We classified healthcare workers as primary providers or healthcare administrators based on the occupational description provided by the participant.
Data Analyses
The data analysis for this paper was generated using SAS software, Version 9.3 of the SAS System for Windows. (Copyright 2000–2010 SAS Institute Inc. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc., Cary, NC.) Data collected from interviewed and reviewed participants were analyzed using descriptive statistics, t tests, and χ2 tests. Analogous secondary analyses were performed using only data collected from interviewed participants.
Results
PMDs accounted for 3.2% of initial visits to the University of Maryland Movement Disorder Clinic. Using the UMMDD, 152 PMD cases and 189 controls were identified and met criteria to participate in the study (Fig. 1). Opt‐out postcards were mailed back by 25 PMD cases and 42 controls. From our initial sample, we attempted to contact 84% (n = 127) of the PMD cases and 78% (n = 147) of the controls, and successfully interviewed 35% (n = 53) of PMD cases and 51% (n = 97) of controls. A total of 79 PMD cases and 51 controls were unable to be interviewed by phone but had available demographic, educational, and occupational data in the chart and/or database. Combining interviewed and reviewed participants, our final sample included 132 PMD cases (87% of eligible cases) and 148 controls (78% of eligible controls).
Figure 1.
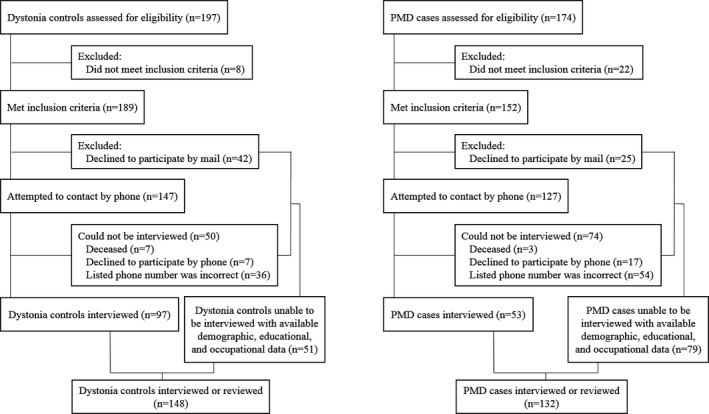
Enrollment diagram of dystonia controls and psychogenic movement disorder (PMD) cases from the University of Maryland Movement Disorders Database (UMMDD).
The subtype of PMD or isolated focal dystonia was noted for PMD cases and controls with some participants having multiple subtypes. For the 132 PMD cases, subtypes included psychogenic gait (13%, n = 20), psychogenic dystonia (8%, n = 13), psychogenic myoclonus (15%, n = 23), psychogenic tremor (50%, n = 79), and other (15%, n = 24). For the 148 controls, subtypes included blepharospasm (14%, n = 23), cervical/craniocervical dystonia (51%, n = 87), orofacial/oromandibular dystonia (8%, n = 14), spasmodic dysphonia (10%, n = 17), writer's dystonia (12%, n = 20), and other (5%, n = 9).
Controls were older than PMD cases, with an average age of 61.4 and 52.1 years, respectively (t (df = 278, n = 280) = 5.97, P < 0.001). There were no significant differences between the groups with respect to gender, education level, and ethnicity (Table 1).
Table 1.
Demographics of Dystonia Controls and Psychogenic Movement Disorder (PMD) Cases
| Demographic | Interviewed and Reviewed Dystonia Controls (n = 148) | Interviewed and Reviewed PMD Cases (n = 132) | P | Interviewed Dystonia Controls (n = 97) | Interviewed PMD Cases (n = 53) | P |
|---|---|---|---|---|---|---|
| Age | <0.001 | <0.001 | ||||
| Mean (SD) | 61.4 (12.4) | 52.2 (13.5) | 62.3 (12.1) | 52.2 (12.5) | ||
| Gender, n (%) | 0.52 | 0.88 | ||||
| Male | 43 (29) | 43 (33) | 30 (31) | 17 (32) | ||
| Female | 105 (71) | 89 (67) | 67 (69) | 36 (68) | ||
| Education, n (%) | 0.91 | 0.57 | ||||
| High school or less | 58 (39) | 55 (42) | 33 (34) | 14 (26) | ||
| College or trade school | 56 (38) | 51 (39) | 31 (32) | 23 (43) | ||
| Advanced degree | 32 (22) | 24 (18) | 29 (30) | 14 (26) | ||
| No information | 2 (1) | 2 (2) | 4 (4) | 2 (4) | ||
| Race, n (%) | 0.11 | 0.19 | ||||
| Caucasian | 122 (82) | 101 (77) | 78 (80) | 38 (72) | ||
| African American | 22 (15) | 18 (14) | 15 (15) | 8 (15) | ||
| Hispanic | 1 (1) | 1 (1) | 0 (0) | 1 (2) | ||
| Multiple | 2 (1) | 4 (3) | 2 (2) | 1 (2) | ||
| No information | 1 (1) | 8 (6) | 2 (2) | 5 (9) |
SD, standard deviation.
Of the PMD cases, 25% (n = 33) had, at least at some point, been employed in the healthcare field compared to 20% (n = 29) of controls (Fig. S1). The proportion of healthcare workers was not significantly different between PMD cases and controls (χ2 (df = 1, n = 280) = 1.18, P = 0.28). Of the 33 PMD cases who had been healthcare workers, 48% (n = 16) were primary providers and 52% (n = 17) were healthcare administrators. Of the 29 controls who had been healthcare workers, 45% (n = 15) were primary providers and 55% (n = 16) were healthcare administrators (Fig. S2). The distribution of healthcare workers, subdivided into provider and administrative roles, was not significantly different between PMD cases and controls (χ2 (df = 1, n = 62) = 0.08, P = 0.77). Furthermore, the distribution of healthcare workers, subdivided into provider and administrative roles, and non‐healthcare workers (Fig. 2) was not significantly different between PMD cases and controls (χ2 (df = 2, n = 280) = 1.27, P = 0.53). Finally, there was no significant difference in the proportion of healthcare workers within each PMD subtype compared to controls, although the numbers of each type were small (Table S1).
Figure 2.
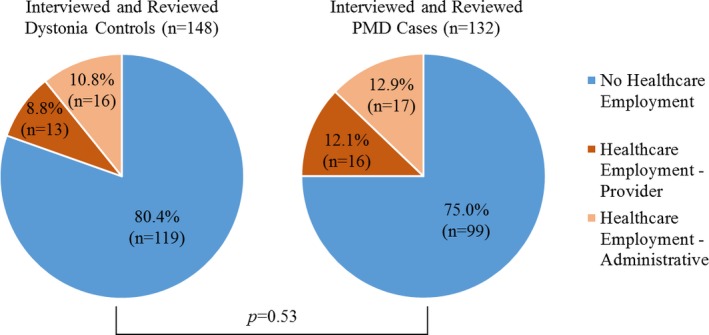
Distribution of healthcare workers, subdivided into provider and administrative roles, and non‐healthcare workers, among interviewed and reviewed dystonia controls and psychogenic movement disorder (PMD) cases. (χ2 (df = 2, n = 280) = 1.27, P = 0.53).
To validate that results were not distorted by the inclusion of participants who were not interviewed for additional occupational information (i.e, reviewed PMD cases and reviewed controls), analogous secondary analyses were performed using only data collected from interviewed participants. Interviewed controls were older than interviewed PMD cases with an average age of 62.3 and 52.2 years, respectively (t (df = 148, n = 150) = 4.86, P < 0.001). There were no significant differences between the groups with respect to gender, education level, and ethnicity (Table 1).
Of the interviewed PMD cases, 34% (n = 18) indicated that they had, at least at some point, been employed in the healthcare field, compared to 26% (n = 25) of interviewed controls (Fig. S3). The proportion of healthcare workers was not significantly different between interviewed PMD cases and interviewed controls (χ2 (df = 1, n = 150) = 1.12, P = 0.29). Of the 18 interviewed PMD cases who had been healthcare workers, 28% (n = 5) were primary providers and 72% (n = 13) were healthcare administrators. Of the 25 interviewed controls who had been healthcare workers, 48% (n = 12) were primary providers and 52% (n = 13) were healthcare administrators (Fig. S4). The distribution of healthcare workers, subdivided into provider and administrative roles, was not significantly different between interviewed PMD cases and interviewed controls (χ2 (df = 1, n = 43) = 1.79, P = 0.18). Furthermore, the distribution of healthcare workers, subdivided into provider and administrative roles, and non‐healthcare workers (Fig. 3) was not significantly different between interviewed PMD cases and interviewed controls (χ2 (df = 2, n = 150) = 3.03, P = 0.22).
Figure 3.
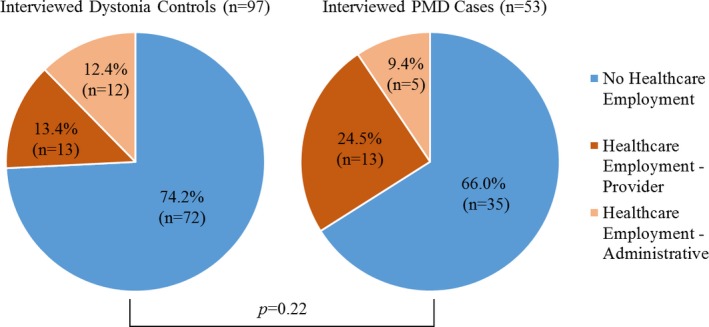
Distribution of healthcare workers, subdivided into provider and administrative roles, and non‐healthcare workers, among interviewed dystonia controls and psychogenic movement disorder (PMD) cases. (χ2 (df = 2, n = 150) = 3.03, P = 0.22).
Discussion
Our results demonstrate that patients with a PMD were no more likely to have been employed in the healthcare field than patients diagnosed with the organic movement disorder, isolated focal dystonia. These results are consistent with the findings of Kenney et al.,27 in which no significant difference in healthcare employment status was observed among patients with essential tremor and patients with psychogenic tremor. Yet many authors continue to list employment in healthcare as a hint or clue suggesting a PMD.7, 8, 16, 18, 19, 21, 22, 25, 26
The origin of the suggestion that PMD patients are more likely to be employed in healthcare is unknown. The earliest mention of such an association lists “Employed in allied health professions” in a table entitled, “Other medical factors suggesting psychogenic tremor” by Koller et al.19 By 2009, “Employed in allied health professions” was still listed as a diagnostic clue but was qualified as “infrequent,” suggesting that some doubt had been cast on the validity of this association.16
In 2006, Shill and Gerber proposed the idea of disease modeling, which suggested that previous exposure to neurological disease was a risk factor for the development of PMD.15 Comparing disease exposure status in 29 psychogenic cases to 50 unmatched controls with an organic movement disorder, they found that 55% of psychogenic cases reported previous exposure to neurological disease versus 24% of control patients (P = 0.01).15
The results presented here are from the largest PMD case‐control study to date to investigate the traditional teaching that employment in healthcare is indeed more common in patients with a PMD and, as such, is a reliable supporting criterion. That we did not find such an association suggests that this clinical feature should be viewed with skepticism. Furthermore, the lack of a difference between patients with a PMD and those with organic focal dystonia suggests that reliance on employment in healthcare has the potential to lead to a misdiagnosis of a PMD. Similarly, Espay and Lang have also suggested recently that many of the traditional historical clues for a PMD are not reliable, although they did not specifically address employment in healthcare.17 Instead, they suggest that the diagnosis of a PMD should rest predominantly on clinical phenomenology and should be made only by movement disorder specialist.
The large number of patients with a PMD is a strength of our study, as is the thorough occupational history obtained by phone interview. A weakness is that most of the occupational history obtained in the medical record and database was limited. Yet, because no difference in healthcare employment was found comparing those reached by phone and those not, it suggests that we were unlikely to have underestimated the number of participants employed in healthcare. It is possible that using a different control group would have yielded a different result, but we chose isolated focal dystonia because, among the various movement disorders, it is most similar to patients with a PMD in terms of gender and age. It is possible that referral bias influenced the number of healthcare workers in our PMD and control group and, as such, these results may not generalize to all patients with PMD. The vulnerabilities and precipitants for development of a PMD remain unknown, but this study suggests that disease modeling through employment in healthcare is not likely to play a significant role.
Author Roles
1. Research Project: A. Conception, B. Organization, C. Execution; 2. Statistical Analysis: A. Design, B. Execution, C. Review and Critique; 3. Manuscript: A. Writing of the First Draft, B. Review and Critique.
C.G.P.: 1B, 1C, 2A, 2B, 2C, 3A, 3B
K.G.H.: 1B, 1C, 2A, 2B, 2C, 3B
A.L.G.‐B.: 1A, 1B, 2A, 2B, 2C, 3B
K.E.A.: 1A, 3B
L.M.S.: 1A, 3B
W.J.W.: 1A,
S.G.R.: 1A, 1B, 1C, 2C, 3B
Disclosures
Funding Sources and Conflict of Interest: The University of Maryland School of Medicine, Department of Neurology, funded this research. The Rosalyn Newman Foundation supports the University of Maryland Movement Disorders Database. The authors report no conflicts of interest.
Financial Disclosures for the previous 12 months: Lisa M. Shulman received research support from the National Institutes of Health, the Rosalyn Newman Foundation, and Kyowa Pharmaceuticals. Stephen G. Reich received research support from the National Institutes of Health and was a paid consultant for UpToDate; royalties: Informa. Christina G. Perry, Katherine G. Holmes, Ann L. Gruber‐Baldini, Karen E. Anderson, and William J. Weiner report no disclosures.
Supporting information
Figure S1. Distribution of healthcare and non‐healthcare workers among interviewed and reviewed dystonia controls and psychogenic movement disorder (PMD) cases. (χ2 (df = 1, n = 280) = 1.18, P = 0.28.)
Figure S2. Distribution of healthcare workers, subdivided into provider and administrative roles, among interviewed and reviewed dystonia controls and psychogenic movement disorder (PMD) cases. (χ2 (df = 1, n = 62) = 0.08, P = 0.77.)
Figure S3. Distribution of healthcare and non‐healthcare workers among interviewed dystonia controls and psychogenic movement disorder (PMD) cases. (χ2 (df = 1, n = 150) = 1.12, P = 0.29.)
Figure S4. Distribution of healthcare workers, subdivided into provider and administrative roles, among interviewed dystonia controls and psychogenic movement disorder (PMD) cases. (χ2 (df = 1, n = 43) = 1.79, P = 0.18.)
Table S1. Distribution of Healthcare Workers Among Interviewed and Reviewed Psychogenic Movement Disorder (PMD) Cases Within Each PMD Subtype, Compared to the Distribution of Healthcare Workers Among Interviewed and Reviewed Controls (n = 29, 20% Healthcare Employment; n = 119, 80% No Healthcare Employment)
Acknowledgments
We gratefully acknowledge and thank all patients of the University of Maryland Movement Disorders Clinic.
Relevant disclosures and conflicts of interest are listed at the end of this article.
References
- 1. Hallett M. Psychogenic movement disorders: a crisis for neurology. Curr Neurol Neurosci Rep 2006;6:269–271. [DOI] [PubMed] [Google Scholar]
- 2. Marsden CD. Hysteria—a neurologist's view. Psychol Med 1986;16:277–288. [DOI] [PubMed] [Google Scholar]
- 3. Lempert T, Dieterich M, Huppert D, Brandt T. Psychogenic disorders in neurology: frequency and clinical spectrum. Acta Neurol Scand 1990;82:335–340. [DOI] [PubMed] [Google Scholar]
- 4. Factor SA, Podskalny GD, Molho ES. Psychogenic movement disorders: frequency, clinical profile, and characteristics. J Neurol Neurosurg Psychiatry 1995;59:406–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Feinstein A, Stergiopoulos V, Fine J, Lang AE. Psychiatric outcome in patients with a psychogenic movement disorder: a prospective study. Neuropsychiatry Neuropsychol Behav Neurol 2001;14:169–176. [PubMed] [Google Scholar]
- 6. Thomas M, Jankovic J. Psychogenic movement disorders: diagnosis and management. CNS Drugs 2004;18:437–452. [DOI] [PubMed] [Google Scholar]
- 7. Reich SG. Psychogenic movement disorders. Semin Neurol 2006;26:289–296. [DOI] [PubMed] [Google Scholar]
- 8. Miyasaki JM, Sa DS, Galvez‐Jimenez N, Lang AE. Psychogenic movement disorders. Can J Neurol Sci 2003;30:S94–S100. [DOI] [PubMed] [Google Scholar]
- 9. Fahn S. Psychogenic movement disorders In: C. David Marsden, Stanley Fahn, eds. Movement Disorders 3. London: Buterworth‐Heinemann; 1994:359–372. [Google Scholar]
- 10. Williams DT, Ford B, Fahn S. Phenomenology and psychopathology related to psychogenic movement disorders. Adv Neurol 1995;65:231–257. [PubMed] [Google Scholar]
- 11. Fahn S, Williams DT, Ford B. Psychogenic movement disorders In: John Noseworthy, ed. Neurological Therapeutics: Principles and Practice, vol. 1. London: Taylor and Francis; 2003:2677–2687. [Google Scholar]
- 12. Sa DS, Galvez‐Jimenez N, Lang AE. Psychogenic Movement Disorders In: Ray Watts, William Koller, eds. Movement Disorders: Neurologic Principles and Practice. 2nd ed New York: McGraw‐Hill Professional; 2004:891–914. [Google Scholar]
- 13. Schrag A, Lang AE. Psychogenic movement disorders. Curr Opin Neurol 2005;18:399–404. [DOI] [PubMed] [Google Scholar]
- 14. Hallett M, Fahn S, Jankovic J, Lang AE, Cloninger CR, Yudofsky SC. Psychogenic Movement Disorders: Neurology and Neuropsychiatry. Philadelphia: Lippincott Williams & Wilkins; 2006. [Google Scholar]
- 15. Shill H, Gerber P. Evaluation of clinical diagnostic criteria for psychogenic movement disorders. Mov Disord 2006;21:1163–1168. [DOI] [PubMed] [Google Scholar]
- 16. Gupta A, Lang AE. Psychogenic movement disorders. Curr Opin Neurol 2009;22:430–436. [DOI] [PubMed] [Google Scholar]
- 17. Espay AJ, Lang AE. Phenotype‐specific diagnosis of functional (psychogenic) movement disorders. Curr Neurol Neurosci Rep 2015;15:32. [DOI] [PubMed] [Google Scholar]
- 18. Thenganatt MA, Jankovic J. Psychogenic tremor: a video guide to its distinguishing features. Tremor Other Hyperkinet Mov (NY) 2014;4:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Koller W, Lang A, Vetere‐Overfield B, et al. Psychogenic tremors. Neurology 1989;39:1094–1099. [DOI] [PubMed] [Google Scholar]
- 20. Anderson KE, Gruber‐Baldini AL, Vaughan CG, et al. Impact of psychogenic movement disorders versus Parkinson's on disability, quality of life, and psychopathology. Mov Disord 2007;22:2204–2209. [DOI] [PubMed] [Google Scholar]
- 21. Nowak DA, Fink GR. Psychogenic movement disorders: aetiology, phenomenology, neuroanatomical correlates and therapeutic approaches. Neuroimage 2009;47:1015–1025. [DOI] [PubMed] [Google Scholar]
- 22. Peckham EL, Hallett M. Psychogenic movement disorders. Neurol Clin 2009;27:801–819, vii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ertan S, Uluduz D, Ozekmekci S, et al. Clinical characteristics of 49 patients with psychogenic movement disorders in a tertiary clinic in Turkey. Mov Disord 2009;24:759–762. [DOI] [PubMed] [Google Scholar]
- 24. Jankovic J. Diagnosis and treatment of psychogenic parkinsonism. J Neurol Neurosurg Psychiatry 2011;82:1300–1303. [DOI] [PubMed] [Google Scholar]
- 25. Miyasaki JM. Functional movement disorders. 2015. Available from: http://www.uptodate.com/contents/functional-movement-disorders. Accessed July 7, 2015.
- 26. Evens A, Vendetta L, Krebs K, Herath P. Medically unexplained neurologic symptoms: a primer for physicians who make the initial encounter. Am J Med 2015;128:1059–1064. [DOI] [PubMed] [Google Scholar]
- 27. Kenney C, Diamond A, Mejia N, Davidson A, Hunter C, Jankovic J. Distinguishing psychogenic and essential tremor. J Neurol Sci 2007;263:94–99. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Distribution of healthcare and non‐healthcare workers among interviewed and reviewed dystonia controls and psychogenic movement disorder (PMD) cases. (χ2 (df = 1, n = 280) = 1.18, P = 0.28.)
Figure S2. Distribution of healthcare workers, subdivided into provider and administrative roles, among interviewed and reviewed dystonia controls and psychogenic movement disorder (PMD) cases. (χ2 (df = 1, n = 62) = 0.08, P = 0.77.)
Figure S3. Distribution of healthcare and non‐healthcare workers among interviewed dystonia controls and psychogenic movement disorder (PMD) cases. (χ2 (df = 1, n = 150) = 1.12, P = 0.29.)
Figure S4. Distribution of healthcare workers, subdivided into provider and administrative roles, among interviewed dystonia controls and psychogenic movement disorder (PMD) cases. (χ2 (df = 1, n = 43) = 1.79, P = 0.18.)
Table S1. Distribution of Healthcare Workers Among Interviewed and Reviewed Psychogenic Movement Disorder (PMD) Cases Within Each PMD Subtype, Compared to the Distribution of Healthcare Workers Among Interviewed and Reviewed Controls (n = 29, 20% Healthcare Employment; n = 119, 80% No Healthcare Employment)


