In the last 30 years, treatment of cervical dystonia (CD) has come to focus on botulinum neurotoxin as the preferred method of choice.1 On the one hand, a considerable number of controlled studies have confirmed its high degree of efficacy in open and double‐blind studies, with a responder rate of between 58% and 95%, and usually at 80%.2 On the other hand, however, the most frequent adverse effects are difficulty in swallowing and weakness of neck muscles.2 These points highlight the current problems of recent work and their potential solutions. If we fully analyze movement patterns and inject the muscles concerned with an adequately adjusted dose, then the responder rate should be higher and the occurrence of disorders in swallowing should be lower.3 One major advance for selecting the relevant muscles came with our ability to distinguish at just which level of the cervical spine the muscles do attach.3 A second major advance was the introduction of sonography for better targeting the muscles and also for properly locating muscles.4 Hereby, we are able to inject the muscles precisely, even deep muscles.4
Anatomy, Muscle Functions, and CD
Before deciding on any particular muscles, an analysis and classification of their movement pattern has to be completed first, and this requires knowing the muscles' origins, their insertions, and their functions. We proposed here a synthetic view of the anatomic organization of the main cervical muscles (Table 1) and schematic view of their action in CD according to the so‐called Col‐Cap concept (Fig. 1).
Table 1.
Anatomic patterns of the main cervical muscles
| Posterior cervical muscles |
| Trapezius pars descendens |
| Linea nuchalis superior—Clavicula (lateral part) |
| Splenius capitis |
| Processus spinosus C3‐Th3—Processus mastoideus |
| Splenius cervicis |
| Processus spinosus Th3‐Th5—Processus transversus C1‐C2 |
| Semispinalis capitis |
| Processus transversus C3‐Th6 and processus spinosus C3‐Th1—Linea nuchalis superior |
| Semispinalis cervicis |
| Processus transversus Th1‐Th6—Processus spinosus C2‐C7 |
| Longissimus capitis |
| Processus transversus C3‐Th3—Processus mastoideus |
| Longissimus cervicis |
| Processus transversus Th1‐TH6—Processus transversus C2‐C6 |
| Obliquus capitis inferior |
| Processus spinosus C2—Processus transversus C1 |
| Lateral cervical muscles |
| Sternocleidomastoideus |
| Suprasternal notch and clavicula (medial part)—Processus mastoideus and linea nuchalis superior |
| Levator scapulae |
| Processus transversus C1‐C4—Scapula (angulus superior) |
| Scalenus medius |
| Processus transversus C2‐C7—First rib |
| Scalenus anterior |
| Processus transversus C3‐C6—First rib |
| Anterior cervical muscles |
| Longus capitis |
| Processus transversus C3‐C6—Occipital bone (basilar part) |
| Longus colli |
| Processus transversus C2‐C5—Atlas (anterior tubercle) |
Figure 1.
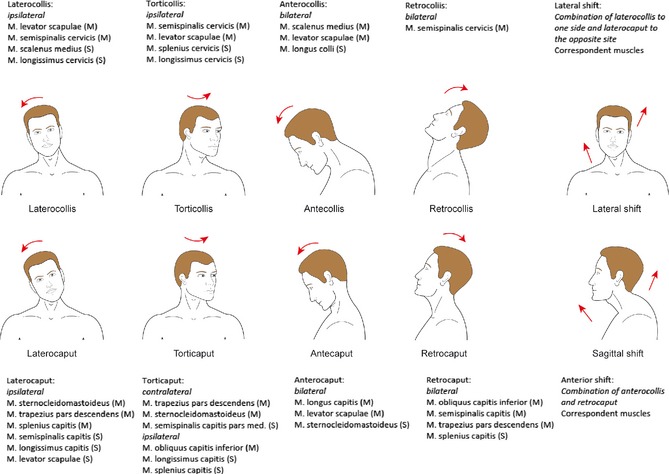
Subtypes of cervical dystonia according to the Col‐Cap concept, with the muscles involved (m, main; s, secondary muscle).
Broadly speaking, the three dimensions of movement can be distinguished. We always have to keep in mind the fact that the cervical spine consists of several vertebrae, joints, and their particular, concomitant levels of movement. From a functional point of view, two levels of movement can be defined: the upper one between the skull and C2 and the lower one between C2 and C7. The C2 vertebra can then be regarded as a kind of fixed point. Although this was not considered important in the classical definitions of laterocollis, retrocollis, anterocollis, and rotatory torticollis, levels of movement of the neck in relation to the trunk and for those of the head relative to the neck have to be distinguished.
When muscles that induce a rotation rostral to C3 are dystonic, the head demonstrates a pivotal movement in relation to the neck, called a torticaput. If movement takes place caudal to C2, a rotation of the neck occurs in relation to the trunk, termed torticollis. The position of the larynx offers help here in clinical orientation: In cases of torticaput, the larynx remains rather more in a medial position, and in torticollis it rotates laterally (Fig. 1). Of course, in cases of torticollis, the head is also rotated, but the main muscles involved act on the C2 to C7 level.
With a lateral flexion, dystonia in the muscles that have their site of origin or insertion in the skull or the first cervical vertebra, induces a malposturing only of the head, but a proper posture of the cervical spine (laterocaput). If those muscles, which originate or insert between C2 and C7 are involved, then the neck is flexed, thus corresponding to laterocollis. In this case, the head and neck are in the same plane (see Fig. 1). Of course, the two conditions can occur in common in cases.
A lateral shift, finally, means the combination of laterocollis to the one side plus a laterocaput to the contralateral side (Fig. 1).
A similar differentiation obtains for head and neck flexion: anterocaput versus anterocollis and retrocaput versus retrocollis (Fig. 1).
Some more‐specific patterns can be described: An anterior shift signifies the combination of anterocollis with retrocaput, and a lateral shift means the combination of laterocollis to the one side plus a laterocaput to the contralateral side.
Another semiological issue frequently observed in CD is shoulder elevation. In some cases, it should be seen not as dystonic, but rather as a compensatory movement.
Discussion
Our recommendations here have considered our own many years of clinical experience, anatomical and electromyographical studies, the most recent data from work in sonography, and publications in the field. Nonetheless, they, of course, remain but a preliminary orientation and simplification. The majority of patients present with combinations of different forms, which means their respective musculature has to be selected as well. Initial treatment stipulates considering just which muscles are primarily involved and usually begins with the muscles most strongly affected.
The more complex the CD becomes, the more difficult is the final selection of muscles for treatment. This necessitates a thorough neurological examination and, frequently, an electromyographical examination.5 The advantage in using sonography is that we can visualize the targeted muscle and inject it with direct sight control.4 The disadvantage is that we cannot decide whether the muscle is actually involved in the dystonia at all, something which is better detailed using electromyography (EMG), which, however, does not aid in reliably assigning the activity to one specific muscle. Another problem is that random EMG activity (which is meant to serve actively balancing out the dystonic posturing and movements) can be mistaken for dystonic activity. It would be an ideal situation if physicians thus have not only access to both techniques, but also extensive experience in their use.
Taking these aspects into consideration means that the relevancy of certain muscles has been lessened, for example, that of the sternocleidomastoideus muscle, whereas others, considered of less importance to date, have attained key status, such as the levator scapulae and the obliquus capitis inferior muscles (Fig. 1).
The problem of dystonic tremor is still unresolved as of yet. In this case, the underlying CD is primarily treated, but then the tremor usually does not improve or even worsens. Often, the contralateral muscles were injected as well, such as the semispinalis and splenius capitis muscles, with no clear evidence until now.
Unfortunately, the scales and ratings presently in use are not sufficiently valid to assess the forms of dystonia detailed above. This means that some of the different forms are rated inadequately.6 In any future revisions of these rating scales, this would have to be taken into consideration. In addition, the actual therapeutic success of earlier studies will now have to be viewed far more critically in light of these arguments.
Author Roles
Manuscript Preparation: A. Writing of the First Draft, B. Review and Critique.
W.H.J.: A, B
L.T.: A, B
Disclosures
Funding Sources and Conflicts of Interest: The authors report no sources of funding and no conflicts of interest.
Financial Disclosures for previous 12 months: W.H.J. and L.T. are speakers and consultants for Allergan, Ipsen, and Merz.
Relevant disclosures and conflicts of interest are listed at the end of this article.
References
- 1. Tsui JK, Eisen A, Mak E, et al. A pilot study on the use of botulinum toxin in spasmodic torticollis. Can J Neurol Sci 1985;12:314–316. [DOI] [PubMed] [Google Scholar]
- 2. Truong D, Jost WH. Therapeutical use of botulinum toxin. Parkinsonism Relat Disord 2006;12:331–355. [DOI] [PubMed] [Google Scholar]
- 3. Reichel G. Cervical dystonia: a new phenomenological classification for botulinum toxin therapy. Basal Ganglia 2011;1:5–12. [Google Scholar]
- 4. Schramm A, Bäumer T, Fietzek U, Heitmann S, Walter U, Jost WH. Relevance of ultrasonography for botulinum toxin treatment of cervical dystonia – an expert recommendation. J Neural Transm 2014. doi: 10.1007/s00702-014-1356-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lee LH, Chang WN, Chang CS. The finding and evaluation of EMG‐guided BOTOX injection in cervical dystonia. Acta Neurol Taiwan 2004;13:71–76. [PubMed] [Google Scholar]
- 6. Jost WH, Hefter H, Stenner A, Reichel G. Rating scales for cervical dystonia: a critical evaluation of tools for outcome assessment of botulinum toxin therapy. J Neural Transm 2013;120:487–496. [DOI] [PMC free article] [PubMed] [Google Scholar]


