A 51‐year‐old man was admitted to the emergency room with an 8‐hour history of sudden right hemiparesis. On examination, right upper extremity strength was graded as 1 proximally, 2 distally, 3 for the lower limb, and there were also right central facial paralysis and motor aphasia. He had a previous medical history of hypertension, dyslipidemia, type 2 diabetes, obesity, and a stroke 3 years before with mild residual right hemiparesis. A head CT showed a large fronto‐parieto‐temporal hypodense area consistent with a left middle cerebral artery (MCA) territory stroke (Fig. 1). A Doppler ultrasound of the carotid and vertebral arteries revealed occlusion of the left internal carotid artery. Arteriography confirmed the left MCA occlusion and revealed two critical intracranial stenosis in the right internal carotid artery. Electrocardiogram showed a slow atrial fibrillation, and an echocardiogram revealed a left ventricular intracavitary thrombus. Before admission, he was on acetyl salicylic acid 100 mg daily, subcutaneous regular insulin 30 U twice‐daily, losartan 50 mg daily, and simvastatin 40 mg daily.
Figure 1.
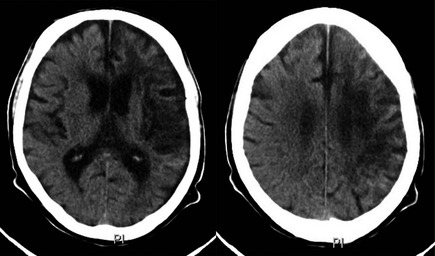
Head CT scan showing a hypodense lesion of left MCA territory suggestive of a stroke.
After approximately 48 hours of admission, he developed patterned involuntary movements in the right upper limb during yawning. The movements, as shown in the video segment (see Video 1), consisted of simultaneous lifting of the entire right upper limb associated with tremor. Upon cessation of yawning, the limb returned to its resting, paretic position. The movement reoccurred continuously with every yawn, and during the episodes, the level of consciousness was preserved, as it was between them. The phenomena ceased spontaneously 12 hours after they were first noticed.
The patient remained with the same neurological deficits throughout admission. He underwent proximal and distal right internal carotid artery angioplasty and subsequent anticoagulation targeting the intracavitary thrombus. Unfortunately, after a 2‐month hospital stay complicated by recurrent episodes of pulmonary and urinary tract sepsis, the patient died as a result of septic shock.
Here, we describe the phenomenon termed parakinesia braquialis oscitans (PBO), recently proposed by Walusinski et al.1 Descriptions of PBO are quite consistent, with jaw opening during the yawn, accompanied by elevation of the paretic limb, and subsequent drop upon ending the movement.1, 2, 3 This phenomenon typically occurs in the upper limbs and may be associated with milder concomitant movement of the lower extremity. In terms of localization of the correspondent brain injury, PBO has been associated with lesions that affect the internal capsule, and basal ganglia and their connections, ranging from cerebrovascular, demyelinating, infectious, and expansive lesions. From a timing perspective, most cases are acute; however, they have been described even within 6 months of the injury.4
Yawning is a stereotyped, involuntary, and repetitive movement observed in almost all vertebrates.4 It is believed that the paraventricular nucleus in hypothalamus plays a role in yawning, as well as medullary and pontine regions, with connections toward the frontal region and cervical spine. The movement is mediated by oxytocin neurons projecting to the hippocampus, reticular formation, and locus ceruleus in the brainstem, but other hormones and neurotransmitters potentially play a role, including serotonin, estrogens, hypocretin, and testosterone. Dopamine, excitatory amino acids, or even oxytocin itself can stimulate further release of oxytocin in these various subcortical structures triggering yawning. On the other hand, opioids can inhibit the oxytocinergic activation, preventing it.2, 4, 5
The pathophysiology of PBO is unknown, but there are at least three theories trying to explain it: (1) Subcortical structures disinhibited by the cerebral cortical damage might release the reticular brainstem formation interconnected with motor pathways, which can be activated by yawning; (2) an “emotional motor system” would be responsible for the involuntary movement of the hemiplegic limb and yawning would activate it as a consequence of an emotional state related to drowsiness, coactivating the bulbar and motor neurons in the brainstem2, 4; and (3) Walusinski et al.5 also propose a mechanism related to the connection between the respiratory peacemaker in pre‐Botzinger complex in ventrolateral medulla of the brainstem and the lateral reticular nucleus during yawning. In this mechanism, the stereotyped movement may lead to lateral reticular nucleus stimulation inducing involuntary limb movement.
The internal capsule is the most common lesion site related with PBO, which can be explained by a corticopontocerebellar tract lesion linking the cerebral cortex to the cerebellum by extrapyramidal motor system neurons. This pathway passes through the internal capsule on each side of the pyramidal tract. PBO is more likely to occur when the damage involves the first neuron of the tract interrupting not only corticospinal and corticonuclear pathways, but also the extrapyramidal corticostriate, corticorubral, corticonigral, and corticoreticular pathways.4 Joining anatomical and physiological observations, another possibility is that cases with previous lesions in the region homologous to the acute insult may be more prone to develop PBO. This a purely speculative observation that cannot be implied by a single observation, but may explain why PBO is almost never observed after large MCA strokes, given that most patients do not have previous pathology in the contralateral hemisphere.
Although the case described here presented a tragic outcome, our review of the sparse literature on PBO does not provide enough substrate to indicate any consistent prognostic value. Also, PBO tends to disappear spontaneously or once motor recovery occurs.1 Overall, many questions remain unanswered regarding this intriguing semiological finding, including its clinical relevance, true prevalence, phenomenology, and physiological implications.
Author Roles
(1) Research Project: A. Conception, B. Organization, C. Execution; (2) Statistical Analysis: A. Design, B. Execution, C. Review and Critique; (3) Manuscript: A. Writing of the First Draft, B. Review and Critique.
M.F.: 3A, 3B
I.B.: 3A
G.B.: 3A
R.P.M.: 3A, 3B
Disclosures
Funding Sources and Conflicts of Interest: The authors report no sources of funding and no conflicts of interest.
Financial Disclosures for previous 12 months: The authors declare that there are no disclosures to report.
Supporting information
A video accompanying this article is available in the supporting information here.
Video 1. Lifting of the paretic right upper limb associated with tremor during yawning. Upon cessation of yawning, the limb returned to its resting paretic position.
Relevant disclosures and conflicts of interest are listed at the end of this article.
References
- 1. Walusinski O, Quoirin E, Neau JP. Parakinesia brachialis oscitans. Rev Neurol (Paris) 2005;161:193–200. [DOI] [PubMed] [Google Scholar]
- 2. Blin O, Rascol O, Azulay JP, Serratrice G. A single report of an hemiplegic arm stretching related to yawning. J Neurol Sci 1994;126:225e7. [DOI] [PubMed] [Google Scholar]
- 3. Lanari A, Delbono O. The yawning and stretching sign in hemiplegics. Medicina (B Aires) 1983;43:355–356. [PubMed] [Google Scholar]
- 4. de Lima PM, Munhoz RP, Becker N, Teive HA. Parakinesia brachialis oscitans: report of three cases. Parkinsonism Relat Disord 2012;18:204–206. [DOI] [PubMed] [Google Scholar]
- 5. Walusinski O, Neau JP, Bogousslavsky J. Hand up! Yawn and raise your arm. Int J Stroke 2010;5:21–27. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A video accompanying this article is available in the supporting information here.
Video 1. Lifting of the paretic right upper limb associated with tremor during yawning. Upon cessation of yawning, the limb returned to its resting paretic position.


