Abstract
Study Design:
Controlled laboratory cross-sectional
Objectives:
To investigate the relationship between femoral version (FV), measured by MRI (FVMRI), Craig’s test and hip rotation range of motion (ROM). To determine rotation ROM values associated with FVMRI categories: excessive anteversion, normal version and retroversion.
Background:
Abnormal FV values are associated with hip disorders, such as osteoarthritis, structural instability, acetabular labral tears and femoroacetabular impingement. Clinical assessment of FV may allow clinician to identify the effect of bony abnormalities on hip rotation ROM to guide clinical decisions.
Methods:
Thirty-eight participants with chronic hip joint pain (CHJP) and 38 matched controls participated. MRI was used to determine FVMRI. A digital inclinometer was used to assess Craig’s test, hip internal rotation (IR) and external rotation (ER) with hip flexed to 90°(90°), and hip IR/ER with hip in neutral flexion/extension (0°). ROM differences (ROMdif) were determined by subtracting ER from IR. Pearson correlation coefficients were used to assess the relationship between FVMRI and clinical variables. One-way analysis of variance (ANOVA) was used to compare rotation ROM among FVMRI categories.
Results:
There were no differences between CHJP and control groups in demographics, FVMRI, Craig’s test or ROM. ROMdif0° showed the highest correlation (r=0.63) with FVMRI, then IR90°(r=0.61) and Craig’s test (r=0.61). Differences were noted among FVMRI categories for rotation ROM except hip ER90°.
Conclusion:
Hip rotation ROM and Craig’s test may be used for screening when imaging is not indicated. A 20° difference between hip IR and ER ROM would be suggestive of abnormal FV.
Keywords: femoral version, range of motion, Craig’s test, movement system, classification
Introduction
Femoral version (FV) is the angle of relative rotation between the femoral neck and shaft(Fabry, et al., 1973). Increased FV, known as excessive femoral anteversion, is associated with anterior acetabular labral tears and structural instability(Beall, et al., 2008; Botser, et al., 2012; Ejnisman, et al., 2013). Decreased FV, known as femoral retroversion, are associated with femoroacetabular impingement and early signs of osteoarthritis(Tonnis and Heinecke, 1991; Ejnisman, et al., 2013). Given the associations among abnormal FV and hip disorders, it is important for clinicians to be able to assess FV, even in the absence imaging. A classification system using reliable, clinically-feasible methods is needed to assist clinicians in screening for abnormal FV.
Normative FV angles in typically developing adults have yet to be established. Historically, 15-20° of anterior rotation of the femoral neck have been used to define the normal FV, however, these values are based on studies that used outdated measurement methods, included small participant samples(Reikeras, et al., 1983) or were completed in children(Fabry, et al., 1973), thus limiting their generalizability. More recent studies suggest adult FV angles are smaller than previously believed(Gulan, et al., 2000; Toogood, et al., 2009; Srimathi, et al., 2012; Ejnisman, et al., 2013). Therefore, establishing categorical cutoffs for increased, normal and decreased FV angles in the adult utilizing published normative data would be useful.
Imaging methods have been considered the gold standard to quantify FV. Computed tomography (CT) has been the most utilized method of measurement(Hernandez, et al., 1981; Mesgarzadeh, et al., 1987; Abel, et al., 1994; Kim, et al., 2008) however, more recently magnetic resonance imaging (MRI) has come into favor due to absence of radiation exposure(Tomczak, et al., 1997; Ito, et al., 2001). Femoral version values quantified by MRI and CT have been shown to be highly correlated(Botser, et al., 2012). Although imaging is effective in determining FV angles, these techniques are expensive, time consuming, and inaccessible in rehabilitation settings.
The most commonly reported clinical methods to assess FV are the Craig’s test, also known as the trochanteric prominence angle test,(Ruwe, et al., 1992; Sangeux, et al., 2014) and hip rotation range of motion (ROM) (Cibulka, 2004; Sangeux, et al., 2014). In 1992, Ruwe et al(Ruwe, et al., 1992) reported Craig’s test as being both accurate and valid for determining FV compared to CT. Chung et al(Chung, et al., 2010) also found high correlations between Craig’s test and CT values in children with cerebral palsy. However, other studies have reported low correlations between Craig’s test and imaging or intra-operative studies(Staheli, et al., 1985; Davids, et al., 2002; Sangeux, et al., 2014). Given the inconsistency, alternative clinical methods using hip rotation ROM to determine FV have been suggested(Botser, et al., 2012; Ejnisman, et al., 2013).
Hip rotation ROM may be an appropriate clinical measure to estimate FV, as it is commonly performed during clinical examination, has good reliability(Holm, et al., 2000) and is associated with FV(Botser, et al., 2012; Ejnisman, et al., 2013). Increased FV values are associated with decreased external rotation (ER) and increased internal rotation (IR) ROM, while decreased FV may contribute to decreased IR ROM increased ER ROM(Botser, et al., 2012; Ejnisman, et al., 2013). Although this relationship has been reported, a method using ROM values to detect FV categories has not been established. Additionally, few have reported on the relationship between FV and the difference between IR and ER ROM(Holm, et al., 2000). Using both IR and ER ROM may provide additional information to that obtained from Craig’s test and isolated ROM values.
The first purpose of this study was to investigate the relationship between femoral version measured by MRI (FVMRI) and hip rotation ROM. We hypothesized the rotation ROM differences (ROMdif) would demonstrate a higher correlation with FVMRI compared to Craig’s test and isolated ROM values. Second, we used previously published, normative data(Toogood, et al., 2009) to define three categories of FV, excessive anteversion, normal version and retroversion, and compared hip rotation ROM among the three categories. We hypothesized that compared to those with normal version, those with excessive anteversion would demonstrate decreased ER, and those with retroversion would demonstrate decreased IR. Finally, we used our hip rotation ROM difference findings to propose a clinically, feasible method to screen for and categorize abnormal FV. We were interested to see if the clinical tests would perform similarly among asymptomatic and symptomatic people due to the possibility that symptomatic people may have limited ROM compared to asymptomatic people, therefore we performed the tests on those with chronic hip joint pain (CHJP) and those with no history of hip pain.
Methods
Participants
Participants in this study were a subset from a cohort study assessing proposed risk factors for CHJP. People with CHJP and asymptomatic controls were recruited from [blinded] research volunteer database, Orthopaedic and Physical Therapy clinics and public announcements.
Participants with CHJP had to report deep hip joint or anterior groin pain lasting three months or more, which was reproducible with the flexion-adduction-internal-rotation test (FADIR). The FADIR is highly sensitive for identifying the hip joint as the location of pain, however is not specific to a particular tissue source(Martin, et al., 2008; Maslowski, et al., 2010). Control participants had no history of hip pain and were matched to participants with CHJP, one to one, by sex, age (within five years), BMI (within five kg/m2), and limb side. For both groups, participants were excluded if they met the following criteria: 1) previous hip surgery or fracture, 2) contraindications to MRI, 3) known pregnancy, 4) neurological involvement impacting coordination or balance, 5) BMI greater than 30 or 6) screening tests indicated lumbar spine radiculopathy. The involved limb or most symptomatic limb (if bilateral involvement) of the CHJP participant was assessed.
Ethical Approval Statement
This study was approved by [blinded] Human Research Protection Office. Prior to study participation, a signed statement of informed consent was obtained.
Procedure
Participants completed self-report questionnaires for demographic information, medical history, hip pain history and the University of California Los Angeles Activity Score (UCLA)(Amstutz, et al., 1984). The Hip Disability and Osteoarthritis Outcome Score (HOOS),(Klassbo, et al., 2003; Nilsdotter, et al., 2003) was administered to determine level of hip-specific functional disability in the CHJP group.
MRI Measure of Femoral Version (FVMRI)
The procedures for image acquisition and angle measurement have been reported previously(Harris-Hayes, et al., 2014). MRI images were attained using a 1.5T MR system (Avanto, Siemens; Erlangen, Germany). Two-3D fat suppressed gradient echo imaging sequences were acquired, a coronal sequence centered at the pelvis and an axial sequence centered at the distal femora, using the following parameters: repetition time 15.96 ms, echo time 6.2 ms, flip angle 25°, field of view 400 mm, matrix 512×512, and slice thickness 0.82 mm. Using a standard technique, participants were positioned supine with hips in neutral hip flexion, abduction and rotation. Coils and spacers were placed to maintain limb position and minimize movement during image acquisition. Total acquisition time was approximately 14 minutes.
The proximal 3D MR image was post-processed (LEONARDO; Siemens; Erlangen, Germany) to create a 2D axial oblique pelvic image through the femoral neck center. ANALYZE 11.0 (Biomedical Imaging Resource, Mayo Foundation, Rochester, MN) software was used to complete FVMRI measurements. FVMRI was represented by the angle between the femoral neck axis (Figure 1a) and femoral condylar axis (Figure 1b). A line vertical to the pelvic coronal axis was used as reference. FVMRI was then calculated by subtracting the femoral condylar axis value from the femoral neck axis value. To limit variability due to different examiners, a single examiner, blinded to group, performed all measurements. Inter-rater reliability of our methods has been reported previously(Harris-Hayes, et al., 2014) and is excellent, ICC2,1 = 0.97, standard error of measurement (SEM) was 1.1°.
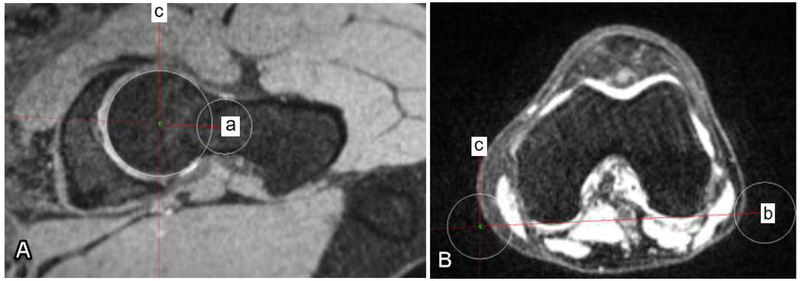
Figure 1.
Femoral version as measured by MRI (FVMRI) is represented by the angle between (A) line a that extends from the center of the femoral head to the center of the femoral neck and (B) line b that aligns along the most posterior aspect of the distal femoral condyles. Line c represents a vertical reference line that is perpendicular to the pelvic coronal axis.
Clinical Measures
A licensed physical therapist (MHH) with 16 years of experience performed the clinical measures. An assistant helped with documentation and limb stabilization. A microFET3 (Hoggan Health Industries, West Jordan, UT) digital inclinometer was used to capture angular measures for Craig’s test and ROM tests. The accuracy of the microFET in measuring ROM is within 1°.
Prior to testing, each participant performed a five-minute warm-up using a comfortable pace on a stationary bike or treadmill. To ensure standard placement of the inclinometer during testing, marks were placed 4 cm proximal to the medial malleoli. Tests were completed in the following order: IR and ER ROM with hip flexed to 90°, Craig’s test, then IR and ER with hip in neutral flexion/extension.
For each of the clinical measures, the examiner first positioned the hip in the starting position with the shank vertical to the testing surface. To eliminate the effect of tibial angulation on the final measure, the inclinometer was placed on the previously placed mark proximal to the medial malleolus (Figure 2) to obtain the starting angle of the shank. The examiner then used one hand for stabilization of adjacent segment while using the other hand to passively rotate the participant’s hip into IR or ER. For hip rotation ROM measures, end of hip joint ROM was defined as a firm or bony end-feel, without additional motion occurring at the pelvis or knee. Motion occurring at the knee(Harris-Hayes, et al., 2007) or pelvis may artificially inflate hip rotation ROM values. Once the end range was determined, the assistant held the limb as the examiner placed the inclinometer and obtained the ending angle of the shank. The inclinometer then calculated the final value using the starting and ending shank angles. Due to the technique necessary to ensure accurate collection, the examiner was not blinded to the values displayed on the inclinometer, however the examiner had no knowledge of the patient’s femoral version as measured by MRI. Each test was performed and measured three times. If there was a difference greater than 5° among the values, the trial was omitted and an additional measurement was performed. Previous reports have stated that differences between examiners can be as high as 7° for internal and external rotation of the hip(Dobson, et al., 2012; Ratzlaff, et al., 2013), therefore we believe a difference of 5° to be conservative. With each trial, the assistant documented if the participant reported pain during the test and if the reported pain prevented the examiner from achieving end ROM.
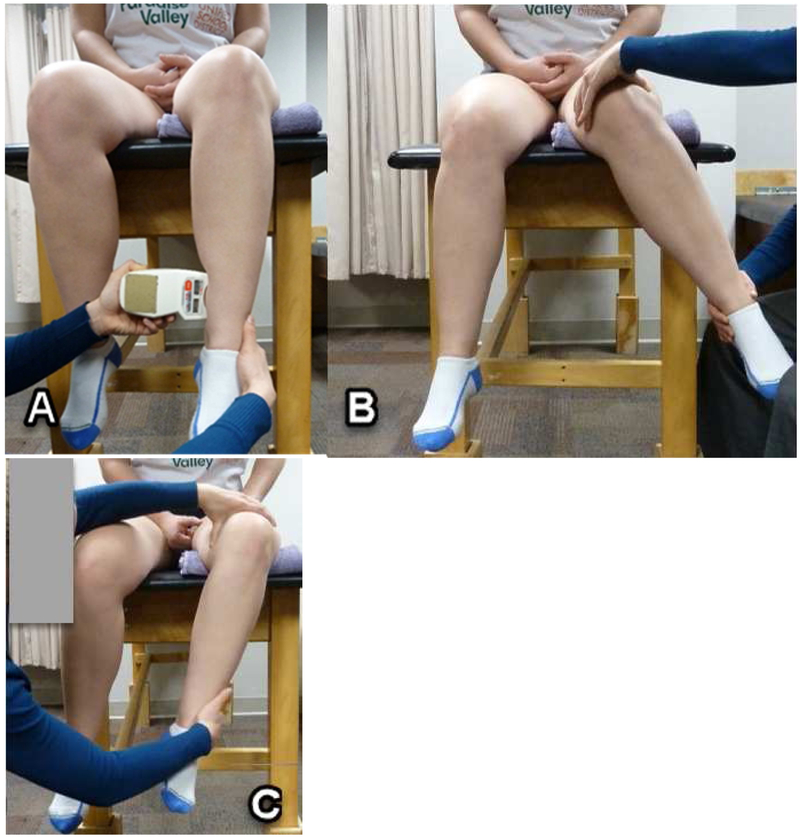
Figure 2.
Methods to assess hip rotation range of motion (ROM). (2A) Placement of the inclinometer. Position shown is for rotation ROM with the hip flexed to 90°. With the shank in vertical position, the inclinometer was placed four cm proximal to the medial malleoli and “zeroed” to eliminate the effect of tibial angulation on the final measure. For the Craig’s test and rotation ROM with the hip in neutral flexion/extension, the person was in prone, with the shank in vertical position. (2B) End of joint rotation range of motion (ROM) with the hip flexed to 90° for Hip internal rotation and (2C) for Hip exte rnal rotation. A folded towel was placed under the distal femur to ensure the 90° hip flexed position was attained. The pelvis and knee were monitored to prevent additional motion occurring at these adjacent joints.
To collect measures for ROM with the hip flexed to 90° (Figure 2), participants sat with their knees flexed, hanging over the testing surface. The examiner placed the tested limb so the hip was in 90° flexion and neutral abduction/adduction. To determine IR ROM, the examiner placed one hand on the distal thigh to maintain the thigh position while using the opposite hand to passively rotate the participant’s hip into IR. Similar methods were used for ER ROM, however the hip was rotated into ER.
To attain data for ROM with the hip in neutral flexion/extension (Figure 3), participants were positioned in prone with the knee flexed to 90°. For IR ROM, the hip was placed in neutral abduction/adduction. The examiner placed one hand on the pelvis to prevent pelvic motion while using the opposite hand to passively rotate the participant’s hip into IR. Prior to performing ER ROM, the hip was abducted 15° to reduce the influence of the ten sor fascia latae-iliotibial band (TFL-ITB) on ER ROM(Kendall, et al., 2005). Methods similar to that of IR ROM were then used for ER ROM, however the hip was rotated into ER.
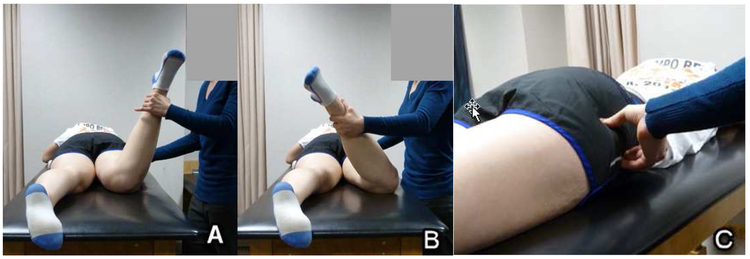
Figure 3.
End of hip joint rotation range of motion (ROM) with the hip in neutral flexion/extension and Craig’s test. (3A) Hip internal rotation with the hip in 0° of abduction, (3B) Hip external rotation with the hip in 15° of abduction. The pelvis and knee were monitored to prevent additional motion occurring at these adjacent joints. (3C) Hand placement for the Craig’s test, demonstrating the hip position where the greater trochanter is in its most lateral position.
To perform Craig’s test, the participant was positioned in prone with the knee flexed to 90°. The examiner rotated the hip alternately into IR and ER to determine the hip position where the greater trochanter was in its most lateral position (Figure 3). The angle between the shank and the vertical reference was used as the FV angle. For each clinical variable, three trials were averaged. The ROM difference with hip flexed to 90° (ROMdif90°) and with hip in neutral flexion/extension (ROMdif0°) was determined by subtracting the ER angle from the IR angle measured in the respective positions. Test-retest reliability and SEMs for ROM and Craig’s test are provided (Table 1).
Table 1.
Test-retest reliability and standard error of measurement of range of motion and Craig’s tests.
| Variable | ICC (3,3) | SEM (°) |
|---|---|---|
| ER90° | 0.82 (0.32, 0.95) | 3 |
| IR90° | 0.96 (0.84, 0.99) | 3 |
| Craig’s test | 0.97 (0.89, 0.99) | 2 |
| ER0° | 0.99 (0.95, 1.00) | 2 |
| IR0° | 0.92 (0.69, 0.98) | 3 |
Abbreviations: ICC, intraclass correlation coefficient; SEM, standard error of measurement; ROM, range of motion; ER90°, external rotation ROM with hip flexed to 90°; IR90°, internal rotation ROM with hip flexed to 90°, ER0°, external rotation ROM with hip in neutral flexion/extension; IR0°, internal rotation ROM with hip in neutral flexion/extension 0°
Statistical Analysis
This study is a secondary analysis of data collected in the parent study. For the parent study, an a priori power calculation indicated a sample size of 80 participants, 40 per group, would provide statistical power of at least 0.80 to detect differences in our primary variable of hip abductor strength, with effect sizes of at least 0.64 at an alpha of .05 using 2-tailed tests. For statistical analysis, Levene’s test was used to test for homogeneity of variance. Participant characteristics were compared between groups using independent t-tests except for the UCLA, in which case Mann-Whitney U Test was used. There were no differences between groups for FVMRI, Craig’s test or hip ROM values (Table 2). Therefore, we collapsed data from both groups to determine bivariate correlation and to determine ROM differences between FV categories. Pearson correlation coefficients were used to assess the relationship between FVMRI and the clinical variables.
Table 2.
Group characteristics.
| Variable | CHJP N=38 |
Control N=38 |
P
Value |
|---|---|---|---|
| Demographics | |||
| Sex | 32F:6M | 32F:6M | |
| Limb side | 22R:16L | 22R:16L | |
| Age, years* | 28.1±5.0 | 27.7±5.6 | 0.78† |
| BMI, kg/m2* | 24.1±3.1 | 24.0±2.6 | 0.90† |
| UCLA‡ǁ | 9 (3-10) | 10 (4-10) | 0.20§ |
| FVMRI | 8.0±8.4 | 10.2±7.5 | 0.24† |
| Craig’s test | 16±7 | 16±7 | 0.99† |
| Hip ROM | |||
| ER90°, deg * | 40±6¶ | 38±6 | 0.25† |
| IR90°, deg * | 39±9 | 40±7 | 0.77† |
| ER0°, deg * | 42±9 | 40±10 | 0.58† |
| IR0°, deg * | 32±10 | 32±8 | 0.79† |
Abbreviations: CHJP, Chronic hip joint pain; F, Female; M, Male; R, Right; L, Left; BMI, body mass index; kg, kilogram; m, meters; UCLA, University of California Los Angeles Activity Score; FVMRI, femoral version by MRI; ROM, range of motion; ER90°, external rotation ROM with hip flexed to 90°; deg, degrees; IR90°, internal rotation ROM with hip flexed to 90°; ER0°, external rotation ROM with hip in neutral flexion/extension; IR0°, internal rotation ROM with hip in neutral flexion/extension; deg, degrees
Values are mean ± standard deviation.
Independent sample t-tests were used.
UCLA: participants are asked to rate their activity level over the previous 6 months. 1=wholly inactive, dependent on others; 10=regularly participates in impact sports such as jogging, tennis, skiing, acrobatics, ballet, heavy labor, or backpacking.
Values are median (range)
Mann-Whitney U Test was performed. One control participant did not complete UCLA.
Data from one participant with CHJP was omitted secondary to pain limiting end range of motion.
Due to the discrepancies previously reported for normative femoral version values for healthy adults, we used Toogood et al’s(Toogood, et al., 2009) reported values as the basis for our categorical cut-offs. We defined abnormal femoral version as those values that were one standard deviation above and below the reported mean. Using the reported mean and standard deviation, 9.73°+9.28°, normal FV ranged from 0.45°to 19.01° , femoral retroversion was defined as values less than 0.45° and excessive fem oral anteversion was defined as values greater than 19.01°. Differences among the three FVMRI categories in ROM variables were compared using one-way analysis of variance (ANOVA). Tukey honest significant difference (HSD) were used for Post Hoc group comparisons. Statistical analyses were performed using SPSS version #23 statistical software (SPSS Inc, Chicago, Illinois). Statistical significance was considered when p <0.05.
Results
We recruited 80 participants but we experienced technical difficulties with MRI acquisition for two participants, therefore two matched groups were excluded from this analysis, leaving 38 matched pairs. The majority of our subjects were female. There were no between group differences in age, BMI, activity level, FVMRI or clinical measures (Table 2). Participants with CHJP reported a long pain duration and moderate disability (Table 3). Twelve participants with CHJP reported pain during at least one clinical test. Pain prevented the examiner from achieving the end range for ER90° in one participant with CHJP, therefore the individual’s data for that test was omitted from the analysis.
Table 3.
Descriptive data reporting pain and patient-reported outcome measures in participants with chronic hip joint pain.
| Variable | CHJP N=38 |
|---|---|
| Pain duration, years* | 3.4 (0.4-13) |
| Avg pain† | 3.0 (1-8) |
| Worst pain† | 6.0 (2-10) |
| HOOSPain‡ | 74.6 ± 14.6 |
| HOOSSymptoms‡ | 71.4 ± 17.4 |
| HOOSADL‡ | 89.6 ± 11.3 |
| HOOSSport‡ | 71.2 ± 21.1 |
| HOOSQOL‡ | 57.4 ± 21.1 |
| MHHS‡ | 78.8 ± 11.9 |
Abbreviations: CHJP, chronic hip joint pain; Avg, average; HOOS, Hip Disability and Osteoarthritis Outcome Score; MHHS, Modified Harris Hip Score; ADL, function in activities of daily living; Sport, function in sports and recreation; QOL, quality of life
Value is mean (range).
Pain rated by the participant using a verbal numerical pain rating scale. 0=no pain; 10=worst pain imaginable. Values are median (range)
Patient-reported outcome measures with 100=no disability. Values are means ± SD.
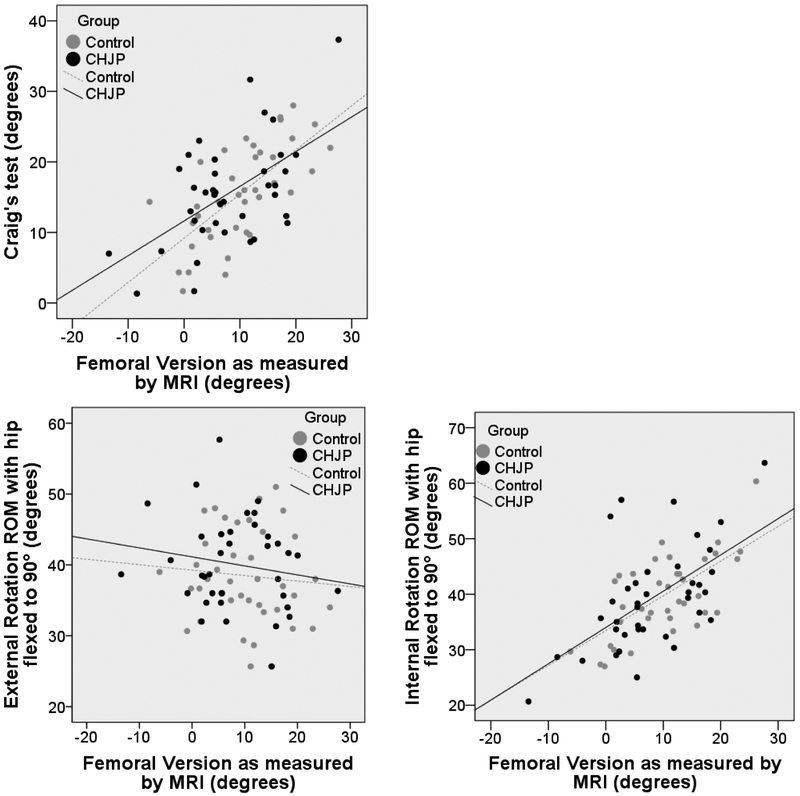
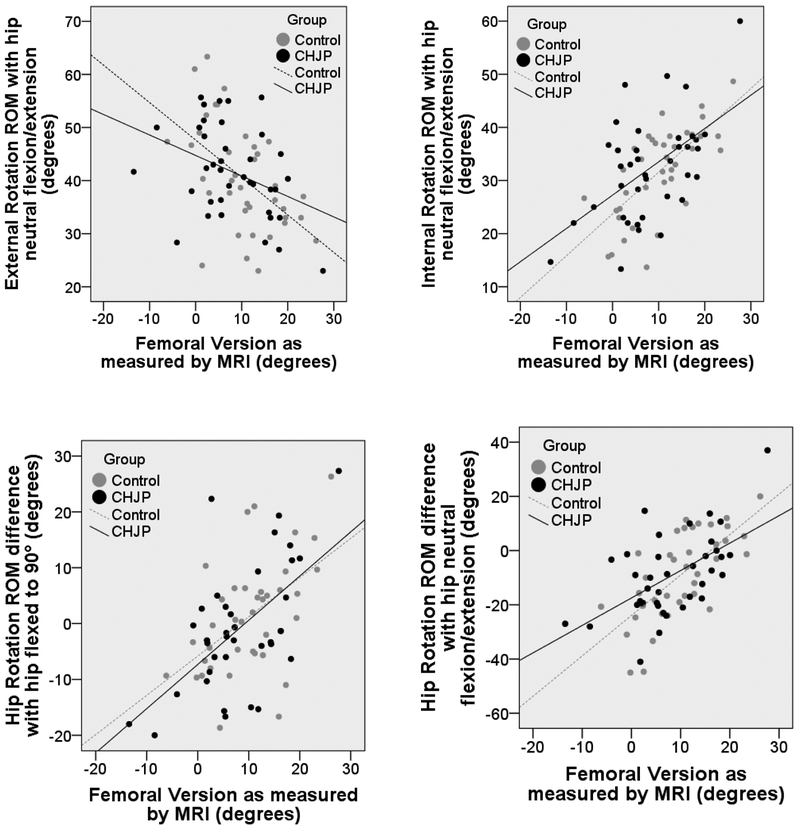
All clinical measures, except ER90°, were correlated with FVMRI (Table 4; Figure 4). ROMdif0° showed the highest correlation, followed by IR90° and Craig’s test. Correlations were slightly lower in participants with CHJP compared to control participants. Using our defined categories, 7 hips (4 CHJP; 3 controls) were classified as femoral retroversion, 61 (32 CHJP; 29 controls) as normal version and 8 (2 CHJP; 6 controls) as excessive anteversion. Differences among the FVMRI categories were found for all rotation ROM variables except hip ER90° (Table 5).
Table 4.
Correlation between clinical tests and femoral version as measured by magnetic resonance imaging (MRI).
| All | Control | CHJP | ||||
|---|---|---|---|---|---|---|
| Variable | r | P | r | P | r | P |
| FV MRI, deg | ||||||
| Craig’s test, deg | 0.61 | <0.01 | 0.68 | <0.01 | 0.56 | <0.01 |
| Hip ROM | ||||||
| ER90°, deg* | −0.14 | 0.22 | −0.09 | 0.59 | −0.17 | 0.32 |
| IR90°, deg | 0.61 | <0.01 | 0.66 | <0.01 | 0.59 | <0.01 |
| ER0°, deg | −0.45 | <0.01 | −0.52 | 0.01 | −0.38 | 0.02 |
| IR0°, deg | 0.60 | <0.01 | 0.70 | <0.01 | 0.54 | <0.01 |
| Hip ROM difference† | ||||||
| ROMdif90°, deg* | 0.56 | <0.01 | 0.51 | 0.01 | 0.59 | <0.01 |
| ROMdif0°, deg | 0.63 | <0.01 | 0.70 | <0.01 | 0.57 | <0.01 |
Abbreviations: CHJP, Chronic hip joint pain; FVMRI, femoral version by MRI; deg, degrees; ROM, range of motion; ER90°, external rotation ROM with hip flexed to 90°; IR90°, internal rotation ROM with hip flexed to 90°; ER0°, external rotation ROM with hip in neutral flexion/extension; IR0°, internal rotation ROM with hip in neutral flexion/extension; ROMdif90°, difference in ROM with hip flexed to 90°; ROMdif0°, difference in ROM with hip in neutral flexion/extension
Data from one participant with CHJP was omitted secondary to pain limiting endrange of motion.
ROM difference was calculated by subtracting ER ROM from IR ROM
Figure 4.
Scatter-plot charts demonstrating the correlation between clinical tests and femoral version as measured by magnetic resonance imaging (MRI). ROM = range of motion; MRI = magnetic resonance imaging; CHJP = chronic hip joint pain.
Table 5.
Range of motion values by femoral version category
| Variable | Anteversion < 0.45° |
Normal 0.45°-19.01° |
Retroversion >19.01° |
P
Value |
|---|---|---|---|---|
| Mean ± SD N = 8 |
Mean ± SD N = 61 |
Mean ± SD N = 7 |
||
| FVMRI, deg | 22.27 ± 3.31 | 8.99 ± 5.50 | −4.88 ± 4.86 | <0.01‡ |
| Craig’s test, deg | 24 ± 7 | 15 ± 6 | 8 ± 7 | <0.01‡ |
| Hip ROM | ||||
| ER90°, deg* | 36 ± 5 | 40 ± 7 | 39 ± 5 | 0.39 |
| IR90°, deg | 51 ± 8 | 39 ± 7 | 28 ± 4 | <0.01‡ |
| ER0° deg | 33 ± 5 | 42 ± 9 | 45 ± 10 | 0.02§ |
| IR0°, deg | 43 ± 8 | 32 ± 8 | 22 ± 16 | <0.01‡ |
| Hip ROM difference† | ||||
| ROMdif90° deg* | 14 ± 9 | 0 ± 10 | −10 ± 7 | <0.01‡ |
| ROMdif0°, deg | 11 ± 13 | −10 ± 13 | −22 ± 9 | <0.01§ |
Abbreviations: SD, standard deviation; FVMRI, femoral version as measured by magnetic resonance imaging; deg, degrees; ROM, range of motion; ER90°, external rotation ROM with hip flexed to 90°; IR90° internal rotation ROM with hip flexed to 90°; ER0°, external rotation ROM with hip in neutral flexion/extension; IR0°, internal rotation ROM with hip in neutral flexion/extension; ROMdif90°, difference in ROM with hip flexed to 90°; ROMdif0°, difference in ROM with hip in neutral flexion/extension
Data from one participant with chronic hip joint pain was omitted secondary to pain limiting end range of motion.
ROM difference was calculated by subtracting ER ROM from IR ROM
Significant difference between anteversion and normal; anteversion and retroversion; normal and retroversion
Significant difference between anteversion and normal; anteversion and retroversion
Discussion
We investigated the relationship between FVMRI and clinical measures among young to middle aged adults with and without CHJP. Our findings suggest that hip rotation ROM measures and Craig’s test may be used for screening purposes when imaging is not available or indicated. Among all participants, ROMdif0° had the highest correlation with FVMRI, however, it was only slightly higher than IR90° and Craig’s test. As expected, we noted significant differences in hip ER ROM and IR ROM among participants classified by their FVMRI category. Finally, we present ROM difference values that may be used to classify FV categories among those with existing injury or potentially, those seeking preventative screenings.
We found similar correlations between hip rotation ROM and Craig’s test with FVMRI. Given these findings, individual characteristics of the person may be considered when selecting clinical tests. One challenge to performing the Craig’s test is palpation of the greater trochanter, particularly in those with adipose tissue surrounding the greater trochanter. In these cases, the ROM measures may be preferred. This concept is supported by Souza and Powers,(Souza and Powers, 2009) who noted that those with the highest BMI had the largest errors between MRI and Craig’s test. However, Craig’s test may be preferred over ROM measures in populations with neuromuscular conditions that result in muscle spasticity or joint contractures that directly influence hip joint ROM(Ruwe, et al., 1992; Davids, et al., 2002; Chung, et al., 2010). For example, a child with cerebral palsy may demonstrate limited hip rotation ROM due to muscle spasticity, therefore the rotation ROM measures in this child may be less predictive of femoral version.
The moderate correlation between ROM measures and FVMRI indicate other factors contribute to hip ROM, such as additional bony abnormalities and soft tissue extensibility. For example, hip IR90° may be restricted by a reduced femoral head-neck offset. We performed a post hoc analysis using maximum alpha angle to quantify femoral head-neck offset and detect cam morphology. Surprisingly, we found no correlation (r = −0.06, P = 0.61) between alpha angle and hip IR90°. Further, removing participants with cam morphology (9 CHJP; 4 controls) from the analysis did not significantly change the correlations between rotation ROM and FVMRI. Finally, extensibility of soft tissues including muscle and capsule contribute to hip rotation ROM, however, quantifiable methods to determine their contribution in vivo have many challenges.
We have introduced new criteria to define excessive femoral anteversion, normal version and retroversion, using published normative data.(Toogood, et al., 2009) In their study, Toogood et al(Toogood, et al., 2009) examined femoral version in a large sample of adult skeletons with a broad representation of gender and race, therefore we believe the cutoffs (< 0.45° and > 19. 01°) we established based on Toogood’s normative data are generalizable to a large population. Other recent studies report similar mean values to those of Toogood et al, further supporting that normal femoral version angles are likely closer to 10°(Srimathi, et al., 2012; Ejnisman, et al., 2013) than the previously suggested 15-20°. We do not know if the categories for femoral version as defined in this study indicate an increased risk for injury, therefore, future investigation of this relationship is needed. In the current study, we have demonstrated that hip rotation ROM does vary among the three categories, which may be important in rehabilitation programs.
Using our defined categories for FVMRI, we confirmed that those with femoral retroversion have decreased IR ROM in both hip positions compared to those with normal version and excessive anteversion. Those with excessive femoral anteversion have decreased ER ROM when the hip is positioned in neutral flexion/extension compared to those with normal version or retroversion. Our findings are important when considering the activities in which people participate. For example, IR creates a mechanical abutment between the anterolateral femoral head-neck junction and the anterior acetabular rim, thus resulting in stresses being placed on the anterior acetabular labrum and articular cartilage(Bedi, et al., 2013). A patient with femoral retroversion and thus decreased hip internal rotation, will experience this mechanical abutment earlier in the limb motion. If the patient participates in an activity requiring repetitive IR motion, repetitive microtrauma of the anterior joint structures may accumulate, leading to eventual macrotrauma and subsequent injury.(Mesgarzadeh, et al., 1987; Silveira and Piedade, 2014; Avila, et al., 2016). Conversely, ER creates a mechanical abutment between the posterolateral femoral head-neck junction and the posterior acetabular rim, potentially resulting in repetitive stresses on the posterior acetabular labrum and articular cartilage(Bedi, et al., 2013).
Although not the purpose of this report, it is important to note that there were no differences in FVMRI when comparing those with CHJP and asymptomatic controls (Table 2). This finding may call into question the clinical importance of assessing femoral version, given the values of femoral version do not discriminate between people with CHJP and asymptomatic controls. Although the type of femoral version did not discriminate between people with CHJP and asymptomatic controls in this study, we believe more research is needed to examine the relationship between femoral version and injury. A theoretical mechanical explanation exists for the relationship between abnormal femoral version and injury, however there is a paucity of evidence related to the temporal relationship. Prospective studies are needed. Nevertheless, a number of studies have reported an association between abnormal femoral version and hip joint disorders, such as osteoarthritis, femoroacetabular impingement and structural instability(Tonnis and Heinecke, 1991; Beall, et al., 2008; Botser, et al., 2012; Ejnisman, et al., 2013). Although current evidence is limited, it may be useful to consider a patient’s femoral version when prescribing exercise and assessing daily tasks. By identifying a patient’s femoral version category and assessing the amount of hip rotation ROM required during their daily activities, particularly those activities that are symptom-provoking, we may better instruct people in alignment and movement strategies to reduce stresses within the hip joint.
Previous authors have suggested comparing the amount of IR ROM to ER ROM to determine femoral version category, however, this is the first study to investigate rotation ROM differences among adults. Cibulka(Cibulka, 2004) concluded that differences of 30° between hip IR an d ER may be suggestive of abnormal femoral version. For example, if IR ROM was greater than ER ROM by 30°, then excessive femoral anteversion may be suspected. The value of 30°, however, was based on studies performed primarily in children. Our data from adults aged 18-40 years, suggests the critical value may be closer to 20° and may be dependent on the hip position tested. Looking specifically at ROMdif0°, the variable most highly correlated with FVMRI, ER ROM that is 20° greater than IR ROM would suggest femoral retroversion. However, IR ROM that is only 10° greater than ER ROM may indicate excessive anteversion. The value indicative of abnormal version in the ROMdif90° position was 10° and 15°for retroversion and excessive anteversion respectively. Taking all of this into account, a difference of 20° could be used as a conservative value to clinically categorize FVMRI in all testing positions. Furthermore, asymmetries greater than 20° would likely indicate a greater abnormality in FVMRI.
Limitations
As discussed, we did not take into account other bony abnormalities that may contribute to hip ROM values, likely moderating the relationship between hip rotation ROM and FVMRI. The population in this study was relatively homogeneous with specific criteria on age and BMI, prompting the need for further research using a broader population in regards to age, anthropometrics and gender. The majority of females in the current study may have impacted our results as it has been reported that females and males may demonstrate differences in morphologic presentation(Nepple, et al., 2014). We included people with CHJP, whose ROM may be affected by their condition. We were able to achieve the end ROM for all participants, except for ER90° in one participant. Additionally, our analysis determined there were no differences in ROM between the participants with CHJP and their matched controls. A strength of this paper is that we focused on a population who are less likely to have advanced age-related structural changes in the hip joint, such as the presence of osteoarthritis, that would affect clinical and MRI measures. To minimize the effect of TFL-ITB passiveness stiffness on ER0°, we abducted the hip 15°. To our knowledge, no evidence is available on the role of abducting the hip to measure ER ROM in prone versus neutral abduction positioning, however, we believe the abducted position would be more representative of the ROM associated with FV. Finally, one examiner performed all of the FVMRI measures and another examiner performed all of the clinical measures, therefore generalization to other examiners may be limited.
Conclusion
Identifying abnormal femoral version and understanding its effect on hip mobility may assist in individualizing exercise prescription and performance of functional tasks. Clinical tests, such as Craig’s test or hip rotation ROM, may be used to screen FV abnormalities. We used previously published normative data to propose criteria to define three categories of FVMRI, excessive anteversion, normal version, and retroversion. We confirmed that compared to those with normal FVMRI, those with excessive femoral anteversion demonstrate decreased hip ER ROM and those with femoral retroversion demonstrate decreased hip IR ROM. Although ROM difference values vary by hip position, a difference of 20° between hip IR ROM and ER ROM in either hip flexion or neutral hip flexion/extension would be suggestive of abnormal femoral version.
Highlights.
Hip rotation range of motion and Craig’s test may be used to screen for femoral version abnormalities
Femoral retroversion is associated with limited hip internal rotation
Excessive femoral anteversion is associated with limited hip external rotation
20° difference in hip internal and external rotation motion may suggest abnormal femoral version
Acknowledgements
The authors would like to acknowledge Darrah Snozek for her assistance with data collection.
Funding
This work was supported by the following grants: Harris-Hayes was supported by grant K23 HD067343 and K12 HD055931 from the National Center for Medical Rehabilitation Research, National Institute of Child Health and Human Development, and National Institute of Neurological Disorders and Stroke and grant UL1 RR 024992-01 from the National Center for Research Resources, components of the National Institutes of Health and NIH Roadmap for Medical Research. Additional support was provided by Program in Physical Therapy at Washington University School of Medicine, Clinical and Translational Science Award (CTSA) Grant [UL1 TR000448] and Siteman Comprehensive Cancer Center and NCI Cancer Center Support Grant P30 CA091842
Footnotes
Statement of Financial Disclosure and Conflict of Interest
I affirm that I have no financial affiliation (including research funding) or involvement with any commercial organization that has a direct financial interest in any matter included in this manuscript, except as disclosed in an attachment and cited in the manuscript. Any other conflict of interest (ie, personal associations or involvement as a director, officer, or expert witness) is also disclosed in an attachment.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abel MF, Sutherland DH, Wenger DR, Mubarak SJ. Evaluation of ct scans and 3-d reformatted images for quantitative assessment of the hip. J Pediatr Orthop. 1994;14:48–53. [DOI] [PubMed] [Google Scholar]
- Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66:228–241. [PubMed] [Google Scholar]
- Avila EM, Castro JV, Scaramussa K, Gomes JLE. Behavior of risk factors for acl injury in amateur soccer players. J Orth Rhe Sp Med. 2016;1:1–4. [Google Scholar]
- Beall DP, Martin HD, Mintz DN, Ly JQ, Costello RR, Braly BA, Yoosefian F. Anatomic and structural evaluation of the hip: A cross-sectional imaging technique combining anatomic and biomechanical evaluations. Clin Imaging. 2008;32:372–381. [DOI] [PubMed] [Google Scholar]
- Bedi A, Thompson M, Uliana C, Magennis E, Kelly BT. Assessment of range of motion and contact zones with commonly performed physical exam manoeuvers for femoroacetabular impingement (fai): What do these tests mean? Hip Int. 2013;23 Suppl 9:S27–34. [DOI] [PubMed] [Google Scholar]
- Botser IB, Ozoude GC, Martin DE, Siddiqi AJ, Kuppuswami S, Domb BG. Femoral anteversion in the hip: Comparison of measurement by computed tomography, magnetic resonance imaging, and physical examination. Arthroscopy. 2012;28:619–627. [DOI] [PubMed] [Google Scholar]
- Chung CY, Lee KM, Park MS, Lee SH, Choi IH, Cho TJ. Validity and reliability of measuring femoral anteversion and neck-shaft angle in patients with cerebral palsy. J Bone Joint Surg Am. 2010;92:1195–1205. [DOI] [PubMed] [Google Scholar]
- Cibulka MT. Determination and significance of femoral neck anteversion. [review] [51 refs]. Physical Therapy 84(6):550–8. 2004. [PubMed] [Google Scholar]
- Davids JR, Benfanti P, Blackhurst DW, Allen BL. Assessment of femoral anteversion in children with cerebral palsy: Accuracy of the trochanteric prominence angle test. JPediatrOrthop. 2002;22:173–178. [PubMed] [Google Scholar]
- Dobson F, Choi YM, Hall M, Hinman RS. Clinimetric properties of observer-assessed impairment tests used to evaluate hip and groin impairments: A systematic review. Arthritis Care Res (Hoboken). 2012;64:1565–1575. [DOI] [PubMed] [Google Scholar]
- Ejnisman L, Philippon MJ, Lertwanich P, Pennock AT, Herzog MM, Briggs KK, Ho CP. Relationship between femoral anteversion and findings in hips with femoroacetabular impingement. Orthopedics. 2013;36:e293–300. [DOI] [PubMed] [Google Scholar]
- Fabry G, MacEwen GD, Shands AR Jr., Torsion of the femur. A follow-up study in normal and abnormal conditions. J Bone Joint Surg Am 1973; 55:1726–1738. [PubMed] [Google Scholar]
- Gulan G, Matovinovic D, Nemec B, Rubinic D, Ravlic-Gulan J. Femoral neck anteversion: Values, development, measurement, common problems. Coll Antropol. 2000;24:521–527. [PubMed] [Google Scholar]
- Harris-Hayes M, Commean PK, Patterson JD, Clohisy JC, Hillen T. Bony abnormalities of the hip joint: A new comprehensive, reliable and radiation-free measurement method using magnetic resonance imaging. Journal of Hip Preservation Surgery. 2014;1:62–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris-Hayes M, Wendl PM, Sahrmann SA, an Dillen LR. Does stabilization of the tibiofemoral joint affect passive prone hip rotation range of motion measures in unimpaired individuals? A preliminary report. . Physiother Theory Pract. 2007;in press [DOI] [PubMed] [Google Scholar]
- Hernandez RJ, Tachdjian MO, Poznanski AK, Dias LS. Ct determination of femoral torsion. AJR Am J Roentgenol. 1981;137:97–101. [DOI] [PubMed] [Google Scholar]
- Holm I, Bolstad B, Lutken T, Ervik A, Rokkum M, Steen H. Reliability of goniometric measurements and visual estimates of hip rom in patients with osteoarthrosis. Physiother Res Int. 2000;5:241–248. [DOI] [PubMed] [Google Scholar]
- Ito K, Minka MA, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. A mri-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176. [DOI] [PubMed] [Google Scholar]
- Kendall FP, McCreary EK, Provance PG, Rodgers MM, Romani WA. (2005). Muscles: Testing and function with posture and pain (Vol. 5th). Baltimore: Lippincott Williams & Wilkins. [Google Scholar]
- Kim YJ, Bixby S, Mamisch TC, Clohisy JC, Carlisle JC. Imaging structural abnormalities in the hip joint: Instability and impingement as a cause of osteoarthritis. Seminars in Musculoskeletal Radiology. 2008;12:334–345. [DOI] [PubMed] [Google Scholar]
- Klassbo M, Larsson E, Mannevik E. Hip disability and osteoarthritis outcome score. An extension of the western ontario and mcmaster universities osteoarthritis index. Scandinavian Journal of Rheumatology 32(1):46–51. 2003. [DOI] [PubMed] [Google Scholar]
- Martin RL, Irrgang JJ, Sekiya JK. The diagnostic accuracy of a clinical examination in determining intra-articular hip pain for potential hip arthroscopy candidates. Arthroscopy. 2008;24:1013–1018. [DOI] [PubMed] [Google Scholar]
- Maslowski E, Sullivan W, Forster HJ, Gonzalez P, Kaufman M, Vidal A, Akuthota V. The diagnostic validity of hip provocation maneuvers to detect intra-articular hip pathology. Pm & R. 2010;2:174–181. [DOI] [PubMed] [Google Scholar]
- Mesgarzadeh M, Revesz G, Bonakdarpour A. Femoral neck torsion angle measurement by computed tomography. J Comput Assist Tomogr. 1987;11:799–803. [DOI] [PubMed] [Google Scholar]
- Nepple JJ, Riggs CN, Ross JR, Clohisy JC. Clinical presentation and disease characteristics of femoroacetabular impingement are sex-dependent. J Bone Joint Surg Am. 2014;96:1683–1689. [DOI] [PubMed] [Google Scholar]
- Nilsdotter AK, Lohmander LS, Klassbo M, Roos EM. Hip disability and osteoarthritis outcome score (hoos)--validity and responsiveness in total hip replacement. BMC MusculoskeletDisord. 2003;4:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratzlaff C, Simatovic J, Wong H, Li L, Ezzat A, Langford D, Esdaile JM, Kennedy C, Embley P, Caves D, Hopkins T, Cibere J. Reliability of hip examination tests for femoroacetabular impingement. Arthritis Care Res (Hoboken). 2013;65:1690–1696. [DOI] [PubMed] [Google Scholar]
- Reikeras O, Bjerkreim I, Kolbenstvedt A. Anteversion of the acetabulum and femoral neck in normals and in patients with osteoarthritis of the hip. Acta OrthopScand. 1983;54:18–23. [DOI] [PubMed] [Google Scholar]
- Ruwe PA, Gage JR, Ozonoff MB, DeLuca PA. Clinical determination of femoral anteversion. A comparison with established techniques. J Bone Joint Surg Am. 1992;74:820–830. [PubMed] [Google Scholar]
- Sangeux M, Mahy J, Graham HK. Do physical examination and ct-scan measures of femoral neck anteversion and tibial torsion relate to each other? Gait Posture. 2014;39:12–16. [DOI] [PubMed] [Google Scholar]
- Silveira PF, Piedade SR. Factors that influence in the turnout in ballet dancers with knee pain. Fisioter Pesqui. 2014;21:209–216. [Google Scholar]
- Souza RB, Powers CM. Concurrent criterion-related validity and reliability of a clinical test to measure femoral anteversion. J OrthopSports PhysTher. 2009;39:586–592. [DOI] [PubMed] [Google Scholar]
- Srimathi T, Muthukumar T, Anandarani VS, Umapathy S, Rameshkumar S. A study on femoral neck anteversion and its clinical correlation. J Clin Diagn Res. 2012;6:155–158. [Google Scholar]
- Staheli LT, Corbett M, Wyss C, King H. Lower-extremity rotational problems in children. Normal values to guide management. Journal of Bone & Joint Surgery - American Volume. 1985;67:39–47. [PubMed] [Google Scholar]
- Tomczak RJ, Guenther KP, Rieber A, Mergo P, Ros PR, Brambs HJ. Mr imaging measurement of the femoral antetorsional angle as a new technique: Comparison with ct in children and adults. AJR Am J Roentgenol. 1997;168:791–794. [DOI] [PubMed] [Google Scholar]
- Tonnis D, Heinecke A. Diminished femoral antetorsion syndrome: A cause of pain and osteoarthritis. J Pediatr Orthop. 1991;11:419–431. [DOI] [PubMed] [Google Scholar]
- Toogood PA, Skalak A, Cooperman DR. Proximal femoral anatomy in the normal human population. Clin Orthop Relat Res. 2009;467:876–885. [DOI] [PMC free article] [PubMed] [Google Scholar]