Abstract
Background/objective
High-intensity interval training (HIIT) can produce similar or improved results compare with traditional training, but the question as to whether HIIT can be used in the setting of physical education (PE) remains unanswered. The aim of this systematic review was to critically analyze the feasibility of incorporating HIIT programs into PE classes to improve the body compositions and cardiorespiratory fitness of overweight students.
Methods
We conducted database searches for literature dating between January 2012 and January 2017. Of the final six studies selected, three were conducted in children under 12 years old and three involved adolescents between 12 and 18 years old.
Results
The HIIT protocols consisted of 2–3 sessions per week, with intervals of 15 s and passive or active rests of 15 s, totaling up to 6 min of work with 4 min of rest. The duration of HIIT programs was 6–24 weeks. Significant changes were reported in body composition, body mass index, body fat (%), waist circumference, and sum of skinfolds; and increases in muscle mass were observed. The inclusion of HIIT programmes improved maximal oxygen uptake (VO2max), performance in the intermittent Yo-Yo test and maximal aerobic speed.
Conclusions
The HIIT programmes showed improvements in the variables studied, with interventions two or three times weekly. Therefore, they can be used in schools, as a strategy to combat the childhood obesity pandemic and HIIT can be use alongside with existing PE activities within the same lesson or in specific periods during day school.
Keywords: Children, High-intensity interval training, Physical fitness
Introduction
Childhood obesity is a complex condition that can drive many risk factors.1 It is characterized, among other factors, by an imbalance between food input and energy expenditure which results in an increase in body mass index (BMI).2 This pathology is a worldwide health problem, increasingly prevalent in child and adolescent populations, especially over the last few decades.3,4 This increase has been associated with a concomitant increase in various chronic illnesses such as metabolic syndrome, type 2 diabetes, cardiovascular disease, cancer, and arthritis as well as a higher probability of obesity and low cardiorespiratory capacity in adulthood.5,6 Cardiorespiratory capacity is a measurement of how the body functions and develops, and should, through training, play an important role in activities related to improving physical activity. This is a fundamental component of a healthy lifestyle for children and adolescents.5 Furthermore, high cardiorespiratory capacity is associated with lower cardiometabolic risk.6
Effective strategies for the prevention and treatment of childhood obesity require the involvement of the school environment. Modification of physical education (PE) curricula in schools have resulted in consistent changes in the quantity of physical activity and student motivation, with positive effects on quality of life and other biomarkers.7,9 Adequate exposure to PE effectively contributes to the development of a healthier lifestyle among children, which continues throughout their lifespan. However, many PE programs do not comply with recommendations in terms of class times and intensity (moderate-to-vigorous physical activity) due to time lost to management-related activities.8,9
To combat childhood obesity, a healthy diet and/or aerobic training are essential.10 Although continuous aerobic training is generally included in intervention programs, low volume high-intensity interval training (HIIT) can produce similar or improved responses compared with traditional continuous aerobic training, despite the short amount of time that HIIT requires.11
Alvarez et al. observed that following a HIIT program for a total of 18 sessions (three times per week) improved the insulin resistance levels (assessed by homeostatic model assessment of insulin resistance [HOMA-IR]) as well as the anthropometric, cardiovascular, and physical performance of insulin-resistant schoolchildren.12 A systematic review on children and adolescents reported that HIIT programs are a time-efficient tool for improving the biomarkers of cardiovascular disease.13 However, recommendations regarding the intensity, volume, frequency of the exercise, and rest intervals remain scarce which hinders the application of HIIT in the context of school PE classes. The question of whether HIIT could be used for the treatment and prevention of obesity in school-aged children, and the feasibility of applying HIIT in school PE programs, remain to be addressed. Therefore, the aim of this systematic review was to critically analyze the feasibility of including HIIT-based programs in PE classes to improve the body compositions and cardiorespiratory fitness of overweight and obese students.
Methods
Search strategy
This systematic review was carried out following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) recommendations.14 The following databases were used: Web of Science, Scopus, MEDLINE, SPORTDiscus and PUBMED. The keywords used in the search and their possible combinations were: obesity or overweight or obese and child or adolescents or children or teen and high-intensity interval training or high-intensity interval exercise or high-intensity intermittent exercise.
Inclusion criteria
The inclusion criteria were as follows: a) children and adolescents classified as overweight or obese between 6 and 19 years old exclusively, b) studies published between 31 January 2012 and 31 January 2017, c) studies that included anthropometric and cardiorespiratory capacity evaluations in pre- and post-intervention, d) studies in English published in peer-reviewed journals, and e) studies that used HIIT alone or combined with other methods.15,16
Studies where caloric restriction was applied, interventions that used pharmaceuticals, or those centered on programs aimed at adolescents with hormonal imbalances and eating disorders were excluded.
Quality assessment
Two reviewers (P.D. and D.J.) independently selected titles and abstracts of potential studies identified by the search strategy. Study quality was determined through the Evidential Physiotherapy (PEDro) database,17 with scores ranging from 0 to 11 points.
Results
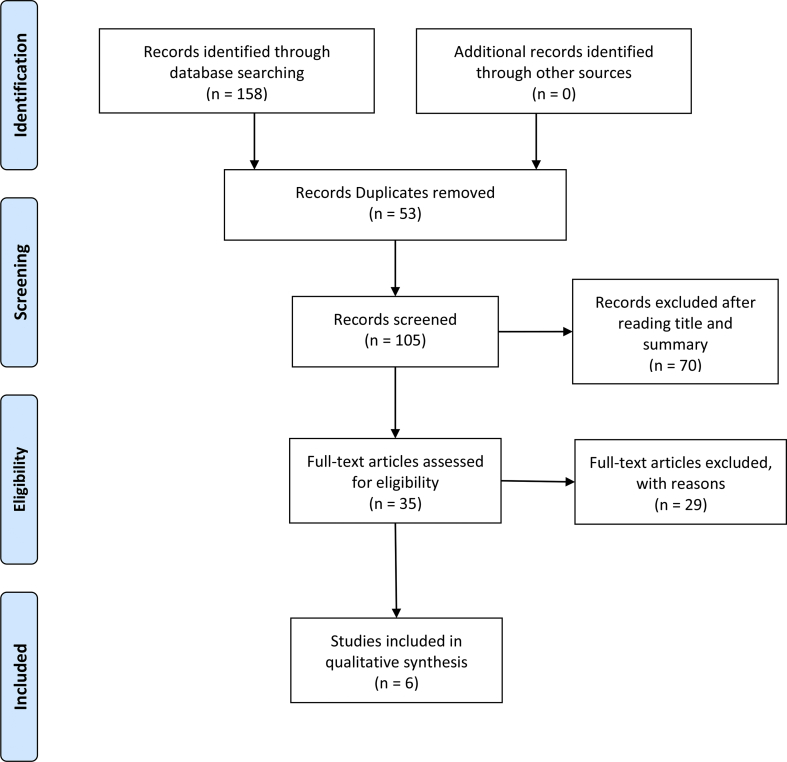
The search procedure identified 158 potential articles (Web of Science, n = 29; SCOPUS, n = 81; Medline, n = 14; SPORTDiscus, n = 10; PUBMED, n = 24). In the initial analysis, 53 publications were excluded due to duplication. Subsequently, 70 articles were excluded after reading the title and summary. The remaining 35 articles were read in full and six were selected as eligible after quality assessment18, 19, 20, 21, 22, 23 (Fig. 1).
Fig. 1.
Flowchart illustrating the different phases of the search and selection of studies.
High-intensity training modalities, outcome measures, and results of different interventions are presented in Table 1. Of the six studies selected, three were conducted in children under 12 years old18,22,23 and three focused on adolescents between 12 and 18 years old.19, 20, 21 The HIIT protocols consisted of 2–3 sessions per week, with working times of 15 s and passive or active rest periods of 15 s, totaling up to 6 min work with 4 min rest. The durations of the programs were 6–24 weeks. According to the studies included in this review, significant changes were reported in body composition Body mass index (BMI), BMI z-score, % body fat (%BF) and waist circumference (WC),19 in the sum of skinfolds,18 in body mass (BM), BMI, BF% and WC,21 and increase in muscle mass.23 HIIT programmes improved maximal oxygen uptake (VO2max),19,21, 22, 23 performance in the intermittent Yo-Yo test, maximal aerobic speed (MAS)18 and aerobic capacity.20
Table 1.
Results of studies examining the effects of HIIT on cardiorespiratory fitness and anthropometric parameters in obese children and adolescents (n = 6).
| Studies | Subject description | Study design | Training program | Outcomes | Result |
|---|---|---|---|---|---|
| Lau et al. (2014) | n = 15 Age: 11.0 ± 0.6 years BM: 51.1 ± 6.6 kg Size: 146.7 ± 5.2 cm |
Randomized clinical trial. HIIE, LIIE and CON |
HIIE = 12 sets x 15-s at 120% MAS followed by a 15- second passive recovery. Duration: 6 weeks, three times a week. |
BMI (kg/m2)
Skinfold thickness (mm) Sum of skinfolds (mm) YYIET (level one) |
↓ Sum of skinfolds (mm) ↑ YYIET distance covered (m) |
| Racil et al. (2016) | n = 17 Age: 14.2 ± 1.2 years. BM: 87.3 ± 4.5 kg Size: 164.0 ± 5.0 cm |
Randomized clinical trial. HIIT, MIIT and CON | HIIT = 3 sessions × 4–8 min (15 s/15 s)15-s at 100% MAS follow by 15 s recovery at 50% MAS. 3-min of inter-session passive recovery period. Duration: 12 weeks, three times a week. |
BM (kg) BMI–Z-score BF (%) WC (cm) VO2max (L·min−1) |
↓ BM (kg) ↓ BMI Z-score ↓ WC (cm) ↓ BF (%) ↑ VO2max (ml/kg/min) |
| Hay et al. (2015) | n = 38 Age: 15.3 ± 1.7 years BM:89.1 ± 15.7 kg Size: not reported |
Randomized clinical trial. HIIT, moderate-intensity and CON | HIIT = 70–85% HRres Duration: 6- month, three times a week. |
BM (kg) BMI (kg⋅m2) WC (cm), BF% trunk fat % VO2max (ml/kg/min) |
↑ VO2max (ml/kg/min) |
| Racil et al. (2015) | n = 23 Age: 16,6 ± 0,9 years BM: 83.9 ± 4.5 kg Size: 163 ± 5.0 cm |
Randomized clinical trial HIIT, P+HIIT and CON | HIIT = 6–8 blocks per session of 30-s runs at 100%MAS, with 30-s active recovery between bouts at 50%. Duration: 12 weeks, three times a week. |
BMI Z-score WC (cm) BF (%) LM (kg) VO2max (ml/kg/min). |
↓ BM (kg) ↓ BMI Z-score ↓WC (cm) ↓ BF (%) ↑ VO2max (ml/kg/min) |
| McNarry et al. (2015) | n = 15 Age: 9.3 ± 0.9 years BM: 49.1 ± 10.8 Kg Size: 143.3 ± 9.2 cm |
Randomized clinical trial EX and CON | EX = 6-min high- intensity exercise followed by 2 min of recovery (6 games per session) and a 4-min circuit. Duration: 6 weeks, two times a week |
BM (kg) BMI (kg⋅m2) VO2max (ml/kg/min). |
↑ VO2max (ml/kg/min) |
| Lambrick et al. (2015) | n = 28 Age: 9.3 ± 0.9 years BM 48.9 ± 11.0 kg Size: 143.3 ± 9.0 cm |
Randomized clinical trial EX and CON |
EX = 6-min high- intensity exercise followed by 2 min of recovery (6 games per session) and a 4-min circuit. Duration: 6 weeks, two times a week. |
BM (kg) BMI (kg⋅m2) WC(cm) BF(%) LM (kg) VO2max (ml/kg/min). |
↓ WC (cm) ↑LM (kg) ↑ VO2max (ml/kg/min). |
BM = body mass; BMI = body mass index; WC = waist circumference; BF = body fat; LM = lean mass; FFM = free fat mass; LIIE = low intensity intermittent exercise; HIIE = high intensity intermittent exercise; HIIT = high intensity interval training; MIIT = moderate-intensity interval training; CON = control group; AT = aerobic training; P = plyometric training; P+HIIT = plyometric exercise combined with HIIT; EX = exercise; YYIET= Yo-Yo intermittent endurance test; MAS = maximal aerobic speed; HRres = reserve heart rate; VO2max= maximal oxygen uptake; ↑; =Significant increase; ↓ = Significant reduction.
Quality assessment
Study quality for the seven selected articles using the PEDro scale. This returned a score of seven points out of a maximum of eleven (Table 2). The lost points were mainly due to: i) assignment concealment not being entirely relevant in studies of this nature, ii) difficulty in blinding the participants, as they are previously informed of the type of activity that will be undertaken, and iii) blinding the persons who apply the interventions (specifically, teachers) was not applicable.
Table 2.
Physiotherapy evidence database scale (PEDro).
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | Total Score | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lau et al. (2015) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Racilet al.(2016) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Hay et al. (2016) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Racilet al. (2015) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| McNarry et al. (2015) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Lambrick et al. (2015) | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
Notes: 0 = item was not satisfied; 1 = item was satisfied. Item 1: eligibility criteria were specified; Item 2: subjects were randomly allocated to groups; Item 3: allocation was concealed; Item 4: the groups were similar at baseline regarding the most important prognostic indicators; Item 5: there was blinding of all subjects; Item 6: there was blinding of all therapists who administered the therapy; Item 7: there was blinding of all assessors who measured at least one key outcome; Item 8: measurements of at least one key outcome were obtained from more than 85% of the subjects initially allocated to groups; Item 9: all subjects for whom outcome measurements were available received the treatment or control condition as allocated, or where this was not the case, data for at least one key outcome were analyzed by “intention to treat”; Item 10: the results of between groups statistical comparisons are reported for at least one key outcome; Item 11: the study provides bothpoint measurements and measurements of variability for at least one key outcome.
Discussion
The main findings of this review were: 1) HIIT programs resulted in improvements in body composition in less time than less-intense exercise, 2) HIIT programs resulted in improvements in cardiorespiratory fitness, and 3) the HIIT protocols are highly applicable to PE classes due to their short duration and adaptability to the school setting.
Body composition
This review revealed that HIIT resulted in significant changes in several parameters compared with control groups that performed other types of exercises or did not receive intervention. Racil et al.19 compared HIIT with moderate-intensity interval training (MIIT) and found that HIIT led to greater improvements on cardio-metabolic variables. Lau et al.18 observed a significant decrease in the sum of skinfolds of overweight children who followed HIIT programs in comparison with low-intensity (LI) interval exercises. In another investigation, Racil et al., compared HIIT programs with HIIT-plus-plyometric programs and reported that both approaches produced significant results (BMI, BF%, WC).21 Hay et al.,20 however, did not report any differences in adiposity measurements between groups who undertook HIIT and those who followed a moderate-intensity endurance training (ET) program. Lambrick et al.23 through high intensity discontinuous games found that the anthropometric parameters of obese children improved significantly compared with the control group. However, McNarry,22 who performed an intervention with similar characteristics to that of Lambrick et al.,23 reported no anthropometric variations.
In some studies, similar results were reported for body composition when comparing HIIT with ET, although the duration of HIIT sessions was 70% less than ET sessions.24 In another study, HIIT proved to be a more effective approach for weight loss in obese adolescents compared with ET.25 An intervention which employed different exercise methods reported that HIIT groups achieved greater increases in fat oxidation rates and greater decreases in BMI than the LI groups.26 Racil et al.27 observed a greater decrease in BF% in HIIT groups compared with MIIT groups. With regard to WC, the application of HIIT for obese adolescents resulted in a greater decrease than moderate exercise.28 Subjects of both HIIT and ET reported similar energy expenditures in the 24 h post-session,29 which could explain the similar results for body composition in some cases, despite the lower total volume of training and time commitment of HIIT.30 A further benefit of high-intensity compared with LI training for obesity and cardiovascular health is the improvement of parasympathetic tone and autonomic heart modulation in obese adolescents.31
Cardiorespiratory capacity
The HIIT programs included in this review improved VO2max,19,21, 22, 23 performance in the intermittent Yo-Yo test, MAS,18 and aerobic capacity.20 When comparing the results found in this review with previous studies, we found that 4 × 4 min interval exercises at 90% maximal heart rate (HR) generated significant improvements in VO2MAX after 3 months.32 Hottenrott et al.33 showed that HIIT exercise caused significantly greater improvements in VO2MAX than ET. According to a recent review, HIIT is a time-efficient tool for increasing cardiorespiratory fitness in adolescents.34
Araujo et al.24 found that the improvements in VO2max for continuous training at 80% peak HR for 30–60 min are similar to those achieved by HIIT through sprints. After following an 8 week HIIT program, performing four repetitions at 90–100% max HR for 20 s with 10 s rest periods, significant increases in VO2max of adolescents with low physical activity levels were observed.35 Gillen et al.36 reported that 12 weeks of HIIT with a total time of 10 min, resulted in similar improvements in VO2max when compared with 50 min sessions of aerobic training. Similar improvements were seen in systolic and diastolic heart functions following twice weekly HIIT sessions for 13 weeks in place of standard aerobic training.37 In addition, an intervention which compared HIIT with LI aerobic training for 6 months showed significant reductions in systolic and diastolic blood pressure of participants in both groups. However, beneficial changes in HR and HR variability were only observed in the HIIT group.31 It is important to consider that while aerobic training is beneficial, its application requires longer session times to achieve similar results to HIIT.
On the other hand, HIIT increase metabolic and cardiorespiratory stress. A single exercise session using a 4 × 4 min protocol at 90–95% peak power output causes increased VO2, average HR, ventilation, and ventilatory equivalent.38 These results are supported by a recent study conducted on 17 school-age children, which revealed increased VO2 following 12 intervals of 30 s at 90% max HR.39 Revised HIIT protocols can result in improved cardiorespiratory capacity, increased VO2max, and significantly decreased systolic and diastolic blood pressure. Maintaining optimal levels of these parameters plays a fundamental role in limiting the risk factors in overweight adolescents.
Limitations
The limitations of this systematic review are as follows: 1) the studies considered performed HIIT with different exercises (games, running, etc.) and combined with other training methods, making it difficult to generate a specific intervention protocol; 2) studies with caloric restrictions were not accepted, mainly because this is an uncontrollable variable for the application of these methodologies in overweight and obese school-age children; and 3) sex was not considered when analyzing results.
Conclusion and practical application
In conclusion, HIIT programs can result in improvements in body composition and cardiorespiratory capacity, as well as improvements in health markers. In addition, HIIT methods require less time than low-intensity activities, making them applicable for use in schools as a strategy to combat the childhood obesity pandemic. The incorporation of HIIT programs could be carried out alongside existing PE activities within the same lesson or in specific periods during the school day. The authors suggest that in order to guarantee HIIT effectiveness, programs should include 2–3 sessions per week, with intervals of 15–30 s and passive or active rest periods of 15–30 s. For higher volume programs, discontinuous games of up to 6 min work with 4 min rest periods for a total session time of 40 min can be used.
Despite this study highlights the importance and feasibility of HIIT methodology in a school setting, some questions need to be addressed. Future research should identify the optimal duration of HIIT sessions for improving physical, physiological and cognitive health in young children. Likewise, future studies should determine the optimal frequency within the school calendar for this type of programs.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
The author(s) have no conflicts of interest relevant to this article.
Author contributions
PDF revised the literature and wrote the manuscript; PLR and FGP critically reviewed the study; DJM and FCN reviewed the literature and helped write the study. All authors have read and approved the final version of this paper and agree with the order of its presentation.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jesf.2018.11.003.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Karnik S., Kanekar A. Childhood obesity: a global public health crisis. Int J Prev Med. Jan 2012;3(1):1–7. [PMC free article] [PubMed] [Google Scholar]
- 2.Swinburn B.A., Sacks G., Lo S.K. Estimating the changes in energy flux that characterize the rise in obesity prevalence. Am J Clin Nutr. Jun 2009;89(6):1723–1728. doi: 10.3945/ajcn.2008.27061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lob-Corzilius T. Overweight and obesity in childhood--a special challenge for public health. Int J Hyg Environ Health. Oct 2007;210(5):585–589. doi: 10.1016/j.ijheh.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 4.Kosti R.I., Panagiotakos D.B. The epidemic of obesity in children and adolescents in the world. Cent Eur J Publ Health. Dec 2006;14(4):151–159. doi: 10.21101/cejph.a3398. [DOI] [PubMed] [Google Scholar]
- 5.Jankowski M., Niedzielska A., Brzezinski M., Drabik J. Cardiorespiratory fitness in children: a simple screening test for population studies. Pediatr Cardiol. Jan 2015;36(1):27–32. doi: 10.1007/s00246-014-0960-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diez-Fernandez A., Sanchez-Lopez M., Mora-Rodriguez R., Notario-Pacheco B., Torrijos-Nino C., Martinez-Vizcaino V. Obesity as a mediator of the influence of cardiorespiratory fitness on cardiometabolic risk: a mediation analysis. Diabetes Care. 2014;37(3):855–862. doi: 10.2337/dc13-0416. [DOI] [PubMed] [Google Scholar]
- 7.Carrel A.L., Clark R.R., Peterson S.E., Nemeth B.A., Sullivan J., Allen D.B. Improvement of fitness, body composition, and insulin sensitivity in overweight children in a school-based exercise program: a randomized, controlled study. Arch Pediatr Adolesc Med. Oct 2005;159(10):963–968. doi: 10.1001/archpedi.159.10.963. [DOI] [PubMed] [Google Scholar]
- 8.Hollis J.L., Williams A.J., Sutherland R. A systematic review and meta-analysis of moderate-to-vigorous physical activity levels in elementary school physical education lessons. Prev Med. May 2016;86:34–54. doi: 10.1016/j.ypmed.2015.11.018. [DOI] [PubMed] [Google Scholar]
- 9.Bevans K.B., Fitzpatrick L.A., Sanchez B.M., Riley A.W., Forrest C. Physical education resources, class management, and student physical activity levels: a structure-process-outcome approach to evaluating physical education effectiveness. J Sch Health. Dec 2010;80(12):573–580. doi: 10.1111/j.1746-1561.2010.00544.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kelishadi R., Azizi-Soleiman F. Controlling childhood obesity: a systematic review on strategies and challenges. J Res Med Sci : Offic J Isfahan Univ Med Sci. Oct 2014;19(10):993–1008. [PMC free article] [PubMed] [Google Scholar]
- 11.Thivel D., Masurier J., Baquet G. High-intensity interval training in overweight and obese children and adolescents: systematic review and meta-analysis. J Sports Med Phys Fit. Mar 27 2018 doi: 10.23736/S0022-4707.18.08075-1. [DOI] [PubMed] [Google Scholar]
- 12.Alvarez C., Ramirez-Campillo R., Ramirez-Velez R., Izquierdo M. Effects of 6-weeks high-intensity interval training in schoolchildren with insulin resistance: influence of biological maturation on metabolic, body composition, cardiovascular and performance non-responses. Front Physiol. 2017;8:444. doi: 10.3389/fphys.2017.00444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eddolls W.T.B., McNarry M.A., Stratton G., Winn C.O.N., Mackintosh K.A. High-intensity interval training interventions in children and adolescents: a systematic review. Sports Med. Jun 22 2017:1–12. doi: 10.1007/s40279-017-0753-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hutton B., Catala-Lopez F., Moher D. The PRISMA statement extension for systematic reviews incorporating network meta-analysis: PRISMA-NMA. Med Clínica. Sep 16 2016;147(6):262–266. doi: 10.1016/j.medcli.2016.02.025. [DOI] [PubMed] [Google Scholar]
- 15.Gibala M.J., Little J.P., Macdonald M.J., Hawley J.A. Physiological adaptations to low-volume, high-intensity interval training in health and disease. J Physiol. Mar 01 2012;590(5):1077–1084. doi: 10.1113/jphysiol.2011.224725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Buchheit M., Laursen P.B. High-intensity interval training, solutions to the programming puzzle. Sports Med. 2013;43(5):313–338. doi: 10.1007/s40279-013-0029-x. [DOI] [PubMed] [Google Scholar]
- 17.Sherrington C., Herbert R.D., Maher C.G., Moseley A.M., PEDro A database of randomized trials and systematic reviews in physiotherapy. Man Ther. Nov 2000;5(4):223–226. doi: 10.1054/math.2000.0372. [DOI] [PubMed] [Google Scholar]
- 18.Lau P.W., Wong del P., Ngo J.K., Liang Y., Kim C.G., Kim H.S. Effects of high-intensity intermittent running exercise in overweight children. Eur J Sport Sci. 2015;15(2):182–190. doi: 10.1080/17461391.2014.933880. [DOI] [PubMed] [Google Scholar]
- 19.Racil G., Coquart J.B., Elmontassar W. Greater effects of high- compared with moderate-intensity interval training on cardio-metabolic variables, blood leptin concentration and ratings of perceived exertion in obese adolescent females. Biol Sport. Jun 2016;33(2):145–152. doi: 10.5604/20831862.1198633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hay J., Wittmeier K., MacIntosh A. Physical activity intensity and type 2 diabetes risk in overweight youth: a randomized trial. Int J Obes. Apr 2016;40(4):607–614. doi: 10.1038/ijo.2015.241. [DOI] [PubMed] [Google Scholar]
- 21.Racil G., Zouhal H., Elmontassar W. Plyometric exercise combined with high-intensity interval training improves metabolic abnormalities in young obese females more so than interval training alone. Appl Physiol Nutr Metabol. 2015;41(1):103–109. doi: 10.1139/apnm-2015-0384. [DOI] [PubMed] [Google Scholar]
- 22.McNarry M.A., Lambrick D., Westrupp N., Faulkner J. The influence of a six-week, high-intensity games intervention on the pulmonary oxygen uptake kinetics in prepubertal obese and normal-weight children. Appl Physiol Nutr Metabol. 2015;40(10):1012–1018. doi: 10.1139/apnm-2015-0051. [DOI] [PubMed] [Google Scholar]
- 23.Lambrick D., Westrupp N., Kaufmann S., Stoner L., Faulkner J. The effectiveness of a high-intensity games intervention on improving indices of health in young children. J Sports Sci. 2016/02/01 2016;34(3):190–198. doi: 10.1080/02640414.2015.1048521. [DOI] [PubMed] [Google Scholar]
- 24.Corte de Araujo A.C., Roschel H., Picanco A.R. Similar health benefits of endurance and high-intensity interval training in obese children. PLoS One. 2012;7(8) doi: 10.1371/journal.pone.0042747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kargarfard M., Lam E.T., Shariat A. Effects of endurance and high intensity training on ICAM-1 and VCAM-1 levels and arterial pressure in obese and normal weight adolescents. Phys Sportsmed. Sep 2016;44(3):208–216. doi: 10.1080/00913847.2016.1200442. [DOI] [PubMed] [Google Scholar]
- 26.Lazzer S., Tringali G., Caccavale M., De Micheli R., Abbruzzese L., Sartorio A. Effects of high-intensity interval training on physical capacities and substrate oxidation rate in obese adolescents. J Endocrinol Invest. Feb 2017;40(2):217–226. doi: 10.1007/s40618-016-0551-4. [DOI] [PubMed] [Google Scholar]
- 27.Racil G., Ben Ounis O., Hammouda O. Effects of high vs. moderate exercise intensity during interval training on lipids and adiponectin levels in obese young females. Eur J Appl Physiol. Oct 2013;113(10):2531–2540. doi: 10.1007/s00421-013-2689-5. [DOI] [PubMed] [Google Scholar]
- 28.Starkoff B.E., Eneli I.U., Bonny A.E., Hoffman R.P., Devor S.T. Estimated aerobic capacity changes in adolescents with obesity following high intensity interval exercise. Appl Physiol Nutr Metab. 2014;2(3):1. [Google Scholar]
- 29.Francois M.E., Graham M.J., Parr E.B. Similar metabolic response to lower-versus upper-body interval exercise or endurance exercise. Metabolism. 2017;68:1–10. doi: 10.1016/j.metabol.2016.11.009. [DOI] [PubMed] [Google Scholar]
- 30.Skelly L.E., Andrews P.C., Gillen J.B., Martin B.J., Percival M.E., Gibala M.J. High-intensity interval exercise induces 24-h energy expenditure similar to traditional endurance exercise despite reduced time commitment. Appl Physiol Nutr Metab. Jul 2014;39(7):845–848. doi: 10.1139/apnm-2013-0562. [DOI] [PubMed] [Google Scholar]
- 31.Farah B., Ritti-Dias R., Balagopal P., Hill J., Prado W. Does exercise intensity affect blood pressure and heart rate in obese adolescents? A 6-month multidisciplinary randomized intervention study. Pediatr Obes. 2014;9(2):111–120. doi: 10.1111/j.2047-6310.2012.00145.x. [DOI] [PubMed] [Google Scholar]
- 32.Tjønna A.E., Stølen T.O., Bye A. Aerobic interval training reduces cardiovascular risk factors more than a multitreatment approach in overweight adolescents. Clin Sci. 2009;116(4):317–326. doi: 10.1042/CS20080249. [DOI] [PubMed] [Google Scholar]
- 33.Hottenrott K., Ludyga S., Schulze S. Effects of high intensity training and continuous endurance training on aerobic capacity and body composition in recreationally active runners. J Sports Sci Med. 2012;11(3):483–488. [PMC free article] [PubMed] [Google Scholar]
- 34.Costigan S.A., Eather N., Plotnikoff R.C., Taaffe D.R., Lubans D.R. High-intensity interval training for improving health-related fitness in adolescents: a systematic review and meta-analysis. Br J Sports Med. Oct 2015;49(19):1253–1261. doi: 10.1136/bjsports-2014-094490. [DOI] [PubMed] [Google Scholar]
- 35.Logan G.R., Harris N., Duncan S., Plank L.D., Merien F., Schofield G. Low-active male adolescents: a dose response to high-intensity interval training. Med Sci Sports Exerc. Mar 2016;48(3):481–490. doi: 10.1249/MSS.0000000000000799. [DOI] [PubMed] [Google Scholar]
- 36.Gillen J.B., Martin B.J., MacInnis M.J., Skelly L.E., Tarnopolsky M.A., Gibala M.J. Twelve weeks of sprint interval training improves indices of cardiometabolic health similar to traditional endurance training despite a five-fold lower exercise volume and time commitment. PLoS One. 2016;11(4) doi: 10.1371/journal.pone.0154075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ingul C.B., Tjonna A.E., Stolen T.O., Stoylen A., Wisloff U. Impaired cardiac function among obese adolescents: effect of aerobic interval training. Arch Pediatr Adolesc Med. 2010;164(9):852–859. doi: 10.1001/archpediatrics.2010.158. [DOI] [PubMed] [Google Scholar]
- 38.Kilian Y., Engel F., Wahl P., Achtzehn S., Sperlich B., Mester J. Markers of biological stress in response to a single session of high-intensity interval training and high-volume training in young athletes. Eur J Appl Physiol. Dec 2016;116(11-12):2177–2186. doi: 10.1007/s00421-016-3467-y. [DOI] [PubMed] [Google Scholar]
- 39.Harris N.K., Dulson D.K., Logan G.R.M., Warbrick I.B., Merien F.L.R., Lubans D.R. Acute responses to resistance and high-intensity interval training in early adolescents. J Strength Cond Res. May 2017;31(5):1177–1186. doi: 10.1519/JSC.0000000000001590. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.