Abstract
Type I diabetes (T1D) is a rapidly increasing autoimmune disease especially in the Western countries and poses a serious global health problem. Incidence of T1D cannot be fully explained by genetic background, and environmental factors have been assumed to play a role. Environmental conditions and composition of human microbiome have been found to correlate with the incidence of T1D. We asked whether mothers’ prevalent vaginal microbiome could correlate with the incidence of T1D in child. To test this hypothesis, we collected samples of vaginal microbiomes from eight mothers that had at least one child with T1D (child age maximum of 11 years at the time of sampling), born with a vaginal delivery. Eight control mothers had child/children with vaginal delivery and no diabetic child/children. The microbiomes were studied by using 16S rRNA Ion Torrent high throughput sequencing. We found that composition of total and Lactobacillus microbiome was altered, and saw an indication that diversity of vaginal microbiomes of the mothers with a diabetic child could be higher. Based on these pilot observations, we strongly encourage a larger population study to verify whether mother vaginal microbiome diversity and composition are linked to the prevalence of T1D in children.
Introduction
Type I diabetes (T1D) is one of the most common pediatric chronic diseases1. The incidence of T1D has been increasing drastically especially in the population of the Western countries during the past decades2–4 and this increase has been most dramatic among the children of 0–4 years of age2,4. Globally, there is a high geographical variation in the incidence of T1D; the highest increase rates being reported in Europe1. Finland and Sardinia have the highest incidence of T1D, annually about 60 and 40 cases per 100 000 people, respectively3. Although very recent reports from Nordic countries indicate that the accelerating increase of T1D may be levelling off5–7, the incidence of T1D is still quite high in these countries4,6. The role of enterovirus infections preceding T1D has especially gained attention8, and a vaccination has been developed being in a testing phase at present9.
The genetic determination behind T1D is polygenic with at least 40 loci to date known to affect10. However, all genetically susceptible individuals do not get T1D as e.g. in Finland 20% of the population bears the susceptible HLA-mediated genes but only 1–2% will get T1D11. As all genetically susceptible individuals do not get T1D, the environmental factors therefore should play a role4,12–14. Several factors such as diet15, hygienic conditions16–18, vitamin D level19, enterovirus infections8 and gut microbiome20,21 have been found to correlate with autoimmunity and incidence of T1D. In particular, much attention has been paid to the alterations in gut microbiome as a potential factor in the predisposition of T1D4.
Human microbiome is primarily determined at the birth22 but changes in its composition also occur later in life23–25. The mode of delivery affects the microbiome of the neonate, i.e., children born via cesarean section have different microbial profiles than vaginally delivered ones26–28. Skin and vaginal bacterial communities are known to be dominated by different phyla26,29–32. Children born by cesarean section have been reported to have a 20% higher risk to get T1D33.
Healthy vaginal microbiome of a single individual, has been found to be inhabited by at least 30 bacterial groups, dominated by Lactobacilli; also including pathogenic bacterial groups in low numbers34–37. Communities may be highly individual36,37. The vaginal microbiome is considered to be relatively stable and resilient during the reproductive age until the menarche36,37, but temporal variation related to menstrual cycle, sexual activity and original bacterial community composition has been described37–39.
As the vaginal microbiome of the mother (i) may correlate with the microbiome of vaginally delivered neonates22, (ii) the mode of delivery is correlated with the child microbiome26,27 and (iii) because the child gut microbiome has been found to be altered in the progression of T1D4, we asked whether there would be systematic differences in the prevalent vaginal microbial communities between mothers with and without a T1D child/children. To investigate this hypothesis, we studied vaginal microbiomes from a pilot group of mothers in Northern Finland, Oulu area, by using 16S rRNA Ion Torrent sequencing. Specific attention was paid to Lactobacillus community.
Results and Discussion
The total number of sequence reads was 251 431, and the average number per sample was 7857 ± 807.1 SD. For the subsequent analyses, the sequences were rarified into the lowest number of reads per sample (4341 reads). The reads were clustered into 185 operational taxonomic units (OTUs), representing seven identified phyla and 73 identified genera.
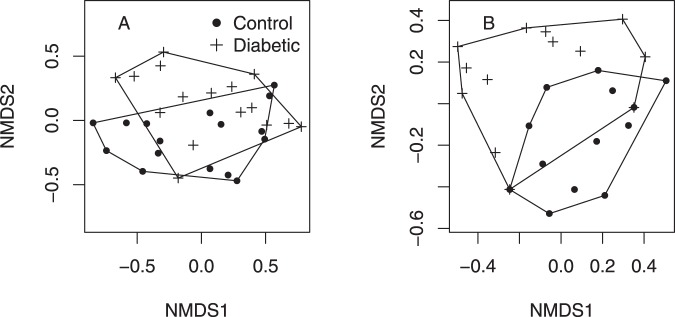
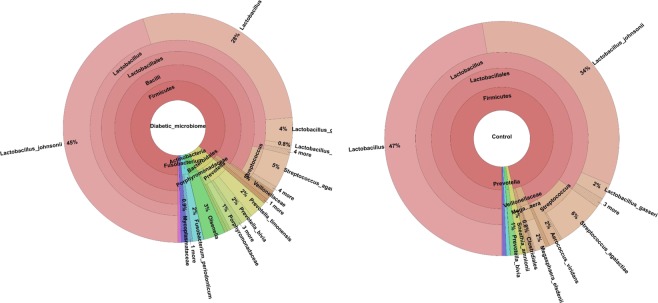
There was no difference in the total relative abundance of OTUs (Supplementary Information 1, 2 and 3), but there was an indication that the microbiome diversity may have been increased in the group of T1D mothers suggested by marginally significant Simpson diversity index (Fig. 1, F(1,14) = 4.36 , P = 0.055). Chao1 and Shannon indices did not suggest differences between groups (Supplementary Information 2). The composition of microbiomes was altered (presence/absence data, PERMANOVA F(1,30) = 2.02, P = 0.049, Figs 2A and 3). Lactobacilli were the most common OTUs in both studied groups (Supplementary Information 4), and the composition of Lactobacillus community was found to be altered (presence-absence data, PERMANOVA F(1,30) = 10.0, P < 0.001, Figs 2B and 3) between groups.
Figure 1.
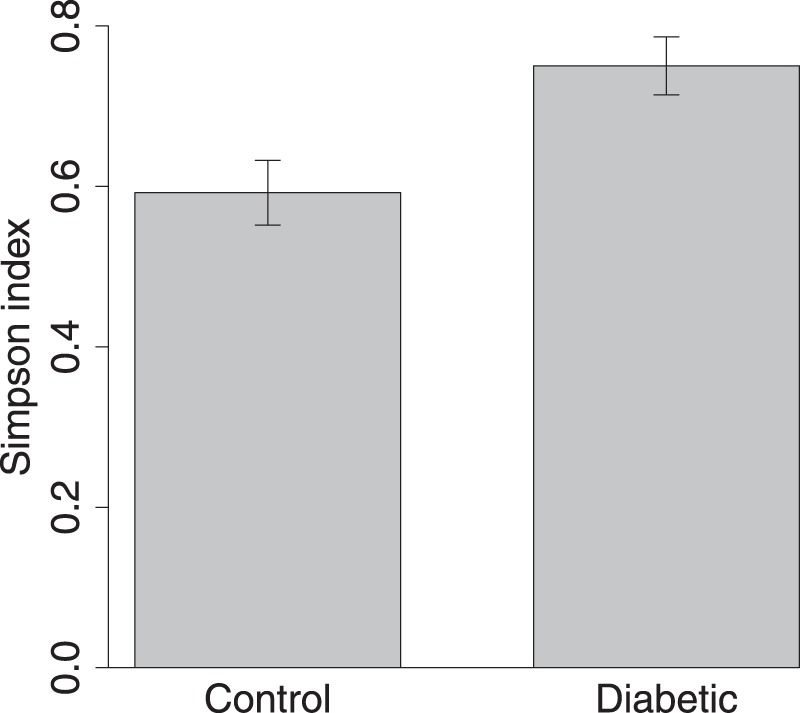
Vaginal microbiome Simpson’s diversity index (±SE). Control = in mothers without T1D child and Diabetic = in mothers with one or more child/children with T1D. F(1,14) = 4.36, P = 0.055. N = 8.
Figure 2.
NMDS ordination of the microbiomes of control and diabetic samples based on presence/absence data. (A) All OTUs, PERMANOVA F(1,30) = 2.02, P = 0.049. (B) Lactobacillus-OTUs. PERMANOVA F(1,30) = 10.0, P < 0.001. N = 8 (16 microbiomes in the figure are based on swab type duplicates. Swab type was used as a random factor in the analysis).
Figure 3.
Microbiomes of mothers of diabetic and control groups visualized at different taxonomic levels. N = 8.
To our knowledge, this is the first comparison of vaginal microbiomes between mothers with a diabetic child versus mothers without diabetic child. Although the sample size is low (N = 8), we were able to find an indication that the prevalent vaginal microbiome of mothers with a T1D child may have higher OTU diversity than the vaginal microbiome of the control mothers and we found that the composition of microbiomes was different. Potential changes in diversity of T1D mother vaginal microbiomes were linked with alteration in the community of the dominant bacterial genus Lactobacillus37. Different Lactobacillus community, and decreased dominance of Lactobacillus in the vaginal bacterial flora may be linked to the more diverse microbial community in T1D mothers. In the gut microbiota, especially L. johnsonii abundance has been found to correlate negatively with the incidence of diabetes in a rat model40,41. De Goffau et al. reported increased microbial diversity in the gut of diabetic children (over 2.9 years) compared to non-diabetic children42, although it is known that in the late progression phase of T1D in humans, the gut microbiome becomes more monotonous4. The amount of Lactobacilli in the vagina is related to production of lactic acid and vaginal pH37,39,43,44.
The vaginal microbiome is considered being relatively stable and resilient during the reproductive age until the menarche37. However, temporal variation related to menstrual cycle, sexual activity and gestation have been found37,39,44. Therefore, factors such as mother age, age at birth of child/children, stage of menstrual cycle and information about the sexual activity should be controlled in the future studies. In contrast to earlier studies (e.g. Cho & Blaser)22, Drell et al. recently found that vaginal microbiome of the mother and the child microbiome (e.g. child gut microbiome) do not correlate with each other although they share same bacterial taxa31. There may thus also be other than microbiome-related mechanisms between increased risk of the child to get T1D than mother vaginal microbiome.
In addition, characteristic bacterial groups in the microbiomes of the mothers with a T1D child/children were Actinobacteria, Fusobacteria and Prevotella. Prevotella has been found common in the vaginal microbiome in women who have other than Lactobacillus-dominated microbiome36. Although other than Lactobacillus-dominated vaginal microbiomes are less common, they are considered as normal, i.e. healthy vaginal microbiomes44.
Our results, based on a small pilot study, suggest that vaginal microbiome of T1D mothers may differ from the mothers without a T1D child several years after delivery. They also provide material to develop a hypothesis that mother’s vaginal microbiome plays a role in the incidence of a T1D breakout in children and this may be related to increased microbial diversity in the vagina. More detailed research on the potential connection between the mother vaginal microbiome and the child T1D is therefore of major importance. We also suggest that vaginal seeding of neonates born by cesarean section45 should be applied with caution until we know whether a vaginal microbiome could pose a health risk related to T1D or other more common disease46. We emphasize that our results should be treated as indicative, and they need to be verified by a more extensive population study; especially with a more thorough background information collected from the study units (mothers), the age of child/children, and antibiotic treatments controlled.
Methods
The material for this study was collected in the OYS hospital June 16 2014 - June 15 2015. Institutional committee of Pohjois-Pohjanmaan sairaanhoitopiirin kuntayhtymä approved the study and the patient consent (Statement of the regional Ethics committee February 18, 2012). All research was performed in accordance with relevant regulations, and informed consent was obtained from all participants. The material for the study was collected from 8 mothers with at least one T1D child by vaginal delivery (child age less than 11 years at the time of sampling and the child being diagnosed with diabetes at the age of 0–4 y old) and from 8 control mothers with at least one vaginal delivery and no diagnosed diabetic child/children. The age of the mothers was set to be between 22–40 years at the time of sampling. The samples were collected during in Oulu area, Northern Finland. No other background information on the mothers was collected.
As the type of the swab could affect the quality of the DNA, the samples were collected by using both Dacron (EnviroTrans) and cotton swabs (Constix) in a normal protocol of vaginal surface sampling. After sampling, the tip of the swab was immediately placed into a sterile Eppendorf tube and preserved at −80 °C.
DNA extraction and amplification of bacterial rRNA genes
DNA was extracted from the dacron and cotton swabs using the Qiagen DNeasy Blood and Tissue kit (Qiagen, USA) according to manufacturer’s protocol and stored at −20 °C until used. The DNA was quantified using a Nanodrop spectrophotometer. Bacterial primers F519 (5-CAGCMGCCGCGGTAATWC-3) and R926 (5-CCGTCAATTCCTTTRAGTTT-3) were used to amplify the V4-V5 region of 16S small-subunit ribosomal gene. The F519 primer contained an Ion Torrent pyrosequencing adapter sequence A (Lifescience Technologies, USA), a 9-bp unique barcode sequence and one nucleotide linker, while the R926 primer contained an Ion Torrent adapter trP1 sequence. Triplicate PCR reactions were performed, each containing 1x Phusion GC buffer, 0.4 µM of the forward and reverse primers, 200 µM dNTPs, 0.5 U of Phusion enzyme (Finnzymes, Finland) and 10 ng of genomic community DNA as the template, together with molecular-grade water in a total reaction volume of 20 µl. The cycling conditions were 30 cycles at 98 °C for 10 s, 64 °C for 30 sec and 72 °C for 20 sec after an initial denaturation at 98 °C for 3 min. The triplicate pooled PCR amplified reactions were purified using the AMPure XP PCR clean-up kit (Agencourt Bioscience, CA, USA) and the DNA concentration was measured on a Bioanalyzer DNA chip (Agilent Technologies, CA, USA). Individual samples were pooled in an equivalent amount, size selected using BluePippin automated electrophoresis system (Sage Science, MA, USA) on 1.5% agarose gel, twice purified with AMPure XP kit, final DNA concentration was measured using Bioanalyzer DNA chip and sequenced on a 316 v2 chip using Ion Torrent 400 bp chemistry (Life Technologies, USA) using to 15 pM sample concentration.
Bioinformatics analysis
The hypervariable regions V4-V5 of the 16S rRNA gene were sequenced using Ion Torrent to characterize the microbiomes of the vaginal samples. The Ion Torrent sequences were processed and analyzed with QIIME using state-of-the-art procedures47. Briefly, the sequences were binned according to sample-specific barcodes using the QIIME split_libraries.py tool, after which the barcode and primer sequences were trimmed and filtered for quality using the default parameters. Chimeric sequences were removed with the Usearch quality-filtering tool in QIIME using the rRNA16S.gold.fasta reference database. The final dataset consisted of 251 431 reads from 4 × 8 (32) samples after filtering out low-quality and chimeric readings, with a median of 7,612 reads per sample. The sequences were clustered into operational taxonomic units (OTUs) employing a similarity threshold of 97% in an RDP Naive Bayesian Classifier. The OTUs represent taxonomic units based on differences between sequences of bacterial DNA data. The total number of OTUs serves as an estimate of the total number of bacterial species in the sample but is not an exact equivalent of the number of different microbiological species. The phylogenetic trees were constructed from NAST-trimmed aligned sequences in FastTree248. The OTU table was constructed using the Biom formatted table in QIIME v1.9 and all the samples were rarefied to 4300 sequences prior the OTU-based analysis, as it was the lowest number of readings observed in the community. Taxonomy was assigned using gut-specific microbiome HITdb49. We have deposited the raw Ion Torrent data in NCBI-SRA with the accession number SRP132770. Chao1, Shannon and Simpson indices were used to estimate the diversity of the microbiome. Data is available from the corresponding author on request.
Statistical analysis
Before analyses, the sequences were rarified to the lowest number of sequences in a sample in QIIME. Because there were no differences between cotton and dacron swabs (Supplementary Information 2), these data were later combined in the analysis. Statistical analysis was conducted using a linear mixed effects model with the total OTU relative abundance, Chao1, Simpson and Shannon diversity indices as the dependent variables, and the mother group (control or with a T1D child) as an explanatory factor. The swab type was used as a random factor in the analyses and mother was used as an additional random factor (by nesting swab within mother) for OTU relative abundance and diversity indices. We carried out non-metric multidimensional scaling (NMDS) and the statistical test by PERMANOVA (functions metaMDS and adonis is package vegan 2.3.550) analysis for the bacterial communities, both for relative abundance and presence/absence data. The fit of the statistical models was confirmed by using diagnostic plots51 and suitable transformation/s were carried out for the dependent variable when appropriate. The analyses were conducted in R-environment, v. 3.152.
Supplementary information
Acknowledgements
The authors thank the volunteers providing samples for this study. The project was funded by Academy of Finland (project #138309 to AM) and K59780 (to A.T.-M.).
Author Contributions
All authors planned the sampling, A.T.-M. carried out sampling, M.V.T. carried out the laboratory work. and analysis, all authors contributed to writing.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-37467-w.
References
- 1.Dabelea D. The accelerating epidemic of childhood diabetes. Lancet. 2009;373:1999–2000. doi: 10.1016/S0140-6736(09)60874-6. [DOI] [PubMed] [Google Scholar]
- 2.Harjutsalo V, Sjöberg L, Tuomilehto J. Time trends in the incidence of type 1 diabetes in Finnish children: a cohort study. Lancet. 2008;371:1777–1782. doi: 10.1016/S0140-6736(08)60765-5. [DOI] [PubMed] [Google Scholar]
- 3.Atkinson MA, Eisenbarth GS, Michels AW. Type I diabetes. Lancet. 2014;383:69–82. doi: 10.1016/S0140-6736(13)60591-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knip M, Siljander H. The role of the intestinal microbiota in type 1 diabetes mellitus. Nat. Rev. Endocrinol. 2016;12:154–167. doi: 10.1038/nrendo.2015.218. [DOI] [PubMed] [Google Scholar]
- 5.Berhan Y, Waernbaum I, Lind T, Mollsten A, Dahlquist G. Thirty years of prospective nationwide incidence of childhood type I diabetes: the accelerating increase by time trends to level off in Sweden. Diabetes. 2011;60:577–581. doi: 10.2337/db10-0813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harjutsalo V, Sund R, Knip M, Groop PH. Incidence of type I diabetes in Finland. JAMA. 2013;310:427–428. doi: 10.1001/jama.2013.8399. [DOI] [PubMed] [Google Scholar]
- 7.Skrivarhaug T, et al. Incidence of type I diabetes in Norway among children aged 0-14 years between 1989 and 2012: has the incidence stopped rising? Results from Norwegian Childhood Diabetes Registry. Diabetologia. 2014;57:57–62. doi: 10.1007/s00125-013-3090-y. [DOI] [PubMed] [Google Scholar]
- 8.Yeung, W. C., Rawlinson, W. D. & Craig, M. E. Enterovirus infection and type 1 diabetes mellitus; systematic review and meta-analysis of observational molecular studies. BMJ. d342–d35 (2011). [DOI] [PMC free article] [PubMed]
- 9.Hyöty H, Knip M. Developing a vaccine for Type 1 diabetes through targeting enteroviral infections. Expert Rev. Vaccines. 2014;13:989–999. doi: 10.1586/14760584.2014.933078. [DOI] [PubMed] [Google Scholar]
- 10.Concannon P, Rich SS, Nepom GT. Genetics of type 1A diabetes. N. Engl. J. Med. 2009;360:1646–1654. doi: 10.1056/NEJMra0808284. [DOI] [PubMed] [Google Scholar]
- 11.Knip M. Environmental triggers and determinants of beta-cell autoimmunity in type 1 diabetes. Rev. Endocr. Metab. Disord. 2003;4:213–223. doi: 10.1023/A:1025121510678. [DOI] [PubMed] [Google Scholar]
- 12.Hermann R, et al. Temporal changes in the frequencies of HLA genotypes in patients with type 1 diabetes – indication of an increased environmental pressure? Diabetologia. 2003;46:420–425. doi: 10.1007/s00125-003-1045-4. [DOI] [PubMed] [Google Scholar]
- 13.Knip. M, Simell O. Environmental triggers of type 1diabetes. Cold Spring Harb. Perspect. Med. 2012;2:a007690. doi: 10.1101/cshperspect.a007690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paun A, Yau C, Danska JS. The influence of the microbiome on type I diabetes. J. Immunol. 2017;198:590–595. doi: 10.4049/jimmunol.1601519. [DOI] [PubMed] [Google Scholar]
- 15.Virtanen SM. Dietary factors in the development of type 1 diabetes. Pediatr. Diabetes. 2016;17(Suppl 22):49–55. doi: 10.1111/pedi.12341. [DOI] [PubMed] [Google Scholar]
- 16.Kondrashova A, et al. A six-fold gradient in the incidence of type 1 diabetes at the eastern border of Finland. Annals of Medicine. 2005;37:67–72. doi: 10.1080/07853890410018952. [DOI] [PubMed] [Google Scholar]
- 17.Kondrashova A, et al. Signs of β-cell autoimmunity in nondiabetic schoolchildren. Diabetes Care. 2007;30:95–100. doi: 10.2337/dc06-0711. [DOI] [PubMed] [Google Scholar]
- 18.Kondrashova A, et al. The’Hygiene hypothesis’ and the sharp gradient in the incidence of autoimmune and allergic diseases between Russian Carelia and Finland. APMIS. 2013;21:478–493. doi: 10.1111/apm.12023. [DOI] [PubMed] [Google Scholar]
- 19.Viskari H, Kondrashova A, Koskela P, Knip M, Hyöty H. Circulating vitamin D concentration in two neighbouring populations with markedly different incidence of type 1 diabetes. Diabetes Care. 2006;29:1458–1459. doi: 10.2337/dc06-2559. [DOI] [PubMed] [Google Scholar]
- 20.Sysi-Aho M, et al. Metabolic regulation in progression to autoimmune diabetes. PloS Comput. Biol. 2011;7:e1002257. doi: 10.1371/journal.pcbi.1002257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Livanos AE, Greiner TU, Vangay P. Antibiotic-mediated gut microbiome perturbation accelerates development of type 1 diabetes in mice. Nature Microbiol. 2016;1:16140. doi: 10.1038/nmicrobiol.2016.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cho I, Blaser MJ. The human microbiome: at the interface of health and disease. Nat Rev. 2012;13:260–270. doi: 10.1038/nrg3182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Costello E, et al. Bacterial community variation in human body habitats across space and time. Science. 2009;326:694. doi: 10.1126/science.1177486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The Integrative HMP (iHMP) Research Network Consortium The Integrative Human Microbiome Project: Dynamic Analysis of Microbiome-Host Omics Profiles during Periods of Human Health and Disease. Cell Host Microbe. 2014;16:276–289. doi: 10.1016/j.chom.2014.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yassour M, et al. Natural history of the infant gut microbiome and impact of antibiotic treatment on bacterial strain diversity and stability. Sci. Transl. Med. 2016;8:343ra81. doi: 10.1126/scitranslmed.aad0917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Biasucci G, et al. Mode of delivery affects the bacterial community in the newborn gut. Early Hum. Dev. 2010;86(suppl):13–15. doi: 10.1016/j.earlhumdev.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 27.Gregory KE. Microbiome aspects of perinatal and neonatal health. J. Perinat. Neonat. Nurs. 2011;25:158–162. doi: 10.1097/JPN.0b013e3182169346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Azad M, et al. Gut microbiota of healthy Canadian infants: profiles by mode of delivery and infant diet at 4 months. CMAJ. 2013;185:385–394. doi: 10.1503/cmaj.121189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Penders J, et al. Factors influencing the composition of the intestinal microbiota in early infancy. Pediatrics. 2006;118:511–521. doi: 10.1542/peds.2005-2824. [DOI] [PubMed] [Google Scholar]
- 30.Dominquez-Bello MG, et al. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. PNAS. 2010;107:11971–11975. doi: 10.1073/pnas.1002601107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Drell T, et al. The influence of different maternal microbial communities on the development of infant gut and oral microbiota. Nat. Sci. Rep. 2017;7:9940. doi: 10.1038/s41598-017-09278-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Johnson CL, Versalovic J. The human microbiome and its potential importance to pediatrics. Pediatrics. 2012;129:950–960. doi: 10.1542/peds.2011-2736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cardwell CR, et al. Caesarean section is associated with an increased risk of childhood-onset type 1 diabetes mellitus: a meta-analysis of observational studies. Diabetologia. 2008;51:726–735. doi: 10.1007/s00125-008-0941-z. [DOI] [PubMed] [Google Scholar]
- 34.Onderdonk AB, et al. Qualitative assessment of vaginal microflora during use of tampons of various compositions. Appl. Environ. Microbiol. 1987;53:2779–2784. doi: 10.1128/aem.53.12.2779-2784.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Genc MR, Onderdonk A. Endogenous bacterial flora in pregnant women and the influence on maternal genetic variation. BJOG. 2011;118:154–163. doi: 10.1111/j.1471-0528.2010.02772.x.. [DOI] [PubMed] [Google Scholar]
- 36.Ravel J, et al. Vaginal microbiome of reproductive age women. PNAS. 2011;108:4680–7. doi: 10.1073/pnas.1002611107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huang B, Fettweis JM, Brooks JP, Jefferson KK, Buck GA. The changing landscape of the vaginal microbiome. Clin. Lab. Med. 2014;34:747–761. doi: 10.1016/j.cll.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hickey RJ, Zhou X, Pierson JD, Ravel J, Forney LI. Understanding vaginal microbiome complexity from an ecological perspective. Transl. Res. 2012;160:267–282. doi: 10.1016/j.trsl.2012.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gajer, P., Brotman, R. M. & Bai, G. Temporal dynamics of the human vaginal microbiota. Sci. Transl. Med. 4, 10.1126/scitranslmed.3003605 (2012). [DOI] [PMC free article] [PubMed]
- 40.Roesch LF, et al. Culture-independent identification of gut bacteria correlated with the onset of diabetes in a rat model. ISME J. 2009;5:536–548. doi: 10.1038/ismej.2009.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Valladres R, et al. Lactobacillus johnsonii N6.2 Mitigates the Development of Type 1 Diabetes in BB-DP Rats. PLOS One. 2010;5:e10507. doi: 10.1371/journal.pone.0010507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.De Goffau MC, et al. Aberrant gut microbiota composition at the onset of type 1 diabetes in young children. Diabetologia. 2014;57:1569–1577. doi: 10.1007/s00125-014-3274-0. [DOI] [PubMed] [Google Scholar]
- 43.Mueller NT, Bakacs E, Combellick J, Grigoryan Z, Dominguez-Bello MG. The infant microbiome development: mom matters. Trends Mol. Med. 2015;21:109–117. doi: 10.1016/j.molmed.2014.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Forney LJ, Foster JA, Ledger W. The vaginal flora of healthy women in not always dominated by Lactobacillus species. JID. 2006;194:1468–1469. doi: 10.1086/508497. [DOI] [PubMed] [Google Scholar]
- 45.Dominquez-Bello MG, et al. Partial restoration of the microbiota of caesarean-born infants via vaginal microbial transfer. Nat. Med. 2016;22:250–253. doi: 10.1038/nm.4039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aagaard K, Stewart CJ, Chu D. Una destinatio, viae diversae. Does exposure to the vaginal microbiota confer health benefits to the infant, and does lack of exposure confer disease risk? EMBO Reports. 2016;17:1679–1684. doi: 10.15252/embr.201643483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Caporaso JG, et al. QIIME allows analysis of high-throughput community sequencing data. Nat. Met. 2010;7:335–336. doi: 10.1038/nmeth.f.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Price MN, Dehal PS, Arkin AP. FastTree 2–approximately maximum-likelihood trees for large alignments. PLoS One. 2010;5:e949. doi: 10.1371/journal.pone.0009490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ritari J, Salojarvi J, Lahti L, Le Vos WM. Improved taxonomic assignment of human intestinal 16S rRNA sequences by a dedicated reference database. BMC Genomics. 2015;16:1056. doi: 10.1186/s12864-015-2265-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Oksanen, J. et al. Vegan: Community Ecology Package. R package version 2.3-5. http://CRAN.R-project.org/package=vegan (2016).
- 51.Crawley, M. The R book. Wiley & Sons, London. 942 p. (2007).
- 52.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria, http://www.R-project.org/ (2014).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.