Abstract
BACKGROUND
Late infantile ceroid lipofuscinosis is a rare neurodegenerative disorder that appears between the ages of 2 and 4 years and is difficult to diagnose. In this report we present two sisters with this condition, and the clinical course consisted of delayed developmental skills initially and later regression of previously acquired skills. The cases were initially considered as childhood disintegrative disorder (CDD); however, when whole exome sequencing (WES) genetic testing was done, they proved to be variant late infantile ceroid lipofuscinosis. This is the first report from Jordan.
CASE SUMMARY
Clinical presentation included developmental delay and initially speech delay, followed by lose of sphincter control. Motor development was normal until 4 years of age, then they developed ataxia (fear of going downstairs) and weakness while walking. Atonic and myoclonic seizures become intractable, and this was followed by inability to stand or sit and loss of expressive language. In addition to complete blood count test, liver function test, kidney function test, serum electrolyte test, and blood sugar test, serum amino acid profile, B12 level test, thyroid function test, and a brain computed tomography scan were also normal. An electroencephalogram showed a generalized spike and wave pattern, and magnetic resonance imaging showed little to no abnormalities. After dealing with the cases as CDD, WES testing proved a final diagnosis of variant late infantile ceroid lipofuscinosis. Current treatment is anti-epileptic drugs and supportive care at home, and they are now in vegetative state.
CONCLUSION
This report highlights the importance of WES for the identification of genetic diseases, especially neurodegenerative disorders.
Keywords: Ceroid lipofuscinosis, Childhood disintegrative disorder, Lysosomal storage disorders, Neurodegenerative disorders, Variant late infantile, Case report
Core tip: Neuronal ceroid lipofuscinoses are a collection of neurodegenerative lysosomal storage disorders that are typically inherited in an autosomal recessive manner. In this case, we present the first incidence of this disorder in Jordan. It appears to have affected two siblings who experienced a slightly different clinical course from that which has typically been reported. This report also highlights the importance of whole exome sequencing for the identification of genetic causes of disease.
INTRODUCTION
Neuronal ceroid lipofuscinoses are a collection of neurodegenerative lysosomal storage disorders that are typically inherited in an autosomal recessive manner[1] and are associated with an accumulation of autofluorescent lipopigments in various tissues. The incidence of such disorders in the United States has been estimated to be around 1:12500[2]. Collectively, they are the most common type of hereditary neurodegenerative disease in childhood[3].
Neuronal ceroid lipofuscinoses have been classified based on their age at onset and clinical symptoms[4]. However, newer classifications have categorized the disorders based on their associated genes[5]. The late infantile type appears between the ages of 2 and 4 years, with clinical features that include visual loss, myoclonus, seizures, ataxia, and both mental and physical deterioration. Mutations in various genes have been linked to the late infantile type, including in CLN2, CLN5, CLN6, and CLN8[6].
Patients with variant late infantile neuronal ceroid lipofuscinosis caused by a mutation in the CLN6 gene have been reported in a number of countries worldwide, including in Costa Rica, Portugal, the Czech Republic, Sudan, Turkey, Saudi Arabia, Pakistan, and Japan[6-10]. The age at onset of this disease was slightly later than that of the late infantile type and most affected patients did not survive beyond their mid-20s[11]. Here, we present the first incidence of this disorder in Jordan, which affected two siblings who experienced a slightly different clinical course from that which has typically been reported.
CASE PRESENTATION
Chief complaints and history of present illness
The first child was a 10-year-old girl who presented with severe developmental speech delay until she reached 3 years old, at which point she began to speak minimally. At the age of 3 years, it was discovered that she suffered from short-term memory loss, although her long-term memories remained intact. At the age of 4 years, she began to lose sphincter control and was no longer able to control urination or defecation. She had shown normal motor development until 4 years of age, at which point she began to develop ataxia (fear of going downstairs) and weakness while walking. Atonic and myoclonic seizures also began to affect her at this age and could not be completely controlled despite the use of three anti-epileptic drugs (topiramate, levetiracetam, and valproate). Over the course of the subsequent year, her motor skills continued to decline, as she went from having difficulty walking to being limited to crawling. At 5 years old, she was completely unable to stand or sit, and was found to have very poor concentration and a very short attention span. Moreover, she had almost no expressive language, only vocalizing and echoing single words or screams with unclear sounds. She was incapable of imitating or playing with other children. At 5 years old, her mental age according to the Stanford-Binet Intelligence Scale was below the age of 2 years and her IQ was below 35.
Personal and family history
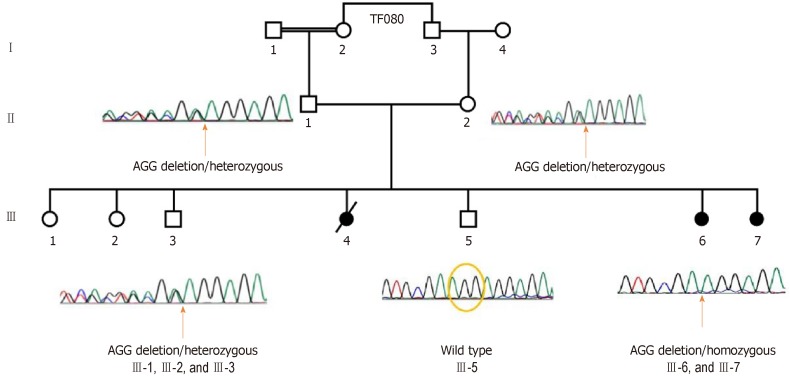
She was born by spontaneous delivery after a healthy 40-wk pregnancy with a typical birth weight of 3.5 kg and no postnatal complications. The family consisted of consanguineous parents (first cousins), two affected children, four healthy progenies, and one deceased daughter (Figure 1). The daughter died at 8 years of age, was reported to have had a clinical presentation similar to that of the current two affected children, but was not diagnosed or tested genetically. Both affected children (sisters) had a similar clinical course and the same family history. There was no other relevant family history.
Figure 1.
Family pedigree and segregation analysis of the identified variant NM_017882.2:c.794_796delCCT;p.Ser265del based on Sanger sequencing. The sequences shown are reverse complementary to CCT(AGG). The probands III-6 and III-7 are homozygous for the variant. The parents (II-1 and II-2) are heterozygous for the variant. The healthy siblings III-1, III-2, and III-3 are heterozygous for the variant.
Laboratory examinations
It is important to note that the patients had otherwise normal laboratory values. Complete blood count (CBC) test, liver function test, kidney function test, serum electrolyte test, and blood sugar test were all normal. Other tests included a serum amino acid profile, B12 level test, and thyroid function test.
Neuroimaging
A computed tomography (CT) scan at the time showed no abnormalities, and an electroencephalogram (EEG) showed a generalized spike and wave pattern. Subsequent brain magnetic resonance imaging (MRI) showed mild fronto-parietal brain atrophy.
Current medication
Topiramate, levetiracetam, and valproate.
Summary of the second child
The second child was a 9-year-old girl who was born by spontaneous delivery after a healthy 38-wk pregnancy with a typical birth weight of 3.25 kg and no postnatal complications. She had normal gross motor, fine motor, hearing, speech, and social behavioral skills until the age of 4 years. At this age, her expressive language began to decline, although her concentration and attention span remained acceptable. When she reached an age of 4 years and 8 mo, her mental age according to the Stanford-Binet Intelligence Scale corresponded to an age of 2 years and 7 mo, with an IQ score of 47. She complained of some minor dizziness and imbalance while walking and was reported to have mildly decreased short-term memory. At this age, she was able to imitate children at play and was able to play with her siblings. She had no vision or hearing loss, and no loss of sphincter function.
It is important to note that the patients had otherwise normal laboratory values. CBC test, liver function test, kidney function test, serum electrolyte test, and blood sugar test were all normal. Other tests including a serum amino acid profile, B12 level test, thyroid function test, and a brain CT scan were also normal.
A subsequent brain MRI also showed no abnormalities. However, her condition progressively declined until she turned 8 years old, when she could no longer stand, had very poor short-term memory, very poor speech, and had lost the ability to control urination and defecation. She required three anti-epileptic drugs (topiramate, levetiracetam, and valproate) to help manage her intractable atonic and myoclonic seizures, which were confirmed by EEG showing a generalized spike and wave pattern. Currently, at 9 years old, her hearing and vision have continued to decline and she is beginning to have some difficulty recognizing her mother.
Both patients were initially thought to have a form of regressive autism [childhood disintegrative disorder (CDD)] due to their poor social skills and normal initial laboratory tests and imaging results. Interestingly, there do exist lysosomal storage disorders which are associated with CDD[12-14]. A neurodegenerative disorder was suspected when MRI results revealed mild brain atrophy in the older sister and when the disease in both siblings began increasing in severity.
Differential diagnoses included leukodystrophy, subacute sclerosing panencephalitis, tuberous sclerosis, and CDD. The first three differential diagnoses were ruled out based on history, examinations, and investigations. Specifically, leukodystrophy was ruled out based on MRI results, subacute sclerosing panencephalitis was ruled out since EEG recordings failed to show any periodic patterns, and tuberous sclerosis was excluded due to the absence of any skin manifestations. A diagnosis of CDD was therefore tentatively established. Eventually, when the opportunity arose to perform whole exome sequencing (WES) on a group of patients from our hospital, we selected these two cases given that we still had not yet obtained a final diagnosis. Not only did the WES results give us a definitive diagnosis, they also increased our awareness of the value of WES for similar cases.
Genetic testing
WES was conducted on the proband III-6 using an Illumina HiSeq 2500 platform (Illumina) and Sure Select XT Human All Exon (Agilent). Sequencing reads were mapped to the Genome Reference Consortium Human Genome Build 37 (GRCh37) using BWA-0.5.10[15]. Polymerase chain reaction duplicates were removed using samblaster[16]. Single-nucleotide variants and small insertions/deletions (indels) were identified with freebayes[17] and annotated with SnpEff-3.3 (Ensembl-GRCh37.73)[18]. Sequencing was performed in the Institute of Medical Genetics and Applied Genomics at Tübingen University in Germany using the pipeline megSAP[19]. Variants that were located in the protein coding region (according to Ensembl database v68) were identified with at least 20X coverage and a mapping quality score ≥ 60.
The homozygous variant NM_017882.2:c.794_796delCCT;p.Ser265del was identified in the CLN6 gene. The variant was inspected visually with Integrative Genomic Viewer (IGV)[20]. The variant is homozygous in the second proband III-7 and segregates accordingly in the parents and in the non-affected siblings according to Sanger sequencing results (Figure 1). Despite reporting this variant as pathogenic[6], it is reported in Clinvar with conflicting interpretations of its pathogenicity.
FINAL DIAGNOSIS
Variable late infantile lipofuccinosis.
TREATMENT
Now, they are being on three antiepileptic drugs (topiramate, levetiracetam, and valproate) and supportive care.
OUTCOME AND FOLLOW-UP
Her vision and hearing have both been declining and by the age of 9 years, she was no longer able to recognize her mother by both sight and sound. Currently, at the age of 10 years, she was completely blind in both eyes. In addition to the loss of all motor skills and sphincter control, she lost expressive and receptive speech. Her life is almost as vegetative state, completely dependent on others.
DISCUSSION
Clinical symptoms of variant late infantile neuronal ceroid lipofuscinosis are similar to those of the late infantile type. However, the typical age at onset in patients with mutations in the CLN6 gene is between 3 and 8 years, which is slightly later than in the late infantile type[4]. Between the ages of 4 and 10 years, all motor skills are typically lost and vision is progressively impaired[21]. While consistent with those of previous reports, the cases presented here are not entirely typical. Most published cases present with seizures and motor difficulties prior to speech impairment. However, both sisters presented here suffered from speech impairments, with the older sister showing speech delay years before the emergence of other symptoms[4]. The two sisters also complained of hearing loss, which is not commonly seen in patients with variant late infantile neuronal ceroid lipofuscinosis.
In addition, the lack of significant brain MRI findings is another unique feature of our cases, with only mild fronto-parietal atrophy observed in the older sister. Previous reports suggest that a T2-weighted MRI would be expected to show high intensity in the periventricular white matter and decreased intensity in the putamen and thalamus of affected individuals[22]. Severe diffuse atrophy and marked dilatation of the ventricular system have also been associated with the condition[23]. This was unfortunately not assessed since only MRI reports, rather than actual images, were available for the patients. In addition, it is interesting to note that hydrogen-1 MR spectroscopy had been shown to enable noninvasive in vivo quantification of metabolite concentrations, reported as ratios (e.g., relative to creatine), in the brain. While a recent study concluded that the NAA/Cr and Cho/Cr ratios of the frontal region can be used to differentiate patients with metabolic syndrome from healthy volunteers[24], this could unfortunately not be performed in our case due to unavailability of the MRI data. Overall, while it is possible to obtain normal brain imaging results even at later stages of disease, the lack of significant MRI findings challenges the accuracy of the diagnosis.
In conclusion, our presentation of the two sisters with variant late infantile neuronal ceroid lipofuscinosis with hearing loss and relatively normal brain MRI findings provides further evidence of the pathogenicity of the identified variant. This report further demonstrates the value of WES in identifying genetic causes of neurodegenerative disorders.
CONCLUSION
Late infantile ceroid lipofuscinosis is a rare neurodegenerative disorder that is difficult to diagnose. This report highlights the value of WES genetic testing in the diagnosis of neurodegenerative diseases, especially when the presentation is not typical.
Footnotes
Informed consent statement: Consent was obtained from parents of the patients for publication of this report.
Conflict-of-interest statement: The authors declare that they have no conflicts of interest.
CARE Checklist (2016) statement: The guidelines of the CARE Checklist have been adopted.
Manuscript source: Unsolicited manuscript
Peer-review started: September 18, 2018
First decision: October 25, 2018
Article in press: December 15, 2018
Specialty type: Medicine, research and experimental
Country of origin: Jordan
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Hernanda PY, Kaya M, Razek AAKA S- Editor: Ji FF L- Editor: Wang TQ E- Editor: Wu YXJ
Contributor Information
Omar Nafi, Department of Pediatrics, Faculty of Medicine, Mutah University, Al Karak 61710, Jordan. omarnafi@mutah.edu.jo.
Bashar Ramadan, Department of Pediatrics, Faculty of Medicine, Mutah University, Al Karak 61710, Jordan.
Olaf Riess, Institute of Medical Genetics and Applied Genomics, Rare Disease Center, University of Tübingen, Tübingen 72076, Germany.
Rebecca Buchert, Institute of Medical Genetics and Applied Genomics, Rare Disease Center, University of Tübingen, Tübingen 72076, Germany.
Tawfiq Froukh, Department of Biotechnology and Genetic Engineering, Philadelphia University, Amman 11118, Jordan.
References
- 1.Pardo CA, Rabin BA, Palmer DN, Price DL. Accumulation of the adenosine triphosphate synthase subunit C in the mnd mutant mouse. A model for neuronal ceroid lipofuscinosis. Am J Pathol. 1994;144:829–835. [PMC free article] [PubMed] [Google Scholar]
- 2.Rider JA, Rider DL. Batten disease: past, present, and future. Am J Med Genet Suppl. 1988;5:21–26. doi: 10.1002/ajmg.1320310606. [DOI] [PubMed] [Google Scholar]
- 3.Zeman W, Dyken P. Neuronal ceroid-lipofuscinosis (Batten's disease): relationship to amaurotic family idiocy? Pediatrics. 1969;44:570–583. [PubMed] [Google Scholar]
- 4.Mole SE, Williams RE, Goebel HH. Correlations between genotype, ultrastructural morphology and clinical phenotype in the neuronal ceroid lipofuscinoses. Neurogenetics. 2005;6:107–126. doi: 10.1007/s10048-005-0218-3. [DOI] [PubMed] [Google Scholar]
- 5.Ceroid lipofuscinosis, neuronal, 1; CLN1#256730. Online Mendelian Inheritance in Man, Johns Hopkins University (Baltimore, MD); 2015 [cited 2018 Jun 4] Available from: https://omim.org/entry/256730.
- 6.Sharp JD, Wheeler RB, Parker KA, Gardiner RM, Williams RE, Mole SE. Spectrum of CLN6 mutations in variant late infantile neuronal ceroid lipofuscinosis. Hum Mutat. 2003;22:35–42. doi: 10.1002/humu.10227. [DOI] [PubMed] [Google Scholar]
- 7.Sato R, Inui T, Endo W, Okubo Y, Takezawa Y, Anzai M, Morita H, Saitsu H, Matsumoto N, Haginoya K. First Japanese variant of late infantile neuronal ceroid lipofuscinosis caused by novel CLN6 mutations. Brain Dev. 2016;38:852–856. doi: 10.1016/j.braindev.2016.04.007. [DOI] [PubMed] [Google Scholar]
- 8.Al-Muhaizea MA, Al-Hassnan ZN, Chedrawi A. Variant late infantile neuronal ceroid lipofuscinosis (CLN6 gene) in Saudi Arabia. Pediatr Neurol. 2009;41:74–76. doi: 10.1016/j.pediatrneurol.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 9.Siintola E, Topcu M, Kohlschütter A, Salonen T, Joensuu T, Anttonen AK, Lehesjoki AE. Two novel CLN6 mutations in variant late-infantile neuronal ceroid lipofuscinosis patients of Turkish origin. Clin Genet. 2005;68:167–173. doi: 10.1111/j.1399-0004.2005.00471.x. [DOI] [PubMed] [Google Scholar]
- 10.Mole SE, Michaux G, Codlin S, Wheeler RB, Sharp JD, Cutler DF. CLN6, which is associated with a lysosomal storage disease, is an endoplasmic reticulum protein. Exp Cell Res. 2004;298:399–406. doi: 10.1016/j.yexcr.2004.04.042. [DOI] [PubMed] [Google Scholar]
- 11.Warrier V, Vieira M, Mole SE. Genetic basis and phenotypic correlations of the neuronal ceroid lipofusinoses. Biochim Biophys Acta. 2013;1832:1827–1830. doi: 10.1016/j.bbadis.2013.03.017. [DOI] [PubMed] [Google Scholar]
- 12.Malhotra S, Gupta N. Childhood disintegrative disorder. J Autism Dev Disord. 1999;29:491–498. doi: 10.1023/a:1022247903401. [DOI] [PubMed] [Google Scholar]
- 13.Malamud N. Heller's disease and childhood schizophrenia. Am J Psychiatry. 1959;116:215–218. doi: 10.1176/ajp.116.3.215. [DOI] [PubMed] [Google Scholar]
- 14.Corbett J, Harris R. Progressive disintegrative psychosis of childhood. J Child Psychol Psychiatry. 1977;18:211–219. doi: 10.1111/j.1469-7610.1977.tb00433.x. [DOI] [PubMed] [Google Scholar]
- 15.Li H, Durbin R. Fast and accurate long-read alignment with Burrows-Wheeler transform. Bioinformatics. 2010;26:589–595. doi: 10.1093/bioinformatics/btp698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Faust GG, Hall IM. SAMBLASTER: fast duplicate marking and structural variant read extraction. Bioinformatics. 2014;30:2503–2505. doi: 10.1093/bioinformatics/btu314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garrison E, Marth G. Haplotype-based variant detection from short-read sequencing; 2012. Available from: https://arxiv.org/abs/1207.3907.
- 18.Cingolani P, Platts A, Wang le L, Coon M, Nguyen T, Wang L, Land SJ, Lu X, Ruden DM. A program for annotating and predicting the effects of single nucleotide polymorphisms, SnpEff: SNPs in the genome of Drosophila melanogaster strain w1118; iso-2; iso-3. Fly (Austin) 2012;6:80–92. doi: 10.4161/fly.19695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sturm MCS, Shroeder C, Haack T. 2017. megSAP a medical genetics sequence analysis pipeline. European Society of Human Genetics Annual Meeting; pp. April 3–5; Barcelona, Spain 2017. [Google Scholar]
- 20.Thorvaldsdóttir H, Robinson JT, Mesirov JP. Integrative Genomics Viewer (IGV): high-performance genomics data visualization and exploration. Brief Bioinform. 2013;14:178–192. doi: 10.1093/bib/bbs017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Teixeira CA, Espinola J, Huo L, Kohlschütter J, Persaud Sawin DA, Minassian B, Bessa CJ, Guimarães A, Stephan DA, Sá Miranda MC, MacDonald ME, Ribeiro MG, Boustany RM. Novel mutations in the CLN6 gene causing a variant late infantile neuronal ceroid lipofuscinosis. Hum Mutat. 2003;21:502–508. doi: 10.1002/humu.10207. [DOI] [PubMed] [Google Scholar]
- 22.Nardocci N, Morbin M, Bugiani M, Lamantea E, Bugiani O. Neuronal ceroid lipofuscinosis: detection of atypical forms. Neurol Sci. 2000;21:S57–S61. doi: 10.1007/s100720070041. [DOI] [PubMed] [Google Scholar]
- 23.Davidson BL, Cabrera-Salazar MA, Pearce DA. The neuronal ceroid lipofuscinoses: clinical features and molecular basis of disease. In: Barranger JA, Cabrera-Salazar MA. Lysosomal Storage Disorders. Springer; 2007. pp. 371–388. [Google Scholar]
- 24.El-mewafy Z, Abdel Razek AAAK, El-Eshmawy M, Abo El-Eneen N, EL-Biaomy A. MR spectroscopy of the frontal region in patients with metabolic syndrome: Correlation with anthropometric measurement. Polish J Radiol. 2018;83:e215–e219. doi: 10.5114/pjr.2018.76024. [DOI] [PMC free article] [PubMed] [Google Scholar]