Abstract
Background:
Repetitive pitching produces significant stress on the elbow that may result in structural abnormalities discernable on magnetic resonance imaging (MRI) without causing symptoms.
Purpose:
To determine whether there exists an association between subclinical MRI findings in asymptomatic elbows of Major League Baseball (MLB) players and future placement on the disabled list (DL) or future operative procedure.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
MRI scans of the elbows of professional-level baseball pitchers, taken during routine presigning imaging at a single organization from 2005 to 2017, were retrospectively reviewed. Publicly available databases were queried to exclude pitchers with an injury before the earliest session of elbow MRI. Three blinded reviewers reviewed all MRI scans independently to evaluate for the presence of chondral damage to the joint, loose bodies, ulnar collateral ligament (UCL) heterogeneity or tears, flexor pronator mass defects, and signs of posteromedial (PM) impingement. Binary imaging findings were related to future placement on the DL for elbow complaints and future elbow surgery.
Results:
A total of 41 pitchers had asymptomatic MRI findings with no prior DL placement. For players who eventually went on the DL, there were a statistically greater number of players with UCL heterogeneity (P = .021), humeral-sided partial UCL tears (P = .031), and PM impingement (P = .004) on preinjury MRI compared with players who remained healthy. PM impingement was related to future elbow-related surgery (P = .003). Pitchers with UCL heterogeneity were associated with reduced career strike zone percentage, innings pitched, and fastball percentage (P < .05 for all).
Conclusion:
UCL heterogeneity, PM impingement, and humeral-sided partial tears were correlated with future DL placement for elbow-related reasons in MLB pitchers. Asymptomatic PM impingement may be a precursor to future surgery.
Keywords: Major League Baseball, elbow, injury, magnetic resonance imaging, baseball
The Major League Baseball (MLB) pitch is recognized as one of the fastest motions achievable, with current velocities consistently greater than 90 miles per hour.10 Over the past 10 years, the incidence of ulnar collateral ligament (UCL) tears has risen,6,8 and the increasing level of competition and higher incidence of injuries make predicting the physical health of a pitcher’s elbow vital to an MLB organization. Additionally, the sum of yearly spending on pitchers in MLB is greater than on any other single position in all American sports, at approximately US$1.5 billion in 2018.27 This adds a financial incentive for organizations to ensure sustained physical health and career longevity and identify preinjury factors that may be detrimental to players.
Repetitive pitching has been shown to apply significant valgus stress on the elbow, resulting in posteromedial (PM) joint space narrowing in the elbow.15,24 Changes in the elbow joint are only exacerbated by the length and intensity of one’s pitching career. Magnetic resonance imaging (MRI) has demonstrated substantial structural changes to both the shoulder and elbow joints of asymptomatic professional pitchers.7,20,21,31 UCL abnormalities and PM impingement were noted in 87.5% and 81.3%, respectively, on asymptomatic MRI scans.20 However, it is unknown whether these structural abnormalities pose any long-term clinical significance. Along with the high incidence of abnormalities, 1 previous study has demonstrated an association between asymptomatic structural abnormalities on shoulder MRI and reduced innings pitched, although no association was determined for future injuries.21
Team physicians base clinical decisions on patient complaints, physical examination results, and radiographic findings. Without patient complaints, there is little reason at present for physicians to consult diagnostic imaging. However, it has become common practice for professional organizations to have affiliated athletes undergo MRI before contract signing to screen for potential abnormalities.14 MRI is the imaging modality that can best aid in establishing the diagnoses of elbow abnormalities, with 57% sensitivity and 100% specificity in diagnosing UCL injuries.9,25,28 However, the importance of subclinical findings on diagnostic imaging is still under debate, particularly with respect to the elbow. Findings predictive of a future injury have obvious value to players and professional organizations, as injuries have significant financial implications and affect career performance. These findings may persuade athletic trainers, medical staff, and physicians to employ additional preventive measures to avoid time lost to an injury. A previous study of MRI changes in the elbow of pitchers corroborated a high prevalence of abnormalities, although it was underpowered to draw any significant clinical conclusion.14 Further understanding of this aspect would be highly valuable in preventing future injuries and would allow physicians to better stratify incoming players by injury risk.
The purpose of this study was to determine whether there exists an association between subclinical MRI findings in asymptomatic elbows of MLB players and future placement on the disabled list (DL) or future operative procedure. It was our hypothesis that common structural abnormalities in professional pitchers, such as UCL heterogeneity, are predictive of future injuries and surgery.
Methods
Player Selection
We retrospectively reviewed the MRI scans of the pitching elbow of all MLB pitchers from 2005 to 2017 at a single organization. For all pitchers with available scans, publicly available databases were queried to determine injury history, surgical history, and placement on the DL; the databases queried were www.fangraphs.com 13 and www.baseball-reference.com.2 Publicly available databases were utilized for this study because alternative sources would be deidentified and preclude cross-referencing of MRI scans and patient medical records.
A pitcher’s MRI scan was considered asymptomatic if MRI was performed at least 6 months before DL placement for any elbow-related injury. Pitchers were excluded if they had a history of DL placement for any elbow-related injury or surgery before MRI. Pitchers who went on to spend time on the DL were categorized in the injured group, while those without DL placement were categorized in the healthy group to serve as a control. A total of 41 pitchers had asymptomatic MRI findings with no prior DL placement. The mean age of the pitchers at the time of MRI was 22.3 ± 3.5 years, and the mean number of career games was 115.0 ± 132.8. The mean body mass index was 26.0 ± 3.1 kg/m2. There were 27 right-handed pitchers (66%) and 14 left-handed pitchers (34%).
Data Collection
Pitchers who eventually went on the DL were reviewed for the number of days and number of times placed on the DL for any elbow-related complaint. Patient medical records were retrospectively reviewed to determine medical and surgical history and confirm these data. The above publicly available databases were also reviewed for career innings pitched, career games started, career pitch count, and career maximum velocity of pitch. These statistics were acquired at intervals with respect to the MRI date: 1 year after MRI, 2 years after MRI, 3 years after MRI, 5 years after MRI, and career statistics independent of MRI time. Sabermetric pitching statistics were collected using PITCHf/x (Sportvision) after 2007.3 Before 2007, these statistics were collected by Baseball Info Solutions and were not standard across stadiums. These statistics were only collected for major league play.
Radiographic Analysis
Three blinded reviewers (G.H.G., J.R.M., N.N.V.) evaluated all MRI scans independently. Reviewers were blinded to the pitcher’s name and whether he belonged to the injured group or healthy group. Two fellowship-trained orthopaedic sports medicine surgeons (G.H.G., N.N.V.) and 1 fellowship-trained musculoskeletal radiologist (J.R.M.) read all MRI scans. Radiological findings were separated into binary outcomes for the presence of the following: chondral damage to the radiocapitellar joint, chondral damage to the ulnohumeral joint, bone edema, loose bodies, UCL heterogeneity, ulnar-sided UCL tear, humeral-sided UCL tear, flexor pronator mass heterogeneity, flexor pronator mass defect, and PM impingement. UCL heterogeneity was defined as any hyperintense signal of the UCL. A flexor pronator mass defect was defined by hyperintensity, edema, or inflammation in the flexor pronator mass. PM impingement was defined by the presence of a hyperintense signal in the PM aspect of the olecranon with or without osteophyte formation.
Statistical Analysis
Statistical analysis was performed using RStudio software (v 1.0.143; RStudio). The injured and healthy groups were compared using the Student t test and Fisher exact test. The univariate Fisher exact test was used to determine the association of each radiographic finding to future placement on the DL. Interrater reliability was measured using the Fleiss kappa statistic. Pitchers with a radiological sign were compared with pitchers without that sign using the Student t test to compare the number of times placed on the DL, days spent on the DL, and all sabermetric statistics.
Results
Of the 41 pitchers included, 16 (39.0%) had normal elbow MRI findings, while 25 (61.0%) had at least 1 abnormal finding. There were 2 cases suggestive of chondral damage to the radiocapitellar joint, 1 case of chondral damage to the ulnohumeral joint, 1 case of bone edema, and 1 player with loose bodies. There were 14 pitchers with evidence of a UCL heterogeneous/hyperintense signal, 2 with an ulnar-sided tear, 11 with a humeral-sided tear, and none with a full-thickness tear (Figure 1). There were 5 pitchers with heterogeneity/hyperintensity of the flexor pronator mass, 0 with a defect of the mass, and 8 pitchers with PM impingement (Figure 2). One pitcher with PM impingement had evidence of an osteophyte within the same location. There were 16 players who were eventually placed on the DL because of an elbow-related complaint. Within this injured group, MRI was performed a mean of 821.8 ± 690.9 days before placement on the DL for an elbow injury. Reasons for DL placement included a UCL injury (n = 10), elbow inflammation (n = 3), elbow sprain (n = 1), elbow strain (n = 1), and flexor pronator mass strain (n = 1). Eleven players eventually went on to undergo elbow surgery. Nine players underwent reconstruction of the UCL; 1 patient undergoing UCL reconstruction also underwent subsequent ulnar nerve transposition. Of the remaining 2 players, 1 underwent cubital tunnel release with ulnar nerve transposition and neuroplasty of the medial antebrachial cutaneous nerve, and 1 underwent arthroscopic elbow debridement with coracoid resection, capsular release, and posterior debridement. The demographics of the injured group were not statistically different from those of the healthy group (Table 1).
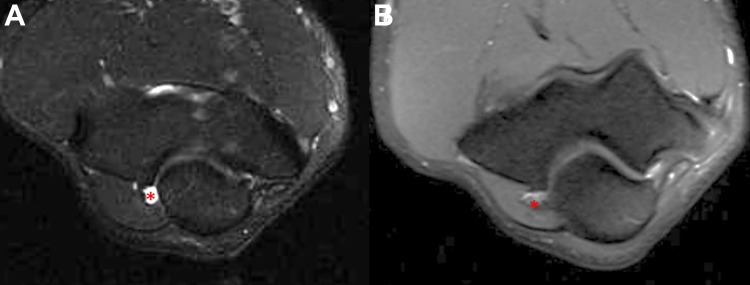
Figure 1.
Coronal slice of T2-weighted magnetic resonance imaging demonstrating ulnar collateral ligament (UCL) hyperintensity in 2 professional Major League Baseball pitchers. *Indicative of abnormality.
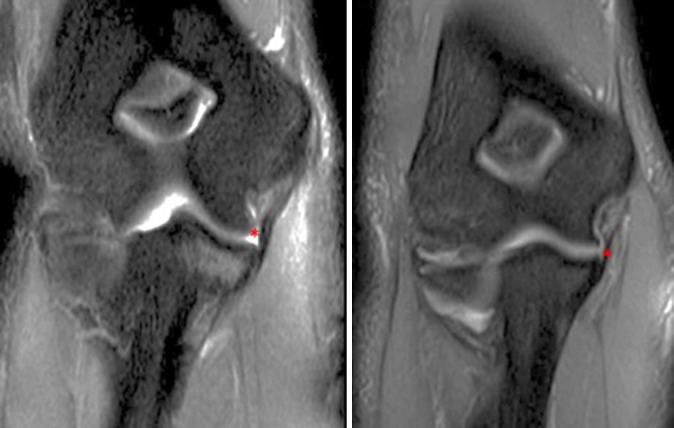
Figure 2.
Axial slice of T2-weighted magnetic resonance imaging demonstrating (A) posteromedial (PM) impingement and (B) PM impingement with an osteophyte in 2 professional Major League Baseball pitchers. *Indicative of abnormality.
TABLE 1.
Demographics of Study Pitchersa
| Characteristic | Injured (n = 16) | Healthy (n = 25) | P Value |
|---|---|---|---|
| Age, y | 21.6 ± 2.8 | 22.8 ± 3.8 | .257 |
| Height, in | 75.5 ± 1.9 | 75.4 ± 2.3 | .830 |
| Weight, lb | 204.4 ± 19.6 | 215.4 ± 29.1 | .153 |
| No. of games played | 100.9 ± 83.1 | 122.9 ± 155.7 | .577 |
| Handedness, right/left, n | 10/6 | 17/8 | .693 |
aData are reported as mean ± SD unless otherwise specified.
Pitchers who were placed on the DL spent a mean of 123.1 ± 69.7 days only because of elbow-related injuries and were placed on the DL a mean of 1.3 ± 0.4 times for elbow-related complaints. No preinjury MRI findings were associated with time that players spent on the DL. For players who eventually went on the DL, there were a statistically greater number of players with a heterogeneous signal of the UCL (P = .021), humeral-sided partial tearing of the UCL (P = .031), and PM impingement (P = .004) on preinjury MRI in comparison with those players who remained healthy (Table 2).
TABLE 2.
MRI Findings and Relationship to Future Placement on the DL and Future Surgerya
| MRI Finding | Incidence of Finding (Injured vs Healthy) | P Value | Kappa (P Value) | |||
|---|---|---|---|---|---|---|
| Future DL Placement | No. of DL Placements | Time on DL | Future Surgery | |||
| Chondral damage: radiocapitellar | 6.3% vs 4.0% | >.999 | NA | NA | >.999 | 0.129 (.404) |
| Chondral damage: ulnohumeral | 6.3% vs 0.0% | .390 | NA | NA | .268 | 0.225 (.011) |
| Bone edema | 6.3% vs 0.0% | .390 | NA | NA | .268 | –0.013 (.883) |
| Loose bodies | 6.3% vs 0.0% | .390 | .273 | .268 | .263 | –0.008 (.928) |
| Heterogeneity of UCL | 56.3% vs 24.0% | .021 | .254 | .254 | .469 | 0.469 (.002) |
| Ulnar-sided partial tear | 6.3% vs 4.0% | >.999 | NA | NA | >.999 | 0.162 (.068) |
| Humeral-sided partial tear | 50.0% vs 16.0% | .031 | .792 | .572 | .136 | 0.179 (.045) |
| Heterogeneity of flexor pronator mass | 18.8% vs 8.0% | .361 | .110 | .794 | .247 | 0.294 (.001) |
| Defect in flexor pronator mass | 0.0% vs 0.0% | NA | NA | NA | NA | –0.068 (.447) |
| Posteromedial impingement | 43.8% vs 4.0% | .004 | .200 | .179 | .003 | 0.213 (.016) |
aBolded values indicate statistical significance (P < .05). DL, disabled list; MRI, magnetic resonance imaging; NA, not applicable (analysis was not performed because of insufficient number of players in either group); UCL, ulnar collateral ligament.
Of the 11 players who eventually underwent surgery, 5 had findings of UCL heterogeneity, 5 had findings of a humeral-sided UCL tear, and 6 had signs of PM impingement. Of the 9 players who underwent UCL reconstruction, 4 had findings of UCL heterogeneity, 4 had findings of a humeral-sided UCL tear, and 4 had findings of PM impingement. One patient with a PM osteophyte required cubital tunnel release with ulnar nerve transposition. For the players who eventually underwent surgery, MRI signs of PM impingement were significantly higher on preinjury MRI compared with the nonsurgical group (P = .003).
Future pitching statistics were also associated with significant preinjury MRI findings. UCL heterogeneity was found to be correlated with the most significant findings. Pitchers with UCL heterogeneity versus those without this finding had decreased strikeouts per 9 innings pitched at 3 years after MRI (6.6 vs 9.3, respectively; P = .007) and a reduced strike zone percentage at 2 years after MRI (40.1% vs 49.7%, respectively; P = .010). For fastball percentage, there were differences at 2 years (36.2% vs 54.4%, respectively; P = .010) and 3 years (36.6% vs 64.5%, respectively; P = .009) after preinjury MRI. More importantly, over these pitchers’ entire career, there was a reduced strike zone percentage (42.3% vs 46.1%, respectively; P = .040), fewer innings pitched (65.0 vs 428.9, respectively; P = .042), and lower percentage of fastballs thrown (36.6% vs 53.6%, respectively; P = .007) when UCL heterogeneity was found on preinjury MRI.
Humeral-sided partial tears were only associated with a reduced strikeout percentage at 2 years after MRI (12.4% vs 25.5%, respectively; P = .039). For PM impingement findings, there was a decreased batting average on balls in play at 3 years after MRI (24.8% vs 31.4%, respectively; P = .036), reduced strike zone percentage at 2 years after MRI (40.8% vs 49.5%, respectively; P = .014), and increased fastball percentage at 1 year (53.0% vs 36.6%, respectively; P = .011) and 3 years (58.2% vs 37.5%, respectively; P = .048) after MRI (Table 3).
TABLE 3.
Statistical Difference in Sabermetric Pitching Measurementsa
| Pitching Statistic | P Value | Pitching Statistic | P Value | ||||
|---|---|---|---|---|---|---|---|
| Heterogeneity of UCL | Humeral- Sided Partial Tear | Posteromedial Impingement | Heterogeneity of UCL | Humeral- Sided Partial Tear | Posteromedial Impingement | ||
| Earned run average | Strike zone percentage | ||||||
| 1 y | .995 | .279 | .318 | 1 y | .105 | .927 | .150 |
| 2 y | .589 | .914 | .972 | 2 y | .010 | .355 | .014 |
| 3 y | .390 | .235 | .330 | 3 y | .632 | .895 | .662 |
| 5 y | .855 | .388 | 5 y | .953 | .953 | ||
| Career | .734 | .496 | .675 | Career | .040 | .551 | .437 |
| Batting average on balls in play | Innings pitched | ||||||
| 1 y | .709 | .199 | .169 | 1 y | .129 | .565 | .159 |
| 2 y | .852 | .063 | .928 | 2 y | .225 | .065 | .210 |
| 3 y | .163 | .219 | .036 | 3 y | .095 | .085 | .143 |
| 5 y | .671 | .671 | 5 y | .371 | .371 | ||
| Career | .417 | .436 | .453 | Career | .042 | .058 | .113 |
| Strikeout-to-walk ratio | Total pitches | ||||||
| 1 y | .082 | .517 | .075 | 1 y | .164 | .385 | .187 |
| 2 y | .166 | .390 | .575 | 2 y | .260 | .082 | .223 |
| 3 y | .735 | .954 | .753 | 3 y | .089 | .097 | .115 |
| 5 y | .922 | .922 | 5 y | .348 | .348 | ||
| Career | .086 | .065 | .688 | Career | .053 | .086 | .146 |
| Strikeouts per 9 innings pitched | Fastball percentage | ||||||
| 1 y | .247 | .426 | .083 | 1 y | .065 | .404 | .011 |
| 2 y | .916 | .400 | .349 | 2 y | .010 | .278 | .064 |
| 3 y | .007 | .092 | .124 | 3 y | .009 | .076 | .048 |
| 5 y | .706 | .706 | 5 y | .173 | .173 | ||
| Career | .657 | .951 | .396 | Career | .007 | .317 | .094 |
| Walks plus hits per inning pitched | Fastball velocity | ||||||
| 1 y | .368 | .268 | .144 | 1 y | .427 | .295 | .202 |
| 2 y | .739 | .091 | .891 | 2 y | .748 | .898 | .460 |
| 3 y | .977 | .888 | .528 | 3 y | .559 | .803 | .065 |
| 5 y | .347 | .347 | 5 y | .200 | .201 | ||
| Career | .093 | .846 | .511 | Career | .301 | .189 | .132 |
| Pitches per inning | Fielding independent pitching | ||||||
| 1 y | .344 | .404 | .554 | 1 y | .686 | .497 | .313 |
| 2 y | .877 | .162 | .812 | 2 y | .659 | .098 | .892 |
| 3 y | .795 | .999 | .390 | 3 y | .483 | .487 | .671 |
| 5 y | .823 | .823 | 5 y | .351 | .351 | ||
| Career | .318 | .358 | .368 | Career | .054 | .066 | .795 |
| Strikeout percentage | |||||||
| 1 y | .221 | .698 | .150 | ||||
| 2 y | .428 | .039 | .816 | ||||
| 3 y | .317 | .836 | .692 | ||||
| 5 y | .071 | ||||||
| Career | .071 | .554 | .826 | ||||
aBolded values indicate statistical significance (P < .05). UCL, ulnar collateral ligament.
Discussion
This study established the novel finding that asymptomatic MRI abnormalities have predictive value in the future injury status of MLB pitchers. Pitchers who went on to be placed on the DL had a significantly higher incidence of UCL heterogeneity, humeral-sided partial tears, and PM impingement on preinjury MRI. Furthermore, PM impingement was associated with future elbow surgery. Additionally, UCL heterogeneity on preinjury MRI was associated with detrimental effects such as decreased strike zone percentage, innings pitched, and fastball percentage throughout the rest of the player’s career. These findings may prove useful as cautionary signals for the risk assessment of new players or for use in establishing preventive programs for these players.
There is a high prevalence of subclinical abnormal MRI findings in athletes of all professional sports leagues in the United States.17,18,20,21,26 These findings are expected because of the degree of competition and extended hours of repetitive movements, but it remains to be seen whether they have any clinical significance.26 UCL heterogeneity was previously reported in 87.5% of asymptomatic professional baseball players, while PM impingement was present in 81.3%.20 In our study, we found a lower rate of 34.1% for UCL heterogeneity and 19.5% for PM impingement. The current study is the first to report that both of these preinjury findings are correlated with future DL placement. Only Gutierrez et al14 have evaluated this topic, finding no correlation with preoperative MRI and future DL placement, although they did report a trend toward signal change and PM osteophytes (P = .07). Given the economic impact of the current study on MLB pitchers, further research is needed to evaluate programs to mitigate these risks, thus reducing future DL placement in players with these findings.
While placement on the DL has significant economic impact on an MLB team, players needing surgical interventions are even more detrimental. The fact that PM impingement may predict the need for future surgery (majority UCL reconstruction) is highly relevant. Primary UCL reconstruction boasts very impressive results, with up to 90% returning to play and 67% resuming the original level of play.12,23,32 Although the revision rate is low, 37% of revision reconstructions occur within 3 years of index surgery, after which there is a steep drop in performance.12,16,22
Ideally, an intervention should begin during the subclinical phase so that efforts may be placed toward injury prevention to avoid future surgery. Time missed because of an injury and surgery accrues high opportunity costs for the organization and may affect future contracts for the pitcher.27 Stretching protocols may be instituted for injury prevention, as previous studies have suggested that reduced shoulder flexion and external rotation increased the risk of these elbow injuries.5,30 Although dependent on the time of the season and pitching level, decreasing pitch counts and longer periods of rest may be alternative methods of prevention in pitchers with these subclinical findings.1,4,11
Overall, the MRI findings that correlated with pitching statistics were limited except for UCL heterogeneity. This study found that 3 major career statistics were significantly correlated with UCL heterogeneity, including a reduced strike zone percentage, fewer innings pitched, and lower fastball percentage. Of these, reduced innings pitched over a pitcher’s career may have major clinical significance. One thought may be that this finding is a precursor to overuse, decreased accuracy (strike zone percentage), and decreased endurance (fastball percentage), leading coaches to limit the pitcher’s appropriated innings. This preinjury MRI finding of UCL heterogeneity is further validated in that was also associated with DL placement, which may be why innings pitched were decreased as well. These results are intriguing and may have a large impact on predicting a pitcher’s future performance. Whiteside et al29 demonstrated that a smaller repertoire of pitches, fewer days between games, and a greater pitch count were other factors associated with the need for future UCL reconstruction. However, the same association between pitching volume and the need for surgery was not present in predicting the need for revision UCL surgery.19 Further evaluations are needed to validate these findings and better stratify the risk associated with signing players with this finding of UCL heterogeneity on presigning MRI.
Currently, only Gutierrez et al14 have attempted to evaluate MRI elbow findings in MLB players with respect to future DL placement. They reported on 26 pitchers with 1 MRI evaluator and found no significant correlation with DL placement or long-term pitching statistics. This varies from our results, in which UCL heterogeneity and PM impingement were significantly correlated with future DL placement and had a significant correlation with poor career statistics. The major discrepancy between the studies may be that Gutierrez et al14 had limited MRI evaluators, a smaller sample size, and neither PM impingement nor UCL heterogeneity being evaluated. An early study from Wright et al31 evaluated 57 pitchers with elbow radiographs but found no correlation with future placement on the DL. The main explanation for the difference from our results is likely the lack of detailed imaging (ie, MRI), which has demonstrated higher sensitivity and specificity compared with elbow radiographs and is now the gold standard for the presigning evaluation of elbow abnormalities.9 To date, the current analysis is the only study to correlate elbow abnormalities on preinjury MRI with future placement on the DL in MLB pitchers. Of note, elbow abnormalities may also cause differences in throwing mechanics that can result in shoulder injuries. These injuries were not reflected within the analysis, as this was outside the scope of the study. However, the relationship of throwing mechanics with elbow abnormalities may be of interest to future studies.
This study is not without its limitations. The primary limitation is the retrospective design of this study. Presigning MRI may be performed at different time points of a professional pitcher’s career, depending on whether the contract was negotiated during the MLB draft or during a trade of an older player. Public databases and medical charts were scrutinized to limit this bias by excluding all pitchers with prior elbow injuries; however, college and high school records were unavailable for review. Further, there is no objective classification or grading scale for many of these radiological signs. Consequently, there is likely some observer bias that exists when readers are reviewing MRI scans of major league pitchers. To mitigate this risk, highly trained readers with significant experience in reading professional baseball players’ elbow MRI scans were utilized. Also, the present study had appropriate interrater reliability for all significant findings.
A further limitation is that publicly available databases were utilized for injury history, time spent injured, and future surgery. It is important to note that these databases were compiled from third-party sources, although these websites have been frequently used in prior studies for the purposes of analyzing events of injury and pitching outcomes.6,11,12,16,22,23,32 However, it is also important to note that the accuracy of these databases has not been verified. The present study was limited in its sample size, as it was a single-institution study. The inclusion of multiple organizations may allow for extended analyses to make broader conclusions. Additionally, pitcher performance is likely confounded by factors outside those related to elbow health. Other considerations such as player experience, physical fitness, coaching staff, fatigue, and aging may limit the conclusions that can be drawn from a decline in sabermetric pitching statistics. These factors were not controlled for, and a correlation with MRI findings may not necessarily demonstrate the causality of declining performance. Overall, despite these limitations, the results of this study may have strong implications with regard to the preinjury evaluation and risk assessment of MLB pitchers.
Conclusion
MLB pitchers frequently have asymptomatic degenerative changes on MRI. This study demonstrates that UCL heterogeneity, PM impingement, and humeral-sided partial tears on preinjury MRI were correlated with future placement on the DL. In addition, asymptomatic PM impingement may be a precursor to future surgery. As for future play, asymptomatic UCL heterogeneity on MRI was found to correlate with worse career pitching performance. Overall, these data may prove useful for coaches, trainers, and team physicians to appropriately risk stratify new players and establish algorithms to prevent the overall impact of these elbow injuries.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: G.H.G. has received educational support from Smith & Nephew. A.A.R. receives royalties from Arthrex and Saunders/Mosby; is a paid speaker/presenter for Arthrex; is a consultant for Arthrex; and receives research support from Arthrex, DJO Surgical, Smith & Nephew, and Ossur. N.N.V. is a consultant for Smith & Nephew and Medacta; receives royalties from Smith & Nephew; has received hospitality payments from Stryker, Arthrex, and Wright Medical; is a paid speaker/presenter for Pacira Pharmaceuticals; has received educational support from Medwest Associates; and has stock/stock options in CyMedica Orthopedics. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Rush University Medical Center Institutional Review Board.
References
- 1. Anz AW, Bushnell BD, Griffin LP, Noonan TJ, Torry MR, Hawkins RJ. Correlation of torque and elbow injury in professional baseball pitchers. Am J Sports Med. 2010;38(7):1368–1374. [DOI] [PubMed] [Google Scholar]
- 2. Baseball-Reference. Home page. Available at: www.baseball-reference.com. Accessed November 1, 2017.
- 3. Brooks Baseball. Home page. Available at: http://www.brooksbaseball.net/. Accessed November 1, 2017.
- 4. Camp CL, Tubbs TG, Fleisig GS, et al. The relationship of throwing arm mechanics and elbow varus torque: within-subject variation for professional baseball pitchers across 82,000 throws. Am J Sports Med. 2017;45(13):3030–3035. [DOI] [PubMed] [Google Scholar]
- 5. Camp CL, Zajac JM, Pearson DB, et al. Decreased shoulder external rotation and flexion are greater predictors of injury than internal rotation deficits: analysis of 132 pitcher-seasons in professional baseball. Arthroscopy. 2017;33(9):1629–1636. [DOI] [PubMed] [Google Scholar]
- 6. Chalmers PN, Erickson BJ, Ball B, Romeo AA, Verma NN. Fastball pitch velocity helps predict ulnar collateral ligament reconstruction in Major League Baseball pitchers. Am J Sports Med. 2016;44(8):2130–2135. [DOI] [PubMed] [Google Scholar]
- 7. Cohen SB, Valko C, Zoga A, Dodson CC, Ciccotti MG. Posteromedial elbow impingement: magnetic resonance imaging findings in overhead throwing athletes and results of arthroscopic treatment. Arthroscopy. 2011;27(10):1364–1370. [DOI] [PubMed] [Google Scholar]
- 8. DeFroda SF, Kriz PK, Hall AM, Zurakowski D, Fadale PD. Risk stratification for ulnar collateral ligament injury in Major League Baseball players: a retrospective study from 2007 to 2014. Orthop J Sports Med. 2016;4(2):2325967115627126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dewan AK, Chhabra AB, Khanna AJ, Anderson MW, Brunton LM. MRI of the elbow: techniques and spectrum of disease. AAOS exhibit selection. J Bone Joint Surg Am. 2013;95(14):e99. [DOI] [PubMed] [Google Scholar]
- 10. Dillman CJ, Fleisig GS, Andrews JR. Biomechanics of pitching with emphasis upon shoulder kinematics. J Orthop Sports Phys Ther. 1993;18(2):402–408. [DOI] [PubMed] [Google Scholar]
- 11. Erickson BJ, Cvetanovich GL, Bach BRJ, Bush-Joseph CA, Verma NN, Romeo AA. Should we limit innings pitched after ulnar collateral ligament reconstruction in Major League Baseball pitchers? Am J Sports Med. 2016;44(9):2210–2213. [DOI] [PubMed] [Google Scholar]
- 12. Erickson BJ, Gupta AK, Harris JD, et al. Rate of return to pitching and performance after Tommy John surgery in Major League Baseball pitchers. Am J Sports Med. 2014;42(3):536–543. [DOI] [PubMed] [Google Scholar]
- 13. FanGraphs. Home page. Available at: www.fangraphs.com. Accessed November 1, 2017.
- 14. Gutierrez NM, Granville C, Kaplan L, Baraga M, Jose J. Elbow MRI findings do not correlate with future placement on the disabled list in asymptomatic professional baseball pitchers. Sports Health. 2017;9(3):222–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hattori H, Akasaka K, Otsudo T, Hall T, Amemiya K, Mori Y. The effect of repetitive baseball pitching on medial elbow joint space gapping associated with 2 elbow valgus stressors in high school baseball players. J Shoulder Elbow Surg. 2018;27(4):592–598. [DOI] [PubMed] [Google Scholar]
- 16. Jones KJ, Conte S, Patterson N, ElAttrache NS, Dines JS. Functional outcomes following revision ulnar collateral ligament reconstruction in Major League Baseball pitchers. J Shoulder Elbow Surg. 2013;22(5):642–646. [DOI] [PubMed] [Google Scholar]
- 17. Jost B, Zumstein M, Pfirrmann CWA, Zanetti M, Gerber C. MRI findings in throwing shoulders: abnormalities in professional handball players. Clin Orthop Relat Res. 2005;(434):130–137. [DOI] [PubMed] [Google Scholar]
- 18. Kaplan LD, Schurhoff MR, Selesnick H, Thorpe M, Uribe JW. Magnetic resonance imaging of the knee in asymptomatic professional basketball players. Arthroscopy. 2005;21(5):557–561. [DOI] [PubMed] [Google Scholar]
- 19. Keller RA, Mehran N, Marshall NE, et al. Major league pitching workload after primary ulnar collateral ligament reconstruction and risk for revision surgery. J Shoulder Elbow Surg. 2017;26(2):288–294. [DOI] [PubMed] [Google Scholar]
- 20. Kooima CL, Anderson K, Craig JV, Teeter DM, van Holsbeeck M. Evidence of subclinical medial collateral ligament injury and posteromedial impingement in professional baseball players. Am J Sports Med. 2004;32(7):1602–1606. [DOI] [PubMed] [Google Scholar]
- 21. Lesniak BP, Baraga MG, Jose J, Smith MK, Cunningham S, Kaplan LD. Glenohumeral findings on magnetic resonance imaging correlate with innings pitched in asymptomatic pitchers. Am J Sports Med. 2013;41(9):2022–2027. [DOI] [PubMed] [Google Scholar]
- 22. Liu JN, Garcia GH, Conte S, ElAttrache N, Altchek DW, Dines JS. Outcomes in revision Tommy John surgery in Major League Baseball pitchers. J Shoulder Elbow Surg. 2016;25(1):90–97. [DOI] [PubMed] [Google Scholar]
- 23. Makhni EC, Lee RW, Morrow ZS, Gualtieri AP, Gorroochurn P, Ahmad CS. Performance, return to competition, and reinjury after Tommy John surgery in Major League Baseball pitchers: a review of 147 cases. Am J Sports Med. 2014;42(6):1323–1332. [DOI] [PubMed] [Google Scholar]
- 24. Morrey BF, An KN. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med. 1983;11(5):315–319. [DOI] [PubMed] [Google Scholar]
- 25. Schweitzer M, Morrison WB. Arthropathies and inflammatory conditions of the elbow. Magn Reson Imaging Clin N Am. 1997;5(3):603–617. [PubMed] [Google Scholar]
- 26. Silvis ML, Mosher TJ, Smetana BS, et al. High prevalence of pelvic and hip magnetic resonance imaging findings in asymptomatic collegiate and professional hockey players. Am J Sports Med. 2011;39(4):715–721. [DOI] [PubMed] [Google Scholar]
- 27. Spotrac. MLB positional payrolls. Available at: http://www.spotrac.com/mlb/positional/. Accessed November 1, 2017.
- 28. Timmerman LA, Schwartz ML, Andrews JR. Preoperative evaluation of the ulnar collateral ligament by magnetic resonance imaging and computed tomography arthrography: evaluation in 25 baseball players with surgical confirmation. Am J Sports Med. 1994;22(1):26–31. [DOI] [PubMed] [Google Scholar]
- 29. Whiteside D, Martini DN, Lepley AS, Zernicke RF, Goulet GC. Predictors of ulnar collateral ligament reconstruction in Major League Baseball pitchers. Am J Sports Med. 2016;44(9):2202–2209. [DOI] [PubMed] [Google Scholar]
- 30. Wilk KE, Macrina LC, Fleisig GS, et al. Deficits in glenohumeral passive range of motion increase risk of elbow injury in professional baseball pitchers: a prospective study. Am J Sports Med. 2014;42(9):2075–2081. [DOI] [PubMed] [Google Scholar]
- 31. Wright RW, Steger-May K, Klein SE. Radiographic findings in the shoulder and elbow of Major League Baseball pitchers. Am J Sports Med. 2007;35(11):1839–1843. [DOI] [PubMed] [Google Scholar]
- 32. Wymore L, Chin P, Geary C, et al. Performance and injury characteristics of pitchers entering the Major League Baseball draft after ulnar collateral ligament reconstruction. Am J Sports Med. 2016;44(12):3165–3170. [DOI] [PubMed] [Google Scholar]