Abstract
We present a rare case of traumatic facial and vestibulocochlear nerve injury in the internal acoustic canal in the absence of a temporal bone fracture. A 2.5-year-old female presented with sudden-onset left-sided facial paralysis and ipsilateral total hearing loss after being hit by a falling television. High-resolution computed tomography revealed an occipital fracture line that spared the temporal bone and otic capsule. Diagnostic auditory brainstem response testing showed that wave V at 90-db normal hearing level was absent in the left ear. Needle electromyography revealed severe axonal injury. Facial paralysis regressed to House–Brackmann grade IV 9 months after the trauma, and no surgical intervention was scheduled. Traumatic facial and vestibulocochlear nerve injury can occur in the absence of a temporal bone fracture. Thus, careful evaluation of the internal acoustic canal is mandatory if concurrent 7th and 8th cranial nerve paralyses exist with no visible fracture line.
Keywords: Facial nerve, vestibulocochlear nerve, avulsion, facial paralysis, facial nerve injuries
INTRODUCTION
Traumatic injuries constitute the second most common cause of facial nerve palsy worldwide [1]. Traumatic facial nerve palsy usually occurs after a temporal bone fracture, which is most often caused by motor vehicle accidents and falls [2]. In its intratemporal course, the facial nerve enters the fallopian canal, which is situated between the lateral end of the internal acoustic canal and the stylomastoid foramen. Fracture lines involving this canal can cause partial or complete impairment of facial nerve function. Temporal bone fractures are classically described according to the long axis of the petrous bone being classified as longitudinal, transverse, or mixed [3]. Immediate-onset facial paralysis and total sensorineural hearing loss are hallmarks of a transverse fracture involving the otic capsule that transects the facial nerve. Moreover, there is a new classification system based on whether or not the fracture line violates or spares the otic capsule, and it is thought to be a better clinical predictor than the classical classification [4].
Here, we present the case of a patient with immediate-onset facial paralysis and complete deafness caused due to being hit by a falling television. The patient was diagnosed with complete transection of the facial and vestibulocochlear nerve complex in the internal acoustic canal in the absence of a temporal bone fracture. To the best of our knowledge, this is the second such case to be reported in the English-language literature.
CASE PRESENTATION
A 2.5-year-old female presented to our clinic with immediate-onset complete left-sided facial paralysis and total hearing loss due to head trauma caused by a falling television. The accident occurred 1 month prior to the presentation. The patient was referred from another institute for detailed evaluation and surgery, if necessary. Otolaryngologic examination showed House–Brackmann grade VI facial paralysis on the left side. The external auditory canal and tympanic membrane were normal on both sides. Facial nerve tests were not performed at the referring institute. The parents of the patient provided written informed consent.
High-resolution computed tomography (HRCT) showed a non-depressed occipital cranial fracture line that spared the otic capsule and temporal bone (Figure 1). The facial canal was completely intact up to the stylomastoid foramen, and no injury to the facial nerve was detected along its course. Automated auditory brainstem response (ABR) was absent on the left side, and a diagnostic ABR was performed under general anesthesia. Wave V at 90-db normal hearing level was absent and cochlear microphonic was detected in the left ear (Figure 2). The ABR findings and co-occurrence of the 7th and 8th cranial nerve palsies raised suspicions of a retrocochlear pathology. Thus, a 1.5-Tesla magnetic resonance imaging (MRI) was performed, and constructive interference in steady-state sequences using the T2-weighted three-dimensional gradient-echo technique showed a signal intensity difference between the left side and the unaffected right side, as well as adhesion around the facial and vestibulocochlear nerve complex at the fundus of the internal acoustic canal. The reticular contrasting pattern was interpreted as granulation tissue and/or fibrosis caused by traumatic nerve injury considering the clinical findings and history of the patient (Figure 3).
Figure 1. a, b.
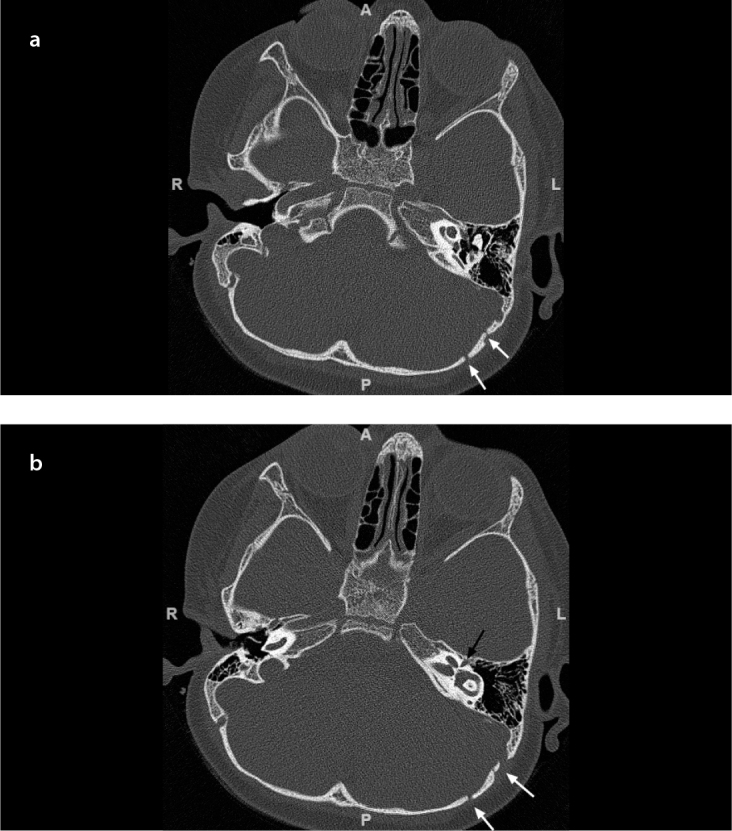
(a) Axial temporal CT section shows no sign of a temporal fracture in the otic capsule. (b) CT section at the level of the geniculate ganglion (black arrow) shows no sign of a temporal fracture line. White arrows depict the occipital fracture lines. CT, computed tomography
Figure 2. a, b.
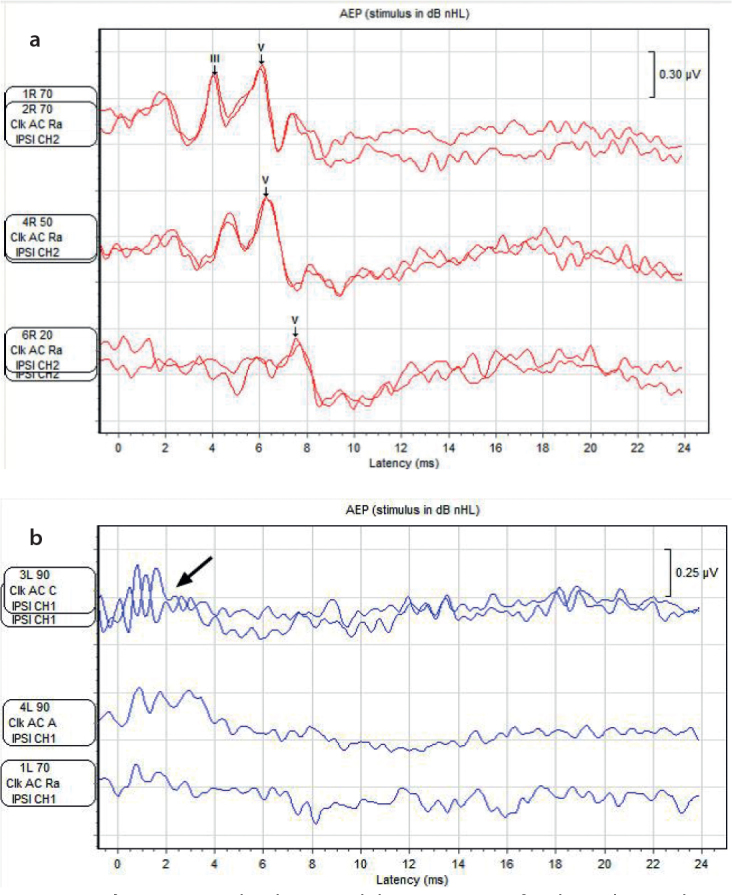
(a) A completely normal diagnostic ABR for the right ear shows waves III and V. (b) Wave V is absent in the left ear. Black arrow indicates the cochlear microphonic. ABR, auditory brainstem response
Figure 3. a, b.
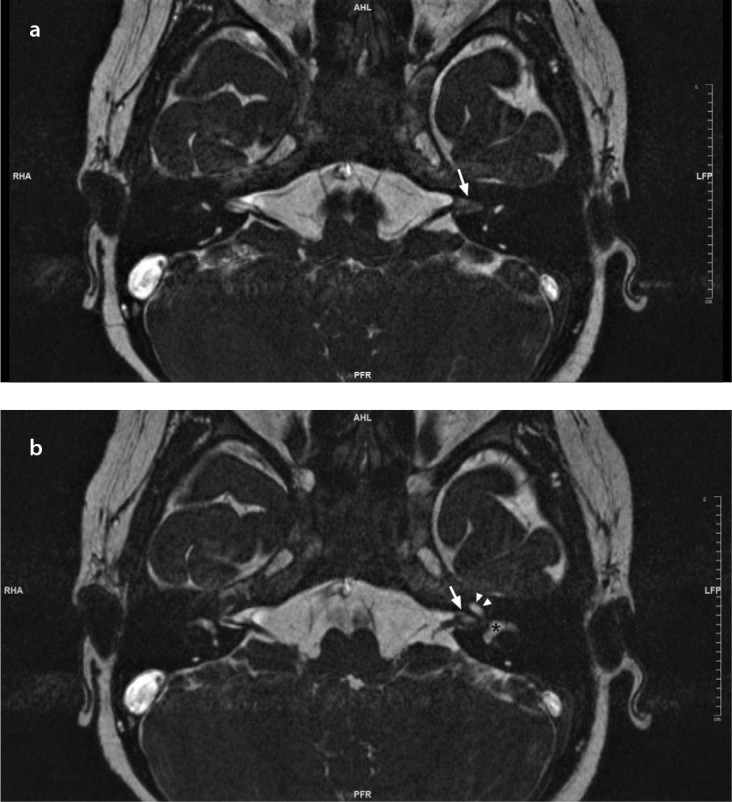
Consecutive T2-weighted axial MRI scans show a difference in the contrast-enhanced signal intensity between the internal acoustic canal on the left side (white arrow) and the right side, indicating fibrosis–granulation tissue caused by traumatic nerve injury. Asterisk indicates the vestibule. Arrowheads indicate the cochlea. MRI, magnetic resonance imaging
Concentric needle electromyography (EMG) of the left orbicularis oris and orbicularis oculi muscles was performed at rest and during voluntary contraction 2 months post-injury. Resting EMG showed denervation potentials (spontaneous fibrillation and positive sharp wave potentials) (Figure 4a). There were no motor unit potentials or reinnervation potentials during voluntary activity. The patient’s injury was graded as severe axonal injury based on these neurophysiological findings. She was scheduled for monthly follow-up to monitor for any signs of spontaneous recovery. Minimal functional recovery of the orbicularis oculi and orbicularis oris muscles was observed 5 months post-injury. The patient’s facial paralysis had regressed to House–Brackmann grade IV at 9 months post-injury. Denervation potentials were determined at rest, as in her previous EMG examination, on her follow-up EMG. Interestingly, during voluntary contraction, polyphasic reinnervation motor unit potentials appeared in her needle EMG reflecting her clinical recovery (Figure 4b). Surgical intervention was not scheduled for the patient because initiation of the spontaneous healing process was observed.
Figure 4. a, b.
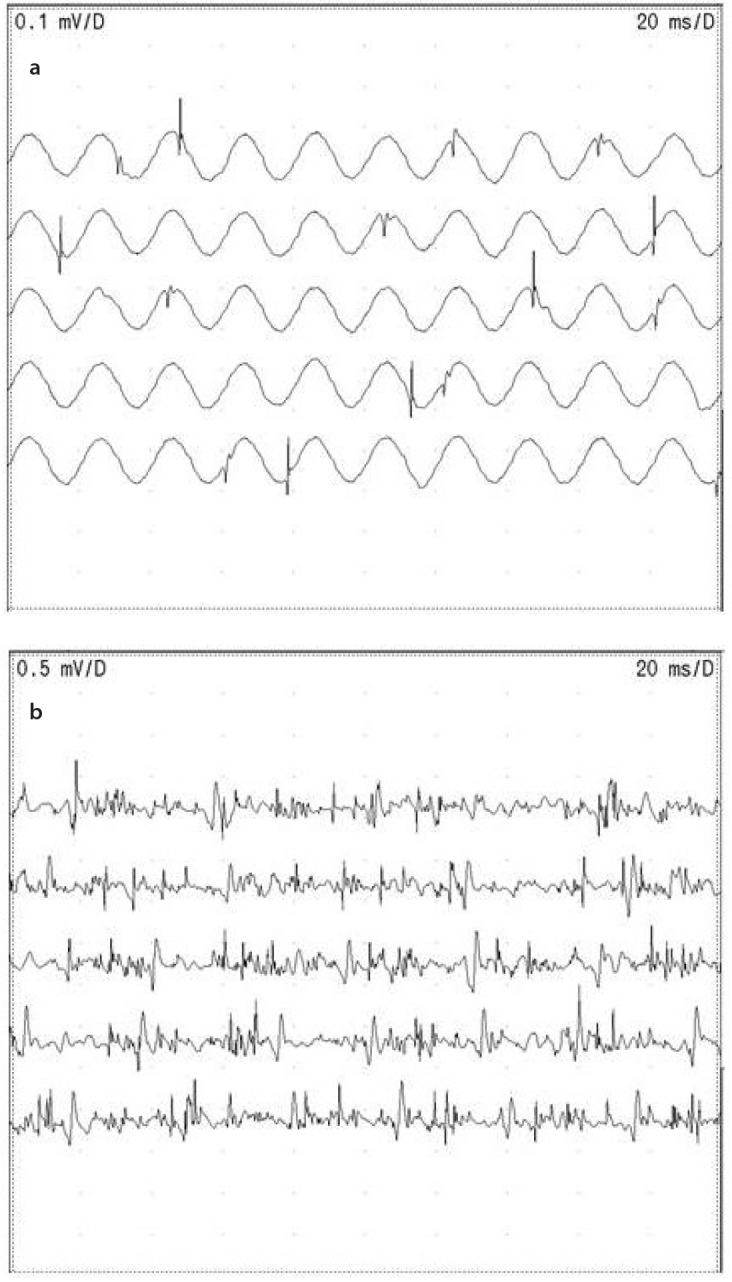
(a) Resting EMG shows the denervation potentials. (b) Voluntary EMG at 9th month follow-up post-injury demonstrates polyphasic reinnervation motor unit potentials. EMG, electromyography
DISCUSSION
Immediate-onset facial paralysis following blunt trauma is most likely associated with nerve transection. Several mechanisms have been proposed to explain the pathophysiology: 1. Temporal fractures involving the fallopian canal and disrupting the facial nerve; 2. Transection of the facial nerve by an adjacent bone spicule; 3. The medially directed vectoral force of the trauma applied to the cranium and brain, leading to avulsion of the nerve [5]. HRCT is adequate for visualizing a temporal fracture line in most cases; however, it may not detect osseous microfractures or bone spicules. Cone beam CT, which has a higher resolution (range: 0.09–0.4-mm slice thickness), might aid in the visualization of microfractures and bone spicules, although it is not available at all institutes. MRI should be used for visualizing nerve integrity, neural ischemia, edema, intraneural hematoma, and possible adjacent dural enhancement. Dural enhancement along the anterior border of the petrous bone, or in the internal acoustic canal, may be an indicator of osseous micro- or macrofractures that cannot be radiologically detected [6].
In the presented case, adjacent dural enhancement was not detected in the internal acoustic canal and the possibility of an unidentified osseous microfracture was excluded. Another possible mechanism for immediate-onset facial paralysis following blunt trauma is transection of the facial nerve by a bone spicule. However, it is unlikely that a bone spicule broke off from its bed in the absence of a temporal fracture in the presented case; moreover, even if we make such an assumption, it would not have been possible for the nerve fibers to reconnect with their conjugate fibers and initiate the regeneration process, as a physical bony obstruction would block the fibers. In the presented case, there were no radiological findings of a temporal fracture line or bone spicule and an initiation of the partial recovery of the facial nerve function was observed.
In the first published case of transection of the facial and vestibulocochlear nerve complex in the internal acoustic canal, it was reported that the facial and vestibulocochlear nerves were avulsed in the internal acoustic canal [5]. Similar to our patient, the patient in the previous pediatric case had experienced blunt trauma during a motor vehicle accident directed toward the ipsilateral occipital region, causing immediate-onset facial and vestibulocochlear nerve paralyses due to injury to the nerve complex in the lateral internal acoustic canal. In the previous case, it was radiologically and surgically observed that both nerves were totally avulsed at the osseous entry point in the fundus of the internal acoustic canal and their proximal ends were medially displaced after the medially directed traction along the nerve bundle. The researchers suggested that because the pediatric cranium is not as rigidly fixed as the adult cranium, due to immaturity of the synchondroses, external forces can mobilize intracranial structures such as the cerebellum and hindbrain medially while displacing the temporal bone outwardly. Thus, the vestibulocochlear and facial nerve complex ruptures, and the proximal fibers get pulled medially. This theory could explain the mechanism of injury in the present case; however, the proximal nerve bundles were not displaced medially, and no significant gap was found between the bundles. This might have happened because the energy associated with a falling television was lower than that associated with a motor vehicle accident in the previous case, and the nerve bundles in the present case fused, initiating the recovery process.
In conclusion, traumatic facial and vestibulocochlear nerve injuries can occur in the absence of a temporal bone fracture. Concurrent palsy of these two nerves in the absence of a temporal bone fracture may indicate an avulsion injury; therefore, the internal acoustic canal must be carefully evaluated in such cases.
Footnotes
Informed Consent: Written informed consent was obtained from the parents of the patient who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – A.E.P., G.P.; Design – A.E.P.; Supervision – M.D.B., L.S.; Resources – G.P., M.D.B.; Materials – G.P., M.D.B.; Data Collection and/or Processing – A.E.P., G.P., F.G.Y.; Analysis and/or Interpretation – A.E.P., G.P., F.G.Y.; Literature Search – A.E.P.; Writing Manuscript –A.E.P.; Critical Review – M.D.B.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985;93:146–7. doi: 10.1177/019459988509300202. [DOI] [PubMed] [Google Scholar]
- 2.Aslan H, Songu M, Eren E, Basoglu MS, Ozkul Y, Ates D, et al. Results of decompression with middle cranial fossa approach or traumatic intratemporal fascial nerve injury. J Craniofac Surg. 2014;25:1305–8. doi: 10.1097/SCS.0000000000000772. [DOI] [PubMed] [Google Scholar]
- 3.Cannon CR, Jahrsdoerfer RA. Temporal bone fractures. Review of 90 cases. Arch Otolaryngol. 1983;109:285–8. doi: 10.1001/archotol.1983.00800190007002. [DOI] [PubMed] [Google Scholar]
- 4.Dahiya R, Keller JD, Litofsky NS, Bankey PE, Bonassar LJ, Megerian CA. Temporal bone fractures: otic capsule sparing versus otic capsule violating clinical and radiographic considerations. J Trauma. 1999;47:1079–83. doi: 10.1097/00005373-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Corrales CE, Monfared A, Jackler RK. Facial and vestibulocochlear nerve avulsion at the fundus of the internal auditory canal in a child without a temporal bone fracture. Otol Neurotol. 2010;31:1508–10. doi: 10.1097/MAO.0b013e3181f0c848. [DOI] [PubMed] [Google Scholar]
- 6.Sartoretti-Schefer S, Scherler M, Wichmann W, Valavanis A. Contrast-enhanced MR of the facial nerve in patients with posttraumatic peripheral facial nerve palsy. AJNR Am J Neuroradiol. 1997;18:1115–25. [PMC free article] [PubMed] [Google Scholar]


