Abstract
OBJECTIVES
The aim of this scoping review was to evaluate existing classifications of surgical procedures of the middle ear and mastoid and find a suitable classification that could serve as an international standard.
MATERIALS and METHODS
Scoping review with a systematic literature search using reference tracking and a syntax including all surgical procedures in mastoid and middle ear surgery and their synonyms. Studies were selected based on inclusion and exclusion criteria.
RESULTS
Eleven reported classifications were included; six of which focused on middle ear surgery, two on mastoid surgery, and three on both. However, none of the classifications included all current surgical procedures of mastoid and middle ear surgery.
CONCLUSION
Many classifications have been proposed for innumerable surgical techniques in middle ear and mastoid surgery. Some are outdated, some are incomplete, most are not widely accepted, and only few correspond with all current surgical techniques.
Keywords: Classification, registry, ear surgery, review, middle ear, mastoid
INTRODUCTION
There are a great variety of surgical techniques for diseases of the middle ear and mastoid bone. In order to have meaningful comparison of surgical outcomes, it is important that surgeons use standardized terminologies to describe their operations.
To date, there is no consensus regarding a standardized categorization of tympanomastoid surgery; however, there are a number of classifications based on historical terminologies. This leads to difficulties in making meaningful comparisons or drawing evidence-based conclusions. An internationally approved classification will make it possible to compare and combine surgical series more effectively. This could help in the development of high level evidence and in the creation of evidence-based guidelines.
Over the years, many classifications and categorizations of the middle ear and mastoid surgery have been proposed. For instance, the one presented by Wullstein in 1956 on tympanoplasty is well known and still used today [1]. Conversely, some recent papers do not use the Wullstein classification and present data which is categorized differently or not categorized at all. This non-standardized fashion of presenting data will impede the conduction of meta-analysis or creation of “big data” to overcome the problem of surgical series and to have a higher level of evidence. The International Otology Outcome Group aims to create a better basis for international outcome reporting which will facilitate international collaboration that can lead to the development of high level evidence in otologic surgery. A starting point is to find a standardized way to describe tympanomastoid procedures. One way to achieve this is by grouping the surgical procedures into distinguishable categories. A good classification system should be user-friendly, accepted by the international communities, and include all common surgical techniques. Ideally, it is flexible enough to be used as future proof because tympanomastoid surgery continues to evolve. Some notable examples of recent development are mastoid obliteration and endoscopic ear surgery. This scoping review was set out to present an overview of the available classifications on tympanomastoid surgery and to evaluate their current usability. The aim was to find a suitable classification that could serve as an international standard. This scoping review comprises a systematic literature search, a thorough coverage of available classifications, and an assessment on its potential to serve as an international standard [2].
METHODS
The approach to this scoping review was conducted according to the Arksey and O’Malley framework [2]. This type of scoping review has a framework that facilitates a comprehensive literature search, a thorough coverage of available literature, and is suited to identify research gaps.
Search Strategy
The search strategy involved searching via electronic databases and reference lists. The electronic database search included Cochrane, PubMed, and Embase and was performed on the March 25, 2018. Keywords used for the search combined various synonyms and types of terminology used for classification and tympanomastoid surgery. Specific types of middle ear and mastoid surgeries were included to maximize the likelihood of capturing all eligible studies. The detailed search syntax can be found in appendix 1.
Selection Criteria
Titles and abstracts were screened; studies that seemed relevant to the research question were read in full text (books and journal papers). When relevance was unclear from the abstract, the study was completely read. Criteria were devised post-hoc because the relevance of the selected studies could be determined more effectively based on increasing familiarity with the literature[2]. To be considered for inclusion, studies had to introduce a new or modified classification of middle ear and/or mastoid surgery. Studies were selected for inclusion after approval of all authors. Exclusion criteria included studies not written in English and those cited less than five times. The number of citations was assessed using Google Scholar Citations because this data source also includes books and reports. Google Scholar was checked to be as accurate as Web of Science (Thompson Reuters) for journal citations. The reference list of all eligible studies was searched for additional studies. With regard to the Arksey and O’Malley [2] framework, eligible studies were not individually assessed on quality.
Data Extraction and Analysis
Information was extracted and recorded as follows: author, year of publication, name and type of classification, original or modified classification, the scope of consensus on the classification (single author, multicenter, and national and international otology societies), number of citations, and a short overview of the classification. A consistent reporting strategy to the overviews was used to avoid potential bias in reporting.
RESULTS
Literature Search and Study Selection
Figure 1 summarizes the review process in a flowchart. The electronic database search identified a total of 2,779 publications. After screening of the titles and abstracts, the full text of 29 studies were reviewed for eligibility. In 13 studies, no clear classification was presented [3–15]. Seven studies were excluded because they were not written in English [16–22] and three studies were excluded due to a low number (<5) of citations [23–25]. Six studies met our criteria and five studies [26–30] were added through reference tracking, resulting in a total of 11 studies that were included in this scoping review [1, 26–35].
Figure 1.
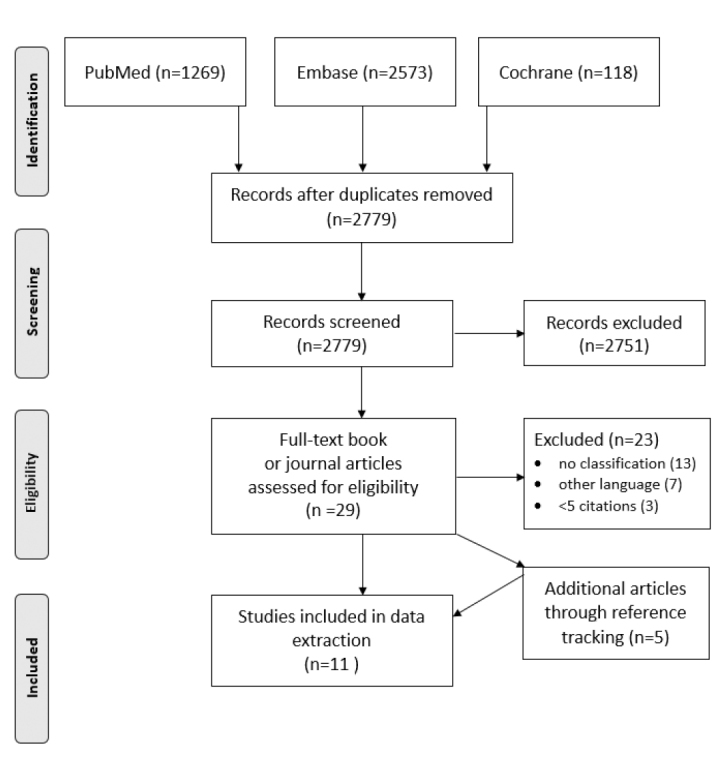
Flowchart with the performed selection process. The literature search was conducted on March 25,-2018.
Study Characteristics
Table 1 summarizes the characteristics of the included studies. Three of the eleven studies included both a middle ear and mastoid surgery classification. The total number of middle ear surgery classifications was nine, of which six solely focused on the middle ear. Five of the middle ear classifications were a modification of the Wullstein classification [1]. One classification consisted solely of ossiculoplasty and another exclusively focused on cartilage tympanoplasty [31, 32]. Mastoid surgery was included in five classifications, which did not include any revisions or modifications of earlier classifications. The oldest classification included was published in 1956 and the newest in 2008. Eight classifications were made by a single author, one was formed by a single center and two by national otology societies [30, 33]. However, no classifications were based on international otologic societies or consensus.
Table 1.
Characteristics and classifications of the 11 included studies (order by year of publication)
| Source | Type of classification | Original or modified classification | Consensus based | Citations |
|---|---|---|---|---|
| Wullstein [1] 1956 | Tympanoplasty | Original | Single author | 365 |
|
| ||||
| Wullstein classification: | ||||
| Type I: Middle ear practically restored to normal; tympanic membrane and middle ear intact. | ||||
| Type II: Middle ear of approximately normal size is tried to preserve in spite of slight defects of the ossicles. | ||||
| Type III: Large defects of the malleus and incus warrant the removal of the ossicular chain and of the epitympanum. The tympanic membrane must be directly connected with the head of the stapes. | ||||
| Type IV: The stapedial footplate is movable, but the crurae are missing. The tympanoplasty reconstructs a middle ear comprising only of the tube and the hypotympanum with sound protection for the round window. | ||||
| Type V: The stapedial footplate is fixed and a fenestra novovalis is necessary. | ||||
|
| ||||
| Lierle [30] 1965 | Tympanoplasty Mastoidectomy | Original | American otologic society | 17 |
|
| ||||
| Classification of the common operations performed in surgery for chronic ear infection: | ||||
| A: Radical or modified radical mastoidectomy | D: Tympanoplasty without mastoidectomy | |||
| B: Mastoid obliteration operation | E: Tympanoplasty with mastoidectomy | |||
| C: Myringoplasty | ||||
|
| ||||
| Farrior [26] 1971 | Tympanoplasty | Modified Wullstein classification | Single author | 19 |
|
| ||||
| Classification of tympanoplasty type III and IV (modification of Wullstein): | ||||
| Type IV: | No columella | Type III: | Drums on stapes | |
| Type IV: IG | Incus graft | Type III: IG | Incus graft | |
| Type IV: MG | Malleus graft | Type III: IGM | Incus graft to malleus | |
| Type IV: BG | Bone graft | Type III: MR | Malleus repositioned | |
| Type IV: C SS | Cartilage graft with stainless steel | Type III: MG | Malleus graft | |
| Type IV: HG MIS | Homograft drum with malleus, incus and stapes | Type III: BG | Bone graft | |
| Type III: SS MS | Stainless steel malleus to stapes | |||
|
| ||||
| Bellucci [27] 1973 | Tympanoplasty | Modified Wullstein classification | Single author | 87 |
|
| ||||
| Tympanoplasty: A dual classification (modification of Wullstein): | ||||
| Bellucci classification Pre-Operative. | Wullstein classification Post-operative. | |||
| Group I: Good prognosis. Ear is stabilized for long period. | Type I: Ossicles intact. Middle ear function nearly normal. | |||
| Group II: Fair prognosis. Stabilized but discharges during URI. | Type II: Same as type I but with minor ossicular defects. | |||
| Alternates dry and wet. | Type III: Severe ossicular defects. Columella. | |||
| Group III: Poor prognosis persistent discharge. No periods of quiescence. Mastoiditis. | Stapes arch intact. | |||
| Type IV: Stapes arch absent. Cavum minor. | ||||
| Group IV: Very poor prognosis. Chronic discharge. | Footplate exposed. | |||
| Nasopharyngeal malformations. | Type V: Fixed stapes footplate fenestration. Cavum minor. | |||
|
| ||||
| Pratt [34] 1974 | Tympanoplasty Mastoidectomy | Modified Wullstein classification | Single author | 5 |
|
| ||||
| Modified Wullstein and Farrior classification by adding a sixth type of tympanoplasty and describing how the mastoid was managed: | ||||
| Type VI: The removal of the stapes footplate | ||||
| M: Mastoidectomy | M1: Modified radical mastoidectomy | |||
| M2: Simple mastoidectomy with atticoantrotomy | M3: The same as M2 plus a posterior tympanotomy | |||
| M4: The reconstruction of the posterior canal | M5: Radical mastoidectomy | |||
|
| ||||
| Marres [35] 1985 | Mastoidectomy | Original | Single author | 5 |
|
| ||||
| Management of the mastoid, UDT classification: | ||||
| Surgical technique | Surgical region | |||
| U: Canal wall up | I: Attic | III: Tip of the mastoid | ||
| D: Canal wall down | II: Antrum | IV: Area of the posterior tympanotomy | ||
|
| ||||
| Tos [28] 1993 | Mastoidectomy | Original | Single author | 233 |
|
| ||||
| Tos subclassification: | ||||
| Canal wall up | Canal wall down | |||
| 1. Simple/ cortical / complete / Schwartze’s mastoidectomy | Atticotomy | |||
| 2. Classic intact canal wall mastoidectomy / combined approach tympanoplasty (CAT) | Atticoantrotomy | |||
| Radical mastoidectomy | ||||
| Modified radical mastoidectomy / Bondy’s procedure | ||||
| Retrograde mastoidectomy | ||||
|
| ||||
| McGee and Hough [31] 1999 | Ossiculoplasty | Original | Single center | 32 |
|
| ||||
| Classification of ossicular reconstruction: | ||||
| Pathology | Surgical technique | |||
| Type I: Incudostapedial joint separation | Connecting the head of the stapes with the handle of the malleus | |||
| Type II: Long process of incus not connected to the head of the stapes. Crural arch of the stapes is missing | Building a connective bridge from the footplate of the stapes to the handle of the malleus | |||
| Type III: Same defect as type II but also has the head of the stapes removed | Same reconstruction as type II but with the sealing of the open oval window with a perichondial graft | |||
| Type IV A: Malleus and incus are missing but the stapes is still present | Replacing the malleus with a bone graft shaft medial to the tympanic membrane | |||
| Type IV B: Malleus and incus are missing and tympanic membrane is perforated | Same as type IV A and the tympanic membrane is reconstructed with fascia | |||
| Type V A: Malleus handle, the incus, and stapedial arch are all missing | Same as type IV A, except that the bone graft from the handle of the malleus must reach to the stapedial footplate | |||
| Type V B: Pathology is the same as type V A, but tympanic membrane is perforated | Same as type V A but in addition the tympanic membrane must be reconstructed with fascia | |||
|
| ||||
| Nadol and McKenna [29] 2005 | Tympanoplasty | Modified Wullstein classification | Dual center | 105 |
|
| ||||
| Nadol and Schuknecht modification of the Wullstein classification: | ||||
| Type I: Myringoplasty (intact and mobile ossicular chain) | ||||
| Type II: Use of prosthesis to connect a discontinuity between the long process of incus and stapes head | ||||
| Type III: Subdivided into three categories: | ||||
| Stapes collumela: placement of TM graft on the stapes head | ||||
| Minor collumela: strut from stapes head to manubrium / TM | ||||
| Major collumela: strut from stapes footplate to manubrium / TM | ||||
|
| ||||
| Kim [33] 2007 | Tympanoplasty Mastoidectomy | Original with Wullstein classification | Korean otologic society | 22 |
|
| ||||
| Standardized classification system for middle ear surgery: | ||||
| Type T0: Tympanic membrane reconstruction with no hearing gain | Extraneous procedures | Concurrent procedures | ||
| Type T1–T4: Same as original Wullstein classification | Simple mastoidectomy | Canaloplasty | ||
| Si (interposition over stapes head) | Modified radical mastoidectomy | Atticotomy | ||
| Sc (columella over stapes head) | Radical mastoidectomy | Mastoidotomy | ||
| Fi (interposition over stapes footplate) | Exploratory tympanotomy | Attic reconstruction | ||
| Fc (columella over stapes footplate) | Canal wall reconstruction | |||
| Mastoid obliteration | ||||
| Mastoidectomy | Intact bridge technique | |||
| Canal wall up mastoidectomy | ||||
| Canal wall down mastoidectomy | ||||
|
| ||||
| Tos [32] 2008 | Cartilage tympanoplasty | Original classification | Single author | 67 |
|
| ||||
| The 23 known cartilage tympanoplasty methods are classified in six main groups: | ||||
| Group A: Cartilage tympanoplasty with palisades, stripes, and slices. The eardrum is reconstructed by full thickness pieces of cartilage with attached perichondrium of the ear canal side. | ||||
| Group B: Cartilage tympanoplasty with foils, thin plates, and thick plates, not covered with the perichondrium. | ||||
| Group C: Tympanoplasty with cartilage-perichondrium composite island grafts. The perichondrium flap suspends or fixates the cartilage. | ||||
| Group D: Tympanoplasty with special total pars tensa cartilage-perichondrium composite grafts. All three methods are used to close a total perforation, but differ from each. | ||||
| Group E: Cartilage-perichondrium composite island grafts tympanoplasty for anterior, inferior, and subtotal perforations. | ||||
| Group F: Special cartilage tympanoplasty methods: The cartilage disc is placed under the perforation, the perichondrium onto the denuded eardrum remnant. | ||||
URI: upper respiratory infection; TM: Tympanic membrane
Classification overview
The Wullstein classification [1] describes the degree of damage found in the middle ear and the method of reconstruction. Five modification proposals for this classification have been included in this scoping review. In 1971, Farrior [26] introduced a classification, which preserves the Wullstein classification, and included a scheme for describing some ossicle modifications. Bellucci [27] proposed a dual classification comprising a nomenclature of the stability of the ear against infection and the original Wullstein classification. Pratt [34] modified the Wullstein classification by introducing a sixth type of tympanoplasty comprising the removal of the footplate of the stapes and describing how the mastoid was managed. The Nadol and Schuknecht [29] modification included the removal of types IV and V and the subdivision of type III into three categories: stapes columella, minor columella, and major columella. In 2007, Kim [33] introduced the most recent modification of Wullstein by adding type 0, representing tympanic membrane reconstruction with no hearing gain, and by removing type V. This classification also comprises mastoidectomy, extraneous procedures, and concurrent procedures, such as obliteration. Lierle [30] classified the most common surgeries performed for chronic ear infections into five types, including both tympanoplasty and mastoid surgery. Marres [35] introduced a mastoidectomy classification comprising the performed technique (canal wall up or canal wall down) and a division of the surgical region of the attic and mastoid into four different areas. In 1993, Toss [28] proposed a mastoidectomy classification comprising the surgical technique (canal wall up or canal wall down) and further subdivisions of the technique. McGee [31] proposed a dual classification of ossicular reconstruction comprising a description of the pathology (subdivided in five types) and the associated surgery. Lastly, Tos [32] proposed a cartilage tympanoplasty classification by categorizing the 23 known cartilage tympanoplasty methods into six main groups.
DISCUSSION
This scoping review was intended to present an overview of the existing classifications of middle ear and mastoid surgery. The classifications were evaluated with regard to their applicability, and the aim was to find a suitable classification that could serve as an international standard.
The literature search identified 11 classifications of middle ear and mastoid surgery published in journals and books from 1956 to 2008. Six classifications focused on middle ear surgery, two on mastoid surgery, and three on both (Table 1).
An internationally approved classification should be well accepted, unambiguous, and encompass all common and current surgical techniques.
The number of citations of each classification roughly reveals the number of studies that used this classification to report their data, to give an idea of international “acceptance.” Six out of eleven classifications were cited less than 20 times and only two were based on national consensus [30, 33]. None were based on international consensus. The middle ear surgery classification of Wullstein and the mastoid classification of Tos are the most cited and still used today [1, 28]. However, these two classifications could not be directly translated into a broadly accepted international classification. The Wullstein classification describes five methods to reconstruct the middle ear and has formed the basis of modification classifications promoted by others [26, 27, 29, 33, 34]. The classification includes many good points but does not accommodate new surgical options, such as a prosthesis from the footplate to the tympanic membrane in the presence of the stapes suprastructure[36]. Even in the newer Wullstein modifications [29, 33] some middle ear reconstructions were not included, such as prosthesis from incus/malleus to vestibule as in stapes surgery. Another popular classification is by Tos on mastoid procedures [28]. Tos deliberately maintained the historical terminologies of simple mastoidectomy (cortical, complete, Schwartze) for translational purpose. It also concludes five categories for a canal wall down procedure (refer to Table 1), one of the categories comprises two techniques (modified radical mastoidectomy and Bondy’s procedure). However, it is unclear if a (modified) radical mastoidectomy truly differs from a retrograde mastoidectomy, other than the approach to surgery.
Many of the classifications were incomplete in their categorization of surgical techniques and miss out some of the current surgical approaches. For instance, mastoid obliteration was described in only two classifications, [30, 33] and techniques that are often used during an endoscopic approach (atticotomy and atticoantrotomy) are missing in some mastoid classifications [30, 35]. In addition, some classifications only focused on specific procedures, such as the Tos’s classification on cartilage tympanoplasty [32]. The Korean Otologic Society has presented a classification, which is close to a comprehensive overview of existing terminologies, yet it has limited structure [33]. For example, a mastoidectomy is labeled either “canal wall up” or “canal wall down,” but missed out on other additional or optional procedures.
Many classifications identified in this study used historical or ambiguous terminologies that are open to personal interpretation and do not correspond with the current ICD-10 nomenclature. “Tympanoplasty” is used in Wullstein for myringoplasty as well as for ossicular chain reconstruction, which leads to confusion among other classifications in which “tympanoplasty” is used only for ossicular chain procedures and “myringoplasty” is separately mentioned [1, 30]. Bellucci used the terms minor- or severe ossicular defect, with further definition missing [27]. Other terms were outdated, such as “cavum minor,” created by a medialized tympanic membrane [27] and “fenestra novovalis [1].” Some terms are new, such as “mastoidotomy” in the same classification as “mastoidectomy” and “atticotomy [33].”
In the classification suggested by Pratt [34], there are five types of mastoidectomy, but strangely enough, one of them is not a mastoidectomy but a type of reconstruction (reconstruction of the posterior wall). Classifying both procedures with the same abbreviation (M) seems illogical as both techniques could be performed in the same procedure.
With regard to the above limitations, the authors could not identify an existing classification that could serve as an international standard. The international otologic society needs to start an international consensus project on the classification of middle ear and mastoid surgery. This could aid international collaboration and greatly improve evidence-based clinical research to create more “big” data to improve surgical outcomes, and facilitate international consensus and evidence for guidelines.
CONCLUSION
Many classifications have been proposed for innumerable surgical techniques in middle ear and mastoid surgery. Some are ambiguous, some are incomplete, most are not widely accepted and only few correspond with most of the current surgical techniques. There is no single classification that could meet what is currently needed to start an international outcome comparison for middle ear and mastoid surgery.
Appendix 1. Search was performed on the 25th of March
| Database | Search syntax | Hits |
|---|---|---|
| Cochrane | “classification”:ti,ab,kw or “definition”:ti,ab,kw or “terminology”:ti,ab,kw or “nomenclature”:ti,ab,kw or “categorization”:ti,ab,kw or “grade”:ti,ab,kw or “grading” or “theory” AND “mastoid”:ti,ab,kw or “tympanic membrane”:ti,ab,kw or “ear”:ti,ab,kw or “tympanoplasty”:ti,ab,kw or “myringoplasty”:ti,ab,kw or “stapes”:ti,ab,kw or “tympanic”:ti,ab,kw or “otology”:ti,ab,kw or “otologic”:ti,ab,kw or “tympanomastoid”:ti,ab,kw or “mastoidectomy”:ti,ab,kw or “stapedotomy”:ti,ab,kw or “stapedectomy”:ti,ab,kw or “ossiculoplasty”:ti,ab,kw or “atticotomy”:ti,ab,kw or “petrosectomy”:ti,ab,kw or “tympanotomy”:ti,ab,kw AND “surgery”:ti,ab,kw or “procedure”:ti,ab,kw or “surgical”:ti,ab,kw | 118 |
| PubMed | (((((((((((classification[MeSH Terms]) OR definition[Title/Abstract]) OR terminology[Title/Abstract]) OR nomenclature[Title/Abstract]) OR categorization[Title/Abstract]) OR grade[Title/Abstract]) OR grading[Title/Abstract]) OR theory[Title/Abstract]) OR classification[Title/Abstract])) AND (((((((((((((((((((((mastoid[MeSH Terms]) OR tympanic membrane[MeSH Terms]) OR ear[MeSH Terms]) OR tympanoplasty[MeSH Terms]) OR myringoplasty[MeSH Terms]) OR stapes[MeSH Terms]) OR mastoid[Title/Abstract]) OR tympanic[Title/Abstract]) OR ear[Title/Abstract]) OR otology[Title/Abstract]) OR otologic[Title/Abstract]) OR tympanomastoid[Title/Abstract]) OR myringoplasty[Title/Abstract]) OR tympanoplasty[Title/Abstract]) OR stapedotomy[Title/Abstract]) OR stapedectomy[Title/Abstract]) OR ossiculoplasty[Title/Abstract]) OR mastoidectomy[Title/Abstract]) OR atticotomy[Title/Abstract]) OR petrosectomy[Title/Abstract]) OR tympanotomy[Title/Abstract])) AND (((Surgery[Title/Abstract]) OR procedure[Title/Abstract]) OR surgical[Title/Abstract]) | 1269 |
| EMBASE | ((‘classification’/exp OR ‘definition’:ti,ab OR ‘terminology’:ti,ab OR ‘nomenclature’:ti,ab OR ‘classification’:ti,ab OR ‘categorization’:ti,ab OR ‘grade’:ti,ab OR ‘grading’:ti,ab OR ‘theory’/exp OR theory) AND (‘surgery’:ti,ab OR ‘procedure’:ti,ab OR ‘surgical’:ti,ab) AND (‘mastoid’/exp OR ‘eardrum’/exp OR ‘ear’/exp OR ‘tympanoplasty’/exp OR ‘myringoplasty’/exp OR ‘stapes’/exp OR ‘mastoid’:ti,ab OR ‘tympanic’:ti,ab OR ‘ear’:ti,ab OR ‘otology’:ti,ab OR ‘otologic’:ti,ab OR ‘tympanomastoid’:ti,ab OR ‘myringoplasty’:ti,ab OR ‘tympanoplasty’:ti,ab OR ‘stapedotomy’:ti,ab OR ‘stapedectomy’:ti,ab OR ‘ossiculoplasty’:ti,ab OR ‘mastoidectomy’:ti,ab OR ‘atticotomy’:ti,ab OR ‘petrosectomy’:ti,ab OR ‘tympanotomy’:ti,ab)) | 2573 |
Footnotes
This study was presented at the 31st Politzer Society Meeting & Global Otology Research Forum, February 23, 2018, Las Palmas de Gran Canarias, Spain.
Peer-review: Externally peer-reviewed.
Author contributions: Concept – P.M., P.K., F.Z., M.Y.; Design - P.M., P.K., F.Z.,; Supervision - P.M., M.Y..; Resource - P.K., F.Z..; Materials – P.M., P.K., F.Z., X.X.; Data Collection and/or Processing - P.K., F.Z.,; Analysis and/or Interpretation - P.M., P.K., F.Z.,; Literature Search - P.K., F.Z.; Writing -P.M., P.K., F.Z., M.Y.; Critical Reviews - P.M., M.Y.
Conflict of Interest: The authors have no conflict of interest to declare.
You can reach the appendix of this article at https://doi.org/10.5152/10.5152/iao.2018.5570
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Wullstein H. Theory and practice of tympanoplasty. Laryngoscope. 1956;66:1076–93. doi: 10.1288/00005537-195608000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 3.Paparella MM, Froymovich O. Surgical advances in treating otitis media. Ann Otol Rhinol Laryngol Suppl. 1994;163:49–53. doi: 10.1177/00034894941030S514. [DOI] [PubMed] [Google Scholar]
- 4.Karkanevatos A, De S, Srinivasan VR, Roland NJ, Lesser TH. Day-case myringoplasty: five years’ experience. J Laryngol Otol. 2003;117:763–5. doi: 10.1258/002221503770716160. [DOI] [PubMed] [Google Scholar]
- 5.Sanna M, Fois P, Pasanisi E, Russo A, Bacciu A. Middle ear and mastoid glomus tumors (glomus tympanicum): an algorithm for the surgical management. Auris Nasus Larynx. 2010;37:661–8. doi: 10.1016/j.anl.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 6.Bellucci RJ. A guide for stapes surgery based on a new surgical classification of otosclerosis. Laryngoscope. 1958;68:741–59. doi: 10.1288/00005537-195804000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Zollner F. The principles of plastic surgery of the sound-conducting apparatus. J Laryngol Otol. 1955;69:637–52. doi: 10.1017/S0022215100051240. [DOI] [PubMed] [Google Scholar]
- 8.Goycoolea MV. Mastoid and tympanomastoid procedures in otitis media: classic mastoidectomy (simple, modified, and radical) and current adaptations; open-cavity, closed-cavity, and intact-bridge tympanomastoidectomy. Otolaryngol Clin North Am. 1999;32:513–23. doi: 10.1016/S0030-6665(05)70149-3. [DOI] [PubMed] [Google Scholar]
- 9.Indorewala S. The anterior tympanotomy. Indian J Otolaryngol Head Neck Surg. 1997;49:122–4. doi: 10.1007/BF03023787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duckert LG, Makielski KH, Helms J. Management of anterior epitympanic cholesteatoma: expectations after epitympanic approach and canal wall reconstruction. Otol Neurotol. 2002;23:8–13. doi: 10.1097/00129492-200201000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Kim CW, Oh JI, Choi KY, Park SM, Park MI. A technique for concurrent procedure of mastoid obliteration and meatoplasty after canal wall down mastoidectomy. Auris Nasus Larynx. 2012;39:557–61. doi: 10.1016/j.anl.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 12.Anschuetz L, Presutti L, Marchioni D, Bonali M, Wimmer W, Villari D, et al. discovering middle ear anatomy by transcanal endoscopic ear surgery: a dissection manual. J Vis Exp. 2018;(131) doi: 10.3791/56390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bellucci RJ. Selection of cases and classification of tympanoplasty. Otolaryngol Clin North Am. 1989;22:911–26. [PubMed] [Google Scholar]
- 14.da Costa SS, Alves de Souza LC, Ribeiro de Toledo Piza M. The flexible endaural tympanoplasty: pathology-guided, pathogenesis-oriented surgery for the middle ear. Otolaryngol Clin North Am. 1999;32:413–41. doi: 10.1016/S0030-6665(05)70143-2. [DOI] [PubMed] [Google Scholar]
- 15.Nankivell PC, Pothier DD. Surgery for tympanic membrane retraction pockets. Cochrane Database Syst Rev. 2010:CD007943. doi: 10.1002/14651858.CD007943.pub2. [DOI] [PubMed] [Google Scholar]
- 16.Alberty J, Franz D. ENT relevant changes in the German OPS procedure classification system for 2006. Laryngorhinootologie. 2006;85:435–40. doi: 10.1055/s-2006-925196. [DOI] [PubMed] [Google Scholar]
- 17.Ramirez Camacho R, Trinidad A, Vicente J, Herrero J. Tympanosclerosis. I: proposed anatomical-surgical classification. Acta Otorrinolaringol Esp. 1999;50:6–8. [PubMed] [Google Scholar]
- 18.Novotny Z. Nomenclature of middle-ear surgery. Cesk Otolaryngol. 1976;25:241–5. [PubMed] [Google Scholar]
- 19.Musebeck K. Classification of tympanomastoidoplasty. Relationship between the course of chronic otitis media and restorative surgery. Z Laryngol Rhinol Otol. 1970;49:212–27. [PubMed] [Google Scholar]
- 20.Savic D, Djeric D, Jesic S. Proposal for the surgical classification of chronic purulent inflammatory processes in the middle ear. Srp Arh Celok Lek. 1986;114:65–79. [PubMed] [Google Scholar]
- 21.Novotný Z. Nomenclature of tympanoplastic and stapes surgery (author’s transl) Laryngol Rhinol Otol (Stuttg) 1976;55:551–5. [PubMed] [Google Scholar]
- 22.Moryama H, Yamamoto E, Yuasa E. Classification and nomenclature of ossicular reconstruction (2000) Otology Japan. 2001;11:64–8. [Google Scholar]
- 23.Farrior JB. XXXII Wherry Memorial Lecture. The ear surgeon of tomorrow. Tympanomastoidectomy techniques and classification. Trans Sect Otolaryngol Am Acad Ophthalmol Otolaryngol. 1977;84:15–37. [PubMed] [Google Scholar]
- 24.Cohen MS, Basonbul RA, Barber SR, Kozin ED, Rivas AC, Lee DJ. Development and validation of an endoscopic ear surgery classification system. Laryngoscope. 2018;128:967–70. doi: 10.1002/lary.26802. [DOI] [PubMed] [Google Scholar]
- 25.Preobrazhensky YB. Some suggestions on tympanoplasty classification. Arch Otolaryngol. 1963;78:766–9. doi: 10.1001/archotol.1963.00750020782006. [DOI] [PubMed] [Google Scholar]
- 26.Farrior JB. Classification of tympanoplasty. Arch Otolaryngol. 1971;93:548–50. doi: 10.1001/archotol.1971.00770060850002. [DOI] [PubMed] [Google Scholar]
- 27.Bellucci RJ. Dual classification of tympanoplasty. Laryngoscope. 1973;83:1754–8. doi: 10.1002/lary.5540831102. [DOI] [PubMed] [Google Scholar]
- 28.Tos M. Manual of middle ear surgery. Georg Thieme Stuttgart; 1993. [Google Scholar]
- 29.Nadol JB, McKenna MJ. Surgery of the ear and temporal bone. Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 30.Lierle DM. Standard Classification for Surgery of Chronic Ear Infection. I. Of Technical Procedures in Surgery for Chronic Ear Infection. II. Of Gross Pathology Found at Such Operations. III. For Reporting of Postoperative Results of Surgical Procedures Mentioned. Arch Otolaryngol. 1965;81:204–5. doi: 10.1001/archotol.1965.00750050211018. [DOI] [Google Scholar]
- 31.McGee M, Hough JV. Ossiculoplasty. Otolaryngol Clin North Am. 1999;32:471–88. doi: 10.1016/S0030-6665(05)70146-8. [DOI] [PubMed] [Google Scholar]
- 32.Tos M. Cartilage tympanoplasty methods: proposal of a classification. Otolaryngol Head Neck Surg. 2008;139:747–58. doi: 10.1016/j.otohns.2008.09.021. [DOI] [PubMed] [Google Scholar]
- 33.Kim HJ. A standardized database management of middle ear surgery in Korea. Acta Otolaryngol Suppl. 2007:54–60. doi: 10.1080/03655230701624871. [DOI] [PubMed] [Google Scholar]
- 34.Pratt LL. Surgical classification for chronic otitis media. Laryngoscope. 1974;84:1388–96. doi: 10.1288/00005537-197408000-00014. [DOI] [PubMed] [Google Scholar]
- 35.Marres E. Surgery and Pathology of the Middle Ear. Springer; 1985. Management of the mastoid—The UDT-system; a new classification in ear surgery; pp. 58–61. [Google Scholar]
- 36.Vincent R, Sperling NM, Oates J, Osborne J. Ossiculoplasty with intact stapes and absent malleus: the silastic banding technique. Otol Neurotol. 2005;26:846–52. doi: 10.1097/01.mao.0000185068.50575.92. [DOI] [PubMed] [Google Scholar]


