Abstract
OBJECTIVES
The natural history of tympanic membrane retraction is unpredictable. To obtain prognostic information for guiding surveillance and treatment, a cohort of children with retraction from cleft palate were prospectively followed for over 5 years.
MATERIALS and METHODS
This was a prospective observational study at a tertiary academic institution. Children with pars tensa retraction were selected from a cohort of 143 children with cleft palate. Thirty-seven ears were assessed with otoendoscopic image capture and audiometry at a median age of 9 years and reassessed at a median follow-up interval of 6.4 years. The severity of tympanic membrane retraction in the serial images of each ear was compared by four pediatric otolaryngologists blinded to the dates of the images.
RESULTS
Initially, 19/37 retractions (51%) demonstrated contact with the incus and/or promontory. Follow-up images were rated as stable (n=16) or better (n=12) for 28/37 retractions (76%). Of the nine retractions that became more extensive, two developed cholesteatoma (5% of the total). No ossicular erosion developed in ears without cholesteatoma. Conductive hearing loss (4-tone average air-bone gap >25 decibels hearing level) was initially present in five ears, worsened in one, and normalized without intervention in others. No ears with initial normal hearing developed hearing loss.
CONCLUSION
Most tympanic membrane retractions remained stable or improved over time in this cohort of children who were at a risk of persistent eustachian tube dysfunction. Clinically significant progression occurred infrequently, justifying the conservative approach taken to manage these retractions. Such data are necessary to weigh the potential benefit of preventive intervention over observation.
Keywords: Eustachian tube, middle ear, cleft palate, otitis media, chronic otitis media, conductive hearing loss
INTRODUCTION
The prevalence of tympanic membrane (TM) retraction in children has been reported to be 8%–10%, with most cases described as mild [1]. While some retractions are reflective of a transient negative pressure state in the middle ear, others become chronic. In pediatric patients, most retractions arise from the pars tensa, as opposed to the pars flaccida [2, 3]. When pars tensa retractions worsen, adherence to the medial tympanic wall and incus may occur. Once a retraction establishes contact with the ossicular chain, concern arises for the development of permanent hearing loss. However, little is known about the incidence of permanent hearing loss in such retraction cases. Similarly, the risk of cholesteatoma formation from a pars tensa retraction remains to be clarified. As such, our current understanding of when and why to operate on retracted TMs is based more on assumptions than on actual evidence.
To investigate the natural history of this poorly understood pathology, a cohort of children with TM retraction was followed over time. All were previously identified during a cross-sectional analysis of a consecutive series of children with cleft palate [3]. This sample was selected because of the higher risk for chronic retraction and sequelae, including hearing loss and cholesteatoma, in the setting of cleft palate [4–7].
MATERIALS and METHODS
Approval for this study was granted by the institution’s Research Ethics Board. Potential study participants were recruited from a cohort of 143 children with cleft palate. All the children had been evaluated with otoendoscopic imaging, audiometry, and tympanometry and were monitored for chronic ear disease according to standard clinical care processes [3]. This typically involved routine 5-year follow-up for normal ears, more frequent observation of retracted TMs according to severity, and operative intervention only for symptomatic middle ear effusions, perforation, or cholesteatoma. All the children in whom retraction of the pars tensa (n=76 ears) had been identified on initial assessment were targeted for prospective follow-up. Most were invited to participate in their routine visits at approximately 5 years after the initial evaluation. Those who had been lost to follow-up (e.g., after graduation to adult services) were contacted and invited to revisit the clinic for evaluation. For patients who could not be reached, data from their last clinic follow-up were used.
Following written consent from the child or caregiver to participate, otoendoscopic imaging was performed by either the senior author or a pediatric otolaryngology fellow. TMs were assessed with 4 or 2.7 mm 0° otoendoscopes, which were positioned and focused to include a view of the entire TM. If necessary, microdebridement was performed to obtain a clear view. Digital images were displayed on a dedicated computer and saved in a secure networked drive. During the same visit, pure tone audiometry and tympanometry were completed. An interval history was also obtained, and any otologic surgery after the initial assessment was noted. For patients who underwent otologic surgery, images and audiometric data from the clinic visit just prior to the surgery were used in the analysis to ensure that no surgical intervention occurred between the visits during which the images were captured.
Image pairs were later created for each retracted TM, with one image extracted from the initial study and second from the reassessment. A study number was assigned to each pair, and all the identifying information was removed. The image pairs were then compiled into a PowerPoint (Microsoft, Redmond, WA, USA) presentation for review. The order of the side-by-side images (initial vs. follow-up, follow-up vs. initial) was randomized. The PowerPoint presentation was assessed on two separate occasions (>1 week apart) by four pediatric otolaryngologists, all of whom had a subspecialty focus in otology. Each reviewer was blinded to the order of the images. Acknowledging that the application of traditional staging systems to TM image review has poor reliability, reviewers were not asked to stage the retractions [3, 8]. Instead, they were instructed to identify which pars tensa appeared worse overall and which appeared worse with respect to each of the following clinically relevant variables: 1) size (surface area of the retraction), 2) visibility of edges and depth, 3) contact with promontory, 4) contact with incus or stapes or both, 5) ossicular erosion, and 6) cleanliness. If there was no appreciable difference or any of the aforementioned variables was not present in any image, then reviewers could select “no difference.”
The primary outcome measure was evaluated based on whether the pars tensa became more or less retracted overall. For data analysis, the study code was broken to determine whether retractions were graded as worse, better, or unchanged over time. The majority of assessments across the four reviewers were used to determine the overall change in appearance. In the event of a 2–2 split, the retraction was considered stable. To facilitate statistical analysis, retractions rated as better or stable were grouped together. This grouping was justified by the lack of a distinction between the two assessments with respect to clinical decision-making. Intra- and inter-rater Kappa statistics with 95% confidence intervals were calculated. Using the criteria described by Landis and Koch, Kappa statistics were then interpreted for reliability [9].
To determine the incidence of cholesteatoma from TM retraction during the study period, an institutional pathology database was cross-referenced to identify all diagnoses of cholesteatoma arising within the initial cohort of 76 retracted TMs.
Secondary analyses were performed to look for features associated with deterioration (worsening appearance or hearing) at the time of initial assessment. Worsening of hearing was defined as an elevation of the pure tone average (PTA) of >5 dB. The senior author reviewed the initial images on two separate occasions and assessed for the presence or absence of the following: promontory contact, incus contact, stapes contact, depth of retraction out of sight, and accumulation of keratin medial to the annulus. During this review, retractions were dichotomized into two groups: mild retraction not contacting the middle ear structures (equivalent to Sade stage 1) and more severe retraction (contact with the incus or promontory or both, i.e., Sade stage >1) [10]. The Fisher’s exact test was employed to investigate whether each variable was associated with a change in appearance or hearing over time. Initial PTAs were compared between the group of retractions that worsened and the group that remained stable or improved using a pooled t-test. Initial PTAs were also compared between the group of retractions that developed further hearing loss and that with stable or improved hearing using a t-test with Satterthwaite adjustment (unequal variances).
Additional secondary analyses were performed to determine whether deterioration of any individual variables assessed was associated with the deterioration of the overall appearance or hearing. Again, the Fisher’s exact test was used for analyzing categorical data, and t-tests were employed for evaluating the association with PTA at follow-up.
Statistical Analysis System Version 9.4 (SAS Institute, Cary, NC, USA) was used for all statistical analyses, which were performed by an independent biostatistician.
RESULTS
Of the 76 pars tensa retractions identified in the original study, 37 (15 unilateral, 11 bilateral) were re-evaluated in 26 patients at a median follow-up interval of 6.4 years (range, 0.75–7.6 years). The median age at reassessment was 15 years (range, 9–21 years). Fifteen patients had a history of complete hard palate cleft (seven with associated cleft lip), seven had incomplete clefts of the hard palate, and four had a history of soft palate cleft alone. Two children were syndromic (Stickler, van der Woude) and three were born with Pierre Robin sequence.
Natural History of Retractions
Follow-up images were rated as stable (n=16) or better (n=12) for 28/37 retractions (76%). No obvious ossicular erosion developed during the study period. Of the nine retractions that worsened, two (5%) ultimately required surgery for cholesteatoma during the study period (diagnosed at 17 and 44 months after the original assessment). No additional operative interventions occurred during the study period. Conductive hearing loss (4-tone average air-bone gap >25 dB-HL), initially present in five ears with retraction, worsened in one ear (PTA elevation from 28 to 50 dB) and normalized without intervention in others. No ears with initially normal hearing developed hearing loss.
The institutional pathology database used to determine this prevalence was also cross-referenced with the entire list of patients examined during the previous study (n=76 retracted TMs), and no other instances of cholesteatoma were identified. Original images were saved between January 2007 and June 2008, and the pathology database was queried in December 2016. Thus, the incidence of cholesteatoma in our original cohort of children with cleft palate with TM retraction over an 8.5-year period was 2.6%.
Reliability of Retraction Assessment
Intra-rater agreement ranged from moderate to 100% across all comparisons. For the primary outcome measure comparing the overall change in severity between the two otoscopic images, inter-rater agreement was moderate. With respect to the individual variables, assessments of bony contact (promontory or incudostapedial) and cleanliness proved to be reliable (moderate to substantial agreement). There was more variability in comparing the depths of the retraction pockets (fair agreement) and ossicular erosion (slight agreement).
Lack of Association between Individual Features and Deterioration
Features noted on unblinded review of the initial images are detailed in Table 1, along with initial tympanometric data. The only feature initially present in both ears that later developed into cholesteatoma was promontory contact. Regarding the whole cohort, however, 88% (14/16) of retractions with promontory contact remained free of cholesteatoma over the study period. Based on these data, the positive predictive value of promontory contact leading to cholesteatoma formation was only 0.125 (95% confidence interval, 0.025–0.125). Neither retraction that led to cholesteatoma demonstrated contact with the ossicular chain, incomplete visibility, or accumulation of keratin debris at the initial assessment.
Table 1.
Characteristics of initial retractions noted on unblinded review
| Feature | n |
|---|---|
| Tympanometry | |
| Type A | 15 |
| Type B | 8 |
| Type C | 9 |
| Not tested | 5 |
| Severity | |
| Mild (shallow, Sade 1) | 18 |
| More severe (Sade >1) | 19 |
| Promontory contact | 16 |
| Incus contact | 7 |
| Stapes contact | 5 |
| Visibility | |
| Depth in view | 30 |
| Depth of out of sight | 7 |
| Cleanliness | |
| No debris | 33 |
| Keratin medial to annulus | 4 |
There was no association between initial retraction severity (mild/Sade 1 vs. more severe/Sade >1) and worsening appearance (p=0.71) or hearing (p=0.60) according to the two-tailed Fisher’s exact test. There were no significant associations between the presence of clinically relevant features assessed (promontory contact, incus contact, stapes contact, depth of retraction out of sight, and accumulation of keratin medial to the annulus) and deterioration of the overall tensa appearance or hearing.
The mean initial PTA for retractions that worsened at follow-up was 10 dB, while the mean for retractions that improved was 17 dB; this difference was not significant (p=0.11, pooled t-test). The mean initial PTA for retractions that developed elevated pure tone thresholds over the study period was 24 dB, whereas the mean for retractions with stable or improved hearing was 11.21 dB; this difference was not statistically significant (p=0.275, t-test with Satterthwaite correction).
Characteristics of Deterioration
Worsened appearance with respect to both promontory contact (19%) and incudostapedial contact (8%) was significantly associated with overall worsening of the retraction (p<0.01 and p=0.01, respectively, two-tailed Fisher’s exact test). There were no significant associations between any variables that worsened and hearing loss (Table 2).
Table 2.
Lack of association between initial hearing thresholds and deterioration of retraction features
| Variable (n from majority assessment) | Mean PTA in dB | t-test p |
|---|---|---|
| Surface area | ||
| Worse (7) | 12.7 | |
| Better (30) | 13.0 | 0.93 |
| Visibility of depth | ||
| Worse (2) | 13.1 | |
| Better (35) | 12.9 | 0.98 |
| Promontory contact | ||
| Worse (7) | 12.5 | |
| Better (30) | 13.0 | 0.88 |
| Incudostapedial contact | ||
| Worse (3) | 10.4 | |
| Better (34) | 13.2 | 0.60 |
| Ossicular erosion | ||
| Worse (1) | 6.3 | |
| Better (36) | 13.1 | 0.43 |
| Cleanliness | ||
| Worse (5) | 24.5 | |
| Better (32) | 11.1 | 0.13* |
Satterthwaite correction applied for unequal variances
PTA: pure tone average
DISCUSSION
In this study sample of children at risk for persistent eustachian tube dysfunction from cleft palate, most TM retractions remained stable or improved over time. They were managed conservatively in this series, thereby allowing for observation of the natural history of the pathology. Clinically significant progression occurred infrequently, at least during the time course followed in this study, which approximates to the teenage years. The overall incidence of cholesteatoma development in children with cleft palate with TM retraction was 2.6% over the 8.5-year period, which was predominantly during the teenage years. This is comparable with the 2% risk of acquired cholesteatoma in all children with cleft palate reported from our center previously [6]. In our healthcare system, it is improbable that children from this series would have undergone surgery for cholesteatoma at another institution. None of the other ears followed in this series demonstrated any visible sign of ossicular erosion, and hearing thresholds deteriorated in only one ear. No ears with initially normal hearing thresholds developed hearing loss, although one diffusely retracted TM with both promontory and incus contacts demonstrated progression of hearing loss.
Based on the finding that only 1 in 50 children with cleft palate develop cholesteatoma throughout adolescence [6], this study did not have the power to definitively ascertain the risk of cholesteatoma formation from TM retraction in this population. Therefore, the observations should not be dismissed because there is a paucity of longitudinal data pertaining to TM retractions. The relatively small sample size of this study is simply a reflection of the difficulty in following a cohort in this age range prospectively over a 5-year period. Although only 37 out of 76 retractions identified in the pilot study were captured in the follow-up, the remaining 38 were cross-referenced with an institutional pathology database, and no additional cases of cholesteatoma were identified.
The objective of this study was to provide data on the natural history of pars tensa retraction, which could be used to compare the effectiveness of outcomes from surgical treatment. For example, from our findings, it can be estimated that to prevent cholesteatoma in teenagers with cleft palate and a pars tensa retraction contacting the promontory or incus, the number needed to treat would be nine (assuming that the intervention is effective 100% of the time). If the intervention had to be repeated annually, similar to that in repeated tympanostomy tube insertion used for management, approximately 80 interventions may be necessary to prevent one case of cholesteatoma from a retraction with bony contact. These are approximate estimates because treatment outcome is unlikely to be 100% effective, and unintended consequences of intervention, such as retained tympanostomy tubes or subsequent TM perforation, may alter the outcome. Furthermore, many other factors must be evaluated when considering the appropriateness of surgical intervention. These include, but are not limited to, the progression of retraction and development of adherence, presence of otitis media, hearing thresholds, status of the contralateral ear, and parental or patient preference. Nevertheless, this series provides some necessary understanding of the natural history of the disorder that can be incorporated into clinical decision-making when surgical intervention is being considered.
More than 50% of TM retractions followed in this study were noted to have bony contact (i.e., Sade stage >1) at the original assessment. A priori, we had hypothesized that this subgroup would be more likely to progress than that with Sade stage 1 retractions. At the end of the study, no group showed much progression and the difference between the two groups was not statistically significant. In fact, none of the factors examined were associated with worsened appearance or hearing over time. Similarly, there was no association between initial PTA and natural history. Taken together, our study was simply underpowered to uncover any factors associated with deterioration.
Recognizing that the progression or improvement of TM retractions is not necessarily ordinal when using traditional staging systems, we believed that serial endoscopic image comparison would more effectively capture the natural history of this disease entity. The factors included in the image review were thought to be clinically relevant and were extrapolated from a multicomponent assessment previously shown to have substantial inter-rater reliability [3]. In this study, reviewers were asked to consider all individual factors before making an overall assessment of the pars tensa. Inter-rater agreement for this primary outcome measure was ultimately moderate. However, the intra-rater agreement was better (moderate for one reviewer, substantial for two, and almost perfect for another). This discrepancy may be reflective of differences in the relative significance ascribed to each feature across clinicians and highlights one of the challenges facing clinicians making decisions about how to manage TM retraction.
There are some notable limitations to evaluating the natural history of retraction with endoscopic image comparison. First, given the static nature of the image, adherence cannot be adequately assessed. Although adherence is often mentioned as an important characteristic of TM retraction severity, there is a scarcity of studies validating the assessment with different techniques (i.e., Valsalva maneuver, pneumatic otoscopy, nitrous oxide anesthesia, or surgical dissection). Additionally, there is a lack of evidence with respect to any correlation between adherence and prognosis. It has also been stated that ossicular adherence is irreversible [10, 11]. As such, some authors advocate prophylactic tympanoplasty when ossicular contact is identified to prevent the erosion of the incus [12]. In our cohort, seven retractions were noted to be making contact with the incus (seemingly adherent) in the original images. Three of these were thought to be stable, three to be improved, and one to be worse. One of the improved retractions had perforated, but the other two resolved spontaneously without any evident residual ossicular contact (Figure 1). Even without assessing adherence, these data argue against any rapid progression from incus contact to adherence to erosion and permanent hearing loss. Currently, we hypothesize that ossicular erosion is stimulated by inflammatory reactions under accumulated keratin debris and not simply by the contact of clean TM skin on an ossicle. We consider that debridement of the eardrum may be required to prevent ossicular erosion. It should be noted that one instance of worsened hearing occurred in this subgroup but the incus contact was stable without any visible erosion. Clinicians must be wary of the fact that the angulation of an endoscope can alter the perception and potentially impair accurate diagnosis (Figure 2). Finally, hair in the ear canal and ceruminous debris in patients intolerant of microdebridement can make it difficult to to bring the TM into focus, thereby reducing the yield of examination.
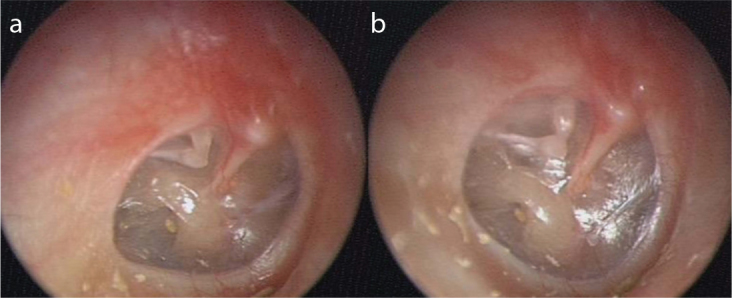
Figure 1. a, b.

Serial otoendoscopic images taken of the right tympanic membrane in a child with cleft palate. (a) Pars tensa retraction contacting the promontory, long process of the incus, stapes capitulum, and stapedius tendon. (b) Spontaneous lateralization of the retraction noted 7 years later with no further evidence of any ossicular contact
Figure 2. a, b.
Otoendoscopic images taken of the right tympanic membrane from the same ear on the same day. (a) Diffuse retraction of the pars tensa with obvious ossicular contact but no definitive erosion of the incus. (b) Change in angulation of the scope clearly demonstrates distal erosion of the incus long process
CONCLUSION
Clinically significant progression of TM retraction was infrequent during the teenage years in our cohort, a group at risk for chronic eustachian tube and middle ear dysfunction from cleft palate. This relatively benign natural history should be considered when weighing the risks and benefits of surgical intervention for TM retraction without cholesteatoma in this age group.
Acknowledgements
The authors would like to credit Derek Stephens, M.Sc., from the Department of Biostatistics, Design and Analysis at The Hospital for Sick Children for all of the statistical analysis.
Footnotes
This study was presented at the Spring Meeting of the American Society of Pediatric Otolaryngology on May 19, 2017, Austin, Texas, USA.
Ethics Committee Approval: Ethics committee approval was received for this study from the Research Ethics Board (1000036525, approved 2013-03-04).
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - W.P., L.M., A.J.; Design - W.P., L.M., A.J.; Supervision - S.C., B.P., A.J.; Resource -W.P., L.M., S.C., B.P., A.J.; Materials - W.P., L.M., S.C., B.P., A.J.; Data Collection and/or Processing - W.P., L.M., A.J.; Analysis and/or Interpretation - W.P., L.M., S.C., B.P., A.J.; Literature Search -W.P., A.J.; Writing - W.P., L.M., S.C., B.P., A.J.; Critical Reviews - W.P., L.M., S.C., B.P., A.J.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Maw AR, Hall AJ, Pothier DD, Gregory SP, Steer CD. The prevalence of tympanic membrane and related middle ear pathology in children: a large longitudinal cohort study followed from birth to age ten. Otol Neurotol. 2011;32:1256–61. doi: 10.1097/MAO.0b013e31822f10cf. [DOI] [PubMed] [Google Scholar]
- 2.Borgstein J, Gerritsma TV, Wieringa MH, Bruce IA. The Erasmus atelectasis classification: proposal of a new classification for atelectasis of the middle ear in children. Laryngoscope. 2007;117:1255–9. doi: 10.1097/MLG.0b013e31805d0160. [DOI] [PubMed] [Google Scholar]
- 3.James AL, Papsin BC, Trimble K, Ramsden J, Sanjeevan N, Bailie N, et al. Tympanic membrane retraction: an endoscopic evaluation of staging systems. Laryngoscope. 2012;122:1115–20. doi: 10.1002/lary.23203. [DOI] [PubMed] [Google Scholar]
- 4.Goudy S, Lott D, Canady J, Smith RJ. Conductive hearing loss and otopathology in cleft palate patients. Otolaryngol Head Neck Surg. 2006;134:946–8. doi: 10.1016/j.otohns.2005.12.020. [DOI] [PubMed] [Google Scholar]
- 5.Flynn T, Lohmander A. A longitudinal study of hearing and middle ear status in individuals with UCLP. Otol Neurotol. 2014;35:989–96. doi: 10.1097/MAO.0000000000000429. [DOI] [PubMed] [Google Scholar]
- 6.Harris L, Cushing SL, Hubbard B, Fisher D, Papsin BC, James AL. Impact of cleft palate type on the incidence of acquired cholesteatoma. Int J Pediatr Otorhinolaryngol. 2013;77:695–8. doi: 10.1016/j.ijporl.2013.01.020. [DOI] [PubMed] [Google Scholar]
- 7.Djurhuus BD, Skytthe A, Faber CE, Christensen K. Cholesteatoma risk in 8,593 orofacial cleft cases and 6,989 siblings: a nationwide study. Laryngoscope. 2015;125:1225–9. doi: 10.1002/lary.25022. [DOI] [PubMed] [Google Scholar]
- 8.Pothier DD. The Sadé and Tos staging systems: not adequately reliable methods of staging retraction of the tympanic membrane? Clin Otolaryngol. 2009;34:506–7. doi: 10.1111/j.1749-4486.2009.02015.x. [DOI] [PubMed] [Google Scholar]
- 9.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 10.Sade J, Avraham S, Brown M. Atelectasis, retraction pockets and cholesteatoma. Acta Otolaryngol. 1981;92:501–12. doi: 10.3109/00016488109133289. [DOI] [PubMed] [Google Scholar]
- 11.Borgstein J. In reference to tympanic membrane retraction: an endoscopic evaluation of staging systems. Laryngoscope. 2012;122:2359. doi: 10.1002/lary.23449. author reply 2360–1. [DOI] [PubMed] [Google Scholar]
- 12.Borgstein J, Gerritsma TV, Bruce IA. Erosion of the incus in pediatric posterior tympanic membrane retraction pockets without cholesteatoma. Int J Pediatr Otorhinolaryngol. 2008;72:1419–23. doi: 10.1016/j.ijporl.2008.06.004. [DOI] [PubMed] [Google Scholar]


