Abstract
Balloon Eustachian tuboplasty (BET) aims to improve the function of the Eustachian tube (ET). The objective of this study was to review the long-term outcome of BET and present the process and results of outlining indications for BET by the Finnish Otosurgical Society. The literature review is based on a database search performed in May 2017. The search resulted in 100 individual articles, which were screened for relevance. Five articles fulfilled the inclusion criteria (follow-up ≥12 months). Five additional articles (follow-up, 6–11 months) were analyzed to obtain supportive information. The proposed BET indications were constituted in the 2016 annual meeting of the Finnish Otosurgical Society. The workshop included a review of the Eustachian tube physiology, middle ear aeration mechanisms, and BET outcome studies. Thereafter, the members of the Society first voted and then discussed 14 cases in order to conclude whether BET was indicated in each case, and subsequently, a consensus statement on the indications for BET was outlined. The long-term follow-up studies were heterogeneous regarding the Eustachian tube dysfunction (ETD) definition, patient selection, follow-up duration, additional treatments, and outcome measures. The current, but limited, evidence suggests that BET is effective in the long-term. However, more long-term studies with uniform criteria and outcome measures as well as placebo-controlled studies are needed. The proposed indications for BET by the Finnish Otosurgical Society include chronic bothersome symptoms referring to ETD, ETD-related symptoms when pressure changes rapidly, or recurring serous otitis media. With the current evidence, we suggest treating only adults with BET.
Keywords: Eustachian tube dysfunction, balloon dilation, balloon Eustachian tuboplasty, outcome, indication
INTRODUCTION
The Eustachian tube (ET) equalizes pressure between the middle ear and the nasopharynx and drains accumulated secretions from the middle ear. If the ET function is compromised, symptoms such as aural fullness, feeling of pressure, pain, clogged feeling, or popping in the ears may appear [1]. Chronic Eustachian tube dysfunction (ETD) may lead to recurrent or persistent otitis media with effusion (OME), hearing loss, temporary lag in speech development in children, retraction of the tympanic membrane, or even cholesteatoma [2]. Balloon Eustachian tuboplasty (BET) aims to prevent, reverse, or stop the progression of these conditions by widening the medial cartilaginous part of the ET, hence improving its function. Since its introduction in patients in 2010 [3], several studies on the effect of BET have been published. However, study populations tend to be small, and follow-up times are mostly short. Also, the heterogeneity of the studies with regard to indications, duration of follow-ups, and outcome measures complicates comparison of the results.
UK National Institute for Health Research Health Technology Assessment Program commissioned a review of treatments for ETD. The review found that the evidence of BET outcomes was insufficient to show efficacy and pointed the need for consensus on definition and diagnostic criteria of ETD [4]. To reach a consensus on these subjects, an international panel gathered in Amsterdam in June 2014. They concluded that the clinical assessment of ETD should include otoscopy/otomicroscopy, tympanometry, tuning fork tests or pure tone audiometry, and nasopharyngoscopy. The diagnosis of ETD should include ETD symptoms and negative pressure in the middle ear observed either in the tympanogram or as a retraction of the tympanic membrane [1]. Additional tools for evaluating ETD and the effect of BET include Valsalva and Toynbee maneuvers, tubomanometry, Eustachian Tube Score (ETS), ETS-7 (extension of ETS), and Eustachian Tube Dysfunction Questionnaire (ETDQ-7) [3,5–7]. However, till date, there is no gold standard for measuring BET outcomes.
Since no international consensus for the indications of BET has been reached, the Finnish Otosurgical Society agreed on proposed indications in its annual meeting held in April 2016. The indications were based on a review of ET physiology, middle ear aeration mechanisms, studies on BET outcome, and voting and discussion of patient cases related to ETD and BET.
This report aims to summarize the current evidence of the long-term (≥12 months) effects of BET and present indications for the procedure as proposed by the Finnish Otosurgical Society.
METHODS
As the literature search for the meeting of the Finnish Otosurgical Society was performed in 2016, we wished to update the search when starting to work with this manuscript. Therefore, we scanned the PubMed and Scopus on May 24, 2017 using the keywords “Eustachian tube’ AND ‘balloon’, ‘Eustachian’ AND ‘balloon dilation’, ‘Eustachian’ AND ‘balloon dilatation’, and ‘Balloon Eustachian tuboplasty’ (Fig. 1). The search resulted in 100 individual articles. The inclusion criteria were full-text articles available in English with a minimum of 12-month follow-up. Exclusion criteria included articles in language other than English (n=24), articles unrelated to ET (4), cadaver or animal studies (18), reviews (5), editorial or other short correspondences (4), transtympanic BET (3), case reports (3), studies with no follow-up (16), and follow-up <12 months or unclear (18). Since only five studies fulfilled the 12-month follow-up criterion, we also accepted studies (five articles) with follow-up of 6–11 months as supportive information. Studies on both adults and children, separately or mixed, were included.
Figure 1.
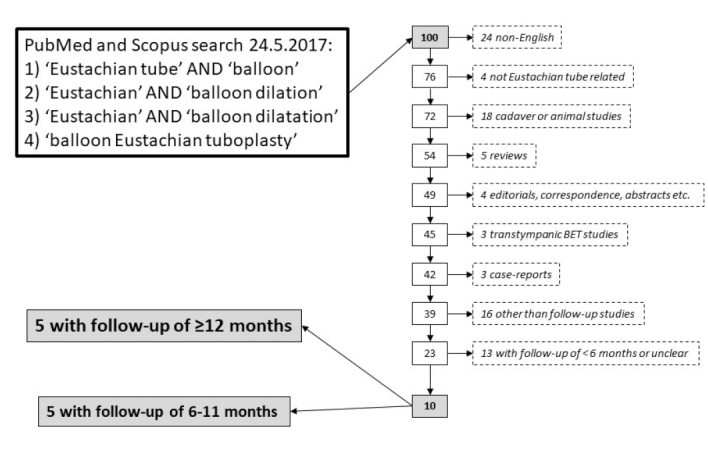
Flowchart for the literature search performed on May 24, 2017
From the studies that met the inclusion criteria, we extracted the following information: study setting, number of patients and ears treated, number of drop-outs, age of patients, follow-up duration, type of balloon dilation catheter, surgical technique, type of anesthesia, inclusion and exclusion criteria, preoperative investigations, other procedures performed simultaneously with BET or during follow-up, conservative treatment given preoperatively or postoperatively, outcome measures, and complications.
Outcome measures of BET
Since there is no consensus on the optimal outcome measures of BET, different studies have used different parameters. To help to comprehend the results, we have listed the main outcome measures used and their rationale below.
Symptoms and Disease-Specific Questionnaire ETDQ-7
Typical ear symptoms suggestive of ETD include fullness, pressure, pain, clogged feeling, and popping [1]. Even though no symptom is specific to ETD alone and differential diagnostics has to be carefully considered, symptoms have an important role in the diagnosis of ETD together with clinical findings.
ETDQ-7 is a validated, disease-specific questionnaire for ETD diagnosis. It also serves in the evaluation of treatment effect when used both pre and postoperatively. From the previous month, patients rate the severity of seven symptoms that are suggestive of ETD on a scale ranging from 1 (no problem) to 7 (severe problem). Dividing the total score by seven yields the mean item score. A total score of ≥14.5 and mean item score of ≥2.1 indicate ETD [6].
Valsalva and Toynbee Maneuvers
In Valsalva maneuver, closing the nose and mouth while blowing air directs the air to the ETs and is supposed to help the ETs open. Toynbee maneuver is positive when the tympanic membrane moves while the patient swallows with the nose closed. Swallowing involves the muscles tensor veli palatini and levator veli palatini that simultaneously also act to open the ET. Positive Valsalva and Toynbee maneuvers require at least a partly functional ET. Therefore, if positive, the maneuvers may serve as signs of ET function. However, Valsalva maneuver might be difficult to perform even with perfectly functioning ETs, and if Valsalva remains negative it is difficult for the examiner to ensure that the patient performs the maneuver correctly. Therefore, with negative Valsalva, the examiner remains with the question whether the result is negative because of poor technique or whether it is negative because ET does not open despite correctly performed Valsalva. To conclude, the maneuvers by themselves are unreliable measures of ET function but they provide supporting information in the diagnostics of ETD [1]. The maneuvers can be measured objectively with the help of oto(micro)scopy, impedance measurements, or sound recordings.
Tympanometry
Tympanometry provides information on the middle ear pressure, which, if negative, reflects ETD or other middle ear pathology. However, normal middle ear pressure does not exclude baro-challenge-induced ETD.
Computed Tomography (CT) Scans
The main purpose of preoperative computed tomography (CT) scans has mainly been to exclude dehiscence or anomaly of the internal carotid artery and thereby avoid complications involving damage to the internal carotid artery.
Tubomanometry
Tubomanometry measures the latency of ET opening after swallowing [7]. The subject swallows water while 30, 40, or 50 mbar pressure is applied through the nose. A pressure sensor in the external ear canal registers changes in pressure when the ET opens. Opening latency index (R value) of ≤1 suggests immediate opening of the ET after swallowing, R>1 reflects late opening, and non-measurable R indicates that the ET stays closed.
ETS and ETS-7
ETS combines tubomanometry at three pressure levels with subjectively positive Valsalva maneuver and clicking sound when swallowing [5]. The subjective Valsalva and clicking sound when swallowing are evaluated from the period of previous two months. Each parameter receives a value from 0 (the worst) to 2 (the best) yielding minimum and maximum total score of 0 and 10, respectively. ETS-7 adds the tympanometry and the objectively evaluated Valsalva to ETS and its score ranges from 0 (the worst value) to 14 (the best value) [5]. An ETS≤5 and ETS-7≤7 suggest diagnosis of chronic ETD.
Workshop To Define The Proposed Indications For BET By The Finnish Otosurgical Society
In the annual meeting of the Finnish Otosurgical Society held in April 2016 (Pallas, Finland), we covered ET physiology, middle ear ventilation mechanisms, and transmucosal gas exchange in the middle ear and the mastoid. We also reviewed studies on the effects of BET published so far in English and the consensus statement on ETD [1].
After agreeing on the diagnostic criteria of ETD, we reviewed 14 imaginary cases, of both adults and children, having different signs and symptoms related to ETD. The cases, translated to English, are in the Supplementary File 1. On the basis of their personal experience and the current literature, the members of the Finnish Otosurgical Society individually voted on each case whether they considered BET to be indicated or not or whether they were unable to decide. The voting proceeded with personal mobile phones and the Kahoot application (https://kahoot.it). The votes were divided into three different categories: (i) ENT specialists routinely performing BET (n=15), (ii) ENT specialists irregularly performing BET (n=6), and (iii) ENT residents (n=5). The voting results are shown in Supplementary Table 1. After voting, each case and the result of the vote were discussed before proceeding to the next case. After discussing all the cases, we agreed on proposed indications for BET, which are presented in the section “The proposed indications for BET by the Finnish Otosurgical Society”.
REVIEW of LITERATURE
Studies With Follow-Up Period Of ≥12 Months
Study Characteristics
Five studies fulfilled the inclusion criteria. Maximal follow-up periods ranged between 12 and 50 months, and the number of patients and their outcome at ≥12 month time points were clearly identifiable. Two of the studies were prospective case series [8, 9], and the rest were retrospective case series [2, 10, 11]. The level of evidence according to Oxford Centre for Evidence-based Medicine was 4 in all studies. All the studies included a total of 968 patients (i.e., 1615 ears were treated with BET), but 1 year postoperatively, the loss to follow-up was >70% in three studies [2, 9, 10]. The patients were 3–88 years old; mean or median age, if reported, was 7–48 years. Four studies performed BET with balloon dilation instrument from Spiggle & Theis (Spiggle & Theis Medizintechnik GmbH, Overath, Germany) [2, 9–11]. One study used Acclarent Relieva Solo catheter (Acclarent Inc., Menlo Park, CA, USA) [8]. Inflation pressures ranged from 8 to 12 bars. All studies using Spiggle & Theis device kept the balloon inflated for 2 min at once. Silvola et al. [8] started with 1-min inflation for the first 15 ears but the rest 26 ears received 1-min dilation two times in a row. The Acclarent device was wider and shorter than the one from Spiggle & Theis (7×16 mm vs. 3.2–3.3×20 mm, respectively). The findings are listed in Table 1a.
Table 1a.
Characteristics of studies with a follow-up period of minimum 12 months
| Publication | Study setting | Level of evidence | n (patients) | n (ears) | Age (years) (mean) [range] | Follow-up (months) [range] | Dilation instrument; inflation pressure and time |
|---|---|---|---|---|---|---|---|
| Silvola et al., 2014 [8] | Prospective case series | 4 | 37 (36 at the end of the follow-up) | 42 (41 at the end of the follow-up) | 48 [15–38] | Mean 30, [18–50] | Acclarent Relieva Solo 7×16 mm; 15 cases 12 bar, 1 min, 26 cases 12 bar 1 minx2 |
| Schröder et al., 2015 [10] | Retrospective case series | 4 | 622 | Total 1076 2 months: 506 of 1029 1 year: 188 of 671 2 years: 34 of 344 3 years: 11 of 119 4 years: 2 of 17 |
No mean reported [7–84] | [2–48] | Spiggle & Theis 3.3×20 mm; 10 bar, 2 min |
| Dalchow et al., 2016 [9] | Prospective case series | 4 | Total 217 1 month: 175 3 months: 92 6 months: 43 9 months: 29 12 months: 19 |
342 | Median 46 [6–88] | [1–12] | Spiggle & Theis 3.3×20 mm; 10 bar, 2 min |
| Xiong et al., 2016 [11] | Retrospective case series | 4 | 40 | 58 | 42 [21–70] | 12 | Spiggle & Theis 3.3×20 mm; 10 bar, 2 min |
| Leichtle et al., 2017 [2] | Retrospective case series | 4 | Total 52 2 weeks: 41 2 months: 38 6 months: 27 12 months: 14 |
97 | 7 [3–15] | [0–12] | Spiggle & Theis, 3.2×20 mm; 8 bar, 2 min |
Inclusion and Exclusion Criteria And Preoperative Examinations
The inclusion criteria varied between the studies. One study included patients with ETD symptoms refractory to the conservative treatment and required no objective findings of negative pressure in the middle ear [9]. Another study involved patients with ETD symptoms together with evidence of normal tympanic membrane for at least 6 months preoperatively [11]. Two studies required an objective sign of negative pressure in the middle ear but no symptoms [2, 8]. In one retrospective study, the indications for BET changed during the chosen time frame of the analysis [10]. Three studies reported exclusion criteria but they were different in each study [2, 9, 11]. The findings are listed in Table 1b.
Table 1b.
Inclusion and exclusion criteria, preoperative examination in studies with follow-up period of minimum 12 months
| Publication | Inclusion criteria | Exclusion criteria | Preoperative examination |
|---|---|---|---|
| Silvola et al., 2014 [8] | Uni or bilateral persistent OME or remarkable nonadherent atelectasis of the TM for min 5 years; findings refractory to nasal corticosteroid treatment of minimum 1 month | NR | Otomicroscopy, video endoscopy of the nose, nasopharynx and ET orifices, objective Valsalva (with/without the help of Politzer balloon), CT |
| Schröder et al., 2015 [10] | 1. ETD symptoms or previous middle ear surgery because of undiagnosed ETD or chronic persistent OME 2. ETS≤5 or ETS-7≤7 and at least one of the following: pressure in the ear (especially during changes of atmospheric pressure), inability to do Valsalva, chronic middle ear effusion, adhesive otitis media, tympanometry type B, early retraction after repair of tympanic membrane |
NR | Symptoms, ETDQ-7, history of ear diseases and previous ear surgery clinical examination, Valsalva, Toynbee, tympanometry, TMM, audiometry |
| Dalchow et al., 2016 [9] | Symptoms of chronic obstructive ETD refractory to detumescent nasal sprays with or without cortisone, systemic cortisone or tube training | Revision BET | Pressure in the ear, otomicroscopy, nasopharyngoscopy, Valsalva, Toynbee, tympanometry, TMM, audiometry, digital volume tomography |
| Xiong et al., 2016 [11] | Aural fullness with or without otalgia, muffled hearing and tinnitus, normal TM for minimum 6 months preoperatively; symptoms refractory to minimum 6 months autoinsufflation, nasal decongestants, antihistamines, and nasal corticosteroids | TMJ problems, endolymphatic hydrops, OME, TM atelectasis, history of any middle ear disease | Symptoms, otoscopy, Valsalva, ETS, TMM, audiometry, impedance audiometry, HRCT |
| Leichtle et al., 2017 [2] | Persistent/recurrent otitis media with or without chronic middle ear effusion or chronic adhesions with poorly mobile tympanic membrane, persistent perforation of the TM or cholesteatoma; clinical findings refractory to conventional therapy after adenotomy and tympanostomy | Acute upper respiratory tract infection, cleft palate, other craniofacial malformation | Lübecker questionnaire, clinical examination, tympanometry, TMM at 50 mbar, audiometry/children’s audiometry |
BET, balloon Eustachian tuboplasty; CT, computed tomography; ET, Eustachian tube; ETD, Eustachian tube dysfunction; ETDQ-7, Eustachian Tube Dysfunction Questionnaire; ETS, Eustachian Tube Score; ETS-7, extended Eustachian Tube Score; HRCT, high resolution computed tomography; NR, not reported; OME, otitis media with effusion; TM, tympanic membrane; TMJ, temporomandibular joint; TMM, tubomanometry.
Four studies required that, before proceeding to BET, conservative treatment had been given but that its effect was inadequate [2, 8, 9, 11]. The prerequisite treatment modalities varied from decongestive nasal sprays to adenotomy. The most common conservative treatment was nasal corticosteroids which was reported in three studies [8, 9, 11]. The minimum duration of the preoperative conservative treatment was 1–6 months. Two studies reported no duration for the conservative treatment [2, 9]. In one of them, patients had received tympanostomy and adenotomy before the evaluation of the effect of the conservative treatment, but the type of the conservative treatment used was unspecified [2].
The combinations of preoperative examinations were different in the five studies even though some overlap of the methods used existed between the studies. None of the studies used all preoperative investigation methods at the control visits. Otomicroscopy/otoscopy/clinical examination was the only preoperative investigation included in all the studies. Three of the five studies performed a preoperative radiologic examination [8, 9, 11].
Other Operations, Corticosteroid Treatment, and Complications
Two studies reported no other operations than BET at the time when BET was performed. [10, 11]. Others provided grommets at the time of BET if the tympanic membrane was intact [8] or tympanocenthesis or tympanoplasty to a part of the study population [2, 9]. Some patients received tympanoplasty before BET and others in conjunction with BET. Indications for tympanocenthesis or tympanoplasty remained unclear. One study reported additional procedures during the follow-up for 10% of the patients because they experienced no benefit from BET [8]. Four studies performed revision BET in 2%–11% of their patients because no improvement was observed following the first BET [2,8–10]. Four studies used corticosteroids preoperatively or postoperatively or both [8–11]; duration of the corticosteroid treatment varied from a single dose to 6 months of regular use. Only one study considered postoperative antibiotic prophylaxis to be necessary [9]. Two studies emphasized support and motivation for Valsalva and Politzer maneuvers during the follow-up [2, 8]. The findings are summarized in Table 1c.
Table 1c.
Other operations, corticosteroid treatment, and complications in studies with a follow-up of minimum 12 months
| Publication | Other operations in conjunction with BET | Operations during follow-up | Corticosteroids pre/postop | Other instructions or medication | Complications |
|---|---|---|---|---|---|
| Silvola et al., 2014 [8] | No TM perforation or grommet → tympanostomy | Valsalva positive at 1 month → grommet removal 1 pt unable to do Valsalva → revision BET 3 pt BET to contralateral side 4 pt did not improve → technetium scintigraphy and for 3 of them explorative tympanotomy and middle ear endoscopy (one had carotid dehiscence and received no further operations) |
Nasal corticosteroid for min 1 month preoperatively and 1 month postoperatively | Valsalva 2 times/day; if Valsalva negative at 1 week, Politzer maneuver → some could perform Valsalva after that | NR |
| Schröder et al., 2015 [10] | No | Revision BET to 68/622 pt marked as lost to follow-up for the first operation at the time of revision | Nasal corticosteroid for 6 weeks postop | NR | Emphysema in the parotid region (0.3%), minor bleeding, temporary increase of tinnitus, all resolved with time; insertion of balloon catheter unsuccessful in 3 pt (4 ears) |
| Dalchow et al., 2016 [9] | Tympanoplasty to 124/342 pt before or in conjunction with BET | Revision BET to 38/342 pt | 250 mg prednisolone on day 1 postoperatively | Cefuroxime 500 mg ×2 for 5 days postoperatively | No |
| Xiong et al., 2016 [11] | NR | NR | Nasal corticosteroid, minimum 6 months preoperatively | NR | No |
| Leichtle et al., 2017 [2] | BET+tympanocenthesis (24 cases), tympanoplasty type I (5 cases), tympanoplasty type III (3 cases) | Revision BET (2 cases) | NR | Instructions and motivation for Valsalva and/or Politzer at every visit | Hemotympanum (7%) resolved with time, minor nasal bleeding (21%) resolved with intranasal xylometazoline |
BET, balloon Eustachian tuboplasty; NR, not reported; pt, patient(s); TM, tympanic membrane
Complications reported in these studies were few and minor. They included minor bleeding, emphysema in the parotid region, hemotympanum, and temporary increase of tinnitus. They all resolved with time. In the studies that reported the rates of different complications, the rates ranged between 0.3% and 21%.
Main Outcome Measures
No single outcome parameter was used in all the studies. Three studies reported that preoperatively 0%–28% of the patients could perform Valsalva maneuver, but one year postoperatively, 80%–98% could successfully perform it [2, 8, 11]. Additionally, the proportions of type B and C tympanograms reduced during the follow-up and that of type A increased [2, 8, 11]. Only two studies reported oto(micro)scopy results[8, 11]. In a study requiring normal tympanic membranes in otoscopy for at least 6 months before the operation, all otoscopic findings remained normal during the follow-up [11]. Another study found that effusion decreased from 93% to 2%, but retraction and atelectasis remained unchanged (7%) at the end of the follow-up [8].
Xiong et al. [11] reported a positive change in tubomanometry for all three pressure levels (30, 40, and 50 mbar). Leichtle et al. found it difficult to perform tubomanometry in children and performed the measurement only with 50 mbar of pressure. They found greater proportion of patients having normal R value (<1) postoperatively than preoperatively [2]. Two studies reported tubomanometry only as a part of ETS [9, 10].
ETS defined by Ockermann et al. [3], including tubomanometry at three pressure levels, subjective Valsalva, and clicking sound when swallowing, was reported in two studies [10, 11]. Xiong et al. [11] reported a significant improvement in ETS one year postoperatively. Schröder et al. also noted a significant improvement in ETS at 1, 2, and 3 years when compared with the preoperative ETS [10]. They could reach only two patients for follow-up 4 years after BET, and both patients had decreased ETS compared to the preoperative value. However, the patient population was not the same at 1, 2, 3, and 4 years postoperatively. Dalchow et al. developed a different ETS consisting of tympanometry and tubomanometry scores only [9]. Their scale ranged from 1 (the worst value) to 4 (the best value), and the mean value improved at one year postoperatively. However, they reported only ETS and no separate tympanometry or tubomanometry results, making the comparison of their results with those of the other studies impossible. These findings are shown in Table 1d.
Table 1d.
Main outcome measures in studies with a follow-up period of minimum 12 months
| Publication | Valsalva positive (%, preoperatively → postoperatively) | Tympanometry type (%, preoperatively → postoperatively) | Oto(micro)scopy (%, preoperatively → postoperatively) | Tubomanometry (%, preoperatively → postoperatively) | ETS (mean value, preoperatively → postoperatively) |
|---|---|---|---|---|---|
| Silvola et al., 2014 [8] | 0 → 80, p<0.0001 | A: 2 → 56 C: 24 → 15 B: 15 → 0 Open: 59 → 29 p<0.0001 |
Normal: 0 → 90 Effusion: 93 → 2 Retraction/atelectasis: 7 → 7 p<0.0001 |
NR | NR |
| Schröder et al., 2015 [10] | NR | NR | NR | Included in ETS | 1 year ago: 3.13 → 5.75, p≤0.001 2 years ago: 2.65 → 6.26, p≤0.001 3 years ago: 2.36 → 5.27, p≤0.05 |
| Dalchow et al., 2016 [9] | NR | Included in ETS | NR | Included in ETS | 2.23 → 2.68, p<0.05 (own ETS scale of 1–4) |
| Xiong et al., 2016 [11] | 0 → 98, p<0.05 | A:74 → 98 C: 26 → 2, p<0.05 B: 0 → 0 |
Normal: 100 → 100 | R<1: 30 mbar: 36 → 79, p<0.05 40 mbar: 43 → 86, p<0.05 50 mbar: 50 → 90, p<0.05 |
3.3 → 7.9, p<0.05 |
| Leichtle et al., 2017 [2] | 28 → 88 | A: 14 → 50 C: 16 → 13* B: 56 → 26 |
NR | 50 mbar: R<1: 19 → 47 R=0: 51 → 15 |
NR |
p-values taken from publications, if given.
, numbers estimated from a figure. ETS, Eustachian Tube Score; NR, not reported.
Subjective Symptoms and Other Parameters
Three studies reported overall subjective symptoms which improved in 73%–98% of the patients [8, 10, 11]. Leichtle et al. [2] separately investigated the pressure in the ear, otalgia, and subjective hearing loss, and all these symptoms also showed a trend of improvement. Two years after BET, Schröder et al. [10] sent 89 patients (14%) an ETDQ-7, presumably with additional questions on subjective satisfaction, and 30 patients (34%) returned the questionnaire. However, the study reported no ETDQ-7 scores but only stated that 47% had no complaints and 26% experienced improvement.
Single studies also used outcome measures such as mucosal inflammation score [8], limitations in daily life [2], and general satisfaction, with the effect of BET [10]. Mucosal inflammation score and limitation in daily life diminished during the follow-up. At two years, 80% patients were at least partly satisfied with the treatment result [10]. None of the four studies [2, 9–11]. performing preoperative audiometry presented postoperative audiogram results. The findings are shown in Table 1e.
Table 1e.
Subjective symptoms and other measurements of studies with a follow-up period of minimum 12 months
| Publication | Symptoms | ETDQ-7 | Other |
|---|---|---|---|
| Silvola et al., 2014 [8] | Improvement: 90% | NR | Mean mucosal inflammation score 2.8 → 1.4 (scale 1–4), p<0.0001 |
| Schröder et al., 2015 [10] | At 2 year 89 patients (154 ears), 34% responded: no complaints: 47% improvement: 26% no improvement: 27% |
NR | At 2 year: 60% satisfied 20% completely satisfied only for the first few months 20% dissatisfied |
| Dalchow et al., 2016 [9] | NR | NR | NR |
| Xiong et al., 2016 [11] | Overall reduced in 98%; Aural fullness disappeared in 83%; Aural fullness 8.2 (VAS 1–10 scale) → 1.3, p<0.05 Muffled hearing (VAS) 6.7 → 1.5, p<0.05 Otalgia (VAS) 5.2 → 1.9, p<0.05 Tinnitus (VAS) 4.4 → 2.2, p<0.05 |
NR | NR |
| Leichtle et al., 2017 2 | Pressure in the ear: always: 59% → 4% mostly: 24% → 6%* sometimes: 6% → 10%* rarely: 5% → 48%* never: 5% → 31%* Subjective hearing loss: severe: 18% → 4% moderate: 19% → 4%* low-grade: 26% → 20%* slight: 21% → 35%* no: 16% → 37% Otalgia: always: 5% → 5%* mostly: 16% → 5%* sometimes: 18% → 16%* rarely: 29% → 37%* never: 31% → 37%* |
NR | Limitation in daily life: severe: 25% → 5% moderate: 35% → 13% low-grade: 23% → 11% no: 6% → 46% Totally or moderately satisfied: 73% |
p-values taken from publication if given.
, numbers estimated from a figure. ETDQ-7, Eustachian Tube Dysfunction Questionnaire; NR, not reported; VAS = Visual Analog Scale.
Studies With Follow-Up Period Of 6–11 Months
Study Characteristics
Five studies fulfilled all the other original inclusion criteria, but instead of a minimum follow-up of 1 year, they had follow-up periods of 6–11 months. We analyzed these studies as additional information as only five studies fulfilled our inclusion criterion of 12-month follow-up. Four of these five short-term studies were prospective. The level of evidence was 1b in one prospective randomized controlled trial [12] and 4 in the rest. Study populations ranged from 11 to 90 patients (11–90 ears). The median follow-up, if reported, was 7–10 months, and the follow-up time varied between 5 and 18 months. Of the five studies, two used Acclarent Relieva Solo catheter [13, 14], two used Spiggle & Theis [12, 15], and one used Acclarent Aera (Acclarent Inc., Menlo Park, CA, USA) [16]. The study characteristics and balloon sizes are indicated in Table 2a.
Table 2a.
Characteristics of studies with a follow-up period of 6–11 months
| Publication | Study setting | Level of evidence | n (patients) | n (ears) | Age (mean, years) [range] | Follow-up (months) [range] | Dilation instrument; inflation pressure and time |
|---|---|---|---|---|---|---|---|
| Poe et al., 2011 [13] | Prospective case series | 4 | 11 | 11 | 52 [33–76] | Median 7 [6–14] | Acclarent Relieva Solo 7×16 mm; 7 cases 12 bar, 1 min 4 cases 8–10 bar, 1 min |
| McCoul et al., 2012 [14] | Prospective case series | 4 | Total 22 0–6 weeks: 22 12 weeks: 19 6 months: 18 |
35 | 55 | Median 10 [5–14] | Acclarent Relieva Solo 5×24 mm or 7×24 mm; 10 bar, 2 min |
| Bast et al., 2013 [15] | Retrospective questionnaire study | 4 | 30 | NA | 50 [24–73] | [6–18] | Spiggle & Theis 3.3×20 mm; inflation pressure and time not reported |
| Liang et al., 2016 [12] | Prospective randomized controlled trial (unblinded) | 1b | 90 | 90 | No mean reported [20–52] | 6 | Spiggle & Theis 3.3×20 mm; 10 bar, 2 min |
| Bowles et al., 2017 [16] | Prospective case series | 4 | 39 | 55 | 46 [19–74] | 6 | Acclarent Aera 6×16 mm; 12 bar, 2 min |
Inclusion and Exclusion Criteria and Preoperative Examination
Inclusion and exclusion criteria also varied between the short-term studies. In two studies, all patients had OME preoperatively [12, 13]. In one study, the inclusion criteria were or abnormal panogram and abnormal otoscopy [14]. One study required ETDQ-7>14.5 in order to treat ETD with BET [16] (Table 2b). A previous unsuccessful conservative treatment was a prerequisite in three studies [12, 14, 16]. Moreover, the preoperative investigations varied between the five studies.
Table 2b.
Inclusion and exclusion criteria and preoperative examinations of studies with a follow-up period of 6–11 months
| Publication | Inclusion criteria | Exclusion criteria | Preoperative examination |
|---|---|---|---|
| Poe et al., 2011 [13] | Uni- or bilateral OME of min 5 years (only improved with tympanostomy tubes or perforations) | NR | Otomicroscopy, video endoscopy of the ET with slow-motion review, mucosal inflammation score, tympanometry, and CT |
| McCoul et al., 2012 [14] | Age>18 years, abnormal tympanogram and abnormal otoscopy, ETD symtoms; no response to 2-month therapy with per oral antihistamine, nasal corticosteroid, and Valsalva | H&N surgery<3 months ago, radiotherapy to H&N, sino-nasal carcinoma, acute upper respiratory infection (also acute otitis media), hypertrophy of the adenoid tonsil, nasal polyposis, cleft palate (also previously operated), craniofacial syndromes (also Down syndrome), cystic fibrosis, dysmotile cilia, and systemic immunodeficiency | ETDQ-7, SNOT22, clinical examination, tympanometry, audiometry, and CT of the sinuses |
| Bast et al., 2013 [15] | Chronic ETD treated with BET | Contraindications for BET: age <18 years, unidentifiable ET orifice, carotid dehiscence, severe septal deviation, hyperplastic turbinates, contraindications for general anesthesia | Clinical examination, tympanometry, audiometry, and thin-layer CT |
| Liang et al., 2016 [12] | Unilateral severe COME of minimum 6 months (type B tympanogram and otoscopic findings), refractory to treatments such as medications, Valsalva, tympanocenthesis, and/or tympanostomies | Physiological defect of the ear or nasopharynx, carotid dehiscence, malformation, tumor or aneurysm in the ET or carotis interna, inability to participate follow-up | Otic endoscopic findings and tympanometry |
| Bowles et al., 2017 [16] | Clinical history of ETD and ETDQ-7 score >14.5 despite min 3-mo therapy with nasal corticosteroids, autoinflation devices, and Valsalva | NR | ETDQ-7, otoscopy, nasofiberoscopy, subjective Valsalva, tympanometry, and audiometry |
BET, balloon Eustachian tuboplasty; COME, chronic otitis media with effusion; CT, computed tomography; ET, Eustachian tube; ETD, Eustachian tube dysfunction; ETDQ-7, Eustachian Tube Dysfunction Questionnaire; H&N, head and neck; NR, not reported; OME, otitis media with effusion; SNOT-22, Sino-Nasal Outcome Test.
Other Operations, Corticosteroid Treatment, and Complications
Three studies performed operations (other than BET) to at least a part of the study population in conjunction with BET [12–14]. These included tympanocenthesis, insertion or removal of tympanostomy tubes, myringoplasty, partial inferior turbinectomy, and other sinonasal operations. In one study, 6% of the study population received a revision BET during follow-up because of unimproved symptoms [14] (Table 2c).
Table 2c.
Other operations, corticosteroid treatment, and complications in studies with a follow-up period of 6–11 months
| Publication | Other operations in conjunction with BET | Operations during follow-up | Corticosteroids pre/postop | Complications |
|---|---|---|---|---|
| Poe et al., 2011 [13] | Tympanostomy if OME (18%), removal of tympanostomy tube (27%) | No | Nasal corticosteroid 1 month preoperatively and 1 month postoperatively | Contralateral C6-7 radiculopathy (9%), mucosal laserations (45%), all resolved with time |
| McCoul et al., 2012 [14] | Partial inferior turbinectomy to all, septoplasty if required to reach the ET orifice (43%), sphenoetmoidectomy and antrostomy of the middle meatus (34%), revision ethmoidectomy (6%), revision sphenotomy (9%), removal of clogged tympanostomy tube (3%), myringoplasty (3%) | Revision BET with a bigger balloon (6%) because of symptoms at 6 months | NR | Bleeding from the turbinectomy site → bilateral hemotympanum (3%) resolved with tympanocenthesis |
| Bast et al., 2013 [15] | No | No | NR | NR |
| Liang et al., 2016 [12] | According to randomization either no other operations than BET, tympanocenthesis + BET or only tympanocenthesis | NR | NR | NR |
| Bowles et al., 2017 [16] | No | No | Nasal corticosteroid 3 months preoperatively | No |
BET, balloon Eustachian tuboplasty; ET, Eustachian tube; NR, not reported; OME, otitis media with effusion.
Two studies reported corticosteroid treatment [13, 16]. One of them [13] advised nasal corticosteroid use for 1 month both preoperatively and postoperatively, and the other [16] instructed to use nasal corticosteroids for 3 months postoperatively.
Objective Outcome Measures
As with the long-term studies, no single outcome parameter was used in all these short-term studies. Liang et al. randomized 90 patients with similar preoperative clinical status to three different groups: group 1 received BET only, group 2 received BET and tympanocenthesis, and group 3 received tympanocenthesis only [12]. Tympanometry and otomicroscopy results were significantly better in group 1 and 2 than in group 3, in which they remained nearly unchanged postoperatively. Results of group 2 were slightly better than those of group 1 but the difference between them was statistically insignificant. None of the short-term studies provided tubomanometry or ETS results. Valsalva maneuver improved in 96%–100% [13, 16] and tympanometry normalized in 36%–97% [12–14, 16] of the study population. The review data are summarized in Table 2d.
Table 2d.
Main outcome measures; follow-up 6–11 months
| Publication | Valsalva positive (%, preoperatively → postoperatively) | Tympanometry type (%, preoperatively → postoperatively) | Oto(micro)scopy (%, preoperatively → postoperatively) | Tubomanometry | ETS |
|---|---|---|---|---|---|
| Poe et al., 2011 [13] | 0 → 100, p<0.001 always: 64% sometimes: 36% |
A: 0 → 36 C: 9 → 9 B: 27 → 0 Open: 64 → 55 |
Grommet: 45 → 36 Perforation: 18 → 18 Atelectasis: 9 → 0 Retraction: 9 → 0 OME: 18 → 0 Normal: 0 → 45 |
NR | NR |
| McCoul et al., 2012 [14] | NR | A: 0 → 97, p<0.001 As: 29 → 0 C: 57 → 0 B: 14 → 3 |
NR | NR | NR |
| Bast et al., 2013 [15] | NR | NR | NR | NR | NR |
| Liang et al., 2016 [12] | NR |
Only BET: A: 0 → 80 C: 0 → 3 B: 100 → 17 BET + tympanocenthesis: A: 0 → 83 C: 0 → 7 B: 100 → 10 Only tympanocenthesis: A: 0 → 7 C: 0 → 7 B: 100 → 87 |
Only BET: no effusion: 0 → 80 partial effusion: 0 → 7 complete effusion: 100 → 13 BET + tympanocenthesis: no effusion: 0 → 87 partial effusion: 0 → 7 complete effusion: 100 → 7 Only tympanocenthesis: no effusion: 0 → 7 partial effusion: 0 → 7 complete effusion: 100 → 87 |
NR | NR |
| Bowles et al., 2017 [16] | 0 → 96 | A: 40 → 95* C: 26 → 2* B: 23 → 4* |
NR | NR | NR |
p-values taken from publication if given.
, numbers estimated from a figure. BET, balloon Eustachian tuboplasty; ETS, Eustachian Tube Score; NR, not reported; OME, otitis media with effusion.
Subjective Symptoms and Other Parameters
Of the two studies reporting data from ETDQ-7, one [16] applied it separately to evaluate each ear, whereas the other [14] used it to evaluate both ears combined. The mean item score of ETDQ-7 improved from 4.9 to 2.0 and from 4.2 to 2.8 in these studies, respectively. The short-term studies provided no other information on overall symptoms. One questionnaire study investigated only general quality of life 6–18 months after BET using Glasgow Benefit Inventory (GBI) [15]. GBI showed significant improvement in the total score and in two subscores, ‘general health’ and ‘physical health’.
One study used mucosal inflammation score as an outcome parameter and noted significant improvement in it after BET [13]. Another study applied the Sino-Nasal Outcome Test (SNOT-22) together with ETDQ-7 and found a significant decrease also in SNOT-22 points [14]. None of the three studies that included preoperative audiometry presented postoperative audiogram results. Results of subjective symptoms and other miscellaneous parameters are reported in Table 2e.
Table 2e.
Subjective symptoms and other measurements with a follow-up period of minimum 6 months
| Publication | Symptoms | ETDQ-7 (symptom-specific mean, preoperatively → postoperatively | Other |
|---|---|---|---|
| Poe et al., 2011 [13] | NR | NR | Mean mucosal inflammation score 2.91 → 1.73 (scale 1–4). p=0.003 View to ET lumen postoperatively: <4 mm if treated with 8 bar, at least 4 mm but not up to isthmus if treated with 10 bar, isthmus visible in 83 patients,33% of those who were treated with 12 bar, p=0.004 (for full dilation associated with 12 bar) |
| McCoul et al., 2012 [14] | NR | 4.5 → 2.8, p<0.001 | SNOT-22 mean 51.4 → 30.0, p=0.001 |
| Bast et al., 2013 [15] | NR | NR | Improvement in total score (p = 0.001) and the subscores “general health” (p=0.001) and “physical health” (p=0.039) of GBI |
| Liang et al., 2016 [12] | NR | NR | NR |
| Bowles et al., 2017 [16] | NR | 4.9 → 2.0, p<0.0001 | NR |
p-values taken from publication if given. ET, Eustachian tube; ETDQ-7, Eustachian Tube Dysfunction Questionnaire; GBI, Glasgow Benefit Inventory; NR, not reported; SNOT-22, Sino-Nasal Outcome Test.
Studies With Unclear Follow-Up Time
Some studies from our article search mentioned no duration of follow-up at all. Others specified the follow-up time, but the time point when the presented results were obtained remained unclear. If we were unable to specify that the outcome was measured at least 6 months or 1 year postoperatively for a certain amount of patients, we excluded the study from this report.
Dai et al. [17] prospectively followed eight patients (12 ears) for 3–15 months after BET. They found that otomicroscopic findings normalized in 71% patients by 6 months and proportion of type A and C tympanograms increased while that of type B tympanogram decreased during the follow-up. However, only five patients (seven ears) and two patients (three ears) were available for the analysis at 6 and 12 months, respectively. Because of the small number of patients at 6 and 12 months, we excluded this study from our review.
The Proposed Indications For Bet By The Finnish Otosurgical Society
In the meeting of the Finnish Otosurgical Society in April 2016, we had a workshop with the objective of formulating national indications for BET. We reviewed the consensus statement on ETD [1] as well as the results of the long-term follow-up studies of BET published so far in English. Thereafter, we discussed 14 imaginary patient cases (Supplementary File 1) related to ETD, and the members of the society individually voted on each case whether they thought BET was indicated or not. After each case, we discussed the results of the vote before proceeding to the next case. The voting results are shown in the Supplementary Table 1. On the basis of this workshop, the members of the society present in the meeting agreed on indications for BET. After the meeting, the indications were published on the society’s web page and distributed to national ENT colleagues by e-mail.
The Finnish Otosurgical Society’s members largely agreed with the guidelines provided in the consensus statement [1] concerning definition, types, clinical presentation, and diagnostics of ETD. The society wanted to modify the diagnostic work-up so that also middle ear effusion would qualify as a sign of possible chronic dilatory ETD. The society recommends that to diagnose ETD, the patient should have both symptoms and clinical findings referring to ETD. These ear symptoms include a feeling of fullness, popping, discomfort or pain, pressure, clogged feeling, crackling, ringing, or muffled hearing. The evidence of a negative pressure in the middle ear should be reflected either as a negative pressure in tympanogram or as a serous middle ear effusion or retraction of the tympanic membrane in otomicroscopy. In case of baro-challenge-induced dysfunction, the diagnosis is based on the patient history as clinical status is usually normal in the normobaric circumstances of the office.
Chronic rhinosinusitis, nasal polyposis, allergies, gastric reflux, or adenoid hypertrophy should be treated first before considering BET. Also, the patients should be encouraged to quit smoking before proceeding to an operative treatment, even though we do not consider smoking as a contraindication for BET. We also agreed that patients should undergo tympanostomy before BET (excluding baro-challenge-induced dysfunction), as we considered that a positive result with the tympanostomy tube treatment suggests that the patient may benefit from BET. However, if patient has experienced no benefit from tympanostomy tubes, he/she is unlikely to benefit from BET.
Based on the literature and expert opinion given by the society’s members, the Finnish Otosurgical Society recommends that BET may be considered when an adult patient has (i) chronic bothersome symptoms referring to ETD, (ii) ETD-related symptoms following rapid pressure changes, or (iii) recurring serous otitis media taking into account the above-mentioned conditions (Table 3).
Table 3.
Indications for BET by the Finnish Otosurgical Society
|
ETD, Eustachian tube dysfunction; SOM, serous otitis media.
DISCUSSION
Studies on the effect of BET on chronic ETD are heterogeneous regarding patient selection, duration of follow-up, additional conservative or operative treatments given, and outcome measures chosen. Trends in the improvement of symptoms and clinical findings after BET are evident, but for each particular outcome measure, only a couple of studies provide exact results. Therefore, a thorough comparison of all the studies selected for this review is impossible.
During the preparation of this review, Huisman et al. published a systematic review and meta-analysis on the treatment of ETD with BET on the basis of an article search conducted in May 2016 [18]. Of the 103 articles, 15 received critical appraisal. Because of the heterogeneity of the studies, meta-analysis was possible only for four outcomes. It revealed improvements in Valsalva maneuver, otoscopy, tympanometry, and ETS in 3–9 studies. The review excluded studies with only children, and it included studies with follow-up as short as 5–6 weeks [19, 20]. As several studies have shown that the short-term outcome of BET is promising, we were interested in the long-term outcome, which is an important aspect when considering indications for BET.
The effect of BET seems to vary depending on the outcome parameters used. In the studies with a minimum of 12-month follow-up, the Valsalva maneuver improved in 80%–98%, overall subjective symptoms in 73%–98%, otoscopic findings in 90%, tympanometry in 24%–54%, and tubomanometry in 28%–43% of the patients (Table 1d). Two studies with follow-up of 1–3 years presented an improvement in ETS [2, 10]. Two years after BET, 80% of the patients were at least partly satisfied with the result (Table 1e), although only 34% (30 of 89) of the patients responded to the questionnaire asking about satisfaction with the treatment result [10]. In another study, 73% of the patients (all children) were totally or moderately satisfied with the result one year after BET [2]. The limitation in daily life caused by ear symptoms [2] and mean mucosal inflammation score [8] reduced. Aural fullness disappeared in 83% of the patients and the severity of aural fullness, muffled hearing, otalgia, and tinnitus reduced significantly on Visual Analog Scale [11]. Feeling of pressure disappeared in 26%, subjective hearing loss in 21%, and otalgia in 6% [2] of the patients. The results from the studies with 6–11 months of follow-up support these findings of a positive effect of BET (Table 2d and 2e). As indications for BET are inconsistent and the study populations differ in the analyzed studies, predicting the effect of BET on a certain patient group is impossible. Therefore, an open discussion with the patient on expected outcome of BET is an important part of preoperative counseling. However, BET seems to be a safe procedure not only in adults but also in children. No major complications arose, and even minor adverse effects were rare and were resolved during the follow-up (Table 1c and 2c) [2, 8–18].
The balloon catheters used in these 10 studies were officially 3.2–7 mm in diameter and 16–24 mm in length (Tables 1a and 2a). It could be suggested that a balloon with a larger diameter or a longer balloon would produce greater effect, but the longest catheter among the ones used here was the narrowest and the widest was the shortest. In the long-term follow-up group, only one study used the Acclarent device (7 mm × 16 mm) [8], whereas four studies used the Spiggle & Theis catheter (3.2–3.3 mm × 20 mm) [2, 9–11]. The outcome measures vary greatly between these studies making comparisons difficult if not impossible at the moment. On the basis of our review, no trends of thicker or longer balloon dilation catheters producing better outcome are evident. In fact, Acclarent gives the length of the even middle part of the balloon, but the total length of the balloon is unspecified. However, the total length is quite close to that of the Spiggle &Theis balloon.
One objective of treating ETD with BET is to avoid tympanostomies and other otosurgical operations. The cost of BET is significantly higher than that of a one-time tympanostomy. However, with repeating tympanostomies, the costs increase. The need for leave of absence from work in order to come to clinic and other related expenses should also be considered when considering the cost-effectiveness of BET versus repeated tympanostomies or other treatments. However, there are no data available on the total costs of different treatment options.
Liang et al. [12] showed that in 6 months of follow-up, the difference between results of BET with tympanocentesis and BET alone was insignificant. Tympanogram improved from type B to A in 83% of patients receiving BET along with tympanocenthesis and in 80% of those receiving BET only. Both groups showed significant improvement as compared with the third group receiving only tympanocenthesis. However, the evidence to conclude if tympanocenthesis or tympanostomy has additional value to BET is insufficient.
In this review, two studies used specific outcome measures that were applied only in the given study [9, 15]. These seldom used parameters also yield important information but comparing them to some commonly agreed clinical tests would enhance the benefit of the results for clinical work. Therefore, it would be important to agree on definitions and diagnostic parameters of ETD and perform future long-term studies with more uniform outcome measures. Schilder et al. [1] suggested using symptoms, otoscopy, tympanometry, and pure tone audiometry as outcome measures in future studies. Smith et al. [21] studied the reliability of eight tests for ET function and found tubomanometry to be superior. However, they concluded that a single measurement of any clinical test is inadequate in assessing the opening of the ET, and repeating the chosen tests a few times immediately might be helpful. Combining tubomanometry with other clinical tests (as in ETS-7, for example) and numeric symptom evaluation (as in ETDQ-7) seems tempting, but no such composite scores exist till date. There is clearly room for methodological improvement in this respect.
Three long-term studies [8, 9, 11] and three studies with 6 to 11-months of follow-up [13–15] performed CT scans preoperatively mainly to exclude the possibility of damage to the internal carotid artery. With this intent, CT scan seems to be unnecessary [1, 22]. However, some anomalies, such as superior semicircular canal dehiscence or large vestibular aqueduct, may mimic ETD symptoms and are visible in CT scans. CT scans may also be useful in case of problems with insertion of the catheter. Thus, CT may be helpful in selected cases.
The Finnish Otosurgical Society agreed on indications for BET in its meeting in April 2016. Our indications for BET are (i) chronic bothersome symptoms referring to ETD, (ii) ETD-related symptoms following rapid pressure changes, or (iii) recurring serous otitis media. With the current evidence, we suggest using BET for treating only adult patients with ETD. The patient should also have previous positive experience from tympanostomy tube (excluding baro-challenge-induced dysfunction). In our experience, if the patient experiences no benefit from tympanostomy tubes, he/she is unlikely to benefit from BET. We suggest treating chronic rhinosinusitis, nasal polyposis, allergies, gastric reflux, or adenoid hypertrophy prior to BET treatment. We also strongly encourage patients to quit smoking.
Randomized placebo-controlled studies are needed to show the true long-term effect of BET. The effect of the balloon size, nasal pathology, inflammation of the ET mucosa, and some other parameters such as patient’s body mass index need to be studied more thoroughly.
CONCLUSION
Five studies with at least 12-month follow-up fulfilled the inclusion criteria of this review. They suggest that the long-term outcome of BET is promising: Valsalva improved in 80%–98%, overall subjective symptoms in 73%–98%, and otoscopic findings in 90% of the patients. Tympanometry and tubomanometry clearly improved less, in 24%–54% and 28%–43% patients, respectively. Moreover, ETS improved for up to 3 years after treatment with BET. Five additional studies with a follow-up of 6–11 months support the findings from the long-term studies. However, more controlled prospective studies with long-term (>12 months) follow-up and more uniform outcome measures are needed.
On the basis of a workshop at the annual meeting in 2016, the Finnish Otosurgical Society outlined indications for BET. Our indications for BET in adult patients are (i) chronic bothersome symptoms referring to ETD, (ii) ETD-related symptoms in conjunction with rapid pressure changes, or (iii) recurring serous otitis media. At this point, with the lack of evidence, we do not suggest regularly providing BET as treatment for children with ETD. No international indications for BET exist and, to the best of our knowledge, these are the first established indications for BET outlined by a national otosurgical society. These indications will hopefully help clinicians treating ETD patients. They will also provide equality in terms of patient care as well as promote research on ETD and BET by unifying clinical practices.
Supplementary File 1
Exemplary patient cases for voting and discussing indications for BET in the annual meeting of the Finnish Otosurgical Society, April 2016
Case 1
History: An otherwise healthy 42-year-old woman presented with a subjective hearing loss and constant clogged feeling in her both ears. She had a history of few otitis media and experienced pressure and pain in the ears for weeks in association with common colds. Previously, the symptoms had improved with tympanostomy tubes but now she wishes not to have more tubes because she swims as a hobby.
Clinical status: Translucent tympanic membranes with slight retraction and negative Valsalva on both sides of the ear. The nasopharynx is normal. Audiogram reveales normal hearing.
Case 2
History: An otherwise healthy 32-year-old man experienced a few otitis media in childhood. He works as a flight attendant and experiences severe pain in the ears during takeoffs and landings; he has had two secretory otitis media and two perforations of tympanic membrane in history. Previous therapy with local xylometazoline, mometasone, and a combination of acrivastine and pseudoephedrine had little effect on the symptoms. He experiences no subjective hearing impairment.
Clinical status: Tympanic membranes are translucent and easily movable, without retraction. The nasophrarynx is normal, and the ET orifices are open. Rinne test −/−, Weber test shows no lateralization.
Case 3
History: An otherwise healthy 7-year-old boy has had tympanostomy tubes inserted twice because of recurrent otitis media. None of the tubes are now in place, and the otitis media episodes keep recurring.
Clinical status: The tympanic membranes are translucent and easily movable, without any retraction. The nasopharynx is normal, and the ET orifices are open. An audiogram reveales normal hearing.
New tympanostomy has been scheduled.
Case 4
History: An otherwise healthy 37-year-old man has had seven otitis media episodes and two tympanic membrane perforations in the right ear during the last 4 years. He always feels pressure and pain in the right ear during episodes of common cold. He has no ear symptoms in the absence of a common cold.
Clinical status: Right ear: a secondary membrane detected in the lower part of the tympanic membrane, which is easily movable and has a slight retraction. Left ear: normal. Valsalva −/+. An audiogram reveales normal hearing.
Case 5
History: An otherwise healthy 4-year-old girl has had recurring secretory otitis media on both sides since she was 2 years old, with a recurrence immediately when the tympanostomy tubes fall out. Adenotomy was performed earlier and no residual adenoid tonsil was present when the nasopharynx was checked in conjunction with last tympanostomy. Her teenage sister has had tympanostomy tubes inserted 15 times, and she still has recurring secretory otitis media.
Clinical status: Tympanic membrane retractions and thick mucous secretions are observed in both ears. The patient breathes through her nose, but her hearing seems to be impaired.
Her mother has asks if anything else could be done in addition to inserting new tubes.
Case 6
History: An otherwise healthy 25-year-old woman has had frequent tympanostomies because of secretory otitis media since childhood. She received adenotonsillectomy earlier, but now the tubes have fallen out; both her ears remain clogged following a common cold. She is completely tired of repetitive tympanostomies and tubes in her ears. The nasal corticosteroid treatment provided no improvement.
Clinical status: Tympanic membrane retractions present in both ears, with sclerosis in the lower parts. Mucous secretion observed behind the tympanic membranes. The nasopharynx is normal, and the orifices of the ETs are open. Audiogram shows conductive hearing loss on both sides with PTA 35/35 dB.
A new tympanostomy is being suggested, but could BET be considered as treatment?
Case 7
History: An otherwise healthy 33-year-old woman experiences pressure and clogged feeling in the ears as well as tinnitus during common cold. She has a few episodes of otitis media in the history. She swims regularly.
Clinical status: Translucent tympanic membranes are observed. Posterior retraction of pars tensa on both sides, but it moves with pneumatic otoscopy. Valsalva −/−. The nasopharynx is normal. A slight conductive hearing loss is detected in both ears in audiogram, PTA 25/25 dB.
Case 8
History: An otherwise healthy 33-year-old woman experiences pressure and clogged feeling in the ears as well as tinnitus during common cold. She has had few otitis media episodes in the past and does not swim.
Clinical status: She has translucent and easily movable tympanic membranes. No retractions are observed in the pars tensa on either side but deep retractions are seen in pars flaccida on both sides without any deposits in the retractions. Valsalva +/+, Toynbee +/+. The nasopharynx is normal; the audiogram reveales normal hearing.
Case 9
History: An otherwise healthy 57-year-old man presented with an otitis media and tympanic membrane perforation in the right ear 6 months ago. The perforation has not healed yet.
Clinical status: Right ear: a central perforation is observed in the lower anterior part of the tympanic membrane; the middle ear is normal with no secretion. Left ear: the tympanic membrane is translucent with no retraction. Valsalva −/−. The nasopharynx is normal. A conductive hearing loss is detected on the right in the audiogram.
Supplementary Table 1.
Voting results on patient cases
| Case | Specialists routinely performing BET (n=15) | Specialists not routinely performing BET (n=6) | ENT Residents (n=5) | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Yes (n%) | No (%) | Unable to decide (%) | Yes (n%) | No (%) | Unable to decide (%) | Yes (n%) | No (%) | Unable to decide (%) | |
| 1 | 87 | 0 | 13 | 67 | 17 | 17 | 100 | 0 | 0 |
|
| |||||||||
| 2 | 100 | 0 | 0 | 67 | 17 | 17 | 100 | 0 | 0 |
|
| |||||||||
| 3 | 0 | 87 | 13 | 0 | 100 | 0 | 0 | 100 | 0 |
|
| |||||||||
| 4 | 69 | 13 | 19 | 17 | 33 | 50 | 60 | 0 | 40 |
|
| |||||||||
| 5 | 0 | 100 | 0 | 0 | 100 | 0 | 0 | 100 | 0 |
|
| |||||||||
| 6 | 93 | 0 | 7 | 100 | 0 | 0 | 100 | 0 | 0 |
|
| |||||||||
| 7 | 13 | 38 | 50 | 0 | 67 | 33 | 0 | 0 | 100 |
|
| |||||||||
| 8 | 0 | 93 | 7 | 0 | 100 | 0 | 0 | 100 | 0 |
|
| |||||||||
| 9 | 0 | 100 | 0 | 0 | 100 | 0 | 0 | 100 | 0 |
|
| |||||||||
| 10 | 73 | 7 | 20 | 33 | 50 | 17 | 0 | 0 | 100 |
|
| |||||||||
| 11 | 0 | 100 | 0 | 0 | 100 | 0 | 0 | 100 | 0 |
|
| |||||||||
| 12 | 7 | 93 | 0 | 0 | 100 | 0 | 0 | 100 | 0 |
|
| |||||||||
| 13 | 0 | 88 | 13 | 0 | 71 | 29 | 0 | 20 | 80 |
|
| |||||||||
| 14 | 33 | 40 | 27 | 14 | 71 | 14 | 0 | 20 | 80 |
For each patient case (for the description of the cases, see Supplementary File 1), the members of the Finnish Otosurgical Society and the residents present in the meeting voted if they thought that BET was indicated or not or whether they were unable to decide. The votes were divided to three groups according to if the person voting was an ENT specialist routinely performing BET, an ENT specialist not routinely performing BET, or an ENT resident.
BET, balloon Eustachian tuboplasty.
Case 10
History: An otherwise healthy 57-year-old man had an otitis media and tympanic membrane perforation on the right 4 years ago. Myringoplasty with fascia was performed 3 years ago but a new perforation appeared. Another myringoplasty with cartilage and perichondrium was performed two years ago. One year ago, the perforation appeared again. The patient has triathlon as a hobby.
Clinical status: Right ear: a perforation along the border of the tympanic membrane in the anterior lower part and anterior to the cartilage inserted earlier is observed. The tympanum is free of any secretion. Left ear: translucent the tympanic membrane is in the normal position. Valsalva indifferent/+. Nasopharynx is normal, and a slight conductive hearing loss on the right is detected in the audiogram.
Case 11
History: An otherwise healthy 57-year-old man presented with an otitis media 2 years ago for the first time in his life and had a perforation of the tympanic membrane on the right. After that, he has had five episodes of purulent secretion from the right ear.
Clinical status: Right ear: a thick tympanic membrane with central perforation is observed in the lower part. The mucous membrane of the middle ear is swollen and moist. Left ear: a translucent and easily movable tympanic membrane is in the normal position. Valsalva −/−. A conductive hearing loss is observed on the right in an audiogram.
Case 12
History: An otherwise healthy 25-year-old woman has underwent repetitive tympanostomies because of secretory otitis media since childhood. She has received adenotonsillectomy. During the past years, the tubes have stayed in place only for a very short time.
Clinical status: Adhesive tympanic membranes are present on both the sides. Valsalva −/−. Normal nasopharynx. The orifices of the ETs are open. A conductive hearing loss is detected on both sides in the audiogram, PTA 43/43 dB.
Case 13
History: An otherwise healthy 33-year old woman had a secretory otitis media in her childhood and had no ear complaints after that for a long time. The right ear became clogged 6 months ago.
Clinical status: Right ear: retraction cholesteatoma is seen in the posterosuperior part of the pars tensa. Left ear: a retraction is observed in the posterior part of the part tensa. Valsalva −/+. The nasopharynx is normal. A marked conductive hearing loss is observed on the right in the audiogram, PTA 45/12 dB. A CT scan revealed an eroded processus longus of the incus with soft tissue around it; shadowing continuing to the mastoid is also observed.
You have planned a tympanomastoidectomy. But should BET be performed before that?
Case 14
History: An otherwise healthy 33-year-old woman had secretory otitis media in childhood and no ear complaints for a long time after that. Her right ear became clogged 6 months ago.
Clinical status: Right ear: a retraction cholesteatoma is seen in the posterosuperior part of the pars tensa. Left ear: a retraction is observed in the posterior part of part tensa. Valsalva-/+. The nasopharynx is normal. A marked conductive hearing loss on the right is recorded in the audiogram, PTA 45/12 dB. A CT reveales an eroded processus longus of the incus with soft tissue shadowing around it; the soft tissue shadowing continues to the mastoid.
You have planned a tympanomastoidectomy. But should BET be performed in conjunction with it?
Acknowledgements
The authors wish to thank all the members of the Finnish Otosurgical Society and ENT residents that participated in the process of outlining indications for BET in the annual meeting in 2016.
Footnotes
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - V.L., I.K., J.S., J.J., S.T.S.; Design - V.L., I.K., J.S., J.J., S.T.S.; Data Collection and/or Processing - V.L., I.K., S.T.S.; Analysis and/or Interpretation - V.L., I.K., J.S., J.J., S.T.S.; Literature Search - V.L.; Writing Manuscript - V.L., I.K., J.S., J.J., S.T.S.; Critical Review - V.L., I.K., J.S., J.J., S.T.S.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Schilder AG, Bhutta MF, Butler CC, Holy C, Levine LH, Kvaerner KJ, et al. Eustachian tube dysfunction: consensus statement on definition, types, clinical presentation and diagnosis. Clin Otolaryngol. 2015;40:407–11. doi: 10.1111/coa.12475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leichtle A, Hollfelder D, Wollenberg B, Bruchhage KL. Balloon Eustachian Tuboplasty in children. Eur Arch Otorhinolaryngol. 2017;274:2411–2419. doi: 10.1007/s00405-017-4517-8. [DOI] [PubMed] [Google Scholar]
- 3.Ockermann T, Reineke U, Upile T, Ebmeyer J, Sudhoff HH. Balloon dilatation eustachian tuboplasty: a clinical study. Laryngoscope. 2010;120:1411–6. doi: 10.1002/lary.20950. [DOI] [PubMed] [Google Scholar]
- 4.Llewellyn A, Norman G, Harden M, Coatesworth A, Kimberling D, Schilder A, et al. Interventions for adult Eustachian tube dysfunction: a systematic review. Health Technol Assess. 2014;18:1–180. doi: 10.3310/hta18460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schröder S, Lehmann M, Sauzet O, Ebmeyer J, Sudhoff H. A novel diagnostic tool for chronic obstructive eustachian tube dysfunction—the eustachian tube score. Laryngoscope. 2015;125:703–8. doi: 10.1002/lary.24922. [DOI] [PubMed] [Google Scholar]
- 6.McCoul ED, Anand VK, Christos PJ. Validating the clinical assessment of eustachian tube dysfunction: The Eustachian Tube Dysfunction Questionnaire (ETDQ-7) Laryngoscope. 2012;122:1137–41. doi: 10.1002/lary.23223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schröder S, Lehmann M, Korbmacher D, Sauzet O, Sudhoff H, Ebmeyer J. Evaluation of tubomanometry as a routine diagnostic tool for chronic obstructive Eustachian tube dysfunction. Clin Otolaryngol. 2015;40:691–7. doi: 10.1111/coa.12451. [DOI] [PubMed] [Google Scholar]
- 8.Silvola J, Kivekäs I, Poe DS. Balloon Dilation of the Cartilaginous Portion of the Eustachian Tube. Otolaryngol Head Neck Surg. 2014;151:125–30. doi: 10.1177/0194599814529538. [DOI] [PubMed] [Google Scholar]
- 9.Dalchow CV, Loewenthal M, Kappo N, Jenckel F, Loerincz BB, Knecht R. First results of Endonasal dilatation of the Eustachian tube (EET) in patients with chronic obstructive tube dysfunction. Eur Arch Otorhinolaryngol. 2016;273:607–13. doi: 10.1007/s00405-015-3602-0. [DOI] [PubMed] [Google Scholar]
- 10.Schröder S, Lehmann M, Ebmeyer J, Upile T, Sudhoff H. Balloon Eustachian tuboplasty: a retrospective cohort study. Clin Otolaryngol. 2015;40:629–38. doi: 10.1111/coa.12429. [DOI] [PubMed] [Google Scholar]
- 11.Xiong H, Liang M, Zhang Z, Xu Y, Ou Y, Chen S, et al. Efficacy of balloon dilation in the treatment of symptomatic Eustachian tube dysfunction: One year follow-up study. Am J Otolaryngol. 2016;37:99–102. doi: 10.1016/j.amjoto.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 12.Liang M, Xiong H, Cai Y, Chen Y, Zhang Z, Chen S, et al. Effect of the combination of balloon Eustachian tuboplasty and tympanic paracentesis on intractable chronic otitis media with effusion. Am J Otolaryngol. 2016;37:442–6. doi: 10.1016/j.amjoto.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 13.Poe DS, Silvola J, Pyykkö I. Balloon dilation of the cartilaginous eustachian tube. Otolaryngol Head Neck Surg. 2011;144:563–9. doi: 10.1177/0194599811399866. [DOI] [PubMed] [Google Scholar]
- 14.McCoul ED, Anand VK. Eustachian tube balloon dilation surgery. Int Forum Allergy Rhinol. 2012;2:191–8. doi: 10.1002/alr.21007. [DOI] [PubMed] [Google Scholar]
- 15.Bast F, Frank A, Schrom T. Balloon dilatation of the Eustachian tube: postoperative validation of patient satisfaction. ORL J Otorhinolaryngol Relat Spec. 2013;75:361–5. doi: 10.1159/000358254. [DOI] [PubMed] [Google Scholar]
- 16.Bowles PF, Agrawal S, Salam MA. Balloon tuboplasty in patients with Eustachian tube dysfunction: a prospective study in 39 patients (55 ears) Clin Otolaryngol 2017. 2017;42:1057–60. doi: 10.1111/coa.12812. [DOI] [PubMed] [Google Scholar]
- 17.Dai S, Guan GF, Jia J, Li H, Sang Y, Chang D, et al. Clinical evaluation of balloon dilation eustachian tuboplasty surgery in adult otitis media with effusion. Acta Otolaryngol. 2016;136:764–7. doi: 10.3109/00016489.2016.1159328. [DOI] [PubMed] [Google Scholar]
- 18.Huisman JML, Verdam FJ, Stegeman I, de Ru JA. Treatment of Eustachian tube dysfunction with balloon dilation: A systematic review. Laryngoscope. 2017 Aug 11; doi: 10.1002/lary.26800. doi: 10.1002/lary.26800. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 19.Kivekäs I, Chao WC, Faquin W, Hollowell M, Silvola J, Rasooly T, et al. Histopathology of balloon-dilation Eustachian tuboplasty. Laryngoscope. 2015;125:436–41. doi: 10.1002/lary.24894. [DOI] [PubMed] [Google Scholar]
- 20.Jurkiewicz D, Bień D, Szczygielski K, Kantor I. Clinical evaluation of balloon dilation Eustachian tuboplasty in the Eustachian tube dysfunction. Eur Arch Otorhinolaryngol. 2013;270:1157–60. doi: 10.1007/s00405-012-2243-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith ME, Zou CC, Baker C, Blythe AJ, Hutchinson PJ, Tysome JR. The repeatability of tests of eustachian tube function in healthy ears. Laryngoscope. 2017 Feb 22; doi: 10.1002/lary.26534. doi: 10.1002/lary.26534. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 22.Abdel-Aziz T, Schröder S, Lehmann M, Gehl HB, Ebmeyer J, Sudhoff H. Computed tomography before balloon Eustachian tuboplasty – a true necessity? Otol Neurotol. 2014;35:635–8. doi: 10.1097/MAO.0000000000000214. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1.
Voting results on patient cases
| Case | Specialists routinely performing BET (n=15) | Specialists not routinely performing BET (n=6) | ENT Residents (n=5) | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Yes (n%) | No (%) | Unable to decide (%) | Yes (n%) | No (%) | Unable to decide (%) | Yes (n%) | No (%) | Unable to decide (%) | |
| 1 | 87 | 0 | 13 | 67 | 17 | 17 | 100 | 0 | 0 |
|
| |||||||||
| 2 | 100 | 0 | 0 | 67 | 17 | 17 | 100 | 0 | 0 |
|
| |||||||||
| 3 | 0 | 87 | 13 | 0 | 100 | 0 | 0 | 100 | 0 |
|
| |||||||||
| 4 | 69 | 13 | 19 | 17 | 33 | 50 | 60 | 0 | 40 |
|
| |||||||||
| 5 | 0 | 100 | 0 | 0 | 100 | 0 | 0 | 100 | 0 |
|
| |||||||||
| 6 | 93 | 0 | 7 | 100 | 0 | 0 | 100 | 0 | 0 |
|
| |||||||||
| 7 | 13 | 38 | 50 | 0 | 67 | 33 | 0 | 0 | 100 |
|
| |||||||||
| 8 | 0 | 93 | 7 | 0 | 100 | 0 | 0 | 100 | 0 |
|
| |||||||||
| 9 | 0 | 100 | 0 | 0 | 100 | 0 | 0 | 100 | 0 |
|
| |||||||||
| 10 | 73 | 7 | 20 | 33 | 50 | 17 | 0 | 0 | 100 |
|
| |||||||||
| 11 | 0 | 100 | 0 | 0 | 100 | 0 | 0 | 100 | 0 |
|
| |||||||||
| 12 | 7 | 93 | 0 | 0 | 100 | 0 | 0 | 100 | 0 |
|
| |||||||||
| 13 | 0 | 88 | 13 | 0 | 71 | 29 | 0 | 20 | 80 |
|
| |||||||||
| 14 | 33 | 40 | 27 | 14 | 71 | 14 | 0 | 20 | 80 |
For each patient case (for the description of the cases, see Supplementary File 1), the members of the Finnish Otosurgical Society and the residents present in the meeting voted if they thought that BET was indicated or not or whether they were unable to decide. The votes were divided to three groups according to if the person voting was an ENT specialist routinely performing BET, an ENT specialist not routinely performing BET, or an ENT resident.
BET, balloon Eustachian tuboplasty.


