Abstract
OBJECTIVES
The aim of this study was to quantify the natural behavior of asymptomatic deep pars tensa retraction in both adults and children.
MATERIALS and METHODS
Asymptomatic pars tensa retraction pockets that contacted the promontory were included. Persistently symptomatic pars tensa retraction, pars tensa retraction that did not contact the promontory, patients with attic retraction pockets and patients with cholesteatoma were excluded. Patients were followed up annually and were eliminated from the study if they required active intervention or recovered so that their ears were persistently ventilated with no contact of the tympanic membrane to the promontory. Outcome variables included surgical intervention, surgical intervention for cholesteatoma, and spontaneous improvement and were studied using the life table method.
RESULTS
In total, 64 children and 25 adults were enrolled, of whom 19 children and five adults required intervention and five children and two adults developed pars tensa cholesteatomas. No significant difference was observed between children and adults. In total, three children, but no adults, developed attic cholesteatomas without progression of the pars tensa disease. Furthermore, the ears of 20 children, but not even one adult ear, returned to normal over the 10-year study period.
DISCUSSION
Most retracted adult ears did not change. Over 10 years, the most common finding in children was the return of their ears to normal. Ear of all children recovered during the second decade. Deterioration to form cholesteatoma was not influenced by age. Attic cholesteatoma without the progression of pars tensa disease was observed in children, but not in adults.
Keywords: Tympanic membrane, cholesteatoma, middle ear, age groups
INTRODUCTION
Pars tensa retraction occurs when areas of the tympanic membrane that lack a fibrous layer are displaced medially in the presence of reduced middle ear pressure [1]. A proportion may become associated with otalgia, reduced hearing, or otorrhoea. Persistently symptomatic pars tensa retraction is treatable [2]. However, there is some debate regarding the optimum treatment of pars tensa retractions that remain asymptomatic. The controversy hinges on the relationship between pars tensa retraction and cholesteatoma; it has been established that a proportion of pars tensa retractions may act as a precursor to cholesteatoma, and some authorities justify surgical intervention for asymptomatic pars tensa retraction on the grounds of prophylaxis against cholesteatoma formation [3–6]. However, surgery is associated with risks to the patient, such as sensorineural hearing loss, worsening of conductive hearing loss, dizziness, tinnitus, facial palsy, generation of residual cholesteatoma, and perforation of the pars tensa, each of which is a burden to a previously asymptomatic patient. The clinical judgement as to whether prophylactic intervention is justifiable or reckless may be refined by quantitative information regarding the natural behavior of the untreated pars tensa retraction.
Scientific data on the natural history of asymptomatic pars tensa retraction are limited. Four studies, namely two population-based [7, 8], and two hospital-based [9, 10] studies, on retraction as part of the otitis media spectrum have been published. Limited by their study sample, these studies largely deal with shallow retraction and do not provide guidance on the association of cholesteatoma with pars tensa retraction. A previous study on pars tensa retraction was biased by recruitment of large numbers of patients with mild, generalized retraction without pars tensa atrophy. Nonetheless, this study revealed that such early disease rarely progresses to atrophy. Accordingly, we consider this stage to be the best considered part of the otitis media spectrum [11]. Only one other long-term observational study directed specifically at the natural history of pars tensa retraction has been published. This study noted that approximately 10%–20% of all pars tensa retractions deteriorate during the study period. However, only a small proportion (2%) of an advanced group progressed to form cholesteatoma over an average follow-up period of 3 years [3]. In that study, the number of advanced retractions was low, and various interventions were performed on the patients, thereby making it more difficult to assess the natural behavior of these ears.
It is important to note that the present study also identified some ears that ceased to retract and spontaneously returned to normal. It follows that it would be unjustifiable to offer prophylactic surgery to any subgroup that had the propensity to behave in this way.
We believed that there was room to learn more about the risk of progression of asymptomatic retracted ears to form cholesteatoma and to evaluate the potential of retracted ears to return to normal. We designed a longitudinal observational study of one subgroup of pars tensa retractions, those that contact the promontory (deep pars tensa retraction) but do not cause symptoms. This type of retraction is related to the subgroup identified by Sade as having the highest risk of deterioration to cholesteatoma.
The aim of the present study was to establish the rate at which asymptomatic deep pars tensa retraction (ADPTR) progresses to require surgical intervention as well as the rate at which they improve to cease presenting a risk of deterioration. Our secondary aim was to investigate whether any clinical features at presentation are associated with subsequent deterioration or improvement of the retraction.
MATERIALS and METHODS
This study was performed in compliance with the ethical principles of, and was approved by, the Hospital Quality Improvement board. Data was anonymized, and treatment was provided in accordance with standard clinical practice, consistent with the ethical standards of the Declaration of Helsinki [12]. Consent was not required for this retrospective survey of normal practice.
Probands were retrospectively included into this study from general otology clinics of the senior author’s practice in secondary care over the period 2003–2012. Only patients with asymptomatic pars tensa retraction pockets that contacted the promontory were included. Ears that were persistently symptomatic on presentation, pars tensa retraction that did not contact the promontory, patients with attic retraction pockets, and patients with cholesteatoma were excluded. All age groups were enrolled.
Patients were followed up annually. The physical appearance of the ear was noted at each visit. The following parameters were recorded: patient age, month of the year, new symptoms, retraction appearance (touching the promontory or not), erosion of ossicles (intact chain or not), erosion of the posterior annulus (yes or no), presence of keratin debris within the retracted area (yes or no), and presence of a middle ear effusion (yes or no). A pure tone audiogram was performed at each visit, and the conductive hearing loss was recorded according to the recommendations of the American Academy of Otolaryngology-Head and Neck Surgery [13].
If the ear became symptomatic, the patient was provided with appropriate medical treatment and reviewed again in 3 months. If the ear returned to being asymptomatic, the patient returned for annual follow-up. If not, the patient was again treated by medical means and reviewed again for 3 months. If improvement was observed, the patient returned for annual follow-up. If not, the patient was considered for surgical treatment.
The ears were considered healthy if they had two consecutive annual clinic visits without symptoms in the preceding year and on otoscopy on each occasion, were found to have a ventilated middle ear space with a tympanic membrane no longer in contact with the promontory.
Follow-up was censored by surgical intervention, improvement, or becoming lost to follow-up. Otherwise, patients were followed up until the trial ceased.
Data were analyzed using SPSS version 24 (IBM Corporation, Armonk, USA). The Kaplan–Meier method was used to estimate the behavior of the ears over time after surgery with the following outcomes: surgical intervention, surgical intervention for cholesteatoma, and spontaneous improvement [14]. Testing of the association of baseline factors measured at initial presentation with the survival function for each of the above outcomes was performed using Cox’s proportional hazards regression model [15].
RESULTS
The study group comprised 89 patients, 25 of whom were adults and 64 were children. Figure 1 shows the age distribution of the study sample.
Figure 1.
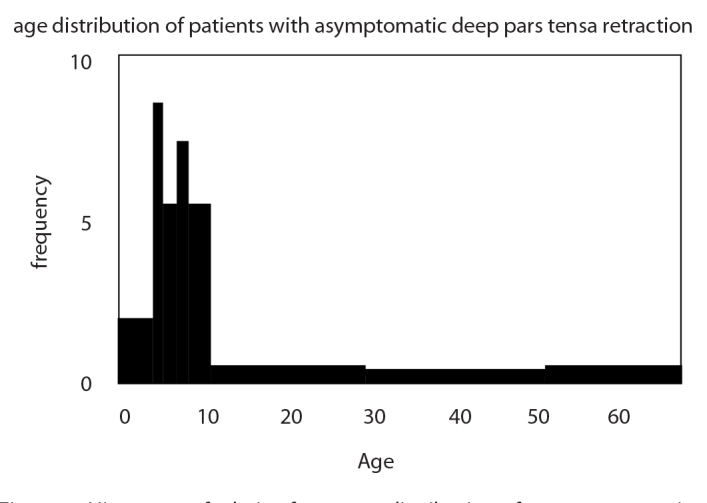
Histogram of relative frequency distribution of age at presentation of patients with ADPTR in the present study
Twenty-four ears required surgical intervention for pain, hearing loss, ear discharge, or the development of cholesteatoma within 5 years (Figure 2). Overall, 19 patients first seen as children and five adults required treatment. Four of these children were adults by the time that they required surgical treatment.
Figure 2.
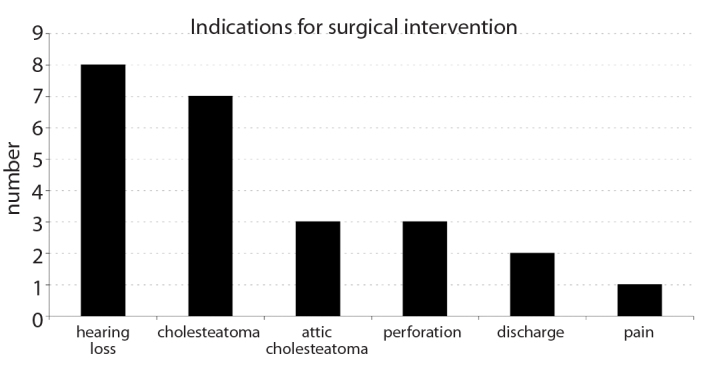
Indications for surgery in the ears with deep pars tensa retraction that, at presentation, was asymptomatic
The proportion of children who did not need surgical intervention was 0.76 (CI 0.66–0.86) at 5 years. The proportion of adults surviving without surgical intervention was 0.86 (CI 0.72–1.00) over the same interval. By 10 years, the corresponding statistics were 0.74 (CI 0.60–0.88) for children and 0.72 (CI 0.50–0.94) for adults. The behavior of these two groups was not noticeably different (Wilcoxon signed-rank test, p=0.97; Figure 3).
Figure 3.
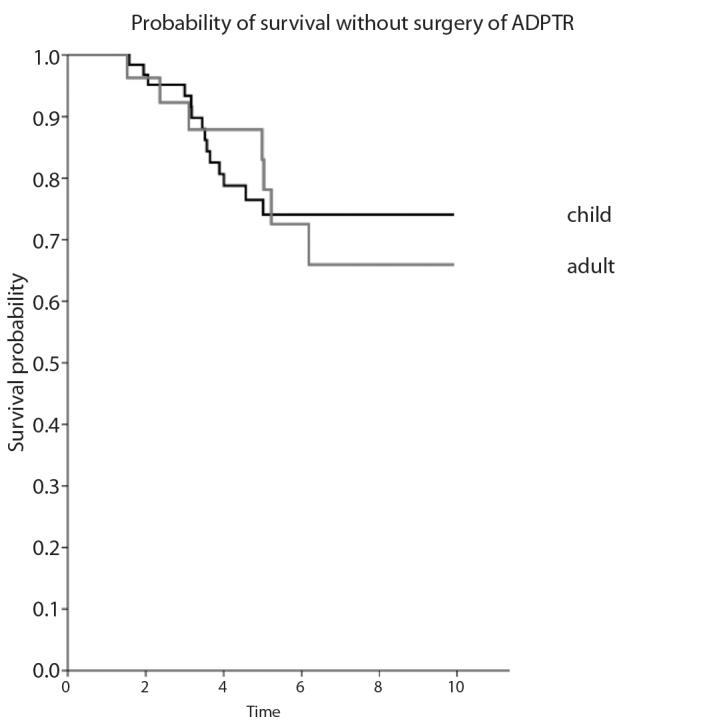
Comparison of Kaplan–Meier estimates of time dependent rates of surgical intervention in adults and children with ADPTR at presentation. No significant statistical difference was observed in the rates of overall surgical intervention between the two groups (log-rank test, P = 0.97)
Of these ears, seven required intervention for pars tensa cholesteatoma within 10 years. Five patients who were first seen as children and two adults required treatment. The proportion of children not requiring surgery for pars tensa cholesteatoma was 0.91 (CI 0.83–0.99) at 5 years. The proportion of adults surviving without surgery for cholesteatoma was 0.90 (CI 0.78–1.00) over the same interval. The corresponding statistics at 10 years were 0.88 (CI 0.76–1.00) for children and 0.88 (CI 0.72–1.00) for adults. There was no statistically significant difference between these two groups (Wilcoxon signed-rank test, p=0.99; Figure 4). In addition, three children presented with deep pars tensa retraction and subsequently developed attic cholesteatomas without the progression of pars tensa changes.
Figure 4.
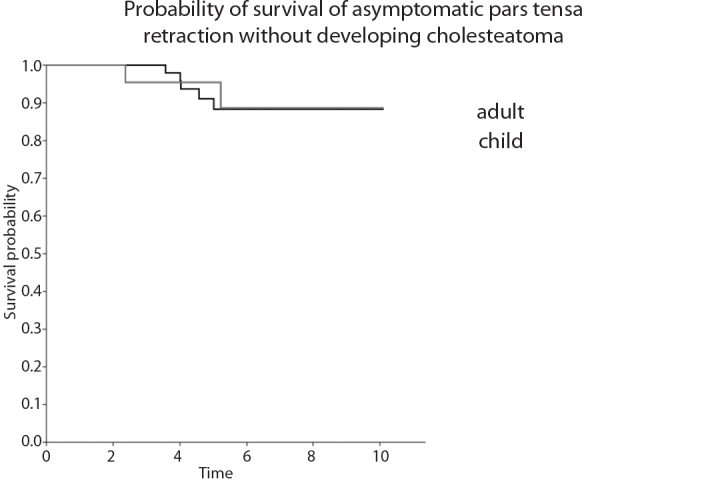
Comparison of Kaplan–Meier estimates of rates of time dependent surgical intervention for pars tensa cholesteatoma in adults and children with ADPTR at presentation. No significant statistical difference was observed in the rates of conversion to cholesteatoma between the two groups (log-rank test, p=0.81)
In total, nine ears spontaneously improved within 5 years, all of which were of children. No adult ear improved spontaneously. By 10 years, the ears of 20 children had improved spontaneously, but not one adult’s ear had improved. The proportion of children whose ears improved at 5 years was 0.19 (CI 0.09–0.29), which increased to 0.56 (CI 0.38–0.74) by 10 years. The difference between these two groups was significant (Wilcoxon signed-rank test, p=0.006; Figure 5).
Figure 5.
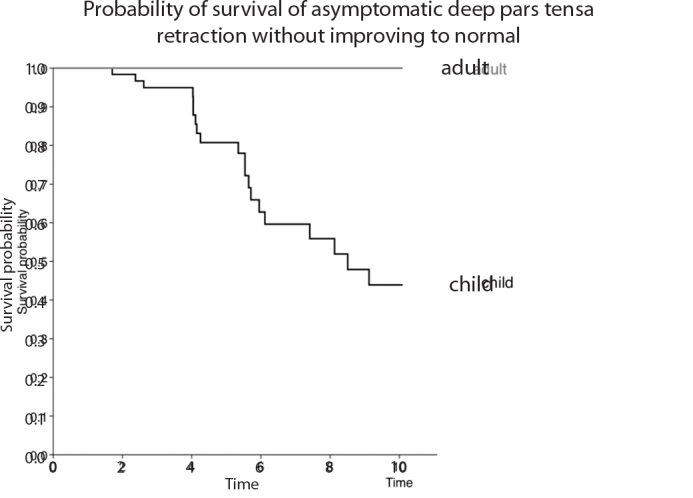
Comparison of Kaplan–Meier estimates of time dependent rates of spontaneous recovery to persistent ventilated ear in adults and children with ADPTR at presentation. The visually obvious difference between the two groups was statistically significant (log-rank test, p=0.002)
No baseline variates were associated with progression to surgery, whether for cholesteatoma or other reasons. Because no adult ear showed improvement, Cox’s regression analysis against improvement was restricted to children only. No baseline variates were associated with a subsequent improvement to normal.
DISCUSSION
The present study identified a statistically significant difference in the behavior of ADPTR between children and adults. Children’s ears have the potential to recover to normal. In children, ADPTR is more likely to end in resolution than in progression to cholesteatoma or any other symptomatic state, such as hearing loss due to ossicular erosion or recurrent otalgia. The distribution of age at which children’s retracted ears spontaneously recovered to normal was centered around the 13th year (median: 12.6 years) with a narrow spread (interquartile range: 3.9 years). Half of the patients who improved were between 12.0 and 14.9 years old. No patient in the present study recovered spontaneously after 19 years of age. There appears to be an interval in the second decade for recovery, in which even deep pars tensa retraction can return to normal (Figure 6). The argument that the pars tensa retracted onto the promontory should undergo prophylactic surgery because it will reduce the risk of ear damage or hearing loss secondary to inevitable progression to cholesteatoma can be confidently rejected in children. Many of these ears returned to normal, with no evidence of a middle ear ventilation disorder. The grounds for rejection of this argument in adults is less sure as no adult ear was devoid of the risk of cholesteatoma in the same manner as children’s ears. Furthermore, our sample size of adults was small.
Figure 6.
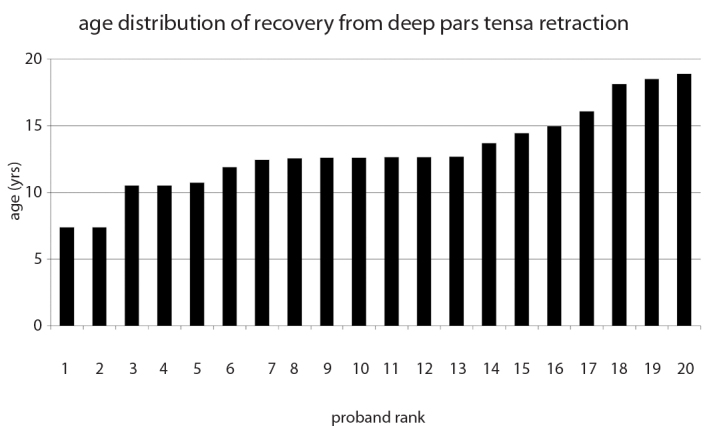
The age distribution of the group of patients who spontaneously developed persistent middle ear ventilation without pars tensa retraction having presented with ADPTR
Progression to cholesteatoma occurred across all age groups, even in the second decade. The progression to disease was measured in years, and therefore, a follow-up interval of 12 months seems appropriate. The extent of cholesteatoma in all these ears was much more circumscribed than generally associated with pediatric cholesteatoma. This suggests that progression from deep pars tensa retraction to cholesteatoma is not be the typical pathogenesis of acquired cholesteatoma. The etiology of the disease arising from the pars tensa that initially presents as cholesteatoma may be different from that which presents initially as ADPTR and then progresses. The former may be extensive even in young children, whereas the latter progresses much more slowly and does not extend widely even over the span of a decade. We were also interested in identifying cases of children alone in whom a spatially distinct cholesteatoma arose without progression of the presenting pars tensa pathology. We intend to explore this interesting and relatively unknown phenomenon in a different study.
We did not identify any factors that were predictive of progression to cholesteatoma. This may be owing to several reasons, including the small number of ears that developed cholesteatoma, indicating that the present study may not have had sufficient statistical power to discern effects from baseline variates. The output of the analysis can only be based on the input measurements. Our data were limited to simple clinical measurements. Although it would have been clinically convenient to identify the risk factors among such readily collected information, perhaps it was optimistic to expect simple clinical data from an initial visit to influence progression to cholesteatoma many years later. We did not collect any physiological data about nasal, eustachian tube, or mastoid function. Previous studies have found such factors that are associated with subsequent conversion to cholesteatoma.
Magnuson identified sniffing, directed at relieving middle ear symptoms, as a risk factor for recurrent cholesteatoma after primary surgery [16]. Mansour et al. [17] asserted that soft tissue density in the anterior epitympanic recess represents an unfavorable prognosis for pars tensa retraction, although their study sample with pars tensa disease was very small. The presence of a small mastoid is associated with the ears that have cholesteatoma [18, 19]. However, the association need not imply prediction, so the value of such measures remains to be established. As clinical factors alone do not provide accurate information to identify the ears that will deteriorate to form cholesteatoma, future studies should consider including these physiological and radiological measures for testing. Sade measured a higher rate of conversion to cholesteatoma in the group with pars tensa retraction adherent to the promontory [3]. The present study did not differentiate between pars tensa retraction that merely contacted the promontory and that which was adherent to the promontory. The children repeatedly found the intervention to determine fixation to the promontory to be uncomfortable, and we did not feel that repeated painful assessment in the clinic could be justified. We restricted our assessment of the ears to visual inspection and pure tone audiometry and could therefore not assess whether fixation to the promontory was an independent risk factor for cholesteatoma.
The present study was performed in secondary care. Our patients required a reason to be referred from primary care to our clinics, so many were symptomatic when first seen, and few were referred as incidental findings. We filtered and excluded the initially symptomatic ears from the present study, so the age distribution that we encountered may not reflect that of pars tensa retraction onto the promontory in the general community. There may be a larger proportion of adults with asymptomatic retracted ear drums in the general population. Accordingly, ENT surgeons in countries with different referral patterns may be exposed to a quite different sampling of the general population [3, 20].
Despite the limitations of the study described above, we expect that the distinct behavior of asymptomatic deep retraction of the pars tensa in children and adults should be reproducible and that the conclusions reached should be relevant to the clinical practice.
CONCLUSION
The behavior of asymptomatic pars tensa retractions significantly differs between children and adults. There is a substantial likelihood that such ears in children will recover spontaneously. The period of opportunity for this phenomenon is limited to the second decade. Accordingly, it is not reasonable to undertake prophylactic surgery on asymptomatic deeply retracted ears in children. There is no simple clinical means of identifying which ears will deteriorate to accumulate keratin debris in the pars tensa retraction, a phenomenon that is not influenced by age. In children, the pars tensa retraction may remain unchanged while the pars flaccida deteriorates to form cholesteatoma.
Footnotes
Politzer Prize Finalist - 31st Politzer Society Meeting - 21–24 February 2018, Las Palmas de Gran Canaria, Spain
Ethics Committee Approval: Authors declared that the research approved by hospital quality improvement board (Gloucestershire Hospitals Trust. Number: SP0048; Date: 01/07/2015).
Informed Consent: Informed consent is not necessary due to the retrospective nature of this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – J.H.; Design - J.H.; Supervision - J.H.; Materials - J.H.; Data Collection and/or Processing - J.H., M.N., J.C., B.T.; Analysis and/or Interpretation - J.H., J.C., B.T.; Literature Search - M.N., J.C., B.T., J.H.; Writing - J.C., J.H.; Critical Reviews - M.N., J.C.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Sade J. Secretory Otitis media and its sequelae. London: Churchill Livingstone Publ; 1979. The atelectatic ear; pp. 64–88. [Google Scholar]
- 2.Black B. The collapsed pars tensa: surgical classification and management. In: Magnan J, Chays A, editors. Proceedings of the 6th International Conference on Cholesteatoma and Ear Surgery; 2000; Cannes, France. Marseille: Label Publications; 2001. pp. 267–9. [Google Scholar]
- 3.Sade J, Avraham S, Brown M. Atelectasis, retraction pockets and cholesteatoma. Acta Otolaryngol. 1981;92:501–12. doi: 10.3109/00016488109133289. [DOI] [PubMed] [Google Scholar]
- 4.Tos M. Can cholesteatoma be prevented? In: Cholesteatoma and Mastoid Surgery. Proceedings of the 2nd International Conference; 1981; Jerusalem, Israel. Amsterdam: Kugler Publications; 1982. pp. 591–7. [Google Scholar]
- 5.Charachon R, Barthez M, Lejeune J. Spontaneous retraction pockets In Chronic Otitis Media Medical and Surgical Therapy. ENT Journal. 1992;71:578–83. [PubMed] [Google Scholar]
- 6.Borgstein J, Gerritsma T, Bruce I, Feenstra L. Atelectasis of the middle ear in paediatric patients: safety of surgical intervention. Int J Pediatr Otorhinolaryngol. 2009;73:257–61. doi: 10.1016/j.ijporl.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 7.Maw AR, Hall AJ, Pothier DD, Gregory SP, Steer CD. The prevalence of tympanic membrane and related middle ear pathology in children: a longitudinal cohort study followed from birth to age ten. Otol Neurotol. 2011;32:1256–61. doi: 10.1097/MAO.0b013e31822f10cf. [DOI] [PubMed] [Google Scholar]
- 8.De Beer BA, Schilder AG, Zielhuis GA, Graamans K. Natural course of tympanic membrane pathology related to otitis media and ventilation tubes between ages 8 and 18 years. Otol Neurotol. 2005;26:1016–21. doi: 10.1097/01.mao.0000185058.89586.ed. [DOI] [PubMed] [Google Scholar]
- 9.Maw AR, Bawden R. Tympanic membrane atrophy, scarring, atelectasis and attic retraction in persistent, untreated otitis media with effusion and following ventilation tube insertion. Int J Pen Otolaryngol. 1994;30:189–204. doi: 10.1016/0165-5876(94)90060-4. [DOI] [PubMed] [Google Scholar]
- 10.Yale L, Hunter L, Margolis R, Levine S, Lindgren B, Daly K, Giebink GS. Prospective study of tympanic membrane retraction, hearing loss, and multifrequency tympanometry. Otolaryngol Head Neck Surg. 1999;121:514–22. doi: 10.1016/S0194-5998(99)70049-5. [DOI] [PubMed] [Google Scholar]
- 11.Tay HL, Mills RP. Tympanic membrane atelectasis in childhood otitis media with effusion. Journal Laryngol Otol. 1995;109:495–8. doi: 10.1017/S0022215100130555. [DOI] [PubMed] [Google Scholar]
- 12.World Medical Association. Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2000;284:3043–5. doi: 10.1001/jama.284.23.3043. [DOI] [PubMed] [Google Scholar]
- 13.Committee on Hearing and Equilibrium guidelines for the evaluation of results of treatment of conductive hearing loss. American Academy of Otolaryngology-Head and Neck Surgery Foundation, Inc. Otolaryngol Head Neck Surg. 1995;113:186–7. doi: 10.1016/S0194-5998(95)70103-6. [DOI] [PubMed] [Google Scholar]
- 14.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Amer Statist Assn. 1958;53:457–81. doi: 10.1080/01621459.1958.10501452. [DOI] [Google Scholar]
- 15.Cox DR. Regression Models and Life-Tables. Journal of the Royal Statistical Society, Series B. 1972;34:187–220. [Google Scholar]
- 16.Magnuson B. Tympanoplasty and recurrent disease: sniff-induced high negative pressure in the middle ear space. Am J Otolaryngol. 1981;2:277–83. doi: 10.1016/S0196-0709(81)80002-6. [DOI] [PubMed] [Google Scholar]
- 17.Mansour S, Magnan J, Haidar H, Nicolas K. Tympanic Membrane Retraction Pocket. Switzerland: Springer International Publishing; 2015. Management of Retraction Pockets; pp. 58–68. [DOI] [Google Scholar]
- 18.Diamant M. The ‘pathologic size’ of the mastoid air cell system. Acta Otolaryngol. 1965;60:1–10. doi: 10.3109/00016486509126982. [DOI] [PubMed] [Google Scholar]
- 19.Sade J, Fuchs C. A comparison of mastoid pneumatization in adults and children with cholesteatoma. Eur Arch Otorhinolaryngol. 1994;251:191–5. doi: 10.1007/BF00628421. [DOI] [PubMed] [Google Scholar]
- 20.Grewal DS, Hathiram BT, Moliorikar AV, Davis S, Rajeevan T. Retraction pockets in chronic suppurative otitis media- our experience. Indian J Otolaryngol Head Neck Surg. 2003;55:107–12. doi: 10.1007/BF02974614. [DOI] [PMC free article] [PubMed] [Google Scholar]


