Abstract
This clinical report describes and evaluates a novel periosteal flap design. This technique was applied in 26 patients who underwent cochlear implantation surgery at two tertiary referral centers. No complications were observed during or after the surgery. Additionally, there was no evidence of device migration, wound infection, wound hematoma, or delayed wound healing. Notably, the mastoid emissary vein was intact in all cases. In conclusion, this modified anterior-based periosteal flap is a safe procedure and is aimed at avoiding mastoid emissary vein bleeding and allowing complete repositioning of the periosteum over the implanted device.
Keywords: Cochlear implant, periosteal flap, subperiosteal pocket
INTRODUCTION
Numerous skin incisions and flap designs have been described and used for cochlear implantation surgery. A postauricular incision and an anterior-based periosteal flap are commonly used by many surgeons for cochlear implantation [1, 2]. Many surgeons nowadays prefer minor skin incisions and minimally invasive techniques.
Special attention should be directed toward the incision and flap design to minimize the surgical complications of cochlear implantation, which were historically related to the flaps or improper electrode insertion [3]. This study is a description and evaluation report of a novel periosteal flap design.
PATIENT and METHOD
This technique was applied in 26 patients who underwent cochlear implantation surgery at two tertiary referral centers (16 and 10 patients were operated by the first and second author, respectively). The study population comprised 15 males and 11 females; 17 and 9 cases included children and adults, respectively. The age of the children ranged from 7 to 50 m, and the age of adults ranged from 32 to 75 y.
All described procedures in this article are in accordance with the ethical standards of the Institutional Research Committee (Zagazig University 2016) and the 1964 Helsinki Declaration. All patients or their parents signed an informed consent, and all steps of the procedure were explained before the surgery.
Surgical Procedure
The surgeries were performed under general anesthesia without the use of paralytic agents to facilitate facial nerve monitoring.
The skin incision was performed 2–5 mm posterior to the postauricular sulcus in the postauricular area, and it extended from just above the mastoid tip to the upper edge of the auricular attachment.
Supraperiosteal scalp flaps were then anteriorly and posteriorly raised, allowing the pericranium and temporalis fascia to remain fixed. These flaps are elevated anteriorly toward the external auditory canal and posteriorly to allow good exposure for performing the periosteal incisions, accessing the subperiosteal pocket and creating the bony well.
A short anteriorly based periosteal flap is then formed between three incisions: The first incision is along the temporal line at the lower border of the temporalis muscle, which is approximately 2–3 cm in length; the second incision is just above the mastoid tip and isposteriorly curved; and the third vertical incision connects the first and second incisions (Figure 1).
Figure 1.
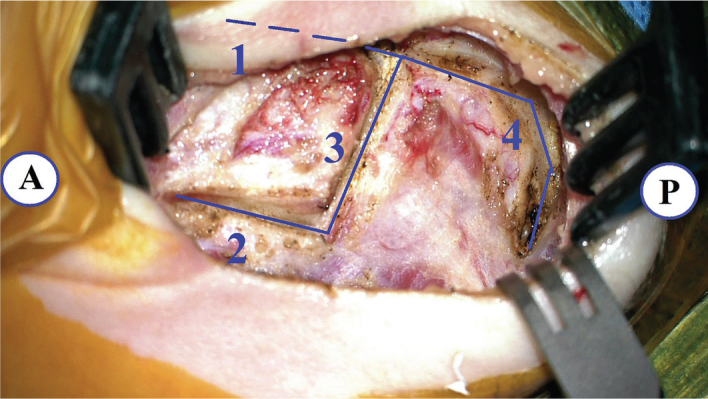
The periosteal incisions of the left ear
A = anterior; P = posterior; 1, 2, 3 = the superior, inferior, and vertical incisions of the anterior flap, respectively; 4 = extension of the superior incision
Further, the superior horizontal incision is posteriorly extended to approximately 3 cm, and it is further gently curved downward and backward to approximately 2 cm (Figure 1). A small piece of pericranium is excised for the purpose of packing around the electrode within the cochleostomy.
The anteriorly based periosteal flap (Palva flap) is carefully elevated to the external auditory canal and anteriorly fixed by a suture or tissue hook. The other inferiorly based periosteal flap is partially and carefully elevated to avoid disruption of the mastoid emissary vein (Figure 2).
Figure 2.
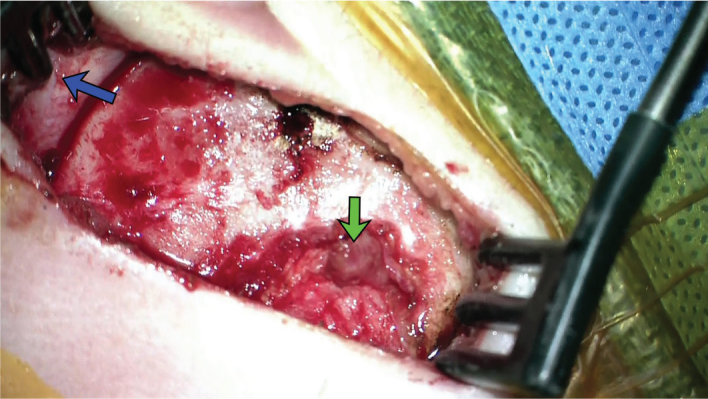
The anterior- and inferior-based periosteal flaps
Left blue arrow = anterior-based periosteal flap and downward green arrow = inferior-based periosteal flap
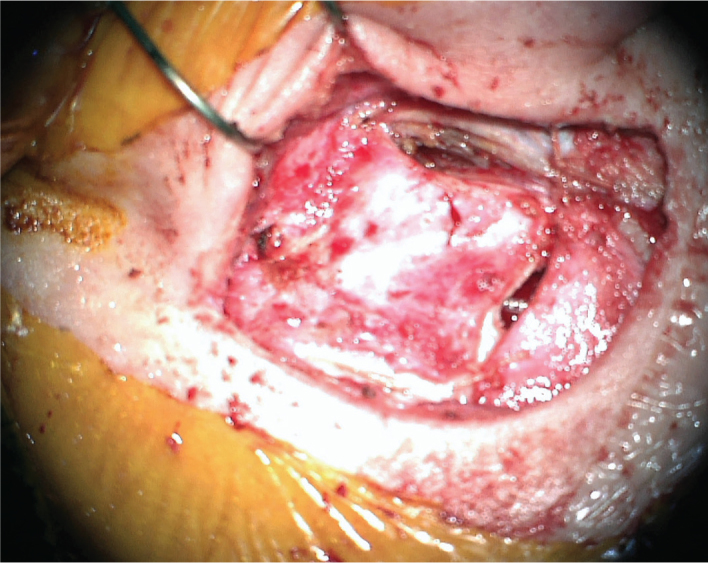
A posterosuperior subperiosteal pocket for the receiver/stimulator is created with a periosteal or freer elevator at an angle of 45° using the canthomeatal line. The dissection initiates below the downward curvature of the upper periosteal incision. The size of this pocket is determined by the size of the receiver/stimulator and can be measured with the appropriate implant template. The receiver/stimulator well or seat is then created using a cutting or diamond burs (Figure 3).
Figure 3.

The subperiosteal well created in the subperiosteal pocket for the receiver/stimulator
Mastoidectomy, posterior tympanotomy, and cochleostomy are typically performed. Additionally, a groove is drilled for the electrode lead wires connecting the receiver/stimulator seat to the mastoidectomy cavity. The whole field is then irrigated free of all blood and bone dust, hemostasis is obtained, and the receiver/stimulator is placed in its seat in the subperiosteal pocket. The inferior-based periosteal flap is placed over the device and sutured with 2/0 ticron suture (non-absorbable braided nylon suture) (Figure 4). This suture should connect the inferior and superior sides of the curving periosteal incision, and it should be tightly secured to hold the device in place, preventing anterior migration.
Figure 4.

Tie-down suture (blue arrow)
The electrode lead wires are placed in the groove; then, electrode insertion is performed, and the cochleostomy is packed by periosteum. An absorbable (vicryl 2/0) suture is placed connecting the anterior-based flap, the inferior-based flap, and temporalis muscle (Figure 5).
Figure 5.
Periosteum was easily repositioned with only two sutures in the corners of periosteal flaps
Other absorbable sutures (vicryl 2/0) are placed between the periosteal flaps aiming at almost total coverage of the device and the electrode by periosteum (Figure 6). The skin is then closed in the usual fashion with deep interrupted inverted vicryl and subcuticular monocryl continuous sutures.
Figure 6.
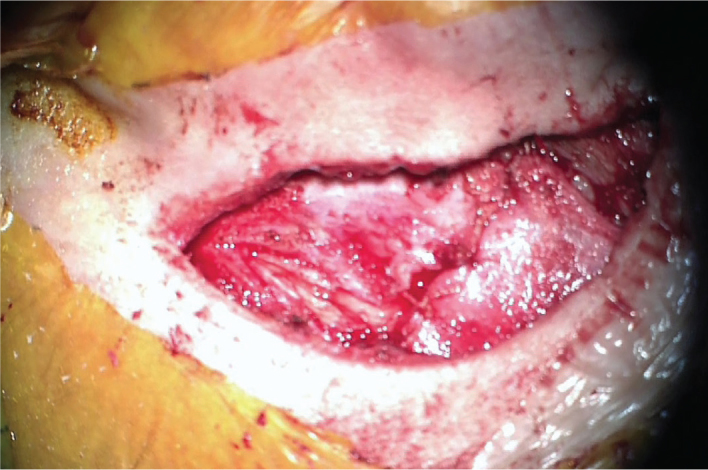
Complete periosteal covering after suturing of the periosteal flaps
RESULTS
Seven cases were implanted with CI 512 (4 cases) or CI 532 (3 cases) (cochlear, Lane Cove, Australia). Eight cases were implanted with the AB HiRes90-K MSE (Advanced Bionic, Los Angeles, California, United States), and 11 cases were implanted with MED-EL Sonata standard electrode (MED-EL, Innsbruck, Austria). The device was activated in all patients 3 weeks after surgery.
The follow-up period ranged from six months to one year. No complications were seen during or after the surgeries. There was no evidence of device migration, wound infection, wound hematoma, or delayed wound healing. The mastoid emissary vein was intact in all cases.
DISCUSSION
The postauricular incision and the anterior-based periosteal flap are common techniques for cochlear implantation. We present a new modification for the “classic” anterior-based periosteal flap that can be used in all cases of cochlear implantation.
Many techniques have been described for performing the periosteal flap and the subperiosteal pocket in cochlear implantation surgery. One of these techniques, Tailed Palva flap in the subperiosteal pocket technique, is somewhat similar to our described technique [4]. The difference between the two is that we drilled a seat for the receiver/stimulator under the subperiosteal pocket for further stabilization, and to be able to perform this seat, we formed the downward curvature of the superior periosteal incision, creating an inferior flap for good exposure. This inferior flap is relocated to its original position and fixed by tie sutures.
Such a modification facilitates the creation of a tight pocket and well-positioned seat for the receiver/stimulator, aiming to decrease the risk of device migration. In addition, this technique is relatively easier to perform than the other techniques that have been described for the same purpose, including using nonabsorbable sutures that were passed through monocortically drilled holes on each side of the R/S [1] or passed through two 4-mm titanium screws on either side of the well, [5] using polypropylene mesh that is fixed with titanium screws, [6] or using ionomeric bone cement for device fixation [7].
The risk of interruption of the emissary veins on the lower posterior border of the mastoid is lower with this modification. If emissary bleeding occurs, it can easily be controlled with pressure, bone wax, or crushed muscle; however, there are reports of extensive emissary bleeding that required discontinuation of the surgery [8]. Subdural hematoma has also been reported from mastoid emissary vein injury and from efforts to stop the bleeding [9]. Therefore, avoiding interruption of this venous structure is recommended.
With this modification, the resultant anterior-based flap might have a better blood supply as the base is nearly the same length of the apex, as the surviving duration of the random flap increases significantly with increasing base width [10].
This modified periosteal flap is easy to perform and allows good access to create a subperiosteal pocket, and also complete repositioning of the periosteum aiming at reducing the risks of device migration. However, this is a “how I do it” study by two authors with their preliminary results. Further studies with larger series and longer follow-up periods are warranted.
CONCLUSION
The modified anterior-based periosteal flap is a safe procedure aimed at avoiding the mastoid emissary vein bleeding and allowing complete repositioning of the periosteum over the implanted device.
Footnotes
Ethics Committee Approval: Ethic committee approval was received for this study from ethics committee of Zagazig University (4/2016).
Informed Consent: Written inform consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author contributions: Concept - Y.A.F.; Design - Y.A.F.; Supervision - R.J.T.; Resource - Y.A.F., R.J.T.; Materials - Y.A.F., R.J.T.; Data Collection and/or Processing - Y.A.F.; Analysis and/or Interpretation - Y.A.F., R.J.T.; Literature Search - Y.A.F.; Writing - Y.A.F., R.J.T.; Critical Reviews - R.J.T.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study received no financial support.
REFERENCES
- 1.Cohen NL, Roland JT, Jr, Fishman A. Surgical technique for the Nucleus Contour cochlear ımplant. Ear Hear. 2002;23:59S–66S. doi: 10.1097/00003446-200202001-00007. [DOI] [PubMed] [Google Scholar]
- 2.Adunka OF, Buchman CA. Cochlear implant fixation in children using periosteal sutures. Otol Neurotol. 2007;28:768–70. doi: 10.1097/MAO.0b013e318067bd60. [DOI] [PubMed] [Google Scholar]
- 3.Cohen NL, Hoffman RA. Complications of cochlear implant surgery in adults and children. Ann Otol Rhinol Laryngol. 1991;100:708–11. doi: 10.1177/000348949110000903. [DOI] [PubMed] [Google Scholar]
- 4.Orhan KS, Polat B, Enver N, Güldiken Y. Tailed Palva flap in the subperiosteal pocket technique for cochlear implantation. J Laryngol Otol. 2015;129:916–8. doi: 10.1017/S0022215115001905. [DOI] [PubMed] [Google Scholar]
- 5.Lee DJ, Driver M. Cochlear implant fixation using titanium screws. Laryngoscope. 2005;115:910–1. doi: 10.1097/01.MLG0000154537.05252.A0. [DOI] [PubMed] [Google Scholar]
- 6.Davis BM, Labadie RF, McMenomey SO, Haynes DS. Cochlear implant fixation using polypropylene mesh and titanium screws. Laryngoscope. 2004;114:2116–8. doi: 10.1097/01.mlg.0000149443.22393.ab. [DOI] [PubMed] [Google Scholar]
- 7.Rüdel C, Zöllner W. Ionomeric cement--a bone glue for device fixation. Ear Nose Throat J. 1994;73:189–91. [PubMed] [Google Scholar]
- 8.Webb RL, Lehnhardt E, Clark GM, Laszig R, Pyman BC, Franz BK. Surgical complications with the cochlear multiple-channel intracochlear implant: experience at Hannover and Melbourne. Ann Otol Rhinol Laryngol. 1991;100:131–6. doi: 10.1177/000348949110000208. [DOI] [PubMed] [Google Scholar]
- 9.Sunkaraneni VS, Banerjee A, Gray RF. Subdural haematoma: a complication of cochlear implantation. J Laryngol Otol. 2004;118:980–2. doi: 10.1258/0022215042790646. [DOI] [PubMed] [Google Scholar]
- 10.Stell PM, Green JR. The viability of triangular skin flaps. Br J Plast Surg. 1975;28:247–50. doi: 10.1016/0007-1226(75)90025-9. [DOI] [PubMed] [Google Scholar]


