Abstract
Background
We investigated whether the duration of postoperative physiotherapy supervision by a physiotherapist affects clinical outcome, speed, and agility in males 8 months after anterior cruciate ligament reconstruction (ACLR).
Material/Methods
From a group of 248 patients 8 months after ACLR, we used strict exclusion criteria to identify 2 groups of men who were well trained and frequently participated in sports pre-injury, with different durations of postoperative physiotherapy supervision: Group I (n=15; x=27.40 weeks) and Group II (n=15; x=8.07 weeks). Group III (n=30) were controls. Clinical evaluation (manual ligament assessment, knee joint and thigh circumferences, range of motion), pain assessment, and run test with maximal speed and change-of-direction manoeuvres, was performed.
Results
No clinically significant abnormalities were noted in any studied groups in terms of clinical and pain assessments. The time of the run test was significantly increased in Group II (x=23.77 s) compared with Group I (x=21.76 s) and Group III (x=21.15 s). The average speed was significantly reduced in Group II (x=2.05 m*s−1) compared with Group I (x=2.22 m*s−1) and Group III (x=2.27 m*s−1). The duration of physiotherapy supervision was significantly negatively correlated with the time results of the run test (r=−0.353; p=0.046) and positively correlated with the average speed (r=0.360; p=0.049).
Conclusions
Both shorter and longer duration of postoperative physiotherapy supervision resulted in successful clinical outcomes in terms of studied features in males 8 months after ACLR. Nevertheless, longer physiotherapy supervision was more effective for improving speed and agility to the level of healthy individuals.
MeSH Keywords: Anterior Cruciate Ligament, Anterior Cruciate Ligament Reconstruction, Physical Therapist Assistants
Background
The frequency of isolated anterior cruciate ligament (ACL) tears is 68.6 per 100 000 person-years, making it the most frequently injured of all knee ligaments [1]. These injuries account for up to 64% of all knee injuries in sports that involve cutting and pivoting motions [2]. Arthroscopically-assisted ACL reconstruction remains a standard surgical treatment, especially for patients unable to participate in sports involving jumping and cutting manoeuvres due to knee instability [3].
Comparisons of supervised versus so-called non-supervised postoperative physiotherapeutic procedures following the ACL reconstruction evaluate whether the quality and results of clinic-based treatment may be obtained in less expensive gym-based or home-based exercises. Nevertheless, the amount of physiotherapy input attained with non-supervised, home-based rehabilitation [4] and the terminology concerning these physiotherapy modes remain debatable issues. From the nineties of the last century there could have been reports on ACL reconstruction and rehabilitation programs generally supporting the equal effectiveness of both physiotherapy modes in terms of knee laxity, range of motion, and function at 6 months to 1 year after the reconstruction [5,6], and at longer follow-ups [7]. It had been assumed that a home-based rehabilitation program produces results equal to those obtained with a clinic-based procedure in terms of muscle strength [8–10] and 1-leg hop tests [8–10]. The general assumption has been slowly changing [8], however, and to date, the effect of so-called non-supervised physiotherapeutic procedures on other motor skills, such as speed and agility, has not been demonstrated.
The present study investigated whether the duration of postoperative physiotherapy supervision affects clinical outcome, speed, and agility in males 8 months after ACL reconstruction.
Material and Methods
The experiment was given approval number 1/2012 from our local ethics committee, and was conducted according to the ethics guidelines and principles of the Declaration of Helsinki. All participants in the study were informed about the purpose and approach to be used and signed an informed consent form to participate in the study. The cohort study was performed in an academic physiotherapy center from 2012 to 2016.
Group I and the Group II included participants matched in terms of time since ACL reconstruction, general health condition, type of graft used for the reconstruction, lack of any additional procedures during the reconstruction, lack of any abnormalities in the contralateral knee, pre-injury physical activity level, gender, age, and body mass index (BMI). Group III (healthy controls) were matched in terms of general health condition, lack of any musculoskeletal injuries in the history, gender, age, physical activity level, and BMI.
The initial sample consisted of 248 patients who started the postoperative physiotherapeutic procedure after primary unilateral intra-articular reconstruction in the physiotherapy center where the study was conducted between 2012 and 2016, and were asked to take part in the following study at an average of 8 months after surgery. From the initial sample, patients were excluded who had at least 1 of the following diagnosed medical problems: heart disease, high blood pressure, asthma or pulmonary disease, diabetes (n=1), ulcer or stomach disease, kidney disease, liver disease, anemia or other blood disease, osteoarthritis, degenerative osteoarthritis, rheumatoid arthritis, back pain, Lyme disease, or alcoholism. We excluded following participants: females (n=113); participants who underwent ACL reconstruction with the use of a method other than autologous ipsilateral hamstring tendon graft (n=32); participants with any abnormalities in the contrateral knee (n=10); participants who underwent at least 1 of the following procedures: medial and/or lateral meniscectomy, medial and/or lateral meniscal transplant, posterior cruciate ligament repair, or medial, and/or lateral collateral ligament repair/reconstruction (n=26); extensor mechanism surgery (n=7); patellofemoral surgery (n=10); osteoarthritis surgery other than shaving (n=7); participants exhibiting pre-injury activity level greater than 8 or lower than 5 according to Tegner Activity Level Scale, TAS (n=0); participants less than 18 years old or older than 35 years old (n=10); and participants with a BMI value less than 18.50 or greater than 29.99 (n=2).
The final 2 groups of ACL-reconstructed males were well trained and frequently participated in sports pre-injury but differed regarding the amount of time each was subject to postoperative supervised physiotherapy. Then, the remaining participants (n=30) were divided into Group I (n=15) who underwent supervised physiotherapy (≥6 months) with supervised full return to sport and Group II (n=15) who underwent supervised physiotherapy (≤3 months), followed by independent return to structured gym exercises and return to activity.
The participants from Group I and Group II were at a mean of 27.40 and 32.60 weeks after the reconstruction, respectively. However, the duration of postoperative physiotherapy varied significantly in the studied groups, at a mean of 27.40 weeks in Group I and 8.07 weeks in Group II.
Group III (controls) included adult 30 healthy males who were identified from the initial sample of 36 volunteers. From the initial sample, we excluded participants who had at least 1 of the following diagnosed medical problems: heart disease, high blood pressure, asthma or pulmonary disease, diabetes, ulcer or stomach disease, kidney disease, liver disease, anemia or other blood disease, osteoarthritis, degenerative osteoarthritis, rheumatoid arthritis, back pain, Lyme disease, or alcoholism, musculoskeletal injuries, females, participants exhibiting pre-injury activity level greater than 8 or smaller than 5 according to TAS; participants less than 18 years old or older than 35 years old; and participants with a BMI value less than 18.50 or greater than 29.99.
The characteristics of the studied participants are presented in Table 1.
Table 1.
Characteristics of the studied participants.
| Test compound | Group I (n=15) | Group II (n=15) | Group III (n=30) | p |
|---|---|---|---|---|
| Age (years) | 24.60 (22.16, 27.04) | 27.60 (25.35, 29.85) | 25.27 (24.00, 26.11) | 0.079 |
| Body mass (kg) | 77.73 (72.47, 83.00) | 79.40 (74.09, 84.71) | 79.63 (76.44, 82.92) | 0.794 |
| Body height (cm) | 179.53 (177.18, 181.89) | 179.80 (176.89, 182.71) | 182.50 (179.68, 185.32) | 0.231 |
| Body mass index (kg*m−2) | 24.07 (22.81, 25.33) | 24.55 (23.09, 26.02) | 23.93 (23.05, 24.80) | 0.712 |
| Tegner Activity Level Scale (level) | 6.80 (6.13, 7.47) | 6.60 (6.14, 7.06) | 6.73 (6.41, 7.06) | 0.841 |
| Time since ACLR (weeks) | 27.40 (24.64, 30.16) | 32.60 (28.50, 36.70) | n/a | 0.065 |
| Physiotherapy (weeks) | 27.40 (24.64, 30.16) | 8.07 (5.10, 11.03) | n/a | ≤0.001 |
| Involved leg: right/left (n) | 10/5 | 13/2 | n/a | – |
| ACL injury mechanism (n/c) | 15/0 | 15/0 | n/a | – |
Values expressed as the mean and 95% confidence interval. ACLR – anterior cruciate ligament reconstruction; c – contact; Group I – fully supervised physiotherapy participants; Group II – participants with a shorter duration of physiotherapy supervision; Group III – control group; n – number of individuals in the studied group; n – non-contact; n/a – not applicable; p – level of significance; physiotherapy, postoperative supervised physiotherapy duration. p≤0.05 is indicated in bold.
Surgical procedure
Group I and Group II included adult participants who underwent post-traumatic ACL reconstruction. The mean time between the injury and the reconstruction was 33.00±29.70 weeks in Group I and 33.00±56.19 weeks in Group II. All of the participants from Group I and Group II underwent arthroscopically-assisted primary unilateral single-bundle ACL reconstruction with the use of an autologous ipsilateral hamstring graft. The reconstructions were performed by the same 2 senior surgeons.
During reconstruction, the semitendinosus (ST) and gracilis (GR) tendons were harvested using a tendon striper through a 25–30-mm oblique incision over the pes anserinus. The tendons were prepared as a 4-stranded double-looped hamstring autograft. The ACL tibial guide was set to 45° from the medial tibial cortex to the center of footprints to prepare the tibial tunnel according to the harvested tendon diameter, which varied from 7 to 8 mm. A femoral tunnel created through an anteromedial portal with a minimum of 120° knee flexion was placed on the posterior aspect of the notch at an approximately 10: 30 orientation for the right knee joint or an approximately 1: 30 orientation for the left knee joint. Then, the graft was introduced through the tibial tunnel to the femoral tunnel and fixed on the lateral femoral cortex by flipping the EndoButton (Smith & Nephew, Andover, MA, USA). The graft was manually tensioned at 30° knee flexion, and the tibial side was fixed with a bioabsorbable tibial interference screw (Biomet, Warsaw, IA, USA).
Postoperative physiotherapy
In Group I and Group II, postoperative physiotherapy followed the procedure described by Czamara et al. (2011) [11]. The physiotherapeutic procedure was divided into 4 stages: first stage (1st–5th week postoperatively); second stage (6th–12th week postoperatively); third stage (13th–20th week postoperatively); and fourth stage (21st week up to 8 months postoperatively) [11]. The main goals of the first stage of postoperative physiotherapy from the day of surgery were based on pain and effusion reduction and restoration of knee range of motion and gait. Participants were educated by the physiotherapist on how best to exercise correctly at home and which activities should be avoided. The second stage was focused on improving the gait pattern and proprioceptive stimulation. The third stage aimed to reduce strength asymmetries and teach proper landing technique and running for general endurance training. The last stage mainly involved practising complex movement patterns, strength, power, and specific endurance training [11].
Group I underwent the full 4-staged physiotherapeutic procedure in the rehabilitation center where the study was conducted. The physiotherapy procedure was fully supervised, which means that all physiotherapy sessions were held at the rehabilitation center under the strict supervision of a physiotherapist. The physiotherapeutic treatment in all the cases studied was carried out by a team of 3 experienced physiotherapists in accordance with 1 physiotherapy programme determined in advance [11]. The frequency of physiotherapy attendance was 4–5 times a week for the first stage, 4 times a week for the second stage, 4 times a week for the third stage, and 3 times weekly for the fourth stage of the postoperative physiotherapeutic procedure. Therefore, it could be assumed that in Group I, the average total number of meetings with a physiotherapist was 101 with an average frequency of 3.70 visits per week for an average of 27 weeks. Each session with a physiotherapist lasted 2 h. The physiotherapy program was regularly monitored [12].
Group II participants underwent only the 2 first stages of the fully supervised postoperative procedure on average. The average total number of meetings with a physiotherapist was 32 with an average frequency of 4.00 visits per week for an average of 8 weeks postoperatively. Each session with a physiotherapist lasted 2 h. Based on reasons independent of their surgeons and physiotherapists, they refused to continue the supervised physiotherapy. These participants were informed about the main goals and characteristic of the 2 remaining stages of the physiotherapeutic procedures and continued home-based physiotherapy without physiotherapist supervision.
The participants from Group I, Group II, and Group III underwent clinical examination and the run test with maximal speed and change-of-direction manoeuvres.
Clinical examination
In the beginning, the history was taken, and all of the study participants underwent clinical examination according to the 2000 International Knee Documentation Committee (IKDC) Knee Examination Form [13]. The examination was performed bilaterally, starting from the uninvolved lower limb in Group I and Group II and the dominant lower limb in Group III. The generalized laxity, alignment, patella position, patella subluxation/dislocation, and range of motion were assessed. The evaluation of effusion, passive motion deficits, manual ligaments involving the Lachman test, anterior drawer test, and pivot shift test were also performed [13]. The thigh and knee joint circumferences were measured at 10 cm from the base of the patella, and at the joint space level, respectively, with accuracy to 0.5 cm. The active range of motion of the knee joint was measured using a standard goniometer [14] with an accuracy to 1 degree. The clinical assessment in the Group I and Group II was supported by the everyday pain assessment of the involved limb using the 100-mm visual analogue scale (VAS). The everyday pain lower limb assessment was not performed in Group III, as only participants with no musculoskeletal problems were included.
Run test with maximal speed and change-of-direction manoeuvres procedure
The test was performed as described by Czamara et al. (2015) [15]. The test was introduced by Czamara (2010) to assess the level of physical fitness in patients undergoing rehabilitation following ACL reconstruction [11,12]. Before all testing, participants were asked to abstain from unaccustomed strenuous exercise for at least 24 h. Participants were also asked to avoid eating a heavy breakfast the morning before the test and eating within 2 h of the test. Participants dressed in a comfortable sports outfit and sports shoes.
The test was preceded by a 12-min warm-up on a cycloergometer. The examiner used verbal ‘start’ and ‘stop’ commands. In the field of the test (square 5×5 m), 4 cones were set in the corners, and 1 was placed in the middle of the field (Figure 1). The participant ran laterally from the starting cone (number 1) to the right. Then, passing cone number 2 on the right, the participant ran forward to the cone in the middle (number 3). He passed the cone in the middle on the left and continued running forward to cone number 4. After passing cone number 4 on the right, the participant ran laterally to cone number 5. He passed the cone on the left and ran backward to the cone in the middle (number 3). The participant continued to run forward, passed cone number 3 on the right and ran to cone number 1. The distance was covered twice without a break. The test required the participant to run a course in the shortest possible time. The time required for each participant to cover the distance was measured to an accuracy of 0.01 second using a TMP-30 Pulsometer (Tech-Med, Warsaw, Poland). The covered distance was 48 m. Additionally, the average speed (m*s−1) of each participant in an interval of time was calculated as the distance covered by the participant divided by the duration of interval. The participant performed a trial test until he felt comfortable with the protocol. For safety reasons, the participants were informed about the necessity to stop the test in the event of pain, fall, or the so-called ‘giving way’ knee sensation. The test was supported by information regarding pain during the test, 3 min after the test, and 1 day after the test assessment using the VAS. The same examiner performed all of the measurements. The pain assessment concerned involved limb in Group I and Group II, and the right limb in the Group III.
Figure 1.
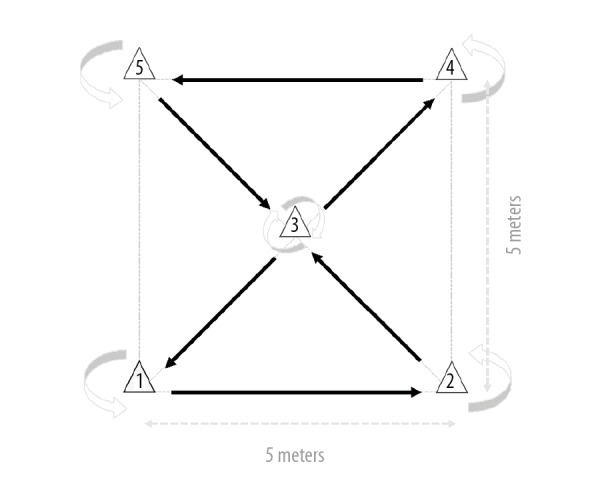
A scheme depicting consecutively numbered cones, the running direction during the test (black arrows), and the direction of bypassing particular cones (grey arrows). The dotted lines indicate the field of the test being performed.
Statistical analysis
Microsoft Office Excel 2007 (Microsoft, Redmond, WA, USA) and IBM SPSS Statistics 20 (IBM, Armonk, NY, USA) were used for statistical analysis. The arithmetic mean (x) and the 95% confidence interval for the 3 examined groups were calculated for particular studied features. The number of individuals was indicated as n. Inter-group characteristic comparisons of age, body mass, body height, and body mass index (BMI) were performed using the one-way analysis of variance (ANOVA) test and the post hoc Tukey’s test consecutively. In comparisons between Group I and Group II regarding the time since ACL reconstruction and the duration of postoperative physiotherapy, the normality Shapiro-Wilk test was used to study the distribution followed by a parametric test for independent samples. One-way ANOVA and post hoc Tukey’s tests were used in the inter-group comparisons of the run test with maximal speed and change-of-direction manoeuvres results. Regarding the circumferences and range of motion inter-group comparisons, the involved limbs (Group I, Group II) were compared to the right limbs (Group III) given that the right limb was the primary limb involved in both groups of ACL-reconstructed patients. In the intra-group comparisons, the Shapiro-Wilk test was first performed. The parametric test for dependent samples was consecutively performed and the linear Pearson’s correlation coefficient calculation was also performed. Correlation coefficient r-values were calculated for the strength and direction of a linear relationship between the selected parameters and the run test results. The p-values ≤0.05 were considered significant.
Results
Clinical examination
Analysis of the manual anterior tibial translation testing results based on the Lachman and anterior drawer tests revealed no abnormalities in any of the studied groups. The pivot shift was negative in all studied participants.
Pain assessment results showed that none of the participants in Group I or Group II reported everyday pain of the involved limb.
The intra-group comparison revealed significant differences in knee joint circumference in Group II, thigh circumferences in Group I and Group II, and knee joint flexion in Group II (Table 2). Due to small deficits, the differences did not appear to be clinically relevant (Table 2).
Table 2.
Intra-group and inter-group comparisons of circumferences and range of motion values.
| Studied limb | Group I | Group II | Studied limb | Group III | p | |
|---|---|---|---|---|---|---|
| Knee joint circumference (cm) | Involved | 36.33 (35.17, 37.50) | 37.13 (36.16, 38.11) | Right | 37.12 (36.49, 37.74) | 0.351 |
| Uninvolved | 36.17 (35.14, 37.20) | 36.83 (35.84, 37.83) | Left | 37.18 (36.56, 37.80) | 0.196 | |
| p | 0.173 | 0.023 | 0.969 | |||
| Thigh circumference (cm) | Involved | 46.90 (45.23, 48.57) | 46.70 (45.04, 48.36) | Right | 46.83 (45.83, 46.84) | 0.981 |
| Uninvolved | 47.67 (45.64, 49.69) | 47.73 (46.12, 49.35) | Left | 46.70 (45.59, 47.81) | 0.472 | |
| p | 0.034 | 0.009 | 0.972 | |||
| Knee joint extension (°) | Involved | −1.67 (−2.68, −0.65) | −0.07 (−2.26, 2.12) | Right | −0.70 (−1.53, 0.13) | 0.263 |
| Uninvolved | −1.80 (−3.22, −0.38) | −1.00 (−3.47, 1.47) | Left | −0.70 (1.53, 0.13) | 0.513 | |
| p | 0.792 | 0.121 | n/a | |||
| Knee joint flexion (°) | Involved | 131.33 (125.97, 136.69) | 124.73 (121.94, 127.52) | Right | 137.67 (134.98, 140.45) | ≤0.001 |
| Uninvolved | 133.93 (128.44, 139.43) | 126.67 (123.85, 129.48) | Left | 137.92 (135.31, 140.53) | ≤0.001 | |
| p | 0.123 | 0.041 | 0.976 |
Values expressed as the mean and 95% confidence interval. Group I – fully supervised physiotherapy participants; Group II – participants with a shorter duration of physiotherapy supervision; Group III – control group; n/a – not applicable; p – level of significance. p≤0.05 is indicated in bold.
The inter-group comparison revealed no differences in terms of thigh and knee joint circumferences and knee extension (Table 2). Knee flexion was significantly better in Group III compared with the involved knees in Group I (p=0.023) and Group II (p≤0.001). There were also significant differences between the involved limbs of Group I and Group II (p=0.048).
Knee flexion was significantly worse in the uninvolved knee in the Group II compared with Group III (p≤0.001) and Group I (p=0.026). No differences were noted between the uninvolved limbs in Group I and Group III (p=0.217). However, the clinical relevance of these differences also remains questionable.
Run test with maximal speed and change-of-direction manoeuvres
Statistically significant differences were noted in the inter-group comparisons of the run test results with maximal speed and change-of-direction manoeuvres (Table 3). Post hoc test results revealed that Group II performed significantly worse compared with Group I (p=0.027) and Group III (p≤0.001). No statistically significant differences in the run test results were noted between Group I and Group III (p=0.624). Group II covered the running distance significantly slower than Group I (p=0.023) and Group III (p≤0.001). The speeds in Group I and Group III were comparable (p=0.634).
Table 3.
Inter-group comparisons of the run test results with maximal speed and change-of-direction manoeuvres.
| Run test results with maximal speed and change-of-direction manoeuvres | |||
|---|---|---|---|
| Time (s) | Distance (m) | Average speed (m*s−1) | |
| Group I | 21.76 (20.59, 22.92) | 48.00 (n/a) | 2.22 (2.11, 2.34) |
| Group II | 23.77 (21.94, 25.59) | 48.00 (n/a) | 2.05 (1.92, 2.18) |
| Group III | 21.15 (20.76, 21.53) | 48.00 (n/a) | 2.27 (2.23, 2.32) |
| p | 0.001 | n/a | 0.001 |
Values expressed as the mean and 95% confidence interval. Group I – fully supervised physiotherapy participants; Group II – participants with a shorter duration of physiotherapy supervision; Group III – control group; n/a – not applicable; p – level of significance. p≤0.05 is indicated in bold.
A statistically significant negative relationship was noted between the duration of postoperative supervised physiotherapy and the run test results, and a statistically significant positive relationship was noted between the duration of postoperative supervised physiotherapy and the average speed for the estimated distance (Table 4).
Table 4.
Correlation between the obtained run test results with maximal speed and change-of-direction manoeuvres and age, body mass, body height, body mass index, time since ACL reconstruction, and the duration of postoperative supervised physiotherapy duration.
| Test compound | Run test results with maximal speed and change-of-direction manoeuvres | |||
|---|---|---|---|---|
| Time (s) | Average speed (m*s−1) | |||
| r | p | r | p | |
| Age (years) | 0.105 | 0.582 | −0.161 | 0.396 |
| Body mass (kg) | 0.263 | 0.160 | −0.307 | 0.099 |
| Body height (cm) | 0.185 | 0.328 | −0.166 | 0.380 |
| Body mass index (kg*m−2) | 0.227 | 0.227 | −0.288 | 0.123 |
| Tegner Activity Level Scale | 0.074 | 0.698 | −0.085 | 0.656 |
| Time since ACLR (weeks) | 0.016 | 0.933 | −0.061 | 0.747 |
| Physiotherapy (weeks) | −0.353 | 0.046 | 0.360 | 0.049 |
ACLR – anterior cruciate ligament reconstruction; p – level of significance; physiotherapy, postoperative supervised physiotherapy duration; r – correlation coefficient. p≤0.05 is indicated in bold.
All participants completed the run test. None of the participants reported feeling the so-called “giving way” their knees. In addition, no pain was reported during the test, 3 min after the test, or 1 day after the test.
Discussion
The duration of postoperative physiotherapy supervision did not affect the clinical outcome in patients 8 months after the ACL reconstruction in terms of the knee joint stability, thigh and knee joint circumferences, active range of motion, and everyday pain. Both modes of physiotherapy were successful regarding these parameters. Nevertheless, longer postoperative physiotherapy supervision more effectively improved speed and agility in patients 8 months after ACL reconstruction to the level of healthy individuals. The run test results with maximal speed and change-of-direction manoeuvres were correlated with the duration of postoperative supervision of physiotherapy. The longer the duration of postoperative physiotherapy under the supervision of a physiotherapist, the shorter the test time and the higher the average speed of the test.
According to the opinion of the vast majority of authors discussing the issue, a minimally supervised physical therapy program is cost-saving [10] and can result in successful ACL rehabilitation [9,10,16,17]. In addition, the long-term results seem to be encouraging [7]. On the other hand, some authors focus on the moderate evidence of reviews comparing the home-based to clinic-based physiotherapy, with a lack of clarity concerning the amount of physiotherapy received with home-based rehabilitation being crucial to determine when considering the evidence that this mode of physiotherapy is as effective as a supervised method [4]. Thus, there is no consensus as to what is considered supervised versus unsupervised physiotherapy. Nevertheless, it can be assumed that the present study assessed the influence of postoperative physiotherapy supervision duration provided by a specialist.
Some authors use the pivot-shift clinical examination technique, where knee flexion and axial load combined with tibial rotation and valgus force aim to reproduce the original mechanisms of ACL injury [18]. Of note, most ACL injuries are sustained with minimal or no contact at the time of injury [19]. The sport-related activities at the moment of noncontact injury mostly involve a change in speed or the generation of multi-directional force across the knee joint while bearing weight [20]. Jump-landing, twisting, and pivoting have also been associated with ACL injuries [19]. A combination of valgus and rotational moments at the knee is commonly noted as a significant stressor on the ACL, and the addition of these forces to the coronal forces in a hyperextended knee can multiply the ligament tension [21,22]. Contact ACL injuries are also mostly an effect of multiplanar mechanisms [18]. Despite limited evidence for a strict timeline for return to play after ACL reconstruction, the authors allow return to play without restrictions at 6 months postoperatively, whereas most doctors permit return to sports at 9 months [23]. Several studies aimed to define objective criteria to guide return to play after ACL reconstruction [24]. A series of hop tests, most often including single-leg hop for distance, the single-leg triple hop for distance, the single-leg timed hop, the single-leg crossover hop for distance, and the vertical jump test, represent measures used to evaluate the capacity for successful return to play [24]. Although hop testing is a reliable and valid tool replicating the demands of high-level activities [25], some authors emphasize that it may not be sufficiently sensitive to identify functional limitations associated with multiplanar movements [24]. However, increased rates of graft re-rupture after return to play are noted in athletes participating in cutting or pivoting sports compared with athletes involved in straight-line activities or jumpers [26–28]. Based on these findings, the test used in the present study to evaluate speed, quickness, and body control in multiple planes of movement and to assess lower-limbs control, including the ability to perform plant and cut types of movements in a correct manner, appear to be a valid tool for assessment of the ACL-reconstructed knee. The Illinois Agility Test, Agility Shuttle Run Test, 505 Agility Test, Agility T-Test, and 3-Cone Shuttle Drill test are commonly used tools to measure agility. The Agility T-Test [23] is the most commonly used. The Agility T-Test was designed to determine speed and directional change. However, unlike other agility tests, this test focuses on backpedalling and lateral shuffles. The Agility T-Test includes forward, backward, and lateral running. However, the test does not involve dynamic pivoting, which is crucial in the assessment of a patient after ACL reconstruction. Thus, the selection of the correct research tool in this study is important.
The advantage of the present’s study agility test is that it requires minimum equipment and space and is easy to perform. The equipment required to perform the test includes a standard measuring tape, a stopwatch, and 5 cones. Thus, this test is inexpensive. The test was performed on the parquet floor in the rehabilitation center. According to Czamara et al. (2015), the run test with maximal speed and change-of-direction manoeuvres has excellent intra-rater reliability (intraclass correlation coefficient is 0.96) [15]. Based on the absence of pain during the test, 3 min after the test, and the day after the test, as well as the fact that none of the participants experienced a fall during the run test, it can be concluded that this assessment tool is safe for patients at least within this time period after the reconstruction. In the future, the test result should be correlated with muscle strength assessment results.
The obtained time results of the run test in Group I and Group III were comparable to the results noted by Czamara (2010). The mean value was 21.40±2.20 s in patients at 6 months after unilateral primary arthroscopically-assisted ACLR with the use of STGR tendon graft who underwent fully supervised physiotherapeutic procedures for 24 weeks and 21.90±2.00 in healthy males [11]. Participants in the Czamara (2010) study were about the same age as the participants in the present study. In addition, body mass, body height, and physical activity level were comparable among the participants in both studies [11]. On the other hand, the time results in the present study were improved in the study comparing male patients after single-bundle (22.20±0.98 s) versus double-bundle (21.67±4.67 s) ACL reconstruction in terms of the knee joint during activities involving change-of-direction manoeuvres [15]. Although the studied patients underwent fully supervised postoperative physiotherapy for 24 weeks, they were older (30.40±11.66 years old vs. 28.40±8.10 years old in the single-bundle and double-bundle groups, respectively) [15]. This difference might affect their performance. As the previous studies noted, there were no differences between the 2 types of ACL reconstruction in terms of the run test with maximal speed and change-of-direction manoeuvres [15], and patients undergoing single-bundle and double-bundle reconstruction were included in the present study.
According to Wright et al. (2015), even the effect of the best surgical treatment of ACL injury can be reduced by inappropriate or ineffective postoperative physiotherapy [29]. There is a general consensus regarding the effectiveness of the postoperative physiotherapy program; however, the optimal components of such a program remain debated [30]. Regardless of whether the goal of postoperative physiotherapy is to prepare the patient for returning to physical activity at the level of professional or recreational sports, the last stages of the procedure should focus on improving work capacity in the ability to undertake load acceptance in multiple planes of movement and developing the ability to perform specific multi-directional running and landing tasks. There is common agreement that home-based rehabilitation following ACL reconstruction is deleterious when prescribed to motivated patients [29]. However, it is unclear whether even the most motivated patient has sufficient knowledge and skills to prepare to return to sports even at occasional or recreational levels without being supervised by a specialist.
Speed is defined as the ability to achieve high velocity, whereas agility is the ability to quickly change directions in an accurate manner. Agility has also been defied as a sudden change of direction and the movement of the entire body and limbs. Agility is particularly helpful in sports that require quickness and alertness [31]. Speed and agility training include types of exercises with bodyweight resistance. Speed training aims to increase maximal speed and is designed for sports requiring short bursts of energy, such as baseball or football. Sprinting is based on the creation of fast, powerful, and coordinated muscle contractions [32]. Agility drills are exercises requiring quick movement combined with changes in direction for the entire body, aiming to improve coordination, proprioception, and dynamic balance. Agility drills involve elements of mental training, as the participant is forced to think and react quickly, and these drills stimulate a chaotic sports environment [32]. Given that the vast majority of sport activities require fast movements of either the upper limbs or lower limbs, speed and agility training can precisely improve skills in these components. Thus, patients can benefit when speed, agility, and quickness training is integrated into their physiotherapeutic procedure.
Apart from the gender, age, and general body composition, activity levels have the potential to provide a valuable dimension to outcome measurement. In order to present data on the activity of the study participants, we used the TAS that originally was designed as a score for activity level to complement the functional Lysholm knee score for patients with ligament injuries [33]. The TAS scores a person’s activity level between 0 and 10, where 0 is “on sick leave/disability” and 10 is “participation in competitive sports”. The instrument is commonly used to measure change in activity level in ACL-reconstructed patients, but in this study it was used to obtain the most homogeneous groups, and the control group was appropriately selected for the pre-injury level of physical activity of patients from ACL-reconstructed groups.
The small number of participants may be considered a limitation of the study. On the other hand, the limited number of patients was a result of the meticulous selection of the test sample, considering all types of factors that could affect speed and agility. One of the study’s limitations is the lack of output data on the examined patients from the period before reconstruction. Of course, it was also impossible to perform a running test 8 weeks after reconstruction. Thus, an additional control group was created that included age-matched males appropriately selected for the studied patients in terms of body composition and level of physical activity. The manual ligament laxity assessment may also be considered as a limitation.
The present data can serve as a reference point for analysis and interpretation of results from well-trained males who frequently participate in sports. However, there remains a need for establishing normal values for athletes. In addition, the normal values for women should be established. In the future, an interesting aspect would involve research on a variety of surfaces depending on the sports discipline being practised. Further research is needed to identify sport-specific outcomes for returning to sports at the recreational level for patients after ACL reconstruction following home-based physiotherapeutic procedures.
Conclusions
The duration of postoperative physiotherapy supervision does not affect the clinical outcome in males 8 months after ACL reconstruction in terms of knee joint stability, thigh and knee joint circumferences, active range of motion, and everyday pain. Both modes of physiotherapy were successful regarding these factors.
Nevertheless, longer postoperative physiotherapy supervision was more effective for improving speed and agility in males 8 months after ACL reconstruction to the level of healthy individuals.
Supervision by a specialist during the final stages of physiotherapy after ACL reconstruction, practising strength, power, complex movement patterns, running, and endurance training seem to be crucial to restore speed and agility to the level of healthy individuals.
Footnotes
Source of support: Departmental sources
Conflict of interest
None.
References
- 1.Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: A 21-year population-based study. Am J Sports Med. 2016;44(6):1502–7. doi: 10.1177/0363546516629944. [DOI] [PubMed] [Google Scholar]
- 2.Rishiraj N, Taunton JE, Lloyd-Smith R, et al. The potential role of prophylactic/functional knee bracing in preventing knee ligament injury. Sports Med. 2009;39(11):937–60. doi: 10.2165/11317790-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 3.Gianotti SM, Marshall SW, Hume PA, Bunt L, et al. Incidence of anterior cruciate ligament injury and other knee ligament injuries: A national population-based study. J Sci Med Sport. 2009;12(6):622–27. doi: 10.1016/j.jsams.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 4.Lobb R, Tumilty S, Claydon LS. A review of systematic reviews on anterior cruciate ligament reconstruction rehabilitation. Phys Ther Sport. 2012;13(4):270–78. doi: 10.1016/j.ptsp.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 5.Andersson D, Samuelsson K, Karlsson J. Treatment of anterior cruciate ligament injuries with special reference to surgical technique and rehabilitation: An assessment of randomized controlled trials. Arthroscopy. 2009;25(6):653–85. doi: 10.1016/j.arthro.2009.04.066. [DOI] [PubMed] [Google Scholar]
- 6.Trees AH, Howe TE, Dixon J, White L. Exercise for treating isolated anterior cruciate ligament injuries in adults. Cochrane Database Syst Rev. 2005;(4):Cd005316. doi: 10.1002/14651858.CD005316.pub2. [DOI] [PubMed] [Google Scholar]
- 7.Grant JA, Mohtadi NG. Two- to 4-year follow-up to a comparison of home versus physical therapy-supervised rehabilitation programs after anterior cruciate ligament reconstruction. Am J Sports Med. 2010;38(7):1389–94. doi: 10.1177/0363546509359763. [DOI] [PubMed] [Google Scholar]
- 8.Fischer DA, Tewes DP, Boyd JL, et al. Home based rehabilitation for anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 1998;(347):194–99. [PubMed] [Google Scholar]
- 9.Beard DJ, Dodd CA. Home or supervised rehabilitation following anterior cruciate ligament reconstruction: A randomized controlled trial. J Orthop Sports Phys Ther. 1998;27(2):134–43. doi: 10.2519/jospt.1998.27.2.134. [DOI] [PubMed] [Google Scholar]
- 10.Schenck RC, Jr, Blaschak MJ, Lance ED, et al. A prospective outcome study of rehabilitation programs and anterior cruciate ligament reconstruction. Arthroscopy. 1997;13(3):285–90. doi: 10.1016/s0749-8063(97)90022-0. [DOI] [PubMed] [Google Scholar]
- 11.Czamara A. Evaluation of physiotherapeutic procedures after ACL recontruction in males. Archives of Budo. 2010;6(2):73–81. [Google Scholar]
- 12.Czamara A. Functional benchmarking of rehabilitation outcomes following anterior cruciate ligament reconstruction. Ortop Traumatol Rehabil. 2010;12(6):519–33. [PubMed] [Google Scholar]
- 13.Anderson AF, Irrgang JJ, Kocher MS, et al. The International Knee Documentation Committee Subjective Knee Evaluation Form: Normative data. Am J Sports Med. 2006;34(1):128–35. doi: 10.1177/0363546505280214. [DOI] [PubMed] [Google Scholar]
- 14.Norkin CC, White DJ. Measurement of joint motion: A Guide to Goniometry. F.A. Davis; 2009. [Google Scholar]
- 15.Czamara A, Królikowska A, Szuba Ł, et al. Single- vs. double-bundle anterior cruciate ligament reconstruction: A new aspect of knee assessment during activities involving dynamic knee rotation. J Strength Cond Res. 2015;29(2):489–99. doi: 10.1519/JSC.0000000000000638. [DOI] [PubMed] [Google Scholar]
- 16.Grant JA, Mohtadi NG, Maitland ME, Zernicke RF. Comparison of home versus physical therapy-supervised rehabilitation programs after anterior cruciate ligament reconstruction: A randomized clinical trial. Am J Sports Med. 2005;33(9):1288–97. doi: 10.1177/0363546504273051. [DOI] [PubMed] [Google Scholar]
- 17.Revenäs Å, Johansson A, Leppert J. A randomized study of two physiotherapeutic approaches after knee ligament reconstruction. Advances in Physiotherapy. 2009;11(1):30–41. [Google Scholar]
- 18.Quatman CE, Quatman-Yates CC, Hewett TE. A ‘plane’ explanation of anterior cruciate ligament injury mechanisms: A systematic review. Sports Med. 2010;40(9):729–46. doi: 10.2165/11534950-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 19.Boden BP, Dean GS, Feagin JA, Jr, Garrett WE., Jr Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23(6):573–78. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- 20.Wetters N, Weber AE, Wuerz TH, et al. Mechanism of injury and risk factors for anterior cruciate ligament injury. Operative Techniques in Sports Medicine. 2016;24(1):2–6. [Google Scholar]
- 21.Markolf KL, Gorek JF, Kabo JM, Shapiro MS. Direct measurement of resultant forces in the anterior cruciate ligament. An in vitro study performed with a new experimental technique. J Bone Joint Surg Am. 1990;72(4):557–67. [PubMed] [Google Scholar]
- 22.Markolf KL, O’Neill G, Jackson SR, McAllister DR. Effects of applied quadriceps and hamstrings muscle loads on forces in the anterior and posterior cruciate ligaments. Am J Sports Med. 2004;32(5):1144–49. doi: 10.1177/0363546503262198. [DOI] [PubMed] [Google Scholar]
- 23.Harris JD, Abrams GD, Bach BR, et al. Return to sport after ACL reconstruction. Orthopedics. 2014;37(2):e103–8. doi: 10.3928/01477447-20140124-10. [DOI] [PubMed] [Google Scholar]
- 24.Ellman MB, Sherman SL, Forsythe B, et al. Return to play following anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2015;23(5):283–96. doi: 10.5435/JAAOS-D-13-00183. [DOI] [PubMed] [Google Scholar]
- 25.Reid A, Birmingham TB, Stratford PW, et al. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther. 2007;87(3):337–49. doi: 10.2522/ptj.20060143. [DOI] [PubMed] [Google Scholar]
- 26.George MS, Dunn WR, Spindler KP. Current concepts review: Revision anterior cruciate ligament reconstruction. Am J Sports Med. 2006;34(12):2026–37. doi: 10.1177/0363546506295026. [DOI] [PubMed] [Google Scholar]
- 27.Mehta VM, Mandala C, Foster D, Petsche TS. Comparison of revision rates in bone-patella tendon-bone autograft and allograft anterior cruciate ligament reconstruction. Orthopedics. 2010;33(1):12. doi: 10.3928/01477447-20091124-15. [DOI] [PubMed] [Google Scholar]
- 28.Gudas R, Jurkonis R, Smailys A. comparison of return to pre-injury sport after 10 mm size bone-patellar tendon-bone (BPTB) versus 8 mm hamstring anterior cruciate ligament reconstruction: a retrospective study with a two-year follow-up. Med Sci Monit. 2018;24:987–96. doi: 10.12659/MSM.904709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wright RW, Haas AK, Anderson J, et al. Anterior cruciate ligament reconstruction rehabilitation: MOON guidelines. Sports Health. 2015;7(3):239–43. doi: 10.1177/1941738113517855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arna Risberg M, Lewek M, Snyder-Mackler L. A systematic review of evidence for anterior cruciate ligament rehabilitation: how much and what type? Physical Therapy in Sport. 2004;5(3):125–45. [Google Scholar]
- 31.Delextrat A, Grosgeorge B, Bieuzen F. Determinants of performance in a new test of planned agility for young elite basketball players. Int J Sports Physiol Perform. 2015;10(2):160–65. doi: 10.1123/ijspp.2014-0097. [DOI] [PubMed] [Google Scholar]
- 32.Muscolino JE. Elsevier Health Sciences. 2014. Kinesiology – E-Book: The skeletal system and muscle function. [Google Scholar]
- 33.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;(198):43–49. [PubMed] [Google Scholar]


