Abstract
Background
The aim of this study was to evaluate the reconstruction of a torn anterior cruciate ligament (ACL) with 10 mm diameter BPTB (bone-patellar tendon-bone) autograft versus 8 mm HT (hamstring tendon) autografts, to compare the ability to restore pre-injury sports activities and reduce revision risk after these procedures.
Material/Methods
A prospective clinical review was performed to compare results of patients who underwent primary anatomical ACLR with 10 mm BPTB autografts with patients who underwent 8 mm diameter HT autografts, between January 2011 and January 2014.
Results
There were 183 patients evaluated: the 8 mm HT group showed statistically significant higher knee laxity values compared to the 10 mm BPTB group (p=0.042), and significant difference were detected in subjective International Knee Documentation Committee (IKDC) evaluation scores; the average subjective IKDC evaluations after two-year follow-up in the HT group was 88.45±2.8 versus 89.24±2.5 in BPTB group (p=0.047). In the evaluation of the IKDC objective protocol, results were excellent and good in 83 patients (94.3%) after BPTB and in 78 patients (82%) after HT ACLR (p<0.05). The average score on the Tegner activity scale in the HT group decreased from 6.5 at pre-injury to 5.8 at two-year follow-up (p<0.001) and from 6.7 at pre-injury to 6.5 at two-year follow-up in the BPTB group (p=0.4). The ability to restore pre-injury sports activities was higher in the BPTB group (6.5) versus the HT group (5.8) (p<0.001). Revision was required for two patients (2.2%) in the BPTB group compared with 14 patients (14.7%) in the HT group (p<0.05).
Conclusions
Smaller HT graft size was a predictor of higher knee laxity and greater revision risk at two-year post primary ACL reconstruction. Larger diameter BPTB ACL grafts had a better ability to restore knee stability and greater ability to restore pre-injury sports activities.
MeSH Keywords: Anterior Cruciate Ligament Reconstruction, Arthroscopy, Bone-Patellar Tendon-Bone Grafts
Background
Although 10 to 11 mm size of bone-patellar tendon-bone (BPTB) autograft has traditionally been the gold standard for anterior cruciate ligament reconstruction (ACLR) in athletic population, an 8 mm average size of quadrupled hamstring tendon (HT) is used mostly for lower physical activity people [1–3]. It has been shown in the literature that quadrupled HTs are biomechanically equivalent in strength when compared with BPTB autograft and clinically can result in less donor-site morbidity [4–8]. Unlike BPTB grafts, the diameter of a HT graft may vary in every case. There is increasing interest in HT ACLR because of the large variability in size of the HT graft harvested and case selected ACLR can be performed. Unfortunately, there have been no studies that have shown outcomes between BPTB and HT autografts related to graft diameter. Most clinical HT grafts vary between 6 and 10 mm, thus it is difficult to compare HT ACLR outcomes with traditional 10 mm BPTB graft outcomes. Clinically, grafts with a diameter less than 7 mm have been associated with an increased rate of early revision [2,9] and it is clear that HT graft should be larger than 7 mm. The large variability of HT graft size obtained during surgery could significantly influence the outcome of ACLR, and this led us to the search for an optimal HT graft size that would be as strong as a 10 mm BPTB graft.
The purpose of this study was to determine whether outcomes of ACLR with 8 mm HT grafts were comparable with traditional 10 mm BPTB grafts. We hypothesized that the 8 mm HT graft compared to 10 mm BPTB graft would be associated with equal clinical results.
Material and Methods
From January 2011 to January 2014, a retrospective chart review of prospectively collected data was performed, and 183 of 200 consecutive patients (91.5%) with a mean age of 23.3 years (18 to 32 years) who underwent primary ACLR with BPTB or HT autografts were evaluated: 8 mm diameter HT anatomical single-bundle (n=95), and 10 mm diameter BPTB single-bundle (n=88). Graft type, size, patient age, sex, and body mass index were recorded at the time of ACLR (Table 1). Baseline characters were similar in the two groups (Table 1). There were 43 professionals (competitive sports level) athletes in the HT group (19 baseball, 11 football, two volleyball, nine handball players and two cyclists), and 45 in the BPTB group (15 baseball, 12 football, 10 handball, five volleyball and three rugby’s players). Both groups were matched accordingly to associated meniscal injury and surgical repair incidence (Table 2).
Table 1.
Pre-operative data.
| Characteristic | 8 mm HT group (n=95) | 10 mm BPTB group (n=88) | p Value |
|---|---|---|---|
| Gender | |||
| Male | 66 | 61 | 0.44 |
| Female | 29 | 27 | |
|
| |||
| Age, years | 25.1 | 26 | 0.2 |
|
| |||
| Body mass index | 20.50 | 20.58 | 0.73 |
|
| |||
| Lachman | 0.45 | ||
| IKDC A | 0 | 0 | |
| IKDC B | 0 | 0 | |
| IKDC C | 44 | 54 | |
| IKDC D | 51 | 34 | |
|
| |||
| Pivot shift | 0.41 | ||
| IKDC A | 0 | 0 | |
| IKDC B | 0 | 0 | |
| IKDC C | 62 | 57 | |
| IKDC D | 33 | 31 | |
|
| |||
| IKDC subjective score | 65.49 | 64.79 | 0.353 |
|
| |||
| Tegner activity score | 6.5 | 6.7 | 0.14 |
|
| |||
| Professional athletes (competitive level) | 43 | 45 | 0.32 |
Table 2.
Procedures of the menisci data during the ACLR of the two groups.
| 8 mm HT group (n=95) | 10 mm BPTB group (n=88) | Total | p Value | |
|---|---|---|---|---|
| Lateral meniscus | ||||
| Partial meniscectomy | 16 (16.7%) | 10 (11.1%) | 26 (14.0%) | 0.239 |
| Meniscal repair | 15 (15.6%) | 12 (13.3%) | 27 (14.5%) | 0.564 |
|
| ||||
| Medial meniscus | ||||
| Partial meniscectomy | 28 (29.2%) | 29 (32.2%) | 57 (30.6%) | 0.895 |
| Meniscal repair | 12 (12.5%) | 10 (11.1%) | 22 (11.8%) | 0.670 |
|
| ||||
| Both menisci | ||||
| Partial meniscectomy | 15 (15.6%) | 24 (26.7%) | 39 (21.0%) | 0.150 |
| Meniscal repair | 10 (10.4%) | 5 (5.6%) | 15 (8.1%) | 0.197 |
Inclusion criteria were as follows: (a) isolated primary ACLR (partial meniscectomies and meniscal repairs included); (b) no significant chondral damage seen at time of surgery (grade-III or more evaluate during arthroscopy); (c) normal contralateral knee; (d) minimum follow-up of 24 months; (e) Tegner activity level >5 (recreational or competitive sports; (f) age 18 to 35 years. Patients were excluded if they had had a previous injury of or operation on either knee or if they had a concurrent osteoarthritis, or injury of the posterior cruciate ligament, lateral collateral ligament, or posterolateral complex of the knee, or bilateral ACL lesions, or a grade-III tear of the medial collateral ligament. Patients with a grade-I or grade-II tear of the medial collateral ligament were considered eligible.
Preoperative and two-year follow-up postoperative International Knee Documentation Committee (IKDC) [10] objective and subjective scales and questionnaires, pre-injury and two-year postoperative Tegner activity level scores [11], ability to return to a pre-injury sports activities, and whether each patient underwent revision ACLR during the two-year follow-up period were recorded.
Surgical technique and postoperative rehabilitation
After diagnostic arthroscopy and, if needed, meniscal procedures, the ST/G (semitendinosus and gracilis) or patella tendons were harvested through a short typical vertical incisions located medial to the tibia tuberosity and patella tendon.
The 8 mm diameter doubled semitendinosus autografts and 10 mm diameter BPTB autografts were included in this study. Each HT graft was doubled with sutures at both ends of the graft (Vicryl 2-0 sutures on the femoral side of the graft, and non-absorbable sutures on the tibia side of the graft). The diameter of the graft was measured using a calibrator (accuracy: 0.5 mm) at its middle part. The anatomical [12,13] femoral tunnels were drilled first. They were created ante grade through one very low anteromedial (AM) portal. The diameters of the AM femoral tunnels were 8 mm for HT and 10 mm for BPTB, and the depth of the tunnels was 25 mm in HT and 20–23 mm for BPTB. Next, the tibia tunnel was prepared; the arthroscopic aimer was inserted to the knee through the AM portal and was adjusted to 45°, when drilling, and was positioned approximately 5 mm behind the anterior meniscal ligament in a middle distance between the anterior horn of lateral meniscus and medial eminence of tibia. After the guide pin was drilled, the drill guide was removed and the knee was passively extended to exclude an impingement on the anterior intercondylar notch and medial wall of lateral femoral condyle. Once a check was performed, the tibia tunnel was established with a cannulated reamer to the graft diameter. The reaming debris was evacuated with a synovial shaver to minimize the fat pad inflammatory response. After the tunnels on both the femoral and tibia side were created, grafts were inserted and then fixed with bioabsorbable interference screws proximally and distally. The knee was cycled several times through range of motion and the graft was examined arthroscopically to check tension and fixation quality and to exclude graft impingement.
The postoperative care and rehabilitation protocol was the same in the two groups. An extension knee brace was used for two weeks with protected weight bearing allowed for two weeks as tolerated. On the second postoperative week, the brace was fixed to allow motion between 0° and 60° of flexion, quadriceps activity against gravity, and hamstring contractions were permitted. Four weeks after surgery, patients were allowed knee motions between 0° and 90° of flexion, and quadriceps exercises were allowed between 45° and 90° of flexion. At six to eight weeks, full isotonic hamstring contraction, hip abductor-adductor exercises, and swimming were permitted. At eight weeks, patients were encouraged to achieve a full range of motion, to extend the knee against unlimited resistance between 45° and 90° of flexion, and to ride a stationary bicycle with resistance. At twelve weeks, unrestricted isotonic quadriceps-strengthening was allowed between 0° and 90° of flexion. Return to sports activity was allowed gradually eight to 12 months postoperatively, and after one year without any restrictions.
Clinical assessments and postoperative evaluation
IKDC and Tegner activity level scores were evaluated in this study. The main objective of our investigation was to evaluate the return to pre-injury level of sport activities. Clinical evaluations of knee function and laxity were performed by the operating surgeon and two independent examiners preoperatively and at six months, one year, and two years postoperatively. The clinical outcome measures included the Lachman, pivot-shift tests and examination for determination of subjective IKDC rating, and the completed Tegner score. The side-to-side laxity difference (Lachman) on manual examination was graded in three grades (based on IKDC objective scale): normal – 0–3 mm difference (hard endpoint), grade A; slight – 3–5 mm difference (soft endpoint) – grade B; 6–10 mm difference, grade C; very unstable >10 mm difference, grade D. The pivot shift test was graded as normal (no difference between the knees), a glide (a mild difference or a moderate difference or subluxation) and a clear pivot shift (a severe difference or marked subluxation).
Statistical analysis
Patient demographics and outcome data were collected and tabulated, and summary statistics were generated. Comparison of normally distributed continuous variables between groups was performed using the Student’s t-test, and comparison within a group before and after the investigation was done using the paired Student t-test. Continuous variables that were not normally distributed were compared between groups by using the Mann-Whitney U test. Categorical data were analyzed using the Pearson chi-squared (χ2) test and Fisher’s exact test. The level of significance was set at 5% for all the tests. One of our main outcome measurements was the subjective IKDC score. With a difference of 10 points, clinically significant differences between the treatment groups were acknowledged. Thus, accepting less than 5% probability of a type I error and a power of 80%, sufficient total sample size would be 80 in each group (160 totals). With the inclusion of a total of 183 cases, the statistical power was adequate. Statistical analysis was performed using the Statistica-7 statistical package.
Results
After we controlled for age, sex, body mass index, preoperative IKDC, and pre-injury Tegner scores, there were no differences between the two study groups preoperatively, except of graft choice and size (Table 1).
All data and patient outcomes at two-years postoperative were available in 183 patients (91.5%). The time interval from injury to operation was 6.2±6.2 weeks in the 10 mm BPTB group and 5.1±3.2 weeks in the 8 mm HT group (NS).
Associated injuries and treatment
There were 57 concomitant partial medial meniscectomies and 26 partial lateral meniscectomies (Table 2).
In total, 49 meniscal repairs were done. There was no difference in the prevalence of meniscal tears between the two groups (Table 2). Articular surface damage or localized degenerative changes of grade I or II were found during the procedure in 35 patients in the 10 mm BPTB group and in 26 patients in the 8 mm HT group. There were 21 medial collateral ligament tears (grade II), two in the 10 mm BPTB group and 14 in the 8 mm HT group. Meniscal procedures did not differ significantly in both groups. Thus, menisci injuries in both groups were equal and equally could bias the results, either repaired or removed, so statistically had the same influence on the difference of the final ACLR results in both groups.
IKDC subjective evaluations
According to subjective IKDC score, all patients in the two groups got significantly better at the two-year follow-up (p<0.001). However, the 8 mm HT ACLR group showed significant lower subjective IKDC evaluation compared to the 10 mm BPTB group (88.45±2.8 versus 89.24±2.5; p<0.047) (Figure 1).
Figure 1.
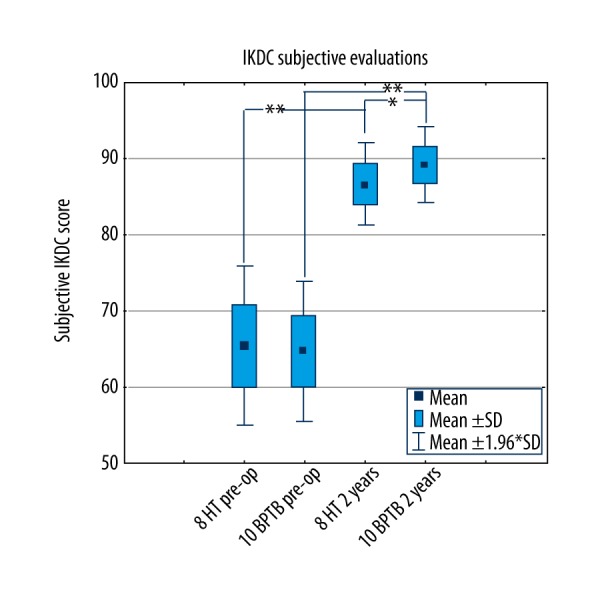
The mean IKDC subjective scores pre-surgery and at two years after the ACLR. * Significant difference at p<0.05, ** significant difference at p<0.001.
IKDC objective evaluations and knee stability IKDC objective results were excellent (grade A) and good (grade B) in 83 of 88 patients (94.3%) after 10 mm BPTB and in 78 of 95 patients (82%) after 8 mm HT ACLR (p<0.001) (Table 3).
Table 3.
Data of the two groups at two-year follow-up: evaluation of manual anterior-posterior knee laxity according to IKDC.
| Characteristic | 8 mm HT (n=95) | 10 mm BPTB (n=88) | p Value |
|---|---|---|---|
| IKDC A, B – normal and nearly normal | 78 | 83 | p<0.001 |
| IKDC C, D – abnormal | 17 | 5 | p<0.001 |
| Lachman test IKDC A – normal: side-to-side laxity difference 0–2 mm |
61 | 73 | p<0.05 |
| Lachman test IKDC B nearly normal: side-to-side laxity difference 3–5 mm |
17 | 10 | p<0.001 |
| Lachman test IKDC C, D: clear: side-to-side laxity difference >5 mm |
17 | 5 | p<0.001 |
| Pivot shift IKDC A – normal (negative) |
72 | 81 | p<0.05 |
| Pivot shift IKDC B – glide (positive) |
11 | 5 | p<0.05 |
| Pivot shift IKDC C, D – clear (positive) |
12 | 2 | p<0.001 |
| IKDC subjective score for 17–20 year subgroup | 85.47±2.1 | 89.9±2.0 | p<0.001 |
| IKDC subjective score for 20–25 year subgroup | 87.17±2.5 | 89.19±2.9 | p=0.006 |
| IKDC subjective score for 25–32 year subgroup | 86.93±2.9 | 89.1±2.3 | p<0.001 |
| IKDC subjective score for women | 86.4±2.9 | 89.2±1.2 | p<0.001 |
| IKDC subjective score for men | 86.7±2.8 | 89.2±2.5 | P<0.001 |
| Average Tegner activity scores | 5.8±1.1 | 6.5±1.1 | p<0.001 |
| Average Tegner activity scores for 17–20 year subgroup | 5.3±1.2 | 6.9±1.3 | p=0.001 |
| Average Tegner activity scores for 20–25 y subgroup | 6.4±1.2 | 6.6±1.2 | p=0.43 |
| Average Tegner activity scores for 25–32 y subgroup | 5.7±0.9 | 6.4±1.0 | p=0.002 |
There was no difference between the groups with respect to range of motion at the two-year follow-up (p=0.44). The percentage of manual anterior-posterior knee laxity and positive pivot-shift signs was higher in the 8 mm HT ACLR group compared to the 10 mm BPTB group at two years (p<0.001; Table 3). At the two-year point, 81 patients (92%) who had the 10 mm BPTB technique had a negative pivot-shift sign and five patients (6%) had a glide-positive sign and two patients (2%) had moderate and marked subluxation. At the same time-interval, 72 patients (76%) who had an 8 mm HT ACLR technique had no pivot-shift sign, 12 patients (12%) had a glide-positive sign and 12 patients (12%) had moderate and marked subluxation (Table 3).
Activity level and return to pre-injury sport activities
There were 83 of the 88 patients (94%) in 10 mm BPTB group and 69 of the 95 patients (73%) in 8 mm HT group who were successful in returning to their previous level of sports activity at different times after ACLR (Table 4).
Table 4.
Time period from surgery to return to pre-injury sports and revision rate.
| Time from surgery to return to sports | 8 mm HT patients (n=95) | 10 mm BPTB patients (n=88) |
|---|---|---|
| 6–8 months | 6 | 12 |
| 8–10 months | 32 | 35 |
| 10–12 months | 41 | 37 |
| ≥12 months | 16 | 4 |
| Average return time, months | 9.2 | 9.8 |
| Returned to pre-injury sports | 69 | 83 |
| Did not returned to pre-injury sports | 26 | 5 |
| Needed revision ACLR: | 14 | 2 |
| 17–20 years – ACLR revisions | 7 | 0 |
| 20–25 years – ACLR revisions | 3 | 2 |
| 25–32 years – ACLR revisions | 4 | 0 |
The average scores of Tegner activity in the 8 mm HT group decreased from 6.5 at pre-injury to 5.8 at two-year follow-up (p<0.001) and from 6.7 at pre-injury to 6.5 at two-year follow-up (p=0.4) in the 10 mm BPTB group; the ability to restore pre-injury sports activities was higher after ACLR with 10 mm BPTB graft (6.5) compared to 8 mm HT graft (5.8) (p<0.001) (Figure 2).
Figure 2.
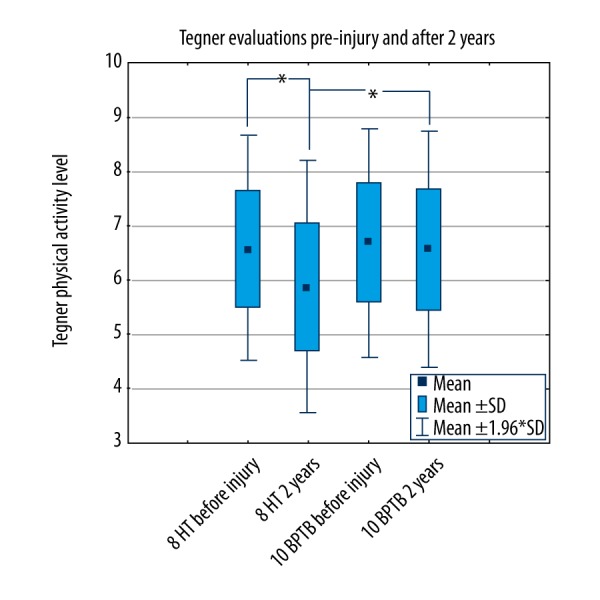
The Tegner scores pre-injury and at two years after the ACLR. * Significant difference at p<0.001.
10 mm BPTB ACLR women’s subjective IKDC evaluations favored against 8 mm HT ACLR
There was no significant difference in subjective IKDC evaluations between the women and men for either groups at two years (p>0.05); however, the 10 mm BPTB ACLR group of women had significant higher IKDC evaluations compared to men from the 8 mm HT ACLR group (p<0.001) (Table 3).
IKDC subjective and Tegner evaluations were lower in younger patients after 8 mm HT ACLR
Subjective IKDC evaluations of the patients younger than 20 years of age in the 8 mm HT ACLR group were significantly lower compared to patients older than 20 years of age (p=0.02) (Table 3; Figure 3).
Figure 3.

Subjective IKDC evaluations accordingly to age. * Significant difference at p<0.001.
Also, patients younger than 20 years old in the 8 mm HT ACLR group had decreased sports activity levels evaluated by Tegner score (p<0.04) (Table 3; Figure 4).
Figure 4.
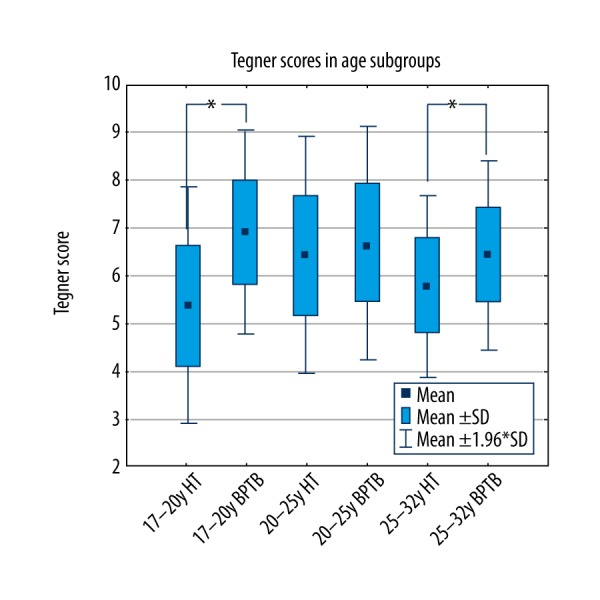
The Tegner scores two years after the ACLR in different age groups. * Significant difference at p<0.01.
Revisions rate
Autograft with 8 mm HT ACLR correlated with higher rate of revision ACL reconstruction: revision was required in two of 88 patients (2.2%) in the BPTB group compared with 14 of 95 patients (14.7%) in the 8 mm HT group (p<0.05) (Table 4). Interestingly, almost all revision ACLRs were performed for men (15 men versus one woman): one revision ACLR was performed for a 17-year-old girl from the HT group, two revisions for a 24-year-old man from the BPTB group. In the HT group there were four revisions in the subgroup of patients 25–32 years of age; three revisions in the subgroup of 20–25-year-olds; and six revisions in the subgroup of 17–20 years olds (Table 4).
Discussion
In our study we compared an 8 mm HT graft group with a 10 mm BPTB group for ACLR outcomes at two-year follow-up and found that the smaller graft size was a predictor of higher knee laxity and greater revision rate. We also found that patients in the 10 mm BPTB group might have better ability to restore pre-injury sports activities, as they reached higher IKDC subjective scores, their IKDC objective scores were grade A and B, and they had better outcome test results (Lachman and pivot-shift).
A number of prospective randomized studies using different fixation methods have been conducted to evaluate the differences between patellar tendon and hamstring grafts [6,14–17]. Most of these studies have failed to show significant differences in knee functional outcome scores. The number of ACL reconstructions using a patellar tendon autograft is gradually decreasing in all countries [1]. Granan et al. [18] reported that 71% of patients in Denmark were reconstructed with HT autografts, 61% in Norway, and 86% in Sweden. In our study, the number in the HT group was also higher than in the BPTB group (95 versus 88). The reason for this is probably that a number of randomized studies have shown comparable results between these two graft types, apart from donor-site morbidity and anterior knee problems, which are more frequent after using a patellar tendon autograft [19–22]. Our study results showed that BPTB ACLR was significantly more favorable compared to HT ACLR.
To analyze differences, a meta-analysis was performed by Persson et al.[23] who found that the revision rate after two years in the quadrupled HT group was 2.8% versus 0.7% (p=0.001) in the BPTB group, especially in the younger 15–19-year old) subgroup: quadrupled HT was 5.4% versus 1.2% for BPTB graft) [23]. The previous studies have shown younger age (25 years and younger) as an important risk factor for revision with significantly higher failure rates [24–27]. Our study results were in line with these findings. In our study, one 17-year-old girl from the HT group, two 24-year-old men from the BPTB group, and four 25–32-year-old patients from the HT group, three 20–25-year-old patients from the HT group, and six 17–20-year-old patients from the HT group underwent revision surgery. The revision rate in our study was 8.7% (2.2% BPTB and 14.7% HT), quite high compared with other studies. A Danish study report only 2.9% revision rate after two-year follow-up, nearly the same as a Swedish study (4.1% after five-year follow-up) [1,28,29]. But these studies did not report separated revision rates according to the graft groups. A systematic review by Lewis et al. [30] analyzed 11 studies and found that postoperative graft failure occurred in 32 of 921 ACL reconstructions (3.5%). A case-control study by Hettrich et al. [26] included 980 patients prospectively followed, and after two years reported a revision rate after ACLR of 7.7%. These findings were similar to our findings, but do not report group revision rates. These were also similar results reported by Maletis et al. [31] based on data from Kaiser Permanente registry. They found 1.82 times higher risk of early revision for HT grafts compared with BPTB grafts with mean follow-up of 1.5 years (p=0.019). A systematic review by Spindler reported increased knee laxity after hamstring ACLR in three of seven studies. The most significant finding was a significant correlation between increased patient-reported IKDC outcome score and decreased risk of revision surgery after BPTB ACLR [32]. These data demonstrated that despite HT and BPTB grafts showing no differences in subjective scores after ACLR, HT ACLR has more risks for revisions and greater knee laxity compared to BPTB [33–36].
All of these studies lacked ACL graft size matching. ACL graft diameter is still controversial and no evidence is available to make decisions for ideal graft size. According to our study data, both the 8 mm hamstring and 10 mm patella tendon ACLR patients did significantly better at the two-year follow-up; however, the 8 mm HT ACLR group showed significant higher knee laxity values compared to the 10 mm BPTB group. This finding may be related to graft type and graft size. Many studies have shown no significant clinical differences between these two techniques, but no emphasize on the graft diameters were clearly outlined. In the Magnussen et al. study [2], the revision rate was significantly higher in patients with grafts sized 7 mm or smaller. This threshold was higher for patients younger than 20 years of age and was found to be 8 mm.
The association of activity level with ACLR failure and revision ACLR has been shown in several studies also with different graft types, but this associations in BPTB groups seems to be less important [2,25,37,38].
The ability to restore pre-injury sports activities was higher in the 10 mm BPTB ACLR group (score 6.5) compared to the 8 mm HT ACLR group (score 5.8) in our study. Comparison of pre-injury Tegner activity scores to postoperative scores revealed that patients in the HT group did not return to their pre-injury level of activity as well as patients in the BPTB group. Patients in the HT group had a significant increase in pain compared with the BPTB group (p=0.034) [39]. Aglietti et al. [5] also confirmed that return to sports activities was more frequent among patellar tendon graft patients. Our study showed that 94% of the BPTB group and 73% of the HT group successfully returned to pre-injury level. Maletis et al. [40] found more patients after BPTB compared to HT were able to return to pre-injury Tegner physical activity level at two years. They concluded that although not statistically significant, the hamstring group had more failures, more laxity on clinical examination, and more patients with larger KT-1000 arthrometer differences. These results indicate a trend toward increased graft laxity in female patients undergoing reconstruction with hamstring autograft compared with patellar tendon when evaluated by a single surgeon using similar fixation techniques at short- to medium-range follow-up.
The IKDC evaluation showed that 82% of the HT group and 94% of the BPTB group patients classified as normal in our study; nearly the same as reported in by Corry et al. [41] where 82% of the patellar tendon group and 89% of the hamstring tendon group had normal or nearly normal scores on IKDC assessment, and in comparison with Ericsson et al. study [42], where only 58% of the patients were classified as normal or nearly normal, and 42% as abnormal or severely abnormal at follow-up.
Our study revealed that subjective IKDC evaluations and decreased sports activity levels of the patients younger than 20 years old in the 8 mm HT ACLR group were significantly lower compared to patients older than 20 years of age. Age, self-evaluations, and Tegner sport activity level did not correlated in the 10 mm BPTB group. In the 8 mm HT ACLR group the need for revision ACL reconstruction was correlated. Higher sports activity levels have previously been shown to be associated with a higher failure rate of ACLR when graft size was less, and this association has been shown to be important for different graft types and depends of graft size [24,40,43,44].
Limited emphasis has previously been placed on the return to pre-injury sports activities after ACL reconstructions comparing graft size. Tegner activity level did not correlate statistically with ACLR failure in our study, although we expected to find an association. Younger patients tend to demonstrate higher activity levels, represented by higher Tegner scores [11]. As discussed by Kamien et al. [45], an increased activity level is generally implicated in the higher failure rate in this population, but a higher frequency of re-injury likely also plays a role. This association was previously described by Shelbourne et al. [25] and Borchers et al. [37]. Kamien et al. reported that the mean Tegner activity score was higher in younger patients compared with older patients (5.58 versus 4.28), the difference between them approached but did not reach statistical significance (p=0.066). Our study revealed nearly the same results (6.4 versus 5.7 in the HT group, 6.6 versus 6.4 in BPTB group).
Wiger et al. [46] reported that only 40% of patients returned to their pre-injury level. In comparison, our study found that the ability to restore pre-injury sports activities was higher after 10 mm BPTB ACLR (6.5) compared to 8 mm HT ACLR (5.8), and 94% of patients in the 10 BPTB group and 73% in the HT group were successful in returning to their previous level of sports activity.
From the gender point of view, Anderson et al. [47] discussed that female athletes have a disproportionately high number of ACL injuries when compared with their male counterparts. Neither Shelbourne et al. nor Gwinn et al. found extrinsic differences that make women more likely to sustain ACL tears [48,49]; and neither did we. Ericsson et al. [42] also found no differences between men and women in outcome scores (VAS, Lysholm, IKDC, patellofemoral score). In our study, there was no significant difference in subjective IKDC evaluations between women and the men inside both groups at two-year follow-up; however, women from the 10 mm BPTB ACLR group had significant higher IKDC evaluations compared to men from the 8 mm HT ACLR group. Also, the HT group had more failures, more knee laxity, and results indicated a trend toward increased graft laxity in female patients undergoing reconstruction with HT autograft compared with patellar tendon when evaluated by a single surgeon using similar fixation techniques at short-range to medium-range follow-up [39].
There were several weaknesses of our study. One was the retrospective nature of the study. The small number of patients limited our ability to detect differences. The other problem was the number of patients with small diameter grafts (8 mm). This did not give us enough power to calculate significant differences, if such existed, in the failure rates between smaller and larger grafts. We did not register other possible causes of failure, and did not analyze the tunnel and graft position. Postoperative Tegner activity level and stability were the only outcome measures used in this study.
Conclusions
Based on our results, comparing 8 mm hamstring graft with 10 mm bone-patellar-tendon-bone graft ACLR outcomes at two-year follow-up, we concluded that smaller graft size was a predictor of higher knee laxity and greater revision rate, and that patients after ACLR using 10 mm BPTB graft had better ability to restore pre-injury sports activities, and had better outcome results based on IKDC scores and reached better knee stability.
Footnotes
Source of support: Departmental sources
Conflict of interests
None.
Reference
- 1.Ahlden M, Samuelsson K, Sernert N, et al. The Swedish National Anterior Cruciate Ligament Register: A report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012;40:2230–35. doi: 10.1177/0363546512457348. [DOI] [PubMed] [Google Scholar]
- 2.Magnussen RA, Lawrence JTR, West RL, et al. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthrosc – J Arthrosc Relat Surg. 2012;28:526–31. doi: 10.1016/j.arthro.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 3.Park SY, Oh H, Park S, et al. Factors predicting hamstring tendon autograft diameters and resulting failure rates after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21:1111–18. doi: 10.1007/s00167-012-2085-4. [DOI] [PubMed] [Google Scholar]
- 4.Ahmad CS, Gardner TR, Groh M, et al. Mechanical properties of soft tissue femoral fixation devices for anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:635–40. doi: 10.1177/0363546503261714. [DOI] [PubMed] [Google Scholar]
- 5.Aglietti P, Buzzi R, Zaccherotti G, De Biase P. Patellar tendon versus doubled semitendinosus and gracilis tendons for anterior cruciate ligament reconstruction. Am J Sports Med. 1994;22:211–17. doi: 10.1177/036354659402200210. discussion 217–18. [DOI] [PubMed] [Google Scholar]
- 6.Aune AK, Holm I, Risberg MA, et al. Four-strand hamstring tendon autograft compared with patellar tendon-bone autograft for anterior cruciate ligament reconstruction. A randomized study with two-year follow-up. Am J Sports Med. 2001;29:722–28. doi: 10.1177/03635465010290060901. [DOI] [PubMed] [Google Scholar]
- 7.Becker R, Voigt D, Stärke C, et al. Biomechanical properties of quadruple tendon and patellar tendon femoral fixation techniques. Knee Surgery, Sport Traumatol Arthrosc. 2001;9:337–42. doi: 10.1007/s001670100223. [DOI] [PubMed] [Google Scholar]
- 8.Giurea M, Zorilla P, Amis AA, Aichroth P. Comparative pull-out and cyclic-loading strength tests of anchorage of hamstring tendon grafts in anterior cruciate ligament reconstruction. Am J Sports Med. 1999;27:621–25. doi: 10.1177/03635465990270051301. [DOI] [PubMed] [Google Scholar]
- 9.Mariscalco MW, Flanigan DC, Mitchell J, et al. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: A multicenter orthopaedic outcomes network (MOON) cohort study. Arthrosc – J Arthrosc Relat Surg. 2013;29:1948–53. doi: 10.1016/j.arthro.2013.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hefti E, Müller W, Jakob RP, Stäubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surgery, Sport Traumatol Arthrosc. 1993;1:226–34. doi: 10.1007/BF01560215. [DOI] [PubMed] [Google Scholar]
- 11.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985:43–49. [PubMed] [Google Scholar]
- 12.Edwards A, Bull AMJ, Amis AA. The attachments of the anteromedial and posterolateral fibre bundles of the anterior cruciate ligament: PPPart 2: Femoral attachment. Knee Surgery, Sport Traumatol Arthrosc. 2008;16:29–36. doi: 10.1007/s00167-007-0410-0. [DOI] [PubMed] [Google Scholar]
- 13.Ferretti M, Ekdahl M, Shen W, Fu FH. Osseous landmarks of the femoral attachment of the anterior cruciate ligament: an anatomic study. Arthrosc – J Arthrosc Relat Surg. 2007;23:1218–25. doi: 10.1016/j.arthro.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 14.Aglietti P, Giron F, Buzzi R, et al. Anterior cruciate ligament reconstruction: bone-patellar tendon-bone compared with double semitendinosus and gracilis tendon grafts. A prospective, randomized clinical trial. J Bone Joint Surg Am. 2004;86–A:2143–55. [PubMed] [Google Scholar]
- 15.Webster KE, Feller JA, Hartnett N, et al. Comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction: A 15-year follow-up of a randomized controlled trial. Am J Sports Med. 2016;44:83–90. doi: 10.1177/0363546515611886. [DOI] [PubMed] [Google Scholar]
- 16.Matsumoto A, Yoshiya S, Muratsu H, et al. A comparison of bone-patellar tendon-bone and bone-hamstring tendon-bone autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2006;34:213–19. doi: 10.1177/0363546505279919. [DOI] [PubMed] [Google Scholar]
- 17.Shaieb MD, Kan DM, Chang SK, et al. A prospective randomized comparison of patellar tendon versus semitendinosus and gracilis tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30:214–20. doi: 10.1177/03635465020300021201. [DOI] [PubMed] [Google Scholar]
- 18.Granan L-P, Forssblad M, Lind M, Engebretsen L. The Scandinavian ACL registries 2004–2007: Baseline epidemiology. Acta Orthop. 2009;80:563–67. doi: 10.3109/17453670903350107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ejerhed L, Kartus J, Sernert N, et al. Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction? A prospective randomized study with a two-year follow-up. Am J Sport Med J Sport Med. 2003;31:19–25. doi: 10.1177/03635465030310011401. [DOI] [PubMed] [Google Scholar]
- 20.Eriksson K, Anderberg P, Hamberg P, et al. There are differences in early morbidity after ACL reconstruction when comparing patellar tendon and semitendinosus tendon graft. A prospective randomized study of 107 patients. Scand J Med Sci Sports. 2001;11:170–77. [PubMed] [Google Scholar]
- 21.Laxdal G, Kartus J, Hansson L, et al. A prospective randomized comparison of bone-patellar tendon-bone and hamstring grafts for anterior cruciate ligament reconstruction; 15650664. Arthrosc – J Arthrosc Relat Surg. 2005;21:34–42. doi: 10.1016/j.arthro.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 22.Liden M, Ejerhed L, Sernert N, et al. Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction: A prospective, randomized study with a 7-Year follow-up. Am J Sports Med. 2007;35:740–48. doi: 10.1177/0363546506298275. [DOI] [PubMed] [Google Scholar]
- 23.Persson A, Fjeldsgaard K, Gjertsen J-E, et al. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: A study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004–2012. Am J Sports Med. 2014;42:285–91. doi: 10.1177/0363546513511419. [DOI] [PubMed] [Google Scholar]
- 24.Barrett AM, Craft JA, Replogle WH, et al. Anterior cruciate ligament graft failure: A comparison of graft type based on age and tegner activity level. Am J Sports Med. 2011;39:2194–98. doi: 10.1177/0363546511415655. [DOI] [PubMed] [Google Scholar]
- 25.Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37:246–51. doi: 10.1177/0363546508325665. [DOI] [PubMed] [Google Scholar]
- 26.Hettrich CM, Dunn WR, Reinke EK, et al. The rate of subsequent surgery and predictors after anterior cruciate ligament reconstruction: Two- and 6-year follow-up results from a multicenter cohort. Am J Sports Med. 2013;41:1534–40. doi: 10.1177/0363546513490277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaeding CC, Aros B, Pedroza A, et al. Allograft versus autograft anterior cruciate ligament reconstruction: predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3:73–81. doi: 10.1177/1941738110386185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lind M, Menhert F, Pedersen AB. The first results from the Danish ACL reconstruction registry: Epidemiologic and 2 year follow-up results from 5,818 knee ligament reconstructions. Knee Surgery, Sport Traumatol Arthrosc. 2009;17:117–24. doi: 10.1007/s00167-008-0654-3. [DOI] [PubMed] [Google Scholar]
- 29.Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind M. Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: Results from the Danish registry of knee ligament reconstruction. Am J Sports Med. 2014;42(2):278–84. doi: 10.1177/0363546513509220. [DOI] [PubMed] [Google Scholar]
- 30.Lewis PB, Parameswaran AD, Rue JH, Bach BR. Systematic review of single-bundle anterior cruciate ligament reconstruction outcomes: A baseline assessment for consideration of double-bundle techniques. Am J Sports Med. 2008;36:2028–36. doi: 10.1177/0363546508322892. [DOI] [PubMed] [Google Scholar]
- 31.Maletis GB, Inacio MCS, Desmond JL, Funahashi TT. Reconstruction of the anterior cruciate ligament: Association of graft choice with increased risk of early revision. Bone Jt J. 2013;95 B:623–28. doi: 10.1302/0301-620X.95B5.30872. [DOI] [PubMed] [Google Scholar]
- 32.Spindler KP. Anterior cruciate ligament reconstruction autograft choice: Bone-tendon-bone versus hamstring: does it really matter? A systematic review. Am J Sports Med. 2004;32:1986–95. doi: 10.1177/0363546504271211. [DOI] [PubMed] [Google Scholar]
- 33.Mohtadi NG, Chan DS, Dainty KN, Whelan DB. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2011;9:CD005960. doi: 10.1002/14651858.CD005960.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Abbas MM, Abulaban AA, Darwish HH. Functional outcomes of bone tendon bone versus soft tissue arthroscopic anterior cruciate ligament reconstruction, a comparative study. Saudi Med J. 2013;34:153–60. [PubMed] [Google Scholar]
- 35.Leys T, Salmon L, Waller A, et al. Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: A prospective study of hamstring and patellar tendon grafts. Am J Sports Med. 2012;40:595–605. doi: 10.1177/0363546511430375. [DOI] [PubMed] [Google Scholar]
- 36.Otero AL, Hutcheson L. A comparison of the doubled semitendinosus/gracilis and central third of the patellar tendon autografts in arthroscopic anterior cruciate ligament reconstruction. Arthroscopy. 1993;9:143–48. doi: 10.1016/s0749-8063(05)80363-9. [DOI] [PubMed] [Google Scholar]
- 37.Borchers JR, Pedroza A, Kaeding C. Activity level and graft type as risk factors for anterior cruciate ligament graft failure: A case-control study. Am J Sports Med. 2009;37:2362–67. doi: 10.1177/0363546509340633. [DOI] [PubMed] [Google Scholar]
- 38.Salmon L, Russell V, Musgrove T, et al. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthrosc – J Arthrosc Relat Surg. 2005;21:948–57. doi: 10.1016/j.arthro.2005.04.110. [DOI] [PubMed] [Google Scholar]
- 39.Barrett GR, Noojin FK, Hartzog CW, Nash CR. Reconstruction of the anterior cruciate ligament in females: A comparison of hamstring versus patellar tendon autograft. Arthroscopy. 2002;18:46–54. doi: 10.1053/jars.2002.25974. [DOI] [PubMed] [Google Scholar]
- 40.Maletis GB, Cameron SL, Tengan JJ, Burchette RJ. A prospective randomized study of anterior cruciate ligament reconstruction: A comparison of patellar tendon and quadruple-strand semitendinosus/gracilis tendons fixed with bioabsorbable interference screws. Am J Sports Med. 2006;35:384–94. doi: 10.1177/0363546506294361. [DOI] [PubMed] [Google Scholar]
- 41.Corry IS, Webb JM, Clingeleffer AJ, Pinczewski LA. Arthroscopic reconstruction of the anterior cruciate ligament. A comparison of patellar tendon autograft and four-strand hamstring tendon autograft. Am J Sports Med. 1999;27:444–54. doi: 10.1177/03635465990270040701. [DOI] [PubMed] [Google Scholar]
- 42.Eriksson K, Anderberg P, Hamberg P, et al. A comparison of quadruple semitendinosus and patellar tendon grafts in reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 2001;83:348–54. doi: 10.1302/0301-620x.83b3.11685. [DOI] [PubMed] [Google Scholar]
- 43.Barrett GR, Luber K, Replogle WH, Manley JL. Allograft anterior cruciate ligament reconstruction in the young, active patient: Tegner activity level and failure rate. Arthrosc – J Arthrosc Relat Surg. 2010;26:1593–601. doi: 10.1016/j.arthro.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 44.Kim S-G, Kurosawa H, Sakuraba K, et al. Analysis of the risk factors regarding anterior cruciate ligament reconstruction using multiple-looped semitendinosus tendon. Knee. 2005;12:366–69. doi: 10.1016/j.knee.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 45.Kamien PM, Hydrick JM, Replogle WH, et al. Age, graft size, and tegner activity level as predictors of failure in anterior cruciate ligament reconstruction with hamstring autograft. Am J Sports Med. 2013;41:1–5. doi: 10.1177/0363546513493896. [DOI] [PubMed] [Google Scholar]
- 46.Wiger P, Brandsson S, Kartus J, et al. A comparison of results after arthroscopic anterior cruciate ligament reconstruction in female and male competitive athletes A two- to five-year follow-up of 429 patients. Scand J Med Sci Sports. 1999;9:290–95. doi: 10.1111/j.1600-0838.1999.tb00248.x. [DOI] [PubMed] [Google Scholar]
- 47.Anderson AF, Dome DC, Gautam S, et al. Correlation of anthropometric measurements, strength, anterior cruciate ligament size, and intercondylar notch characteristics to sex differences in anterior cruciate ligament tear rates. Am J Sports Med. 2001;29:58–66. doi: 10.1177/03635465010290011501. [DOI] [PubMed] [Google Scholar]
- 48.Shelbourne KD, Davis TJ, Klootwyk TE. The relationship between intercondylar notch width of the femur and the incidence of anterior cruciate ligament tears. A prospective study. Am J Sports Med. 1998;26:402–8. doi: 10.1177/03635465980260031001. [DOI] [PubMed] [Google Scholar]
- 49.Gwinn DE, Wilckens JH, McDevitt ER, et al. The relative incidence of anterior cruciate ligament injury in men and women at the United States Naval Academy. Am J Sports Med. 2000;28:98–102. doi: 10.1177/03635465000280012901. [DOI] [PubMed] [Google Scholar]


