Abstract
Background
Bispectral index (BIS) monitoring can reduce the duration of anesthesia. This study aimed to evaluate the effects of BIS monitoring during surgery for resection of colon carcinoma in elderly patients using the Attention Network Test (ANT) to study alerting, orienting, and executive functions, and the Confusion Assessment Method (CAM).
Material/Methods
Eighty-one patients (65–75 years) underwent radical surgery for colon carcinoma with general intravenous anesthesia, propofol (6–8 mg/kg/h), vecuronium (0.03–0.05 mg/kg/min), and remifentanil (0.1–0.2 μg/kg/min). The BIS group (n=41) underwent adjustment of anesthesia to maintain a BIS value between 40–60; the non-BIS group (N=40) underwent standard intraoperative hemodynamic monitoring. Primary endpoints were alerting, orienting, and executive functions assessed pre-operatively and on postoperative days 1 and 5 using the ANT; the secondary endpoint was delirium during the first five postoperative days, assessed using the CAM.
Results
Propofol and remifentanil doses were significantly lower in the BIS group compared with the non-BIS group (P<0.001). Alerting, orienting, and executive functions showed no differences between the two groups pre-operatively but were impaired in both groups on postoperative day 1 compared with pre-operative levels (P<0.001). On postoperative day 5, alerting (P=0.607) and orienting (P=0.851) functions recovered in the BIS group but remained impaired in the non-BIS group (P<0.001). Delirium was significantly lower in the BIS group compared with the non-BIS group (17.5% vs. 27.5%) (P<0.001).
Conclusions
BIS-guided anesthesia was associated with reduced anesthetic exposure, early postoperative recovery of alerting and orienting functions, and reduced postoperative delirium.
MeSH Keywords: Attention, Cognitive Therapy, Consciousness
Background
Advanced age is an independent risk factor for the development of postoperative cognitive dysfunction (POCD) [1–6]. POCD is associated with increased mortality, decreased quality of life, and increased dependency [7,8]. Therefore, it is important to develop strategies to reduce the incidence and severity of POCD. POCD includes impairment in memory, attention, information processing, and cognitive flexibility [9,10]. Among these, attention networks have been proposed to consist of three functional components, alerting, orienting and executive control, which have specific anatomical and biochemical mechanisms in the brain [11–13].
Monitoring of the depth of anesthesia can now be undertaken using the bispectral index (BIS), which has been shown to reduce complications associated with and following general anesthesia [14–20]. Notably, adjusting the anesthetic drug dose to maintain the BIS at between 40–60 during general anesthesia has been shown to be associated with an 11–27% reduction total anesthetic drug dose and to improve early cognitive recovery [14,16]. However, little is known about the effects of general anesthesia and BIS monitoring on attention networks in elderly patients.
The hypothesis that drove this study was that BIS monitoring in elderly patients might reduce their overall exposure to anesthetic drugs during surgery and reduce the extent of postoperative attention network dysfunction. The aims of this study were to evaluate the effects of BIS monitoring during surgery for resection of colon carcinoma in elderly patients using the Attention Network Test (ANT) to study alerting, orienting, and executive functions, and to use the Confusion Assessment Method (CAM) to assess the effects of BIS monitoring on the incidence of acute postoperative delirium in this patient group.
Material and Methods
Study participants and ethical approval
This prospective, double-blind, randomized, parallel group study recruited elderly patients with colon carcinoma who underwent general anesthesia and radical surgery at the First Affiliated Hospital of Anhui Medical University, China, between January 2014 and November 2016.
Ethical approval (No. 20130406) was provided by the Ethical Committee of Anhui Medical University, Hefei, Anhui, China in July 2013. All patients provided written informed consent before enrolment in the study, and all procedures were conducted according to the guidelines from the Declaration of Helsinki. This trial has been registered with the Chinese Clinical Trial Registry (ChiCTR-TRC-1800014707).
The study inclusion criteria were: an American Society of Anesthesiologists (ASA) physical status classifications of between I–III; patient age between 65–75 years; a Mini-Mental State Examination (MMSE) score >27 points [21]; normal vision or corrected visual acuity; duration of surgery expected to be two hours or more; and an anticipated postoperative hospital stay of at least seven days.
The study exclusion criteria were: a diagnosis of Parkinson’s disease; a history of transient ischemic attack (TIA) or stroke; liver or renal insufficiency; a diagnosis of Alzheimer’s disease; visual or sensory disturbance; language difficulties or significant hearing impairment; and the use of drugs affecting cognitive function.
The patients were randomly allocated to a bispectral index (BIS) monitoring group or a non-BIS (control) group according to a computer-generated assignment sequence. The patients, attending anesthesiologist, and surgeons were blinded to the group allocation. Also, the investigators responsible for postoperative data collection and outcome assessment were blinded to the patient data, including the Attention Network Test (ANT), Confusion Assessment Method (CAM), and MMSE scores and the group allocation.
Anesthetic procedures and interventions
The general anesthesia induction strategy included sufentanil (0.35 μg/kg), propofol (1–2 mg/kg), and vecuronium (0.1 mg/kg). The anesthesia maintenance strategy included intravenous administration of propofol (6–8 mg/kg/h), vecuronium (0.03–0.05 mg/kg/min), and remifentanil (0.1–0.2 μg/kg/min).
For patients in the BIS group, a BIS monitor was used to document the BIS values, and the rate of propofol administration during maintenance of anesthesia was adjusted to maintain the BIS value at between 40–60 [14]. The procedure used for anesthesia in the control group was the same as that used in the BIS group, except that the dose of the anesthetic was not adjusted according to the BIS value. Although a BIS monitor was also used for patients in the control group, the attending anesthesiologists were blinded to the BIS value and were not given visual access to the BIS monitor during induction and maintenance of anesthesia. Instead, for patients in the non-BIS or control group, intravenous anesthesia was adjusted according to clinical experience and intraoperative hemodynamic changes. If the intraoperative blood pressure and heart rate decreased by ≥20%, the patient was given vasopressor drugs and the dose of the anesthetic drugs was reduced. If the intraoperative blood pressure and heart rate increased by no more than 20%, the patient was given antihypertensive drugs and the doses of the anesthetic drugs were increased. In both groups (the BIS group and the non-BIS or control group), if the systolic blood pressure fell to less than 20% of the normal value, the fluid infusion rate was accelerated and 5 mg bolus injections of ephedrine were administered. Also, if the heart rate decreased to <60 beats/min, a bolus intravenous injection of 0.3 mg atropine was given. None of the patients received epidural anesthesia or any other form of regional anesthesia. All physicians and anesthesiologists involved in the surgery were senior clinicians with more than five years of relevant clinical experience.
Postoperative analgesia was provided to both groups of patients. During the first 48 hours after surgery, the patients received 100 mL of normal saline solution containing flurbiprofen (100 mg) and sufentanil (2–3 μg/kg), administered by patient-controlled intravenous analgesia, at an infusion rate of 2 mL/h, and a lockout time of 15 min with 0.5 mL bolus doses. A visual analog scale (VAS) (0=no pain, 10=worst possible pain) was used to evaluate the postoperative management of pain during patient-controlled intravenous analgesia [22]. The VAS score for pain was assessed daily during the first five postoperative days. Patients with a VAS score >3, indicating inadequate analgesia, were excluded from this study because the presence of pain can influence the postoperative assessment of attention network functions, particularly the alerting and executive control networks [23], and pain would have been a confounding factor.
Attention Network Test (ANT) software
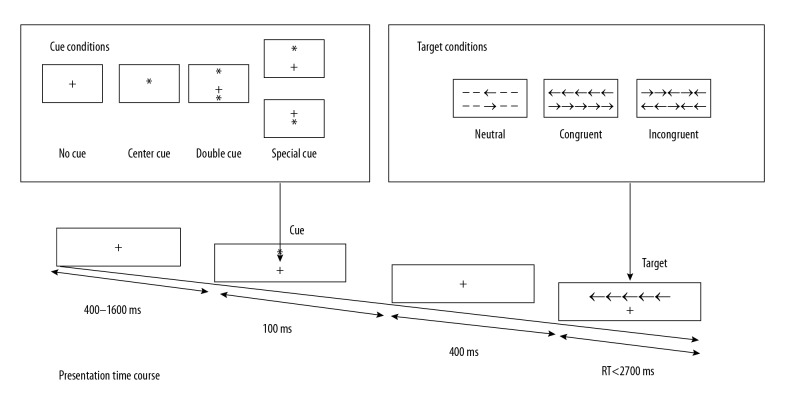
This study used the classical Attention Network Test (ANT) program proposed by Fan and colleagues [24.25]. Firstly, the participant stared at a fixed cross (+) in the center of the computer screen for between 400–1600 ms (Figure 1). Secondly, a cue (*) appeared as a signal for 100 ms. Thirdly, a fixed cross (+) appeared again in the center of the screen for about 400 ms. Finally, the target was presented. After the key target disappeared, participants were asked to press the ← or → button as soon as possible, with a normal reaction time that was expected to be <1700 ms. Each test was divided into four, with four types of cue conditions: no cue, a double cue, a central cue, and a spatial cue.
Figure 1.
Schematic representation of the Attention Network Test (ANT). Shown are the three target stimuli, the four cue conditions, and the sequence of events for the Attention Network Test (ANT) used in the present study. Adapted from Fan et al. [24,25].
According to whether the arrow appeared centrally or at either side, the relationship was divided into three conditions: a single arrow above or below the fixed cross (+), five simultaneous arrows pointing in the same direction above or below the fixed cross (+), or five simultaneous arrows pointing in opposite directions above or below the fixed cross (+). The experiment comprised 336 trials, including 24 practices and 312 formal trials, divided into four stages. The total time required for the test was about 30 minutes, and the participants were allowed to rest for between four and five minutes. The reaction time (RT), average response time, and accuracy were determined. The efficiency of the attention network was calculated as follows:
Alerting effect=RT (no cue)–RT (double cue) (the higher the value, the more efficient the alerting network).
Orienting effect=RT (center cue)–RT (spatial cue) (the higher the value, the more efficient the orienting network).
Executive control network effect=RT (incongruent)–RT (congruent) (the smaller the value, the more efficient the executive control network).
The alerting network represented the sensitivity to incoming stimuli; the orienting network represented the selection of information from sensory input; and the control network represented the ability to resolve conflicts between feelings, thoughts, and responses [9]. The person who administered the ANT was blinded to the scores obtained for the alerting, orienting, and executive control functions. Patients who did not complete the ANT were excluded from the study.
Data collection
The following information was collected for all participants: age, gender, body mass index (BMI), level of education, MMSE score, ASA classification, and data regarding surgery, which included the duration of anesthesia, the duration of surgery, the volume of transfused blood, and the dose of intravenous anesthetics. Attention network function, including alerting, orienting and executive control functions, was assessed pre-operatively and at day 1 and day 5 postoperatively using the ANT.
Delirium was assessed daily (from 9 am to 11 am) during postoperative day 1 to day 5 using the Confusion Assessment Method (CAM). The sensitivity of the CAM has been reported to be between 94–100% and the specificity is between 90–95% [26]. The diagnosis of delirium by CAM required the presence of the following clinical symptoms and signs: (1) an acute onset of cognitive changes with a fluctuating course, (2) inattention, together with either (3) disorganized thinking, or (4) an altered level of consciousness [27]. To maximize accuracy, a trained researcher with more than five years of professional clinical experience, who was blinded to the group allocation, performed all the tests.
Study endpoints
The primary endpoints were the assessments of alerting, orienting, and executive control functions as determined by the ANT. The secondary endpoint was the incidence of delirium during the first five days after surgery, as determined by the CAM.
Sample size calculation
To calculate the sample size needed to assess the agreement between attention network functions and cognition, t-test statistical analysis was undertaken using G*Power 3.1.9.3 statistical power analysis program. The sample size was increased by 20% to account for potential technical difficulties. Based on this analysis, the aim was to recruit at least 45 patients per study group.
Statistical analysis
All statistical analysis was performed using SPSS version 19 software (IBM Corp., Armonk, NY, USA). Quantitative data were tested for normality. Data were presented as the mean ± standard deviation (SD). Comparisons between the BIS and non-BIS groups were made using the independent samples t-test, Fisher’s exact test, or the Mann–Whitney U test, as appropriate. Repeated measures analysis of variance (ANOVA) and the Bonferroni post hoc test were used to analyze the following variables: overall RT, accuracy, and the absolute and proportional scores for the alerting, orienting, and executive control functions. Comparisons of categorical variables were made using the chi-squared (χ2) test or Fisher’s exact test, as appropriate. Univariate ANOVA was used for analysis of the doses of propofol and remifentanil. The correlations between parameters were assessed using Spearman’s correlation coefficient. P<0.05 was considered to be statistically significant.
Results
Participant characteristics and study groups
The study flowchart is shown in Figure 2. Initially, 44 elderly patients were randomized to the bispectral index (BIS) monitoring group (BIS group). However, one patient declined the Attention Network Test (ANT) following surgery, and two patients had a visual analog scale (VAS) score >3 points, resulting in exclusion of three patients and a total number of patients in the BIS group of 41.
Figure 2.
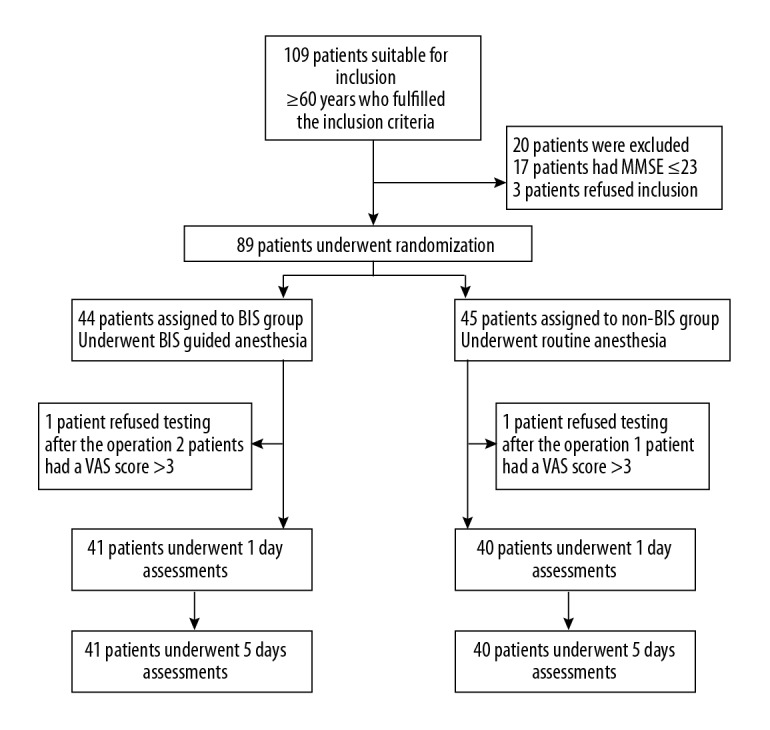
Flowchart of the study design. BIS – bispectral index; MMSE – mini-mental state examination; ANT – Attention Network Test; CAM – Confusion Assessment Method.
Initially, 45 elderly patients were randomized to the non-BIS group. However, five patients were excluded were excluded, as four patients declined the ANT and one patient had a VAS score >3 points, resulting in a total number of patients in the non-BIS group of 40.
The demographic and clinical characteristics of the patients included in the analysis are presented in Table 1. There were no significant differences between the two groups in age, Mini-Mental State Examination (MMSE) score, level of education, duration of anesthesia or duration of surgery (Table 1). Hypotension during anesthesia necessitating the intravenous administration of ephedrine occurred in three patients in the BIS group and five patients in the non-BIS group. No patients required a blood transfusion during surgery.
Table 1.
Demographic and clinical characteristics of the patients in the two groups.
| Characteristic | BIS group (n=41) | Non-BIS group (n=40) | P value |
|---|---|---|---|
| Male sex | 29 (70.7%) | 27 (67.5%) | |
| Age (years) | 68.29±2.81 | 68.90±2.99 | 0.350 |
| Body mass index (kg/m2) | 21.07±1.33 | 21.27±1.09 | 0.476 |
| Comorbidities | |||
| Diabetes | 3 (7.3%) | 4 (10.0%) | 0.757 |
| Hypertension | 7 (17.1%) | 5 (12.5%) | 0.520 |
| Education (years) | 11.46±3.00 | 11.55±3.14 | 0.899 |
| MMSE score | 29.18±0.87 | 28.97±0.89 | 0.318 |
| Anesthetic time (min) | 185.51±14.69 | 184.53±13.81 | 0.756 |
| Operation time (min) | 155.44±14.72 | 154.53±13.81 | 0.774 |
| Blood transfusion (mL) | 0 | 0 | |
| Preoperative ANT results | |||
| Alerting effect (ms) | 28.05±17.52 | 29.50±14.17 | 0.684 |
| Orienting effect (ms) | 34.68±18.77 | 35.65±18.31 | 0.815 |
| Conflict effect (ms) | 150.00±38.98 | 147.10±36.01 | 0.729 |
| Accuracy (%) | 94.27±3.73 | 93.73±3.76 | 0.517 |
| Response time (ms) | 992.98±141.07 | 985.93±140.04 | 0.822 |
| Preoperative delirium | 0 (0.0%) | 0 (0.0%) | |
Data are presented as n (%) or mean ± standard deviation. ANT – attention network test; MMSE – mini-mental state examination.
Total doses of anesthetic and analgesic drugs administered
The total doses of propofol and remifentanil administered during general anesthesia were significantly lower in the BIS group compared with the non-BIS group (P<0.001) (Table 2). However, there were no significant differences between the two groups for the total doses of flurbiprofen or sufentanil given for postoperative analgesia (Table 2).
Table 2.
Total doses of anesthetic medications received by the patients in the two groups.
| Total dose of medication administered | BIS group (n=41) | Non-BIS group (n=40) | P value |
|---|---|---|---|
| General anesthesia | |||
| Propofol (mg) | <0.001 | ||
| Remifentanil (mg) | 811.10±79.45 | 1075±96.75 | <0.001 |
| Postoperative analgesia | 1.57±0.16 | 1.88±0.20 | |
| Flurbiprofen (mg) | 100.00 | 100.00 | NA |
| Sufentanil (μg) | 131.71±24.38 | 137.50±21.93 | 0.265 |
Data are presented as the mean ± standard deviation.
Attention network function
There were no significant differences between the two groups in pre-operative attention network efficiencies. Both the BIS group and non-BIS group exhibited significant impairment in alerting, orienting, and executive control at postoperative day 1, when compared with the corresponding pre-operative values (all P<0.001) (Figures 3, 4). However, at postoperative day 5, the BIS group showed significant recovery in alerting (P=0.608), and orienting (P=0.851) functions, which returned to pre-operative levels (Figure 3). However, alerting (P<0.001) and orienting (P=0.01) functions remained significantly impaired in the non-BIS group (Figure 4). Both groups showed no recovery of executive control function at postoperative day 5 (Figures 3, 4). Direct comparisons showed that the non-BIS group had significantly lower values for alerting effect (P<0.001) and orienting effect (P=0.031) compared with the BIS group at postoperative day 5 (Table 3). These data indicate that BIS monitoring during general anesthesia can alleviate postoperative attention network impairment.
Figure 3.
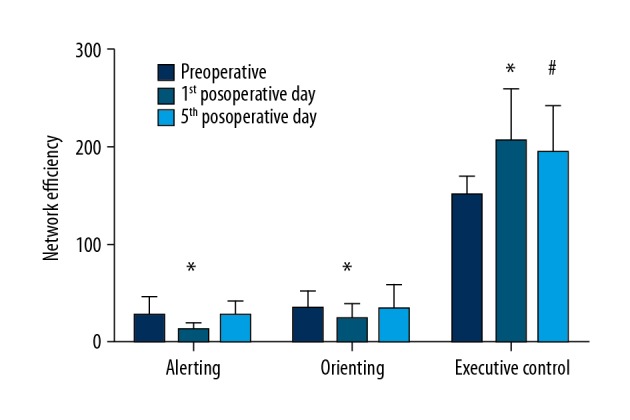
Efficiency of the attention networks in the bispectral index (BIS) monitored group (BIS group). Attention network (alerting, orienting, and executive control) functions in the bispectral index (BIS) group were assessed pre-operatively and at day 1 and day 5 postoperatively. * P<0.05 vs. corresponding pre-operative value; # P<0.05 vs. corresponding pre-operative value.
Figure 4.
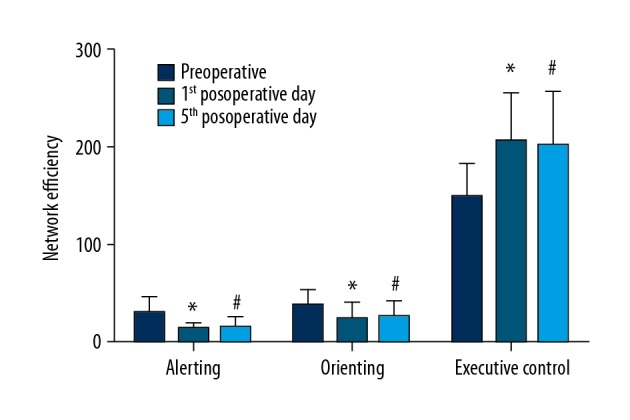
Efficiency of the attention networks in the group not monitored using the bispectral index (BIS) (non-BIS group). Attention network (alerting, orienting, and executive control) functions in the non-bispectral index (BIS) group were assessed pre-operatively and at day 1 and day 5 postoperatively. * P<0.05 vs. corresponding pre-operative value; # P<0.05 vs. corresponding pre-operative value.
Table 3.
Attention network test efficiencies for patients in the two groups.
| Factor | BIS group (n=41) | Non-BIS group (n=40) | P value |
|---|---|---|---|
| Alerting effect (ms) | |||
| Postoperative day 1 | 13.44±7.52 | 12.60±7.89 | 0.626 |
| Postoperative day 5 | 26.12±16.20 | 13.95±9.60 | <0.001 |
| Orienting effect (ms) | |||
| Postoperative day 1 | 23.15±16.56 | 22.63±18.37 | 0.894 |
| Postoperative day 5 | 33.90±18.60 | 25.28±16.60 | 0.031 |
| Conflict effect (ms) | |||
| Postoperative day 1 | 206.07±53.28 | 206.53±47.70 | 0.968 |
| Postoperative day 5 | 193.93±48.14 | 201.00±55.87 | 0.543 |
| Accuracy (%) | |||
| Postoperative day 1 | 91.88±3.47 | 91.45±2.21 | 0.512 |
| Postoperative day 5 | 92.63±3.11 | 90.45±9.41 | 0.163 |
| Response time (ms) | |||
| Postoperative day 1 | 1248.56±131.86 | 1220.65±213.56 | 0.480 |
| Postoperative day 5 | 1026.71±147.10 | 1003.38±208.60 | 0.562 |
Data are presented as the mean ± standard deviation.
Correlation between the total dose of propofol administered during anesthesia and attention network functions
Patient age was significantly correlated with pre-operative alerting function in the BIS group (r=0.72, P<0.001) and non-BIS group (r=0.76, P<0.001). The total dose of propofol administered during general anesthesia was significantly correlated with alerting at postoperative day 1 (r=0.78, P<0.001) and at postoperative day 5 (r=0.84, P<0.001), orienting at postoperative day 1 (r=0.76, P<0.001) and at postoperative day 5 (r=0.80, P<0.001), and executive control at postoperative day 1 (r=0.74, P<0.001) and at postoperative day 5 (r=0.82, P<0.001). These findings indicated that propofol may impair attention network functions.
Bispectral index (BIS) monitoring values
The BIS monitoring values in the BIS group (51.10±0.83) were significantly higher compared with the patients who were not monitored with BIS during surgery (41.44±0.0.78) (P<0.001).
Acute postoperative delirium
The incidence of delirium during the first five days after surgery was significantly lower in the BIS group at 17% (7/41) compared with the non-BIS group at 27.5% (11/40) (P<0.001).
Discussion
To our knowledge, this study is the first to examine attention network changes in patients after propofol anesthesia using the Attention Network Test (ANT) to study alerting, orienting, and executive functions. The study aimed to evaluate the effects of bispectral index (BIS) monitoring during surgery for resection of colon carcinoma in elderly patients and to compare the findings with a non-BIS monitored group. Also, the Confusion Assessment Method (CAM) was used to evaluate the effects of BIS on delirium during the first five postoperative days in this patient group. The results showed that while patients in both study groups developed attention network function impairment after surgery, those in the BIS group showed recovery of alerting and orienting network functions by postoperative day 5, whereas patients in the non-BIS group showed no such recovery. Neither group showed recovery of executive network efficiency within the first five postoperative days. Also, the total doses of propofol and remifentanil administered during surgery were significantly lower in the BIS group compared with the non-BIS group, and the incidence of postoperative delirium was significantly lower in the BIS group compared with the non-BIS group. These results showed that BIS-guided anesthesia can decrease anesthetic exposure, promote early postoperative recovery of attention network functions, and reduce the incidence of postoperative delirium in elderly patients undergoing surgery for colon carcinoma.
The optimal BIS level during surgery has been reported to be between 40–50 [16,19]. A finding of the present study was that the total doses of propofol and remifentanil administered during surgery were significantly lower in the BIS group compared with the non-BIS group. This finding is supported by previously published studies that have shown that BIS monitoring during surgery reduces the levels of general anesthetics administered [14,15,17,28], resulting in advantages that include shorter times to extubation, improved orientation in time and place, and earlier discharge from the operating room or post-anesthetic care unit, as well as a lower risk of postoperative nausea and vomiting, resulting in reduced health costs [15,18].
Age, anesthesia, and surgery are risk factors for postoperative cognitive dysfunction (POCD) [6]. In the present study, BIS monitoring was shown to significantly alleviate postoperative attention network impairment in elderly patients. Previous studies have shown that BIS monitoring can reduce postoperative cognitive impairment. Chan et al. reported that patients with BIS monitoring during anesthesia had a lower rate of POCD at three months following surgery (10.2%) when compared with patients without BIS monitoring during anesthesia (14.7%) [17]. A meta-analysis of clinical studies also concluded that BIS monitoring reduced the incidence of POCD at three months after surgery [18].
The finding from the present study, that age was strongly correlated with alerting, is supported by the findings from a previously published study [5]. Therefore, elderly patients may be at particular risk of postoperative impairment of alerting function. In the current study, the alerting, orienting, and executive attention functions were significantly impaired in both groups of patients (the BIS group and the non-BIS group) at postoperative day 1 compared with the pre-operative values. At postoperative day 5, the alerting and orienting functions had recovered in the BIS group but not in the non-BIS group. The findings from the present study, that BIS monitoring reduced propofol dose and postoperative cognitive impairment, is supported by the findings from previous studies [15,20].
The mechanisms by which general anesthetics affect alerting, orienting, and executive attention functions and cause POCD remain unknown. It is possible that POCD may involve hippocampal and extra-hippocampal dysfunction [29], and may be due to effects on changes in the levels of neurotransmitters, including norepinephrine, acetylcholine, and dopamine [24,30–33]. Since attention network functions have different anatomical locations and neurochemical mechanisms, it is possible to propose that propofol anesthesia may have more substantial effects on the frontal lobe, parts of the parietal lobe, and the temporoparietal regions of the brain that are associated with executive control and orienting network functions.
In the present study, the incidence of delirium during the first five days after surgery was much lower in the BIS group compared with the non-BIS group, which is a finding supported by previously published studies [16–18]. These findings further support the potential benefits of BIS monitoring in elderly patients undergoing general anesthesia for major surgery.
This study had several limitations. The levels of biomarkers in the blood and cerebrospinal fluid (CSF) that might be related to cognitive changes were not measured. Also, patients may not be willing to undergo the ANT in the immediate postoperative period or may provide responses that are affected by cognitive changes. The study sample size in the two study groups was relatively small and further studies are required to confirm and extend the study findings. The follow-up period in this study was short, at only five days, and so the association of the ANT results and the long-term occurrence of POCD and delirium require further study. The CAM evaluation was administered in the morning to avoid disturbing the patients during their recovery, as most patients were resting or sleeping during the evening and at night, but delirium typically manifests during the evening or night. Also, data regarding postoperative opioid use in patient-controlled analgesia at the time of ANT was not recorded. Because opioid use can affect cognitive function, there is the possibility that that differences in postoperative opioid use at the time of the ANT contributed to the observed differences between the study groups.
Conclusions
In elderly patients undergoing radical surgical resection of colon carcinoma, bispectral index (BIS) monitoring during anesthesia, assessed using the Attention Network Test (ANT) to study alerting, orienting, and executive functions, was associated with reduced intravenous propofol anesthetic exposure, early postoperative recovery of alerting and orienting functions by postoperative day 5. In this patient group, the findings from the Confusion Assessment Method (CAM) showed that BIS monitoring during anesthesia reduced postoperative delirium. The findings of this study support the use of BIS monitoring to guide the administration of general anesthesia in elderly patients.
Acknowledgments
This study was partly supported by our colleagues from the Department of Gastrointestinal Surgery of The First Affiliated Hospital of Wannan Medical College; we thank them for their contributions.
Footnotes
Source of support: Departmental sources
References
- 1.Müller-Oehring EM, Schulte T, Rohlfing T, et al. Visual search and the aging brain: Discerning the effects of age-related brain volume shrinkage on alertness, feature binding, and attentional control. Neuropsychology. 2013;27:48–59. doi: 10.1037/a0030921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Monk TG, Weldon BC, Garvan CW, et al. Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiol. 2008;108:18–30. doi: 10.1097/01.anes.0000296071.19434.1e. [DOI] [PubMed] [Google Scholar]
- 3.Krenk L, Rasmussen LS. Postoperative delirium and postoperative cognitive dysfunction in the elderly – what are the differences? Minerva Anesthesiol. 2011;77:742–49. [PubMed] [Google Scholar]
- 4.Hussain M, Berger M, Eckenhoff RG, Seitz DP. General anesthetic and the risk of dementia in elderly patients: Current insights. Clin Interv Aging. 2014;9:1619–28. doi: 10.2147/CIA.S49680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abildstrom H, Rasmussen LS, Rentowl P, et al. Cognitive dysfunction 1–2 years after non-cardiac surgery in the elderly. ISPOCD group. International Study of Post-Operative Cognitive Dysfunction. Acta Anaesthesiol Scand. 2000;44:1246–51. doi: 10.1034/j.1399-6576.2000.441010.x. [DOI] [PubMed] [Google Scholar]
- 6.Kotekar N, Kuruvilla CS, Murthy V. Postoperative cognitive dysfunction in the elderly: A prospective clinical study. Indian J Anaesth. 2014;58:263–68. doi: 10.4103/0019-5049.135034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Newman MF, Grocott HP, Mathew JP, et al. Neurologic Outcome Research Group and the Cardiothoracic Anesthesia Research Endeavors (CARE) Investigators of the Duke Heart Center: Report of the substudy assessing the impact of neurocognitive function on quality of life 5 years after cardiac surgery. Stroke. 2001;32:2874–81. doi: 10.1161/hs1201.099803. [DOI] [PubMed] [Google Scholar]
- 8.Phillips-Bute B, Mathew JP, Blumenthal JA, et al. Association of neurocognitive function and quality of life 1-year after coronary artery bypass graft (CABG) surgery. Psychosom Med. 2006;68:369–75. doi: 10.1097/01.psy.0000221272.77984.e2. [DOI] [PubMed] [Google Scholar]
- 9.Ferro JM, Madureira S. Age-related white matter changes and cognitive impairment. J Neurol Sci. 2002;203–4:221–25. doi: 10.1016/s0022-510x(02)00295-2. [DOI] [PubMed] [Google Scholar]
- 10.Sato C, Sekiguchi A, Kawai M, et al. Postoperative structural brain changes and cognitive dysfunction in patients with breast cancer. PLoS One. 2015;10:e0140655. doi: 10.1371/journal.pone.0140655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Federico F, Marotta A, Adriani T, et al. Attention network test – the impact of social information on executive control, alerting and orienting. Acta Psychol (Amst) 2013;143(1):65–70. doi: 10.1016/j.actpsy.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 12.Spagna A, Martella D, Sebastiani M, et al. Efficiency and interactions of alerting, orienting and executive networks: The impact of the imperative stimulus type. Acta Psychol (Amst) 2014;148:209–15. doi: 10.1016/j.actpsy.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 13.Posner MI, Petersen SE. The attention system of the human brain. Annu Rev Neurosci. 1990;13:25–42. doi: 10.1146/annurev.ne.13.030190.000325. [DOI] [PubMed] [Google Scholar]
- 14.Park SW, Lee H, Ahn H. Bispectral index versus standard monitoring in sedation for endoscopic procedures: A systematic review and meta-analysis. Dig Dis Sci. 2016;61:814–24. doi: 10.1007/s10620-015-3945-9. [DOI] [PubMed] [Google Scholar]
- 15.Ibraheim O, Alshaer A, Mazen K, et al. Effect of bispectral index (BIS) monitoring on postoperative recovery and sevoflurane consumption among morbidly obese patients undergoing laparoscopic gastric banding. Middle East J Anaesthesiol. 2008;19:819–30. [PubMed] [Google Scholar]
- 16.Shu AH, Wang Q, Chen XB. Effect of different depths of anesthesia on postoperative cognitive function in laparoscopic patients: A randomized clinical trial. Curr Med Res Opin. 2015;31:1883–87. doi: 10.1185/03007995.2015.1075968. [DOI] [PubMed] [Google Scholar]
- 17.Chan MT, Cheng BC, Lee TM, Gin T. BIS-guided anesthesia decreases postoperative delirium and cognitive decline. J Neurosurg Anesthesiol. 2013;25:33–42. doi: 10.1097/ANA.0b013e3182712fba. [DOI] [PubMed] [Google Scholar]
- 18.Oliveira CR, Bernardo WM, Nunes VM. Benefit of general anesthesia monitored by bispectral index compared with monitoring guided only by clinical parameters. Systematic review and meta-analysis. Braz J Anesthesiol. 2017;67:72–84. doi: 10.1016/j.bjane.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 19.Jung YS, Han YR, Choi ES, et al. The optimal anesthetic depth for interventional neuroradiology: Comparisons between light anesthesia and deep anesthesia. Korean J Anesthesiol. 2015;68:148–52. doi: 10.4097/kjae.2015.68.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Farag E, Chelune GJ, Schubert A, Mascha EJ. Is depth of anesthesia, as assessed by the bispectral index, related to postoperative cognitive dysfunction and recovery? Anesth Analg. 2006;103:633–40. doi: 10.1213/01.ane.0000228870.48028.b5. [DOI] [PubMed] [Google Scholar]
- 21.Wu Y, Shi Z, Wang M, et al. Different MMSE score is associated with postoperative delirium in young-old and old-old adults. PLoS One. 2015;10:e0139879. doi: 10.1371/journal.pone.0139879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mudgalkar N, Bele SD, Valsangkar S, et al. Utility of numerical and visual analog scales for evaluating the post-operative pain in rural patients. Indian J Anaesth. 2012;56:553–57. doi: 10.4103/0019-5049.104573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu G, Ma HJ, Hu PP, et al. Effects of painful stimulation and acupuncture on attention networks in healthy subjects. Behav Brain Funct. 2013;9:23. doi: 10.1186/1744-9081-9-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fan J, Fossella J, Sommer T, et al. Mapping the genetic variation of executive attention on brain activity. Proc Natl Acad Sci USA. 2003;100:7406–11. doi: 10.1073/pnas.0732088100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fan J, McCandliss BD, Fossella J, et al. The activation of attentional networks. Neuroimage. 2005;26:471–79. doi: 10.1016/j.neuroimage.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 26.Wei LA, Fearing MA, Sternberg EJ, Inouye SK. The Confusion Assessment Method: A systematic review of current usage. J Am Geriatr Soc. 2008;56:823–30. doi: 10.1111/j.1532-5415.2008.01674.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: The confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–48. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 28.Cao YH, Chi P, Zhao YX, Dong XC. Effect of bispectral index-guided anesthesia on consumption of anesthetics and early postoperative cognitive dysfunction after liver transplantation: An observational study. Medicine (Baltimore) 2017;96:e7966. doi: 10.1097/MD.0000000000007966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cascella M, Bimonte S. The role of general anesthetics and the mechanisms of hippocampal and extra-hippocampal dysfunctions in the genesis of postoperative cognitive dysfunction. Neural Regen Res. 2017;12:1780–85. doi: 10.4103/1673-5374.219032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ogura M, Sakamoto H, Morita S. Microinjection of propofol into the perifornical area induces sedation with decreasing cortical acetylcholine release in rats. Anesth Analg. 2010;111:395–402. doi: 10.1213/ANE.0b013e3181e24776. [DOI] [PubMed] [Google Scholar]
- 31.Gamou S, Fukuda SLaalou FZ, et al. Involvement of the basal cholinergic forebrain in the mediation of general (propofol) anesthesia. Anesthesiology. 2008;108:888–96. doi: 10.1097/ALN.0b013e31816d919b. [DOI] [PubMed] [Google Scholar]
- 32.Pashkov VN, Hemmings HC., Jr The effects of general anesthetics on norepinephrine release from isolated rat cortical nerve terminals. Anesth Analg. 2002;95(5):1274–81. doi: 10.1097/00000539-200211000-00032. [DOI] [PubMed] [Google Scholar]
- 33.Wang Y, Yu T, Yuan C, et al. Effects of propofol on the dopamine, metabolites and GABAA receptors in the medial prefrontal cortex in freely moving rats. Am J Transl Res. 2016;8:2301–8. [PMC free article] [PubMed] [Google Scholar]