Abstract
Objective
To describe the routine use of telemedicine-enabled neurologic care in an academic outpatient MS and neuroimmunology clinic and quantify its role in reducing patient burden.
Methods
Between January 2017 and December 2017, we surveyed patients and MS neurologists after 50 consecutive routinely scheduled televideo visits and a convenience sample of 100 in-clinic visits. Summary statistics were calculated and comparisons performed.
Results
Overall, 98% televideo participants found the technology easy to use, and only 17% believed that an in-person examination would have more effectively addressed their needs for the visit. MS neurologists reported achieving their clinical goals in 47/48 (98%) of televideo visits and an adequate physical examination with 2 exceptions (possible cauda equina syndrome and visual field loss). Three emergency department referrals were avoided due to televideo availability. Telemedicine reduced travel burden, including a mean (±SD) travel distance of 160 (±196) miles and avoiding overnight lodging and air travel. Telemedicine also reduced indirect costs, including time off work (65% of employed patients) and caregiver burden (30% avoided caregiver time off from work/obligations). Across 8 domains of provider interpersonal communication skills, telemedicine and in-clinic participants rated only 1 domain to be different (eye contact), and overall, 96% of in-clinic and 100% of telemedicine participants agreed/strongly agreed that their clinical goals had been met.
Conclusions
When incorporated as part of the continuum of MS/neuroimmunology care, clinic to in-home telemedicine reduces travel and caregiver burden and enables efficient, convenient, and effective follow-up.
For people living with a chronic neuroinflammatory disease such as MS, medical appointments can represent one of many “hassles of daily life”1 and have hidden financial and opportunity costs. Various models of telemedicine have been trialed to improve MS care, especially in the realm of rehabilitation,2 symptom management,3 and care coordination.4 In the US, hospital-to-hospital telemedicine models using a trained provider with the patient at the bedside have matured into an important part of the care model for acute stroke5 and some other Veterans Affairs telemedicine solutions.6,7 There is emerging interest in using at-home telemedicine visits to augment or possibly replace in-person clinic visits for management of other chronic neurologic conditions, such as Parkinson disease.8 Telemedicine is part of a larger movement in medicine to promote patient-centered care by developing viable alternatives to traditional in-clinic appointments while preserving the fundamental patient-doctor connection.9
The application of in-home telemedicine as part of routine clinical care of the patient with MS and other neuroinflammatory conditions remains under-explored.10 For the past 4 years, the UCSF MS and Neuroinflammation Center has routinely provided clinic to in-home televideo appointments for established patients. Here, we report on this experience and determine whether the routine use of telemedicine-enabled neurologic care reduces patient and provider burden.
Methods
Setting and participants
We invited UCSF MS and Neuroinflammation Center clinic patients scheduled for clinic to in-home telemedicine visits with each of 5 participating MS neurologists to complete an electronic survey about their visit. Neurologic visits occurred via telemedicine for patients living in California using a secure, web-based teleconferencing platform (zoom.us). Participants were adults (aged ≥18 years) and carried a range of neurologic diagnoses, including MS, neuromyelitis optica spectrum disorder, and other neuroinflammatory disorders (e.g., autoimmune encephalitis and neurosarcoidosis). Participating neurologists were all MS/neuroimmunology experts and at study onset had variable experience with telemedicine in their clinical practice (range 10–100 estimated previous visits, representing between <5% and 40% of a clinician's total weekly scheduled clinical encounters). Patients were consecutively contacted for participation by email by the study coordinator after the telemedicine visit until 50 had completed the surveys (December 2017).
As a reference group, we also invited in-clinic patients seen by these same providers to complete a survey. On clinical days selected based on the research coordinator's availability, all patients seen by these providers were consecutively approached by the coordinator, until 100 had completed the surveys (September 2017).
Data
Surveys were administered on the same day as the clinical visits via a secure, web-based research application (project-redcap.org), with paper surveys as an option if the patients preferred. A follow-up reminder was emailed to participants who had not responded within 1 week of the visit. If surveys were not completed within this time frame, participants were considered nonrespondents. Demographic and clinical details were obtained via medical record review, including clinical diagnosis and, for patients with MS, a neurologist-scored expanded disability status scale (EDSS) within the past year (details of a telemedicine-assessed EDSS are reported elsewhere11). To compare responses between in-clinic and telemedicine-based visits, t tests and χ2 analyses were performed. Data were analyzed using SAS software program JMP, version 13 (Cary, NC).
Standard protocol approvals, registrations, and patient consents
The UCSF Committee of Human Research approved the study protocol (15–18,362), and all participants provided written informed consent completed electronically.
Data availability
An anonymized data set including data not published within the article will be shared on request from any qualified investigator.
Results
Demographic, clinical, and visit characteristics
The overall response rate was 61% (from 246 participants approached; no differences in age or sex between respondents and nonrespondents). The 50 participants seen in televideo were more likely than the 100 participants seen in the clinic to have completed college; there was also a trend for the televideo participants to be older, more often male, less likely to use televideo daily, and more likely than the patients seen in the clinic to have MS, whose diagnoses were more varied. Median EDSS for participants with clinically isolated syndrome (CIS)/MS in both groups was 3 (table 1). All study participants reported access to the internet in a convenient location (such as home). Telemedicine visits were shorter (mean [SD] minutes 29.7 [12.7] vs 53.7 [17.4], p < 0.0001]) and more often focused on specific topics (e.g., symptom management, results review, education, and counseling, p < 0.0001) than in-clinic visits; this was true when we compared telemedicine visits with in-clinic follow-up visits only (N = 68).
Table 1.
Demographic, clinical, and visit characteristics across 100 in-clinic and 50 telemedicine-based visits
Features and outcomes of televideo visits
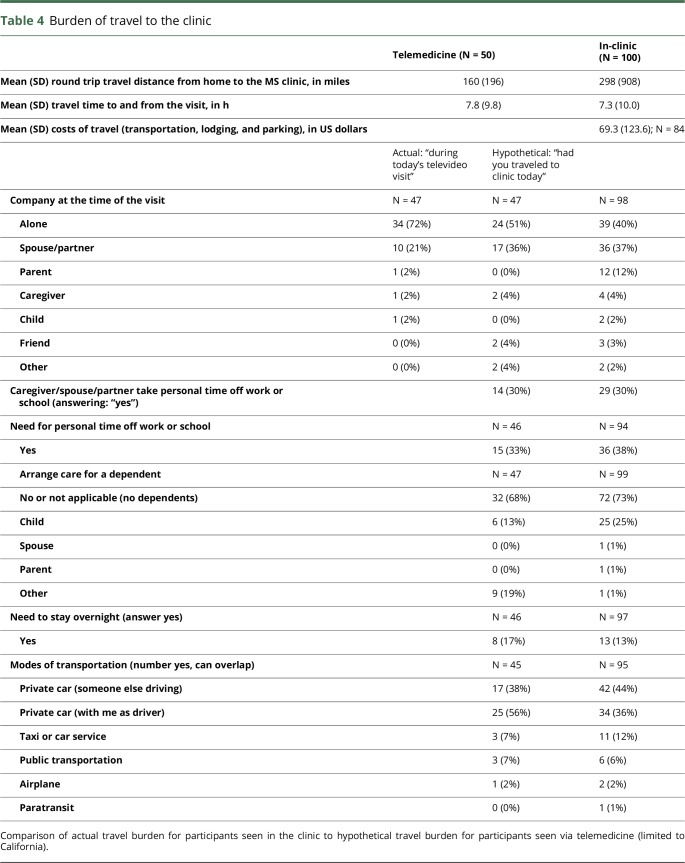
Televideo visits are usually scheduled for routine follow-ups after an annual in-clinic visit, at sooner time frames for ongoing symptomatic management, and more urgently for new symptoms or to review significant results. Patients mostly conducted televideo visits in their homes (79%) and at work (19%). They used laptops (51%), smartphones (33%), desktops (10%), and tablets (6%), which in all cases they currently owned or had access to. In 27% of the cases, a companion (typically their spouse or partner) was present with the patient. Occasionally, a partner or family member joined the televideo visit from a third location. During the encounters, the clinicians followed the usual clinical encounter format, initially eliciting the patients' objectives for the visit, then guiding the patient through subjective reporting and a review of symptoms. For the neurologic examination, instructions for positioning the patient are described elsewhere.11 As many of the visits were focused on symptomatic management, results review, and pregnancy counseling, a full neurologic examination was not always required and was often limited to the relevant functional systems. Physicians reported an adequate physical examination for the purposes of the clinical encounter, in 48 (96%) visits (table 2). In the 2 exceptions when the televideo examination did not provide sufficient sensitivity (concern for cauda equina syndrome and visual field loss), a timely follow-up in-clinic evaluation was recommended. To review results, televideo software allows sharing of screens so that the clinician could display and highlight salient features of MRIs or laboratory results. Physicians reported that televideo visits avoided 3 patients being sent to the emergency department. Overall, physicians reported achieving their clinical goals in 49 (98%) of the televideo visits.
Table 2.
Provider satisfaction with telemedicine visits
Patient satisfaction
Patients reported high satisfaction with their telemedicine care: 98% reported that the televideo technology was easy to use, and only 17% reported that an in-person examination would have been more effective in addressing their visit goals (72% “no,” 11% “I am not sure”). When comparing patient satisfaction across in-clinic and telemedicine visits, satisfaction was globally high, with only minor differences noted (table 3). There was no association between a clinician's number of previous televideo visits and patient satisfaction with the visit. Across 8 domains of provider interpersonal communication skills, only 1 domain was significantly different (maintaining eye contact: 100% vs 96% visits where provider was rated as extremely/moderately good), but for the other 7 domains, satisfaction with in-clinic and telemedicine-based care was similar. Overall, 96% of in-clinic and 100% of telemedicine participants agreed/strongly agreed that their clinical goals had been met.
Table 3.
Patient satisfaction with telemedicine and in-clinic visits
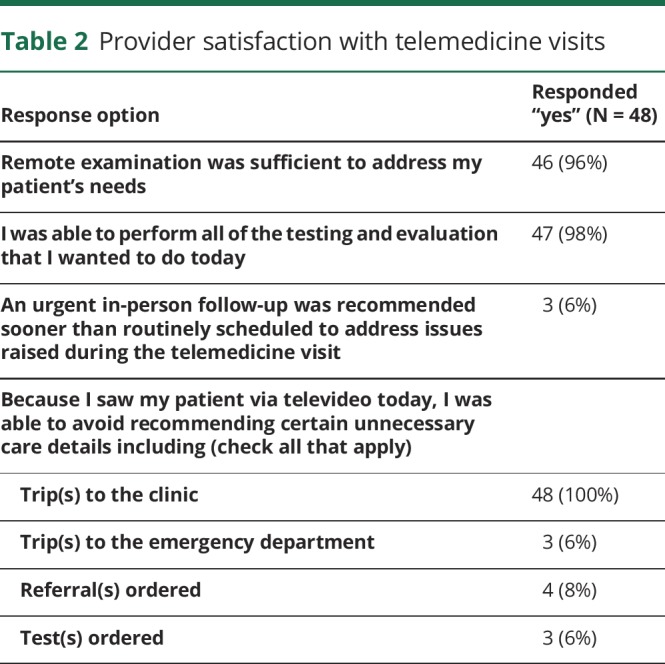
Travel burden
Telemedicine visits offered a distinct advantage in reducing travel burden to the clinic (table 4). The in-clinic participants spent a mean (SD) of 7.3 (10) hours traveling from within and beyond California, with travel costs averaging 69.3 US dollars (SD 123.6, range 0–600), and mean roundtrip travel distance of 298 (SD 908) miles [480 km (SD 1,462)]. The patients seen via televideo, which was restricted to California residents only, reported avoiding an average travel distance of 160 (SD 196) miles [258 km (SD 316)]; 17% avoided overnight lodging, and 1 avoided airfare. Caregiver burden was also reduced: 30% avoided caregiver time off from work, and 13% avoided arranging care for a dependent. Of the 46% of the patients who were employed, 65% avoided taking a day off from work.
Table 4.
Burden of travel to the clinic
Discussion
In this survey study, analyzing experience with clinic to in-home telemedicine in our academic MS and neuroimmunology clinic, travel and caregiver burden were reduced with the convenience of televideo-enabled visits while preserving efficient and effective care in the opinion of both patients and clinicians. These results support the integration of clinic to in-home telemedicine within the continuum of MS/neuroimmunology specialty care.
Overall, patient satisfaction with the neurologic encounter and perception of provider interpersonal skills were similar between telemedicine and in-clinic visits, with the overwhelming number of patients rating all components highly. These results are encouraging, given that many participants did not have considerable previous experience with technology and indicate that being technologically savvy is not necessarily needed to benefit from telemedicine-enabled care.
Patients also reported that substantial time and money were saved for themselves and their families and dependents. In a study of delivery of cognitive evaluations remotely for people with MS, it was estimated that $144 in travel costs and lost wages were saved relative to in-clinic evaluations.12 Further studies are needed to expand on these cost analyses by more comprehensively quantifying the opportunity costs of in-clinic visits, such as “sick days” from work and childcare for children, as well as differences between in-clinic– and telemedicine-related billed health care costs or cost savings.
As might be expected, there were select clinical questions for which timely in-person visits were requested after the telemedicine encounter. There are also components of the neurologic examination that are less reliable or unable to be performed adequately using televideo6,7,11 without a trained provider at the bedside (e.g., deep tendon reflexes) or specialized hardware (e.g., nonmydriatic fundus cameras). As a contingency, in our practice, providers and/or patients could and did request rapid in-person follow-up evaluation if outstanding questions remained after the televideo evaluation. Our results also demonstrate slight qualitative differences in patient assessment of the patient-doctor relationship between in-clinic and televideo clinical visits, particularly lower “eye contact” scores for televideo visits. Response bias could belie differences in patient satisfaction, although there were no clear differences in demographic characteristics between respondents and nonrespondents.
Given the generally high rates of patient satisfaction with the current encounters, it was not possible to probe whether specific aspects of MS-related disability affected the relative benefits and costs of televideo visits. For example, the televideo visit might slightly decrease the sensitivity of the examination to disease progression for a patient with severe ambulatory or cognitive impairment, but provide substantial convenience for a spouse experiencing a large caregiving burden, allowing them to maintain other competing needs (employment, home care, and self-care). For a patient with minimal functional impairment and intact cognition, the televideo visit might allow them to maintain high work productivity, but could limit the examiner's ability to detect subtle changes in vibratory function or muscle tone suggestive of disease progression. Therefore, the determination of the ideal scheduling and ratio of in-clinic to televideo visits will likely continue to be individualized.
More research will be needed to evaluate effects of clinic to in-home telemedicine on health care quality, outcomes, and cost metrics and to study a range of other potential telemedicine applications such as with interprofessional providers and to focus on symptom management and rehabilitation. It will be critical for insurers and policy makers to recognize the inherent value of telemedicine and develop more uniform approaches to reimbursement for telemedicine visits as part of the continuum of subspecialty outpatient care. As the field of neurologic telemedicine matures, it will also be important to develop best practices and to integrate telemedicine teaching into 21st century medical education. Our study supports the expansion of clinic to in-home telemedicine solutions for longitudinal outpatient care for neuroimmunologic conditions.
Glossary
- EDSS
expanded disability status scale
Author contributions
Study concept and design: R. Bove and J.M. Gelfand; Statistical analysis and interpretation of data: R. Bove; Acquisition of data and interpretation of results: P. Garcha, C.J. Bevan, E. Crabtree, R. Bove, and J.M. Gelfand; Manuscript drafting and revision: all authors.
Study funding
This research was supported by the National MS Society Career Transition Award (RB).
Disclosure
R. Bove served on the scientific advisory board of Roche-Genentech, Sanofi Genzyme, and Novartis; has a patent pending for selective estrogen receptor modulators and remyelination; and received research support from Akili Interactive, California initiative to advance precision medicine, the National MS Society, the Hilton Foundation, and the Sherak Foundation. P. Garcha reports no disclosures. C.J. Bevan reports no disclosures. E. Crabtree-Hartman received speaker honoraria from Biogen and Sanofi Genzyme;, consulted for Teva, Novartis, and Biogen; and served on the speaker's bureau for Teva and Biogen. A. Green served on the scientific advisory board of MedImmune, Novartis, Inception 5 Sciences, Pipeline, and Bionure; served on the editorial board of JAMA Neurology; served as an associate editor for Neurology; holds a patent for remyelination molecules and pathways; consulted for Inception 5 Sciences; received research support from Novartis, Inception Sciences SRA, NINDS, NIA, NIH, the National MS Society, the Sherak Foundation, and the Hilton Foundation; holds stock or stock options in Inception 5 Sciences, Pipeline, and Bionure; and served as an expert witness for Mylan Pharmaceuticals v Teva Pharmaceuticals. J. Gelfand is on the editorial board of Neurology: Neuroimmunology & Neuroinflammation; consulted for Biogen; received research support to UCSF from Genentech, MedDay, and Quest Diagnostics; received research support from the National MS Society; and received compensation for medical-legal consulting. Dr. Gelfand's spouse is an associate editor for JAMA Neurology; has received honoraria from UpToDate; and received consulting fees from Zosano, Eli Lilly, Biohaven, and eNeura. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/NN.
References
- 1.van der Hiele K, Spliethoff-Kamminga NG, Ruimschotel RP, Middelkoop HA, Visser LH. Daily hassles reported by Dutch multiple sclerosis patients. J Neurol Sci 2012;320:85–90. [DOI] [PubMed] [Google Scholar]
- 2.Khan F, Amatya B, Kesselring J, Galea MP. Telerehabilitation for persons with multiple sclerosis: a Cochrane review. Eur J Phys Rehabil Med 2015;51:311–325. [PubMed] [Google Scholar]
- 3.Zissman K, Lejbkowicz I, Miller A. Telemedicine for multiple sclerosis patients: assessment using Health Value Compass. Mult Scler 2012;18:472–480. [DOI] [PubMed] [Google Scholar]
- 4.Finkelstein J, Cha E, Wood J, Wallin MT. Predictors of successful acceptance of home telemanagement in veterans with Multiple Sclerosis. Conf Proc IEEE Eng Med Biol Soc 2013;2013:7314–7317. [DOI] [PubMed] [Google Scholar]
- 5.Wechsler LR, Tsao JW, Levine SR, et al. . Teleneurology applications: Report of the Telemedicine Work Group of the American Academy of Neurology. Neurology 2013;80:670–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wood J, Wallin M, Finkelstein J. Can a low-cost webcam be used for a remote neurological exam? Stud Health Technol Inform 2013;190:30–32. [PubMed] [Google Scholar]
- 7.Kane RL, Bever CT, Ehrmantraut M, Forte A, Culpepper WJ, Wallin MT. Teleneurology in patients with multiple sclerosis: EDSS ratings derived remotely and from hands-on examination. J Telemed Telecare 2008;14:190–194. [DOI] [PubMed] [Google Scholar]
- 8.Schneider RB, Biglan KM. The promise of telemedicine for chronic neurological disorders: the example of Parkinson's disease. Lancet Neurol 2017;16:541–551. [DOI] [PubMed] [Google Scholar]
- 9.Duffy S, Lee TH. In-person health care as option B. N Engl J Med 2018;378:104–106. [DOI] [PubMed] [Google Scholar]
- 10.Hatzakis M Jr, Haselkorn J, Williams R, Turner A, Nichol P. Telemedicine and the delivery of health services to veterans with multiple sclerosis. J Rehabil Res Dev 2003;40:265–282. [PubMed] [Google Scholar]
- 11.Bove R, Bevan C, Crabtree E, et al. . Towards a low-cost, in-home, telemedicine-enabled assessment of disability in multiple sclerosis. Mult Scler Epub 2018 Aug 24. [DOI] [PubMed]
- 12.Settle JR, Robinson SA, Kane R, Maloni HW, Wallin MT. Remote cognitive assessments for patients with multiple sclerosis: a feasibility study. Mult Scler 2015;21:1072–1079. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
An anonymized data set including data not published within the article will be shared on request from any qualified investigator.