Abstract
Purpose
Topical agents play a key role in the management of facial seborrheic dermatitis (SD) by reducing inflammation and scale production. The aim of this open-label trial was to assess the efficacy and tolerability of a new non-corticosteroid, antifungal/anti-inflammatory/antiseborrheic cream containing piroctone olamine, stearyl glycyrrhetinate, and zinc PCA in the treatment of facial SD using clinical and instrumental evaluation.
Patients and methods
Twenty adult subjects affected by mild-to-moderate inflamed facial SD were enrolled and instructed to apply the study cream twice daily for 60 days. Efficacy was evaluated at baseline, and at days 15, 30, and 60 by measuring the grade of desquamation, erythema, and pruritus using clinical evaluation, erythema-directed digital photography, colorimetry, and subject-completed Visual Analog Scale. Additionally, an Investigator Global Assessment (IGA) was assessed using a 5-point scale: excellent response (>80% improvement); good response (50%–80% improvement); mild response (<50% improvement); no response (no change); worsening.
Results
After 15 days, a statistically significant decrease from baseline was found in desquamation, erythema, colorimetric scores, and pruritus. At day 60, a significant further improvement for all evaluated parameters was recorded. Moreover, the IGA improved in 90% of patients, with an excellent response in 53% of cases. A good correlation was found between clinical and instrumental evaluations.
Conclusion
Our results indicate that the study facial cream represents an option to consider when dealing with mild-to-moderate SD, being effective, well-tolerated, and free of significant side effects, as confirmed by clinical and instrumental evaluation.
Keywords: seborrheic dermatitis, topical cosmetic, digital photography, colorimeter
Introduction
Facial seborrheic dermatitis (SD) is a common, chronic, recurrent inflammatory disease clinically characterized by erythema, scaling, and pruritus on sebum-rich areas, including the nasolabial folds, malar regions, glabella, and eyebrows. The external auditory meatus and the retroauricular areas can also be affected.1–5
The pathogenesis of SD is still unclear, but it seems to be multifactorial, involving sebaceous gland function, presence on the skin of yeasts belonging to the Malassezia (M.) spp. (formerly called Pityrosporum ovale), and the individual immune response.6–8
Additional precipitating factors include drug intake (lithium, haloperidol, buspirone, chlorpromazine, methyldopa, cimetidine), nutritional deficiency (acrodermatitis enteropathica due to zinc deficiency), neurological and degenerative disorders (Parkinson’s disease), immunosuppression (HIV and non-HIV related), genetic disorders (trisomy 21), as well as environmental factors (cold, low humidity, excessive sun exposure), physical and psychological stress, and unhealthy lifestyle (alcohol consumption).1,2
The therapeutic approach should be selected according to SD severity and the patient’s immune status and compliance. For mild-to-moderate facial SD, topical drugs play a key role in the management by reducing erythema and scale production. These include corticosteroids and antifungals.9–14 The clinical efficacy of current therapeutic agents is widely demonstrated,9–11 although their prolonged use may cause some adverse effects, including skin atrophy, striae, telangiectasia, folliculitis, hypopigmentation, and tachyphylaxis in the case of corticosteroids, irritant contact dermatitis from the use of antifungals, and limitations due to the off-label use of metronidazole, benzoyl peroxide, lithium succinate/lithium gluconate, pimecrolimus, and tacrolimus.
The therapeutic efficacy of topical treatments is generally based on clinical evaluation of erythema and/or scaling severity. Erythema-directed digital photography and colorimetry are noninvasive instrumental techniques that help determine treatment outcome more precisely than simple clinical inspection or standard photography, providing a more accurate evaluation of erythema severity.15–21
The aim of this open-label trial was to assess the efficacy and tolerability of a new topical non-corticosteroid, antifungal/anti-inflammatory/antiseborrheic facial cream in the treatment of mild-to-moderate SD by clinical assessment and by erythema-directed photography and colorimetry evaluation.
Patients and methods
Study design
This was an open-label, prospective clinical trial.
Setting and study period
From September 2017 to March 2018 a total of 20 adult subjects (15M/5F; age range 19–55 years) affected by mild-to-moderate facial SD were enrolled at the Department of Dermatology of the University of Catania. Study duration was 60 days. The study was performed in accordance with the ethical principles originating from the Declaration of Helsinki 1996 and Good Clinical Practices. The protocol was approved by the institutional review board of AOU Policlinico “Vittorio Emanuele” Hospital, Catania. Written informed consent was obtained from each patient before study procedures were started, which included consent to use their images.
Inclusion/exclusion criteria
Inclusion criteria included a wash-out period of at least 2 weeks for topical antimycotic/corticosteroid treatments, and 1 month for oral antifungals/corticosteroids or hormonal therapy. Exclusion criteria were: severe underlying disease, concurrent exposure to sunlight and/or artificial ultraviolet sources, pregnancy, and breastfeeding. No other topical products or drugs were allowed, except for standard daily care products, including mild cleansers, noncomedogenic moisturizers, make-up, and SPF 50+ sunscreens.
Methodology
Patients were instructed to apply the non-corticosteroid facial cream containing piroctone olamine, stearyl glycyrrhetinate and zinc PCA, twice daily (at morning and at bedtime) for 8 weeks. In order to reduce potential evaluator bias, all subjects were assessed by an investigator not directly involved in the study at baseline (T0), and at day 15 (T1), 30 (T2), and 60 (T3).
Study endpoints
The primary end point was efficacy evaluation at day 15 (T1), 30 (T2), and 60 (T3) of all clinical parameters (erythema, desquamation, and pruritus) including global assessment; the secondary endpoint was the evaluation of tolerability and cosmetic acceptability.
Clinical and instrumental evaluation criteria
All clinical and instrumental evaluations were carried out at T0, T1, T2, and T3.
Desquamation was rated by clinical evaluation using a 5-point scale: 4 = severe (many large adherent white flakes); 3 = moderate (several small loose white flakes); 2 = mild (few small loose white flakes); 1 = very mild (very few small loose white flakes); 0 = no desquamation.
Erythema was evaluated using: 1) VISIA-CR imaging system equipped with RBX technology (Canfield, Parsippany, NJ, USA), to provide digital images of the face highlighting red areas corresponding to erythema/inflammatory lesions, scored on a 5-point scale (4 = severe erythema; 3 = moderate erythema; 2 = mild erythema; 1 = very mild erythema; 0 = no erythema), and 2) colorimeter DSM II ColorMeter (Cortex Technology, Hadsund, Denmark) (able to provide the degree of erythema of a 4 mm sample skin area on a numeric scale) through three consecutive measurements of a target-affected facial area (the unaffected skin of the submental region was used as intra-patient control).
Measurement of pruritus was carried out with a Visual Analog Scale from 0 = no pruritus to 100 = severe pruritus.
Clinical assessment included evaluation of global efficacy at day 60 by Investigator Global Assessment (IGA) using a 5-point scale: excellent response (>80% improvement); good response (50%–80% improvement); mild response (<50% improvement); no response (no change); worsening.
Finally, product tolerability was evaluated on a 4-point scale: 0 = very poor; 1 = poor; 2 = good; 3 = excellent, and cosmetic acceptability was evaluated on a 4-point scale: 0 = very poor; 1 = poor; 2 = good; 3 = excellent.
Statistical analysis
The statistical analysis was performed using STATA. Qualitative data were expressed as number and percentage, while quantitative data were expressed as mean ± standard deviation. The statistical analysis considered the whole sample and then only the patients who continued the treatment. The comparisons between data obtained before and after treatment were performed with Student’s t-test. Statistical significance was set at P≤0.05.
Results
Subject demographic and clinical history data are shown in Table 1. Seventeen subjects (mild: 5 cases; moderate: 12 cases) completed the study, and three subjects were lost to follow-up for personal reasons.
Table 1.
Demographic and clinical history data at baseline
| Sex, | |
| Female | 5 (25%) |
| Male | 15 (75%) |
|
| |
| Age (years), range | 19–55 |
|
| |
| Age (years), mean ± standard deviation | 37±10.2 |
|
| |
| SD clinical severity | |
| Mild | 8 (40%) |
| Moderate | 12 (60%) |
|
| |
| SD duration (years), range | 6.2–8 |
|
| |
| Duration of current episode (months), range | 4–9 |
Abbreviation: SD, seborrheic dermatitis.
After 15 days of treatment (T1), a statistically significant reduction from baseline was observed in desquamation (from mean 1.2±0.9 to 0.3±0.6; P<0.001), erythema severity (from mean 1.9±0.9 to 1±0.8; P=0.0005), colorimetric scores (from 8.6±5 to 3.4±3; P<0.001), and pruritus (from mean 69±16.8 to 6.7±10.5; P<0.001) (Table 1, Figure 1). Results from all time points are summarized in Table 2.
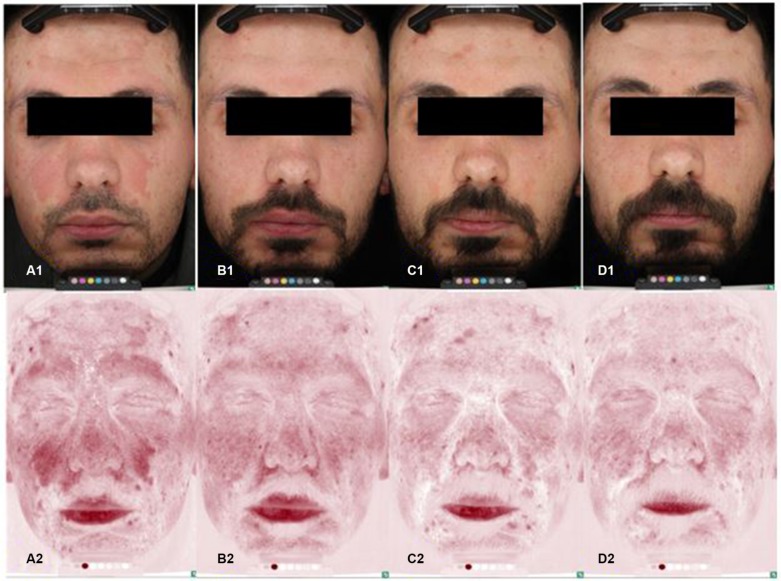
Figure 1.
Standard and erythema-directed digital photography with VISIA-CR of a patient with moderate facial seborrheic dermatitis showing a significant reduction (P<0.001) in erythema after 15 days of treatment (erythema score: 2, B1–B2) compared to baseline (erythema score: 3, A1–A2).
Notes: Erythema scale: 4 = severe erythema; 3 = moderate erythema; 2 = mild erythema; 1 = very mild erythema; 0 = no erythema.
Table 2.
Results from clinical and instrumental assessment of desquamation, erythema, and itch from baseline to study end
| Assessment (n=17) | Baseline (T0) mean ± standard deviation | Day 15 (T1) (mean ± standard deviation) | Day 30 (T2) mean ± standard deviation | Day 60 (T3) mean ± standard deviation |
|---|---|---|---|---|
| Desquamation (clinical) | 1.2±0.9 | 0.3±0.6 (P<0.001) | 0.2±0.4 (P<0.001) | 0.1±0.3 (P<0.001) |
| Erythema (digital photography) | 1.9±0.9 | 1±0.8 (P=0.0005) | 0.7±0.8 (P<0.001) | 0.6±0.6 (P<0.001) |
| Erythema (colorimetry) | 8.6±5 | 3.4±3 (P<0.001) | 2.6±2.8 (P<0.001) | 2.3±2.7 (P<0.001) |
| Itch (VAS) | 69±16.8 | 6.7±10.5 (P<0.001) | 0.6±1.6 (P<0.001) | 0 (P<0.001) |
Abbreviation: VAS, Visual Analog Scale.
At T3, all evaluated parameters showed a progressive, significant reduction (Table 2, Figure 2). IGA showed an excellent response in nine cases (53%), good in five (29.5%), mild in two (11.5%), and no change in one case (6%). No patient showed clinical worsening from baseline. Overall, no signs of local side effects were documented during the study and cosmetic tolerability and acceptability was rated as excellent by all patients.
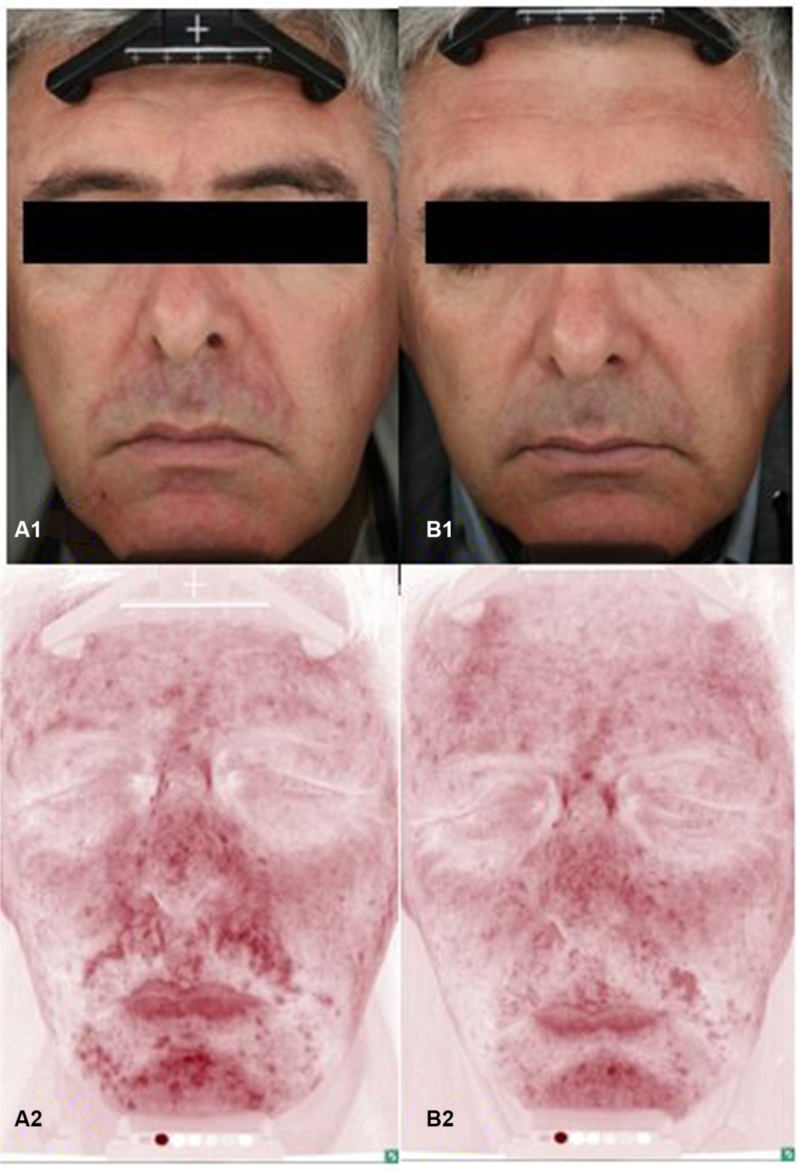
Figure 2.
Standard and erythema-directed digital photography with VISIA-CR of a patient with moderate facial seborrheic dermatitis showing a significant reduction (P<0.001) in erythema at 15 days (erythema score: 2, B1–B2), 30 days (erythema score: 1, C1–C2), and 60 days (erythema score: 0, D1–D2) compared to baseline (erythema score: 3, A1–A2).
Notes: Erythema scale: 4 = severe erythema; 3 = moderate erythema; 2 = mild erythema; 1 = very mild erythema; 0 = no erythema.
Discussion
This pilot, open-label clinical trial with clinical and instrumental evaluation of SD indicates that the non-corticosteroid, antifungal/anti-inflammatory/antiseborrheic facial cream containing piroctone olamine, stearyl glycyrrhetinate, and zinc PCA represents an option to consider when dealing with mild-to-moderate SD, being effective, well-tolerated, and free of significant side effects, as confirmed by clinical and instrumental evaluation. In the 17 subjects who completed the study no serious side effects were recorded.
The mechanisms of action of this fragrance-free product may be related to multiple synergist mechanisms of action of the active ingredients, that include piroctone olamine, an antifungal effective against Malassezia spp. by chelation of iron and other minerals,10 stearyl glycyrrhetinate (a salt and ester of glycyrrhetinic acid) that exhibits anti-inflammatory, soothing and antipruritic effects,22 as well as zinc PCA which combines anti-inflammatory properties with antiseborrheic efficacy.23
We are aware that our study has some limitations: it was an open study from a single center, the number of patients was limited, and there was no control group for comparison – a split-face comparison could also have helped improve the study design and thus the robustness of the results. However, we reduced the possible bias of the open study by requesting an independent investigator to evaluate the clinical signs at four time points and by supporting our clinical results with objective instrumental evaluations, an original approach in SD treatment evaluation. These instrumental assessments are extremely time-consuming and costly and could not be used in routine consultation. Further studies on a larger series are necessary to confirm our results.
Conclusion
This new topical non-corticosteroid antifungal/anti-inflammatory/antiseborrheic combination cream is a good treatment option for mild-to-moderate facial SD and was well-tolerated during the 60 days of treatment.
Acknowledgments
The study was supported financially by ISDIN SA, Spain, which manufacture the product.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Gupta AK, Bluhm R. Seborrheic dermatitis. J Eur Acad Dermatol Venereol. 2004;18(1):13–26. doi: 10.1111/j.1468-3083.2004.00693.x. [DOI] [PubMed] [Google Scholar]
- 2.Naldi L, Rebora A. Clinical practice. seborrheic dermatitis. N Engl J Med. 2009;360(4):387–396. doi: 10.1056/NEJMcp0806464. [DOI] [PubMed] [Google Scholar]
- 3.Berk T, Scheinfeld N. Seborrheic dermatitis. P T. 2010;35(6):348–352. [PMC free article] [PubMed] [Google Scholar]
- 4.Naldi L. Seborrhoeic dermatitis. BMJ Clin Evid. 2010;7:1713. [PMC free article] [PubMed] [Google Scholar]
- 5.Sampaio AL, Mameri AC, Vargas TJ, Ramos-e-Silva M, Nunes AP, Carneiro SC. Seborrheic dermatitis. An Bras Dermatol. 2011;86(6):1061–1071. doi: 10.1590/s0365-05962011000600002. [DOI] [PubMed] [Google Scholar]
- 6.Dessinioti C, Katsambas A. Seborrheic dermatitis: etiology, risk factors, and treatments: facts and controversies. Clin Dermatol. 2013;31(4):343–351. doi: 10.1016/j.clindermatol.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 7.Bukvić Mokos Z, Kralj M, Basta-Juzbašić A, Lakoš Jukić I. Seborrheic dermatitis: an update. Acta Dermatovenerol Croat. 2012;20(2):98–104. [PubMed] [Google Scholar]
- 8.Gary G. Optimizing treatment approaches in seborrheic dermatitis. J Clin Aesthet Dermatol. 2013;6(2):44–49. [PMC free article] [PubMed] [Google Scholar]
- 9.Kastarinen H, Oksanen T, Okokon E, et al. Topical anti-inflammatory agents for seborrhoeic dermatitis of the face or scalp. . Cochrane Database Syst Rev. 2014;5:CD009446. doi: 10.1002/14651858.CD009446.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Okokon E, Verbeek J, Ruotsalainen J, Ojo O, Bakhoya V. Topical antifungals for seborrhoeic dermatitis. . Cochrane Database Syst Rev. 2015;4:CD008138. doi: 10.1002/14651858.CD008138.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kastarinen H, Okokon EO, Verbeek JH. Topical anti-inflammatory agents for seborrheic dermatitis of the face or scalp: summary of a Cochrane review. JAMA Dermatol. 2015;151(2):221–222. doi: 10.1001/jamadermatol.2014.3186. [DOI] [PubMed] [Google Scholar]
- 12.Cheong WK, Yeung CK, Torsekar RG, et al. Treatment of seborrhoeic dermatitis in Asia: a consensus guide. Skin Appendage Disord. 2016;1(4):187–196. doi: 10.1159/000444682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gupta AK, Versteeg SG. Topical treatment of facial seborrheic dermatitis: a systematic review. Am J Clin Dermatol. 2017;18(2):193–213. doi: 10.1007/s40257-016-0232-2. [DOI] [PubMed] [Google Scholar]
- 14.Borda LJ, Perper M, Keri JE. Treatment of seborrheic dermatitis: a comprehensive review. J Dermatolog Treat. 2018;3:1–12. doi: 10.1080/09546634.2018.1473554. [DOI] [PubMed] [Google Scholar]
- 15.Dall’Oglio F, Tedeschi A, Guardabasso V, Micali G. Evaluation of a topical anti-inflammatory/antifungal combination cream in mild-to-moderate facial seborrheic dermatitis: an intra-subject controlled trial examining treated vs. untreated skin utilizing clinical features and erythema-directed digital photography. J Clin Aesthet Dermatol. 2015;8(9):33–38. [PMC free article] [PubMed] [Google Scholar]
- 16.Micali G, Gerber PA, Lacarrubba F, Schäfer G. Improving treatment of erythematotelangiectatic rosacea with laser and/or topical therapy through enhanced discrimination of its clinical features. J Clin Aesthet Dermatol. 2016;9(7):30–39. [PMC free article] [PubMed] [Google Scholar]
- 17.Micali G, Dall’Oglio F, Verzì AE, Luppino I, Bhatt K, Lacarrubba F. Treatment of erythematotelangiectatic rosacea with brimonidine alone or combined with vascular laser based on preliminary instrumental evaluation of the vascular component. Lasers Med Sci. 2018;33(6):1397–1400. doi: 10.1007/s10103-017-2318-3. [DOI] [PubMed] [Google Scholar]
- 18.Dall’Oglio F, Tedeschi A, Fusto CM, Lacarrubba F, Dinotta F, Micali G. A novel cosmetic antifungal/anti-inflammatory topical gel for the treatment of mild to moderate seborrheic dermatitis of the face: an open-label trial utilizing clinical evaluation and erythema-directed digital photography. G Ital Dermatol Venereol. 2017;152(5):436–440. doi: 10.23736/S0392-0488.17.05539-0. [DOI] [PubMed] [Google Scholar]
- 19.Micali G, Dall’Oglio F, Tedeschi A, Lacarrubba F. Erythema-directed digital photography for the enhanced evaluation of topical treatments for acne vulgaris. Skin Res Technol. 2018;24(3):440–444. doi: 10.1111/srt.12448. [DOI] [PubMed] [Google Scholar]
- 20.Andreassi L, Flori L. Practical applications of cutaneous colorimetry. Clin Dermatol. 1995;13(4):369–373. doi: 10.1016/0738-081x(95)00069-r. [DOI] [PubMed] [Google Scholar]
- 21.Matias AR, Ferreira M, Costa P, Neto P. Skin colour, skin redness and melanin biometric measurements: comparison study between Antera(®) 3D, Mexameter(®) and Colorimeter(®) Skin Res Technol. 2015;21(3):346–362. doi: 10.1111/srt.12199. [DOI] [PubMed] [Google Scholar]
- 22.Asl MN, Hosseinzadeh H. Review of pharmacological effects of Glycyrrhiza sp. and its bioactive compounds. Phytother Res. 2008;22(6):709–724. doi: 10.1002/ptr.2362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Takino Y, Okura F, Kitazawa M, Iwasaki K, Tagami H. Zinc l-pyrrolidone carboxylate inhibits the UVA-induced production of matrix metalloproteinase-1 by in vitro cultured skin fibroblasts, whereas it enhances their collagen synthesis. Int J Cosmet Sci. 2012;34(1):23–28. doi: 10.1111/j.1468-2494.2011.00676.x. [DOI] [PubMed] [Google Scholar]