Summary
Aims
To investigate fear of hypoglycaemia (FoH) longitudinally in a cross‐sectional study of adult patients with type 1 diabetes. Specifically, we investigated two subgroups of patients who over 4 years either showed a substantial increase or decrease in level of FoH to identify factors associated with changes in FoH.
Methods
The Swedish version of the Hypoglycaemia Fear Survey (HFS) along with a questionnaire to assess hypoglycaemia history was sent by mail to 764 patients in 2010. The responders in 2010 (n = 469) received another set of the same two questionnaires in 2014. HbA1c, insulin regimen, weight and creatinine from 2010 and 2014 were obtained from medical records. Those with an absolute difference in HFS scores ≥ 75th percentile were included in the subgroup analyses. Statistical analyses included one‐sample t tests, chi‐square and McNemar's test.
Results
The absolute difference in the HFS total score (n = 347) between 2010 and 2014 was m = ±7.6, SD ± 6. In the increased FoH group, more patients reported a high level of moderate hypoglycaemic episodes as well as impaired awareness of hypoglycaemia in 2014 compared with the decreased FoH group. There were more subjects in the increased FoH group with insulin pumps in 2014 and in 2010. In the decreased FoH group, more patients had a high frequency of daily self‐monitoring of blood glucose (SMBG) in 2010 and in 2014.
Conclusions
Fear of hypoglycaemia is stable across time for most patients. Changes in fear level are associated with changes in hypoglycaemia frequency. Thus, asking patients about changes in hypoglycaemia experiences is of great importance.
Keywords: fear of hypoglycaemia, hypoglycaemia, type 1 diabetes
1. INTRODUCTION
Hypoglycaemia is one of the most serious adverse effects of diabetes therapy and the factor that limits achieving tight glycaemic control in individuals with type 1 diabetes.1 An epidemiological observational study reporting hypoglycaemia rates in a global population found that overall hypoglycaemia rates were high and rates of any, nocturnal and severe hypoglycaemia were 73.3, 11.3 and 4.9 events/patient‐year for type 1 diabetes.2 A retrospective observational multicenter study collecting data on hypoglycaemia in real‐life setting showed that a minority of patients accounted for the majority of both severe and symptomatic episodes in type 1 diabetes.3 Structured diabetes education delivered in routine practice for persons with type 1 diabetes have been found to at least halving rates of severe hypoglycaemia (SH) 4 and lead to reduced emergency treatment costs.5
Past experience of SH is associated with greater fear of hypoglycaemia (FoH) in individuals with type 1 diabetes, suggesting that the experience of hypoglycaemia plays an important role in triggering FoH.2, 6, 7, 8, 9 FoH is recognized as a complex and common phenomenon affecting quality of life and diabetes management for individuals with type 1 diabetes.9 Furthermore, worries about hypoglycaemia are also common in family members.10 In a large cohort study, we found gender differences in FoH, suggesting that females are more affected by FoH than men. In addition, impaired awareness of hypoglycaemia (IAH), frequency of mild hypoglycaemia, number of symptoms during mild hypoglycaemia, number of hypoglycaemic symptoms during hyperglycaemia, HbA1c, and visits to the emergency department because of hyperglycaemia were identified as significant factors associated with FoH.6 A recent study in young adults (aged 18‐35 years) with type 1 diabetes showed that FoH was associated with greater glycaemic variability and with higher calorie intake and less physical activity.11 Furthermore, other associations have been shown between FoH diabetes‐related quality of life and psychological well‐being 12 and personality traits such as anxiety.7, 13 FoH is greater at night and may contribute to poor sleep quality.14
Fear of hypoglycaemia remains a problem, despite advances in technology, insulin analogs, and evidence‐based management.11 However, we know very little about what happens with FoH over time if left untreated. Therefore, the aim of this study was to investigate FoH longitudinally in a cross‐sectional study of adult individuals with type 1 diabetes. Specifically, we investigated two subgroups of participants who over 4 years either showed an increase or decrease in FoH level in order to identify factors associated with changes in FoH.
2. PATIENTS AND METHODS
2.1. Participants and procedure
In 2010, 764 patients who participated in a previous FOH study6 received a consent form and a set of questionnaires by mail. In the original study, the inclusion criteria were type 1 diabetes, age ≥18 years and diabetes duration ≥1 year. Participants were identified in the local diabetes registries of two university hospitals in Stockholm, Sweden. The responders in 2010 (n = 469) then received another set of questionnaires in 2014. HbA1c, insulin regimen, weight and creatinine from 2010 and 2014 were obtained from medical records.
2.2. Questionnaires
Cox et al.15 developed the original Hypoglycaemia Fear Survey (HFS) to measure FoH. The questionnaire consists of two subscales containing 23 items rated on a five‐point Likert scale, 0 (never) to 4 (always). The total sum score ranges from 0 to 92. A higher score indicates higher FoH. The HFS Worry subscale includes 13 items measuring anxiety‐provoking aspects of hypoglycaemia; scores range from 0 to 52; and the HFS Behavior subscale includes 10 items measuring behaviour done in order to avoid hypoglycaemia or the consequences of hypoglycaemia, score range from 0 to 40. In this study, we used a Swedish translation of the Hypoglycaemia Fear Survey (Swe‐HFS).16
A diabetes history questionnaire assessing clinical variables regarding hypoglycaemia history (mild, moderate, nocturnal and SH, unawareness, and daytime/nocturnal self‐monitoring of blood glucose [SMBG]) over the past 12 months was used.17
2.3. Statistical analysis
Statistical analysis was performed using spss 22 for Windows (spss Inc.; Chicago, IL, USA).
Responders with an absolute difference in HFS scores ≥75th percentile were included in the subgroup analyses. Statistical analyses included one‐sample t tests, independent samples t tests, chi‐square and McNemar's test, as appropriate.
2.4. Ethical consideration
The study was approved by the regional ethical review board, Dnr‐ 2006/1069‐31/2.
3. RESULTS
Of the 469 subjects who received the questionnaire in 2014, 74% (n = 347) responded, 179 women and 168 men. There was one significant difference between responders and nonresponders with the latter having shorter diabetes duration (32.8 years vs 36.1 years, P .036). Descriptive data on all subjects can be found in Table 1. The absolute difference in the HFS total score) between 2010 and 2014 was m = ±7.6, SD ± 6 (median ± 6.0, range ‐35 ‐ +22). For illustration of HFS‐values 2010 and 2014, see Figure 1. There were no within‐group differences in the hypoglycaemia history variables or medical variables between 2010 and 2014. The gender difference persisted over time with women scoring higher on HFS compared to men (in 2010, 33.4 vs 29.8, P .014 and 2014 33.3 vs 29.7, P .015).
Table 1.
Demographic and clinical characteristics of responders and nonresponders
| Responders n = 347 | Nonresponders n = 122 | P | |||
|---|---|---|---|---|---|
| Mean (range) | SD | Mean (range) | SD | ||
| Age (years) | 52.1 (27‐84) | 13.5 | 49.3 (27‐87) | 14.9 | .104 |
| Diabetes duration (years) | 36.1 (7‐68) | 13.8 | 32.8 (8‐71) | 14.9 | .036* |
| HbA1c 2010(%) | 6.9 (3.6 ‐10.7) | .96 | 7.1 (4.4 ‐11) | 1.2 | .064 |
| HFS 2010 | 31.7 (5‐83) | 14 | 32.1 (6‐75) | 13.4 | .776 |
| HFS 2014 | 31.6 (5‐78) | 13.7 | ‐ | ‐ | |
| Percentage % | |||||
| Gender (% female) | 51.7 | 43.1 | .065 | ||
HFS, Hypoglycaemia Fear Survey.
*Significant at P. 05.
Figure 1.
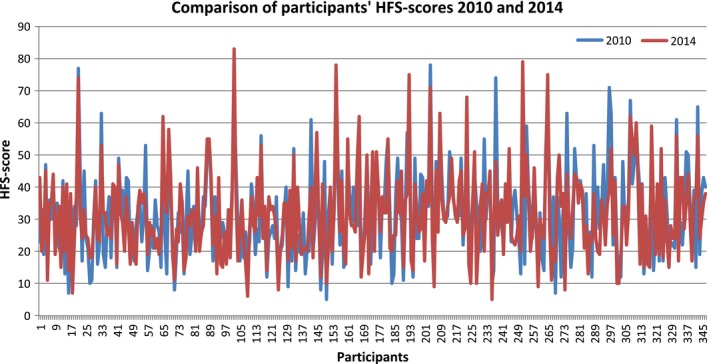
Each participant's individual scores on Hypoglycaemia Fear Survey (HFS) in 2010 (in blue) and in 2014 (in red)
Between‐groups analyses showed that there was a significant difference in long‐acting insulin regimen between the decreased FoH group and the increased FoH group both in 2010 and in 2014. There were more participants in the increased FoH group with insulin pumps compared to the decreased FoH group (47% vs 20% in 2014, 50% vs 16% in 2010). Furthermore, in the decreased FoH group, more participants had a high frequency of daytime SMBG compared to the increased FoH group in 2010 (35% vs 15.5%) and in 2014 (37.5% vs 13.5%). In the increased FoH group, more participants reported a high level of moderate hypoglycaemic episodes (52% vs 23%) as well as IAH (75.5% vs 53.5%) in 2014 compared with the decreased FoH group. All between‐group results can be found in Table 2.
Table 2.
Between‐group differences in self‐monitoring of blood glucose (SMBG), hypoglycaemia history, demographic and medical variables 2010 and 2014
| Between‐group differences | Group w. increased FoH (n = 45) % (n) | Group w. decreased FoH (n = 43) % (n) | χ2 (df) | P |
|---|---|---|---|---|
| High frequency of daytime SMBG | ||||
| 2010 | 16% (7) | 35% (15) | 4.38 (1) | .036a |
| 2014 | 16% (7) | 38% (16) | 4.75 (1) | .030a |
| Gender (women) | 49% | 47% | .04 (1) | .84 |
| High frequency of nocturnal SMBG | ||||
| 2010 | 16% (7) | 26% (11) | 1.36 (1) | .24 |
| 2014 | 24% (11) | 26% (11) | 0.04 (1) | .851 |
| High level of mild hypoglycaemia | ||||
| 2010 | 53% (24) | 47% (20) | 2.82 (1) | .60 |
| 2014 | 68% (31) | 50% (22) | 2.943 (1) | .086 |
| High level of moderate hypoglycaemia | ||||
| 2010 | 38% (17) | 30% (13) | .56 (1) | .46 |
| 2014 | 52% (23) | 23% (10) | 7.77 (1) | .005b |
| High level of nocturnal hypoglycaemia | ||||
| 2014 | 47% (21) | 44% (19) | .11 (1) | .74 |
| High level of severe hypoglycaemia | ||||
| 2010 | 31% (14) | 40% (17) | .68 (1) | .41 |
| 2014 | 43% (19) | 30% (13) | 1.568 (1) | .21 |
| IAH | ||||
| 2010 | 59% (27) | 56% (24) | .10 (1) | .76 |
| 2014 | 76% (34) | 54% (23) | 4.693 (1) | .03a |
| Insulin pump, | ||||
| 2010 | 50% (22) | 16% (7) | 11.34 (3) | .003b |
| 2014 | 47% (21) | 20% (9) | 7.81 (3) | .05a |
| Between‐group differences | Group w. increased FoH (n = 45) | Group w. decreased FoH (n = 43) | t(df) | P |
|---|---|---|---|---|
| Age (years) | 52.2 | 54.7 | .64 (86) | .52 |
| HbA1c | ||||
| 2010 | 60.4 mmol/mol | 59.6 mmol/mol | .043 (86) | .84 |
| 2014 | 60.4 mmol/mol | 61.1 mmol/mol | 1.32 (86) | .25 |
| Weight | ||||
| 2010 | 78.2 kg | 77.3 kg | .003 (86) | .96 |
| 2014 | 78.2 kg | 77.6 kg | 1.06 (86) | .31 |
| Duration (years) | 36.4 | 38.3 | .64 (86) | .39 |
| Creatinine | ||||
| 2010 | 85.8 μmol/L | 82.8 μmol/L | .45 (86) | .50 |
| 2014 | 87.6 μmol/L | 81.9 μmol/L | 1.08 (86) | .30 |
IAH, impaired awareness of hypoglycaemia; FoH, fear of hypoglycaemia.
Significant at P.05.
Significant at P.01.
4. DISCUSSION
To our knowledge, this is the first longitudinal study of FoH in individuals with type 1 diabetes. Our study shows that FoH is stable across time for most people (Figure 1). The absolute mean difference on the HFS over 4 years was ± 7.6 points (median ± 6.0). This study also found additional support for the gender difference found in 2010 that shows FoH to be more frequent among women.
However, the large range in absolute difference scores (−35 ‐ + 22) indicates that there are a number of individuals whose fear levels have changed dramatically, either up or down. Our subgroup data of these results confirm prior research that has shown the experience of hypoglycaemic episodes to be the factor with the strongest influence on the fear level.9 In the group with increased FoH 2014, more participants have a high degree of moderate hypos compared to the decreased FoH group (52% vs 23%). Although not statistically significant, there seems to be a trend towards a within‐group difference for the increased FoH group from 38% in 2010 to 52% in 2014. The increased FoH group also has more participants with IAH than the decreased FoH in 2014, but there was no difference between the two groups in 2010. It is well known that IAH increases the risk of hypoglycaemia and also increases FoH.9
Furthermore, the increased FoH group has a lower level of SMBG both in 2010 and 2014. This indicates that these individuals may benefit from increasing their use of SMBG or using continuous glucose monitoring (CGM). This may especially apply those with IAH. Using SMBG or CGM could improve their ability to prevent, detect and adequately treat hypoglycaemia and perhaps as a result reduce FoH.
A somewhat puzzling find is that there was a difference in insulin regimen between the increased FoH group and the decreased FoH group. More participants in the increased FoH group were on CSII compared to the decreased FoH group. However, there had not been a change in regimen between 2010 and 2014, subjects using a pump in 2014 were also using a pump in 2010. It could be speculated that this group consisted of people with more labile glucose control which is regarded as an indication for pump treatment in Sweden. A systematic review of the clinical effectiveness of CSII 18 found that compared to MDI, treatment with CSII shows reduction in swings in BG levels, fewer problems with hypoglycaemic episodes and a reduction in the chronic fear of SH. However, a study on FoH and CSII by 19 found that FoH is present in many people with CSII. The study also found that the only significant associations to FoH were accumulated episodes of SH and rate of hypoglycaemia.
A limitation of this study is that hypoglycaemia history and SMBG are self‐reported and may therefore be over‐ or underestimated. This has been found in for instance the study by Cariou et al 2015.20 Furthermore, the slight difference in diabetes duration between responders and nonresponders may indicate that subjects with a higher hypoglycaemia risk may have been more inclined to respond since a longer duration has been shown to be associated with risk of hypoglycaemia in previous studies.2
To conclude, this study shows that FoH is persistent over time if not treated and that hypoglycaemia frequency is the strongest predictor of FoH. Thus, asking patients about the occurrence of hypoglycaemia is of the utmost importance as is helping them adequately detect, prevent and treat hypoglycaemia. In order to do so, psychological and behavioural difficulties must be assessed and addressed using psychological methods and therapeutic education.
CONFLICT OF INTEREST
Therese Anderbro, Susanne Amsberg, Erik Moberg, Linda Gonder‐Frederick, Ulf Adamson, Per‐Eric Lins and Unn‐Britt Johansson declare that they have no conflict of interest.
AUTHOR CONTRIBUTION
T.A. researched and interpreted the data and wrote the manuscript. E.M, L.G‐F, P‐E. L and U‐B.J. interpreted the data and reviewed/edited the manuscript. U.A and S.A contributed to discussion and reviewed/edited the manuscript. All authors reviewed, commented on and accepted the manuscript. T.A. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Anderbro TC, Amsberg S, Moberg E, et al. A longitudinal study of fear of hypoglycaemia in adults with type 1 diabetes. Endocrinol Diab Metab. 2018;1:e13 10.1002/edm2.13
Funding information
This study was funded by Sophiahemmet University, the Foundation for Medical Research at Sophiahemmet, Furthermore Consumer Health supported the study.
REFERENCES
- 1. Cryer PE. The barrier of hypoglycemia in diabetes. Diabetes. 2008;57:3169‐3176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Khunti K, Alsifri S, Aronson R, et al. Rates and predictors of hypoglycaemia in 27 585 people from 24 countries with insulin‐treated type 1 and type 2 diabetes: the global HAT study. Diabetes Obes Metab. 2016;18:907‐915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Giorda CB, Ozzello A, Gentile S, et al. Incidence and risk factors for severe and symptomatic hypoglycemia in type 1 diabetes. Results of the HYPOS‐1 study. Acta Diabetol. 2015;52:845‐853. [DOI] [PubMed] [Google Scholar]
- 4. Speight J, Holmes‐Truscott E, Harvey DM, et al. Structured type 1 diabetes education delivered in routine care in Australia reduces diabetes‐related emergencies and severe diabetes‐related distress: the OzDAFNE program. Diabetes Res Clin Pract. 2016;112:65‐72. [DOI] [PubMed] [Google Scholar]
- 5. Elliott J, Jacques RM, Kruger J, et al. Substantial reductions in the number of diabetic ketoacidosis and severe hypoglycaemia episodes requiring emergency treatment lead to reduced costs after structured education in adults with type 1 diabetes. Diabet Med. 2014;31:847‐853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Anderbro T, Amsberg S, Adamson U, et al. Fear of hypoglycaemia in adults with type 1 diabetes. Diabet Med. 2010;27:1151‐1158. [DOI] [PubMed] [Google Scholar]
- 7. Anderbro T, Gonder‐Frederick L, Bolinder J, et al. Fear of hypoglycemia: relationship to hypoglycemic risk and psychological factors. Acta Diabetol. 2015;52:581‐589. [DOI] [PubMed] [Google Scholar]
- 8. Nefs G, Bevelander S, Hendrieckx C, et al. Fear of hypoglycaemia in adults with type 1 diabetes: results from diabetes MILES ‐ The Netherlands. Diabet Med. 2015;32:1289‐1296. [DOI] [PubMed] [Google Scholar]
- 9. Wild D, von Maltzahn R, Brohan E, Christensen T, Clauson P, Gonder‐Frederick L. A critical review of the literature on fear of hypoglycemia in diabetes: implications for diabetes management and patient education. Patient Educ Couns. 2007;68:10‐15. [DOI] [PubMed] [Google Scholar]
- 10. Nefs G, Pouwer F, Holt RI, et al. Correlates and outcomes of worries about hypoglycemia in family members of adults with diabetes: the second Diabetes Attitudes, Wishes and Needs (DAWN2) study. J Psychosom Res. 2016;89:69‐77. [DOI] [PubMed] [Google Scholar]
- 11. Martyn‐Nemeth P, Quinn L, Penckofer S, Park C, Hofer V, Burke L. Fear of hypoglycemia: influence on glycemic variability and self‐management behavior in young adults with type 1 diabetes. J Diabetes Complications. 2017;30:167‐177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Strandberg RB, Graue M, Wentzel‐Larsen T, Peyrot M, Wahl AK, Rokne B. The relationships among fear of hypoglycaemia, diabetes‐related quality of life and psychological well‐being in Norwegian adults with type 1 diabetes. Diabetes Res Clin Pract. 2017;124:11‐19. [DOI] [PubMed] [Google Scholar]
- 13. Gonder‐Frederick LA, Fisher CD, Ritterband LM, et al. Predictors of fear of hypoglycemia in adolescents with type 1 diabetes and their parents. Pediatr Diabetes. 2006;7:215‐222. [DOI] [PubMed] [Google Scholar]
- 14. Martyn‐Nemeth P, Schwarz Farabi S, Mihailescu D, Nemeth J, Quinn L. Fear of hypoglycemia in adults with type 1 diabetes: impact of therapeutic advances and strategies for prevention ‐ a review. J Diabetes Complications. 2016;30:167‐177. [DOI] [PubMed] [Google Scholar]
- 15. Cox DJ, Irvine A, Gonder‐Frederick L, Nowacek G, Butterfield J. Fear of hypoglycemia: quantification, validation, and utilization. Diabetes Care. 1987;10:617‐621. [DOI] [PubMed] [Google Scholar]
- 16. Anderbro T, Amsberg S, Wredling R, et al. Psychometric evaluation of the Swedish version of the Hypoglycaemia fear survey. Patient Educ Couns. 2008;73:127‐131. [DOI] [PubMed] [Google Scholar]
- 17. Wredling R. On the management of insulin dependent diabetes mellitus. Karolinska Institutet (thesis). Stockholm 1991.
- 18. Cummins E, Royle P, Snaith A, et al. Clinical effectiveness and cost‐effectiveness of continuous subcutaneous insulin infusion for diabetes: systematic review and economic evaluation. Health Technol Assess. 2010;14:1‐181. [DOI] [PubMed] [Google Scholar]
- 19. Nixon R, Pickup JC. Fear of hypoglycemia in type 1 diabetes managed by continuous subcutaneous insulin infusion: is it associated with poor glycemic control? Diabetes Technol Ther. 2011;13:93‐98. [DOI] [PubMed] [Google Scholar]
- 20. Cariou B, Fontaine P, Eschwege E, et al. Frequency and predictors of confirmed hypoglycaemia in type 1 and insulin‐treated type 2 diabetes mellitus patients in a real‐life setting: results from the DIALOG study. Diabetes Metab. 2015;2:116‐125. [DOI] [PubMed] [Google Scholar]


