Abstract
Introduction
There have been several educational reforms calling for increasing lesbian, gay, bisexual, and transgender (LGBT) education materials, application of basic sciences to clinical medicine, and active engagement of students. While the amount of educational materials for LGBT clinical cases is increasing, this session for preclinical medical students uniquely combines basic science population genetics, cisgender lesbian, gay, and bisexual (LGB) cultural issues and reproductive endocrinology in a 1.5-hour flipped classroom session.
Methods
Students were assigned a prediscussion video and reading. Facilitators attended a 1.5-hour training session prior to discussion. Each classroom of 30 students with small groups of six was led by a third- or fourth-year medical student facilitator who taught from a PowerPoint that included discussion questions. An audience response system was used to show aggregated, real-time anonymous responses to case questions, a pre- and postsurvey was used to analyze changes in student attitudes and knowledge of assisted reproduction services for same-sex couples, and course evaluations captured overarching student impressions.
Results
All first-year students (N = 180) attended this mandatory session. Audience response questions showed a high level of knowledge of population genetics concepts. Voluntary surveys showed a higher number of assisted reproduction recommendations for LGB patients compared to heterosexual patients before discussion, with this difference disappearing after the discussion. This may indicate a shift in student attitudes and knowledge of LGB patient barriers and assisted reproduction. Course evaluations showed appreciation of LGB material integration within the course.
Discussion
Educators will be able to successfully integrate the application of population genetics, assisted reproduction cases, and an examination of cultural barriers in health care for LGB patients with this session.
Keywords: LGBT, Population Genetics, Health Care Disparities, LGB, Assisted Reproduction
Educational Objectives
At the end of this session, the learner will be able to:
-
1.
Differentiate between population subgroups defined by racial categories or geographic ancestry in terms of genetic variation.
-
2.
Apply the principles of population genetics (e.g., founder effect, Hardy-Weinberg equilibrium, selection pressure) to evaluate genetic risk and predict frequencies of alleles and genotypes in a given population.
-
3.
Compare and contrast the assisted reproduction approaches available for same-sex couples in terms of clinical outcomes, costs, and legal implications.
-
4.
Assess health care barriers that may limit access to same-sex patient couples.
-
5.
Evaluate the significance of testing for the presence of disease alleles in patients from nonmajority ancestral backgrounds and in same-sex couples in a preconception setting.
-
6.
Appraise the potential for false negative results in preconception genetic testing, particularly with respect to donor genetic risk assessment.
Introduction
As genetic technologies continue to emerge, an area of growing clinical application is in the field of reproductive medicine.1 Reproductive genetics are particularly pertinent for same-sex couples and as legally recognized same-sex marriages increase,2,3 the number of same-sex couples seeking assisted reproduction services may increase. However, lesbian, gay, bisexual and transgender (LGBT) individuals experience decreased access to reproductive services due to several factors including: lack of targeted patient education materials,4 lack of insurance coverage of these services for LGBT patients,5 unique ethical and legal considerations with respect to surrogacy and biological custody,6 and providers who have hetero- and gender-normative assumptions and refuse to offer services.7–9 Postulated causes of the provider-induced disparity include lack of formal education in undergraduate medical school, leading to lack of familiarity and comfort with caring for LGBT patients.10
While there are many emerging educational resources on clinical skills, such as taking a sexual history, there is a lack of focus on incorporating LGBT-specific content with basic science concepts, such as how genetic risk profiles may differ when same-sex couples are considered a sperm or an egg donor.11,12 In light of this gap, our goals were to teach population genetics in an applied clinical context, and build upon the body of educational materials for LGBT care by highlighting barriers cisgender lesbian, gay, and bisexual (LGB) same-sex couples may experience when seeking reproductive services.
To create this session, we incorporated information gathered from a literature review,13–16 as well as from interviews with expert fertility practitioners and LGB patients. We built on a prior session learners participated in17by applying the genetic concepts to two scenarios involving cisgender same-sex couples. To facilitate this we used a flipped classroom and progressive disclosure model. The flipped classroom format has students review videos and readings to learn foundational concepts before active class participation, which has been shown to facilitate deeper understanding of the material.18,19 This deeper understanding is made more realistic by the progressive disclosure, where additional information is revealed as the session proceeds, which simulates the decision process,20 and encourages students to fully explore the decision tree of numerous, complex choices that same-sex couples face when deciding to raise a child.
This session was originally designed for first-year medical students enrolled in a genetics course, although it can be taught to medical students of any standing in integrated or discipline-based curricula after they have learned advanced population genetics concepts. The learners should have an intermediate knowledge of reproduction; advanced knowledge of population genetics, genetic testing and genetic diseases; and an awareness of the health care disparities related to LGB sexual orientation. This session fits well as part of a medical genetics course or a reproductive endocrinology course following a medical genetics course.
Methods
To facilitate this session, we recruited and trained third- and fourth-year medical students who had taught several previous genetics sessions. All facilitators had a demonstrated knowledge of direct-to-consumer genetic testing, geographic ancestry, population genetics, and both LGBT health barriers and standards of care. A week before the session we provided the facilitators with the session slides (Appendix A), facilitator's guide (Appendix B), the presession reading (Appendix C), and video (Appendix E) which we reviewed during a 1.5-hour facilitator training a few days before the session. During this session, the cultural aspects of health care barriers for same-sex couples were reviewed in detail, and we also worked through each case question to ensure all facilitators could teach each one and practice using the audience response system software.
One week prior to the session, the presession reading (Appendix C), a textbook chapter,21 and video (Appendix E) were posted on the school's learning management system as a required preclass assignment. Students were asked to spend approximately 1 to 1.5 hours before the session reviewing this material.
On the day of the session, facilitators arrived approximately 10–20 minutes early in order to ensure the classrooms were set up and to troubleshoot any potential technological issues. The case module itself is optimally taught in a 1.5-hour class session, but it has also been implemented at Boston University in a 1-hour class session. We split the group of 30 students into even small groups (five to six students), and separated them into their own classroom. Each of the six rooms was equipped with PowerPoint displays, audience response system software (Turning Point), copies of the discussion handout (Appendix D), a flip chart, and markers. This could also be done in a single room with clustered chairs and tables.
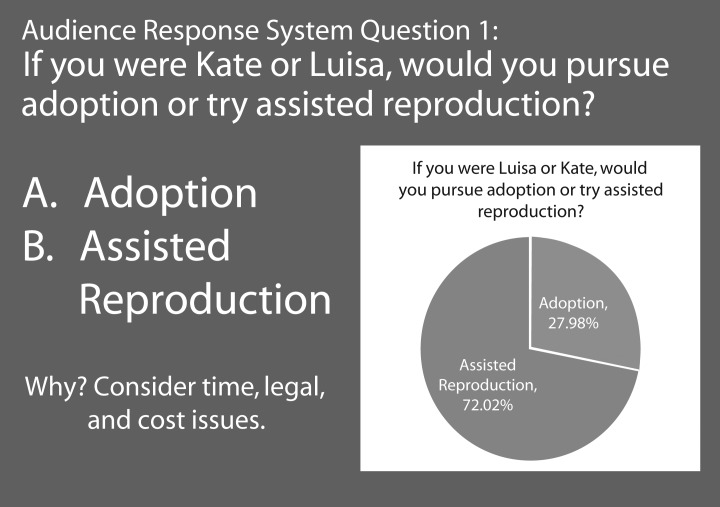
When going through the PowerPoint, facilitators used the audience response system to anonymously record and display audience responses to the multiple-choice questions. This presents student responses in real time, which allows students to see aggregated, anonymous results (Figure 1). In the facilitator's guide (Appendix B), we summarize how students have historically responded in order to prepare facilitators to guide discussion. Facilitators are encouraged to help students consider the pros and cons of each option during audience response questions.
Figure 1. Audience response question with sample classroom response.
Throughout the session, one faculty member specializing in genetics and one specializing in reproduction circulated throughout the classrooms to troubleshoot technological issues and answer any in-depth genetics questions. Because we had six classrooms and two professors, each faculty member spent approximately 20 minutes in each classroom. The faculty members and facilitators also had group texting available in case of any issues.
Assessment
The educational objectives were evaluated by mandatory audience responses questions during the session that tested the learners' ability to apply population genetics concepts as well as by a voluntary pre- and postcurriculum survey (Appendix F) that was deemed exempt by Boston University Institutional Review Board. The survey was distributed to all students via Qualtrics Survey Software before and after the session in order to assess changes in student attitudes and knowledge of same-sex patient couples using questions developed by Kelley L, Chou CL, Dibble SL, and Robertson.22 Responses were analyzed with a two-tailed Fischer's exact test to investigate if the percentage of student recommendations for a same-sex couples differed from heterosexual couples before and after the session. Overall student impressions were collected through course evaluations.
Results
As this was a mandatory session, all 180 students in our first-year class participated in the session and session assessments. Their ability to accurately apply population genetics concepts was demonstrated by the high percentage of correct responses to audience response system questions 4 and 5 (91% and 96%, respectively).
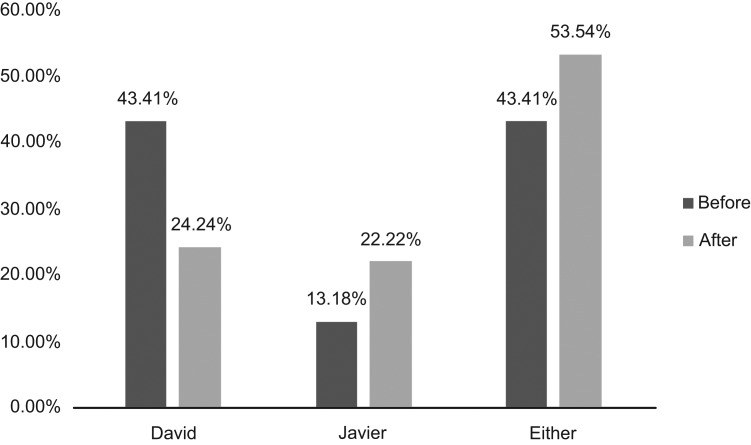
For question seven (Figure 2), 43% learners initially recommended that David, who does not have a history of spinal muscular atrophy, should donate his sperm for gestational surgery. After calculating the risk, 53% of learners recommended that either parent could donate their sperm, which was a statistically significant change (p = 0.0001).
Figure 2. Student Recommendations for Biological Parent Choice Before and After Calculating Genetic Probability (N = 180).
Of the 180 students who attended this mandatory session, 49% of the class initiated the presurvey and 32% initiated the postsurvey, with 35% of the class completing the presurvey and 17% completing the postsurvey. Before the session, students recommended reproductive services about 20% more frequently for same sex couples compared to heterosexual patients. Additional selected results of the Appendix F survey are listed in the Table. It should be noted that on the showcased survey results, heterosexual patients had medical conditions resulting in a similar reproductive condition as the same-sex couple in the case question. Further, intrauterine insemination recommendations between a same-sex female couple and a heterosexual couple were not compared because in vitro fertilization is a more common assisted reproduction choice of heterosexual couples. Results that are not shown included no significant difference in student recommendations between same-sex and heterosexual couples.
Table. Pre- and Postsession Comparison of Student Selection of Case Scenario Recommendations for Cisgender Same-sex Couples as Compared to Heterosexual Couplesa.
| Case Scenarioa | Couple Type | Presession | Postsession | ||||
|---|---|---|---|---|---|---|---|
| % | na | p | % | na | p | ||
| If you were a physician, would you: | |||||||
| 1. Recommend in vitro fertilization? | Same-sex female couple | 81 | 51 | 84 | 25 | ||
| Heterosexual couple | 60 | 38 | .0183 | 77 | 23 | .7480 | |
| 2. Recommend in vitro fertilization? | Same-sex female couple w/ medical condition | 64 | 40 | 93 | 28 | ||
| Heterosexual couple w/ equivalent condition | 83 | 42 | .0264 | 57 | 28 | .4238 | |
| 3. Recommend sperm donation? | Same-sex female couple | 38 | 23 | 57 | 17 | ||
| Heterosexual couple | 16 | 10 | .0085 | 96 | 28 | .1188 | |
| 4. Recommend gestational surrogacy? | Same-sex male couple w/ medical issues | 83 | 52 | 96 | 28 | ||
| Heterosexual couple | 46 | 29 | <.0001 | 66 | 19 | .0054 | |
| 5. Recommend gestational surrogacy for the patients? | Same-sex male couple | 95 | 60 | 100 | 0 | ||
| Heterosexual couple | 76 | 48 | .0040 | 90 | 26 | .2368 | |
Total number of students was 63.
bTotal number of students was 30 for scenarios 1–3, and 29 for scenarios 4 and 5.
In addition to the survey, representative student feedback from course evaluation data describing their reactions of the session are included below:
-
•
“As an openly lesbian woman I can't even begin to describe how much it means to see a SAME-SEX pedigree (I didn't even know those existed?!) or the rest of the our LGBTQI community affirmed as [the facilitator] talked about natural, normal differences in sexual development (DSD), intersex identities, without taking time away from other important topics in this class”
-
•
“[The facilitator] recognized the relevance of race, ethnicity, sexuality, and cultural difference on what she was teaching, and… addressed these topics in a respectful way that enhanced our overall understanding of the material and our ability to provide good care to diverse patient populations. This course should provide the standard for teaching diversity in our other courses.”
Discussion
This session reinforces basic scientific concepts, applies them to a clinical setting, and raises awareness of the barriers experienced by same-sex couples seeking assisted reproduction services. Educational objectives were achieved through various means of assessment. Audience response questions asked students to apply population genetics principles. Figure 2 shows changes in student perceptions of genetic risk before and after completing calculations of risk profiles of different ancestral populations in the module scenarios, reflecting understanding and application. While the application of genetics concepts is shown within session, the extent to which this session influenced this is impacted by the fact that this was implemented within a genetics course. Therefore students may have successfully applied overall course learnings, such as those of the previous session17 to the discussion, as opposed to applying novel population concepts learned from this session. As a result, we must encourage use of this session as an addition to a robust genetics curriculum.
The pre-and postsurveys were used to demonstrate how the session impacted learners attitudes toward and understanding of reproduction counseling for same-sex couples. Notably, some results include initially higher frequency of student recommendations for adoption and assisted reproduction services for same-sex couples compared to heterosexual patients. Whereas after the session, this difference in frequency of recommendations disappeared, resulting in no significant difference in frequency of recommendations for heterosexual patients compared to same-sex couples. Possible explanations for this result include increased clinical knowledge and more appropriate application of assisted reproductive services within the clinical scenarios presented. Estimates of financial costs of each type of procedure and adoption were also presented, which may have affected student responses in recommendations of insurance coverage. Another explanation of these results could be that this session resulted in a shift in the student perceptions of same-sex couples compared to heterosexual couples and both groups were treated the same afterwards. However, these changes were only seen in some of the student survey recommendations. Some results showed a persistent difference in student recommendations for same-sex male couples compared to a heterosexual couple with similar medical conditions, which may indicate that this session did not focus on those teaching points. Other findings showed no initial difference in student recommendations for heterosexual and same-sex couples, which may indicate an awareness of health care requirements for same-sex and heterosexual couples seeking assisted reproduction before this session. A limitation of these results is the low response rate to the postsurvey from a potentially biased sample of students, likely due to the high number of mandatory surveys students are required to complete and the timing of this discussion, which occurred a few days before the end of the school year.
Overall limitations of this session include the lack of materials for transgender patients and their assisted reproduction needs. While preliminary materials were developed, time constraints resulted in lack of incorporation of this material. Thus, future directions include incorporation of transgender cases into a longer session. We also recommend reserving at least 1.5 hours for this session as implementing this session in only 1 hour is rushed. If you have more time, live clinical encounters with patients facing these decisions could allow for deeper consideration of the barriers faced by LGBT patients, but by introducing these topics in case format, students may feel safer in initially exploring topics that may lie outside of their comfort zone. Furthermore, case-based sessions are be more cost-effective and more easily incorporated into a curriculum.
In order to adapt this session to other teaching environments, the multiple-choice questions can be adapted for use with other audience response systems such as PollEverywhere or with simple color-coded index cards th at students can display. The advantage of using an electronic audience response systems is the ability to share anonymous responses in case some students may not wish to have certain responses attributed to them. While we did not give our students a prereading about LGBT terms, if learners to not have exposure to more in-depth LGBT sessions at the institution, educators may wish to provide this glossary of LGBT terms to familiarize students with the vocabulary.23
In summary, this session contributes to the overall body of teaching material for LGB issues and encourages students to discuss culturally sensitive topics while applying population genetics principles. By utilizing a flipped classroom and a progressive disclosure format, active student learning and participation is promoted with open discussion of potentially sensitive issues. Medical student educators can use this inclusive, patient-centered session to build awareness of important health care barriers that same-sex couples face, highlighting what medical students, as future physicians, can do as advocates for their patients.
Appendices
A. Genetics & Cultural Competency Presentation.pptx
B. Facilitator's Guide.docx
C. Prediscussion Reading.docx
D. Discussion Handout.doc
E. Prediscussion Video.mp4
F. LGBT Reproduction and Cultural Attitudes Survey.docx
All appendices are peer reviewed as integral parts of the Original Publication.
Acknowledgements
With many thanks to experts such as Dr. Samuel Pang of the In-Vitro Fertilization New England and practitioners at Fenway Health such as Liz Coolidge, LMHC, Coordinator of the Alternative Insemination Program. We also thank the LGB couples who contributed their knowledge and experiences which helped develop this session.
Disclosures
None to report.
Funding/Support
Helen Jin reports grants from Boston University School of Medicine Medical Student Summer Research Program, during the conduct of the study.
Prior Presentations
H. Jin and S. Dasgupta. Cultural competency in medical genetics education: a discussion exploring LGBT assisted reproduction technology. Association of Professors of Human and Medical Genetics 21th Annual Workshop. Clearwater, FL. May 2015
Ethical Approval
This publication contains data obtained from human subjects and received ethical approval.
References
- 1.Stern HJ. Preimplantation genetic diagnosis: prenatal testing for embryos finally achieving its potential. J Clin Med. 2014;3(1):280–309. https://doi.org/10.3390/jcm3010280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gates GJ, Brown TNT. Marriage and same-sex couples after Obergefell. http://williamsinstitute.law.ucla.edu/wp-content/uploads/Marriage-and-Same-sex-Couples-after-Obergefell-November-2015.pdf Los Angeles, CA: Williams Institute, UCLA School of Law; 2015. [Google Scholar]
- 3.Gates GJ. Marriage and family: LGBT individuals and same-sex couples. Future Child. 2015;25(2):67–87. https://doi.org/10.1353/foc.2015.0013 [Google Scholar]
- 4.Amato P, Morton D. Lesbian health education: a survey of obstetrics and gynecology residency training programs. J Gay Lesbian Med Assoc. 2002;6:47–51. https://doi.org/10.1023/A:1021941405832 [Google Scholar]
- 5.Blake V. It's an art not a science: state-mandated insurance coverage of assisted reproductive technologies and legal implications for gay and unmarried persons. Minn J Law Sci Technol. 2011;12(2):651–713. [Google Scholar]
- 6.Ethics Committee of the American Society for Reproductive Medicine. Consideration of the gestational carrier: a committee opinion. Fertil Steril. 2013;99(7):1838–1841. https://doi.org/10.1016/j.fertnstert.2013.02.042 [DOI] [PubMed] [Google Scholar]
- 7.James-Abra S, Tarasoff LA, Green D, et al. Trans people's experiences with assisted reproduction services: a qualitative study. Hum Reprod. 2015;30(6):1365–1374. https://doi.org/10.1093/humrep/dev087 [DOI] [PubMed] [Google Scholar]
- 8.Stern JE, Cramer CP, Garrod A, Green RM. Attitudes on access to services at assisted reproductive technology clinics: comparisons with clinic policy. Fertil Steril. 2002;77(3):537–541. https://doi.org/10.1016/S0015-0282(01)03208-3 [DOI] [PubMed] [Google Scholar]
- 9.Jin H, Dasgupta S. Disparities between online assisted reproduction patient education for same-sex and heterosexual couples. Hum Reprod. 2016;31(10):2280–2284. https://doi.org/10.1093/humrep/dew182 [DOI] [PubMed] [Google Scholar]
- 10.Obedin-Maliver J, Goldsmith ES, Stewart L, et al. Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA. 2011;306(9):971–977. https://doi.org/10.1001/jama.2011.1255 [DOI] [PubMed] [Google Scholar]
- 11.Bakhai N, Ramos J, Gorfinkle N, et al. Introductory learning of inclusive sexual history taking: an e-lecture, standardized patient case, and facilitated debrief. MedEdPORTAL Publications. 2016;12:10520 https://doi.org/10.15766/mep_2374-8265.10520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gelman A, Amin P, Pletcher J, Fulmer V, Kukic A, Spagnoletti C. A standardized patient case: a teen questioning his/her sexuality is bullied at school. MedEdPORTAL Publications. 2014;10:9876 https://doi.org/10.15766/mep_2374-8265.9876 [Google Scholar]
- 13.Ross LE, Steele LS, Epstein R. Lesbian and bisexual women's recommendations for improving the provision of assisted reproductive technology services. Fertil Steril. 2006;86(3):735–738. https://doi.org/10.1016/j.fertnstert.2006.01.049 [DOI] [PubMed] [Google Scholar]
- 14.Ross LE, Tarasoff LA, Anderson S, Epstein R, Marvel S, Steele LS. Sexual and gender minority peoples' recommendations for assisted human reproduction services. J Obstet Gynaecol Can. 2014;36(2):146–153. https://doi.org/10.1016/S1701-2163(15)30661-7 [DOI] [PubMed] [Google Scholar]
- 15.Committee on Health Care for Underserved Women. Committee opinion number 525: health care for lesbians and bisexual women. Obstet Gynecol. 2012;119(5):1077–1080. https://doi.org/10.1097/AOG.0b013e3182564991 [DOI] [PubMed] [Google Scholar]
- 16.Eyler AE, Pang SC, Clark A. LGBT assisted reproduction: current practice and future possibilities. LGBT Health. 2014;1(3):151–156. https://doi.org/10.1089/lgbt.2014.0045 [DOI] [PubMed] [Google Scholar]
- 17.Dasgupta S, Tuttle K. Human genetic variation: a flipped classroom exercise in cultural competency. MedEdPORTAL Publications. 2013;9:9621 http://doi.org/10.15766/mep_2374-8265.9621 [Google Scholar]
- 18.Rui Z, Lian-rui X, Rong-zheng Y, Jing Z, Xue-hong W, Chuan Z. Friend or foe? flipped classroom for undergraduate electrocardiogram learning: a randomized controlled study. BMC Med Educ. 2017;17:53 https://doi.org/10.1186/s12909-017-0881-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tune JD, Sturek M, Basile DP. Flipped classroom model improves graduate student performance in cardiovascular, respiratory, and renal physiology. Adv Physiol Educ. 2013;37(4):316–320. https://doi.org/10.1152/advan.00091.2013 [DOI] [PubMed] [Google Scholar]
- 20.Vuma S, Sa B. Evaluation of the effectiveness of progressive disclosure questions as an assessment tool for knowledge and skills in a problem based learning setting among third year medical students at The University of The West Indies, Trinidad and Tobago. BMC Res Notes. 2015;8:673 https://doi.org/10.1186/s13104-015-1603-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nussbaum RL, McInnes RR, Willard HF. Genetic variation in individuals and populations: mutation and polymorphism. In: Nussbaum RL, McInnes RR, Willard HF, eds. Thompson and Thompson Genetics in Medicine. 7th ed. Philadelphia, PA: Elsevier; 2007:175–204. [Google Scholar]
- 22.Kelley L, Chou CL, Dibble SL, Robertson PA. A critical intervention in lesbian, gay, bisexual, and transgender health: knowledge and attitude outcomes among second-year medical students. Teach Learn Med. 2008;20(3):248–253. https://doi.org/10.1080/10401330802199567 [DOI] [PubMed] [Google Scholar]
- 23.National LGBT Health Education Center. Glossary of LGBT terms for health care teams. National LGBT Health Education Center Web site. https://www.lgbthealtheducation.org/wp-content/uploads/LGBT-Glossary_March2016.pdf Updated March 2016. Accessed June 10, 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A. Genetics & Cultural Competency Presentation.pptx
B. Facilitator's Guide.docx
C. Prediscussion Reading.docx
D. Discussion Handout.doc
E. Prediscussion Video.mp4
F. LGBT Reproduction and Cultural Attitudes Survey.docx
All appendices are peer reviewed as integral parts of the Original Publication.