Abstract
This paper examines community-based participatory research (CBPR) intervention approaches in promoting cancer-relevant outcomes for 102 Vietnamese women. Results indicated that the intervention was effective in promoting breast and cervical cancer knowledge, positive attitudes towards breast cancer screening, and breast cancer screening. Collectivism moderated the effect of the intervention on attitudes towards breast cancer screening. The intervention led to more favorable attitudes towards breast cancer screening for women with high levels of collectivism but not for women with low levels. Ethnic identity moderated the effect of the intervention on breast cancer screening: the intervention program led to higher probability of getting a clinical breast exam; however, this effect was more pronounced for women with low ethnic identity than for those with high ethnic identity. The study provides evidence for the effectiveness of culturally-tailored strategies in developing cancer screening interventions for the Vietnamese American population.
Keywords: Vietnamese-American, women, breast cancer, cervical cancer, ethnic identity, collectivism, community-based participatory research
The overall mission of Healthy People 2020 is to identify and address nationwide health priorities.1 An ovearching goal is to eliminate health disparities by establishing health equity for all Americans regardless of gender, race, ethnicity, sexual orientation, income, or educational status. A growing body of epidemiological literature suggests that Vietnamese women in the United States experience higher rates of cervical cancer incidence and mortality than White women and other ethnic minority women.2,3 In addition, Vietnamese women experience poorer breast and cervical cancer prognosis, and this is attributable to later stage diagnosis due to low rates of cancer screening.4,5 Though these cancer disparities may, in part, stem from structural barriers such as lack of insurance and access to care,6 sociocultural factors also likely contribute to disparate cancer outcomes for Vietnamese American women.7
The goal of the present study was to implement and evaluate an intervention program that would promote cancer screening knowledge, favorable attitudes towards screening, and screening behavior among Vietnamese American women. We were also interested in examining the potential moderating roles of cultural variables such as ethnic identity and collectivism on the intervention’s effects on cancer screening outcomes. This study was called Suc Khoe La Quan Trong Hon Sac Dep! (Health is Better than Beauty!), a Vietnamese proverb which describes the value placed on one’s health. The study enrolled 102 women in an intervention group or in a print material control group. In the intervention group, participants were exposed to information about female cancers and how and where to access Pap tests and clinical breast exams (CBE). Follow-up data were collected six months after the intervention session to determine whether or not there were longer-term intervention effects. In this study, the term Vietnamese Americans refers to Vietnamese women living in the United States whose ancestry is Vietnamese.
Conceptual frameworks.
Two conceptual frameworks, one methodological and one theoretical, were used to frame this study. Community-based participatory research (CBPR) methods were used to tailor our intervention for the Vietnamese female community by involving this community in the development of the intervention. Community-based participatory research is a collaborative partnership approach to research that combines the efforts of the researchers and stakeholders. These stakeholders are community members or organizational representatives.8 With respect to cancer screening promotion, CBPR has been successful in targeting diverse minority populations in raising knowledge and cancer screening behaviors.9–13
In addition, the Sociocultural Health Behavior Model (SHBM) provided rationale for the focus on cultural variables that may have impacted the intervention’s effects on cancer screening outcomes.14 According to the SHBM, predisposing, enabling, need, family/social support, environmental health systems, and cultural factors all influence health behaviors and outcomes. What distinguishes the SHBM model from other health behavior models is that this model acknowledges the primary role of cultural factors in impacting health behaviors. As a result, the present study examined potential moderating effects of cultural variables (i.e., ethnic identity and collectivism) on the intervention and cancer screening outcomes.
Ethnic identity.
Ethnic identity is the awareness and knowledge of one’s ethnic membership combined with values and attitudes shared by other members of one’s ethnic group.15 The development of ethnic identity for individuals involves reflection on feelings about being a member of an ethnic group and evaluations of that group membership.16 Research suggests that ethnic identity plays a role in promoting healthy practices among ethnic minority populations. Higher levels of ethnic identity may protect against risky health behaviors such as tobacco use, alcohol use, and marijuana use for ethnic minority individuals.17–19 In addition, there is preliminary evidence that ethnic identity may be associated with increased cancer screening.20 However, to our knowledge, there are no studies that have examined the role of ethnic identity in breast and cervical cancer screening behavior among Vietnamese American women.
The protective role of ethnic identity may operate through different mechanisms. Vietnamese women are at increased risk for cervical cancer in comparison with other Asian subgroups.2,3 Among Vietnamese women who are familiar with this knowledge, increased ethnic identity makes cancer risk salient and may motivate women to engage in cancer screening. In addition, ethnic identity promotes pride in ethnic group membership, and this may lead to increased contact and involvement with similar others in the community, resulting in increased exposure to health information and resources. Research suggests that increasing levels of ethnic identity were associated with increased community involvement, increased attendance at religious meetings, and increased psychological well-being among Chinese, Japanese, and Korean American men and women.21 The implications of this study are important as community involvement may help to connect Vietnamese women to health information and resources in the community.
Collectivism.
Members of Western cultures (e.g., U.S., England, and France) typically view the self as an independent being, whereas members of Eastern cultures (e.g., Japan, China, and Vietnam) view the self as an interdependent being.22 The collectivist orientation of Vietnamese culture provides a context in which people are seen within the family structure rather than as independent and autonomous individuals.23 People are expected to subordinate personal interests to those of the family or collective whole and to fulfill their duties to this larger unit.24 Because women in such cultures are expected to be primary caretakers of home, children, and husband,25 cultural values may influence these women’s motivation for maintaining health. We propose that collectivist orientation will predict positive cancer screening outcomes and may motivate Vietnamese women to adhere to screening. To our knowledge, no prior studies have examined the relationship between interdependent self-construals and cancer screening behaviors.
Our study hypotheses are:
Women in the intervention group will report higher increases in breast and cervical cancer screening variables (e.g., knowledge, attitudes, and actual screening behavior) from pretest to six-month follow-up than women in the control group.
Ethnic identity will be positively associated with cancer screening variables.
Collectivism will be positively associated with cancer screening variables.
Both ethnic identity and collectivism will moderate the intervention’s effects on cancer screening variables such that women who are high in both traits will experience the strongest changes after exposure to the intervention.
Methods
Design.
The study utilized a 2 (intervention vs. control) X 2 (baseline vs. follow-up) experimental design. The between-participants variable was the assignment into either the intervention group or the (print materials) control group. The within-participants variable was the time in which questionnaires were administered: baseline (pretest) or six-month follow-up. Potential participants were identified by community liaisons from two faith-based sites and were randomly assigned to the intervention or control condition.
Participants.
An estimated 1.7 million Vietnamese people reside in the U.S. and more than 40% of that population live in California.26 However, smaller pockets of Vietnamese people exist across the U.S. such as enclaves found in the greater Richmond metropolitan area in Virginia, where approximately 5,600 Vietnamese reside.27 One hundred and three Vietnamese American women from the Richmond metropolitan area were recruited to participate in the study.
Participant inclusion criteria.
Participants were required to be at least 18 years of age, to be female, and to self-identify as having a Vietnamese ethnic background. Recruitment targeted women from the ages of 18 and 70 due to the provided rationale: mammograms and clinical breast exams should be continued regardless of a woman’s age;28 however, women who are 65 years and older and who have had three or more consecutive normal Pap test results with no abnormal Pap test results in the last 10 years may choose to stop undergoing cervical cancer screening. As a result, women up to 70 years were recruited to allow for a larger inclusion of women for whom breast cancer screening is still appropriate. All women provided informed consent before participation. Women who reported a previous hysterectomy were eligible to participate, but their data were excluded from analyses that involved cervical cancer screening. As a result, data from eight women with previous hysterectomies were excluded where appropriate.
Materials
Intervention session
Findings from a previous study12 indicated low rates of English proficiency, acculturation, and knowledge of female cancer topics by the targeted female Vietnamese population. Therefore, it was important to have educational intervention materials in the Vietnamese language that were culturally appropriate. The health organization, Suc Khoe La Vang! (Health is Gold!), located on the West Coast, works with a Vietnamese population in prevention topics and was contacted for help with intervention materials. The current intervention used a modified form of the Vietnamese flip charts on female cancer topics used by Suc Khoe La Vang!29.
Participants in the intervention condition attended an educational session that lasted from two hours to two and a half hours. Women were exposed to information about breast and cervical cancer. The women were exposed to cancer-related information including clinical definitions, symptoms, treatment, cancer screening guidelines, and detection methods (e.g., Pap tests, clinical breast exams, mammograms, breast self-exams). After the presentation, women were given take-home booklets on breast and cervical cancer that were available in both English and Vietnamese. Also, women were given contact information for the organizations, clinics, and programs that offered Pap testing and CBEs to non-insured and low-income populations.
All materials used in the intervention session were previously used in a piloted study12 and reviewed by local community leaders and members to ensure that all materials were culturally appropriate and valid, easy to understand, and respectful. The intervention materials were available in both the English and Vietnamese language.
Control group session.
Participants in the control group were provided with printed materials of health-related information that was not related to breast or cervical cancer topics. This information focused on topics such as good nutrition, high blood pressure, smoking, and exercise. Materials were available in both English and Vietnamese.
Measures.
Demographic measures.
Participants provided their age which was measured in years. The following demographic items were measured with categorical response options (which are provided in parentheses): education (1 = some high school, 2 = high school graduate/GED equivalent, 3 = some college, 4 = college graduate, 5 = professional or graduate school training), marital status (1 = single, 2 = married, 3 = divorced, 4 = widowed), income (1 = <$10,000, 2 = $10,000– 15,000, 3 = $15,000– 25,000, 4 = $25,000– 50,000, 5 = $50,000– 75,000, 6 = >$75,000), employment (0 = No, 1 = Yes), health insurance (0 = No, 1 = Yes), whether or not they have a regular physician (0 = No, 1 = Yes), and previous receipt of a hysterectomy (0 = No, 1 = Yes).
Cancer screening awareness and knowledge.
Participants completed measures that assessed knowledge about the symptoms, treatment, cancer screening guidelines, and detection methods of breast and cervical cancer at baseline and follow-up. The 19-item multiple-choice measure included information covered in the curriculum (e.g., Cervical cancer is caused by ___).
Cancer screening attitudes.
Participants completed baseline and follow-up measures of attitudes towards breast and cervical cancer screening. This measure was based on a similar measure by Marteau and colleagues.30 This measure assessed attitudes towards Pap testing among a sample of smokers and non-smokers. Participants responded to the four-item measure (e.g., How important are regular Pap smears for women to remain healthy? How important are regular clinical breast exams for women to remain healthy?) using a Likert-response format (1 = not at all important and 7 = extremely important). Cronbach’s α for the overall scale was .79. Cronbach’s α for the attitudes towards Pap testing subscale scale was .73. Cronbach’s α for the attitudes towards clinical breast examination subscale scale was .82.
Cancer screening-related behavior.
Baseline rates of cancer screening behavior were obtained by asking participants if they have ever received a Pap test or CBE (e.g., Have you ever had a Pap test? Yes = 1 and No = 0) and whether they were up to date with their Pap tests or CBEs (e.g., Have you had a Pap test within the past year? Yes = 1 and No = 0). At follow-up, participants were asked if they had received a CBE or Pap test since the initial session).
Ethnic identity.
Ethnic identity was measured using the East Asian Ethnic Identity Scale.31 The original measure has 41 items. Items are offered in a seven-point Likert scale format where 1 = (strongly disagree), 4 = (neutral), and 7 = (strongly agree). The measure comprises three subscales: family values, ethnic pride, and interpersonal distance. Only the ethnic pride subscale was used in the present study (e.g., Being Vietnamese is an important part of who I am). The 13-item ethnic pride subscale measures ethnic pride, the perceived importance of maintaining one’s native language, and a sense of belonging. Cronbach’s α for the current study was .71.
Interdependency.
A measure of interdependency was used to assess collectivism. The interdependency scale was an adapted version of the Self-Construal Scale.32 The Self-Construal Scale is broken down into two subscales: an interdependent subscale and an independent subscale. Responses are made to a seven-point Likert scale format where 1 = (strongly disagree) and 7 = (strongly agree). Only the 11-item interdependent subscale was used in the current study. An example of an item is “It is important for me to maintain harmony within my group.” Cronbach’s α for the current study was .75.
Procedure.
Community-based participatory strategies.
Prior to discussing the procedure for implementing the intervention, we discuss how CBPR was employed in the current study beginning in 2008. CBPR has several steps. These include (1) developing partnerships and building trust, (2) assessing the community, (3) determining the intervention, (4) implementing the intervention, and (5) evaluating the intervention.33 We briefly summarize the progression of the program through these steps. However, it is worth noting that our community engagement and partnership started in 2005. We believe the present study utilizes a CBPR approach from its inception (from identifying and understanding the problems) to the delivery of the intervention. Refer to Nguyen, Belgrave, and Sholley12 for a fuller description of this process.
Developing partnerships and building trust.
In order to develop community ties and to foster capacity building, the principal investigator, a Vietnamese woman, volunteered to work with the Vietnamese community in several activities. These included helping with childcare, serving as a translator for non-insured women who visited local health clinics, and teaching Vietnamese cultural classes for children at the Buddhist community center.
Assessing the community.
In working with community liaisons from both faith-based communities, we initiated a series of discussions that addressed logistics and action plans. We worked out feasible timeframes, participant recruitment methods, and agreed on physical location, and session procedures.
Determining the intervention.
During program development, we consulted with community leaders and members to ensure the cultural appropriateness of the intervention materials (e.g., PowerPoint presentations, flip charts, questionnaires, and booklets/ pamphlets). Focus groups were conducting after piloting the intervention in order to receive feedback and suggestions from participants that led to modification and refinement of the intervention (e.g., changes in wording and order of presented information).
Implementing the intervention.
Community members who served as liaisons were trained to facilitate all components of the intervention and evaluation. Community members received training in presenting breast and cervical cancer topics, conducting follow-up focus group sessions, administrating and collecting questionnaires, and distributing health literature (e.g., pamphlets, booklets).
Evaluating the intervention.
Participants in the intervention group were asked to take part in focus groups that examined the women’s experiences related to the intervention at follow-up. The women were asked to share their perceptions on the effectiveness, strengths, weaknesses, and areas of needed improvement. We gathered feedback and disseminated published and unpublished data and reports to the community.
Study procedures.
The study obtained institutional review board (IRB) approval before initiation. After approval, participants were recruited with the help of community liaisons from the two faith-based sites, the Vietnamese Church of Martyrs and the Hue Quang Buddhist Temple. The community liaisons included both volunteer female teachers from the Hue Quang Vietnamese Language School and nuns from the Vietnamese Church of Martyrs. We relied on convenience sampling. During the recruitment phase, information about participation in the intervention program, referred to as a “study about health in the Vietnamese community,” was provided to the communities through church/temple bulletins and mass/service announcements. Interested members contacted community liaisons. Community liaisons also approached community members for recruitment.
Because intervention sessions were facilitated by either the investigator or by community members, community members were properly trained by the investigator to facilitate the sessions. On the day of the intervention, women in the intervention group were asked to meet in a conference room at the temple or church. They were greeted upon arrival and were asked to complete consent forms and then pre-test measures. Afterwards, they were invited to serve themselves dinner which consisted of a Vietnamese meal ordered from a local Vietnamese restaurant.
After the women had served themselves and were seated comfortably, facilitators and co-facilitators presented educational materials on breast and cervical cancer for about 30–35 minutes using a PowerPoint presentation. The women were then encouraged to express any concerns, ask questions, and discuss topics of interest based on the PowerPoint presentation. Women were also asked to discuss the perceived effectiveness and relevance of the intervention. The women were then thanked, provided monetary incentives, and provided print materials on breast and cervical cancer to take home. In addition, participants were presented with information on local providers who serve low-income and non-insured members.
Participants in the control group signed consent forms and then took the baseline questionnaire. Following a Vietnamese meal, they were provided with printed materials on general health topics, thanked for their time, and provided an incentive. Prior to participants in each group leaving, investigators confirmed contact information for follow-session with each participant.
Follow-up data were collected from women in both groups to determine whether or not there were longer-term gains in cancer-r elated knowledge, attitudes, and behavior. These sessions were conducted six months after convening the first session. Participants were asked whether they obtained a CBE or Pap since participation in the intervention/ control sessions. To assess potential contamination effects, participants were asked whether they had previously heard of any of the information from the intervention sessions. They were also asked about the nature of the information during debriefing. Some of the participants responded that they had friends who recommended that they participate in the study because of the beneficial knowledge that they had gained. However, none of the women responded that they heard any specific details of the educational sessions
Plan for data analysis.
Changes from pretest to follow-up session in cancer screening attitudes and knowledge were assessed by conducting hierarchical multiple regression. Preliminary analyses were conducted to screen data for outliers and to test assumptions for linear regression. Continuous predictors variables were centered to reduce non-essential multicollinearity and to increase interpretability of constants.
Age, education, household income, and health insurance status were used as covariates because of demonstrated associations with cancer screening variables in prior studies.34–39 These demographic traits were controlled for and entered in the first step of the model. Assignment into intervention conditions (intervention vs. control) and baseline measures of the outcome variable were also entered into the first step of the regression. Ethnic identity and collectivism were entered onto the second step of the model. Higher order interaction effects were entered in the third step. Logistic regression analyses were conducted for dichotomous cancer screening outcomes following identical blocking procedures as mentioned above. All models were tested for overall fit. Next, we assessed improvement of model fit by examining (1) tests of significance of R-square changes with the addition of each step to the regression model for continuous outcomes (i.e., knowledge and attitudes); and (2) comparisons of – 2 log likelihood values for dichotomous outcomes (i.e., cancer screening).
Results
Participant demographic characteristics.
There were a total of 103 Vietnamese American women in the study. Mean age of participants was 39 years (SD = 13.7). The minimum was 18 years while the maximum was 70 years. One participant was 78 years old, and because she exceeded the age limit set in the inclusion criteria, her data were excluded from the analyses, leaving a sample size of 102 participants. Out of 102 participants, 95 returned for the follow-up session.
With respect to education, 28% had some high school education, 25% had attained a high school diploma or equivalent (GED), 18% had some college education, 26% had a college degree, and 3% had post college/professional training. With respect to marital status, 25% were single, 66% were married, 6% were divorced, and 3% were widowed. In addition, 71% of the women had children. For additional information related to participants’ demographics, refer to Table 1.
Table 1.
PARTICIPANT DEMOGRAPHICS
| # | % | |
|---|---|---|
| Education | ||
| Some high school | 28 | 28 |
| High school graduate/ GED | 25 | 25 |
| Some college | 18 | 18 |
| College graduate | 26 | 26 |
| Post college graduate | 3 | 3 |
| Children | ||
| Yes | 72 | 71 |
| No | 30 | 29 |
| Household income | ||
| Less than $10,000 | 16 | 17 |
| $10,000–15,000 | 11 | 12 |
| $15,000–25,000 | 20 | 22 |
| $25,000–50,000 | 18 | 20 |
| $50,000–75,000 | 12 | 13 |
| Over $75,000 | 15 | 16 |
| Marital status | ||
| Single | 25 | 25 |
| Married | 67 | 66 |
| Divorced | 6 | 6 |
| Widowed | 3 | 3 |
| Employed | ||
| Yes | 72 | 72 |
| No | 28 | 28 |
| Regular physician | ||
| Yes | 61 | 61 |
| No | 39 | 39 |
| Health insurance | ||
| Yes | 70 | 70 |
| No | 30 | 30 |
Note: Numbers may not always add up to 102 due to missing responses.
Breast cancer knowledge.
A multiple regression analysis was conducted to assess the effect of the intervention on breast cancer knowledge while also examining potential demographic and cultural correlates following blocking procedures as described above. The results of the analysis indicated that the model accounted for a significant amount of variance in breast cancer knowledge at follow-up, F (10, 82) = 2.87, p = .004; R² = .26. Assignment into the intervention condition led to increased breast cancer knowledge from baseline to follow-up, β = .34, t(93) = 3.28, p = .002. Refer to Table 2 for predictor contributions.
Table 2.
FACTORS ASSOCIATED WITH CANCER KNOWLEDGE
| Breast Cancer Knowledge |
Cervical Cancer Knowledge |
|||||||
|---|---|---|---|---|---|---|---|---|
| Variable | β | B | SE B | 95% CI | β | B | SE B | 95% CI |
| Constant | 4.38 | 1.01 | 2.36, 6.40 | 5.07 | 0.87 | 3.34, 6.81 | ||
| Age (years) | −.10 | −.01 | .02 | −.05, .02 | −.11 | −.01 | .01 | −.04, .01 |
| Educational Attainment | .11 | .17 | .18 | −.18, .53 | .11 | .13 | .13 | −.13, .38 |
| Annual Household Income | −.14 | −.16 | .14 | −.44, .11 | .25* | .21* | .10 | .00, .41 |
| Health Insurance Status | .11 | .46 | .46 | −.46, 1.38 | −.06 | −17 | .33 | −.83, .48 |
| Intervention | .34** | 1.28** | .39 | .50, 2.05 | .40** | 1.08** | .29 | .50, 1.66 |
| Ethnic Identity | .06 | .01 | .04 | −.06, .08 | −.14 | −.02 | .03 | −.07, .03 |
| Collectivism | −.17 | −.05 | .04 | −.13, .04 | .20 | .04 | .03 | −.02, .10 |
| EI x Intervention | −.04 | −.01 | .05 | −.11, .08 | .14 | .03 | .04 | −.04, .10 |
| Collect x Intervention | .14 | .05 | .06 | −.06, .17 | −.14 | −.04 | .04 | −.12, .05 |
| R2 | .26 | .31 | ||||||
| F | 2.87* | 3.34** | ||||||
Note. N = 102.
p < .05
p < .01.
Cervical cancer knowledge.
A multiple regression analysis was conducted to assess the effect of the intervention on cervical cancer knowledge following identical procedures from the previous model. The results of the analysis indicated that the model accounted for a significant amount of variance in cervical cancer knowledge at follow-up, F (10, 74) = 3.34, p = .001; R² = .31. Assignment into the intervention condition led to increased cervical cancer knowledge from baseline to follow-up, β = .40, t(89) = 3.28, p = .002. In addition, household income predicted cervical cancer knowledge, β = .25, t(89) = –2 .90, p = .05. Higher levels of household income were associated with increased knowledge. Refer to Table 2 for predictor contributions.
Attitudes towards breast cancer screening.
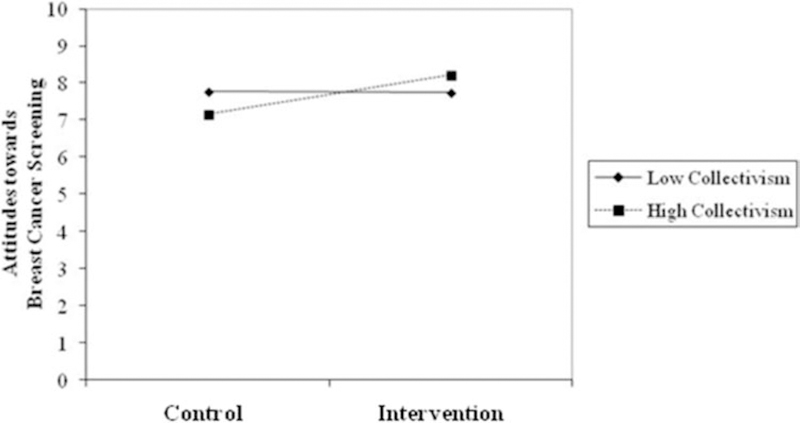
A multiple regression analysis was conducted to assess the effect of the intervention on attitudes towards breast cancer screening following identical procedures from the previous model. The results of the analysis indicated that the model accounted for a significant amount of variance in cervical cancer attitudes at follow-up, F (10, 82) = 3.17, p = .003; R² = .27. Assignment into the intervention condition led to more positive attitudes towards breast cancer screening from baseline to follow-up, β = .23, t(93) = 2.24, p = .03. Finally, collectivism significantly moderated the intervention’s effect on attitudes towards breast cancer screening, β = .37, t(93) = 2.31, p = .02. For women with higher levels of collectivism, the intervention led to more positive attitudes towards breast cancer screening from baseline to six-month follow-up; this relationship was not observed for women with lower levels of collectivism. Refer to Figure 1. Refer to Table 3 for predictor contributions.
Figure 1.
Moderating effect of collectivism on the intervention’s effect on attitudes towards breast cancer screening.
Table 3.
FACTORS ASSOCIATED WITH ATTITUDES TOWARDS CANCER SCREENING
| Breast Cancer |
Cervical Cancer |
|||||||
|---|---|---|---|---|---|---|---|---|
| Variable | β | B | SE B | 95% CI | β | B | SE B | 95% CI |
| Constant | 7.45 | 1.67 | 4.14, 10.77 | 9.77 | 0.97 | 7.85, 11.70 | ||
| Age (years) | −.17 | −.01 | .01 | −.03, .01 | −.11 | −.01 | .01 | −.03, .01 |
| Educational Attainment | −.04 | −.04 | .10 | −.24, .16 | .03 | .03 | .10 | −.17, .24 |
| Annual Household Income | −.09 | −.09 | .08 | −.23, .11 | −.09 | −.06 | .08 | −.22, .11 |
| Health Insurance Status | .28 | .69 | .27 | .15, 1.23 | .31* | .72* | .72* | .19, 1.26 |
| Intervention | .23* | .53* | .24 | .06, .99 | .11 | .23 | .23 | −.23, .69 |
| Ethnic Identity | .23 | .03 | .02 | .00, .07 | −.07 | −.01 | .02 | −.05, .03 |
| Collectivism | −.29 | −.05 | .03 | −.10, .01 | .03 | .01 | .03 | −.05, .06 |
| EI x Intervention | −.08 | −.02 | .03 | −.07, .04 | .17 | .03 | .03 | −.02, .09 |
| Collect x Intervention | .34* | .08* | .04 | −.06, .17 | .12 | .03 | .04 | −.05, .10 |
| R2 | .27 | .29 | ||||||
| F(change in R2) | 3.03** | 2.95** | ||||||
Note. N = 102.
p < .05
p < .01.
Attitudes towards cervical cancer screening.
A multiple regression analysis was conducted to assess the effect of the intervention on attitudes towards cervical cancer screening following identical procedures from the previous model. The results of the analysis indicated that the model accounted for a significant amount of variance in attitudes towards cervical cancer screening at follow-up, F (10, 74) = 2.95, p = .004; R² = .29. Assignment into the intervention condition did not lead to significantly more positive attitudes towards cervical cancer screening from baseline to follow-up, β = .11, t(89) = 1.01, p = .32. Having health insurance was associated with more positive attitudes towards screening, β = .31, t(89) = 2.71, p = .01. Refer to Table 3 for predictor contributions.
Receipt of a clinical breast exam.
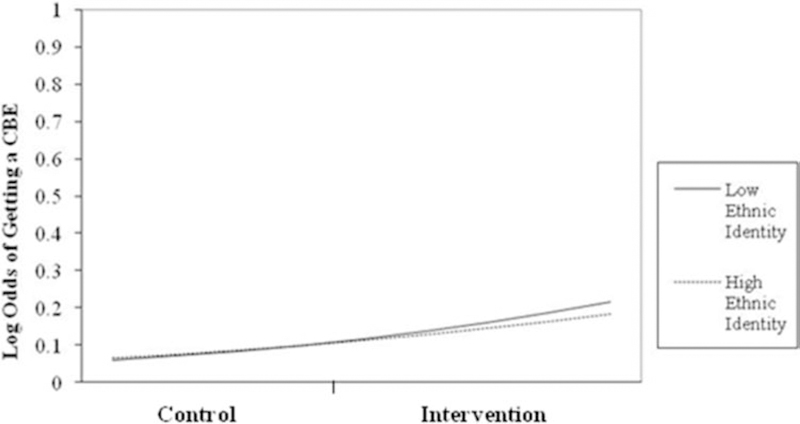
A logistic regression analysis was conducted to assess the effect of the intervention on receipt of a clinical breast exam following identical procedures from the previous model. The model was significant, χ²(10) = 27.24, p = .002. The Nagelkerke R-square value = .36 and the Cox and Snell R-square value = .25. The variables were associated with 74% of the women who had received a CBE. The Hosmer and Lemeshow Test was non-significant, χ²(8) = 5.68, p = .68, indicating that the model did not differ from the observed data and was a good fit. According to the Wald criterion, assignment into the intervention condition led to higher odds of getting a CBE by the six-month follow-up, β = 1.31, χ²(1) = 4.50, p = .03. The change in odds associated with assignment into the intervention condition was 1.10. Ethnic identity significantly moderated the effect of the intervention on the odds of getting a CBE by six-month follow-up, β = – .16, χ²(1) = 3.51, p = .05. Enrollment in the intervention program led to higher probability of getting a CBE; however, this effect was more pronounced for women with low ethnic identity than for those with high ethnic identity. Refer to Figure 2. Refer to Table 4 for predictor contributions.
Figure 2.
Moderating effect of ethnic identity on the intervention’s effect on receipt of a CBE (Clinical Breast Exam).
Table 4.
FACTORS ASSOCIATED WITH PREVIOUS RECEIPT OF A CBE
| Variable | β | SE B | WALD | EXP(B) | 95% CI |
|---|---|---|---|---|---|
| Constant | −2.73 | 1.40 | 3.80 | .07 | |
| Age (years) | .01 | .03 | .10 | 1.01 | .96, 1.06 |
| Educational Attainment | .08 | .25 | .11 | 1.09 | .66, 1,78 |
| Annual Household Income | −.07 | .22 | .10 | .93 | .60, 1.44 |
| Health Insurance Status | .01 | .73 | .00 | 1.00 | .24, 4.22 |
| Intervention | 1.31* | .62* | 4.50 | 3.69 | 1.10, 12.32 |
| Ethnic Identity | .06 | .07 | .80 | 1.07 | .93, 1.22 |
| Collectivism | .16 | .09 | 2.98 | 1.17 | .98, 1.40 |
| EI x Intervention | −.16* | .09* | 3.51 | .85 | .72, 1.00 |
| Collect x Intervention | −.06 | .11 | .31 | .94 | .76, 1.16 |
| Nagelkirke R2 | .36 | ||||
| Cox and Snell R2 | .25 | ||||
| χ2 | 27.24** | ||||
| % Cases Predicted | 74 |
Note. N = 102.
p < .05
p < .01.
Receipt of a Pap test.
A logistic regression analysis was conducted to assess the effect of the intervention on receipt of a Pap test following identical procedures from the previous model. The model was not significant (χ²(8) = 13.80, p = .09. The Nagelkerke R-square value = .21 and the Cox and Snell R-square value = .15). The variables were associated with 66% of the women who had received a Pap test.
Discussion
Our overall goal in this study was to increase cancer screening among Vietnamese American women as they (1) engage in less cancer screening than women from other ethnic and racial groups, and (2) experience higher cervical and breast cancer incidence and worse prognosis. The intervention was effective in increasing breast and cervical cancer knowledge, positive attitudes towards breast cancer screening, and CBE screening from baseline to a six-month follow-up for a female Vietnamese community sample. Our findings support the effectiveness of CBPR in health promotion among ethnic minority populations consistent with previous literature. 9,10,13,40 Identifying and training individuals who are trusted within the community are essential when developing interventions appropriate for the target population.9,41 The partnerships that were fostered between the researcher, community liaisons, and community members were vital in the legitimacy and acceptance of the intervention and crucial in the development, implementation, and evaluation of the program.
The study’s findings indicate that increased levels of household income were associated with increased cervical cancer knowledge, and possession of health insurance was associated with more positive attitudes towards cervical cancer screening. Income and health insurance status constitute enabling factors; they enable individuals to access health information and cancer screening services due to higher levels of financial resource.36 In addition, poor and uninsured ethnic minority individuals are more likely to perceive racial and ethnic bias in the health care setting.42 This increased distrust of health professionals may obstruct ethnic minority individuals from seeking health information and services. Providing health insurance for the uninsured may help reduce this perceived bias among some minority groups and increase adherence to screening guidelines.
It is possible that gendered divisions of labor in traditional collectivist societies and expectations of the subordination of personal needs serve as barriers to Vietnamese women’s personal health care. However, the findings of study suggest that the collectivist orientation of Vietnamese women may not necessarily preclude them from engaging in prevention and screening behaviors. Collectivism significantly moderated the intervention’s effect on attitudes towards breast cancer screening. For women with high collectivism scores, the intervention led to more positive attitudes towards breast cancer screening from baseline to six-month follow-up; this relationship was not observed for women with low collectivism scores. Because women from collectivist cultures are expected to be primarily responsible for taking care of the home and the children,25 Vietnamese women may feel responsible for taking care of their own health in order to care for their husband and children. As a result, Vietnamese women high in collectivism may have positive attitudes towards cancer screening as it may help them maintain their health in order to help others who depend on them.
Ethnic identity significantly moderated the effect of the intervention on the odds of getting a CBE by six-month follow-up. However, the results run contrary to our initial hypothesis in which we predicted that ethnic identity would be positively associated with cancer screening variables. Enrollment in the intervention program led to higher probability of getting a CBE; however, this effect was more pronounced for women with low ethnic identity than for those with high ethnic identity. We offer two possible explanations. First, women with high ethnic identify may rely on different cultural frameworks than women with low ethnic identity. Traditional cultural frameworks guide the interpretation of health and illness and influence cognition, beliefs, and attitudes towards preventive health. The role of the stigmatization of cancer, cultural taboos with strangers touching women’s bodies during screening, and fatalistic beliefs of cancer diagnoses may contribute to the unwillingness of Vietnamese women to engage in cancer screening.43,44 A second explanation involves the role of acculturation. Women who are low in ethnic identity may be high in acculturation, and research has shown that highly acculturated Asian women are more likely to undergo cancer-screening than women who are less acculturated.45–47 However, it is worth noting that acculturation and ethnic identity are orthogonal constructs.48–51 A study by Li suggested that Asian Americans who were born in the U.S. may attribute substantial importance to their ethnic Asian identity and their national American identity, the parts together constituting a type of bicultural identity.51 It is entirely possible that there are lower levels of acculturation within this particular immigrant sample as the Vietnamese immigrated to the U.S. post the Fall of Saigon in 1975. Future should elucidate the relationship between traditional cultural frameworks of health and illness, cultural identity, and health cognitions and behaviors.
Strengths and limitations.
The current study provides contributions in several ways. First, research conducted in the United States on Vietnamese women and cancer screening has been limited. Research that has been conducted has primarily focused on populations located on the West Coast.11,41,52,53 There is a paucity of research on Vietnamese populations in other geographic areas. This study contributes to the literature by examining the health behaviors and beliefs of Vietnamese women on the Southeastern Coast. The experience of Vietnamese on the West Coast (e.g., California) may be atypical for Vietnamese immigrants as many do not live in communities in which a high percentage of their neighbors are also Vietnamese54. The smaller Vietnamese population in a southern mid-sized city such as Richmond may lead to smaller Vietnamese enclaves. It is important to understand the experiences of ethnic minority individuals from divergent communities and geographical locations.
In addition, typical cancer screening interventions do not focus on the influence of cultural variables on health behaviors. The present study contributes to the literature by examining proximal-level cultural orientations and their potential role in motivating women to engage in cancer screening. For example, the collectivist orientation of Vietnamese culture provides a context in which people are seen within the family structure rather than independent and autonomous individuals.22,23 This study’s findings provides initial support for the way in which Vietnamese women’s caretaking roles and the dependence of others can be leveraged as motivators to engage in cancer screening behaviors.
Limitations include a small sample size and a short follow-up period (six months). Reliance on self-report measures of breast and cervical cancer screening also potentially raise issues related to recall error and social desirability. However, studies of the accuracy of self-reported cancer screening procedures suggest that there is relatively high agreement with actual behavior55–57. Still, to ensure accuracy, future studies could request participants to bring documentation or proof of their screening test at follow-up and provide incentives for doing so. In addition, the reliance on faith-based communities in which to recruit participants may have limited potential health intervention topics. For example, there may be stigma related to cervical cancer because of the association with sexual transmission of HPV. However, the emphasis on cancer and illness provides routes for potential acceptance of the topics. On the other hand, it may be difficult for interventions addressing topics such as HIV/AIDS and risky sexual behavior to find acceptance and legitimacy in Vietnamese faith-based communities.
Conclusion.
This study provides initial support for the application of CBPR in developing cancer screening interventions for the Vietnamese population. Health and illness should never be decontextualized as cultural beliefs and values are manifested in the way illness and disease is interpreted and treated.43,44 Multicultural competence underscores the importance of intervention researchers developing knowledge of the ethnic minority population with whom they collaborate. When working with ethnic groups, it is essential for the researcher to have an understanding of the different immigration experiences, history of the group’s experience with institutional and cultural racism, as well as cultural beliefs, practices, and values. Only when we are equipped with knowledge and compassion, are we able to effectively promote health in collaboration with the community.
Acknowledgments
This study was supported by a Ruth L. Kirschstein National Research Service Award (Grant #5F31CA136235) to the first author from the National Cancer Institute. The authors wish to express their gratitude to the women who participated in this study, to the nuns at the Vietnamese Church of Martyrs, and to the teachers at Hue Quang Buddhist Temple for their invaluable support and work.
Contributor Information
Anh B. Nguyen, Behavioral Research Program, Division of Cancer Control & Population Sciences, at the National Cancer Institute, Rockville, MD.
Faye Z. Belgrave, Department of Psychology, at Virginia Commonwealth University, Richmond, VA..
Notes
- 1.U.S. Department of Health and Human Services. Healthy people 2020 framework Washington, DC: Office of Disease Prevention and Health Promotion, 2012. [Google Scholar]
- 2.McCracken M, Olsen M, Chen MS Jr, et al. Cancer incidence, mortality, and associated risk factors among Asian Americans of Chinese, Filipino, Vietnamese, Korean, and Japanese ethnicities. CA Cancer J Clin 2007. Jul-Aug;57(4):190–205. 10.3322/canjclin.57.4.190 [DOI] [PubMed] [Google Scholar]
- 3.Miller BA, Chu KC, Hankey BF, et al. Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations in the U.S. Cancer Causes Control 2008. April;19(3):227–56. Epub 2007 Nov 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kagawa-Singer M, Pourat N, Breen N, et al. Breast and cervical cancer screening rates of subgroups of Asian American women in California. Med Care Res Rev 2007. December;64(6):706–30. Epub 2007 Sep 5. 10.1177/1077558707304638 [DOI] [PubMed] [Google Scholar]
- 5.Ma GX, Shive SE, Wang MQ, et al. Cancer screening behaviors and barriers in Asian Americans. Am J Health Behav 2009. Nov-Dec;33(6):650–60. 10.5993/AJHB.33.6.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pourat N, Kagawa-Singer M, Breen N, et al. Access versus acculturation: identifying modifiable factors to promote cancer screening among Asian American women. Med Care 2010. December;48(12):1088–96. [DOI] [PubMed] [Google Scholar]
- 7.Ma GX, Gao W, Lee S, et al. Health seeking behavioral analysis associated with breast cancer screening among Asian American women. Int J Womens Health 2012;4:235–43. Epub 2012 May 25. 10.2147/IJWH.S30738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Israel BA, Schulz AJ, Parker EA, et al. Community-based participatory research: policy recommendations for promoting a partnership approach in health research. Educ Health (Abingdon) 2001;14(2):182–97. 10.1080/13576280110051055 [DOI] [PubMed] [Google Scholar]
- 9.Beck B, Young S, Ahmed S, et al. Development of a church-based cancer education curriculum using CBPR. J Health Care Poor Underserved 2007. February;18(1):28–34. 10.1353/hpu.2007.0003 [DOI] [PubMed] [Google Scholar]
- 10.Hughes HC, Weathers B, Delmoor E. Developing an academic-community partnership for research in prostate cancer. J Cancer Educ 2006. Summer;21(2):99–103. 10.1207/s15430154jce2102_13 [DOI] [PubMed] [Google Scholar]
- 11.Nguyen TT, McPhee SJ, Bui-Tong N, et al. Community-based participatory research increases cervical cancer screening among Vietnamese-Americans. J Health Car Poor Underserved 2006. May;17(2 Suppl):31–54. 10.1353/hpu.2006.0078 [DOI] [PubMed] [Google Scholar]
- 12.Nguyen AB, Belgrave FZ, Sholley BK. Development of a breast and cervical cancer screening intervention for Vietnamese American women: a community-based participatory approach. Health Promot Pract 2011. November;12(6):876–86. Epub 2010 jun 8. 10.1177/1524839909355518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith A, Christopher S, McCormick AKHG. Development and implementation of a culturally sensitive cervical health survey: a community-based participatory approach. Women Health 2004;40(2):67–86. 10.1300/J013v40n02_05 [DOI] [PubMed] [Google Scholar]
- 14.Ma GX, Shive SE, Gao W, et al. Prostate cancer screening among chinese american men: a structural model. Ame J Health Behav 2012. July;36(4):495–504. 10.5993/AJHB.36.4.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Phinney JS, Chavira V. Ethnic identity and self-esteem: an exploratory longitudinal study. J Adolesc 1992. September;15(3):271–81. 10.1016/0140-1971(92)90030-9 [DOI] [PubMed] [Google Scholar]
- 16.Phinney JS. Ethnic identity and acculturation: advances in theory, measurement, and applied research Washington, DC: American Psychological Association, 2003. [Google Scholar]
- 17.Belgrave FZ, Townsend TG, Cherry VR, et al. The influence of an Africentric world-view and demographic variables on drug knowledge, attitudes, and use among African American youth. J Community Psychol 1997. September;25(5):421–33. [DOI] [Google Scholar]
- 18.Brook JS, Duan T, Brook DW, et al. Pathways to nicotine dependence in African American and Puerto Rican young adults. Am J Addict 2007. Nov-Dec;16(6):450–6. 10.1080/10550490701641132 [DOI] [PubMed] [Google Scholar]
- 19.Love AS, Yin Z, Codina E, et al. Ethnic identity and risky health behaviors in school-age Mexican-American children. Psychol Rep 2006. June;98(3):735–44. 10.2466/pr0.98.3.735-744 [DOI] [PubMed] [Google Scholar]
- 20.Bowen DJ, Singal R, Eng E, et al. Jewish identity and intentions to obtain breast cancer screening. Cultur Divers Ethnic Minor Psychol 2003. February;9(1):79–87. 10.1037/1099-9809.9.1.79 [DOI] [PubMed] [Google Scholar]
- 21.Chae MH, Foley PF. Relationship of ethnic identity, acculturation, and psychological well-being among Chinese, Japanese, and Korean Americans. Journal of Counseling & Development 2010. Fall;88(4):466–76. 10.1002/j.1556-6678.2010.tb00047.x [DOI] [Google Scholar]
- 22.Triandis HC. Individualism and collectivism San Francisco, CA: Westview Press, 1995. [Google Scholar]
- 23.Chung RC-Y, Bemak F. Lifestyle of Vietnamese refugee women. J Individual Psychol 1998;54:373–84. [Google Scholar]
- 24.Bich PV. The Vietnamese family in change: the case of the Red River Delta Padstow, Cornwall: Curzon Press, 1999. [Google Scholar]
- 25.Davis RE. The convergence of health and family in the Vietnamese culture. J Family Nursing 2000. May;6(2):136–56. 10.1177/107484070000600204 [DOI] [Google Scholar]
- 26.Terrazas A, Batog C. Vietnamese Immigrants in the United States Washington, DC: Migration Policy Institute, 2013. [Google Scholar]
- 27.U.S. Census Bureau. 2010 census, summary File 1, Asian alone or in combination with one or more other races, and with one or more Asian categories for selected groups Washington, DC: U.S. Census Bureau, 2011. [Google Scholar]
- 28.American Cancer Society. American Cancer Society guidelines for the early detection of cancer Atlanta, GA: American Cancer Society, 2012. [Google Scholar]
- 29.Bird JA, McPhee SJ, Ha NT, et al. Opening pathways to cancer screening for Vietnamese-American women: lay health workers hold a key. Prev Med 1998. Nov-Dec;27(6):821–9. 10.1006/pmed.1998.0365 [DOI] [PubMed] [Google Scholar]
- 30.Marteau TM, Hankins M, Collins B. Perceptions of risk of cervical cancer and attitudes towards cervical screening: a comparison of smokers and non-smokers. Fam Pract 2002. February;19(1):18–22. 10.1093/fampra/19.1.18 [DOI] [PubMed] [Google Scholar]
- 31.Barry DT. An ethnic identity scale for East Asian immigrants. J Immigr Health 2002. April;4(2):87–94. 10.1023/A:1014598509380 [DOI] [PubMed] [Google Scholar]
- 32.Singelis TM. The measurement of independent and interdependent self-construals. Personality Social Psychology Bulletin 1994. October;20(5):580–91. 10.1177/0146167294205014 [DOI] [Google Scholar]
- 33.Minkler M, Wallerstein N. Community-based participatory research for health San Francisco, CA: Jossey-Bass, 2003. [Google Scholar]
- 34.Benyamini Y, Blumstein T, Boyko V, et al. Cultural and educational disparities in the use of primary and preventive health care services among midlife women in Israel. Womens Health Issues 2008. Jul-Aug;18(4):257–66. Epub 2008 Mar 10. 10.1016/j.whi.2007.12.009 [DOI] [PubMed] [Google Scholar]
- 35.Couture MC, Nguyen CT, Alvarado BE, et al. Inequalities in breast and cervical cancer screening among urban Mexican women. Prev Med 2008. November;47(5):471–6. Epub 2008 Jul 15. 10.1016/j.ypmed.2008.07.005 [DOI] [PubMed] [Google Scholar]
- 36.DeNavas-W alt C, Proctor BD, Smith JC. Income, poverty, and health insurance coverage in the United States: 2007 Washington, DC: U. S. Department of Commerce, 2008. [Google Scholar]
- 37.Ho V, Yamal JM, Atkinson EN, Basen-Engquist K, et al. Predictors of breast and cervical screening in Vietnamese women in Harris County, Houston, Texas. Cancer Nurs 2005. Mar-Apr;28(2):119–29. 10.1097/00002820-200503000-00005 [DOI] [PubMed] [Google Scholar]
- 38.Meissner HI, Yabroff KR, Dodd KW, et al. Are patterns of health behavior associated with cancer screening? Am J Health Promot 2009. Jan-Feb;23(3):168–75. 10.4278/ajhp.07082085 [DOI] [PubMed] [Google Scholar]
- 39.Taylor VM, Yasui Y, Nguyen TT, et al. Pap smear receipt among Vietnamese immigrants: the importance of health care factors. Ethn Health 2009. December;14(6):575–89. 10.1080/13557850903111589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Powell ME, Carter V, Bonsi E, et al. Increasing mammography screening among African American women in rural areas. J Health Care Poor Underserved 2005. November;16(4 Suppl A):11–21. 10.1353/hpu.2005.0071 [DOI] [PubMed] [Google Scholar]
- 41.Mock J, Nguyen T, Nguyen KH, et al. Processes and capacity-building benefits of lay health worker outreach focused on preventing cervical cancer among Vietnamese. Health Promot Pract 2006. July;7(3 Suppl):223S–32S. Epub 2006 Jun 7. 10.1177/1524839906288695 [DOI] [PubMed] [Google Scholar]
- 42.Stepanikova I, Cook KS. Effects of poverty and lack of insurance on perceptions of racial and ethnic bias in health care. Health Serv Res 2008. June;43(3):915–30. 10.1111/j.1475-6773.2007.00816.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Donnelly TT. The health-care practices of Vietnamese-Canadian women: cultural influences on breast and cervical cancer screening. Can J Nurs Res 2006. March;38(1):82–101. [PubMed] [Google Scholar]
- 44.Ma GX, Fang CY, Feng Z, et al. Correlates of cervical cancer screening among Vietnamese American women. Infect Dis Obstet Gynecol 2012;2012:617234 Epub 2012 Sep 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tang TS, Solomon LJ, Yeh CJ, et al. The role of cultural variables in breast self-examination and cervical cancer screening behavior in young Asian women living in the United States. J Behav Med 1999. October;22(5):419–36. 10.1023/A:1018653306776 [DOI] [PubMed] [Google Scholar]
- 46.Tang TS, Solomon LJ, McCracken LM. Cultural barriers to mammography, clinical breast exam and breast self-exam among Chinese-American women 60 and older. Prev Med 2000. November;31(5):575–83. 10.1006/pmed.2000.0753 [DOI] [PubMed] [Google Scholar]
- 47.Yi JK, Reyes-Gibby CC. Breast cancer screening practices among low-income Vietnamese women. Int Quarter Community Health Educ 2002;21(1):41–9. [Google Scholar]
- 48.Costigan CL, Su TF. Orthogonal versus linear models of acculturation among immigrant Chinese Canadians: acomparison of mothers, fathers, and children. Int J Behav Develop 2004. November;28(6):518–27. 10.1080/01650250444000234 [DOI] [Google Scholar]
- 49.Johnson ML, Wall TL, Guanipa C, et al. The psychometric properties of the orthogonal cultural identification scale in Asian Americans. J Multicultural Counseling Develop 2002. July;30(3):181–90. 10.1002/j.2161-1912.2002.tb00490.x [DOI] [Google Scholar]
- 50.Leong FTL, Chou EL. The role of ethnic identity and acculturation in the vocational behavior of Asian Americans: an integrative review. J Vocational Behav 1994. April;44(2):155–72. 10.1006/jvbe.1994.1011 [DOI] [Google Scholar]
- 51.Gong L Ethnic identity and identification with the majority group: relations with national identity and self-esteem. Int J Intercultural Relations 2007. July;31(4):503–23. 10.1016/j.ijintrel.2007.03.002 [DOI] [Google Scholar]
- 52.De Alba I, Ngo-Metzger Q, Sweningson JM, et al. Pap smear use in California: are we closing the racial/ethnic gap? Prev Med 2005. June;40(6):747–55. 10.1016/j.ypmed.2004.09.018 [DOI] [PubMed] [Google Scholar]
- 53.Tung WC, Nguyen DH, Tran DN. Applying the transtheoretical model to cervical cancer screening in Vietnamese-American women. Int Nurs Rev 2008. March;55(1):73–80. 10.1111/j.1466-7657.2007.00602.x [DOI] [PubMed] [Google Scholar]
- 54.D’Andrade R A study of personal and cultural values: American, Japanese, and Vietnamese New York, NY: Palgrave Macmillan, 2008. 10.1057/9780230612099 [DOI] [Google Scholar]
- 55.Caplan LS, McQueen DV, Qualters JR, et al. Validity of women’s self-reports of cancer screening test utilization in a managed care population. Cancer Epidemiol Biomarkers Prev 2003. November;12(11 pt 1):1182–7. [PubMed] [Google Scholar]
- 56.McGovern PG, Lurie N, Margolis KL, et al. Accuracy of self-report of mammography and Pap smear in a low-income urban population. Am J Prev Med 1998. April;14(3):201–8. 10.1016/S0749-3797(97)00076-7 [DOI] [PubMed] [Google Scholar]
- 57.Thompson B, Taylor V, Goldberg H, et al. Mammography status using patient self-reports and computerized radiology database. Am J Prev Med 1999. October;17(3):203–6. 10.1016/S0749-3797(99)00068-9 [DOI] [PubMed] [Google Scholar]