Overview
Introduction
We describe a new technique for treating traumatic brachial plexus avulsion injury with a contralateral C7 nerve transfer with direct coaptation that shortens the time to muscle reinnervation.
Step 1: Explore the Injured Brachial Plexus
Explore the brachial plexus carefully and confirm the nerve-root avulsion injuries from C7 to T1.
Step 2: Harvest the Contralateral C7 Nerve
Dissect the divisions of the contralateral C7 nerve root, divide the nerve at the junction between the divisions and cords, and mobilize it proximally.
Step 3: Create the Prespinal Route
Create the prespinal route to guide the contralateral C7 nerve to the injured side.
Step 4: Humeral Shortening Osteotomy
If the contralateral C7 nerve does not reach the injured lower trunk, perform a humeral shortening osteotomy, generally with <5 cm of shortening in adults.
Step 5: Neurorrhaphy
Suture one end of the sural nerve together with the medial antebrachial cutaneous nerve to the musculocutaneous nerve; anastomose the remainder of the contralateral C7 nerve directly with the lower trunk.
Step 6: Postoperative Care
Use a prefabricated brace to hold the head in the neutral position and immobilize the injured limb for six weeks.

Results
We evaluated the results of the technique in a study of seventy men and five women with a mean age (and standard deviation) of 28 ± 10 years (range, ten to fifty-three years).
Introduction
We describe a new technique for treating traumatic brachial plexus avulsion injury with a contralateral C7 nerve transfer with direct coaptation that shortens the time to muscle reinnervation.
In patients with a total brachial plexus avulsion injury, the contralateral C7 nerve, which provides sufficient myelinated axons, has been used as a donor nerve to repair the injured median nerve. The results of using this technique for restoration of finger flexion have been unsatisfactory, mainly due to the long length of the interpositional nerve graft (placed via the subcutaneous route), which is associated with an extended time for nerve regeneration that inevitably results in irreversible muscle atrophy. To improve the results of finger-flexion reconstruction, we designed a new contralateral C7 nerve transfer procedure that is performed via a shorter, modified prespinal route with direct coaptation of the contralateral C7 nerve to the lower trunk to restore finger flexion, thereby shortening the time to reinnervation of the target muscle. The contralateral C7 nerve is also transferred to the musculocutaneous nerve with interpositional bridging by the medial antebrachial cutaneous nerve arising from the lower trunk.
The procedure is performed with the following steps.
Step 1: Explore the Injured Brachial Plexus
Explore the brachial plexus carefully and confirm the nerve-root avulsion injuries from C7 to T1.
Perform a transverse incision about 2 cm above the clavicle. Expose the upper, middle, and lower trunks completely. Explore the brachial plexus carefully and confirm the nerve-root avulsion injuries from C7 to T1.
Expose the infraclavicular brachial plexus through a deltopectoral approach. Begin the incision from the midpoint of the clavicle and along the deltopectoral groove down to the anterior aspect of the arm, extend it to the medial side, and end it at the midpoint level of the arm. Mobilize the cephalic vein and retract it laterally. Release the insertions of the pectoralis major and minor, leaving a small cuff of tendon behind and tagging it for later repair.
Identify the median nerve, ulnar nerve, and medial antebrachial cutaneous nerve at the medial intermuscular septum of the arm and dissect them proximally to the axilla. Identify the medial cord, lateral cord, and posterior cord. Cut the medial pectoral nerve and the medial brachial cutaneous nerve from its origin on the medial cord. Free the ulnar nerve, medial cord of the median nerve, and medial antebrachial cutaneous nerve to the lower trunk, and cut the posterior division of the lower trunk, allowing the lower trunk to be fully mobilized proximally.
Release the ulnar nerve through the cubital tunnel, and move it anteriorly to a subcutaneous position, allowing it to be fully mobilized proximally. Divide the musculocutaneous nerve at its origin and the medial antebrachial cutaneous nerve above the elbow, making the distal end of the medial antebrachial cutaneous nerve close to the distal end of the musculocutaneous nerve, which is then used to repair the musculocutaneous nerve.
Step 2: Harvest the Contralateral C7 Nerve
Dissect the divisions of the contralateral C7 nerve root, divide the nerve at the junction between the divisions and cords, and mobilize it proximally.
Make a supraclavicular transverse incision on the contralateral side. Identify the contralateral C7 nerve root and dissect its anterior and posterior divisions distally as far as possible. Identify the branch that contributes to the lateral pectoral nerve arising from the anterior division of the contralateral C7. Divide the contralateral C7 at the junction between the divisions and cords, and then mobilize it proximally up to the neuroforamina.
Step 3: Create the Prespinal Route
Create the prespinal route to guide the contralateral C7 nerve to the injured side (Videos 1 and 2).
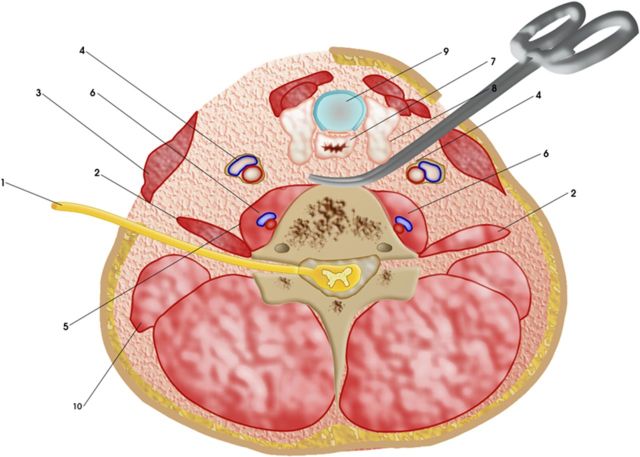
Extend the supraclavicular incision on the injured side to the medial border of the sternocleidomastoid muscle. Dissect longitudinally along its medial border and retract laterally. Expose the carotid sheath and trachea. Expose the anterior vertebrae while retracting the carotid sheath laterally and the esophagus medially. Create a retro-esophageal space by blunt dissection under direct vision (Fig. 1).
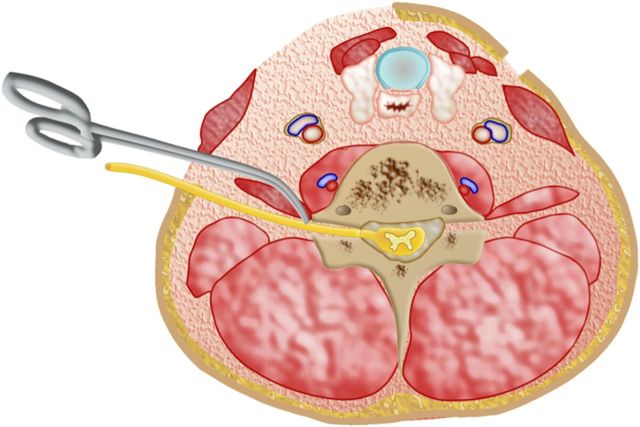
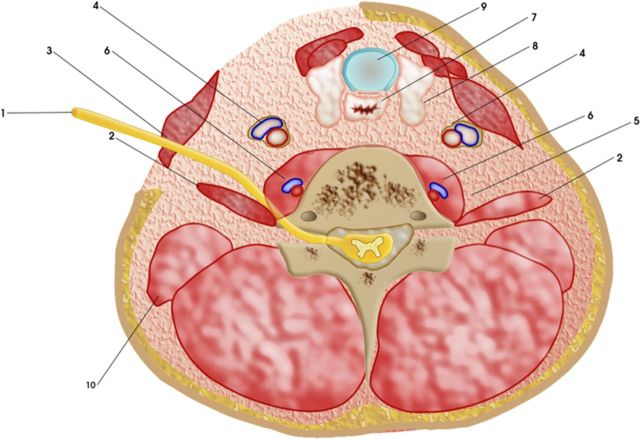
On the contralateral, uninjured side, dissect the anterior aspect of the scalenus anterior muscle to its medial margin. Place the tip of a forceps anterior to the junction of the scalenus anterior muscle origin with the C6 transverse process. Using the forceps, penetrate the scalenus anterior muscle until the contralateral C7 nerve root just emerges from the intervertebral foramen (Fig. 2). Mobilize the contralateral C7 nerve root to the anterior aspect of the scalenus anterior muscle (Fig. 3). Then dissect the anterior aspect of the longus colli muscle bluntly and divide it transversely (be careful of the vertebral artery and vein); the contralateral C7 nerve passes through the route. Connect this tunnel with the prespinal space to the recipient side.
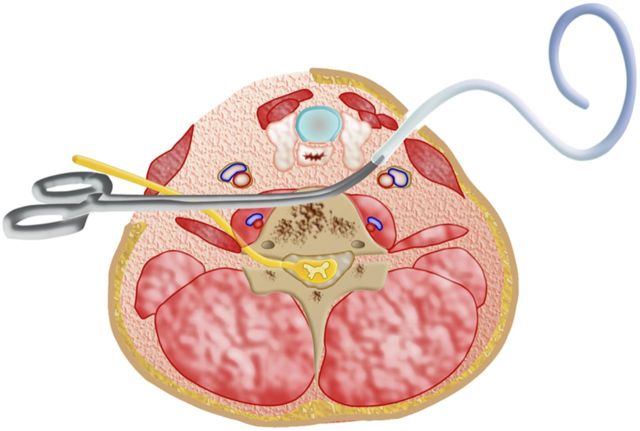
Pass a plastic tube with a diameter of approximately 5 mm through the prefabricated prespinal tunnel from the injured side to the healthy side (Fig. 4). Insert the contralateral C7 nerve root into the plastic tube and suture it in place. Then, pass the contralateral C7 nerve root to the injured side using the plastic tube as a guide (Fig. 5).
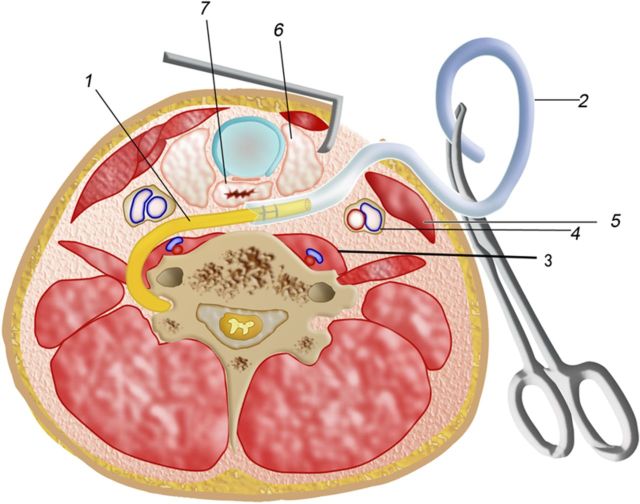
Fig. 1.
Schematic illustration of scissors opening up and creating the prespinal route. 1 = contralateral C7 nerve root, 2 = scalenus anterior muscle, 3 = sternocleidomastoid muscle, 4 = carotid sheath, 5 = longus colli muscle, 6 = vertebral artery and vein, 7 = esophagus, 8 = thyroid gland, 9 = trachea, and 10 = middle scalene muscle.
Fig. 2.
Dissect the anterior aspect of the scalenus anterior muscle to its medial margin. Place the tip of a clamp anterior to the junction of the scalenus anterior muscle origin with the C6 transverse process. Use the clamp to bluntly dissect and penetrate the scalenus anterior muscle, aiming for the site where the contralateral C7 nerve root just emerges from the intervertebral foramen.
Fig. 3.
Pass the contralateral C7 nerve root through to the anterior aspect of the scalenus anterior muscle. 1 = contralateral C7 nerve root, 2 = scalenus anterior muscle, 3 = sternocleidomastoid muscle, 4 = carotid sheath, 5 = angle space, 6 = vertebral artery and vein, 7 = esophagus, 8 = thyroid gland, 9 = trachea, and 10 = middle scalene muscle.
Fig. 4.
Use a plastic tube with a diameter of approximately 5 mm as a passing device. Pass it through the prefabricated prespinal tunnel from the injured side to the contralateral side beside the donor contralateral C7 nerve root.
Fig. 5.
Insert the contralateral C7 nerve root into the plastic tube and suture it in place. Then, pass the contralateral C7 nerve root to the injured side using the plastic tube as a guide. 1 = contralateral C7 nerve root, 2 = plastic tube, 3 = longus colli muscle, 4 = carotid sheath, 5 = sternocleidomastoid muscle, 6 = thyroid gland, and 7 = esophagus.
Video 1.
A video demonstrating the dissection of the prespinal route and how to pass the contralateral C7 (CC7) nerve root to the injured side, as viewed from over the patient's head to the neck region. The total avulsion injury of the brachial plexus (TABPI) is on the patient's left side. MABCN = medial antebrachial cutaneous nerve, and MCN = musculocutaneous nerve.
Video 2.
A diagrammatic video animation of the modified pathway for passage of the contralateral C7 nerve root.
Step 4: Humeral Shortening Osteotomy
If the contralateral C7 nerve does not reach the injured lower trunk, perform a humeral shortening osteotomy, generally with <5 cm of shortening in adults.
Position the injured upper extremity with the shoulder in 0° of adduction and 0° to 10° of anterior flexion, the elbow flexed 90°, and the forearm placed on the abdomen. Pull the previously mobilized lower trunk proximally through the retroclavicular space to the interval between the esophagus and carotid sheath of the recipient side. If the contralateral C7 nerve does not reach the injured lower trunk, perform a humeral shortening osteotomy.
Approach the humeral shaft by retracting the brachial biceps muscle medially and splitting the brachialis muscle. Perform the osteotomy with an oscillating saw just distal to the insertion of the deltoid muscle, tailoring the length of the humeral shortening to the size of the defect between the transferred contralateral C7 nerve and the injured lower trunk. Shortening the humerus by <12% to 14% of the humeral length (generally, <5 cm in adults and <3 cm in children) is advisable to avoid weakening and malfunction of the arm musculature1. Apply a six-hole locking compression plate (LCP) to the medial aspect of the humerus for stable fixation.
Step 5: Neurorrhaphy
Suture one end of the sural nerve together with the medial antebrachial cutaneous nerve to the musculocutaneous nerve; anastomose the remainder of the contralateral C7 nerve directly with the lower trunk.
Measure the length of the defect between the contralateral C7 nerve and musculocutaneous nerve. Harvest the sural nerve for the corresponding length. Suture one end of the sural nerve together with the medial antebrachial cutaneous nerve (bundle suture one end of the sural nerve with the medial antebrachial cutaneous nerve) to the musculocutaneous nerve using 9-0 nylon-suture epineurial neurorrhaphy. Then pass the nerve graft through the same route as the injured lower trunk.
Close all incisions in layers except the supraclavicular incision on the injured side. Dress the injured limb distal to the clavicle. Position the arm with the shoulder in 0° of adduction and 0° to 10° of anterior flexion, the elbow flexed 90°, and the forearm placed on the abdomen.
Anastomose one nerve bundle that arises from the anterior division of the C7 nerve, and contributes to the lateral pectoral nerve, to the sural nerve segmental graft, the other end of which has been anastomosed with the musculocutaneous nerve. Anastomose the remainder of the contralateral C7 nerve directly with the lower trunk using 8-0 nylon (Fig. 6). Close the supraclavicular incision in layers.
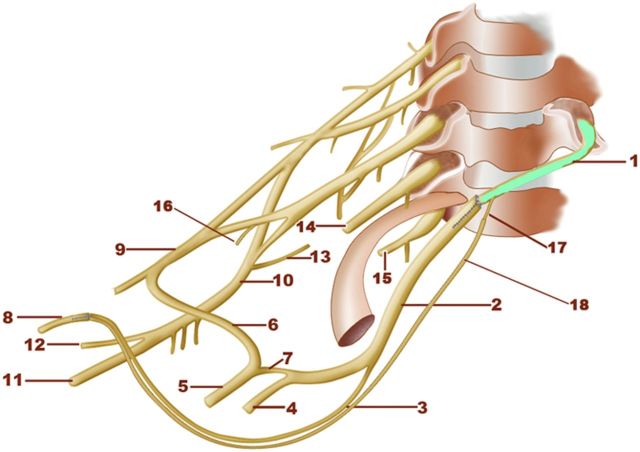
Fig. 6.
Schematic illustration of the direct coaptation of the contralateral C7 nerve with the lower trunk and the transfer of the contralateral C7 nerve to the musculocutaneous nerve through the bridging medial antebrachial cutaneous and sural nerves. The rerouted nerve is indicated by the green color. 1 = contralateral C7 nerve root, 2 = lower trunk, 3 = medial antebrachial cutaneous nerve, 4 = ulnar nerve, 5 = median nerve, 6 = lateral cord of the median nerve, 7 = medial cord of the median nerve, 8 = musculocutaneous nerve, 9 = lateral cord, 10 = posterior cord, 11 = radial nerve, 12 = axillary nerve, 13 = posterior division of the lower trunk, 14 = C8 nerve root, 15 = T1 nerve root, 16 = lateral pectoral nerve arising from the anterior division of the C7 nerve, 17 = lateral pectoral nerve arising from the anterior division of the contralateral C7 nerve, and 18 = sural nerve.
Step 6: Postoperative Care
Use a prefabricated brace to hold the head in the neutral position and immobilize the injured limb for six weeks.
After surgery, use a prefabricated brace to hold the head in the neutral position (Fig. 7).
Immobilize the injured limb for a period of six weeks.
Fig. 7.

A prefabricated brace was used to hold the patient’s head in the neutral position and the injured upper extremity with the shoulder in 0° of adduction and 0° to 10° of anterior flexion and the elbow flexed 90°.
Results (Videos 3, 4, and 5)
We evaluated the results of the technique in a study of seventy men and five women with a mean age (and standard deviation) of 28 ± 10 years (range, ten to fifty-three years)2. The average interval from the injury to the operation was 4 ± 2 months (range, one to eleven months). The average length of the contralateral C7 nerve was 6.5 ± 0.8 cm (range, 4.8 to 8 cm).
At the latest follow-up evaluation, at a mean of 57 ± 6 months (range, forty-eight to seventy-eight months), the motor function was graded as M3+ or greater (good or better according to the modified British Medical Research Council [MRC] muscle grading system) in 60% of the patients for elbow flexion, 64% of the patients for finger flexion, 53% for thumb flexion, and 72% for wrist flexion.
Video 3.
Video made forty-eight months postoperatively showing adequate elbow flexion and shoulder abduction (M3+ according to the modified British Medical Research Council [MRC] muscle grading system).
Video 4.
Video made forty-eight months postoperatively showing strong finger flexion (M4 according to the modified British Medical Research Council [MRC] muscle grading system).
Video 5.
Video made forty-eight months postoperatively showing that the patient could grasp something actively.
What to Watch For
Indications
Total brachial plexus avulsion injury.
Rupture of the C5 nerve with C6-T1 nerve-root avulsion injury.
Rupture of the upper trunk with avulsion of the middle and lower trunks.
Surgical intervention should be carried out less than ten months after the injury.
Contraindications
Extended injury from the C8 and/or T1 nerve roots to the distal portion of the lower trunk, or even to the medial cord.
Severe soft-tissue injuries of the forearm.
More than ten months from the time of injury to the surgical intervention.
Pitfalls & Challenges
If there is an extended injury beyond the lower trunk, or even the medial cord, abandon the direct coaptation and use a nerve graft to bridge the gap.
Generally, the extent of the humeral shortening should not be >5 cm in adults. Otherwise, nerve graft is used to bridge the defect. After the humeral shortening, biceps shortening should be performed at the proximal level.
Avoid injuring the posterior division of the lower trunk when dissecting and transecting the contralateral C7 nerve at the distal end.
Based on an original article: J Bone Joint Surg Am. 2013 May 1;95(9):821-7.
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. None of the authors, or their institution(s), have had any financial relationship, in the thirty-six months prior to submission of this work, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. Also, no author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1. Brady RJ Dean JB Skinner TM Gross MT. Limb length inequality: clinical implications for assessment and intervention. J Orthop Sports Phys Ther. 2003 May;33(5):221-34. [DOI] [PubMed] [Google Scholar]
- 2. Wang SF Li PC Xue YH Yiu HW Li YC Wang HH. Contralateral C7 nerve transfer with direct coaptation to restore lower trunk function after traumatic brachial plexus avulsion. J Bone Joint Surg Am. 2013 May 1;95(9):821-7. [DOI] [PubMed] [Google Scholar]