Overview
Introduction
Arthroscopic Hill-Sachs remplissage describes the fixation of the posterior aspect of the capsule and the infraspinatus tendon into a posterosuperior humeral head impaction fracture in cases of recurrent anteroinferior glenohumeral instability.

Step 1: Anterior Capsulolabral Mobilization and Glenoid Preparation
Perform diagnostic arthroscopy through a standard posterior portal to rule out additional pathology and document the “engaging” nature of the Hill-Sachs defect.
Step 2: Preparation of the Hill-Sachs Defect
With the camera remaining in the posterior portal, the assistant provides visualization of the Hill-Sachs defect by translating the humeral head anteriorly over the glenoid rim with direct pressure on the proximal part of the humerus.
Step 3: Remplissage with the Posterior Aspect of the Capsule and Infraspinatus Tendon
Transfer the camera to the anterior portal and leave a switching stick in the posterior portal; under direct visualization, withdraw the posterolateral cannula from the posterior aspect of the capsule and the infraspinatus tendon until it rests in the subdeltoid space (∼1 cm).
Step 4: Anterior Bankart Repair
Transition the camera back to the standard posterior portal over a switching stick in order to perform the Bankart repair.
Step 5: Postoperative Rehabilitation Protocol
Patients wear a brace and perform pendulum exercises for four weeks, and then initiate range-of-motion exercises; they avoid strengthening for eight weeks and sports for three to six months.
Results
In our recently published series of forty-seven patients (forty-two male and five female; average age, twenty-nine years), the use of Bankart repair combined with Hill-Sachs remplissage performed according to the above algorithm resulted in 98% of the patients being satisfied or very satisfied with their surgical result and a recurrent instability rate of only 2% at a mean of twenty-four months postoperatively.
Introduction
Arthroscopic Hill-Sachs remplissage describes the fixation of the posterior aspect of the capsule and the infraspinatus tendon into a posterosuperior humeral head impaction fracture in cases of recurrent anteroinferior glenohumeral instability. This procedure was initially described as an open procedure by Connolly1, but was later modified by Wolf et al.2,3 to include arthroscopic Hill-Sachs remplissage in combination with Bankart repair. The benefits of the posterior capsulotenodesis are twofold. First, the insertion of the posterior soft tissues into the defect effectively renders the defect extra-articular, thereby inhibiting its ability to “engage” on the anteroinferior glenoid rim during positions of abduction and external rotation. Second, the posterior soft tissues act as a tether, preventing anterior translation of the humeral head and limiting its ability to reach a position of subluxation or dislocation (Fig. 1).
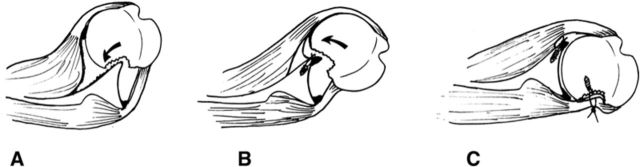
Fig. 1.
Biomechanics of the Hill-Sachs lesion and Hill-Sachs remplissage. Fig. 1-A Impaction of the posterior aspect of the humeral head on the anterior glenoid rim produces the engaging Hill-Sachs lesion. Fig. 1-B Recurrence of anterior instability despite anterior Bankart repair because of engagement of the large Hill-Sachs lesion on the anterior glenoid rim. Fig. 1-C The transfer (and healing) of the capsule and infraspinatus tendon into the bone defect has the dual effects of (1) rendering the humeral osseous lesion extra-articular (exclusion effect) and (2) decreasing anterior translation (checkrein effect).
We have found arthroscopic Bankart repair combined with Hill-Sachs remplissage to be a valuable advancement in our treatment of recurrent anterior glenohumeral instability. Once the pathological condition is confirmed through a thorough history and physical examination, we further stratify this subset of patients using the Instability Severity Index Score (ISIS) (Table I)4. Through our previous work, we have determined that patients with an ISIS of >3 have an unacceptably high level of recurrent instability (>10%) following arthroscopic Bankart repair alone5. In those with an ISIS of >3, we now augment our Bankart repair with an arthroscopic Bristow-Latarjet procedure (in cases of documented anteroinferior glenoid bone loss), an arthroscopic Hill-Sachs remplissage (in cases of an engaging Hill-Sachs lesion with an intact glenoid), or an arthroscopic Trillat procedure (if no glenoid or humeral osseous lesion exists).
TABLE I.
Instability Severity Index Score*
| Prognostic Factor | Points |
| Age at surgery | |
| ≤20 yr | 2 |
| >20 yr | 0 |
| Degree of sports participation preop. | |
| Competitive | 2 |
| Recreational or none | 0 |
| Type of sport preop. | |
| Contact or forced overhead | 1 |
| Other | 0 |
| Shoulder hyperlaxity | |
| Hyperlaxity (anterior or inferior) | 1 |
| Normal laxity | 0 |
| Hill-Sachs defect on anteroposterior radiograph | |
| Visible in external rotation | 2 |
| Not visible in external rotation | 0 |
| Glenoid loss of contour on anteroposterior radiograph | |
| Loss of contour | 2 |
| No lesion | 0 |
| Total possible points | 10 |
The Instability Severity Index Score uses both clinical and radiographic parameters to determine a patient’s risk of recurrence following isolated arthroscopic Bankart repair.
Bankart repair combined with Hill-Sachs remplissage can be used successfully as primary intervention, or as a revision procedure, if the Hill-Sachs defect is thought to be the cause of recurrent instability. Bankart repair combined with Hill-Sachs remplissage is intended for engaging Hill-Sachs defects that are large (>20% of the humeral head surface on computed tomography [CT] scans) and deep (Calandra grade 36, Table II), and is contraindicated in cases of glenoid erosion with bone loss.
TABLE II.
Arthroscopic Grading of Hill-Sachs Defects as Described by Calandra et al.6
| Calandra Grade | Description |
| 1 | Articular surface defect not involving subchondral bone |
| 2 | Articular surface defect including subchondral bone |
| 3 | Large defect in subchondral bone |
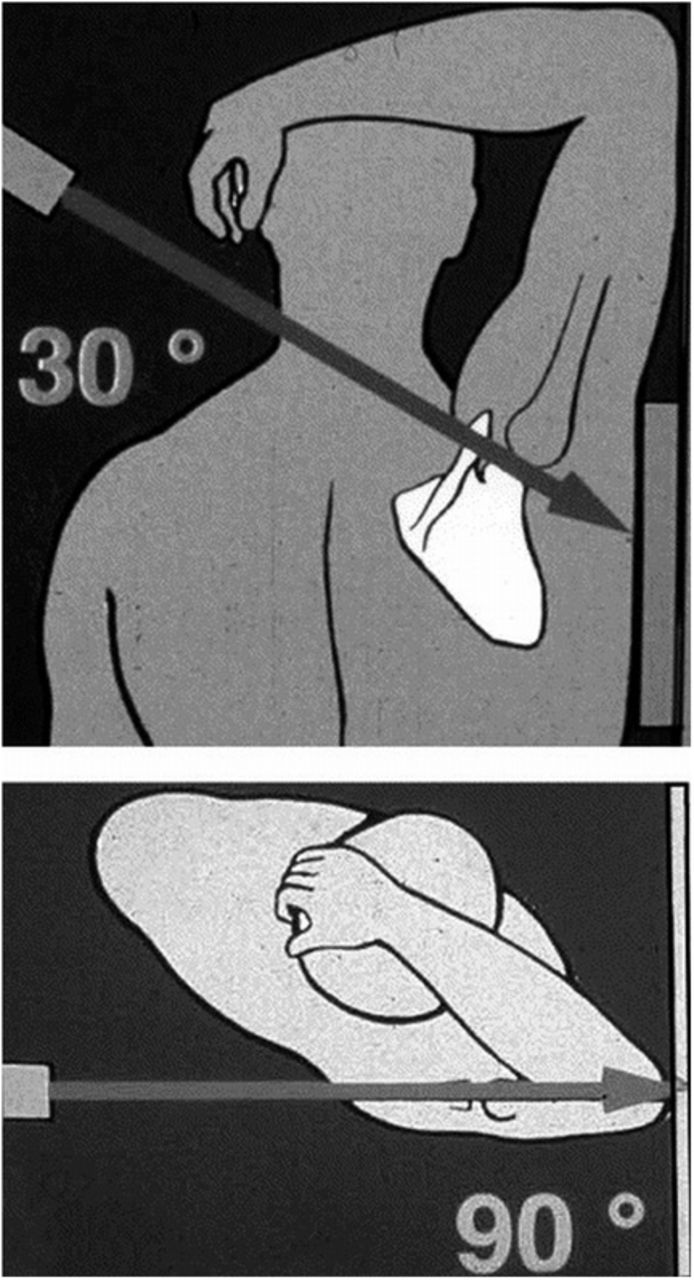
Preoperatively, questions regarding age, activity level, and type and degree of sports participation are particularly salient for this population. Appropriate routine imaging should consist of an anteroposterior radiograph with the shoulder in neutral, internal, and external rotation as well as a Bernageau glenoid profile view (Figs. 2-A and 2-B). If the ISIS is >3 and osseous lesions are suspected on radiographs, a CT scan with three-dimensional reconstructions should be obtained to further evaluate the integrity of the humeral head and glenoid bone stock.
Fig. 2-A.
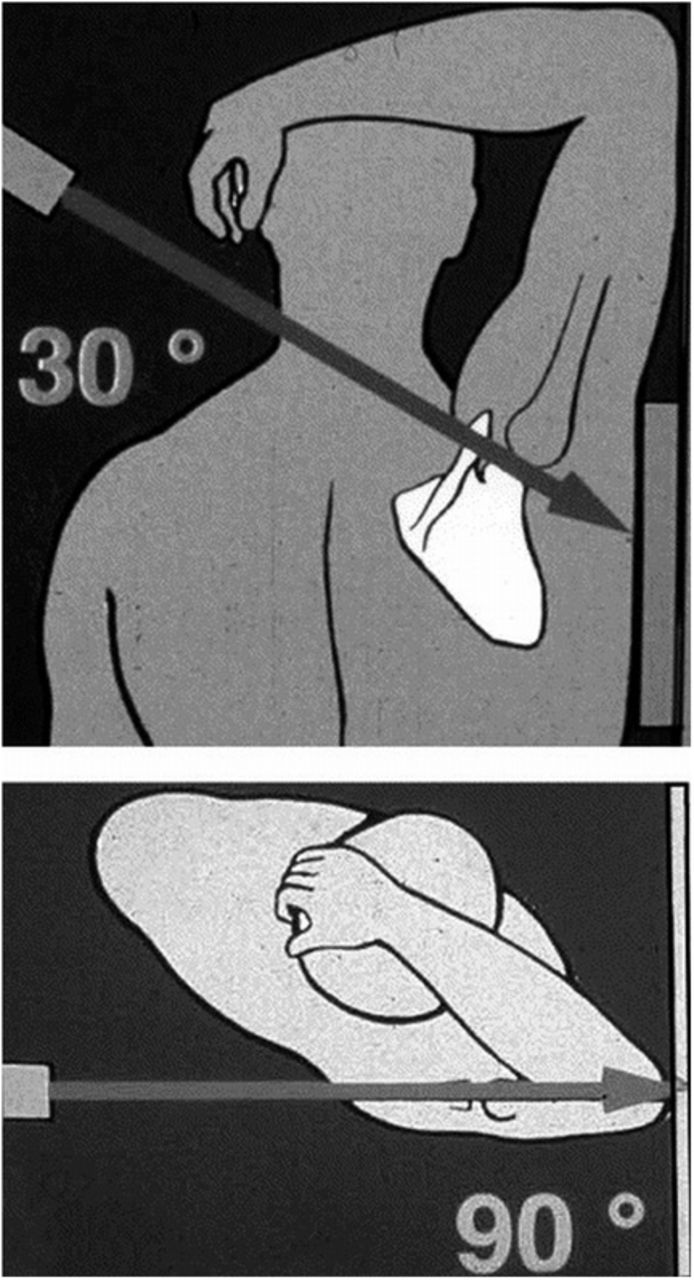
Representation of the appropriate technique for obtaining the Bernageau glenoid profile view. (Reproduced, with permission of Elsevier, from: Edwards TB, Boulahia A, Walch G. Radiographic analysis of bone defects in chronic anterior shoulder instability. Arthroscopy. 2003 Sep;19[7]:732-9.)
Fig. 2-B.

Representative Bernageau glenoid profile view. Note the blunted appearance of the anterior glenoid rim (arrow).
Although it is possible to perform this procedure with the patient in the sitting or lateral position, we prefer the modified beach-chair position and use of general anesthesia with the addition of an interscalene block. Three portals are used: anterior, posterior, and posterolateral.
As is often the case in surgery, the strategy of this procedure is at least as important as the technique. For this combined anterior and posterior procedure, the appropriate strategy helps to maximize efficiency and optimize surgical outcomes. Anterior translation of the humeral head greatly facilitates working in the area of the Hill-Sachs defect. Therefore, if the Bankart repair were completed first, the anterior soft tissues would be too tight to allow for translation of the humeral head, and visualization of the Hill-Sachs defect would be limited. Likewise, if the remplissage portion were completed first, the tightening of the posteroinferior aspect of the capsule would limit access to the anteroinferior capsulolabral tissues needed to perform an effective Bankart/capsular shift. This is why it is crucial to initiate the Bankart portion of the procedure prior to addressing the Hill-Sachs defect, and then return to the Bankart repair at the end.
The procedure is accomplished in four steps, which should always be performed in the following sequence.
Step 1: Anterior Capsulolabral Mobilization and Glenoid Preparation
Perform diagnostic arthroscopy through a standard posterior portal to rule out additional pathology and document the “engaging” nature of the Hill-Sachs defect (Video 1).
Create an anterior portal from outside in using needle localization. The ideal location should have an appropriate angle to access the inferior glenoid rim and be close enough to the supraspinatus tendon to allow visualization of the posterior aspect of the joint.
Temporarily transition the arthroscope to the anterior portal to confirm the absence of glenoid bone loss in excess of 20% to 25% of the anteroposterior diameter. If such glenoid bone loss is present, we recommend the addition of an arthroscopic Bristow-Latarjet procedure.
With the arthroscope returned to the posterior portal, mobilize the anteroinferior aspect of the labrum from six o’clock to two o’clock using a combination of electrocautery and a spatula. Traverse medially until fibers of the subscapularis are visible.
Place a temporary outside traction suture by passing a PDS-II (polydioxanone) monofilament synthetic absorbable suture (Ethicon) at five o’clock, taking both capsule and labrum7. Then replace the suture with a large-diameter Ethibond Excel polyester suture (Ethicon) using a shuttle technique.
Place an 8-mm anterior cannula with the temporary outside traction suture remaining outside, so as not to interfere with the suture from the suture anchors that will be placed and tied through this cannula.
Prepare the glenoid neck with an arthroscopic shaver to enhance healing of the capsulolabral tissue. Using gentle superior traction on the temporary outside traction suture avoids iatrogenic damage to the capsulolabral tissues. We do not use an arthroscopic burr in this situation to avoid compromising glenoid bone stock, which could exacerbate the unstable nature of the glenohumeral joint and predispose the patient to recurrence.
Place a five o’clock single-loaded suture anchor. Use superior traction on the temporary outside traction suture to pass a PDS-II monofilament synthetic absorbable suture through the inferior capsulolabral tissue. Use the PDS-II monofilament synthetic absorbable suture to shuttle the anchor suture through the capsulolabral tissues (inferior to the temporary outside traction suture).
Initiate an arthroscopic sliding knot but do not tighten it. Place a clamp on the post (capsule-sided) strand for later identification. This knot will be completed after the remplissage portion of the procedure.
Video 1.
View from the posterior portal demonstrates the "engaging" nature of the Hill-Sachs defect on the anteroinferior glenoid rim as the shoulder is placed in a position of abduction and external rotation.
Step 2: Preparation of the Hill-Sachs Defect
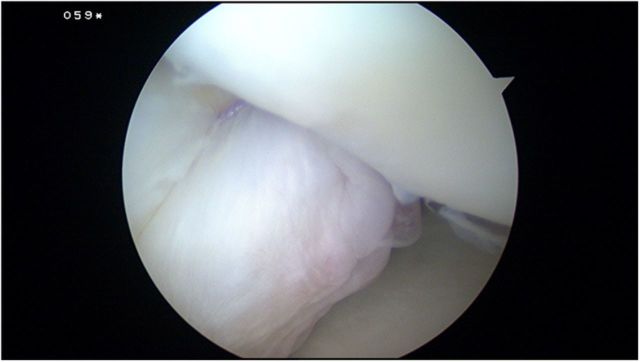
With the camera remaining in the posterior portal, the assistant provides visualization of the Hill-Sachs defect by translating the humeral head anteriorly over the glenoid rim with direct pressure on the proximal part of the humerus (Fig. 3-A).
Adjust the rotation, degree of abduction, and degree of flexion of the arm as needed to optimize visibility of the defect (i.e., modify the position of the arm and arm-holder). The optimal position is often neutral or slight external rotation, ∼30° of abduction, and ∼30° of forward flexion relative to the trunk.
Use a spinal needle to localize the accessory posterolateral portal, two fingerbreadths lateral to the standard posterior portal (Video 2). This represents the angle of future anchor insertion, and the ideal location should be centered over the Hill-Sachs defect in the superoinferior plane, with the needle arriving perpendicular to the humeral head defect and close to the articular margin of the defect.
Place a second 8-mm cannula in the posterolateral portal and debride the soft tissue of the humeral head defect with a shaver. Again, do not use a burr to avoid further compromising the already inadequate humeral head bone stock.
Using the accessory posterolateral portal, place two 5.5-mm single-loaded suture anchors into the humeral head defect close to the articular margin, one superior and one inferior (Fig. 3-B). Use a different color suture on each anchor to facilitate later identification.
Fig. 3-A.
The position of the arm during preparation and remplissage of the Hill-Sachs defect. Note the anterior translation of the humeral head by direct pressure of the surgical assistant’s thumb. Also note the temporary outside traction suture clamped to the drapes and positioned external to the anterior cannula.
Fig. 3-B.
Posterior view demonstrating the placement of the two suture anchors. Ideal placement is close to the articular margin of the defect with roughly 1 cm between the anchors. Care must be taken to ensure that the angle of insertion does not create a risk of penetrating the humeral articular cartilage.
Video 2.
A spinal needle is used to localize the ideal position of the accessory posterolateral portal. This portal will be used to prepare the Hill-Sachs defect, drill and insert the suture anchors, and tie the arthroscopic knots in the subdeltoid space.
Step 3: Remplissage with the Posterior Aspect of the Capsule and Infraspinatus Tendon
Transfer the camera to the anterior portal and leave a switching stick in the posterior portal; under direct visualization, withdraw the posterolateral cannula from the posterior aspect of the capsule and the infraspinatus tendon until it rests in the subdeltoid space (∼1 cm).
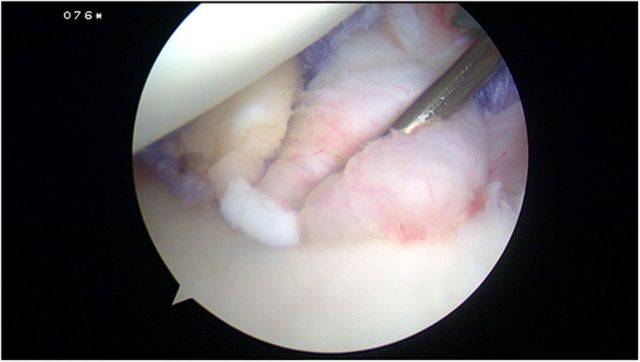
Use a curved tissue-penetrator to penetrate the posterior aspect of the capsule 7 to 8 mm inferior to the defect made by the cannula (but in the same mediolateral plane) and withdraw one suture limb from the inferior anchor (Fig. 4-A). This creates a tissue bridge between the two strands that will then be depressed into the humeral head defect.
Shorten the retrieved suture limb (it becomes the post) and secure the two limbs with a Kelly clamp. Ask your surgical assistant to maintain tension on the suture during the following step to prevent tangling.
Using a curved tissue-penetrator, perform the same procedure superior to the cannula defect, and withdraw one limb from the superior anchor. At this point, one limb from each anchor is passing independently through tissue and the other two limbs are passing through the hole in the posterior aspect of the capsule from the previously placed cannula (Fig. 4-B).
Release the anterior translation force provided by the surgical assistant and, with the patient’s arm in neutral rotation, tie the arthroscopic knots “blindly” in the posterior subdeltoid space. Start with the inferior suture anchor and use the eccentric limb as the post (Fig. 4-C).
Once the two knots have been tightened, perform an initial assessment of stability with anterior translation of the humeral head under arthroscopic visualization. This provides a full appreciation of the contribution of the tether effect in limiting humeral head translation (Video 3).
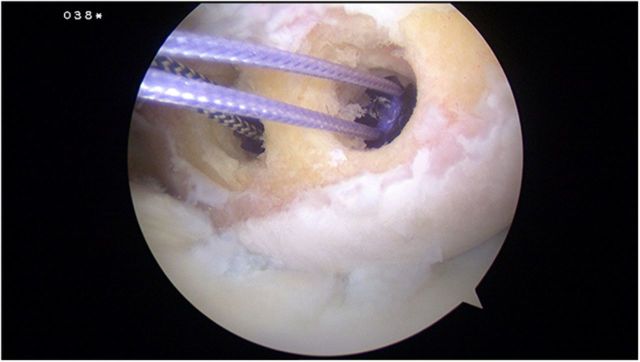
Fig. 4-A.
View from the anterior portal demonstrating a tissue-penetrator piercing the infraspinatus tendon and posterior aspect of the capsule 7 to 8 mm inferior to the defect created by the cannula. One limb from the inferior suture anchor is retrieved.
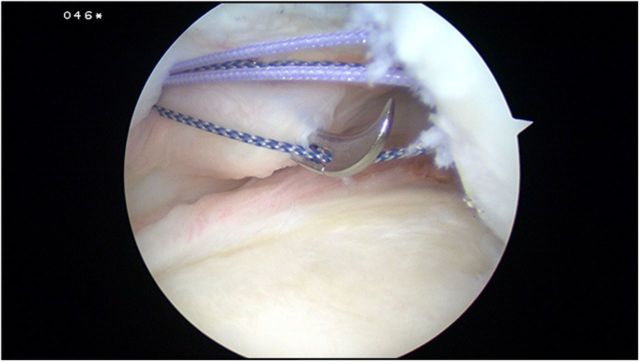
Fig. 4-B.
View from the anterior cannula following tissue penetration both superiorly and inferiorly. Note the two central limbs exiting through the defect left by the accessory posterolateral cannula, while the eccentric limbs penetrate the capsular tissue independently.
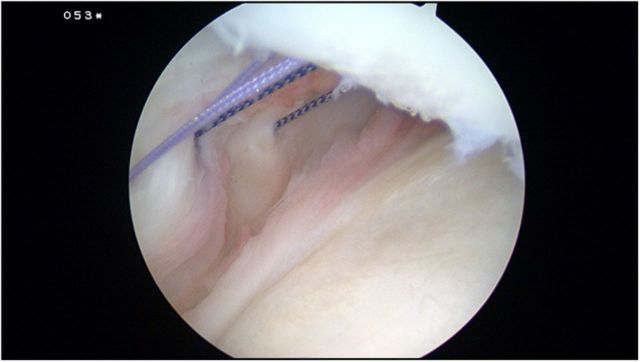
Fig. 4-C.
A final view from the anterior portal demonstrating the remplissage of the posterior soft tissue into the humeral head defect.
Video 3.
Anteriorly directed force on the proximal part of the humerus demonstrates the contribution of the tether effect. Note that the humeral head remains well centered following completion of the remplissage portion of the procedure.
Step 4: Anterior Bankart Repair
Transition the camera back to the standard posterior portal over a switching stick in order to perform the Bankart repair.
Complete the previously prepared arthroscopic knot from the five o’clock anchor. The clamp previously placed on the post strand will prevent confusion and prevent premature locking of the knot.
Perform a standard Bankart repair using the remaining capsulolabral tissue (Fig. 5). The temporary outside traction suture can be used to shuttle the suture from the four o’clock anchor, further streamlining this portion of the procedure and enhancing the south-north capsular shift.
Our typical construct involves three anchors placed at the five o’clock, four o’clock, and three o’clock positions.
Fig. 5.
View of the completed anterior Bankart repair from the standard posterior viewing portal.
Step 5: Postoperative Rehabilitation Protocol
Patients wear a brace and perform pendulum exercises for four weeks, and then initiate range-of-motion exercises; they avoid strengthening for eight weeks and sports for three to six months.
Patients wear a neutral rotation brace for four weeks and are encouraged to perform pendulum exercises daily to maintain passive motion.
At four weeks postoperatively, supervised physical therapy is begun to initiate active and active-assisted range of motion.
Strengthening is avoided until eight weeks postoperatively.
Return to sport is restricted until three to six months postoperatively and is based on progress with rehabilitation and the type of sport.
Results
In our recently published series8 of forty-seven patients (forty-two male and five female; average age, twenty-nine years), the use of Bankart repair combined with Hill-Sachs remplissage performed according to the above algorithm resulted in 98% of the patients being satisfied or very satisfied with their surgical result and a recurrent instability rate of only 2% at a mean of twenty-four months postoperatively. All forty-two patients willing to undergo advanced imaging (CT arthrography or magnetic resonance imaging) postoperatively demonstrated evidence of healing of the posterior aspect of the capsule and the infraspinatus tendon into the humeral defect, with 74% of patients demonstrating filling of ≥75% of the surface area of the Hill-Sachs defect. In addition, a high percentage of patients (90%) were able to return to sports participation, with 68% returning at their previous level of competition. Loss of external rotation was limited to a mean of 8° with the arm at the side and a mean of 9° with the arm in 90° of abduction. The final subjective shoulder value (SSV) averaged 90%, and the mean Constant-Murley score was 94 points.
What to Watch For
Indications
Symptomatic recurrent traumatic anteroinferior glenohumeral instability.
ISIS of >3.
Large and deep Hill-Sachs defect engaging over the anterior glenoid rim in abduction-external rotation.
Absence of substantial anteroinferior glenoid bone loss on preoperative imaging studies and intraoperative arthroscopic examination.
Contraindications
Voluntary, posterior, or multidirectional instability.
ISIS of <3 and no Hill-Sachs lesion.
Anteroinferior glenoid bone loss in excess of 20% to 25% of the glenoid diameter.
Moderate to severe glenohumeral arthritis.
Pitfalls & Challenges
Placement of the first anchor for the Bankart repair prior to the remplissage portion of the procedure is essential. Once the humeral head is tethered by the infraspinatus tendon and associated capsule, visualization of the anteroinferior portion of the glenohumeral joint is exceedingly difficult.
Appropriate arm positioning during the remplissage portion of the procedure optimizes visualization and prevents iatrogenic penetration of the humeral head articular surface. It is essential to adjust the rotation/abduction of the arm so that the angle of the posterolateral portal arrives strictly perpendicular to the surface of the Hill-Sachs defect.
Care should be taken to ensure that the angle of insertion does not change during the remplissage portion of the procedure. We prefer to use bioabsorbable anchors given the possible need for repeat imaging in this patient population. If the anchor is not inserted at the same angle as the drill/tap, anchor breakage is possible as one encounters the dense subchondral bone of the humeral head.
Clinical Comments
What additional techniques have demonstrated efficacy in addressing engaging Hill-Sachs lesions?
What long-term concerns exist about the use of Hill-Sachs remplissage for treatment of recurrent anteroinferior glenohumeral instability?
Based on an original article: J Bone Joint Surg Am. 2012 Apr 4;94(7):618-26.
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. One or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1. Connolly JF. Humeral head defects associated with shoulder dislocations. In: MacAusland Jr, editor. Instructional Course Lectures, American Academy of Orthopaedic Surgeons. St. Louis: Mosby; 1972: p 42-54. [Google Scholar]
- 2. Wolf EM Pollack M. Hill-Sachs “remplissage”: an arthroscopic solution for the engaging Hill-Sachs lesion. Arthroscopy. 2004;20:e14-5(Suppl 1). [DOI] [PubMed] [Google Scholar]
- 3. Purchase RJ Wolf EM Hobgood ER Pollock ME Smalley CC. Hill-Sachs “remplissage”: an arthroscopic solution for the engaging Hill-Sachs lesion. Arthroscopy. 2008 Jun;24(6):723-6. [DOI] [PubMed] [Google Scholar]
- 4. Balg F Boileau P. The Instability Severity Index Score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br. 2007 Nov;89(11):1470-7. [DOI] [PubMed] [Google Scholar]
- 5. Boileau P Villalba M Héry JY Balg F Ahrens P Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006 Aug;88(8):1755-63. [DOI] [PubMed] [Google Scholar]
- 6. Calandra JJ Baker CL Uribe J. The incidence of Hill-Sachs lesions in initial anterior shoulder dislocations. Arthroscopy. 1989;5(4):254-7. [DOI] [PubMed] [Google Scholar]
- 7. Boileau P Ahrens P. The TOTS (temporary outside traction suture): a new technique to allow easy suture placement and improve capsular shift in arthroscopic bankart repair. Arthroscopy. 2003 Jul-Aug;19(6):672-7. [DOI] [PubMed] [Google Scholar]
- 8. Boileau P O’Shea K Vargas P Pinedo M Old J Zumstein M. Anatomical and functional results after arthroscopic Hill-Sachs remplissage. J Bone Joint Surg Am. 2012 Apr 4;94(7):618-26. [DOI] [PubMed] [Google Scholar]