Overview
Introduction
We describe the medial transarticular and dorsal first web-space soft-tissue approaches, used in combination with an osteotomy, for the surgical correction of painful hallux valgus.
Step 1 (Medial Transarticular Approach): Skin Incision and Medial Capsulotomy
Make a medial longitudinal skin incision over the first metatarsophalangeal joint, perform a longitudinal midline capsulotomy, and excise the medial eminence.
Step 2 (Medial Transarticular Approach): Distal Soft-Tissue Procedure
Distract and widen the first metatarsophalangeal joint, apply manual traction to the great toe, transect the adductor hallucis, and apply varus stress to the first metatarsophalangeal joint.
Step 3 (Medial Transarticular Approach): Distal Chevron Osteotomy
Create a v-osteotomy, displace the capital fragment laterally, and impact it onto the shaft.
Step 4 (Medial Transarticular Approach): Postoperative Management
Patients walk in a postoperative shoe after surgery, and early metatarsophalangeal stretching exercises are encouraged.
Step 1 (Dorsal First Web-Space Approach): Skin Incision
Make a 3-cm dorsal longitudinal incision centered on the first intermetatarsal web space.
Step 2 (Dorsal First Web-Space Approach): Distal Soft-Tissue Procedure
Dissect the adductor hallucis tendon, transect the fibular sesamoid-metatarsal and transverse metatarsal ligaments, and perforate the first metatarsophalangeal joint capsule.
Step 3 (Dorsal First Web-Space Approach): Distal Chevron Osteotomy
Perform as for the medial transarticular approach.
Step 4 (Dorsal First Web-Space Approach): Postoperative Management
The same as for the medial transarticular approach.
Results
We studied 122 female patients (122 feet) who had undergone distal chevron osteotomy with a distal soft-tissue procedure for the treatment of symptomatic, unilateral, moderate-to-severe hallux valgus.
Introduction
We describe the medial transarticular and dorsal first web-space soft-tissue approaches, used in combination with an osteotomy, for the surgical correction of painful hallux valgus.
More than 100 different surgical techniques have been described for the correction of hallux valgus1. One of them, which combines an osseous procedure (such as metatarsal osteotomy) with a distal soft-tissue procedure, has shown good overall results and is widely used for the surgical treatment of painful hallux valgus1-3. The distal soft-tissue procedures can be done through either a dorsal first web-space approach or a medial transarticular approach4,5. The dorsal first web-space approach allows fairly easy release of the lateral soft tissue and visual assessment. However, it requires an additional incision and leaves a dorsal scar in the first web space. The benefits of the medial transarticular approach are decreased morbidity due to the avoidance of an additional incision, improved cosmetic appearance, and a reduced risk of osteonecrosis of the first metatarsal head6-8. However, because patients with hallux valgus have lateral and dorsal displacement of the lateral sesamoid bone, the release of the lateral soft tissues through the medial incision tends to be incomplete9.
The medial transarticular approach and dorsal first web-space approach are each done in four stages:
Step 1 (Medial Transarticular Approach): Skin Incision and Medial Capsulotomy
Make a medial longitudinal skin incision over the first metatarsophalangeal joint, perform a longitudinal midline capsulotomy, and excise the medial eminence.
Position the patient supine on a radiolucent operating table and perform regional anesthesia using an ankle block.
Exsanguinate the foot and maintain hemostasis using an ankle Esmarch tourniquet10.
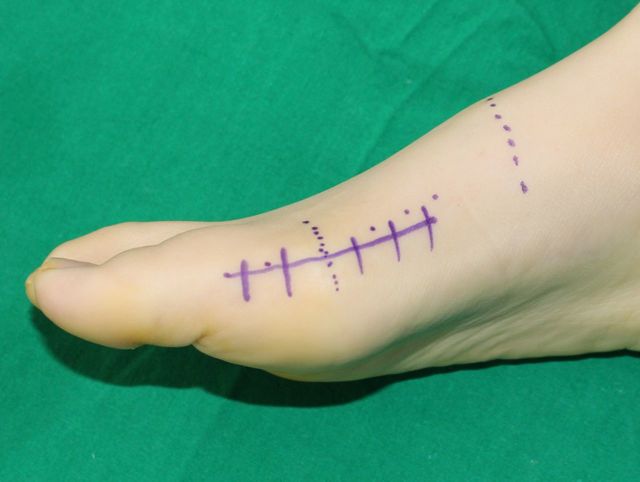
Make a medial longitudinal skin incision over the first metatarsophalangeal joint starting at the midportion of the proximal phalanx and extending it 2 cm proximal to the medial eminence (Fig. 1).
Perform a longitudinal midline capsulotomy in the same plane as that of the incision (Fig. 2).
Excise the medial eminence about 2 mm medial to the sagittal sulcus with a sagittal saw.
Fig. 1.
A medial longitudinal skin incision.
Fig. 2.
A longitudinal midline capsulotomy.
Step 2 (Medial Transarticular Approach): Distal Soft-Tissue Procedure (Video 1, Time Point 00:25 to 00:54)
Distract and widen the first metatarsophalangeal joint, apply manual traction to the great toe, transect the adductor hallucis, and apply varus stress to the first metatarsophalangeal joint.
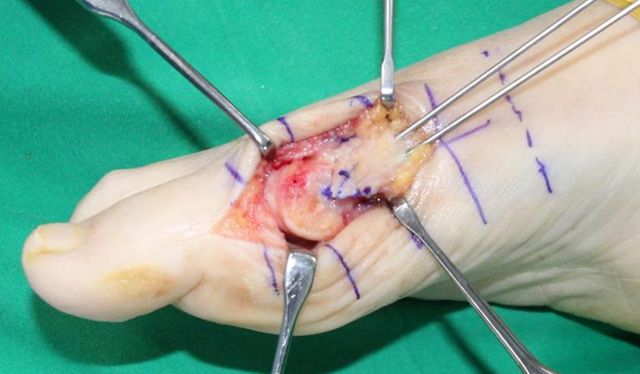
To clearly visualize the lateral capsular structures, distract the first metatarsophalangeal joint distally using two vein retractors and apply manual traction to the great toe (Fig. 3-A).
Insert a curved mosquito clamp into the middle portion of the lateral capsule and use it to widen the metatarsophalangeal joint (Fig 3-B).
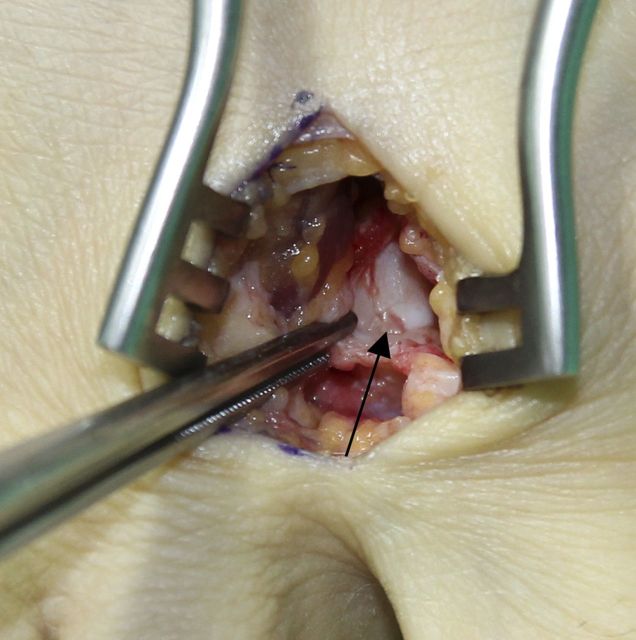
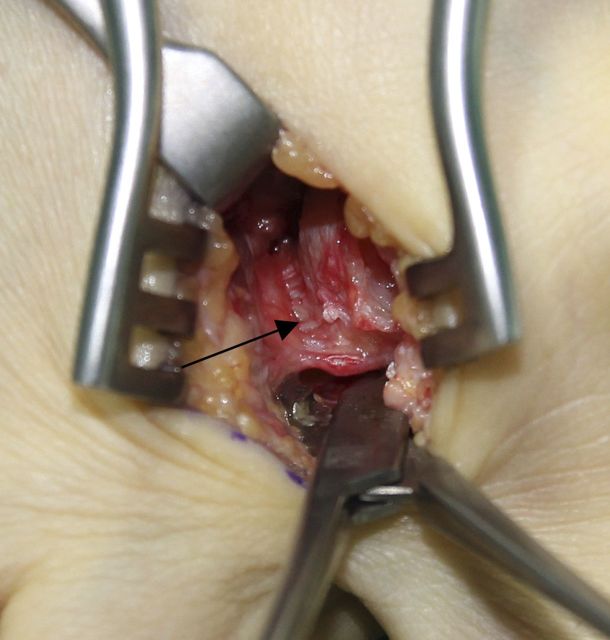
After releasing the lateral joint capsule using a number-15 blade, transect the conjoined tendon of the adductor hallucis completely from its insertion into the base of the proximal phalanx. We transect the lateral joint capsule and adductor hallucis in a direction perpendicular to the longitudinal axis of the toe (Figs. 3-C, 3-D, and 3-E).
Apply varus stress to the first metatarsophalangeal joint to complete the release of the adductor hallucis tendon at the proximal phalanx (Fig. 4 and Video 1, Time Point 00:54 to 00:57).
Figs. 3-A through 3-E Anatomical structures to be released through the medial transarticular approach.
Fig. 3-A.
The first metatarsophalangeal joint is distracted distally with use of two vein retractors and application of manual traction to the great toe to allow clear visualization of the lateral soft-tissue structures.
Fig. 3-B.
The lateral joint capsule (arrow) is visualized through the metatarsophalangeal joint, which is distracted with use of a mosquito clamp.
Fig. 3-C.
After the lateral joint capsule is released with use of a number-15 blade, the adductor hallucis tendon (arrow) is observed.
Fig. 3-D.
The adductor hallucis tendon is released completely. The dotted lines show the released adductor hallucis, the star indicates the remnant of the dorsolateral joint capsule, and the asterisk marks the proximal phalangeal portion of the released lateral joint capsule.
Fig. 3-E.
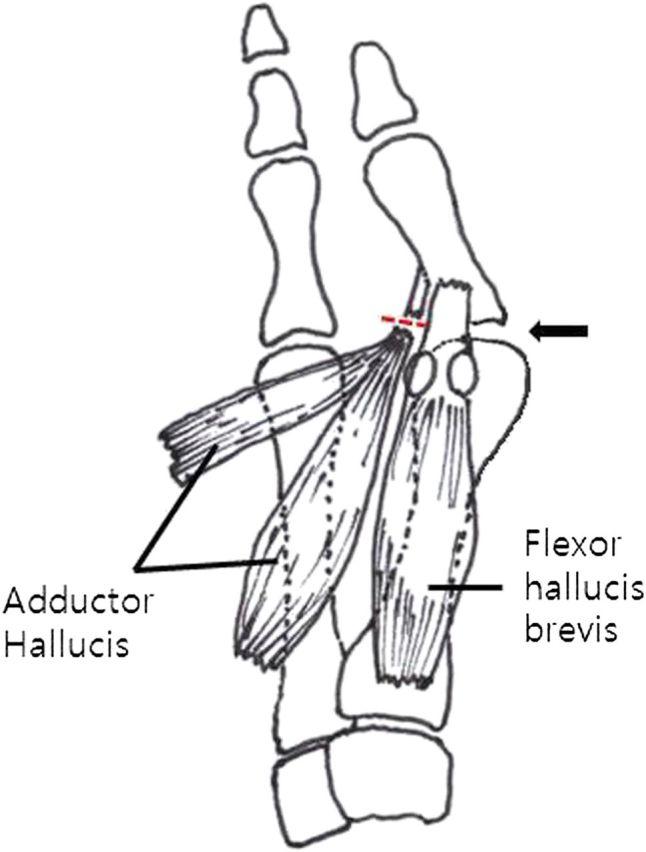
Illustration showing the conjoined tendon of the adductor hallucis tendon transected from its insertion into the base of the proximal phalanx.
Fig. 4.

Varus stress is applied to the first metatarsophalangeal joint to complete the release of the adductor hallucis tendon at the proximal phalanx.
Video 1.
Lateral soft-tissue release with the medial transarticular approach for moderate-to-severe hallux valgus.
Step 3 (Medial Transarticular Approach): Distal Chevron Osteotomy
Create a v-osteotomy, displace the capital fragment laterally, and impact it onto the shaft.
Make a standard medial incision over the first metatarsophalangeal joint starting at the midportion of the proximal phalanx and extending 2 cm proximal to the medial eminence.
After a longitudinal midline capsulotomy has been performed, resect the medial eminence and perform the chevron osteotomy using standard techniques.
Create a 60° v-osteotomy centered in the first metatarsal head, displace the capital fragment by about 5 to 9 mm laterally according to the degree of the deformity, and manually impact the fragment onto the shaft to obtain a stable reduction (Figs. 5-A and 5-B). The amount of displacement of the capital fragment is determined by the severity of the hallux valgus, and the intermetatarsal angle. Generally, 5 mm of displacement is recommended.
Fix the osteotomy site with two medially placed 1.4-mm Kirschner wires (Figs. 6-A and 6-B).
Resect any remaining proximal medial osseous prominence at the osteotomy site after displacement of the metatarsal head.
Reduce the hallux to a neutral position after completing the distal chevron osteotomy.
Close the medial capsule longitudinally after excising the redundant edges.
Figs. 5-A and 5-B Distal metatarsal chevron osteotomy.
Fig. 5-A.
A 60° v-osteotomy is created and centered in the first metatarsal head.
Fig. 5-B.
The capital fragment is translated about 7 mm laterally and manually impacted onto the shaft to obtain a stable reduction.
Figs. 6-A and 6-B Photograph and lateral radiograph showing the osteotomy site fixed with two medially placed 1.4-mm Kirschner wires.
Fig. 6-A.
Fig. 6-B.
Step 4 (Medial Transarticular Approach): Postoperative Management
Patients walk in a postoperative shoe after surgery, and early metatarsophalangeal stretching exercises are encouraged.
After the surgery, apply a gauze wrap dressing, taking care not to pronate the toe or to force it into varus.
Patients are allowed to walk after surgery while wearing a postoperative shoe (Fig. 7), with weight borne on the heel and the outer aspect of the foot.
Early active and passive metatarsophalangeal stretching exercises are encouraged.
The dressing is changed weekly for two weeks, and then the sutures are removed. An elastic bandage is used to hold the corrected toe position for an additional two weeks.
The Kirschner wires are usually removed in the outpatient clinic at six to eight weeks after surgery. The patient is then allowed to wear a soft shoe.
Fig. 7.

Postoperative shoe.
Step 1 (Dorsal First Web-Space Approach): Skin Incision
Make a 3-cm dorsal longitudinal incision centered on the first intermetatarsal web space.
Position the patient supine on a radiolucent operating table and perform regional anesthesia using an ankle block.
Exsanguinate the foot and maintain hemostasis using an ankle Esmarch tourniquet10.
Make a 3-cm dorsal longitudinal incision centered on the first intermetatarsal web space.
Step 2 (Dorsal First Web-Space Approach): Distal Soft-Tissue Procedure
Dissect the adductor hallucis tendon, transect the fibular sesamoid-metatarsal and transverse metatarsal ligaments, and perforate the first metatarsophalangeal joint capsule.
Perform the dissection in the midline to protect the branches of the deep peroneal nerve.
Identify the adductor hallucis tendon.
Dissect the distal end of the adductor tendon that was released from the base of the proximal phalanx of the great toe from the lateral aspect of the fibular sesamoid.
Transect the fibular sesamoid-metatarsal ligament and transverse metatarsal ligament (Figs. 8-A through 8-D).
Perforate the lateral aspect of the first metatarsophalangeal joint capsule with several puncture wounds.
Apply varus stress to the first metatarsophalangeal joint to complete the release of the adductor hallucis tendon from the proximal phalanx.
Figs. 8-A through 8-D Anatomical structures to be released through the dorsal first web-space approach.
Fig. 8-A.
The adductor hallucis tendon is identified with use of a mosquito clamp.
Fig. 8-B.
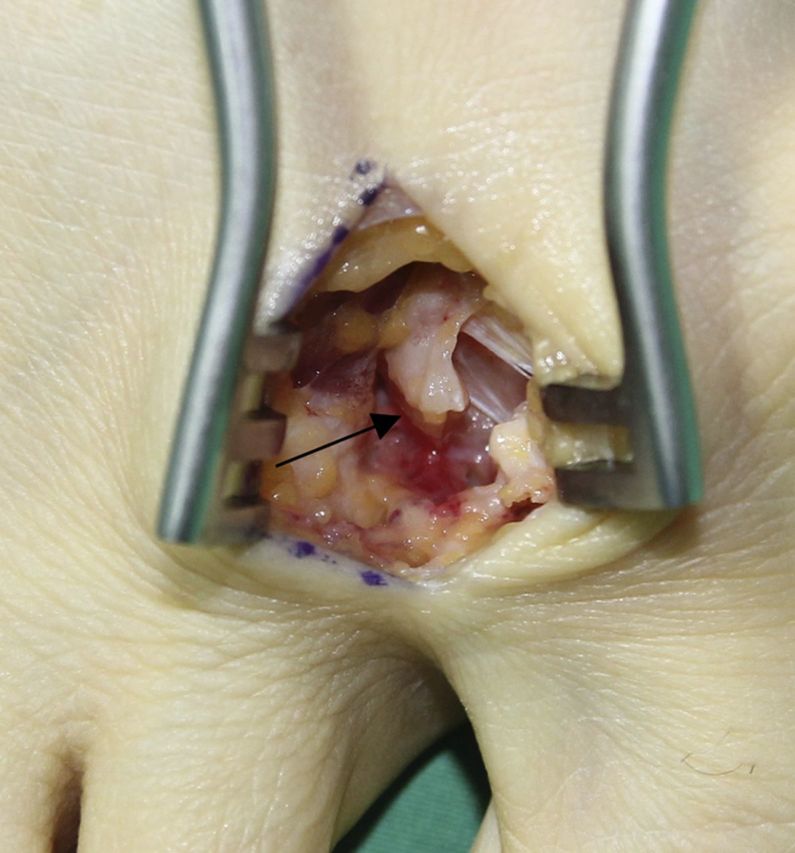
The adductor hallucis tendon (arrow) has been released from its insertion at the base of the proximal phalanx of the great toe.
Fig. 8-C.
After the fibular sesamoid-metatarsal ligament is released, the fibular sesamoid (arrow) can be observed.
Fig. 8-D.
The transverse metatarsal ligament (arrow) has been identified and transected.
Step 3 (Dorsal First Web-Space Approach): Distal Chevron Osteotomy
Perform as for the medial transarticular approach.
Step 4 (Dorsal First Web-Space Approach): Postoperative Management
The same as for the medial transarticular approach.
Results
We studied 122 female patients (122 feet) who had undergone distal chevron osteotomy with a distal soft-tissue procedure for the treatment of symptomatic, unilateral, moderate-to-severe hallux valgus11. Sixty feet were treated with a dorsal first web-space approach (group D) and sixty-two, with a medial transarticular approach (group M). Clinical and radiographic measurements were compared between the two groups at a mean of thirty-eight months postoperatively (Figs. 9-A through 9-E).
Figs. 9-A through 9-E Clinical photographs and radiographs of the left foot of a sixty-year-old woman who underwent distal chevron osteotomy with a distal soft-tissue procedure through the medial transarticular approach for severe hallux valgus deformity.
Fig. 9-A.
The preoperative hallux valgus angle was 38°, the first-second intermetatarsal angle was 19°, and the tibial sesamoid position was grade 3.
Fig. 9-B.

Preoperative clinical photograph.
Fig. 9-C.

Postoperative anteroposterior radiograph.
Fig. 9-D.
The hallux valgus angle was 10°, the first-second intermetatarsal angle was 9°, and the tibial sesamoid position was grade 2 at the time of final follow-up.
Fig. 9-E.
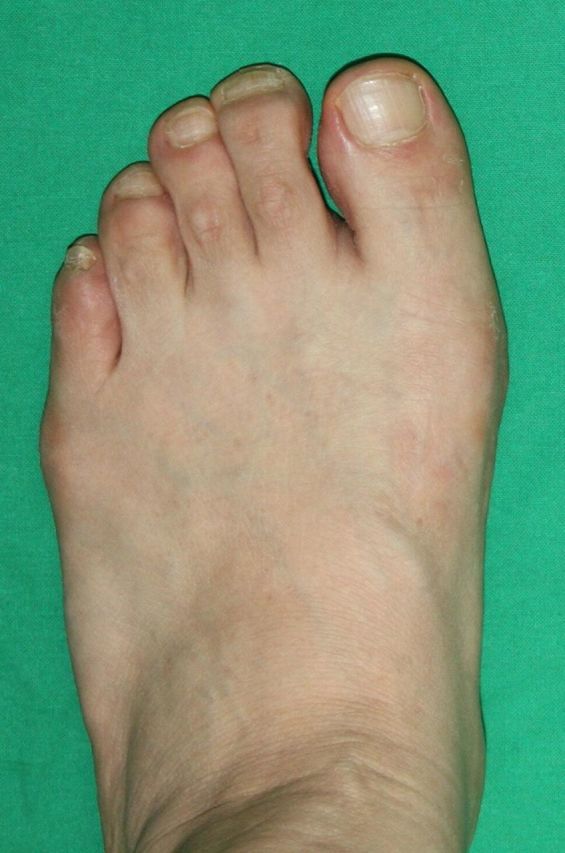
Clinical photograph at the time of final follow-up.
The American Orthopaedic Foot & Ankle Society (AOFAS) scores did not differ significantly between group D and group M at the time of final follow-up (p = 0.635). Each group had significant improvements in the hallux valgus angle and the intermetatarsal angle between the first and second ray at the time of final follow-up (p < 0.05), but the groups did not differ significantly with respect to these measurements (p = 0.64 and 0.79, respectively) at the time of final follow-up.
A total of eleven complications occurred (six in group D and five in group M). The complication rates were 10% and 8.1% in group D and group M, respectively, with no significant difference between the two groups (p = 0.71).
What to Watch For
Indications
Symptomatic hallux valgus deformity such as bunion pain, painful callosity, or shoe irritation caused by a bunion and a second-toe overriding deformity.
Cosmetically unacceptable deformity of the foot.
Incongruent first metatarsophalangeal joint.
Moderate-to-severe hallux valgus deformity.
Contraindications
Active osteomyelitis or a deep tissue infection.
Neuropathic arthropathy of the forefoot.
Patient noncompliance.
Pitfalls & Challenges
Metatarsophalangeal joint stiffness. This is the most common complication, and active and passive metatarsophalangeal joint mobilization exercises are essential postoperatively to avoid it.
Injuries to the first metatarsophalangeal joint intra-articular cartilage and flexor hallucis brevis tendon. These can be avoided by using two vein retractors for more clear visualization and a curved mosquito forceps to guide the number-15 blade during the release.
Osteonecrosis of the first metatarsal head. The risk of this complication may be lower with the medial transarticular approach than with the dorsal first web-space approach because a minimally invasive lateral soft-tissue release results in less release of the lateral capsule (i.e., just the central portion of the capsule) than the dorsal first web-space approach. The risk can also be minimized by avoiding soft-tissue stripping proximal to the capsular attachment and careful use of the power saw to prevent thermal damage.
Delayed hallux varus. Caution should be exercised intraoperatively to avoid excessive release of the lateral joint capsule since, with this technique, the entire capsule has to be incised instead of perforated several times as it is with the dorsal first web-space approach. If an excessive release is performed, delay the range of motion of the metatarsophalangeal joint until the already released lateral soft tissue has healed.
Injury to the dorsal cutaneous branches of the superficial peroneal nerve. In order to prevent this, a medial longitudinal incision is made over the first metatarsophalangeal joint and a longitudinal midline capsulotomy is performed in the same plane as that of the incision.
Clinical Comments
Lateral soft-tissue release with the medial transarticular approach would be difficult for a surgeon without an exact knowledge of the anatomical structure of the lateral soft tissue of the first metatarsophalangeal joint because it is an indirect correction technique. Therefore, sufficient understanding of surgical anatomy is necessary before performing the operation through the medial transarticular approach.
Caution should be exercised intraoperatively to avoid over-release of the lateral joint capsule. The surgeon should incise only the central portion of the lateral joint capsule and adductor hallucis, and then a complete release of the lateral soft tissue should be achieved by gentle varus stress to the first metatarsophalangeal joint.
Footnotes
Based on an original article: J Bone Joint Surg Am. 2013 Nov 6;95(21):e158.
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. None of the authors, or their institution(s), have had any financial relationship, in the thirty-six months prior to submission of this work, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. Also, no author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Chen YJ, Hsu RW, Shih HN, Huang TJ, Hsu KY. Distal chevron osteotomy with intra-articular lateral soft-tissue release for treatment of moderate to severe hallux valgus deformity. J Formos Med Assoc. 1996. October;95(10):776-81. [PubMed] [Google Scholar]
- 2.Johnson JE, Clanton TO, Baxter DE, Gottlieb MS. Comparison of Chevron osteotomy and modified McBride bunionectomy for correction of mild to moderate hallux valgus deformity. Foot Ankle. 1991. October;12(2):61-8. [DOI] [PubMed] [Google Scholar]
- 3.Pochatko DJ, Schlehr FJ, Murphey MD, Hamilton JJ. Distal chevron osteotomy with lateral release for treatment of hallux valgus deformity. Foot Ankle Int. 1994. September;15(9):457-61. [DOI] [PubMed] [Google Scholar]
- 4.Lin I, Bonar SK, Anderson RB, Davis WH. Distal soft tissue release using direct and indirect approaches: an anatomic study. Foot Ankle Int. 1996. August;17(8):458-63. [DOI] [PubMed] [Google Scholar]
- 5.Waldecker U. Lateral release in hallux valgus surgery: comparison of two approaches. Foot Ankle Surg. 2004;10:195-9. [Google Scholar]
- 6.Stamatis ED, Huber MH, Myerson MS. Transarticular distal soft-tissue release with an arthroscopic blade for hallux valgus correction. Foot Ankle Int. 2004. January;25(1):13-8. [DOI] [PubMed] [Google Scholar]
- 7.Potenza V, Caterini R, Farsetti P, Forconi F, Savarese E, Nicoletti S, Ippolito E. Chevron osteotomy with lateral release and adductor tenotomy for hallux valgus. Foot Ankle Int. 2009. June;30(6):512-6. [DOI] [PubMed] [Google Scholar]
- 8.Panchbhavi VK, Rapley J, Trevino SG. First web space soft tissue release in bunion surgery: functional outcomes of a new technique. Foot Ankle Int. 2011. March;32(3):257-61. [DOI] [PubMed] [Google Scholar]
- 9.Lee WC, Kim YM. Correction of hallux valgus using lateral soft-tissue release and proximal Chevron osteotomy through a medial incision. J Bone Joint Surg Am. 2007. October;89(Suppl 3):82-9. [DOI] [PubMed] [Google Scholar]
- 10.Bai LB, Lee KB, Seo CY, Song EK, Yoon TR. Distal chevron osteotomy with distal soft tissue procedure for moderate to severe hallux valgus deformity. Foot Ankle Int. 2010. August;31(8):683-8. [DOI] [PubMed] [Google Scholar]
- 11.Park YB, Lee KB, Kim SK, Seon JK, Lee JY. Comparison of distal soft-tissue procedures combined with a distal chevron osteotomy for moderate to severe hallux valgus: first web-space versus transarticular approach. J Bone Joint Surg Am. 2013. November 6;95(21):e158. [DOI] [PubMed] [Google Scholar]