Abstract
Ankle and knee injuries are two of the most common injuries. It has been shown that ankle sprains can lead to chronic ankle instability thereby affecting the function of the ankle. Since the lower extremity is a kinetic chain anything that affects the ankle is thought to affect the knee and hip as well. Changes in lower extremity function associated with chronic ankle instability may predispose patients for non-contact ACL injuries. The purpose of this study was to provide a systematic review of the research done on chronic ankle instability (CAI) and lower extremity kinematics during landing tasks. SportsDiscus, PubMed, and CINAHL were used to search “ankle instability” and “landing kinematics.” Included articles must have evaluated patients with chronic ankle instability and have identified kinematic changes at the knee to be included in the review. A total of 338 subjects participated in the six studies identified. The principal findings in these studies were that CAI subjects had decreased knee flexion compared to the control group. Hip flexion was the same between CAI and control groups and dorsiflexion range of motion had mixed results. Patients with chronic ankle instability demonstrate decreased knee flexion. Decreased knee flexion has shown to be a key risk factor in non-contact knee injuries. In the future, more research needs to be done comparing chronic ankle instability to non-contact knee injury rates.
Keywords: Non-contact knee injuries, landing kinematics, risk factors
INTRODUCTION
The prevalence of ankle sprains is well established in physically active individuals (16,21). Ankle sprains are a very common problem and often have lasting effects. Estimates are that 73% of individuals who suffer a lateral ankle sprain end up developing chronic ankle instability (CAI) (2,17,24). Ankle instability is caused by multiple changes in the structural integrity of the ankle joint (12). This results in decreased stability and neuromuscular control. These individuals with residual symptoms are classified as suffering from chronic ankle instability (14). Limited mobility or hypermobility in the ankle may lead to restriction of movement further up the chain (6) as well individuals with chronic ankle instability have been found to less adept at the transfer of energy throughout the lower extremity kinetic chain (22).
Following injury, especially injuries with residual symptoms, it is common that these symptoms cause adaptive movement strategies. The ability to adapt to a variety of conditions create a protective effect of the lower extremity whereas some adaptations are also potential causes of injury (10). Since the lower extremity functions as a unit, changes in the adaptive strategies at the ankle will limit the available strategies to more proximal kinetic segments. This could possibly create situations leading injuries associated with the transfer of forces throughout the chain.
Non-contact knee injuries, specifically the anterior-cruciate ligament (ACL), are some of the most debilitating injuries in sports. Common risk factors that predispose athletes to non-contact knee injuries are: change of direction combined with deceleration, landing from a jump in knee extension, pivoting in knee extension with a planted foot, and knee hyperextension and hyperflexion (1). 70% of ACL injuries do not result from direct contact however, the exact causes of non-contact knee injuries are still debated (13). The inability to dissipate energy throughout the kinetic chain associated with chronic ankle instability (22) could increase the rate of non-contact ACL injuries.
Preliminary searches revealed a lack of direct investigation of the risk of ACL injury in patients with chronic ankle instability however it is possible to indirectly ascertain possible risks factors associated with changes within the kinetic chain. Non-contact injuries are thought to frequently be caused during deceleration where there is reduced knee flexion and increased quadriceps contraction. The quadriceps exert the most anterior tibial shear force (ATSF) when knee flexion angles are between 10–30 degrees. At decreased knee flexion, the quadriceps exert a large amount of anterior force that the ACL and hamstrings are not able to counteract (1,13). Therefore, the purpose of this systematic review is to provide an in-depth analysis of the research done on relating chronic ankle instability and lower extremity kinematics during landing tasks.
METHODS
As there was no reported methodological standard established, PRISMA guidelines were used where appropriate (18). Also, as a review article IRB approval and informed consent did not apply. The PICO question for this study was utilized: Does ankle instability predispose individuals to a greater risk of non-contact knee injuries? Due to the lack of direct investigation, the review was expanded to include evidence relating knee kinematic changes during landing activities of individuals with chronic ankle instability.
Participants
Both male and female participants were included to allow for equal data. Subjects needed to demonstrate ankle instability in one of their ankles. The limb of the CAI group was matched to the limb of the comparison group. The chronic ankle instability criterion was: at least one acute lateral ankle sprain older than four months, three episodes of instability in the last year, and no ankle surgery in the last four years. This criterion for CAI is consistent with previous research (25). The control group needed to be free of lower extremity or ankle injuries in the past four years. There were no restrictions on years when obtaining articles and all were found in English.
Protocol
The following databases were used to obtain articles: PubMed, SportsDiscus, CINAHL. Cross-referenced articles were included from the initial search results on PubMed. The search strategy used throughout the three search engines was “ankle instability” and “landing kinematics.” Articles were screened by title, abstract and full-text and eliminated if they did not fit the study. Articles were screened based on the PICO question “Does ankle instability predispose individuals to a greater risk of non-contact knee injuries?” with articles being included that addressed lower extremity kinematics during landing tasks.
Statistical Analysis
This study screened articles for potential bias and scored on the PEDro scale. Articles were screened and scored separately by the two authors. Discrepancies in scoring were addressed through collaboration between the authors until a consensus was reached. Summary measures were based on risk ratios comparing the effects of CAI on the lower extremity to patients in the comparison group. Because of the publication bias extra weight will be given to negative results while evaluating the studies.
RESULTS
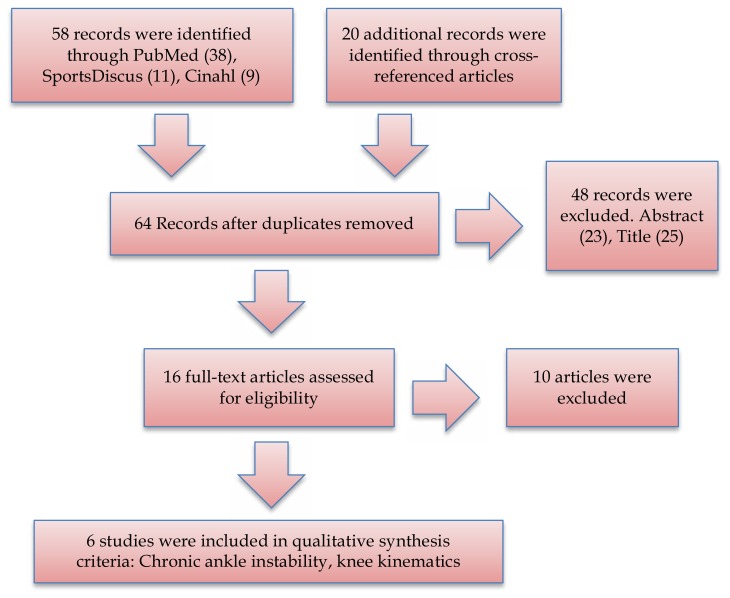
Seventy-eight articles were identified from PubMed, SportsDiscus, CINAHL, and cross-referenced articles. Fourteen of the seventy-eight articles were eliminated based on duplicates. Sixty-four articles were screened based off of their abstract and title with the most common reasons being that the articles related to prevention and rehabilitation programs. Reading the abstract eliminated twenty-three and twenty-one were eliminated by the title. Sixteen full texted articles were obtained through downloading from electronic databases. Studies were extracted based on the PICO question, and relating chronic ankle instability to knee kinematics. Ten studies were eliminated after reviewing full-text articles. Two studies were eliminated because they did not relate the ankle to the knee (4,19). Four articles were eliminated because they did not have a chronic ankle instability group (9,15,19,20). One article was eliminated because it related landing kinematics to fatigue and not directly to CAI (26). Two studies were eliminated because the articles were systematic reviews on prevention programs for non-contact knee injuries (1,11). One study was eliminated because it was a narrative review (13). Eventually, after elimination of articles there were six full-text articles that met the criteria for the systematic review. The studies were used to evaluate the effects of chronic ankle instability on non-contact knee injuries. Figure 1 displays a step-by-step process of the flow chart for why the articles were eliminated.
Figure 1.
Flow chart of the selection process for final articles.
In the six studies that were chosen, 338 subjects were used. Four studies compared chronic ankle instability (90 subjects) to a control group (90 subjects) (4,6,12,23). One study compared CAI (28 subjects) to the ankle coper group (42 subjects) (7). Another study compared mechanical ankle instability (21 subjects), chronic ankle instability (23 subjects), ankle copers (20 subjects), and a control group (24 subjects) (3). Two studies found significant results in knee flexion at ATSF and ground impact (12,23). Less knee flexion was seen at both ATSF and ground impact. Gribble and Robinson also found that time to stabilization (dynamic stability) was longer in the CAI group (12). Doherty et al. found that there was increased hip flexion pre-initial contact (IC), and increased hip joint stiffness after initial contact in CAI compared to copers (7). CAI patients had less dorsiflexion in their ankle during post initial contact and a less externally rotated hip during pre IC (6).
Three studies found that there were no main differences in hip flexion (4,12,23). Two studies found no difference between groups in plantar flexion (12), and another study found the difference in dorsiflexion at peak ATSF was not significant (23). Ridder et al. found that there were no differences between CAI and the control group for knee flexion and also that there was no difference in dorsiflexion (5). Doherty et al. found that there were no differences between CAI and coper groups in ankle and knee joint angular displacement, energetics and ground reaction forces (7). No difference found between the rectus femoris for electromyography (6). In the study comparing variability in the ankle, knee and hip in three planes there was no clinical relevance (3).
Table 1.
Reviewed studies based on chronic ankle instability and if it predisposes individuals to non-contact knee injuries.
| Study | PEDro Score | Subjects | N | Age (years) | Tasks | Measures | Comparison | Outcome |
|---|---|---|---|---|---|---|---|---|
| M. Terada, (2014) | 5 | 19 subjects with CAI. 19 subjects in the control. |
38 | CAI: 20.11 ± (1.6) Control: 21.32 ±(4.0) |
Vertical stop jump | Peak ATSF, posterior GRF, lower extremity kinematics (knee, ankle, hip) | CAI was compared to the control group | CAI did not show significant greater peak anterior tibial shear force (ATSF). No difference in posterior ground force reaction (GFR) at ATSF. Presence of CAI reduces availability of degrees of freedom. Difference between groups at ATSF in dorsiflexion approached significance. Patients with CAI had less knee flexion at ATSF. No group differences in hip flexion. |
| P. A. Gribble, (2009) | 5 | 19 subjects with CAI. 19 subjects in the control.in young volleyball players |
38 | CAI: 20.3 ± (2.9) Control: 23.1 ± (3.9) |
Double leg take off while landing on a single leg | TTS in AP and ML directions, Measurements were taken for plantar flexion, knee and hip flexion. | CAI was compared to the control group | TTS was longer on anteriorposterior in CAI (reduced dynamic stability). Decreased sagittal knee flexion at ground impact in CAI. No main differences were seen in ankle plantar flexion or hip flexion. |
| C. Doherty, (2015) | 5 | 28 subjects with CAI. 42 subjects who were ankle copers |
70 | CAI: 23.2 ± (4.9) Copers: 22.7 ± (1.7) |
Drop landing task onto one leg | Kinematics and kinetics of ankle, knee and hip. Ground reaction forces (GRF) | CAI group was compared to ankle copers | CAI group had position of increased hip flexion during pre-initial contact, reduced flexor movement following initial contact, and an increase in hip joint stiffness after initial contact. No differences between angular displacement of the knee and ankle in CAI and copers group. |
| R. D. Ridder, (2015) | 5 | 28 subjects with CAI 28 subjects were the control |
56 | CAI: 22.3 ± (2.7) Control: 22.5 ± (1.6) |
Barefoot forward and side jumps | Ground reaction forces (GRF), Ankle Knee and Hip ROM. | CAI group is compared to control group | Analysis of kinematics curves of the hip, knee and ankle displayed no differences between the CAI and control group. |
| C. Brown, (2011) | 5 | 21 mechanical ankle instability 23 functional ankle instability 20 copers 24 control |
88 | MAI: M 18.6 ± (3.3) F 19.9 ± (1.0) FAI: M 20.5 ± (1.7) F 20.1 ± (1.5) Copers: M 19.8 ± (1.2) F 20.3 ± (1.1) Control: M 19.8 ± (1.3) F 20.2 ± (1. 0) |
Single leg landings from a 50% maximum vertical jump | Lower extremity kinematics, trunk movement and ground reaction forces (GRF) | Comparisons were made between the four groups | No differences seen between groups for ankle plantar flexion and dorsiflexion, inversion/eversion, internal-external rotation. Knee rotation the FAI group and copers were less variable than controls. Copers were less variable for knee flexion than controls. For hip flexion MAI, FAI, and copers were less variable than controls. MAI was less variable than controls for hip abduction. The FAI group was less variable than control in hip flexion during the lateral jump. The MAI and FAI were less variable than controls in hip abduction during the anterior jump. For the trunk the MAI and control were less variable than FAI in trunk lateral flexion. |
| E. Delahunt, (2006) | 5 | 24 subjects with Functional Instability 24 subjects were the control |
FI: 25 ± (1.3) Control: 22 ± (0.84) |
Single leg jump onto a force plate | Compare electromyography (EMG) of rectus femoris, peroneus longus, tibialis anterior, and soleus. Compare angular displacement and angular velocities of the lower leg. Also compare kinetic patterns. | Functional instability group and a control group | The functional instability group indicated a decrease in pre-IC peroneus longus IEMG. There were no differences shown in the other three muscles. FI subjects were less efficient than the control in reaching the closed packed position of the ankle joint. Subjects had a decreased dorsiflexion position. FI subjects had a less externally rotated hip during pre-IC. |
DISCUSSION
The possibility of changes in the ankle affecting structures higher on the kinetic chain has potential impacts beyond traditional ankle rehabilitation. Changes in athlete range of motion during landing tasks have been investigated for potential increased risk of injury (1,13). Decreased knee flexion has been shown to be a risk factor for non-contact knee injuries. Increased hip flexion is a common way subjects use to help dissipate forces when landing. Decreased dorsiflexion limits the amount of forces that can be dissipated and the range of motion in the lower extremity. The review of research identified that results on knee flexion were mixed. Decreased knee flexion was found in two of the studies to correlate to chronic ankle instability (12,23). Two studies found no correlation between chronic ankle instability and decreased knee flexion (5,7). Hip flexion was increased in one study with subjects who had CAI and three other studies found no difference (5,7,12,23). One study found decreased dorsiflexion and two studies found no difference in dorsiflexion (5,23). In addition, increased Time to stabilization (TTS) typically means that the subject was unable to dissipate forces as well and landed with a high center of mass. TTS was greater in subjects with CAI (12). Decreased hip external rotation is a risk factor for non-contact knee injuries because it can cause genu valgum. Delahunt et al. (6) found decreased hip external rotation in patients with CAI. The tasks used in the two studies that found decreased knee flexion were a vertical stop jump and a double leg take off while landing on one leg (12,23). Previous research has indicated that decreased knee flexion, specifically 10–30 degrees, is when the quadriceps exerts the most anterior tibial shear force (13). The more the ankle, knee and hip are flexed the greater ability they have at dissipating energy which results in less force being transferred to the knee (1). When the knee is in an increased extension the hamstring resultant force is parallel to the ACL, which limits the hamstrings ability to restrict anterior tibial movement.
In the two studies where knee flexion was not decreased the subjects used different jumping tasks in one of the studies and the other study did not have a control group (5,7). One study used forward and side jumps while being barefoot to measure lower extremity kinematics (5). In the two studies where CAI correlated with decreased knee flexion the subjects performed jumps to reach 50% of the maximum vertical height. In the study done by De Ridder et al. the subjects jumped horizontally instead of vertical over a 30 cm hurdle (5). They also performed a side jump over a 15cm hurdle. Since this study had the subjects jumping over objects this already forced their lower extremity to be in a flexed position to get over the hurdle. In the other study where knee flexion was not decreased CAI was compared to ankle copers (7). This study did not have a control group to compare to, so both experimental groups had previous ankle injuries.
An increase in time to stabilization was consistent with previous literature (13). Since the subjects were landing with less knee flexion they had a higher center of gravity (12). TTS deficits were only seen on the affected ankle however kinematic differences were seen bilaterally. Proprioception, dynamic stability, is a mechanism used to help reduce knee injuries by counteracting extreme forces (13).
Hip flexion was seen to be increased in the subjects with CAI while jumping off a platform and landing on one leg (7). Decreased hip flexion is thought to be a risk factor for non-contact knee injuries in the same way decreased knee flexion is (1). Since the hip is in a more extended position it is unable to absorb forces as well and greater forces are transmitted to the knee. However, in this study hip flexion was increased in the CAI group compared to the ankle coper group. One reason for the increase in hip flexion could be a preparatory mechanism to help dissipate forces during impact for patients with CAI. This is a feed forward pattern by the body due to existing awareness of joint instability (12). However, after initial contact hip joint stiffness increased which limits the body’s ability to attenuate forces (7). Landing in an increased hip flexion not only increased stiffness in the sagittal plane it can also affect other lower extremity muscles ability to control excessive motion and reduce ground forces. In the two studies that found no difference in hip flexion they performed procedures that did not require jumping off a platform. Gribble and Robinson acknowledged that since their jump landing task only required 50% of vertical max it did not require enough contribution from the hip (12).
Dorsiflexion range of motion received mixed results throughout the studies. Terada et al. was the only study to measure both ankle dorsiflexion and knee flexion between a CAI group and control group (23). In that study knee flexion was significantly decreased and dorsiflexion approached significance. Patients with greater dorsiflexion range of motion have shown to be able to dissipate ground reaction forces better (9). Increased dorsiflexion also allows the knee to get into greater flexion (15). Since the ankle was unable to reach a normal range of motion or a closed packed position it would be prone to more lateral ankle sprains (6). Therefore, decreased dorsiflexion increases CAI chances, which in result increases risk factors that can lead to non-contact knee injuries. Brown et al. found no differences between CAI and the control group for dorsiflexion (3). In addition, variability in movement was significant with a decreased performance in the CAI group. However, the effect sizes between the two groups were negligible. Therefore, even though this study has significant data it was not clinically relevant.
Delahunt et al. found decreased hip external rotation in patients with CAI (6). This finding cannot be completely explained but helps show that CAI affects the whole kinetic chain of the lower leg. Decreased external rotation puts the knee in a valgus position, which is a severe risk factor for non-contact knee injuries (1). Decreased hip musculature activation has also been shown to limit quadriceps and hamstrings activation (13).
Patients with chronic ankle instability demonstrate decreased knee flexion (Grade of recommendation = B). Decreased knee flexion has shown to be a key risk factor in non-contact knee injuries. Ankle dorsiflexion and time to stabilization had significant differences between CAI and the control group but it is uncertain how these results directly relate to non-contact knee injuries. CAI had little to no effect on the hip flexion range of motion (Grade of recommendation = B). In the future, more research needs to be done comparing chronic ankle instability to non-contact knee injury rates.
REFERENCES
- 1.Alentorn-geli E, Myer GD, Silvers HJ, et al. Prevention of non-contact anterior cruciate ligament injuries in soccer players. part 1: mechanisms of injury and underlying risk factors. Knee Surg Sports Traumatol Arthrosc. 2009;17(7):705–29. doi: 10.1007/s00167-009-0813-1. [DOI] [PubMed] [Google Scholar]
- 2.Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005;39(3):e14. doi: 10.1136/bjsm.2004.011676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown C, Bowser B, Simpson KJ. Movement variability during single leg jump landings in individuals with and without chronic ankle instability. Clin Biomech (Bristol, Avon) 2012;27(1):52–63. doi: 10.1016/j.clinbiomech.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 4.De ridder R, Willems T, Vanrenterghem J, Robinson MA, Palmans T, Roosen P. Multi-segment foot landing kinematics in subjects with chronic ankle instability. Clin Biomech (Bristol, Avon) 2015;30(6):585–92. doi: 10.1016/j.clinbiomech.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 5.De ridder R, Willems T, Vanrenterghem J, Robinson MA, Roosen P. Lower limb landing biomechanics in subjects with chronic ankle instability. Med Sci Sports Exerc. 2015;47(6):1225–31. doi: 10.1249/MSS.0000000000000525. [DOI] [PubMed] [Google Scholar]
- 6.Delahunt E, Monaghan K, Caulfield B. Changes in lower limb kinematics, kinetics, and muscle activity in subjects with functional instability of the ankle joint during a single leg drop jump. J Orthop Res. 2006;24(10):1991–2000. doi: 10.1002/jor.20235. [DOI] [PubMed] [Google Scholar]
- 7.Doherty C, Bleakley C, Hertel J, et al. Coordination and symmetry patterns during the drop vertical jump, 6-months after first-time lateral ankle sprain. J Orthop Res. 2015;33(10):1537–44. doi: 10.1002/jor.22915. [DOI] [PubMed] [Google Scholar]
- 8.Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014;44(1):123–40. doi: 10.1007/s40279-013-0102-5. [DOI] [PubMed] [Google Scholar]
- 9.Fong CM, Blackburn JT, Norcross MF, Mcgrath M, Padua DA. Ankle-dorsiflexion range of motion and landing biomechanics. J Athl Train. 2011;46(1):5–10. doi: 10.4085/1062-6050-46.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Glasgow P, Bleakley CM, Phillips N. Being able to adapt to variable stimuli: the key driver in injury and illness prevention? Br J Sports Med. 2013;47(2):64–5. doi: 10.1136/bjsports-2012-091960. [DOI] [PubMed] [Google Scholar]
- 11.Gribble PA, Hertel J, Plisky P. Using the Star Excursion Balance Test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. J Athl Train. 2012;47(3):339–57. doi: 10.4085/1062-6050-47.3.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gribble PA, Robinson RH. Alterations in knee kinematics and dynamic stability associated with chronic ankle instability. J Athl Train. 2009;44(4):350–5. doi: 10.4085/1062-6050-44.4.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Griffin LY, Agel J, Albohm MJ, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8(3):141–50. doi: 10.5435/00124635-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37(4):364–375. [PMC free article] [PubMed] [Google Scholar]
- 15.Hoch MC, Farwell KE, Gaven SL, Weinhandl JT. Weight-bearing dorsiflexion range of motion and landing biomechanics in individuals with chronic ankle instability. J Athl Train. 2015;50(8):833–9. doi: 10.4085/1062-6050-50.5.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–9. [PMC free article] [PubMed] [Google Scholar]
- 17.Konradsen L, Bech L, Ehrenbjerg M, Nickelsen T. Seven years follow-up after ankle inversion trauma. Scand J Med Sci Sports. 2002;12(3):129–35. doi: 10.1034/j.1600-0838.2002.02104.x. [DOI] [PubMed] [Google Scholar]
- 18.Moher D, Liberati A, Tetzlaff J, Altman DG and PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Medicine. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pionnier R, Découfour N, Barbier F, Popineau C, Simoneau-buessinger E. Unipodal landing in individuals with unilateral chronic ankle instability. Comput Methods Biomech Biomed Engin. 2014;17(Suppl 1):100–1. doi: 10.1080/10255842.2014.931334. [DOI] [PubMed] [Google Scholar]
- 20.Stiffler MR, Pennuto AP, Smith MD, Olson ME, Bell DR. Range of motion, postural alignment, and LESS score differences of those with and without excessive medial knee displacement. Clin J Sport Med. 2015;25(1):61–6. doi: 10.1097/JSM.0000000000000106. [DOI] [PubMed] [Google Scholar]
- 21.Swenson DM, Yard EE, Fields SK, Comstock RD. Patterns of recurrent injuries among US high school athletes. Am J Sports Med. 2009;37(8):1586–93. doi: 10.1177/0363546509332500. [DOI] [PubMed] [Google Scholar]
- 22.Terada M, Pfile KR, Pietrosimone BG, Gribble PA. Effects of chronic ankle instability on energy dissipation in the lower extremity. Med Sci Sports Exerc. 2013;45(11):2120–8. doi: 10.1249/MSS.0b013e31829a3d0b. [DOI] [PubMed] [Google Scholar]
- 23.Terada M, Pietrosimone B, Gribble PA. Individuals with chronic ankle instability exhibit altered landing knee kinematics: potential link with the mechanism of loading for the anterior cruciate ligament. Clin Biomech (Bristol, Avon) 2014;29(10):1125–30. doi: 10.1016/j.clinbiomech.2014.09.014. [DOI] [PubMed] [Google Scholar]
- 24.Van rijn RM, Van os AG, Bernsen RM, Luijsterburg PA, Koes BW, Bierma-zeinstra SM. What is the clinical course of acute ankle sprains? a systematic literature review. Am J Med. 2008;121(4):324–331. doi: 10.1016/j.amjmed.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 25.Webster KA, Gribble PA. Functional rehabilitation interventions for chronic ankle instability: a systematic review. J Sport Rehabil. 2010;19(1):98–114. doi: 10.1123/jsr.19.1.98. [DOI] [PubMed] [Google Scholar]
- 26.Weinhandl JT, Smith JD, Dugan EL. The effects of repetitive drop jumps on impact phase joint kinematics and kinetics. J Appl Biomech. 2011;27(2):108–15. doi: 10.1123/jab.27.2.108. [DOI] [PubMed] [Google Scholar]