Abstract
Exercise intensity is a critical component of the exercise prescription model. However, current research employing various non-specific exercise intensity protocols have reported wide variability in maximum oxygen uptake (VO2max) improvement after training, suggesting a present lack of consensus regarding optimal heart rate (fC) training zones for maximal athletic performance. This study examined the relationship between percentage of time (%time) spent training between the metabolic (VO2θ) and ventilatory thresholds (VEθ), and the resultant change in markers of aerobic performance. Thirteen (6 males) collegiate club-level triathletes were recruited for eight weeks of remote fC monitoring during all running and cycling sessions. Participants donned a forearm-worn optical fC sensor paired to a smartphone that collected and stored fCs. Subjects were categorized into Low and High groups based on %time spent training between the VO2θ and VEθ. Significant increases were observed in relative VO2max (P = 0.007, g = 0.48), VO2θ (P = 0.018, g = 0.35), and VEθ (P = 0.030, g = 0.29) from baseline after eight weeks for both groups. A 95% bootstrapped confidence interval that did not include zero (−0.38, −0.03; g = 1.26) revealed a large and significantly greater change in VO2θ in the High group (0.37 ± 0.15 L/min) versus the Low group (0.17 ± 0.14 L/min). No significant differences were observed in other variables between groups. Increasing triathletes’ %time spent exercising between VO2θ and VEθ may optimize increases in VO2θ after eight weeks of training.
Keywords: Maximal oxygen uptake, ventilatory threshold, exercise intensity, training zones, athletic performance
INTRODUCTION
The goal of any exercise program, whether for a competitive athlete or a general fitness enthusiast, is to maximize effectiveness. Exercise prescription is frequently comprised of four components, sometimes referred to as the FITT principle: frequency, intensity, time, and type of exercise. Of these principles, intensity may play a disproportionate role in driving improvement in cardiorespiratory (VO2) response to exercise training (21). Exercising at suboptimal intensity limits improvement while exceeding optimal levels leads to overtraining and increased injury risk (11). Thus, identification of optimal exercise intensity is crucial for maximizing results.
Traditionally, exercise intensity has been prescribed following the relative percent method (10) with guidance to perform exercise at a certain percentage of maximum heart rate (%fCmax), heart rate reserve (%fCR), or oxygen uptake reserve (%VO2R). Limitations in this approach resulting from wide variability between individuals in metabolic stress at a given percentage of these variables have been reported for decades (12,17,18,26). More specifically, because unbuffered lactate begins accumulating at varying percentages of maximal exertion based on individual fitness level and other factors, and the resulting metabolic acidosis has a pronounced impact on exercise performance, the relative percent methods fails to achieve consistent intensity recommendations across individuals (12). Thus, attempts at more personalized exercise intensity prescription have focused on identifying target zones based on metabolic variables.
Recently the threshold-based fC zone method has garnered attention amongst coaches and athletes as the ideal exercise prescription paradigm. This method typically requires identification of two thresholds—metabolic threshold (VO2θ) and ventilatory threshold (VEθ)— derived from gas exchange and then demarcates three fC zones either below, between, or above these thresholds (3). VO2θ is analogous to the lactate threshold and defined as the disproportionate increase in carbon dioxide output (VCO2) relative to oxygen uptake (VO2) that occurs as a result of the CO2 produced from the bicarbonate buffering of lactic acid. VEθ is analogous to the respiratory compensation point and defined as the disproportionate increase in minute ventilation relative to VCO2 secondary to the continued accumulation of lactic acid. The threshold-based system of exercise intensity prescription has been shown to be superior to the relative percent method both in degree of VO2max improvement and in minimizing non-responders (27). However, there is a lack of agreement on the optimal distribution of training across the fC spectrum such as the recommendation of predominantly low-intensity (16) versus high-intensity training (13). Thus, it remains unknown what percentage of training time (%time) is optimal to spend in each target fC zone and whether the answer is contingent on fitness level (7,23).
This pilot prospective study was performed to categorize the self-selected training intensities of collegiate triathletes by identifying the percent of time spent in each of three fC zones and the subsequent effectiveness of that percentage on training outcomes. It was hypothesized that participants who spend the greatest proportion of time training between VO2θ and VEθ will demonstrate the largest improvements in aerobic capacities.
METHODS
Participants
Thirteen triathletes (6 males) aged 18–25 years were recruited from the club-level triathlete team at University of California, Los Angeles (UCLA) through flyers, direct email, and word of mouth. Because no previous data exist for these parameters in this population, this investigation was treated as a pilot study and thus sample size was not formally determined. Subjects agreed to eight weeks of fC monitoring during all running and cycling sessions and were instructed not to deviate from their typical diet or training regimens. Pre- and post-eight-week testing occurred in the UCLA Exercise Physiology Research Laboratory. All participants were well hydrated and refrained from consuming alcohol and caffeine for at least 24 hours, as well as engaging in strenuous exercise at least 12 hours, prior to testing. The inclusion criterion was active membership in a university club-level triathlon team. Exclusion criteria included the presence of musculoskeletal, cardiovascular, pulmonary, metabolic, or other disorders that would preclude high-intensity exercise testing. Pre- and post-testing included body mass and body fat percentage (%BF) measures and a continuous, incremental maximal treadmill test (VO2max). This study was performed in accordance with the ethical standards of the Helsinki Declaration and was approved by the UCLA Institutional Review Board. All participants provided written informed consent.
Protocol
Anthropometric Measures: Using a recently validated (2), octopolar, multi-frequency bioelectrical impedance analysis scale (InBody R20 scale; Biospace, Inc, Seoul Korea), participants stood upright with the ball and heel of each foot on two metallic footpads with both hands gripping a bar with metallic electrodes. The instrument measured both weight and body fat percentage (%BF) within 30 seconds. Height was measure prior to testing using a wall-mounted stadiometer.
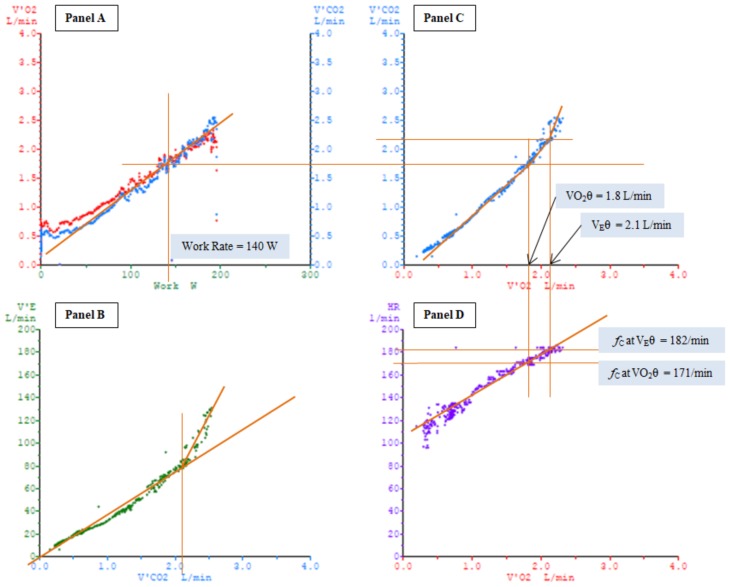
Aerobic Capacity Assessment: Maximum oxygen uptake (VO2max), VO2θ, and VEθ were calculated via gas exchange during an incremental, symptom-limited maximal treadmill exercise test using standard procedures outlined in a prior investigation (3). VO2, VCO2, and pulmonary minute ventilation (VE) were measured breath-by-breath with a metabolic measurement system (Oxycon Pro; CareFusion, Yorba Linda, CA, USA). These data were continuously monitored and recorded during three minutes of warm-up and throughout the exercise test. Similarly, fC was continuously monitored with a 12-lead EKG interfaced to the metabolic measurement system for display and storage. Testing started immediately following a 3-minute walking warm-up with the treadmill set to 4 mph and a grade of 1%. Speed on the treadmill was increased 0.5 mph every minute and grade increased 1% every 2 minutes. Trained and experienced investigators conducted all testing in accordance with established guidelines for cardiopulmonary exercise testing. VO2max was determined from the highest 15-second average and accepted as maximal in the presence of a plateau in VO2 with increasing work rate. Gas exchange indices of VO2 at thresholds were ascertained graphically from plots of VCO2 versus VO2 and/or the ventilatory equivalents for oxygen (VE/VO2) and carbon dioxide (VE/VCO2). Two investigators independently selected VO2 at VO2θ and VEθ using the methodology described in a previous publication (3) and outlined in Figure 1. Briefly, VO2θ was identified as the first inflection point in the VCO2 versus VO2 data, which is indicative of CO2 production outpacing O2 consumption. VEθ was identified as the first inflection point in the VE versus VCO2 data, indicative of ventilation outpacing the need to clear CO2, and then converted to the corresponding VO2 value. If both investigators selected VO2 values at these thresholds which agreed within 150 ml/min, the average was used. If the difference was > 150 ml/min, a consensus value was achieved by discussion. Rating of perceived exertion was taken periodically during and immediately following the test using the Borg 6–20 scale (1).
Figure 1.
Panel A: Diagrammatic representation of oxygen uptake (VO2) in red and carbon dioxide output (VCO2) in blue as a function of work. Panel B: Diagrammatic representation of minute ventilation (VE) as a function of VCO2. VCO2 was measured at the inflection point in VE. Panel C: Diagrammatic representation of VCO2 as a function of VO2. Metabolic threshold (VO2θ) was determined by measuring the VO2 at which the first inflection point in VCO2 occurred. Ventilatory threshold (VEθ) was determined by measuring the VO2 at the corresponding value for VCO2 derived from Panel B. Panel D: Diagrammatic representation of heart rate (fC) as a function of VO2. fC at VO2θ, which served as the boundary between Zone 1 and Zone 2, was determined by measuring the fC at the corresponding value for VO2 derived from Panel C. The identical process was employed to obtain the fC at VEθ, the boundary between Zone 2 and Zone 3.
Heart Rate Zone Threshold Determination: Zone 1 was defined as fCs below VO2θ. Zone 2 was marked by fCs between VO2θ and VEθ (inclusive). Finally, Zone 3 included only fCs above VEθ.
Remote Heart Rate Monitoring: Remote fC monitoring via smartphone technology has been validated (8) and recently implemented in a randomized controlled trial for exercise-based cardiac rehabilitation (15). After baseline VO2max testing, each subject wore a forearm band fC monitor (Rhythm+™; Scosche Industries, Oxnard, California) during all running and cycling sessions. The fC monitor collected fC data every second and paired with any Bluetooth-compatible device. Subjects used their personal cell phones to pair the fC monitor to a smartphone application (iRunner; iReader, Inc., Hong Kong). This application allowed subjects to see their fC in real time during training and upload the data following each session. Along with fC data, subjects provided method of training (running or cycling) and self-reported exercise intensity for each workout.
Statistical Analysis
Heart rate data analysis was performed using Python (version 2.7.11; Python Software Foundation, Wilmington, Delaware). Percentage of fC data below, within, and above ranges delineated by VO2θ and VEθ were then programmatically calculated. After plots for each subject were generated, mean percentages for time spent in each fC zone during training were calculated for all subjects (Figure 2). Participants were then divided into two groups based on the %time spent in Zone 2: Low (< 20%) and High (≥ 20%). Analysis was performed in Excel (Microsoft Corporation, Redmond, Washington) and R (version 3.5.1; R Foundation for Statistical Computing, Vienna, Austria). Descriptive statistics are presented as mean ± standard deviation (SD). Statistical significance was determined based on α = 0.05 and all tests were two-tailed. Continuous variables were first assessed for normality via Shapiro-Wilk tests. Comparisons at baseline and after eight weeks of training were made by paired t-tests using a Holm-Bonferroni correction to control the familywise error rate. Effect sizes were measured by Hedges’ g. Due to the small sample sizes, the changes in variables between the Low and High groups were analyzed using nonparametric bootstrapping with 10,000 replicates to yield a bias-corrected and accelerated 95% confidence interval.
RESULTS
Data at baseline and after eight weeks of training were collected for nine subjects who completed all testing and monitoring. Four of the 13 participants did not complete the study due to incomplete remote fC monitoring (n = 1), failure to complete final testing (n = 2), or injury (n = 1). The breakdown of %time spent in each of the three fC zones is displayed in Table 1. Six triathletes constituted the Low group, and three comprised the High group. All subjects trained primarily in Zone 1 (84.2 ± 15.9%); however, triathletes in the Low group spent significantly more time in Zone 1 (94.2 ± 3.0%) than those in the High group (64.2 ± 9.4%; P = 0.026). In contrast, the Low group trained significantly less in Zone 2 (5.1 ± 2.3%) than the High group (28.5 ± 4.9%; P = 0.008).
Table 1.
Percentage of time training in the three heart rate zones.
| All (n = 9) | Low (n = 6) | High (n = 3) | |
|---|---|---|---|
| Zone 1 (%) | 84.2 ± 15.9 | 94.2 ± 3.0 | 64.2 ± 9.4 |
| Zone 2 (%) | 12.9 ± 12.1 | 5.1 ± 2.3 | 28.5 ± 4.9 |
| Zone 3 (%) | 3.0 ± 5.8 | 0.8 ± 0.9 | 7.3 ± 9.4 |
Values are mean ± SD. Zone 1 = below the metabolic threshold; Zone 2 = between the metabolic and ventilatory thresholds; Zone 3 = above the ventilatory threshold.
At baseline, all participants were at or above the 90th percentile for VO2max based on the American College of Sports Medicine’s age- and sex-matched cardiorespiratory rankings (7) and there were no differences in any aerobic capacity variables between the groups (Table 2). Significant increases were observed in absolute VO2max (P = 0.030, g = 0.29), relative VO2max (P = 0.007, g = 0.48), VO2θ (P = 0.018, g = 0.35), and VEθ (P = 0.030, g = 0.29) after eight weeks of training in all participants (Table 3). No changes occurred in body mass, %BF, or VO2θ/ VO2max. The change in outcome variables between the Low and High groups after eight weeks is depicted in Table 4. A 95% confidence interval that did not include zero (−0.38, −0.03; g = 1.26) revealed a large and significantly greater change in VO2θ in the High group (0.37 ± 0.15 L/min) versus the Low group (0.17 ± 0.14 L/min). Changes in all other measures lacked significance and exhibited small effect sizes.
Table 2.
Outcome variables at baseline and after eight weeks for participants in the Low and High groups.
| Low at Baseline (n = 6) | Low After 8 Weeks (n = 6) | High at Baseline (n = 3) | High After 8 Weeks (n = 3) | |
|---|---|---|---|---|
| Body Mass (kg) | 66.8 ± 7.3 | 65.8 ± 7.3 | 65.5 ± 11.5 | 65.4 ± 11.4 |
| Body Fat (%) | 19.3 ± 8.6 | 19.7 ± 7.3 | 15.8 ± 8.0 | 15.6 ± 7.3 |
| VO2max (L/min) | 3.38 ± 0.84 | 3.58 ± 0.92 | 3.60 ± 0.47 | 3.9 ± 0.60 |
| Relative VO2max (ml/min/kg) | 50.4 ± 9.0 | 54.0 ± 8.7 | 55.8 ± 3.2 | 60.3 ± 1.4 |
| VO2θ (L/min) | 2.92 ± 0.77 | 3.08 ± 0.75 | 2.90 ± 0.35 | 3.3 ± 0.35 |
| VO2θ/VO2max (%) | 86.0 ± 2.5 | 86.3 ± 2.1 | 79.9 ± 2.1 | 83.5 ± 4.0 |
| VEθ (L/min) | 3.25 ± 0.82 | 3.45 ± 0.88 | 3.50 ± 0.46 | 3.8 ± 0.51 |
Values are mean ± SD. VO2max = maximum oxygen uptake; relative VO2max = maximum oxygen uptake normalized by body weight; VO2θ = oxygen uptake at metabolic threshold; VO2θ/VO2max = metabolic threshold as a percent of maximum oxygen uptake; VEθ = oxygen uptake at ventilatory threshold.
Table 3.
Outcome variables at baseline and after eight weeks for all participants
| Baseline (n= 9) | 8 Weeks (n = 9) | P-value† | Hedges’ g | |
|---|---|---|---|---|
| Body mass (kg) | 66.4 ± 8.2 | 65.7 ± 8.1 | 0.747 | 0.08 |
| Body Fat (%) | 18.1 ± 8.1 | 18.4 ± 7.1 | 0.785 | 0.03 |
| VO2max (L/min) | 3.47 ± 0.72 | 3.70 ± 0.81 | 0.030* | 0.29 |
| Relative VO2max (ml/min/kg) | 52.2 ± 7.8 | 56.1 ± 7.6 | 0.007** | 0.48 |
| VO2θ (L/min) | 2.91 ± 0.63 | 3.14 ± 0.63 | 0.018* | 0.35 |
| VO2θ/VO2max (%) | 84.0 ± 3.8 | 85.3 ± 3.0 | 0.747 | 0.38 |
| VEθ (L/min) | 3.33 ± 0.70 | 3.56 ± 0.76 | 0.030* | 0.29 |
Values are mean ± SD. VO2max = maximum oxygen uptake; relative VO2max = maximum oxygen uptake normalized by body weight; VO2θ = oxygen uptake at metabolic threshold; VO2θ/VO2max = metabolic threshold as a percent of maximum oxygen uptake; VEθ = oxygen uptake at ventilatory threshold;
after correcting for multiple comparisons;
P < 0.05;
P < 0.01.
Table 4.
Change in outcome variables after eight weeks for participants in the Low and High groups.
| Low (n = 6) | High (n = 3) | 95% CI† | Hedges’ g | |
|---|---|---|---|---|
| ΔBody Mass (kg) | −1.0 ± 2.1 | −0.1 ± 0.4 | (−3.02, 0.27) | 0.46 |
| ΔBody Fat (%) | 0.5 ± 3.4 | −0.1 ± 0.8 | (−1.62, 3.62) | 0.18 |
| ΔVO2max (L/min) | 0.20 ± 0.20 | 0.30 ± 0.17 | (−0.33, 0.08) | 0.46 |
| ΔRelative VO2max (ml/min/kg) | 3.6 ± 2.4 | 4.5 ± 1.7 | (−3.82, 1.10) | 0.35 |
| ΔVO2θ (L/min) | 0.17 ± 0.14 | 0.37 ± 0.15 | (−0.38, −0.03)* | 1.26 |
| Δ(VO2θ/VO2max) (%) | 0.3 ± 3.0 | 3.6 ± 3.3 | (−7.27, 0.22) | 0.95 |
| ΔVEθ (L/min) | 0.20 ± 0.22 | 0.27 ± 0.06 | (−0.25, 0.08) | 0.32 |
Values are mean ± SD. No significant differences were observed between groups at baseline. VO2max = maximum oxygen uptake; relative VO2max = maximum oxygen uptake normalized by body weight; VO2θ = oxygen uptake at metabolic threshold; VO2θ/VO2max = metabolic threshold as a percent of maximum oxygen uptake; VEθ = oxygen uptake at ventilatory threshold;
difference of means calculated from 10,000 bootstrap replicates;
does not include zero, suggesting a statistically significant difference.
DISCUSSION
This investigation is the first to experimentally derive individualized fC zones for collegiate triathletes, and examine the effect of time training in each zone on aerobic capacities. The most important finding of this study is the significantly greater increases in VO2θ that occurred in triathletes who spent more than 20% of training time in Zone 2 (between VO2θ and VEθ) compared to those who spent greater than 80% of training time in Zone 1 (below VO2θ). While on average all participants saw improvement in this measure, athletes in the High group more than doubled their increase in VO2θ compared to the Low group. Conversely, there was no significant difference between groups for change in VO2max. While VO2max is arguably the most common measure of aerobic capacity, some evidence suggests that VO2θ may be comparable or superior (6). Furthermore, it is not uncommon for conditioned athletes to increase VO2θ as a result of training without a corresponding rise in VO2max (4). Improving VO2θ allows athletes to increase oxygen uptake—and thus their potential work output—without a concomitant increase in lactate accumulation. That is, athletes with a higher VO2θ can maintain a greater level of performance before the development of exercise-induced metabolic acidosis. Our results, therefore, offer evidence for coaches and triathletes that training at least 20% of the time between VO2θ and VEθ may optimize the improvements in aerobic performance obtained from workouts. However, it is important to note that the High group also spent a greater percentage of training time in Zone 3 (above VEθ) compared to the Low group (7.3 ± 9.4% versus 0.8 ± 0.9%, respectively). It is possible this difference also contributed to the significantly greater increase in VO2θ observed in the High group.
Despite a growing body of research examining intensity-dependent training methodologies, a consensus remains elusive. One of the earliest studies to test a threshold-based model concluded that college-aged women who trained above the lactate threshold for 12 weeks demonstrated greater improvement in VO2 at the lactate threshold (equivalent to VO2θ) than participants who exercised at a lower intensity (9). Similarly, a randomized control trial comparing a threshold-based model to the relative percent method reported that participants who trained with reference to thresholds experienced a greater increase in VO2max and reduced the inter-individual variation in VO2max training response (27). In the present study, the distribution of participants’ %time training was pyramidal: the greatest proportion of time was spent exercising at lower intensities, i.e., Zone 1, and diminished as intensity increased (Table 1). Pyramidal training intensity distributions are common in the literature (5,25) although wide variability can exist across studies. The pyramidal stratification in Treff et al. reported elite rowers’ %time training in Zone 1 as 93 ± 2%, in Zone 2 as 3 ± 2%, and in Zone 3 as 2 ± 1% (25) which mimics the Low group in the present study. The authors found no difference in VO2max and average power between athletes that trained according to a pyramidal versus polarized distribution, and attributed the lack of significance to nearly identical %time spent in Zone 1 (93 ± 2% versus 94 ± 3%). Notably, greater improvements were observed in the present study from athletes who shifted training time out of Zone 1 and into Zones 2 and 3. This underscores the efficacy of including higher intensity training or at least suggests the greater importance of doing so as fitness improves. This interpretation is supported by a previous meta-analysis which concluded training near the lactate threshold was an adequate stimulus for sedentary individuals but higher intensities may be required for more conditioned athletes (14).
In contrast, several investigations argue against training between VO2θ and VEθ. Esteve-Lanao et al. placed 12 sub-elite runners into an exercise regimen that emphasized greater %time training in Zone 1 versus Zone 2 (5). Athletes in the lower intensity group spent 80.5 ± 1.8% in Zone 1 and 11.8 ± 2.0% in Zone 2 while runners in the higher intensity group spent 66.8 ± 1.1% in Zone 1 and 24.7 ± 1.5% in Zone 2. This distribution of %time training across all three zones in both groups is pyramidal and the higher intensity group closely resembles the corresponding values obtained in the High group in the present study (Table 1). The authors found that participants in the lower intensity group demonstrated greater improvements in running performance as measured by time required to complete 10.4-km race. Aerobic capacities, however, were not assessed. As the %time spent in Zone 1 for the lower intensity group differed greatly between these two studies (80.5 ± 1.8% versus 94.2 ± 3.0%), it is possible the results are not contradictory but indicative that the true optimal %time in Zone 1 may lie somewhere between the values reported in the present study (64.2 ± 9.4% in the High group and 94.2 ± 3.0% in the Low group). Other studies have compared a threshold-based approach against a polarized training program (20,22,24). For example, small differences in favor of a polarized model were found in recreational 10K runners with respect to race time (20). The same investigators also studied correlations between Ironman triathletes’ %time training in Zone 1 versus Zone 2 and performance time in competition (19). A strong positive correlation (r = 0.94) was reported between %time training in Zone 2 and race time—suggestive of worse performance—while a strong negative correlation (r = −0.92) existed between %time training in Zone 1 and race time. A recent meta-analysis of three studies corroborated the aforementioned findings by concluding that a polarized model offers a moderate improvement in time-trial performance time over a threshold-based approach (22).
In sum, the strengths of the present investigation stem from its novelty, relevance, and practicality in aerobic exercise training. While the participants were exclusively triathletes, this does not preclude the application of the results to other athletic disciplines. The potential improvement in VO2θ by increasing the %time training in Zone 2 to at least 20% can be readily implemented into the regimen of many endurance athletes yet several limitations to this finding ought to be considered. The small sample size precludes our ability to generate specific time percentages for an optimal polarized training program for endurance athletes. Additionally, fC during training for these triathletes was only monitored for cycling and running sessions. The forearm fC monitor was tested in a pool prior to the study, but recording during swim training sessions was not feasible due to loss of connection with the pairing device. A fC monitor capable of capturing data while swimming would be valuable in future studies to allow consideration of all three training modalities and provide a more complete picture of training intensity distribution. Furthermore, the total time spent training (in minutes) in addition to the %time training in each zone was not collected. Ideally, the duration of time training in each zone would be standardized as to eliminate its potential as a confounding variable. Lastly, since athletes self-selected the training intensity for each session in the present study, it is possible our results are significantly impacted by differences in athlete motivation and overall exercise volume. Future studies should incorporate larger groups randomly prescribed to exercise at various percentages above and below 20% in Zone 2 to further clarify the optimal percentage. It will also be important to delineate between effects resulting from training in Zone 2 versus Zone 3 and the long-term implications of each.
REFERENCES
- 1.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–381. [PubMed] [Google Scholar]
- 2.Dolezal BA, Lau MJ, Abrazado M, Storer TW, Cooper CB. Validity of two commercial grade bioelectrical impedance analyzers for measurement of body fat percentage. J Exerc Physiol Online. 2013;16(4):74–83. [Google Scholar]
- 3.Dolezal BA, Storer TW, Neufeld EV, Smooke S, Tseng CH, Cooper CB. A systematic method to detect the metabolic threshold from gas exchange during incremental exercise. J Sports Sci Med. 2017;16(3):396–406. [PMC free article] [PubMed] [Google Scholar]
- 4.Edwards AM, Clark N, Macfadyen AM. Lactate and ventilatory thresholds reflect the training status of professional soccer players where maximum aerobic power is unchanged. J Sports Sci Med. 2003;2(1):23–29. [PMC free article] [PubMed] [Google Scholar]
- 5.Esteve-Lanao J, Foster C, Seiler S, Lucia A. Impact of training intensity distribution on performance in endurance athletes. J Strength Cond Res. 2007;21(3):943–949. doi: 10.1519/R-19725.1. [DOI] [PubMed] [Google Scholar]
- 6.Ghosh AK. Anaerobic threshold: its concept and role in endurance sport. Malays J Med Sci. 2004;11(1):24–36. [PMC free article] [PubMed] [Google Scholar]
- 7.Graves RS, Mahnken JD, Perea RD, Billinger SA, Vidoni ED. Modeling percentile rank of cardiorespiratory fitness across the lifespan. Cardiopulm Phys Ther J. 2015;26(4):108–113. [PMC free article] [PubMed] [Google Scholar]
- 8.Gregoski MJ, Mueller M, Vertegel A, Shaporev A, Jackson BB, Frenzel RM, Sprehn SM, Treiber FA. Development and validation of a smartphone heart rate acquisition application for health promotion and wellness telehealth applications. Int J Telemed Appl. 2012:1–7. doi: 10.1155/2012/696324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Henritze J, Weltman A, Schurrer RL, Barlow K. Effects of training at and above the lactate threshold on the lactate threshold and maximal oxygen uptake. Eur J Appl Physiol Occup Physiol. 1985;54(1):84–88. doi: 10.1007/BF00426304. [DOI] [PubMed] [Google Scholar]
- 10.Jackson JH, Sharkey BJ, Johnston LP. Cardiorespiratory adaptations to training at specified frequencies. Res Q. 1968;39(2):295–300. [PubMed] [Google Scholar]
- 11.Jones BH, Cowan DN, Knapik JJ. Exercise, training and injuries. Sports Med. 1994;18(3):202–214. doi: 10.2165/00007256-199418030-00005. [DOI] [PubMed] [Google Scholar]
- 12.Katch V, Weltman A, Sady S, Freedson P. Validity of the relative percent concept for equating training intensity. Eur J Appl Physiol Occup Physiol. 1978;39(4):219–227. doi: 10.1007/BF00421445. [DOI] [PubMed] [Google Scholar]
- 13.Laursen PB, Jenkins DG. The scientific basis for high-intensity interval training: optimising training programmes and maximising performance in highly trained endurance athletes. Sports Med. 2002;32(1):53–73. doi: 10.2165/00007256-200232010-00003. [DOI] [PubMed] [Google Scholar]
- 14.Londeree BR. Effect of training on lactate/ventilatory thresholds: a meta-analysis. Med Sci Sports Exerc. 1997;29(6):837–843. doi: 10.1097/00005768-199706000-00016. [DOI] [PubMed] [Google Scholar]
- 15.Maddison R, Rawstorn JC, Rolleston A, Whittaker R, Stewart R, Benatar J, Warren I, Jiang Y, Gant N. The remote exercise monitoring trial for exercise-based cardiac rehabilitation (REMOTE-CR): a randomised controlled trial protocol. BMC Public Health. 2014;14:1236. doi: 10.1186/1471-2458-14-1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maffetone P. The Maffetone method: the holistic, low-stress, no-pain way to exceptional fitness. New York: McGraw-Hill Education; 1999. [Google Scholar]
- 17.Mann T, Lamberts RP, Lambert MI. Methods of prescribing relative exercise intensity: physiological and practical considerations. Sports Med. 2013;43(7):613–625. doi: 10.1007/s40279-013-0045-x. [DOI] [PubMed] [Google Scholar]
- 18.Meyer T, Gabriel HH, Kindermann W. Is determination of exercise intensities as percentages of VO2max or HRmax adequate? Med Sci Sports Exerc. 1999;31(9):1342–1345. doi: 10.1097/00005768-199909000-00017. [DOI] [PubMed] [Google Scholar]
- 19.Munoz I, Cejuela R, Seiler S, Larumbe E, Esteve-Lanao J. Training-intensity distribution during an ironman season: relationship with competition performance. Int J Sports Physiol Perform. 2014;9(2):332–339. doi: 10.1123/ijspp.2012-0352. [DOI] [PubMed] [Google Scholar]
- 20.Munoz I, Seiler S, Bautista J, Espana J, Larumbe E, Esteve-Lanao J. Does polarized training improve performance in recreational runners? Int J Sports Physiol Perform. 2014;9(2):265–272. doi: 10.1123/ijspp.2012-0350. [DOI] [PubMed] [Google Scholar]
- 21.Neufer PD. The effect of detraining and reduced training on the physiological adaptations to aerobic exercise training. Sports Med. 1989;8(5):302–320. doi: 10.2165/00007256-198908050-00004. [DOI] [PubMed] [Google Scholar]
- 22.Rosenblat MA, Perrotta AS, Vicenzino B. Polarized vs. threshold training intensity distribution on endurance sport performance: a systematic review and meta-analysis of randomized controlled trials. J Strength Cond Res. 2018 doi: 10.1519/JSC.0000000000002618. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 23.Seiler KS, Kjerland GO. Quantifying training intensity distribution in elite endurance athletes: is there evidence for an "optimal" distribution? Scand J Med Sci Sports. 2006;16(1):49–56. doi: 10.1111/j.1600-0838.2004.00418.x. [DOI] [PubMed] [Google Scholar]
- 24.Stoggl T, Sperlich B. Polarized training has greater impact on key endurance variables than threshold, high intensity, or high-volume training. Front Physiol. 2014;5:33. doi: 10.3389/fphys.2014.00033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Treff G, Winkert K, Sareban M, Steinacker JM, Becker M, Sperlich B. Eleven-week preparation involving polarized intensity distribution is not superior to pyramidal distribution in national elite rowers. Front Physiol. 2017;8:515. doi: 10.3389/fphys.2017.00515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weltman A, Snead D, Seip R, Schurrer R, Weltman J, Rutt R, Rogol A. Percentages of maximal heart rate, heart rate reserve and VO2max for determining endurance training intensity in male runners. Int J Sports Med. 1990;11(3):218–222. doi: 10.1055/s-2007-1024795. [DOI] [PubMed] [Google Scholar]
- 27.Wolpern AE, Burgos DJ, Janot JM, Dalleck LC. Is a threshold-based model a superior method to the relative percent concept for establishing individual exercise intensity? A randomized controlled trial. BMC Sports Sci Med Rehabil. 2015;7(16) doi: 10.1186/s13102-015-0011-z. [DOI] [PMC free article] [PubMed] [Google Scholar]