Abstract
The purpose of this study was to compare the standing lower extremity limb occlusion pressure (LOP) between two units. It was hypothesized that the Delfi unit, which utilizes a wider cuff (11.5 cm), would require significantly less LOP as compared to the KAASTU unit, which utilizes a narrow cuff (5 cm). Twenty-nine healthy participants (22 men, 7 women) mean age 24 years old (± 1.7 SD) volunteered. The procedure was identical for each cuff, completed with 5 minutes of rest in between. The cuff was placed on the proximal left thigh in the standing position. The initial pressure was set to 50 mmHg and then increased in 50 mmHg increments until complete arterial occlusion was achieved or the unit went to its maximum pressure. Arterial blood flow was determined by a mobile ultrasound measured at the left popliteal artery. Paired samples t-tests were used to determine differences in LOP (mmHg) between the Delfi and KAATSU unit cuffs. Significant differences were observed between the cuffs (wide: 239.4 mmHg vs. narrow: 500 mmHg; p < 0.001). We were able to achieve complete arterial occlusion with the wide cuff. The KAATSU unit reached maximum pressure with all participants, therefore we were unable to achieve complete arterial occlusion with the narrow cuff. Although achieving complete arterial occlusion is not indicated or safe for BFR training, relative pressures are used and determined as a percentage of LOP. Our study found that the relative pressure of the wide cuff is lower than the narrow cuff.
Keywords: Occlusion training, tourniquet training, rehabilitation, physical therapy
INTRODUCTION
In order to improve muscular strength and/or achieve muscle hypertrophy, the American College of Sports Medicine (ACSM) recommends resistance training at moderate to high intensity, which is at least 70% of an individual’s one repetition maximum (1RM) (13). Unfortunately, moderate to high intensity resistance training may not be feasible for clinical populations (i.e., acute injury, known disease, post-operative). Therefore, alternative methods to improve muscular strength and/or achieve muscle hypertrophy would be of benefit for these populations.
A once novel approach, but now a well-established method for increasing muscular strength and hypertrophy is known as blood flow restriction (BFR) training. A major benefit of BFR training is the ability to obtain an increase in strength and hypertrophy using intensities as low as 20% of an individual’s 1RM (10). BFR training entails applying a tourniquet-style cuff on the proximal aspect of the limb and then manually or pneumatically tightening the cuff prior to performing exercise. The cuff is tightened to a pressure that typically occludes venous outflow, while allowing partial arterial inflow.
Numerous methods for determining BFR training pressures exist. Absolute or arbitrary pressures have been utilized for BFR training (4), however absolute pressures may compromise safety (3, 9). Reduced arterial blood flow to exercising muscles may result in an abnormal hemodynamic response (i.e., heart rate and blood pressure) (15). This is a valid concern, especially in at-risk populations such as those with cardiovascular risk factors or known disease. Therefore, akin to individualized exercise prescription, the predominant recommendation is to prescribe BFR training pressures based on relative factors (2, 3, 6–9). Examples of these include the circumference of the limb, blood pressure, width and taper of the tourniquet cuff and underlying tissue characteristics.
Cuff width is a significant factor for determining safe BFR training pressures (3, 6–9). Wider cuffs require significantly less pressure to achieve arterial occlusion pressure (LOP) (i.e., 100% occlusion of arterial flow) (2, 8). Although achieving complete arterial occlusion is not indicated for BFR training, the ability to achieve venous occlusion at the lowest possible pressure is considered the safest tourniquet BFR training application. Therefore, setting the training pressure as a percentage of the individual’s LOP is recommended (9). LOP is defined as the minimum pressure required to stop the flow of arterial blood into the limb distal to the cuff (12). LOP is affected by numerous variables which are presented in Table 1 (14).
Table 1.
Variables affecting limb occlusion pressure (LOP).
|
Loenneke and colleagues found that a narrow cuff (5 cm) required significantly higher pressures to achieve arterial occlusion in the LE when compared to a wide cuff (13.5 cm) (8). When examining pulse elimination, narrow cuffs (i.e., 4.5 and 8 cm) were dependent on thigh circumference, whereas wider cuffs (i.e., 12 and 18 cm) were not. Rossow et al. demonstrated that when a narrow and wide cuff were inflated to the same standard pressure the wider cuff resulted in significantly higher hemodynamic responses during exercise (i.e., higher heart rate and blood pressure) (16). Therefore, these results highlight the importance of cuff width and personalization of the pressures to the individual when determining appropriate BFR training pressures.
Currently, there are numerous BFR training units and devices on the market. A unit designed for use in rehabilitation settings is the Delfi Personalized Tourniquet System for BFR (Delfi Medical Innovations Inc., Canada). It is categorized as a Class I medical device (low risk), utilizing a Doppler within the unit to assess LOP, thus allowing the clinician to adjust the desired occlusion pressure as a percentage of the individual’s LOP. To date, no study has investigated the differences in LOP between the Delfi unit and a commonly used unit in the BFR exercise literature (i.e., KAASTU Master, Sato Sports Plaza, Tokyo, Japan). Therefore, the purpose of this study is to compare LE LOP between these units and their corresponding cuffs. It was hypothesized that the LE LOP for the Delfi unit, which utilizes a wide cuff (11.5 cm), would be significantly lower than the KAASTU unit, which utilizes a narrow cuff (5 cm).
METHODS
Participants
Thirty participants volunteered for the present study. Subjects were excluded from the study if they had more than one cardiovascular disease risk factor per the ACSM or known cardiovascular disease. Additional exclusion criteria included reporting any known neurological disorder, LE musculoskeletal disorder affecting gait, clotting disorder, or current use of a medication that would affect blood pressure response. Prior to reporting to the laboratory for the study, the subjects were required to fast for at least four hours prior. Western Kentucky University’s Institutional Review Board approved this study and informed consent was obtained from each participant prior to participation.
Protocol
All participants reported to laboratory for one visit. After providing informed consent, the participants filled out a health history questionnaire for cardiovascular disease risk factors. After confirming they did not meet exclusion criteria, height (to nearest 0.1 cm) and weight (to nearest 0.1 kg) were measured using mechanical scale with an attached telescoping height rod (Detecto model 439 Eye). Body mass index (BMI, kg/m2) was calculated as mass divided by height squared. Resting blood pressure was taken (Welch Allyn 767 Series Mobile Aneroid) after the subjects sat quietly with feet flat; legs uncrossed, the arm free of any clothing, and relaxed for five minutes. Next, the participants were fitted for the appropriate BFR training cuff size in the standing position. Using a crossover study design, the testing order for all the participants began with fitting and measurements with the KAATSU cuff (Kaatsu Master, Sato Sports Plaza, Tokyo Japan) followed by the Delfi Personalized Tourniquet System for Blood Flow Restriction (PTS for BFR) (Delfi Medical Innovations Inc., Canada). Between the two LOP measurements; there was a 5-minute rest period.
The narrow cuff was positioned as close to the torso as possible medially and anteriorly in the most proximal portion of the left thigh (i.e., groin), but distal to the fold of the gluteal muscles. The subjects were standing during the fitting and allowed to self-position the cuff on the left thigh for modesty. The wide cuff was applied on the proximal aspect of the left thigh with the subject in standing. The subject was then asked to lie down in supine in order to determine his/her personalized tourniquet pressure. Delfi describes the unit as a personalized tourniquet system due to the LOP technology embedded within the unit, which can accurately assess LOP and allows the clinician to adjust the settings specifically for the patient (e.g., 80% of LOP) (11).
Once the cuff was in place on the left thigh, resting LE arterial blood flow velocity was measured using a mobile ultrasound with a Doppler probe placed on the popliteal artery (Esaote MyLab™25 Gold; Esaote, Florence, Italy). After resting LE arterial blood flow velocity was measured, the cuff was inflated to 50 mmHG and arterial blood flow velocity was again measured in order to observe a clear detectable pulse. Once a clear detectable pulse was observed, the inflation pressure was increased by 50 mmHG until no detectable pulse was obtained or the unit reached its maximum pressure. This occlusion inflation/maximum pressure was then recorded. KAATSU uses standard KAATSU units (SKU) to measure pressure applied to the cuff; therefore, a pressure gauge was used to establish a conversion from SKU to mmHg. It was found that 1 SKU is equal to 1 mmHg.
Statistical Analysis
Two-tailed analyses with a level of significance set at 0.05 were performed with IBM SPSS Statistics (v24; SPSS Inc., Chicago, IL). The descriptive statistics for the participants are presented as means ± SD. Paired samples t-tests were used to determine differences in LOPs between the narrow and wide cuffs. An observed power analysis was conducted with IBM SPSS Statistics which determined that the 29 participants included in this study had power of 1, with the effect size of 0.5 and an α= 0.05.
RESULTS
Twenty-nine apparently healthy sample of males (n = 22) and females (n = 7) completed the study and were analyzed. Prior to data collection, one participate was excluded from the study due to a known cardiovascular condition. The mean age was 24.0 ± 1.7 years, height 176.6 ± 8.9 cm, body mass 75.0 ± 12.6 kg and Body Mass Index (BMI) 23.9 ± 2.9 kg/m2.
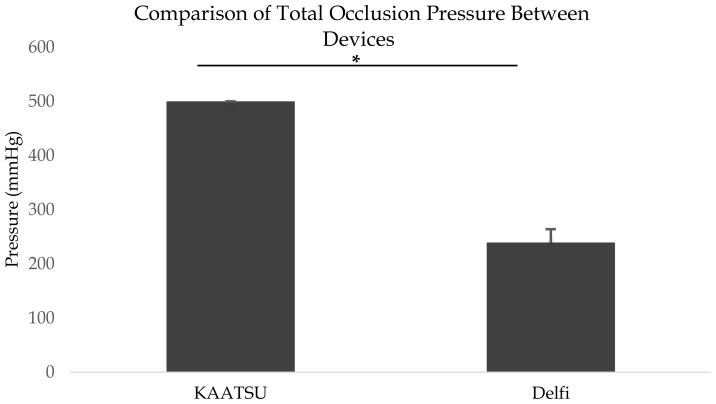
Resting arterial blood flow velocities measured at the popliteal artery were not significantly different between cuffs (KAATSU: 32.9 ± 6.7 cm/s; Delfi: 35.0 ± 8.0 cm/s; p = .134). Additionally, when comparing arterial blood flow velocity of the narrow cuff at resting versus the unit’s maximum pressure (i.e., 500 mmHg), there were no significant differences (resting: 32.9 ± 6.7 cm/s; occlusion: 31.0 ± 7.2 cm/s; p = .125). The highest pressure reached was higher for the narrow cuff compared to the wide cuff (Figure 1). However, we were unable to completely occlude lower limb arterial blood flow measured via the popliteal artery in all of the participants with the narrow cuff (i.e., reached the unit’s maximum pressure output).
Figure 1.
Standing total occlusion pressure achieved by both BFR cuffs. *Indicates differences between BFR cuff total occlusion pressure (p < 0.001)
DISCUSSION
The results of this study indicate meaningful differences between the narrow and wide cuffs for achieving LOP in the LE. We observed arterial occlusion in all subjects with the wide cuff. However, we were unable to alter arterial blood flow velocity with the narrow cuff. Each subject reached the KAASTU’s maximum pressure with the narrow cuff, which is 500 KTU (i.e., 1 KTU = 1 mmHg). Therefore, using the results of this study, the LOP for the narrow cuff, in the standing position, is assumed to be > 500 mmHg.
Our results are consistent with previous findings that wide cuffs require significantly less pressure to achieve LOP (2, 8). Loenneke and colleagues applied both wide and narrow cuffs to the LE and assessed the pressure needed to achieve arterial occlusion (8). This was assessed with their participants in supine and arterial blood flow was measured at the posterior tibialis artery. The authors found that the wide cuff (13.5 cm × 83 cm, Hokanson, SC12, Bellevue, WA) required significantly less pressure to achieve LOP compared to the narrow cuff (5 cm × 135 cm, KAASTU Master, Sato Sports Plaza, Tokyo Japan) (8). Although our results are consistent with previous findings, our study adds to the existing body of literature as follows: 1) assessment of arterial blood flow at the popliteal artery, 2) assessment of arterial blood flow with the participants in standing position, and 3) a direct comparison of the Delphi and KAATSU BFR training units.
We chose to measure arterial blood flow via the popliteal artery. The femoral artery (i.e., site of cuff application) becomes the popliteal artery after it passes through the distal portion of the adductor magnus muscle (i.e., adductor canal). The popliteal artery then branches into other significant arteries that provide blood to the lower limb, including the posterior tibial artery. Even though it may be assumed that the lack of a detectable pulse measured at the posterior tibial artery indicates full occlusion of the femoral artery, the remaining branches of the popliteal artery may still be receiving blood flow. Without direct measurement, this cannot be known for certain. While previous studies have reported complete arterial occlusion with the narrow cuff, we did not achieve complete arterial occlusion in any subject with the narrow cuff. Therefore, pulse measurement at the posterior tibialis artery may not be the most accurate representation to assess tourniquet application to the femoral artery.
We assessed LOP in the standing position based on previous work demonstrating differences in absolute LOP based on participant positioning. For example, Sieljacks and colleagues found LOPs in the sitting position required 17 to 20% more pressure, depending on cuff width, compared to supine positioning (17). In addition, Hughes et. al., found LOPs were significantly higher in standing when compared to sitting (5). Although Loenneke and colleagues were able to achieve complete LOP using the narrow cuff, these authors assessed pulse with their participants in supine (8). Thus, more pressure may have been needed to achieve complete LOP with the narrow cuff had the participants been positioned in sitting or standing. Therefore, our results are consistent with Sieljacks and colleagues recommendation that LOP be assessed in the position for which it is intended to be used (17).
There were several strengths to this current study. First, our study used ultrasound with Doppler to detect arterial occlusion velocity. Although the clinician or researcher may have auditory evidence of arterial blood velocity with a Doppler, the addition of ultrasound imaging allows for visualization of the blood vessel, thus potentially improving accuracy. Second, this study measured arterial occlusion velocity using the popliteal artery. We measured arterial velocity at the popliteal artery due to: 1) its location in regard to the BFR occlusion site (thigh/femoral artery), and 2) it being a direct link off the femoral artery. Therefore, this site was believed to help decrease the possibility of missing blood flow in the lower limb, where there are multiple branches beyond the popliteal artery. Third, we assessed LOP in the standing position. This is important because it is common for LE BFR training sessions to be performed in standing position and the standing position is known to require higher occlusion pressures (17).
Although this study possesses several strengths, it also has some limitations. First, an incremental increase in pressure by 50 mmHg, which was due to time constraints, may have decreased accuracy of LOP for the Delfi units. However, previous studies also used approximately 40–50 mmHg increments to observe total occlusion pressure with their BFR units (1). Second, our study design included a short rest period between applications of the different units. Although the rest period was not different than the previous studies, it could have influenced the arterial blood velocity. However, in this current study there was not an effect on resting arterial blood velocity because both units were about the same resting arterial velocity. Third, we were unable to achieve LOP with the KAATSU unit due to reaching its maximum pressure (i.e., 500 mmHg) with each participant. Therefore, we were unable to compare units on LOP while standing. Forth, we did not randomize the BFR cuff order, which could have caused a procedural bias. However, since there was no difference between resting arterial blood velocity, it is highly unlikely this occurred. Finally, the sample population involved healthy, 18 to 30-year-old college students, which makes generalization to other populations questionable.
Our results are consistent with previous reports that wide cuffs require less absolute pressures. In addition, our study found differences in the pressure needed to achieve complete arterial occlusion compared to previous work. This may be due to differences in the locations of pulse measurements (posterior tibial artery vs. popliteal artery) and participant position (supine vs. standing).
An increasing amount of evidence has demonstrated that the use of blood flow restriction training combined with low-level exercise can augment muscle quantity and quality. This form of training has recently moved from the laboratory setting into clinical practice and clinical trials seeing that moderate to high intensity resistance training is typically not feasible for clinical populations. Therefore, the emergence of BFR training as an alternative is promising for rehabilitation professionals and patients alike. However, emerging interventions must be evaluated prior to widespread adoption. Although achieving complete arterial occlusion is not indicated for BFR training, the ability to achieve venous occlusion at the lowest possible pressure is considered the safest tourniquet BFR training application. Relative pressures are often determined as a percentage of LOP and our study found that the relative pressure was significantly lower with the unit utilizing the wide cuff. Setting the percent limb occlusion based on individual LOP allows for consistent and reproducible BFR treatments.
ACKNOWLEDGEMENTS
All the participants who volunteered for this study.
REFERENCES
- 1.Bezerra de Morais AT, Santos Cerqueira M, Moreira Sales R, Rocha T, Galvão de Moura Filho A. Upper limbs total occlusion pressure assessment: Doppler ultrasound reproducibility and determination of predictive variables. Clin Physiol Funct Imaging. 2017;37(4):437–441. doi: 10.1111/cpf.12330. [DOI] [PubMed] [Google Scholar]
- 2.Crenshaw AG, Hargens AR, Gershuni DH, Rydevik B. Wide tourniquet cuffs more effective at lower inflation pressures. Acta Orthop Scand. 1988;59(4):447–451. doi: 10.3109/17453678809149401. [DOI] [PubMed] [Google Scholar]
- 3.Fahs CA, Loenneke JP, Rossow LM, Tiebaud RS, Bemben MG. Methodological considerations for blood flow restricted resistance exercise. J Trainology. 2012;1(1):14–22. [Google Scholar]
- 4.Gundermann DM, Fry CS, Dickinson JM, Walker DK, Timmerman KL, Drummond MJ, Volpi E, Rasmussen BB. Reactive hyperemia is not responsible for stimulating muscle protein synthesis following blood flow restriction exercise. J Appl Physiol. 2012;112(9):1520–1528. doi: 10.1152/japplphysiol.01267.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hughes L, Jeffries O, Waldron M, Rosenblatt B, Gissane C, Paton B, Patterson SD. Influence and reliability of lower-limb arterial occlusion pressure at different body positions. PeerJ. 2018;6:e4697. doi: 10.7717/peerj.4697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hunt JE, Stodart C, Ferguson RA. The influence of participant characteristics on the relationship between cuff pressure and level of blood flow restriction. Eur J Appl Physiol. 2016;116(7):1421–1432. doi: 10.1007/s00421-016-3399-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jessee MB, Buckner SL, Dankel SJ, Counts BR, Abe T, Loenneke JP. The influence of cuff width, sex, and race on arterial occlusion: Implications for blood flow restriction research. Sports Med. 2016;46(6):913–921. doi: 10.1007/s40279-016-0473-5. [DOI] [PubMed] [Google Scholar]
- 8.Loenneke JP, Fahs CA, Rossow LM, Sherk VD, Thiebaud RS, Abe T, Bemben DA, Bemben MG. Effects of cuff width on arterial occlusion: Implications for blood flow restricted exercise. Eur J Appl Physiol. 2012;112(8):2903–2912. doi: 10.1007/s00421-011-2266-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Loenneke JP, Fahs CA, Rossow LM, Thiebaud RS, Mattocks KT, Abe T, Bemben MG. Blood flow restriction pressure recommendations: A tale of two cuffs. Front Physiol. 2013;4:249. doi: 10.3389/fphys.2013.00249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loenneke JP, Wilson JM, Marín PJ, Zourdos MC, Bemben MG. Low intensity blood flow restriction training: A meta-analysis. Eur J Appl Physiol. 2012;112(5):1849–1859. doi: 10.1007/s00421-011-2167-x. [DOI] [PubMed] [Google Scholar]
- 11.Masri BA, Day B, Younger AS, Jeyasurya J. Technique for measuring limb occlusion pressure that facilitates personalized tourniquet systems: A randomized trial. J Med Biol Eng. 2016;36(5):644–650. doi: 10.1007/s40846-016-0173-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McEwen JA, Owens JG, Jeyasurya J. Why is it crucial to use personalized occlusion pressures in blood flow restriction (BFR) rehabilitation? J Med Biol Eng. 2018:1–5. [Google Scholar]
- 13.Medicine ACoS. ACSM’s guidelines for exercise testing and prescription. Lippincott Williams & Wilkins; 2017. [Google Scholar]
- 14.Noordin S, McEwen JA, Kragh CJF, Jr, Eisen A, Masri BA. Surgical tourniquets in orthopaedics. JBJS. 2009;91(12):2958–2967. doi: 10.2106/JBJS.I.00634. [DOI] [PubMed] [Google Scholar]
- 15.Renzi CP, Tanaka H, Sugawara J. Effects of leg blood flow restriction during walking on cardiovascular function. Med Sci Sports Exerc. 2010;42(4):726. doi: 10.1249/MSS.0b013e3181bdb454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rossow LM, Fahs CA, Loenneke JP, Thiebaud RS, Sherk VD, Abe T, Bemben MG. Cardiovascular and perceptual responses to blood-flow-restricted resistance exercise with differing restrictive cuffs. Clin Physiol Funct Imaging. 2012;32(5):331–337. doi: 10.1111/j.1475-097X.2012.01131.x. [DOI] [PubMed] [Google Scholar]
- 17.Sieljacks P, Knudsen L, Wernbom M, Vissing K. Body position influences arterial occlusion pressure: Implications for the standardization of pressure during blood flow restricted exercise. Eur J Appl Physiol. 2018;118(2):303–312. doi: 10.1007/s00421-017-3770-2. [DOI] [PubMed] [Google Scholar]