Abstract
Exposure to Adverse Childhood Experiences (ACEs) is associated with a host of harmful outcomes, including increased risk for cancer. A scoping review was conducted to gain a better understanding of how ACEs have been studied in association with risk factors for cancer. This review includes 155 quantitative, peer-reviewed articles published between 2005 and 2015 that examined associations between ACEs and modifiable cancer risk factors, including alcohol, environmental carcinogens, chronic inflammation, sex hormones, immunosuppression, infectious agents, obesity, radiation, ultraviolet (UV) radiation, and tobacco, among U.S. adults. This review highlights the growing body of research connecting ACEs to cancer risk factors, particularly alcohol, obesity, and tobacco. Fewer studies investigated the links between ACEs and chronic inflammation or infectious agents. No included publications investigated associations between ACEs and environmental carcinogens, hormones, immunosuppression, radiation, or ultraviolet radiation. Mitigating the impact of ACEs may provide innovative ways to effect comprehensive, upstream cancer prevention.
Keywords: Adverse Childhood Experiences, Cancer risk, Scoping review, Cancer prevention, Child abuse and neglect prevention
Introduction
Research on Adverse Childhood Experiences (ACEs) has found that exposure to early adversity, especially in the absence of protective factors (e.g., supportive family environments and social networks), can result in a host of harmful outcomes immediately and throughout the life course (Brown et al., 2009; Centers for Disease Control and Prevention, 2014; Dube et al., 2001; Felitti et al., 1998; Fortson, Klevens, Merrick, Gilbert, & Alexander, 2016; Garner et al., 2012; Gilbert et al., 2015; Metzler, Merrick, Klevens, Ports, & Ford, 2017; Shonkoff, 2016; Shonkoff et al., 2012). While definitions vary, ACEs generally include child maltreatment (i.e., child abuse and neglect) and household challenges (i.e., witnessing intimate partner violence, parental separation or divorce, mental illness in the household, substance abuse in the household, or parental incarceration) that happen during the first 18 years of life (Felitti et al., 1998). Research demonstrates that ACEs are prevalent (Felitti et al., 1998; Gilbert et al., 2015), and exposure to ACEs has been linked to underdeveloped executive functioning and altered physiological stress responses (Shonkoff, 2016), mental health problems (Dube et al., 2001; Felitti et al., 1998), chronic health conditions (Felitti et al., 1998; Gilbert et al., 2015), health risk behaviors (Felitti et al., 1998), decreased life opportunities (e.g., education and income) (Metzler et al., 2017), and decreased life expectancy (Brown et al., 2009). These linkages highlight the critical association between childhood experiences and ill health and subsequently the importance of preventing ACEs. To ensure that all children reach their maximal health and life potential, professional technical reports (Fortson et al., 2016; Shonkoff et al., 2012) and policy statements (Garner et al., 2012)have emphasized the importance of implementing strategies that prevent exposure to toxic stress in childhood, as well as mitigating the negative effects of ACEs on development and health across the lifespan. Similarly, the Centers for Disease Control and Prevention (CDC) developed a framework for prevention, Essentials for Childhood, to ensure that all children have access to safe, stable, nurturing relationships and environments for optimal health and wellbeing (Centers for Disease Control and Prevention, 2014).
In this paper, the association between ACEs and risk factors or determinant for cancer was of primary concern. Cancer is a leading cause of death worldwide; in 2013, the latest year for which data are available, there were over 1.5 million new cases and nearly 600,000 cancer deaths in the United States (US) (U.S. Cancer Statistics Working Group, 2016). Exposure to ACEs has been linked to cancer in adulthood (Holman et al., 2016). Specifically, a cumulative ACE score is associated with increased risk of reporting exposure to any type of cancer (Bellis et al., 2015; Brown, Thacker, & Cohen, 2013; Felitti et al., 1998; Kelly-Irving et al., 2013; Morton, Schafer, & Ferraro, 2012), as well as increased risk for lung cancer (Brown et al., 2010). Individual ACE exposure, such as physical and psychological abuse have been associated with risk of any type of cancer (Fuller-Thomson & Brennenstuhl, 2009; Hyland, Alkhalaf, & Whalley, 2013; Morton et al., 2012); sexual abuse has been associated with cervical cancer (Coker, Hopenhayn, DeSimone, Bush, & Crofford, 2009). However, less is known about the mechanisms behind these associations, and whether associations between ACEs and risk factors for cancer explain some of the associations between ACEs and cancer incidence found in previous reviews (Holman et al., 2016). While risk factors for cancer are well known, there has been no attempt to summarize the literature connecting childhood experiences to risk factors for cancer. Causal factors for cancer are complex and likely include multiple factors, including harmful exposures, certain behaviors, and less controllable factors like age and genetics (National Cancer Institute, 2015); some of which may be influenced by ACEs. Summarizing the literature that explores associations between childhood experiences and cancer risk factors may lead to more upstream approaches to cancer prevention that include strategies for pediatric nurses, researchers and other health practitioners that address and prevent exposure to ACEs.
The purpose of this paper was to conduct a scoping study to assess the status of published evidence connecting exposure to ACEs and the presence of cancer risk factors among adults. Scoping reviews allow researchers to synthesize existing literature in terms of volume, nature, and characteristics, particularly when the topic has not been extensively reviewed or is complex or heterogeneous in nature (Arksey & O'Malley, 2005; Mays, Roberts, & Popay, 2001). Given the multi-factorial nature of cancer development over the lifespan and the myriad studies investigating ACEs and adult health, a scoping review has the potential to synthesize a broad body of research connecting childhood experiences and cancer risk, highlight gaps in the research, and offer insight on novel cancer prevention and intervention strategies.
Methodology
This review was conducted in accordance with Arksey and colleagues' methodological framework for scoping reviews (Arksey & O'Malley, 2005), which has been highlighted by the EQUATOR (Enhancing the Quality and Transparency of health research). It included the following phases: (1) identifying the research question(s), (2) identifying relevant studies, (3) study selection, (4) charting the data, and (5) collating/summarizing and reporting the results. The process began with the establishment of a research team consisting of experts in both cancer and childhood adversity prevention and control. The team provided critical insight to all aspects of the review. The review was guided by the questions, “What ACEs are utilized in the peer-reviewed literature pertaining to cancer risk factors?” and “What are the associations between ACEs and cancer risk factors in adulthood?” Below we outline search strategies used to identify studies, the study selection process, including inclusion criteria for selection of studies, and data extraction process for charting and summarizing the results.
Search Strategies Used to Identify Studies
For the purposes of this review, ACEs were defined as exposure to one or more of the following adverse events before the age of 18 years:
abuse victimization (physical, sexual, and/or psychological)
neglect (emotional and/or physical)
household challenges (parental death or serious illness, parental separation or divorce, parental incarceration, substance abuse in the household, domestic violence, mental illness in the household, and/or family poverty), and
other types of early adversity or trauma as defined in identified articles.
Search terms were selected to capture the traditional ACEs (i.e., abuse, neglect and household challenges) (Table 1); however, within the literature, ACEs has been broadly defined, and researchers have used ACEs to refer to myriad experiences (Fig. 1).
Table 1.
Summary of search terms used in the PubMed online database to identify articles reporting on the association between Adverse Childhood Experiences (ACEs) and cancer risk factors in adulthood.
| Terms related to adverse childhood experiences | ((“ACE”) OR (“ACEs”) OR (“adverse childhood experiences”) OR (“adverse childhood events”) OR (“childhood maltreatment”) OR (“child maltreatment”) OR (“childhood adversity”) OR (“child adversity”) OR (“childhood adversities”) OR (“child adversities”) OR (“early adversity”) OR (“early adversities”) OR (“physical abuse”) OR (“sexual abuse”) OR (“childhood neglect”) OR (“child neglect”) OR (“physical neglect”) OR (“child abuse”) OR (“childhood abuse”) OR (“emotional abuse”) OR (“child emotional neglect”) OR (“childhood emotional neglect”) OR (“child trauma”) OR (“childhood trauma”) OR (“emotional neglect”) OR (“parental incapacities”) OR (“family incapacities”) OR (“adverse family experiences”) OR (“adverse family events”)) |
| AND | |
| Terms related to cancer riskfactor – Alcohol | ((“alcohol consumption”) OR (“alcohol drinking”) OR (“consumption of alcoholic beverages”) OR (“consumption of alcohol”) OR (“alcohol dependence”) OR (“alcohol abuse”) OR (“excessive drinking”) OR (“binge drinking”) OR (“heavy drinking”) OR (“heavy alcohol drinking”) OR (“underage drinking”) OR (“drinking underage”)) |
| OR | |
| Terms related to cancer risk factor – Environmental Cancer Causing Substance | ((“environmental carcinogens”) OR (“aflatoxins”) OR (“aspergillus flavus”) OR (“aspergillus parasiticus”) OR (“aristolochic acids”) OR (“arsenic”) OR (“asbestos”) OR (“benzene”) OR (“benzidine”) OR (“beryllium”) OR (“1, 3-butadiene”) OR (“cadmium”) OR (“coal tar”) OR (“coal-tar pitch”) OR (“creosote”) OR (“coke-oven emissions”) OR (“crystalline silica”) OR (“erionite”) OR (“ethylene oxide”) OR (“formaldehyde”) OR (“hexavalent chromium compounds”) OR (“indoor emissions from the household combustion of coal”) OR (“indoor emissions”) OR (“household combustion of coal”) OR (“coal combustion”) OR (“mineral oils”) OR (“nickel compounds”) OR (“radon”) OR (“secondhand tobacco smoke”) OR (“secondhand smoke”) OR (“secondhand smoking”) OR (“environmental tobacco smoke”) OR (“soot”) OR (“inorganic acid mists containing sulfuric acid”) OR (“sulfuric acid”) OR (“acid mist”) OR (thorium) OR (“vinyl chloride”) OR (“wood dust”)) |
| OR | |
| Terms related to cancer risk factor – Chronic Inflammation | ((“inflammation”) OR (“CRP”) OR (“C-reactive protein”) OR (“inflammatory response”) OR (“inflammatory markers”) OR (“adiponectin”) OR (“resistin”) OR (“interleukin-6”) OR (“adipokines”) OR (“adipocyte-derived inflammation”) OR (“chronic inflammatory disease”)) |
| OR | |
| Terms related to cancer risk factor – Sex Hormones | ((“estrogen”) OR (“hormone therapy”) OR (“hormone replacement therapy”) OR (“estrogen plus progestin”) OR (“endogenous estrogen and progesterone”) OR (diethylstilbestrol) OR (“DES”) OR (“oral contraception”) OR (“oral contraceptive”) OR (“birth control”)) |
| OR | |
| Terms related to cancer risk factor – Immunosuppression | ((“immunosuppression”) OR (“immunosuppressive drugs”) OR (“immunocompromised”) OR (“compromised immune system”) OR (“transplant recipients”)) |
| OR | |
| Terms related to cancer risk factor – Infectious Agents | ((“human papillomavirus”) OR (“HPV”) OR (“human papilloma virus”) OR (“HPV infection”) OR (“human papilloma virus infection”) OR (“hepatitis B virus”) OR (“hepatitis C virus”) OR (“hepatitis B”) OR (“hepatitis C”) OR (“HBV”) OR (“HCV”) OR (“hepatitis”) OR (“hep C”) OR (“hep B”) OR (“T-cell leukemia”) OR (“T-cell lymphoma”) OR (“lymphoma virus type 1”) OR (“HTLV-1”) OR (“T-cell leukemia/lymphoma”) OR (“HIV”) OR (“human immunodeficiency virus”) OR (“HIV/AIDS”) OR (“AIDS”) OR (“acquired immune deficiency”) OR (“epstein-barr virus”) OR (EBV) OR (“human herpesvirus 8”) OR (“HHV8”) OR (“kaposi sarcoma-associated herpes virus”) OR (“KSHV”) OR (“merkel cell polyomavirus”) OR (“MCPyV”) OR (“helicobacter pylori”) OR (“H. pylori”) OR (“schistosoma haematobium”) OR (“opisthorchis viverrini”)) |
| OR | |
| Terms related to cancer risk factor – Obesity, Physical Activity, Sedentary Behavior | ((“obesity”) OR(“obese”) OR (“overweight”) OR (“over-weight”) OR (“metabolic syndrome”) OR (“BMI”) OR (“body mass index”) OR (“body fat percentage”) OR (“BFP”) OR (“waist-hip ratio”) OR (“waist-to-hip ratio”) OR (“WHR”) OR (“physical activity”) OR (“exercise”) OR (“sedentary behavior”) OR (“sedentary”) OR (“sedentary lifestyle”) OR (“sedentary time”) OR (“screen time”)) |
| OR | |
| Terms related to cancer risk factor – Radiation | ((“radiation”) OR (“ionizing radiation”) OR (“radon”) OR (“radium”) OR (“x-rays”) OR (“gamma rays”) OR (“high-energy radiation”) OR (“alpha particles”) OR (“beta particles”) OR (“neutrons”) OR (“accidents at nuclear power plants”) OR (“atomic weapons”) OR (“fallout”) OR (“iodine-131”) OR (“I-131”) OR (“NRI”) OR (“computed tomography scans”) OR (“CT scans”) OR (“positron emission tomography scans”) OR (“PET scans”) OR (“medical radiation”) OR (“radiation from medical imaging”)) |
| OR | |
| Terms related to cancer risk factor – Ultraviolet Radiation | ((“sunlamps”) OR (“tanning booths”) OR (“tanning”) OR (“ultraviolet radiation”) OR (“UV”) OR (“UVR”) OR (“sun exposure”) OR (“sun damage”) OR (“sunburn”)) |
| OR | |
| Terms related to cancer risk factor – Tobacco | ((“tobacco”) OR (“cigars”) OR (“smoking”) OR (“smoke”) OR (“cigarettes”) OR (“cigarette”) OR (“cigar”) OR (“cigars”) OR (“snuff”) OR (“dip”) OR (“snus”)) |
| AND | |
| Language selection | “English”[Language] |
| AND | |
| Date-Publication | 2005/01/01–2015/12/31 |
| NOT | |
| Excluded search terms | ((“angiotensin-converting enzyme inhibitors”) OR (“ACE inhibitors”) OR (“angiotensin”) OR (“acute care of the elderly”) OR (“ACE-27”) OR (“ACE 27”) OR (“adjuvant chemotherapy and endocrine therapy”) OR (“HPV4A ACE”) OR (“ACE serum”) OR (“acute care for the elderly”) OR (“agitation-calmness evaluation scale”) OR (“ACE polymorphism”) OR (“T-ACE”) OR (“angiotensin-converting enzyme”) OR (“central nucleus of the amygdala”) OR (“ACE inhibitor”) OR (“adverse clinical event”) OR (“ACE inhibitor-drug”) OR (“Auto-capillary Electrophoresis”) OR (“alternative cellular energy”) OR (“comment”[Publication Type]) OR (“meta-analysis”[Publication Type]) OR (“review”[Publication Type])) |
Fig. 1.
Types of adverse childhood experiences included in studies. Note: The size of the word reflects its frequency of measurement in studies. The adversity type may have been measured as an individual item, included as part of a summary or score, or both. The shade of the word has no meaning.
We used the National Cancer Institute's (NCI) list of known cancer risk factors to determine the cancer risk factors that would be included in this review (National Cancer Institute, 2015). Of the factors listed, alcohol, cancer-causing substances in the environment, chronic inflammation, sex hormones, immunosuppression, infectious agents, obesity, radiation, tobacco, and ultraviolet radiation were included. Physical activity was included as a subset of the obesity search terms; however, given that the association between ACEs and obesity and cancer are likely more complex than a simple calorie in versus calorie out relationship, associations between ACEs and physical activity are reported separately. Age was excluded, because age itself is not modifiable.
A string of “NOT” terms was added to exclude irrelevant topics that could inadvertently be captured by the search term “ACE” (e.g., autocapillary electrophoresis). All authors reviewed the final search string for completeness (Table 1). PubMed searches were conducted separately for each cancer risk factor. As such, some articles were considered across multiple risk factors.
Study Selection Process
Studies included in the review were required to be published in peer-reviewed journals and report the statistical association between experiences considered to meet the definition of ACEs and adult cancer incidence. Only studies with samples from the US and published from 2005 to 2015 were included in this review. Studies published online and ahead of print in 2015 were included. Inclusion criteria also included measurement of ACEs before age 18 years, and measurement of cancer risk factors in adulthood (i.e., 18 years or older). Case reports and studies that were not original research, did not involve human subjects, were not written in English were excluded. Grey literature was not included in this review as both ACEs and risk for cancer are well-established fields with myriad peer-reviewed journals.
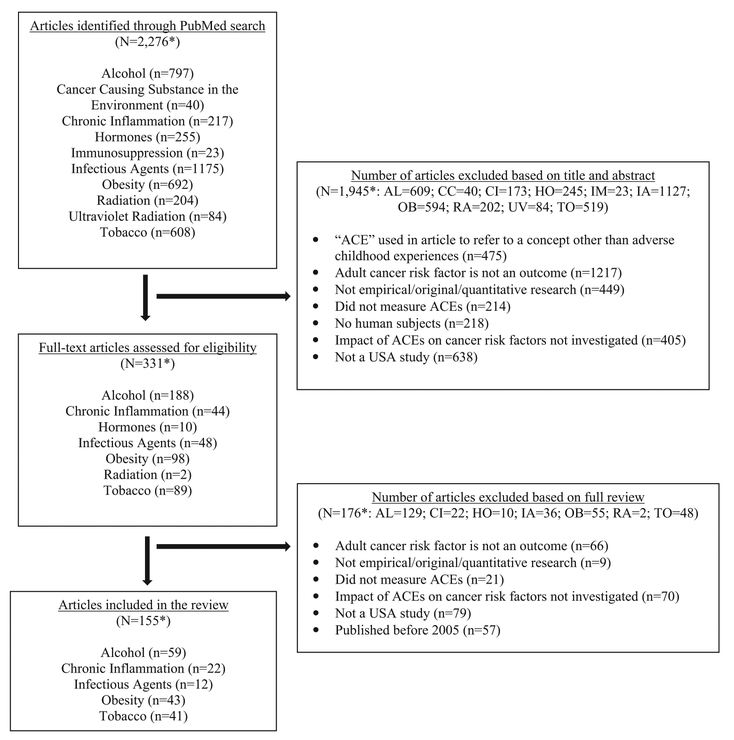
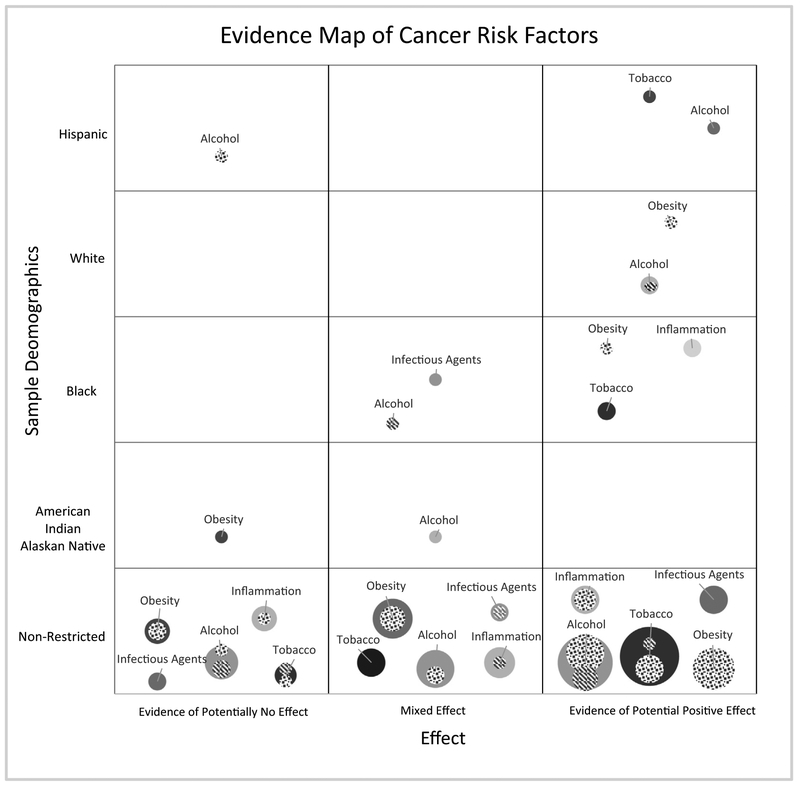
The initial PubMed search returned 2276 unique articles across the cancer risk factors. Of these, 1945 did not meet study criteria based on a title and abstract review. The full text of the remaining 331 articles was then reviewed for relevancy; 155 articles were determined eligible for inclusion with 14 articles included across one or more cancer risk factor (N = 22). Fig. 2 provides a flowchart of the study selection process with reasons for study exclusion. See Fig. 3 for a high-level overview of study findings by risk factor and demographics.
Fig. 2.
Flowchart of study selection. Note. Alcohol = AL; Cancer causing substances in the environment = CC; Chronic inflammation = CI; Hormones = HO; Immunosuppression = IM; Infectious agents (IA); Obesity = OB; Radiation = RA; Ultraviolet radiation = UV; Tobacco = TO; *N = total number of unique articles; some articles addressed multiple topics or were excluded for multiple reasons.
Fig. 3.
Bubble plot of reported associations between ACEs and cancer risk factors by effect and demographics. Key: Size of bubble = the number of articles looking at the association between ACEs and the identified cancer risk factor;  = male-only participants
= male-only participants  = female-only participants. Note: Study samples were non-Hispanic unless noted.
= female-only participants. Note: Study samples were non-Hispanic unless noted.
Data Extraction for Charting and Summarizing
Reviewers independently abstracted the following data from articles that were included for full review: PubMed ID, title, first author, year of publication, sample size, study population, study design, year(s) of data collection, measure(s) of early adversity, measure(s) of cancer risk factor, statistical analyses used, and reported associations between ACEs and cancer outcomes based on adjusted analyses (i.e., risk, odds, and hazard ratios). Approximately 25% of the abstracted data were checked by a second reviewer to assess reliability. The few discrepancies were resolved through meetings and dialogue when necessary. Reviewers outlined the key information from each study in a table format (Appendix 1) and developed a descriptive summary of the observed patterns (outlined below).
Search Results
In total, 33 different ACEs were measured across the studies. A word cloud (Fig. 1) was constructed to visualize the types of adversities included in the studies. The size of the word reflects the frequency of that measure across studies: physical abuse, emotional abuse, and sexual abuse were the most common ACEs measured. Five studies used data from the original CDC-Kaiser Permanente ACE study (Brown et al., 2010; Dong et al., 2005; Dube et al., 2009; Edwards, Anda, Gu, Dube, & Felitti, 2007; Strine et al., 2012), and 18 used ACE data from the Behavioral Risk Factor Surveillance System (BRFSS), which includes an optional ACE module adapted from the original ACE questionnaire (Campbell, Walker, & Egede, 2016; Chapman et al., 2013; Dube, Cook, & Edwards, 2010; Font & Maguire-Jack, 2016; Ford et al., 2011; Fuller-Thomson, Filippelli, & Lue-Crisostomo, 2013; Gjelsvik, Dumont, & Nunn, 2013; McCauley, Blosnich, & Dichter, 2015; Vander Weg, 2011; Walsh & Cawthon, 2014; Yeoman, Safranek, Buss, Cadwell, & Mannino, 2013). All other studies either used an adapted ACE questionnaire or selected unique, but often overlapping, childhood adversities. The adversity type may have been measured as an individual item, included as part of a summary score, or both. Summary scores, regardless of the ACEs included, will heretofore be referred to as adversity scores. Study findings are summarized below by cancer risk factor.
Alcohol
Alcohol use can increase risk for cancers of the pharynx, larynx, oral cavity, esophagus, liver, colorectal, and female breast cancers (IARC Working Group on the Evaluation of Carcinogenic Risk to Humans, 2012c). ACEs have long been associated with alcohol dependence (Dube et al., 2006; Dube, Anda, Felitti, Edwards, & Croft, 2002; Felitti et al., 1998). In total, 59 articles met inclusion criteria. Alcohol use was characterized using multiple measures, most frequently alcohol dependence (N = 19), binge drinking (N = 11), alcohol abuse (N = 8), general alcohol use (N = 8), frequency of alcohol consumption (N = 8), alcohol-related consequences/problems (N = 8), quantity of alcohol consumed (N = 7), and other drinking behaviors (N = 12). The term “problematic alcohol-related behaviors” will be used in subsequent text to encompass these various measures. Twenty-nine different measures of childhood adversity were used, with the majority of studies including a measure of childhood sexual abuse (CSA; N = 49), physical abuse (PA; N = 42), and emotional abuse (N = 30). One study used data from the original ACE study (Strine et al., 2012), and three studies used data from the BRFSS ACE module (Campbell et al., 2016; Font & Maguire-Jack, 2016; Gjelsvik et al., 2013). Associations between early adversity and problematic alcohol-related behaviors varied by study.
In general, summed adversity scores were positively associated with problematic alcohol-related behaviors (Campbell et al., 2016; Carlson, Harden, Kretsch, Corbin, & Fromme, 2015; Fetzner, McMillan, Sareen, & Asmundson, 2011; Font & Maguire-Jack, 2016; Keyes et al., 2012; Kim et al., 2014; Park, Sher, Todorov, & Heath, 2011; Pilowsky, Keyes, & Hasin, 2009; Shin, Hassamal, & Groves, 2015; Young-Wolff, Kendler, Ericson, & Prescott, 2011). These associations existed among Hispanic (Allem, Soto, Baezconde-Garbanati, & Unger, 2015), and African American and European American (Sartor, Wang, Xu, Kranzler, & Gelernter, 2014) samples, as well as samples of adults with substance abuse histories (Banducci, Hoffman, Lejuez, & Koenen, 2014; Wu, Schairer, Dellor, & Grella, 2010) and alcohol dependence (Elliott et al., 2014; Elliott et al., 2016). In addition, experiencing childhood trauma was associated with earlier onset of alcohol use, earlier age of heaviest drinking, and a shorter delay from onset of alcohol use to heavy alcohol use (Waldrop, Ana, Saladin, McRae, & Brady, 2007). Similarly, among those who reported exposure to child maltreatment (CM), increased risk of transitioning from less severe to more hazardous alcohol use was more likely (La Flair et al., 2013).
Individual ACE types were positively associated with problematic alcohol-related behaviors in adulthood. In general, exposure to childhood physical abuse (CPA) (Anderson, Rabi, Lukas, & Teicher, 2010; Fenton et al., 2013; Fetzner et al., 2011; Font & Maguire-Jack, 2016; Shin, Lee, Jeon, & Wills, 2015), CSA (Corstorphine, Waller, Lawson, & Ganis, 2007; Fenton et al., 2013; Fetzner et al., 2011; Keyes et al., 2012; McMillan, Hanson, Bedrick, & Lapham, 2005; Shin, Lee, et al., 2015), emotional abuse (Campbell et al., 2016; Fenton et al., 2013; Fetzner et al., 2011; Font & Maguire-Jack, 2016), mental illness in the household (Font & Maguire-Jack, 2016), neglect (Fenton et al., 2013; Fetzner et al., 2011), household member incarceration (Gjelsvik et al., 2013), substance abuse in the household (Font & Maguire-Jack, 2016), and parental divorce (Pilowsky et al., 2009) were each associated with one or more problematic alcohol-related behaviors. Exposure to CPA (Schwandt, Heilig, Hommer, George, & Ramchandani, 2013), emotional abuse (Schwandt et al., 2013), emotional neglect (Schwandt et al., 2013), physical neglect (Schwandt et al., 2013), and CSA (Elliott et al., 2014; Schwandt et al., 2013) was associated with problematic alcohol-related behaviors in alcohol-dependent samples. Similarly, among individuals with PTSD, those who were alcohol dependent were more likely to have experienced all abuse categories, as well as neglect, parental divorce, and having absent parents or parents with behavioral and substance abuse problems (Blanco et al., 2013). Among persons seeking treatment for alcoholism, CPA, emotional abuse, and physical neglect exposure were associated with alcohol dependence severity, but CSA and emotional neglect were not (Schwandt et al., 2013).
Among male-only and female-only samples, neglect (Goldstein, Flett, & Wekerle, 2010; Snyder & Merritt, 2016; Strine et al., 2012), CSA (Drabble, Trocki, Hughes, Korcha, & Lown, 2013; Grayson & Nolen-Hoeksema, 2005; Lown, Nayak, Korcha, & Greenfield, 2011; McCarty, DePadilla, Elifson, & Sterk, 2012; Najdowski & Ullman, 2009; Sartor et al., 2012; Skinner, Kristman-Valente, & Herrenkohl, 2016; Strine et al., 2012; Trent, Stander, Thomsen, & Merrill, 2007; Walsh, Latzman, & Latzman, 2014; Young, Hansen, Gibson, & Ryan, 2006), CPA (Drabble et al., 2013; Jenkins et al., 2011; Lown et al., 2011; McCarty et al., 2012; Strine et al., 2012; Trent et al., 2007; Walsh et al., 2014; Young et al., 2006), emotional abuse (Strine et al., 2012; Young et al., 2006), substance abuse in the household (Strine et al., 2012), mental illness in the household (Strine et al., 2012; Young et al., 2006), and adversity scores (Eames et al., 2014; Hughes, McCabe, Wilsnack, West, & Boyd, 2010; Jenkins et al., 2011; Sartor et al., 2014; Strine et al., 2012) were associated with problematic alcohol-related behaviors.
Among men, incarcerated household member (Strine et al., 2012), parental rejection (Schellekens et al., 2013), household member with problem drinking (Young et al., 2006), and negative life events scores (Schellekens et al., 2013) were also associated with problematic alcohol-related behaviors. In one study, out-of-home placement (e.g., foster care) was associated with adult alcohol dependence among urban, gay/bisexual male American Indians and Alaskan Natives (AI/AN) (Yuan, Duran, Walters, Pearson, & Evans-Campbell, 2014). However, in the same study being adopted decreased the risk of later binge drinking in a sample of urban, lesbian/bisexual female AI/AN (Yuan et al., 2014). Women who experienced CM developed alcohol dependence earlier than women who did not (Oberleitner, Smith, Weinberger, Mazure, & McKee, 2015), and among lesbian women, neglect (Hughes, McCabe, et al., 2010), CSA (Gilmore et al., 2014; Hughes, Johnson, Wilsnack, & Szalacha, 2007), and CPA (Hughes et al., 2007) were associated with alcohol-related problems. In another study, the highest levels of hazardou s drinking were reported by bisexual women with CSA histories compared to heterosexual and lesbian women with CSA histories (Hughes, Szalacha, et al., 2010).
The majority of studies found significant positive associations between ACEs and problematic adult drinking behavior (N = 35), but several studies reported mixed effects (N = 13), and eleven studies did not find significant associations (Agorastos et al., 2014; Carlson, Oshri, & Kwon, 2015; Horan & Widom, 2015; Hostinar, Lachman, Mroczek, Seeman, & Miller, 2015; Klanecky, McChargue, & Bruggeman, 2012; Klanecky, Woolman, & Becker, 2015; Nikulina, Widom, & Brzustowicz, 2012; Salem et al., 2013; Tyler, Schmitz, & Adams, 2015; Ulibarri, Ulloa, & Salazar, 2015; Ullman & Sigurvinsdottir, 2015). For example, summary adversity scores were not associated with problematic alcohol-related behaviors in multiple study populations, including the MIDUS II Study (Hostinar et al., 2015), male Marines (Agorastos et al., 2014), some samples of college students (Carlson, Oshri, et al., 2015; Goldstein et al., 2010; Klanecky et al., 2012; Klanecky et al., 2015), urban lesbian, gay or bisexual (LGB) AI/AN (Yuan et al., 2014), and recently paroled men (Salem et al., 2013). Individuals with histories of substantiated CM compared to non-abused controls were not more likely to abuse alcohol (Horan & Widom, 2015; Nikulina et al., 2012). In several studies, CSA was not associated with alcohol-related behaviors among samples of college students (Klanecky et al., 2012; Tyler et al., 2015), men (Skinner et al., 2016), women with sexual assault histories (Ullman & Sigurvinsdottir, 2015), low-income Latina women (Ulibarri et al., 2015), and women identified as early-onset alcohol users (Jenkins et al., 2011).
Cancer-Causing Substances in the Environment
Environmental carcinogenic substances are associated with cancer incidence including arsenic, asbestos, secondhand tobacco smoke, and soot (IARC Working Group on the Evaluation of Carcinogenic Risk to Humans, 2012a, 2012b, 2012d, 2012e). Environmental hazards are often contributors to observed health inequities, especially in low-income populations (Adamkiewicz et al., 2014; Evans & Kantrowitz, 2002; Rosenbaum, Hartley, & Holder, 2011). Given that socioeconomic status is associated with risk of ACE exposure (Sedlak et al., 2010), it is possible that individuals at risk of ACEs are also at greater risk of environmental carcinogens. However, none of the identified articles (N = 40) met inclusion criteria.
Chronic Inflammation
Inflammation, a known cancer risk factor, may be one mechanism connecting early trauma to adult health outcomes. Inflammation is a physiological response that promotes a healthy defense against toxins, infections and injuries; however, prolonged or chronic inflammation can cause damage to the body and over time can lead to cancer (Coussens & Werb, 2002). It is hypothesized that those exposed to childhood adversity have increased inflammation levels because stress activates the sympathetic nervous system, triggering inflammation (Danese & McEwen, 2012). In the current review, 22 articles met the inclusion criteria. The studies measured various markers of inflammation, including C-reactive protein (CRP; N = 18), interleukin-6 (IL-6; N = 13), tumor necrosis factor-alpha (TNF-α; N = 6), interleukin-1 beta (IL-1β; N = 3), and other markers (N = 8). Twenty-three different types of ACEs were measured across the 22 studies.
An ACE score of two or more was associated with a host of inflammation-related autoimmune diseases, including rheumatoid arthritis (Dube et al., 2009). In addition, several indicators of early adversity were associated with inflammation summary scores (Friedman, Karlamangla, Gruenewald, Koretz, & Seeman, 2015; Hostinar et al., 2015), but associations varied widely based on the selected measure of early adversity and the inflammation marker of interest. For example, summary childhood adversity scores significantly predicted increased levels of IL-6 in adulthood (Carpenter et al., 2010; Cho, Bower, Kiefe, Seeman, & Irwin, 2012; Gouin, Glaser, Malarkey, Beversdorf, & Kiecolt-Glaser, 2012; Hartwell et al., 2013; Kiecolt-Glaser et al., 2011; Rooks, Veledar, Goldberg, Bremner, & Vaccarino, 2012; Slopen et al., 2010; Tietjen, Khubchandani, Herial, & Shah, 2012). Among breast cancer survivors, childhood abuse, chaotic home environment, and total adversity scores were associated with elevated IL-6 levels (Crosswell, Bower, & Ganz, 2014). ACE score (Tietjen et al., 2012), emotional abuse (Rooks et al., 2012), court-substantiated neglect (Nikulina & Widom, 2014), prenatal adversity (Slopen et al., 2015), and childhood abuse and/or neglect experienced by women (Matthews, Chang, Thurston, & Bromberger, 2014) were also associated with elevated IL-6 levels. However, family poverty (Appleton et al., 2012; Nikulina & Widom, 2014), parental education or occupation (Appleton et al., 2012), neighborhood poverty (Nikulina & Widom, 2014), child abuse or neglect (Bertone-Johnson, Whitcomb, Missmer, Karlson, & Rich-Edwards, 2012; Gouin et al., 2012; Schrepf, Markon, & Lutgendorf, 2014), and total adversity scores (Cho et al., 2012; Crosswell et al., 2014; Hartwell et al., 2013; Joung et al., 2014; Schrepf et al., 2014; Slopen et al., 2015; Slopen, Non, Williams, Roberts, & Albert, 2014) were not associated with CRP levels. One study found that compared to children who did not experience bullying, being a victim of bullying predicted higher increases in CRP levels over time (Copeland et al., 2014). Associations between early adversity and TNF-α level also varied. For example, childhood abuse (Gouin et al., 2012; Kiecolt-Glaser et al., 2011) and other types of early adversity (Kiecolt-Glaser et al., 2011) were not associated with TNF-α level. Among breast cancer survivors, adversity was not associated with TNF-α level, but a chaotic home environment was (Crosswell et al., 2014). In contrast, total adversity scores were associated with TNF-α levels (Hartwell et al., 2013; Tietjen et al., 2012), and significant associations between abuse scores and TNF-α levels in an African American sample were found (Smith et al., 2011).
Sex Hormones
Despite playing a key role in the physiological processes of both women and men, estrogens, a group of structurally related, hormonally active molecules that control sex and growth characteristics (NTP (National Toxicology Program), 2016), are also a known risk factor for certain types of cancer, including breast (Henderson, Ross, & Bernstein, 1988; Yager & Davidson, 2006) and endometrial (Henderson et al., 1988). Endogenous estrogen is produced naturally and has been associated with an increased risk of certain cancers among women (Eliassen & Hankinson, 2008; Hsieh, Trichopoulos, Katsouyanni, & Yuasa, 1990; Kelsey, Gammon, & John, 1993; Layde et al., 1989). Additionally, exogenous estrogen, which is not produced naturally but administered as part of estrogen therapy, has also been associated with an increased risk of certain cancers (Colton et al., 1993; Grady, Gebretsadik, Kerlikowske, Ernster, & Petitti, 1995; Herbst, Ulfelder, & Poskanzer, 1971; Schairer et al., 2000; Smith, Prentice, Thompson, & Herrmann, 1975). ACEs have been associated with changes in physiological processes (Shonkoff, 2016), and could impact the production of sex hormones. However, none of the identified articles (N = 255) met inclusion criteria.
Immunosuppression
Many medical conditions such as organ transplantations, autoimmune diseases, and inflammatory disorders require long-term immunosuppression therapy. Although immunosuppression improves survival and reduces the risk of organ rejection, patients receiving immunosuppressive drugs face an increased risk for various cancers (Engels et al., 2011). Suppression of an individual's immune system weakens their ability to detect and destroy cancer cells and cancer-causing viral infections. For example, people living with HIV/AIDS have an increased risk of cancer due to immune deficiency, and cancer is a prevalent cause of morbidity within this population (Grulich, van Leeuwen, Falster, & Vajdic, 2007). ACEs have been associated with HIV risk (Felitti et al., 1998) as well as changes in physiological processes (Shonkoff, 2016), and could potentially be associated with later need of immunosuppression. Search terms revealed 23 potential articles; however, none met our inclusion criteria.
Infectious Agents
Certain bacterial, viral, and parasitic infections are risk factors for specific cancer types (Parkin, 2006). These include hepatitis B virus, hepatitis C virus, H. pylori, the human papillomavirus (HPV), and human immunodeficiency virus type 1 (HIV-1) (Mueller, 2003). ACE scores have also been associated with acquiring an HIV infection (Hillis, Anda, Felitti, & Marchbanks, 2001; Lu, Mueser, Rosenberg, & Jankowski, 2008), and a graded relationship exists between ACEs and self-reported sexually-transmitted disease (STD) history (Hillis, Anda, Felitti, Nordenberg, & Marchbanks, 2000). Furthermore, ACEs have been linked to risky sexual behaviors, which lead to an increased risk of acquiring STDs (Lu et al., 2008). In addition, because stress is associated with decreased immune response, stress-inducing childhood trauma could potentially increase susceptibility to infection (Anda et al., 2008). In the current review, we identified 12 articles that investigated associations between childhood adversity and exposure to infectious agents in adulthood. The studies measured various infectious agents, including HIV (N = 10), hepatitis B virus (N = 1), hepatitis C virus (N = 3), Epstein-Barr virus (EBV; N = 2), and cytomegalovirus (CMV; N = 1). Fourteen different types of ACEs were measured across the 12 studies, with the majority collecting information on CSA (N = 10). No studies utilized the original ACE questionnaire or BRFSS data.
Significant associations between adversity and HIV were most common, with exposure to adversity predicting increased risk of HIV infection in adulthood. For example, among African American couples, HIVpositive men were more likely to report CSA histories than HIVnegative men (Nimh Multisite HIV/STD Prevention Trial for African American Couples Group, 2010), although this association was not significant for women (Nimh Multisite HIV/STD Prevention Trial for African American Couples Group, 2010). Additional studies highlighted significant associations between CSA and HIV infection among men who have sex with men (MSM) (Arreola, Neilands, Pollack, Paul, & Catania, 2008; Brennan, Hellerstedt, Ross, & Welles, 2007; Friedman, Marshal, Stall, Cheong, & Wright, 2008; Mimiaga et al., 2009; Phillips et al., 2014). In addition, studies found that adversity scores were associated with an incremental increase in HIV risk (Reisner, Falb, & Mimiaga, 2011; Rosenberg, Lu, Mueser, Jankowski, & Cournos, 2007). For example, each additional exposure to childhood adversity was associated with a 32% increase in odds of HIV infection, and 17.8% of HIV infections were attributable to early adversity (Reisner et al., 2011). However, two studies that used the same dataset from substantiated CM records and matched controls did not find associations between CM and HIV infection (Widom, Czaja, Bentley, &Johnson, 2012; Wilson & Widom, 2008).
Associations between childhood adversity and adult hepatitis B and/or C were not significant across three studies (Nimh Multisite HIV/STD Prevention Trial for African American Couples Group, 2010; Rosenberg et al., 2007; Widom et al., 2012). However, among breast cancer survivors, childhood adversity was associated with elevated antibodies to two latent herpesviruses (e.g., EBV and CMV) (Fagundes, Glaser, Malarkey, & Kiecolt-Glaser, 2013). Elevated EBV antibodies were also associated with repeated exposure to CSA, being exposed to CPA in preschool, and having parents with lower educational attainment and job status, but not with family income (Slopen, McLaughlin, Dunn, & Koenen, 2013).
Obesity
Obesity is a known risk factor for several forms of cancer, including endometrial, esophageal, pancreatic, breast, colorectal, ovarian, and renal cancer (International Agency for Research on Cancer, 2016), and people exposed to ACEs have an increased risk of becoming obese later in life (Gustafson & Sarwer, 2004). Obesity results from an energy imbalance between calories consumed and energy expenditure (e.g., physical activity). Forty-three obesity-related studies met inclusion criteria. The most common measurement of obesity or excess body fat and size was BMI (N = 39), followed by waist circumference/girth (N = 5), waist-to-hip ratio (N = 4), and body composition (N = 1). The majority of studies that measured BMI used a cutoff score of 30 kg/m2 or more to indicate obesity; however, some studies measured increased BMI over time, which may or may not have made the cutoff for obesity. As such, articles included in this section may refer to obesity or excess body fat and size, and will heretofore be referred to as obesity-related measures. A total of 23 types of childhood adversity were measured across the 43 studies, with physical (N = 35), sexual (N = 35), and emotional (N = 22) abuse being the most common. Five studies utilized BRFSS ACE data (Campbell et al., 2016; Dube et al., 2010; Font & Maguire-Jack, 2016; Gjelsvik et al., 2013; McCauley et al., 2015).
Collectively, summed adversity scores (Afifi, Mota, MacMillan, & Sareen, 2013; Crowell et al., 2016; Davis, Usher, et al., 2014; Dube et al., 2010; Duncan, Sartor, et al., 2015; Font & Maguire-Jack, 2016; Friedman, Montez, Sheehan, Guenewald, & Seeman, 2015; Greenfield & Marks, 2009; Hostinar et al., 2015; Li, Chassan, Bruer, Gower, & Shelton, 2015; McCauley et al., 2015; Pederson & Wilson, 2009; Richardson, Dietz, & Gordon-Larsen, 2014; Spann et al., 2014), including early socioeconomic hardships (Bae, Wickrama, & O'Neal, 2014; Wickrama, Kwon, Oshri, & Lee, 2014) and academic adversity (Friedman, Montez, et al., 2015), were positively associated with obesity-related measures. These findings were upheld in female-only samples (Alvarez, Pavao, Baumrind, & Kimerling, 2007; Duncan, Sartor, et al., 2015; Midei, Matthews, & Bromberger, 2010; Shinozaki, Romanowicz, Kung, Rundell, & Mrazek, 2012; Tietjen et al., 2012). In the Missouri Adolescent Female Twin Study, CM was positively associated with both obesity and being underweight (Duncan, Sartor, et al., 2015).
Individually, exposure to harsh physical punishment (Afifi et al., 2013), CPA (Bentley & Widom, 2009; Duncan, Auslander, et al., 2015; Li et al., 2015), CSA (Campbell et al., 2016; Font & Maguire-Jack, 2016), mental illness or substance abuse in the household (Font & Maguire-Jack, 2016), and childhood SES (Lehman, Taylor, Kiefe, & Seeman, 2005) were positively associated with obesity measures. In a sample of AI/AN, verbal abuse was associated with obesity (Hodge, Stemmler, & Nandy, 2014), but other CM types were not. In studies with female-only samples, CSA (Boynton-Jarrett, Rosenberg, Palmer, Boggs, & Wise, 2012; Duncan, Sartor, et al., 2015; Noll, Zeller, Trickett, & Putnam, 2007; Rich-Edwards et al., 2010; Rohde et al., 2008; Smith et al., 2010), CPA (Boynton-Jarrett et al., 2012; Francis, Nikulina, & Widom, 2015; Rich-Edwards et al., 2010; Rohde etal., 2008), emotional abuse (Mason et al., 2015), severity of neglect (Pederson & Wilson, 2009), and severity of abuse (Riley, Wright, Jun, Hibert, & Rich-Edwards, 2010) were positively associated with obesity-related measures.
Among lesbian and/or bisexual women, CSA (Aaron & Hughes, 2007; Lehavot & Simoni, 2011), CPA (Lehavot & Simoni, 2011), emotional abuse (Lehavot & Simoni, 2011), emotional neglect (Lehavot & Simoni, 2011), and physical neglect (Lehavot & Simoni, 2011) were associated with obesity-related measures. In addition, several studies found that differences in obesity prevalence between abused and non-abused women grew wider over time (Midei et al., 2010; Rich-Edwards et al., 2010).
Fifteen studies reported mixed findings between obesity and various measures of childhood adversity, and six studies found no significant direct associations (Davis, Dearing, etal., 2014; Grilo et al., 2005; McIntyre et al., 2012; Min, Minnes, Kim, & Singer, 2013; Ramirez & Milan, 2016; Schrepf et al., 2014). For example, childhood trauma was not associated with BMI among a sample of healthy adults; however, in mediation models, trauma was associated with distress, distress with use of food coping, and use of food coping with elevated BMI (Schrepf et al., 2014). Other studies found that adversity scores (Campbell et al., 2016; Davis, Dearing, et al., 2014; Grilo et al., 2005; McIntyre et al., 2012; Richardson et al., 2014), CSA (Bentley & Widom, 2009; Ramirez & Milan, 2016), neglect (Bentley & Widom, 2009), early family environment (Lehman et al., 2005), and severity of abuse (Min et al., 2013) were not associated with obesity-related measures.
Physical Activity
The relationship of ACEs to physical activity was assessed in five studies, and accompanied measurements of BMI or waist circumference. Studies investigating the relationship between early adversity and physical activity were less common, and had varied results. ACE score (Hostinar et al., 2015) and having an incarcerated household member (Gjelsvik et al., 2013) were significantly associated with less physical activity, but childhood adversity was unrelated to physical activity in a sample of middle-aged adults from Boston (Davis, Usher, et al., 2014). In women-only studies, CSA was associated with greater physical activity, although CPA (Bertone-Johnson et al., 2012) and severity of abuse (Riley et al., 2010) were not.
Radiation
Radiation occurring at certain wavelengths can damage DNA and increase cancer risk (El Ghissassi et al., 2009). Radiation occurs naturally in the environment (e.g., radon), but high-energy radiation such as X-rays and gamma rays is also released during nuclear power plant accidents and atomic weapons development, testing, and use. Given that people may be at higher risk for exposure to harmful radiation based on their geographic location (Cohen, 1995) and that exposure to early adversity varies across geographic regions (Stoltenborgh, Bakermans-Kranenburg, & van Ijzendoorn, 2013), it is possible that early adversity may be more prevalent in areas where radiation exposure is also higher. Our search terms revealed 204 potential articles; however, none met our inclusion criteria.
Ultraviolet Radiation
Exposure to ultraviolet (UV) radiation from sunlight or artificial sources, including sunlamps and tanning booths, is associated with skin cancer (Boniol, Autier, Boyle, & Gandini, 2012; El Ghissassi et al., 2009; U.S. Department of Health and Human Services, 2014). Both intentional tanning (i.e., indoor tanning) and ACEs have been associated with mental health and substance abuse (Coups & Phillips, 2011; Felitti et al., 1998), and thus, it is possible that exposure to ACEs could influence sun protection behavior and intentional tanning. However, none of the identified articles (N = 84) met the inclusion criteria.
Tobacco
Tobacco smoking causes cancers of the lung, oral cavity, naso-, oro- and hypopharynx, nasal cavity and accessory sinuses, larynx, esophagus, stomach, pancreas, colorectal, liver, kidney (body and pelvis), ureter, urinary bladder, uterine cervix and ovary (mucinous), and myeloid leukemia (IARC Working Group on the Evaluation of Carcinogenic Risk to Humans, 2012f; Warren, Alberg, Kraft, & Cummings, 2014). Furthermore, smoking can weaken the immune response, blocking the body's ability to fight cancer (U.S. Department of Health and Human Services, 2010). ACEs have been associated with smoking status whereby higher ACE scores correspond to greater odds of being a current smoker (Felitti et al., 1998) and being nicotinedependent (Xie et al., 2012). Furthermore, long-term tobacco use has been identified as a coping strategy for the negative effects of ACEs (Anda et al., 1999). Forty-one articles met inclusion criteria. Various tobacco-related behaviors were measured, including tobacco/nicotine use (N = 5), smoking status (Current N =16; Lifetime N =18; Past year N = 1; Quit N = 1), and other tobacco-related behaviors (N = 11). Twenty-one types of ACEs were assessed across the 41 studies. Ten studies used data from the BRFSS ACE module (Campbell et al., 2016; Chapman et al., 2013; Dube et al., 2010; Font & Maguire-Jack, 2016; Ford et al., 2011; Fuller-Thomson et al., 2013; Gjelsvik et al., 2013; Vander Weg, 2011; Walsh & Cawthon, 2014; Yeoman et al., 2013), and four used data from the original ACE study (Brown et al., 2010; Dong et al., 2005; Edwards et al., 2007; Strine et al., 2012).
Summary adversity scores were positively associated with tobacco-related behaviors (Brown et al., 2010; Campbell et al., 2016; Chapman et al., 2013; Dong et al., 2005; Edwards et al., 2007; Elliott et al., 2014; Font & Maguire-Jack, 2016; Ford et al., 2011; Hostinar et al., 2015; Lehavot & Simoni, 2011; Mersky, Topitzes, & Reynolds, 2013; Mingione, Heffner, Blom, & Anthenelli, 2012; Morton, Mustillo, & Ferraro, 2014; Su et al., 2015; Topitzes, Mersky, & Reynolds, 2010; Vander Weg, 2011; Walsh & Cawthon, 2014; Wu et al., 2010; Yeoman et al., 2013). This positive association was found in a sample of lesbian and bisexual women (Lehavot & Simoni, 2011) and ethnic/racial minority samples (Mersky et al., 2013), including Hispanics (Allem et al., 2015) and African Americans (Slopen et al., 2012). Both severity (Bertone-Johnson et al., 2012; Sacco et al., 2007; Spratt et al., 2009; Taha, Galea, Hien, & Goodwin, 2014) and frequency (Sacco et al., 2007; Taha et al., 2014) of trauma exposures were associated with smoking status.
Individually, CSA (Campbell et al., 2016; Chapman et al., 2013; Elliott et al., 2014; Font & Maguire-Jack, 2016; Ford et al., 2011), CPA (Chapman et al., 2013; Elliott et al., 2014; Ford et al., 2011; Taha et al., 2014), emotional abuse (Allem et al., 2015; Campbell et al., 2016; Chapman et al., 2013; Elliott et al., 2014; Ford et al., 2011; Taha et al., 2014), mental illness (Allem et al., 2015; Chapman et al., 2013; Font & Maguire-Jack, 2016; Ford et al., 2011) or substance abuse (Allem et al., 2015; Campbell et al., 2016; Chapman etal., 2013; Fordet al., 2011) in the household, witnessing domestic violence (Chapman et al., 2013; Ford et al., 2011), family disruption/separation by age 15 (Larson & Halfon, 2013), having an incarcerated household member (Chapman et al., 2013; Font & Maguire-Jack, 2016; Ford et al., 2011), foster care history (Thompson & Hasin, 2011), and parental divorce/separation (Allem et al., 2015; Campbell et al., 2016; Chapman et al., 2013; Font & Maguire-Jack, 2016; Ford et al., 2011; Larson & Halfon, 2013) were all positively associated with tobacco-related behaviors, but emotional neglect was associated with less nicotine dependence in one study (Elliott et al., 2014). Having an incarcerated household member was positively associated with smoking status among Hispanics and non-Hispanic Whites, but not among non-Hispanic Blacks (Gjelsvik et al., 2013). Among patients utilizing services at Indian Health Service clinics in California, both neglect and CPA were associated with smoking, but CSA was not (Hodge & Nandy, 2011).
Among female-only samples, alcohol abuse (Fuller-Thomson et al., 2013) or drug abuse (Fuller-Thomson et al., 2013) in the household, parental separation/divorce (Fuller-Thomson et al., 2013; Strine et al., 2012), having an incarcerated household member (Strine et al., 2012), CSA (Bertone-Johnson et al., 2012; Fuller-Thomson et al., 2013; Jessup, Dibble, & Cooper, 2012; Pederson et al., 2008), CPA (Bertone-Johnson et al., 2012; Fuller-Thomson et al., 2013; Jessup et al., 2012; Pederson et al., 2008; Strine et al., 2012), any abuse (De Von Figueroa-Moseley, Landrine, & Klonoff, 2004), physical neglect (Strine et al., 2012), and verbal/emotional abuse (Fuller-Thomson et al., 2013; Pederson et al., 2008; Strine et al., 2012) were all associated with tobacco use and related behaviors. For men, alcohol abuse or drug abuse in the household, parental separation/divorce, and CPA were associated with smoking status (Fuller-Thomson et al., 2013), and among MSM, CSA was associated with smoking (O'Cleirigh et al., 2015).
Several studies found no significant associations (N = 5) or mixed associations (N = 5). For example, CM was not associated with smoking among never-deployed young male Marines (Agorastos et al., 2014), nor in a sample of primarily poor, urban dwelling African American women with a history of substance use during pregnancy (Min et al., 2013). In other studies, significant associations between smoking status and related behaviors were not found for individuals exposed to CPA (Francis et al., 2015; Kristman-Valente, Brown, & Herrenkohl, 2013), CSA (Kristman-Valente et al., 2013), or CM (Kim & Williams, 2009). ACE score from Wave 2 of the original ACE study was not associated with smoking status, and among men, individual ACE categories were not associated with smoking (Strine et al., 2012). Using BRFSS ACE data, exposure to any child abuse was not associated with smoking status (Dube et al., 2010), but exposure to any household challenges was positively associated (Dube et al., 2010).
Discussion
The purpose of this review was to describe the scope and nature of the published evidence on associations between ACEs and behaviors and exposures in adulthood that are associated with increased risk for cancer. We identified 155 quantitative, peer-reviewed, US-based articles published between 2005 and 2015 that examined associations between childhood adversity and the presence of cancer risk factors in adulthood. The majority of articles investigated associations between ACEs and alcohol, obesity/excess body fat or size, and tobacco. Fewer studies investigated the links between ACEs and chronic inflammation or infectious agents. No publications met our inclusion criteria and investigated associations between ACEs and environmental carcinogens, hormones, immunosuppression, radiation, or ultraviolet radiation, highlighting gaps in the literature. Although not all of these connections are intuitive, ACEs and some of these risk factors share similar underlying risk factors. For example, research suggests that children living in poverty are at higher risk of exposure to both environmental carcinogens (Payne-Sturges & Gee, 2006; Powell & Stewart, 2001) and violence (Sedlak et al., 2010), which may both contribute, independently or cumulatively, to their adult cancer risk.
Associations varied by the ACE measure, the cancer risk factor, sample demographics, and study methodologies. Despite these variations, when taken together, the studies highlight the potential impact of childhood experiences on risk factors for cancer in adulthood, and may explain some of the association between ACEs and cancer found in previous reviews (Holman et al., 2016). As such, efforts to prevent ACEs or minimize their negative impact on individuals' lives may result in reductions in certain cancer risk factors, potentially contributing to decreases in cancer incidence over time. Implications for clinical practice, particularly for pediatric nurses are described below.
This scoping review uncovered notable research gaps and limitations, including inconsistencies in defining and measuring ACEs, the lack of diversity in study samples, and areas of research that have yet to be explored. Addressing these research gaps and limitations could expand our understanding of the associations between early adversity and cancer risk. Recommendations for future research, in the context of our findings, are expounded on below.
Limitations
This review is not without limitations. The diversity in ACE and cancer risk factor measurement and study methodologies resulted in an inability to analytically synthesize the results. Additionally, although our selected inclusion criteria excluded less rigorous studies, it was beyond the scope of this review to assess methodological quality. We also limited study selection to the US and to the previous 10 years; as such, more research may be available that was not included here, including grey literature. The selected search terms may not have picked up important associations between ACEs and cancer risk. For example, the hormone search criteria were limited to words specific to sex hormones, and thus we did not capture articles related to cortisol or other hormones that may significantly contribute to associations between ACEs and cancer risk. Additionally, the selected risk factors may have over simplified the relationship between ACEs and cancer risk. For example, the complex relationship between physical activity, obesity and cancer risk was beyond the scope of this review. Sociodemographic considerations were also limited in this review. However, studies with restricted demographic samples were identified; 12 studies specifically focused on LGBT populations; seven studies included Black participants only; two studies included American Indian/Alaskan Native participants only; and three studies included Hispanic participants only. Finally, cancer risk factors were restricted to those present in adulthood, although many risk factors begin to develop before the age of 18.
Implications for Nursing Practice
Pediatric nurses see a wide range of health issues – both physical and emotional – that have short- and long-term effects on patients. Pediatric nurses are a trusted resource for children and families, and they are often the only service providers who come into contact with all children on a regular basis. As such, pediatric nurses can play an important role in both treating and preventing ACEs. Nurses can help identify children at risk of ACEs and connect families to appropriate services (e.g., social/economic services, parent training, and counseling). They are also ideally suited to break the intergeneration transmission between parents/caregivers, and the children/babies they see in their practice by engaging with parents/caretakers during the child's appointment. In doing so, they can identify parents who may need assistance and connect them to services. This can reduce the risk of children experiencing ACEs. Pediatric nurses may also be the first to identify symptoms related to exposure to ACEs (somatic complaints, mental health issues, behavioral problems) (American Academy of Pediatrics & Pediatric Orthopaedic Society of North America, 2008). Pediatric nurses who are knowledgeable about ACEs may be able to direct families to the services they need to address the root causes of health consequences related to ACEs. As such, being informed about ACEs and equipped with as many treatment options and resources as possible could reduce the number of children and adults that need treatment and care further downstream. It is also important to understand the ways in which ACEs extend beyond the patient populations. ACEs are a significant public health concern that inflict high individual and social costs on patients, their families, and communities at large. Pediatric nurses are ideally situated to educate others about the biology of adversity and healthy child development to improve outcomes for children who experience adversity, and to help decrease the heavy toll ACEs take on our society and collective health.
Recommendations for Future Research
Given the variability in the associations between ACEs and cancer risk factors, the field could benefit from more studies that utilize a uniform approach to measuring adversity and later health. One suggestion is to encourage the use of uniform definitions and best practices for measurement. For example, previous research suggests that behaviorally specific questions may increase disclosure of violence and victimization compared to checklist items (Cook, Gidycz, Koss, & Murphy, 2011); however, many of the included studies relied on checklist items only. Indeed, stronger associations between CSA and alcohol use were found using behavioral questions compared to checklist items (Sartor et al., 2012), which suggests that measurement of ACEs could have significant implications on reported associations, and may have contributed to the varied results in the present review.
Beyond question type, the diversity in ACE categories and dimensions of exposure warrants consideration. Over thirty different types of childhood adversity were measured by the studies included in this review. Some studies created a summed adversity scores and others relied on individual items, which likely contributed to variations in study findings, and made comparisons across studies challenging. In addition, few considered other important dimensions of ACEs, such as age of exposure, severity, frequency, relationship to perpetrator, and symptomology, which all likely contribute to later risk of poorer outcomes. Furthermore, although investigations of protective factors were not within the scope of this review, many studies lacked information on the effects of potential protective factors, such as access to a safe, stable, nurturing relationship with an adult. A thorough understanding of this critical dimension would help to inform novel prevention strategies. A deeper investigation of ACEs and cancer risk, through quantitative and qualitative studies, could better inform cancer risk reduction, and may contribute to innovative ways to change a person's cancer risk trajectory, starting in childhood.
Studies specific to women (N = 43) were more prevalent, particularly for alcohol and obesity outcomes. Future research is needed to better understand the distribution of ACE exposure across different sociodemographic groups and the differential impact of adversity on risk across one's lifetime. To understand the complex connections and interactions between childhood experiences and adult cancer risk, researchers could provide critical information to practitioners and policy-makers by consistently and systematically identifying how race/ethnicity, sexual orientation, gender identity, SES and other markers of advantage and disadvantage contribute to inequities in exposures and outcomes between groups. These explorations can equip researchers and practitioners with a better understanding of risk factors for early adversity and later health conditions, and may contribute to a broader evidence-base for prevention and intervention approaches for all sociodemographic backgrounds.
Despite no found associations between ACEs and sex hormones, the role of other hormones warrants attention in future work. For example, cortisol, an anti-inflammatory hormone that plays a key role in our stress response, has been associated with impaired immune response, which can complicate cancer risk and recovery (Schrepf et al., 2013). Cortisol and distorted physiological stress responses have been linked to childhood trauma (Shonkoff, 2016), and while these topics were beyond the scope of this review, they are an important consideration for future research. In addition, despite the paucity of research, the connection between ACEs and immune response, which likely confounds the relationship of ACEs to other risk factors, including infectious agents, is an important future direction of research. As noted above, researchers have found that childhood trauma is associated with prolonged activation of the stress response system (Shonkoff, 2016); this prolonged activation stimulates irregular cortisol production, which impairs the immune response and alters cancer risk and recovery (Schrepf et al., 2013).
It remains important to consider what contexts place children and families at greater risk of ACEs and cancer risk factors, as well as how context may contribute to the accumulation of adversity and cancer risk over time and compound the impact of exposure on risk of cancer. Twelve studies included measures of family poverty, but little is known about how this may have put children and families at risk of additional adversity across their lives. More research is needed to understand the complexity of such relationships, including how social and structural determinants of health place individuals and families at increased risk of poverty, which then puts them at increased risk of ACEs and poorer health outcomes (Metzler et al., 2017; Sedlak et al., 2010) - cycles that can repeat across generations. To address and prevent ACEs, comprehensive strategies that work across the social ecological levels (individual, relational, community, and societal), generations and sectors are needed. Another important issue to consider is the accumulation of trauma over time. Exposure to ACEs heightens risk for additional violent exposures, which may then compound and accumulate cancer risk. For example, Eames et al. (2014) found that among men with high adult stress, those who experienced higher ACEs consumed more alcohol than men did with no or low ACEs. This suggests that ACEs may intensify the effect of adult stress on drinking behaviors, and possibly other modifiable risk behaviors. Similarly, ACEs can accumulate across and impact future generations (Schofield, Lee, & Merrick, 2013). Therefore, prevention strategies could consider a generational approach whereby parents exposed to childhood adversity are included in intervention strategies.
Conclusion
Despite limitations, this review has important implications for cancer research and health care practice. Given the breadth of the science and noted associations between ACEs and cancer risk, we encourage researchers to take ACEs into account when planning future studies of cancer risk and prevention. Practitioners, including nurses and mental health providers, may wish to implement ACE screening and prevention strategies using clinical interventions and treatment programs. Furthermore, the effective prevention of ACEs and management of subsequent health outcomes require programs and policies that assure that children and families have access to the essentials – safe, stable, nurturing relationships and environments – so that all children can reach their full health and life potential (Centers for Disease Control and Prevention, 2014; Fortson et al., 2016). Antecedents for adult cancer may be rooted in childhood experiences; therefore, the importance of preventing and treating exposure to ACEs before they occur can be innovative in upstream cancer prevention.
Supplementary Material
Acknowledgements
During manuscript preparation, Karen E. Dyer, Ph.D. was supported by the National Cancer Institute R25 Training Program in Behavioral and Health Services Cancer Control Research (R25-CA093423) and by a VA-funded Quality Enhancement Research Initiative (QUERI) project (QUE 15-272).
Abbreviations:
- ACEs
Adverse Childhood Experiences
- AI/AN
American Indians and Alaskan Natives
- BRFSS
Behavioral Risk Factor Surveillance System
- CDC
Centers for Disease Control & Prevention
- CM
child maltreatment
- CPA
childhood physical abuse
- CRP
C-reactive protein
- CSA
childhood sexual abuse
- HPV
human papillomavirus
- IL-1β
interleukin-1 beta
- IL-6
interleukin-6
- LGB
lesbian, gay, bisexual
- MIDUS II Study
the National Survey of Midlife Development in the United States
- MSM
men who have sex with men
- NCI
National Cancer Institute's
- TNF-α
tumor necrosis factor-alpha
- UV
ultraviolet
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pedn.2018.10.009.
References
- Aaron DJ, & Hughes TL (2007). Association of childhood sexual abuse with obesity in a community sample of lesbians. Obesity (Silver Spring), 15(4), 1023–1028. 10.1038/oby.2007.634. [DOI] [PubMed] [Google Scholar]
- Adamkiewicz G, Spengler JD, Harley AE, Stoddard A, Yang M, Alvarez-Reeves M, & Sorensen G (2014). Environmental conditions in low-income urban housing: Clustering and associations with self-reported health. American Journal of Public Health, 104(9), 1650–1656. 10.2105/AJPH.2013.301253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Afifi TO, Mota N, MacMillan HL, & Sareen J (2013). Harsh physical punishment in childhood and adult physical health. Pediatrics, 132(2), e333–e340. 10.1542/peds.2012-4021. [DOI] [PubMed] [Google Scholar]
- Agorastos A, Pittman JO, Angkaw AC, Nievergelt CM, Hansen CJ, Aversa LH,… Baker DG (2014).The cumulative effect of different childhood trauma types on self-reported symptoms of adult male depression and PTSD, substance abuse and health-related quality of life in a large active-duty military cohort. Journal of Psychiatric Research, 58,46–54. 10.1016/j.jpsychires.2014.07.014. [DOI] [PubMed] [Google Scholar]
- Allem JP, Soto DW, Baezconde-Garbanati L, & Unger JB (2015). Adverse childhood experiences and substance use among Hispanic emerging adults in Southern California. Addictive Behaviors, 50, 199–204. 10.1016/j.addbeh.2015.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez J, Pavao J, Baumrind N, & Kimerling R (2007). The relationship between child abuse and adult obesity among California women. American Journal of Preventive Medicine, 33(1), 28–33. 10.1016/j.amepre.2007.02.036. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics, & Pediatric Orthopaedic Society of North America (2008). Management of pediatric trauma. Pediatrics, 121(4), 849–854.18381551 [Google Scholar]
- Anda RF, Brown DW, Dube SR, Bremner JD, Felitti VJ, & Giles WH (2008). Adverse childhood experiences and chronic obstructive pulmonary disease in adults. American Journal of Preventive Medicine, 34(5), 396–403. 10.1016/j.amepre.2008.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anda RF, Croft JB, Felitti VJ, Nordenberg D, Giles WH, Williamson DF, & Giovino GA (1999). Adverse childhood experiences and smoking during adolescence and adulthood. JAMA, 282(17), 1652–1658. [DOI] [PubMed] [Google Scholar]
- Anderson CM, Rabi K, Lukas SE, & Teicher MH (2010). Cerebellar lingula size and experiential risk factors associated with high levels of alcohol and drug use in young adults. Cerebellum, 9(2), 198–209. 10.1007/s12311-009-0141-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appleton AA, Buka SL, McCormick MC, Koenen KC, Loucks EB, & Kubzansky LD (2012). The association between childhood emotional functioning and adulthood inflammation is modified by early-life socioeconomic status. Health Psychology, 31(4), 413–422. 10.1037/a0027300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arksey H, & O'Malley L (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology: Theory and Practice., 8(1), 19–32. [Google Scholar]
- Arreola S, Neilands T, Pollack L, Paul J, & Catania J (2008). Childhood sexual experiences and adult health sequelae among gay and bisexual men: Defining childhood sexual abuse. Journal of Sex Research, 45(3), 246–252. 10.1080/00224490802204431. [DOI] [PubMed] [Google Scholar]
- Bae D, Wickrama KA, & O'Neal CW (2014). Social consequences of early socioeconomic adversity and youth BMI trajectories: Gender and race/ethnicity differences. Journal of Adolescence, 37(6), 883–892. 10.1016/j.adolescence.2014.06.002. [DOI] [PubMed] [Google Scholar]
- Banducci AN, Hoffman E, Lejuez CW, & Koenen KC (2014). The relationship between child abuse and negative outcomes among substance users: Psychopathology, health, and comorbidities. Addictive Behaviors, 39(10), 1522–1527. 10.1016/j.addbeh.2014.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellis MA, Hughes K, Leckenby N, Hardcastle KA, Perkins C, & Lowey H (2015). Measuring mortality and the burden of adult disease associated with adverse childhood experiences in England: A national survey. Journal of Public Health (Oxford, England), 37(3), 445–454. 10.1093/pubmed/fdu065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentley T, & Widom CS (2009). A 30-year follow-up of the effects of child abuse and neglect on obesity in adulthood. Obesity (Silver Spring), 17(10), 1900–1905. 10.1038/oby.2009.160. [DOI] [PubMed] [Google Scholar]
- Bertone-Johnson ER, Whitcomb BW, Missmer SA, Karlson EW, & Rich-Edwards JW (2012). Inflammation and early-life abuse in women. American Journal of Preventive Medicine, 43(6), 611–620. 10.1016/j.amepre.2012.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Xu Y, Brady K, Perez-Fuentes G, Okuda M, & Wang S (2013). Comorbidity of posttraumatic stress disorder with alcohol dependence among US adults: Results from National Epidemiological Survey on Alcohol and Related Conditions. Drug and Alcohol Dependence, 132(3), 630–638. 10.1016/j.drugalcdep.2013.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boniol M, Autier P, Boyle P, & Gandini S (2012). Cutaneous melanoma attributable to sunbed use: Systematic review and meta-analysis. BMJ, 345, e4757 10.1136/bmj.e4757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boynton-Jarrett R, Rosenberg L, Palmer JR, Boggs DA, & Wise LA (2012). Child and adolescent abuse in relation to obesity in adulthood: The Black women's health study. Pediatrics, 130(2), 245–253. 10.1542/peds.2011-1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan DJ, Hellerstedt WL, Ross MW, & Welles SL (2007). History of childhood sexual abuse and HIV risk behaviors in homosexual and bisexual men. American Journal of Public Health, 97(6), 1107–1112. 10.2105/AJPH.2005.071423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown DW, Anda RF, Felitti VJ, Edwards VJ, Malarcher AM, Croft JB, & Giles WH (2010). Adverse childhood experiences are associated with the risk of lung cancer: A prospective cohort study. BMC Public Health, 10, 20 10.1186/1471-2458-10-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown DW, Anda RF, Tiemeier H, Felitti VJ, Edwards VJ, Croft JB, & Giles WH (2009).Adverse childhood experiences and the risk of premature mortality. American Journal of Preventive Medicine, 37(5), 389–396. 10.1016/j.amepre.2009.06.021. [DOI] [PubMed] [Google Scholar]
- Brown MJ, Thacker LR, & Cohen SA (2013). Association between adverse childhood experiences and diagnosis of cancer. PLoS One, 8(6), e65524 10.1371/journal.pone.0065524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell JA, Walker RJ, & Egede LE (2016). Associations between adverse childhood experiences, high-risk behaviors, and morbidity in adulthood. American Journal of Preventive Medicine, 50(3), 344–352. 10.1016/j.amepre.2015.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson M, Oshri A,&Kwon J (2015). Child maltreatment and risk behaviors: The roles of callous/unemotional traits and conscientiousness. Child Abuse & Neglect, 50, 234–243. 10.1016/j.chiabu.2015.07.003. [DOI] [PubMed] [Google Scholar]
- Carlson MD, Harden KP, Kretsch N, Corbin WR, & Fromme K (2015). Interactions between DRD4 and developmentally specific environments in alcohol-dependence symptoms. Journal of Abnormal Psychology, 124(4), 1043–1049. 10.1037/abn0000120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter LL, Gawuga CE, Tyrka AR, Lee JK, Anderson GM, & Price LH (2010). Association between plasma IL-6 response to acute stress and early-life adversity in healthy adults. Neuropsychopharmacology, 35(13), 2617–2623. 10.1038/npp.2010.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2014). Essentials for childhood: steps to create safe, stable, nurturing relationships and environments. Retrieved from http://www.cdc.gov/violenceprevention/pdf/essentials_for_childhood_framework.pdf.
- Chapman DP, Liu Y, Presley-Cantrell LR, Edwards VJ, Wheaton AG, Perry GS, & Croft JB (2013).Adverse childhood experiences and frequent insufficient sleep in 5 U.S. states, 2009: A retrospective cohort study. BMC Public Health, 13, 3 10.1186/1471-2458-13-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho HJ, Bower JE, Kiefe CI, Seeman TE, & Irwin MR (2012). Early life stress and inflammatory mechanisms of fatigue in the Coronary Artery Risk Development in Young Adults (CARDIA) study. Brain, Behavior, and Immunity, 26(6), 859–865. 10.1016/j.bbi.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen BL (1995). Test of the linear-no threshold theory of radiation carcinogenesis for inhaled radon decay products. Health Physics, 68(2), 157–174. [DOI] [PubMed] [Google Scholar]
- Coker AL, Hopenhayn C, DeSimone CP, Bush HM, & Crofford L (2009). Violence against women raises risk of cervical cancer. Journal of Women's Health (2002), 18 (8), 1179–1185. 10.1089/jwh.2008.1048. [DOI] [PubMed] [Google Scholar]
- Colton T, Greenberg ER, Noller K, Resseguie L, Van Bennekom C, Heeren T, & Zhang Y (1993). Breast cancer in mothers prescribed diethylstilbestrol in pregnancy. Further follow-up. JAMA, 269(16), 2096–2100. [PubMed] [Google Scholar]
- Cook SL, Gidycz CA, Koss MP, & Murphy M (2011). Emerging issues in the measurement of rape victimization. Violence Against Women, 17(2), 201–218. 10.1177/1077801210397741. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Wolke D, Lereya ST, Shanahan L, Worthman C, & Costello EJ (2014). Childhood bullying involvement predicts low-grade systemic inflammation into adulthood. Proceedings of the National Academy of Sciences of the United States of America, 111(21), 7570–7575. 10.1073/pnas.1323641111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corstorphine E, Waller G, Lawson R, & Ganis C (2007). Trauma and multi-impulsivity in the eating disorders. Eating Behaviors, 8(1), 23–30. 10.1016/j.eatbeh.2004.08.009. [DOI] [PubMed] [Google Scholar]
- Coups EJ, & Phillips LA (2011).A more systematic review of correlates of indoor tanning. Journal of the European Academy of Dermatology and Venereology, 25(5), 610–616 (author reply 617–618) 10.1111/j.1468-3083.2011.03996.x. [DOI] [PubMed] [Google Scholar]
- Coussens LM, & Werb Z (2002). Inflammation and cancer. Nature, 420(6917), 860–867. 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crosswell AD, Bower JE, & Ganz PA (2014). Childhood adversity and inflammation in breast cancer survivors. Psychosomatic Medicine, 76(3), 208–214. 10.1097/PSY.0000000000000041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowell JA, Davis CR, Joung KE, Usher N, McCormick SP, Dearing E, & Mantzoros CS (2016). Metabolic pathways link childhood adversity to elevated blood pressure in midlife adults. Obesity Research & Clinical Practice, 10(5), 580–588. 10.1016/j.orcp.2015.10.009. [DOI] [PubMed] [Google Scholar]
- Danese A, & McEwen BS (2012). Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiology & Behavior, 106(1), 29–39. 10.1016/j.physbeh.2011.08.019. [DOI] [PubMed] [Google Scholar]
- Davis CR, Dearing E, Usher N, Trifiletti S, Zaichenko L, Ollen E, … Crowell JA (2014). Detailed assessments of childhood adversity enhance prediction of central obesity independent of gender, race, adult psychosocial risk and health behaviors. Metabolism, 63(2), 199–206. 10.1016/j.metabol.2013.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis CR, Usher N, Dearing E, Barkai AR, Crowell-Doom C, Neupert SD, … Crowell JA (2014). Attachment and the metabolic syndrome in midlife: The role of interview-based discourse patterns. Psychosomatic Medicine, 76(8), 611–621. 10.1097/PSY.0000000000000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Von Figueroa-Moseley C, Landrine H, & Klonoff EA (2004). Sexual abuse and smoking among college student women. Addictive Behaviors, 29(2), 245–251. 10.1016/j.addbeh.2003.07.004. [DOI] [PubMed] [Google Scholar]
- Dong M, Anda RF, Felitti VJ, Williamson DF, Dube SR, Brown DW, & Giles WH (2005). Childhood residential mobility and multiple health risks during adolescence and adulthood: The hidden role of adverse childhood experiences. Archives of Pediatrics & Adolescent Medicine, 159(12), 1104–1110. 10.1001/archpedi.159.12.1104. [DOI] [PubMed] [Google Scholar]
- Drabble L, Trocki KF, Hughes TL, Korcha RA, & Lown AE (2013). Sexual orientation differences in the relationship between victimization and hazardous drinking among women in the National Alcohol Survey. Psychology of Addictive Behaviors, 27(3), 639–648. 10.1037/a0031486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, & Giles WH (2001). Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: Findings from the adverse childhood experiences study. JAMA, 286(24), 3089–3096. [DOI] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Edwards VJ, & Croft JB (2002). Adverse childhood experiences and personal alcohol abuse as an adult. Addictive Behaviors, 27(5), 713–725. [DOI] [PubMed] [Google Scholar]
- Dube SR, Cook ML, & Edwards VJ (2010). Health-related outcomes of adverse childhood experiences in Texas, 2002. Preventing Chronic Disease, 7(3), A52. [PMC free article] [PubMed] [Google Scholar]
- Dube SR, Fairweather D, Pearson WS, Felitti VJ, Anda RF, & Croft JB (2009). Cumulative childhood stress and autoimmune diseases in adults. Psychosomatic Medicine, 71(2), 243–250. 10.1097/PSY.0b013e3181907888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube SR, Miller JW, Brown DW, Giles WH, Felitti VJ, Dong M, & Anda RF (2006). Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. The Journal of Adolescent Health, 38 (4),444 ( e441–410) 10.1016/j.jadohealth.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Duncan AE, Auslander WF, Bucholz KK, Hudson DL, Stein RI, & White NH (2015). Relationship between abuse and neglect in childhood and diabetes in adulthood: Differential effects by sex, national longitudinal study of adolescent health. Preventing Chronic Disease, 12, E70 10.5888/pcd12.140434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan AE, Sartor CE, Jonson-Reid M, Munn-Chernoff MA, Eschenbacher MA, Diemer EW, … Heath AC (2015). Associations between body mass index, post-traumatic stress disorder, and child maltreatment in young women. Child Abuse & Neglect, 45,154–162. 10.1016/j.chiabu.2015.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eames SF, Businelle MS, Suris A, Walker R, Rao U, North CS, … Adinoff B (2014). Stress moderates the effect of childhood trauma and adversity on recent drinking in treatment-seeking alcohol-dependent men. Journal of Consulting and Clinical Psychology, 82(3), 441–447. 10.1037/a0036291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards VJ, Anda RF, Gu D, Dube SR, & Felitti VJ (2007). Adverse childhood experiences and smoking persistence in adults with smoking-related symptoms and illness. The Permanente Journal, 11(2), 5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Ghissassi F, Baan R, Straif K, Grosse Y, Secretan B, Bouvard V, … Group, W. H. O. I. A. f. R. o. C. M. W (2009). A review of human carcinogens—Part D: Radiation. The Lancet Oncology, 10(8), 751–752. [DOI] [PubMed] [Google Scholar]
- Eliassen AH, & Hankinson SE (2008). Endogenous hormone levels and risk of breast, endometrial and ovarian cancers: Prospective studies. Advances in Experimental Medicine and Biology, 630,148–165. [PubMed] [Google Scholar]
- Elliott JC, Stohl M, Wall MM, Keyes KM, Goodwin RD, Skodol AE, … Hasin DS (2014). The risk for persistent adult alcohol and nicotine dependence: The role of childhood maltreatment. Addiction, 109(5), 842–850. 10.1111/add.12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott JC, Stohl M, Wall MM, Keyes KM, Skodol AE, Eaton NR,… Hasin DS (2016). Childhood maltreatment, personality disorders and 3-year persistence of adult alcohol and nicotine dependence in a national sample. Addiction, 111(5), 913–923. 10.1111/add.13292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engels EA, Pfeiffer RM, Fraumeni JF Jr., Kasiske BL, Israni AK, Snyder JJ, … Lin M (2011). Spectrum of cancer risk among US solid organ transplant recipients. JAMA, 306(17), 1891–1901. 10.1001/jama.2011.1592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans GW, & Kantrowitz E (2002). Socioeconomic status and health: The potential role of environmental risk exposure. Annual Review of Public Health, 23,303–331. 10.1146/annurev.publhealth.23.112001.112349. [DOI] [PubMed] [Google Scholar]
- Fagundes CP, Glaser R, Malarkey WB, & Kiecolt-Glaser JK (2013). Childhood adversity and herpesvirus latency in breast cancer survivors. Health Psychology, 32(3), 337–344. 10.1037/a0028595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, … Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. [DOI] [PubMed] [Google Scholar]
- Fenton MC, Geier T, Keyes K, Skodol AE, Grant BF, & Hasin DS (2013). Combined role of childhood maltreatment, family history, and gender in the risk for alcohol dependence. Psychological Medicine, 43(5), 1045–1057. 10.1017/S0033291712001729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fetzner MG, McMillan KA, Sareen J, & Asmundson GJ (2011). What is the association between traumatic life events and alcohol abuse/dependence in people with and without PTSD? Findings from a nationally representative sample. Depression and Anxiety, 28(8), 632–638. 10.1002/da.20852. [DOI] [PubMed] [Google Scholar]
- Font SA, & Maguire-Jack K (2016). Pathways from childhood abuse and other adversities to adult health risks: The role of adult socioeconomic conditions. Child Abuse & Neglect, 51, 390–399. 10.1016/j.chiabu.2015.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford ES, Anda RF, Edwards VJ, Perry GS, Zhao G, Li C, & Croft JB (2011). Adverse childhood experiences and smoking status in five states. Preventive Medicine, 53(3), 188–193. 10.1016/j.ypmed.2011.06.015. [DOI] [PubMed] [Google Scholar]
- Fortson BL, Klevens J, Merrick MT, Gilbert LK, & Alexander SP (2016). Preventing child abuse and neglect: A technical package for policy, norm, and programmatic activities. [Google Scholar]
- Francis MM, Nikulina V, & Widom CS (2015). A prospective examination of the mechanisms linking childhood physical abuse to body mass index in adulthood. Child Maltreatment, 20(3),203–213. 10.1177/1077559514568892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman EM, Karlamangla AS, Gruenewald TL, Koretz B, & Seeman TE (2015). Early life adversity and adult biological risk profiles. Psychosomatic Medicine, 77(2), 176–185. 10.1097/PSY.0000000000000147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman EM, Montez JK, Sheehan CM, Guenewald TL, & Seeman TE (2015). Childhood adversities and adult cardiometabolic health: Does the quantity, timing, and type of adversity matter? Journal of Aging and Health, 27(8), 1311–1338. 10.1177/0898264315580122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman MS, Marshal MP, Stall R, Cheong J, & Wright ER (2008). Gay-related development, early abuse and adult health outcomes among gay males. AIDS and Behavior, 12(6), 891–902. 10.1007/s10461-007-9319-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller-Thomson E, & Brennenstuhl S (2009). Making a link between childhood physical abuse and cancer: Results from a regional representative survey. Cancer, 115(14), 3341–3350. 10.1002/cncr.24372. [DOI] [PubMed] [Google Scholar]
- Fuller-Thomson E, Filippelli J, & Lue-Crisostomo CA (2013). Gender-specific association between childhood adversities and smoking in adulthood: Findings from a population-based study. Public Health, 127(5), 449–460. 10.1016/j.puhe.2013.01.006. [DOI] [PubMed] [Google Scholar]
- Garner AS, Shonkoff JP, Committee on Psychosocial Aspects of, C, Family, H, Committee on Early Childhood, A, Dependent, C, … Behavioral, P (2012). Early childhood adversity, toxic stress, and the role of the pediatrician: Translating developmental science into lifelong health. Pediatrics, 129(1), e224–e231. 10.1542/peds.2011-2662. [DOI] [PubMed] [Google Scholar]
- Gilbert LK, Breiding MJ, Merrick MT, Thompson WW, Ford DC, Dhingra SS, & Parks SE (2015). Childhood adversity and adult chronic disease: An update from ten states and the District of Columbia, 2010. American Journal of Preventive Medicine, 48(3), 345–349. 10.1016/j.amepre.2014.09.006. [DOI] [PubMed] [Google Scholar]
- Gilmore AK, Koo KH, Nguyen HV, Granato HF, Hughes TL, & Kaysen D (2014). Sexual assault, drinking norms, and drinking behavior among a national sample of lesbian and bisexual women. Addictive Behaviors, 39(3), 630–636. 10.1016/j.addbeh.2013.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gjelsvik A, Dumont DM, & Nunn A (2013). Incarceration of a household member and Hispanic health disparities: Childhood exposure and adult chronic disease risk behaviors. Preventing Chronic Disease, 10, E69 10.5888/pcd10.120281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein AL, Flett GL, & Wekerle C (2010). Child maltreatment, alcohol use and drinking consequences among male and female college students: An examination of drinking motives as mediators. Addictive Behaviors, 35(6), 636–639. 10.1016/j.addbeh.2010.02.002. [DOI] [PubMed] [Google Scholar]
- Gouin JP, Glaser R, Malarkey WB, Beversdorf D, & Kiecolt-Glaser JK (2012). Childhood abuse and inflammatory responses to daily stressors. Annals of Behavioral Medicine, 44(2), 287–292. 10.1007/s12160-012-9386-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grady D, Gebretsadik T, Kerlikowske K, Ernster V, & Petitti D (1995). Hormone replacement therapy and endometrial cancer risk: A meta-analysis. Obstetrics and Gynecology, 85(2), 304–313. 10.1016/0029-7844(94)00383-O. [DOI] [PubMed] [Google Scholar]
- Grayson CE, & Nolen-Hoeksema S (2005). Motives to drink as mediators between childhood sexual assault and alcohol problems in adult women. Journal of Traumatic Stress, 18(2), 137–145. 10.1002/jts.20021. [DOI] [PubMed] [Google Scholar]
- Greenfield EA, & Marks NF (2009). Violence from parents in childhood and obesity in adulthood: Using food in response to stress as a mediator of risk. Social Science & Medicine, 68(5), 791–798. 10.1016/j.socscimed.2008.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Brody M, Toth C, Burke-Martindale CH, & Rothschild BS (2005). Childhood maltreatment in extremely obese male and female bariatric surgery candidates. Obesity Research, 13(1), 123–130. 10.1038/oby.2005.16. [DOI] [PubMed] [Google Scholar]
- Grulich AE, van Leeuwen MT, Falster MO, & Vajdic CM (2007). Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: A meta-analysis. Lancet, 370(9581), 59–67. 10.1016/S0140-6736(07)61050-2. [DOI] [PubMed] [Google Scholar]
- Gustafson TB, & Sarwer DB (2004). Childhood sexual abuse and obesity. Obesity Reviews, 5(3), 129–135. 10.1111/j.1467-789X.2004.00145.x. [DOI] [PubMed] [Google Scholar]
- Hartwell KJ, Moran-Santa Maria MM, Twal WO, Shaftman S, DeSantis SM, McRae-Clark AL, & Brady KT (2013). Association of elevated cytokines with childhood adversity in a sample of healthy adults. Journal of Psychiatric Research, 47(5), 604–610. 10.1016/j.jpsychires.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson BE, Ross R, & Bernstein L (1988). Estrogens as a cause of human cancer: The Richard and Hinda Rosenthal Foundation award lecture. Cancer Research, 48(2), 246–253. [PubMed] [Google Scholar]
- Herbst AL, Ulfelder H, & Poskanzer DC (1971). Adenocarcinoma of the vagina. Association of maternal stilbestrol therapy with tumor appearance in young women. The New England Journal of Medicine, 284(15), 878–881. 10.1056/NEJM197104222841604. [DOI] [PubMed] [Google Scholar]
- Hillis SD, Anda RF, Felitti VJ, & Marchbanks PA (2001). Adverse childhood experiences and sexual risk behaviors in women: A retrospective cohort study. Family Planning Perspectives, 33(5), 206–211. [PubMed] [Google Scholar]
- Hillis SD, Anda RF, Felitti VJ, Nordenberg D, & Marchbanks PA (2000). Adverse childhood experiences and sexually transmitted diseases in men and women: A retrospective study. Pediatrics, 106(1), E11. [DOI] [PubMed] [Google Scholar]
- Hodge F, & Nandy K (2011). Factors associated with American Indian cigarette smoking in rural settings. International Journal of Environmental Research and Public Health, 8 (4), 944–954. 10.3390/ijerph8040944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodge F, Stemmler MS, & Nandy K (2014). Association between obesity and history of abuse among American Indians in rural California. Journal of Obesity & Weight Loss Theraphy, 4 10.4172/2165-7904.1000208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman DM, Ports KA, Buchanan ND, Hawkins NA, Merrick MT, Metzler M, & Trivers KF (2016). The association between adverse childhood experiences and risk of cancer in adulthood: A systematic review of the literature. Pediatrics, 138(Suppl. 1), S81–S91. 10.1542/peds.2015-4268L. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horan JM, & Widom CS (2015). Does age of onset of risk behaviors mediate the relationship between child abuse and neglect and outcomes in middle adulthood? Journal of Youth and Adolescence, 44(3), 670–682. 10.1007/s10964-014-0161-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hostinar CE, Lachman ME, Mroczek DK, Seeman TE, & Miller GE (2015). Additive contributions of childhood adversity and recent stressors to inflammation at midlife: Findings from the MIDUS study. Developmental Psychology, 51(11), 1630–1644. 10.1037/dev0000049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh CC, Trichopoulos D, Katsouyanni K, & Yuasa S (1990). Age at menarche, age at menopause, height and obesity as risk factors for breast cancer: Associations and interactions in an international case–control study. International Journal of Cancer, 46 (5), 796–800. [DOI] [PubMed] [Google Scholar]
- Hughes T, McCabe SE, Wilsnack SC, West BT, & Boyd CJ (2010). Victimization and substance use disorders in a national sample of heterosexual and sexual minority women and men. Addiction, 105(12), 2130–2140. 10.1111/j.1360-0443.2010.03088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes TL, Johnson TP, Wilsnack SC, & Szalacha LA (2007). Childhood risk factors for alcohol abuse and psychological distress among adult lesbians. Child Abuse & Neglect, 31(7), 769–789. 10.1016/j.chiabu.2006.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes TL, Szalacha LA, Johnson TP, Kinnison KE, Wilsnack SC, & Cho Y (2010). Sexual victimization and hazardous drinking among heterosexual and sexual minority women. Addictive Behaviors, 35(12), 1152–1156. 10.1016/j.addbeh.2010.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland ME, Alkhalaf AM, & Whalley B (2013). Beating and insulting children as a risk for adult cancer, cardiac disease and asthma. Journal of Behavioral Medicine, 36(6), 632–640. 10.1007/s10865-012-9457-6. [DOI] [PubMed] [Google Scholar]
- IARC Working Group on the Evaluation of Carcinogenic Risk to Humans (2012a). Arsenic and arsenic compounds. (100C). Retrieved from http://monographs.iarc.fr/ENG/Monographs/vol100C/mono100C-6.pdf.
- IARC Working Group on the Evaluation of Carcinogenic Risk to Humans (2012b). Asbestos (chrysotile, amosite, crocidolite, tremolite, actinolite and anthophylite). Retrieved from http://monographs.iarc.fr/ENG/Monographs/vol100C/mono100C-11.pdf.
- IARC Working Group on the Evaluation of Carcinogenic Risk to Humans (2012c). Consumption of alcoholic beverages. Retrieved from http://monographs.iarc.fr/ENG/Monographs/vol100E/mono100E-11.pdf.
- IARCWorking Group on the Evaluation of Carcinogenic Risk to Humans (2012d). Secondhand tobacco smoke. Retrieved from http://monographs.iarc.fr/ENG/Monographs/vol100E/mono100E-7.pdf.
- IARC Working Group on the Evaluation of Carcinogenic Risk to Humans (2012e). Soot, as found in occupational exposure of chimney-sweeps. Retrieved from https://monographs.iarc.fr/ENG/Monographs/vol100F/mono100F-21.pdf.
- IARC Working Group on the Evaluation of Carcinogenic Risk to Humans (2012f). Tobacco smoking. Retrieved from http://monographs.iarc.fr/ENG/Monographs/vol100E/mono100E-6.pdf.
- International Agency for Research on Cancer (2016). IARC identifies eight additional cancer sites linked to overweight and obesity. Retrieved from http://www.iarc.fr/en/media-centre/pr/2016/pdfs/pr247_E.pdf (Press release). [PubMed]
- Jenkins MB, Agrawal A, Lynskey MT, Nelson EC, Madden PA, Bucholz KK, & Heath AC (2011). Correlates of alcohol abuse/dependence in early-onset alcoholusing women. The American Journal on Addictions, 20(5), 429–434. 10.1111/j.1521-0391.2011.00151.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jessup MA, Dibble SL, & Cooper BA (2012). Smoking and behavioral health of women. Journal of Women’s Health (2002), 21(7), 783–791. 10.1089/jwh.2011.2886. [DOI] [PubMed] [Google Scholar]
- Joung KE, Park KH, Zaichenko L, Sahin-Efe A, Thakkar B, Brinkoetter M, … Mantzoros CS (2014). Early life adversity is associated with elevated levels of circulating leptin, irisin, and decreased levels of adiponectin in midlife adults. The Journal of Clinical Endocrinology and Metabolism, 99(6), E1055–E1060. 10.1210/jc.2013-3669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly-Irving M, Lepage B, Dedieu D, Lacey R, Cable N, Bartley M, … Delpierre C (2013). Childhood adversity as a risk for cancer: Findings from the 1958 British birth cohort study. BMC Public Health, 13, 767 10.1186/1471-2458-13-767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelsey JL, Gammon MD, & John EM (1993). Reproductive factors and breast cancer. Epidemiologic Reviews, 15(1), 36–47. [DOI] [PubMed] [Google Scholar]
- Keyes KM, McLaughlin KA, Koenen KC, Goldmann E, Uddin M, & Galea S (2012). Child maltreatment increases sensitivity to adverse social contexts: Neighborhood physical disorder and incident binge drinking in Detroit. Drug and Alcohol Dependence, 122(1–2), 77–85. 10.1016/j.drugalcdep.2011.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Gouin JP, Weng NP, Malarkey WB, Beversdorf DQ, & Glaser R (2011). Childhood adversity heightens the impact of later-life caregiving stress on telomere length and inflammation. Psychosomatic Medicine, 73(1), 16–22. 10.1097/PSY.0b013e31820573b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, & Williams S (2009). Linking childhood maltreatment to substance use in college students: The mediating role of self-worth contingencies. Journal of Aggression, Maltreatment & Trauma, 18(1), 88–105. 10.1080/10926770802616399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JH, Martins SS, Shmulewitz D, Santaella J, Wall MM, Keyes KM, … Hasin DS (2014). Childhood maltreatment, stressful life events, and alcohol craving in adult drinkers. Alcoholism, Clinical and Experimental Research, 38(7), 2048–2055. 10.1111/acer.12473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klanecky A, McChargue DE, & Bruggeman L (2012). Desire to dissociate: Implications for problematic drinking in college students with childhood or adolescent sexual abuse exposure. The American Journal on Addictions, 21(3), 250–256. 10.1111/j.1521-0391.2012.00228.x. [DOI] [PubMed] [Google Scholar]
- Klanecky AK, Woolman EO, & Becker MM (2015). Child abuse exposure, emotion regulation, and drinking refusal self-efficacy: An analysis of problem drinking in college students. The American Journal of Drug and Alcohol Abuse, 41(2), 188–196. 10.3109/00952990.2014.998365. [DOI] [PubMed] [Google Scholar]
- Kristman-Valente AN, Brown EC, & Herrenkohl TI (2013). Child physical and sexual abuse and cigarette smoking in adolescence and adulthood. The Journal of Adolescent Health, 53(4), 533–538. 10.1016/j.jadohealth.2013.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Flair LN, Reboussin BA, Storr CL, Letourneau E, Green KM, Mojtabai R, … Crum RM (2013). Childhood abuse and neglect and transitions in stages of alcohol involvement among women: A latent transition analysis approach. Drug and Alcohol Dependence, 132(3), 491–498. 10.1016/j.drugalcdep.2013.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson K, & Halfon N (2013). Parental divorce and adult longevity. International Journal of Public Health, 58(1), 89–97. 10.1007/s00038-012-0373-x. [DOI] [PubMed] [Google Scholar]
- Layde PM, Webster LA, Baughman AL, Wingo PA, Rubin GL, & Ory HW (1989). The independent associations of parity, age at first full term pregnancy, and duration of breastfeeding with the risk of breast cancer. Cancer and Steroid Hormone Study Group. Journal of Clinical Epidemiology, 42(10), 963–973. [DOI] [PubMed] [Google Scholar]
- Lehavot K, & Simoni JM (2011). Victimization, smoking, and chronic physical health problems among sexual minority women. Annals of Behavioral Medicine, 42(2), 269–276. 10.1007/s12160-011-9289-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehman BJ, Taylor SE, Kiefe CI, & Seeman TE (2005). Relation of childhood socioeconomic status and family environment to adult metabolic functioning in the CARDIA study. Psychosomatic Medicine, 67(6), 846–854. 10.1097/01.psy.0000188443.48405.eb. [DOI] [PubMed] [Google Scholar]
- Li L, Chassan RA, Bruer EH, Gower BA, & Shelton RC (2015). Childhood maltreatment increases the risk for visceral obesity. Obesity (Silver Spring), 23(8), 1625–1632. 10.1002/oby.21143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lown EA, Nayak MB, Korcha RA, & Greenfield TK (2011). Child physical and sexual abuse: A comprehensive look at alcohol consumption patterns, consequences, and dependence from the National Alcohol Survey. Alcoholism, Clinical and Experimental Research, 35(2), 317–325. 10.1111/j.1530-0277.2010.01347.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu W, Mueser KT, Rosenberg SD, & Jankowski MK (2008). Correlates of adverse childhood experiences among adults with severe mood disorders. Psychiatric Services, 59(9), 1018–1026. 10.1176/appi.ps.59.9.1018. [DOI] [PubMed] [Google Scholar]
- Mason SM, MacLehose RF, Katz-Wise SL, Austin SB, Neumark-Sztainer D, Harlow BL, & Rich-Edwards JW (2015). Childhood abuse victimization, stress-related eating, and weight status in young women. Annals of Epidemiology, 25(10), 760–766 (e762) 10.1016/j.annepidem.2015.06.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews KA, Chang YF, Thurston RC, & Bromberger JT (2014). Child abuse is related to inflammation in mid-life women: Role of obesity. Brain, Behavior, and Immunity, 36, 29–34. 10.1016/j.bbi.2013.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mays N, Roberts E, & Popay J (2001). Synthesising research evidence. Studying the organisation and delivery of health services: Research methods. 220.. [Google Scholar]
- McCarty F, DePadilla L, Elifson K, & Sterk C (2012). Excessive drinking among African American men: Individual and contextual correlates. Journal of Ethnicity in Substance Abuse, 11(2), 113–129. 10.1080/15332640.2012.675227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCauley HL, Blosnich JR, & Dichter ME (2015). Adverse childhood experiences and adult health outcomes among veteran and non-veteran women. Journal of Women’s Health (2002), 24(9), 723–729. 10.1089/jwh.2014.4997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre RS, Soczynska JK, Liauw SS, Woldeyohannes HO, Brietzke E, Nathanson J, … Kennedy SH (2012). The association between childhood adversity and components of metabolic syndrome in adults with mood disorders: Results from the international mood disorders collaborative project. International Journal of Psychiatry in Medicine, 43(2), 165–177. [DOI] [PubMed] [Google Scholar]
- McMillan GP, Hanson T, Bedrick EJ, & Lapham SC (2005). Using the Bivariate Dale Model to jointly estimate predictors of frequency and quantity of alcohol use. Journal of Studies on Alcohol, 66(5), 688–692. [DOI] [PubMed] [Google Scholar]
- Mersky JP, Topitzes J, & Reynolds AJ (2013). Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: A cohort study of an urban, minority sample in the U.S. Child Abuse & Neglect, 37(11), 917–925. 10.1016/j.chiabu.2013.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metzler M, Merrick MT, Klevens J, Ports KA, & Ford DC (2017). Adverse childhood experiences and life opportunities: Shifting the narrative. Children and Youth Services Review, 72, 141–149. 10.1016/j.childyouth.2016.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Midei AJ, Matthews KA, & Bromberger JT (2010). Childhood abuse is associated with adiposity in midlife women: Possible pathways through trait anger and reproductive hormones. Psychosomatic Medicine, 72(2), 215–223. 10.1097/PSY.0b013e3181cb5c24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mimiaga MJ, Noonan E, Donnell D, Safren SA, Koenen KC, Gortmaker S, … Mayer KH (2009). Childhood sexual abuse is highly associated with HIV risk-taking behavior and infection among MSM in the EXPLORE study. Journal of Acquired Immune Deficiency Syndromes, 51(3), 340–348. 10.1097/QAI.0b013e3181a24b38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min MO, Minnes S, Kim H, & Singer LT (2013). Pathways linking childhood maltreatment and adult physical health. Child Abuse & Neglect, 37(6), 361–373. 10.1016/j.chiabu.2012.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mingione CJ, Heffner JL, Blom TJ, & Anthenelli RM (2012). Childhood adversity, serotonin transporter (5-HTTLPR) genotype, and risk for cigarette smoking and nicotine dependence in alcohol dependent adults. Drug and Alcohol Dependence, 123 (1–3), 201–206. 10.1016/j.drugalcdep.2011.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton PM, Mustillo SA, & Ferraro KF (2014). Does childhood misfortune raise the risk of acute myocardial infarction in adulthood? Social Science & Medicine, 104, 133–141. 10.1016/j.socscimed.2013.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton PM, Schafer MH, & Ferraro KF (2012). Does childhood misfortune increase cancer risk in adulthood? Journal of Aging and Health, 24(6), 948–984. 10.1177/0898264312449184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller NE (2003). Cancers caused by infections: Unequal burdens. Cancer Epidemiology, Biomarkers & Prevention, 12(3), 237s. [PubMed] [Google Scholar]
- Najdowski CJ, & Ullman SE (2009). Prospective effects of sexual victimization on PTSD and problem drinking. Addictive Behaviors, 34(11), 965–968. 10.1016/j.addbeh.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute (2015). Risk factors for cancer. Retrieved from https://www.cancer.gov/about-cancer/causes-prevention/risk.
- Nikulina V, & Widom CS (2014). Do race, neglect, and childhood poverty predict physical health in adulthood? A multilevel prospective analysis. Child Abuse & Neglect, 38 (3), 414–424. 10.1016/j.chiabu.2013.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikulina V, Widom CS, & Brzustowicz LM (2012). Child abuse and neglect, MAOA, and mental health outcomes: A prospective examination. Biological Psychiatry, 71 (4), 350–357. 10.1016/j.biopsych.2011.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nimh Multisite HIV/STD Prevention Trial for African American Couples Group (2010). Prevalence of child and adult sexual abuse and risk taking practices among HIV serodiscordant African-American couples. AIDS and Behavior, 14(5), 1032–1044. 10.1007/s10461-010-9700-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noll JG, Zeller MH, Trickett PK, & Putnam FW (2007). Obesity risk for female victims of childhood sexual abuse: A prospective study. Pediatrics, 120(1), e61–e67. 10.1542/peds.2006-3058. [DOI] [PubMed] [Google Scholar]
- NTP (National Toxicology Program) (2016). Report on carcinogens (Fourteenth ed.) Research Triangle Park, NC: U.S. Retrieved from http://ntp.niehs.nih.gov/go/roc14/. [Google Scholar]
- Oberleitner LM, Smith PH, Weinberger AH, Mazure CM, & McKee SA (2015). Impact of exposure to childhood maltreatment on transitions to alcohol dependence in women and men. Child Maltreatment, 20(4), 301–308. 10.1177/1077559515591270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Cleirigh C, Dale SK, Elsesser S, Pantalone DW, Mayer KH, Bradford JB, & Safren SA (2015). Sexual minority specific and related traumatic experiences are associated with increased risk for smoking among gay and bisexual men. Journal of Psychosomatic Research, 78(5), 472–477. 10.1016/j.jpsychores.2015.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park A, Sher KJ, Todorov AA, & Heath AC (2011). Interaction between the DRD4 VNTR polymorphism and proximal and distal environments in alcohol dependence during emerging and young adulthood. Journal of Abnormal Psychology, 120(3), 585–595. 10.1037/a0022648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parkin DM (2006). The global health burden of infection-associated cancers in the year 2002. International Journal of Cancer, 118(12), 3030–3044. 10.1002/ijc.21731. [DOI] [PubMed] [Google Scholar]
- Payne-Sturges D, & Gee GC (2006). National environmental health measures for minority and low-income populations: Tracking social disparities in environmental health. Environmental Research, 102(2), 154–171. 10.1016/j.envres.2006.05.014. [DOI] [PubMed] [Google Scholar]
- Pederson CL, Vanhorn DR, Wilson JF, Martorano LM, Venema JM, & Kennedy SM (2008). Childhood abuse related to nicotine, illicit and prescription drug use by women: Pilot study. Psychological Reports, 103(2), 459–466. 10.2466/pr0.103.2.459-466. [DOI] [PubMed] [Google Scholar]
- Pederson CL, & Wilson JF (2009). Childhood emotional neglect related to posttraumatic stress disorder symptoms and body mass index in adult women 1, 2. Psychological Reports, 105(1), 99–110. 10.2466/pr0.105.1.111-126. [DOI] [PubMed] [Google Scholar]
- Phillips G 2nd, Magnus M, Kuo I, Rawls A, Peterson J, Montanez L, … Greenberg AE (2014). Childhood sexual abuse and HIV-related risks among men who have sex with men in Washington, DC. Archives of Sexual Behavior, 43(4), 771–778. 10.1007/s10508-014-0267-5. [DOI] [PubMed] [Google Scholar]
- Pilowsky DJ, Keyes KM, & Hasin DS (2009). Adverse childhood events and lifetime alcohol dependence. American Journal of Public Health, 99(2), 258–263. 10.2105/AJPH.2008.139006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell DL, & Stewart V (2001). Children. The unwitting target of environmental injustices. Pediatric Clinics of North America, 48(5), 1291–1305. [DOI] [PubMed] [Google Scholar]
- Ramirez JC, & Milan S (2016). Childhood sexual abuse moderates the relationship between obesity and mental health in low-income women. Child Maltreatment, 21(1), 85–89. 10.1177/1077559515611246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Falb KL, & Mimiaga MJ (2011). Early life traumatic stressors and the mediating role of PTSD in incident HIV infection among US men, comparisons by sexual orientation and race/ethnicity: Results from the NESARC, 2004–2005. Journal of Acquired Immune Deficiency Syndromes, 57(4), 340–350. 10.1097/QAI.0b013e31821d36b4. [DOI] [PubMed] [Google Scholar]
- Richardson AS, Dietz WH, & Gordon-Larsen P (2014). The association between childhood sexual and physical abuse with incident adult severe obesity across 13 years of the National Longitudinal Study of Adolescent Health. Pediatric Obesity, 9(5), 351–361. 10.1111/j.2047-6310.2013.00196.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich-Edwards JW, Spiegelman D, Lividoti Hibert EN, Jun HJ, Todd TJ, Kawachi I, & Wright RJ (2010). Abuse in childhood and adolescence as a predictor of type 2 diabetes in adult women. American Journal of Preventive Medicine, 39(6), 529–536. 10.1016/j.amepre.2010.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley EH, Wright RJ, Jun HJ, Hibert EN, & Rich-Edwards JW (2010). Hypertension in adult survivors of child abuse: Observations from the nurses' health study II. Journal of Epidemiology and Community Health, 64(5), 413–418. 10.1136/jech.2009.095109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde P, Ichikawa L, Simon GE, Ludman EJ, Linde JA, Jeffery RW, & Operskalski BH (2008). Associations of child sexual and physical abuse with obesity and depression in middle-aged women. Child Abuse & Neglect, 32(9), 878–887. 10.1016/j.chiabu.2007.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rooks C, Veledar E, Goldberg J, Bremner JD, & Vaccarino V (2012). Early trauma and inflammation: Role of familial factors in a study of twins. Psychosomatic Medicine, 74 (2), 146–152. 10.1097/PSY.0b013e318240a7d8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum A, Hartley S, & Holder C (2011). Analysis of diesel particulate matter health risk disparities in selected US harbor areas. American Journal of Public Health, 101 (Suppl. 1), S217–S223. 10.2105/AJPH.2011.300190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg SD, Lu W, Mueser KT, Jankowski MK, & Cournos F (2007). Correlates of adverse childhood events among adults with schizophrenia spectrum disorders. Psychiatric Services, 58(2), 245–253. 10.1176/ps.2007.58.2.245. [DOI] [PubMed] [Google Scholar]
- Sacco KA, Head CA, Vessicchio JC, Easton CJ, Prigerson HG, & George TP (2007). Adverse childhood experiences, smoking and mental illness in adulthood: A preliminary study. Annals of Clinical Psychiatry, 19(2), 89–97. 10.1080/10401230701334762. [DOI] [PubMed] [Google Scholar]
- Salem BE, Nyamathi A, Keenan C, Zhang S, Marlow E, Khalilifard F,… Marfisee M (2013). Correlates of risky alcohol and methamphetamine use among currently homeless male parolees. Journal of Addictive Diseases, 32(4), 365–376. 10.1080/10550887.2013.849973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sartor CE, McCutcheon VV, Nelson EC, Duncan AE, Bucholz KK, & Heath AC (2012). Investigating the association between childhood sexual abuse and alcohol use disorders in women: Does it matter how we ask about sexual abuse? Journal of Studies on Alcohol and Drugs, 73(5), 740–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sartor CE, Wang Z, Xu K, Kranzler HR, & Gelernter J (2014). The joint effects of ADH1B variants and childhood adversity on alcohol related phenotypes in African-American and European-American women and men. Alcoholism, Clinical and Experimental Research, 38(12), 2907–2914. 10.1111/acer.12572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schairer C, Lubin J, Troisi R, Sturgeon S, Brinton L, & Hoover R (2000). Menopausal estrogen and estrogen-progestin replacement therapy and breast cancer risk. JAMA, 283(4), 485–491. [DOI] [PubMed] [Google Scholar]
- Schellekens AF, Franke B, Ellenbroek B, Cools A, de Jong CA, Buitelaar JK, & Verkes RJ (2013). COMT Val158Met modulates the effect of childhood adverse experiences on the risk of alcohol dependence. Addiction Biology, 18(2), 344–356. 10.1111/j.1369-1600.2012.00438.x. [DOI] [PubMed] [Google Scholar]
- Schofield TJ, Lee RD, & Merrick MT (2013). Safe, stable, nurturing relationships as a moderator of intergenerational continuity of child maltreatment: A meta-analysis. The Journal of Adolescent Health, 53(4 Suppl), S32–S38. 10.1016/j.jadohealth.2013.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrepf A, Clevenger L, Christensen D, DeGeest K, Bender D, Ahmed A, & Lutgendorf SK (2013). Cortisol and inflammatory processes in ovarian cancer patients following primary treatment: Relationships with depression, fatigue, and disability. Brain, Behavior, and Immunity, 30(Suppl), S126–S134. 10.1016/j.bbi.2012.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrepf A, Markon K, & Lutgendorf SK (2014). From childhood trauma to elevated C-reactive protein in adulthood: The role of anxiety and emotional eating. Psychosomatic Medicine, 76(5), 327–336. 10.1097/PSY.0000000000000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwandt ML, Heilig M, Hommer DW, George DT, & Ramchandani VA (2013). Childhood trauma exposure and alcohol dependence severity in adulthood: Mediation by emotional abuse severity and neuroticism. Alcoholism, Clinical and Experimental Research, 37(6), 984–992. 10.1111/acer.12053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedlak AJ, Mettenburg J, Basena M, Petta I, McPherson K, Greene A, & Li S (2010). Fourth national incidence study of child abuse and neglect (NIS-4): Report to congress, executive summary. (Retrieved from Washington, DC). [Google Scholar]
- Shin SH, Hassamal S, & Groves LP (2015). Examining the role of psychological distress in linking childhood maltreatment and alcohol use in young adulthood. The American Journal on Addictions, 24(7), 628–636. 10.1111/ajad.12276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin SH, Lee S, Jeon SM, & Wills TA (2015). Childhood emotional abuse, negative emotion-driven impulsivity, and alcohol use in young adulthood. Child Abuse & Neglect, 50, 94–103. 10.1016/j.chiabu.2015.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinozaki G, Romanowicz M, Kung S, Rundell J, & Mrazek D (2012). Investigation of serotonin transporter gene (SLC6A4) by child abuse history interaction with body mass index and diabetes mellitus of White female depressed psychiatric inpatients. Psychiatric Genetics, 22(3), 109–114. 10.1097/YPG.0b013e32834f3542. [DOI] [PubMed] [Google Scholar]
- Shonkoff JP (2016). Capitalizing on advances in science to reduce the health consequences of early childhood adversity. JAMA Pediatrics, 170(10), 1003–1007. 10.1001/jamapediatrics.2016.1559. [DOI] [PubMed] [Google Scholar]
- Shonkoff JP, Garner AS, Committee on Psychosocial Aspects of, C, Family, H, Committee on Early Childhood, A, Dependent, C, … Behavioral, P (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129(1), e232–e246. 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- Skinner ML, Kristman-Valente AN, & Herrenkohl TI (2016). Adult binge drinking: Childhood sexual abuse, gender and the role of adolescent alcohol-related experiences. Alcohol and Alcoholism, 51(2), 136–141. 10.1093/alcalc/agv093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N, Dutra LM, Williams DR, Mujahid MS, Lewis TT, Bennett GG, … Albert MA (2012). Psychosocial stressors and cigarette smoking among African American adults in midlife. Nicotine & Tobacco Research, 14(10), 1161–1169. 10.1093/ntr/nts011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N, Lewis TT, Gruenewald TL, Mujahid MS, Ryff CD, Albert MA, & Williams DR (2010). Early life adversity and inflammation in African Americans and whites in the midlife in the United States survey. Psychosomatic Medicine, 72 (7), 694–701. 10.1097/PSY.0b013e3181e9c16f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N, Loucks EB, Appleton AA, Kawachi I, Kubzansky LD, Non AL, … Gilman SE (2015). Early origins of inflammation: An examination of prenatal and childhood social adversity in a prospective cohort study. Psychoneuroendocrinology, 51, 403–413. 10.1016/j.psyneuen.2014.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N, McLaughlin KA, Dunn EC, & Koenen KC (2013). Childhood adversity and cell-mediated immunity in young adulthood: Does type and timing matter? Brain, Behavior, and Immunity, 28, 63–71. 10.1016/j.bbi.2012.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N, Non A, Williams DR, Roberts AL, & Albert MA (2014). Childhood adversity, adult neighborhood context, and cumulative biological risk for chronic diseases in adulthood. Psychosomatic Medicine, 76(7), 481–489. 10.1097/PSY.0000000000000081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith AK, Conneely KN, Kilaru V, Mercer KB, Weiss TE, Bradley B, … Ressler KJ (2011). Differential immune system DNA methylation and cytokine regulation in post-traumatic stress disorder. American Journal of Medical Genetics. Part B, Neuropsychiatric Genetics, 156B(6), 700–708. 10.1002/ajmg.b.31212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DC, Prentice R, Thompson DJ, & Herrmann WL (1975). Association of exogenous estrogen and endometrial carcinoma. The New England Journal of Medicine, 293 (23), 1164–1167. 10.1056/NEJM197512042932302. [DOI] [PubMed] [Google Scholar]
- Smith HA, Markovic N, Danielson ME, Matthews A, Youk A, Talbott EO, … Hughes T (2010). Sexual abuse, sexual orientation, and obesity in women. Journal of Women's Health (2002), 19(8), 1525–1532. 10.1089/jwh.2009.1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder SM, & Merritt DH (2016). The effect of childhood supervisory neglect on emerging adults' drinking. Substance Use & Misuse, 51(1), 1–14. 10.3109/10826084.2015.1073321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spann SJ, Gillespie CF, Davis JS, Brown A, Schwartz A, Wingo A, … Ressler KJ (2014). The association between childhood trauma and lipid levels in an adult low-income, minority population. General Hospital Psychiatry, 36(2), 150–155. 10.1016/j.genhosppsych.2013.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spratt EG, B., S., Yeatts SD, Simpson AN, McRae-Clark A, Moran-Santa Maria MM, … Brady KT (2009). Relationship between child abuse and adult smoking. International Journal of Psychiatry in Medicine, 39(4), 417–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoltenborgh M, Bakermans-Kranenburg MJ, & van Ijzendoorn MH (2013). The neglect of child neglect: A meta-analytic review of the prevalence of neglect. Social Psychiatry and Psychiatric Epidemiology, 48(3), 345–355. 10.1007/s00127-012-0549-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strine TW, Dube SR, Edwards VJ, Prehn AW, Rasmussen S, Wagenfeld M, … Croft JB (2012). Associations between adverse childhood experiences, psychological distress, and adult alcohol problems. American Journal of Health Behavior, 36(3), 408–423. 10.5993/AJHB.36.3.11. [DOI] [PubMed] [Google Scholar]
- Su S, Wang X, Pollock JS, Treiber FA, Xu X, Snieder H, … Harshfield GA (2015). Adverse childhood experiences and blood pressure trajectories from childhood to young adulthood: The Georgia stress and heart study. Circulation, 131(19), 1674–1681. 10.1161/CIRCULATIONAHA.114.013104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taha F, Galea S, Hien D, & Goodwin RD (2014). Childhood maltreatment and the persistence of smoking: A longitudinal study among adults in the US. Child Abuse & Neglect, 38(12), 1995–2006. 10.1016/j.chiabu.2014.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson RG, & Hasin DS (2011). Cigarette, marijuana, and alcohol use and prior drug treatment among newly homeless young adults in New York City: Relationship to a history of foster care. Drug and Alcohol Dependence, 117(1), 66–69. 10.1016/j.drugalcdep.2010.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tietjen GE, Khubchandani J, Herial NA, & Shah K (2012). Adverse childhood experiences are associated with migraine and vascular biomarkers. Headache, 52(6), 920–929. 10.1111/j.1526-4610.2012.02165.x. [DOI] [PubMed] [Google Scholar]
- Topitzes J, Mersky JP, & Reynolds AJ (2010). Child maltreatment and adult cigarette smoking: A long-term developmental model. Journal of Pediatric Psychology, 35(5), 484–498. 10.1093/jpepsy/jsp119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trent L, Stander V, Thomsen C, & Merrill L (2007). Alcohol abuse among U.S. Navy recruits who were maltreated in childhood. Alcohol and Alcoholism, 42(4), 370–375. 10.1093/alcalc/agm036. [DOI] [PubMed] [Google Scholar]
- Tyler KA, Schmitz RM, & Adams SA (2015). Alcohol expectancy, drinking behavior, and sexual victimization among female and male college students. Journal of Interpersonal Violence. 10.1177/0886260515591280. [DOI] [PubMed] [Google Scholar]
- U.S. Cancer Statistics Working Group (2016). United States cancer statistics: 1999–2013 incidence and mortality web-based report. (Retrieved from Atlanta). [Google Scholar]
- U.S. Department of Health and Human Services (2010). How tobacco smoke causes disease: The biology and behavioral basis for smoking-attributable disease: A report of the surgeon general. (Atlanta, GA: ). [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (2014). The surgeon General's call to action to prevent skin cancer. Retrieved from https://www.surgeongeneral.gov/library/calls/prevent-skin-cancer/.
- Ulibarri MD, Ulloa EC, & Salazar M (2015). Associations between mental health, substance use, and sexual abuse experiences among Latinas. Journal of Child Sexual Abuse, 24(1), 35–54. 10.1080/10538712.2015.976303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullman SE, & Sigurvinsdottir R (2015). Intimate partner violence and drinking among victims of adult sexual assault. Journal of Aggression, Maltreatment & Trauma, 24(2), 117–130. 10.1080/10926771.2015.996312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vander Weg MW (2011). Adverse childhood experiences and cigarette smoking: The 2009 Arkansas and Louisiana behavioral risk factor surveillance systems. Nicotine & Tobacco Research, 13(7), 616–622. 10.1093/ntr/ntr023. [DOI] [PubMed] [Google Scholar]
- Waldrop AE, Ana EJ, Saladin ME, McRae AL, & Brady KT (2007). Differences in early onset alcohol use and heavy drinking among persons with childhood and adulthood trauma. The American Journal on Addictions, 16(6), 439–442. 10.1080/10550490701643484. [DOI] [PubMed] [Google Scholar]
- Walsh EG, & Cawthon SW (2014). The mediating role of depressive symptoms in the relationship between adverse childhood experiences and smoking. Addictive Behaviors, 39(10), 1471–1476. 10.1016/j.addbeh.2014.05.020. [DOI] [PubMed] [Google Scholar]
- Walsh K, Latzman NE, & Latzman RD (2014). Pathway from child sexual and physical abuse to risky sex among emerging adults: The role of trauma-related intrusions and alcohol problems. The Journal of Adolescent Health, 54(4), 442–448. 10.1016/j.jadohealth.2013.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren GW, Alberg AJ, Kraft AS, & Cummings KM (2014). The 2014 surgeon general's report: “The health consequences of smoking—50 years of progress”: A paradigm shift in cancer care. Cancer, 120(13), 1914–1916. 10.1002/cncr.28695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickrama KA, Kwon JA, Oshri A, & Lee TK (2014). Early socioeconomic adversity and young adult physical illness: The role of body mass index and depressive symptoms. The Journal of Adolescent Health, 55(4), 556–563. 10.1016/j.jadohealth.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widom CS, Czaja SJ, Bentley T, & Johnson MS (2012). A prospective investigation of physical health outcomes in abused and neglected children: New findings from a 30-year follow-up. American Journal of Public Health, 102(6), 1135–1144. 10.2105/AJPH.2011.300636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson HW, & Widom CS (2008). An examination of risky sexual behavior and HIV in victims of child abuse and neglect: A 30-year follow-up. Health Psychology, 27(2), 149–158. 10.1037/0278-6133.27.2.149. [DOI] [PubMed] [Google Scholar]
- Wu NS, Schairer LC, Dellor E, & Grella C (2010). Childhood trauma and health outcomes in adults with comorbid substance abuse and mental health disorders. Addictive Behaviors, 35(1), 68–71. 10.1016/j.addbeh.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie P, Kranzler HR, Zhang H, Oslin D, Anton RF, Farrer LA, & Gelernter J (2012). Childhood adversity increases risk for nicotine dependence and interacts with alpha5 nicotinic acetylcholine receptor genotype specifically in males. Neuropsychopharmacology, 37(3), 669–676. 10.1038/npp.2011.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yager JD, & Davidson NE (2006). Estrogen carcinogenesis in breast cancer. The New England Journal of Medicine, 354(3), 270–282. 10.1056/NEJMra050776. [DOI] [PubMed] [Google Scholar]
- Yeoman K, Safranek T, Buss B, Cadwell BL, & Mannino D (2013). Adverse childhood experiences and adult smoking, Nebraska, 2011. Preventing Chronic Disease, 10, E159 10.5888/pcd10.130009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young SY, Hansen CJ, Gibson RL, & Ryan MA (2006). Risky alcohol use, age at onset of drinking, and adverse childhood experiences in young men entering the US Marine Corps. Archives of Pediatrics & Adolescent Medicine, 160(12), 1207–1214. 10.1001/archpedi.160.12.1207. [DOI] [PubMed] [Google Scholar]
- Young-Wolff KC, Kendler KS, Ericson ML, & Prescott CA (2011). Accounting for the association between childhood maltreatment and alcohol-use disorders in males: A twin study. Psychological Medicine, 41(1), 59–70. 10.1017/S0033291710000425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan NP, Duran BM, Walters KL, Pearson CR, & Evans-Campbell TA (2014). Alcohol misuse and associations with childhood maltreatment and out-of-home placement among urban two-spirit American Indian and Alaska Native people. International Journal of Environmental Research and Public Health, 11(10), 10461–10479. 10.3390/ijerph111010461. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.