Abstract
Objective:
Chronic pain is a significant health problem that is increasing in prevalence, and advances in treatment are needed.
Methods:
We briefly review the leading evidence-based psychological therapies for chronic pain—cognitive-behavioral and acceptance / mindfulness-based therapies—and examine several limitations and missing perspectives of these approaches. We review six lesser-known interventions that address these limitations, and we describe our integrative model for psychological assessment and treatment of centralized pain. We present a typical patient and describe how we apply this approach, along with challenges to its implementation and possible solutions to these challenges.
Results:
Greater pain treatment efficacy may be possible if clinicians: a) distinguish patients with primarily centralized (i.e., somatoform or nociplastic) pain from those with primarily peripheral (nociceptive, inflammatory, or neuropathic) pain; b) acknowledge the capacity of the brain not only to modulate pain but also generate as well as attenuate or eliminate centralized pain; c) consider the powerful role that adverse life experiences and psychological conflicts play in centralized pain; and d) integrate emotional processing and interpersonal changes into treatment. Our integrative treatment involves delivering a progression of interventions, as needed, to achieve pain reduction: tailored pain neuroscience education, cognitive and mindfulness skills to decrease the pain danger alarm mechanism, behavioral engagement in avoided painful and other feared activities, emotional awareness and expression to reverse emotional avoidance and overcome trauma or psychological conflict, and adaptive communication to decrease interpersonal stress.
Conclusions:
This integrative assessment and treatment model has the potential to substantially reduce and sometimes eliminate centralized pain by changing the cognitive, behavioral, emotional, and interpersonal processes that trigger and maintain centralized pain.
Keywords: Chronic pain, centralized pain, psychological treatment, psychotherapy, emotional awareness and expression, clinical case
I. Introduction of a Typical Patient
Co-author HS saw Mr. A. (a pseudonym), a middle-aged man who, seven years earlier, developed low back pain while exercising, although there was no apparent injury. The pain was initially intermittent but worsened over time, becoming almost constant in the left para-spinal lumbar region, but sometimes on the right side, and occasionally radiating to the left buttock. There was no neurological impairment on examination, and an electromyogram was normal, but magnetic resonance imaging (MRI) showed evidence of degenerative disc disease and a moderate-sized disc bulge at L4–5. Following unsuccessful physical therapy, he received a series of treatments—injections (epidural, Botox, and piriformis), a TENS unit, medications (duloxetine, gabapentin, and oxycodone), and acupuncture—all with little benefit. He then had a L4–5 fusion and later, an SI joint fusion; however, he continued to have significant pain. A few years later, neck pain began, described as constant and dull in nature, which increased over the day. A neck MRI revealed facet degeneration, disc space narrowing, and a small disc bulge at C5–6. A neurosurgeon recommended epidural injections, which Mr. A declined. On a recent vacation, however, Mr. A. had no back or neck pain for several days.
Mr. A. denied adverse childhood events, although his parents had high expectations of him, and he described himself as a sensitive child who worried that he was not good enough. He was often anxious and had stomach aches before school presentations or when he feared disappointing his parents, particularly his father. He first experienced chronic pain as a young man after beginning his first real job. At that time, he had gradual onset pain in his left buttock with radiation to the posterior thigh. There were no neurological findings, and the pain resolved after several months. At the same time, he had tension headaches on most days, but these resolved after several years. At the time of onset of the low back pain, there was upheaval in his workplace, resulting in an increased workload and fear of job loss, which was accompanied by onset of the current episode of low back pain. Over his life course, he has experienced occasional abdominal discomfort, which increases in stressful situations.
II. Definition and Epidemiology of Chronic Pain
According to the International Association for the Study of Pain, pain is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage” (1). Two noteworthy aspects of this definition, as we emphasize below, are the “emotional” aspect of pain and the “potential” of—rather than “actual”—tissue damage.
The various Diagnostic and Statistical Manuals have included diagnoses for chronic pain, but they have struggled with nosology and nomenclature. DSM-IV (2) listed “pain disorder” under somatoform disorders and required clinicians to determine the relative contributions of psychological versus medical conditions to the pain—a task that many scholars and clinicians found problematic, but that we consider valuable, as discussed below. DSM-IV also required differentiating somatoform pain disorder from mood and anxiety disorders, which is a problematic goal given the complex relations between pain and emotion (3). DSM-5 (4) replaced somatoform pain disorder with “somatic symptom disorder with predominant pain,” which applies to people experiencing “distressing or disruptive” pain—that is, excessive thoughts or anxiety about, or time devoted to the pain. We have concerns about the shift from diagnosing chronic pain based on etiologic mechanisms, to viewing patients’ cognitions, emotions, and behaviors as only correlates or consequences of pain. As we argue below, such psychological factors not only result from pain, but also contribute substantially to chronic pain—especially the subtype of “centralized” pain—and ignoring such contributions limits treatment options and efficacy.
Despite the lack of diagnostic consensus, clinicians and patients readily recognize chronic pain: up to one-third of American adults report pain that is present on most days for at least 3 months (5, 6). Moreover, there are substantial costs of chronic pain—depression, disability, relationship disruption, opioid dependence, and even death (7, 8). Although patients often seek and obtain pharmacological, procedural (e.g., injections), or surgical interventions, disappointment with the results, costs, and side effects is common (9). The need for effective psychological treatments is clear.
III. The Leading Behavioral and Psychological Therapies for Chronic Pain
For the purpose of this article, we define psychological therapies for chronic pain as interventions that: a) are provided by therapists directly to patients, b) attempt to change patients’ thoughts, feelings, behaviors, or relationships, and c) have the goal of reducing one or more of the three core chronic pain outcomes: pain severity, pain-related functional impairment, and pain-related mood problems. Psychological therapies for chronic pain vary in their extent of empirical support, inclusion in practice guidelines, and use in clinical settings. Here, we briefly describe the conceptual models and techniques of the two most widely recommended and practiced evidence-based chronic pain therapies in the United States.
Cognitive-behavioral therapy (CBT).
This approach has been tested and supported extensively (10, 11) and is commonly implemented in pain care settings (12). CBT views pain as a chronic health problem, unlikely to remit, but manageable if patients learn skills to change maladaptive cognitive and behavioral processes. In most CBT approaches, patients are presented a conceptual model (e.g., the gate-control model), which helps them understand that changing their behavior, cognitions, and emotions can down-modulate bodily pain and improve functioning and mood. During sessions, patients are taught various self-management skills such as reducing physiological arousal through relaxation training or biofeedback, decreasing pain catastrophizing through cognitive reappraisal, improving mood by engaging in pleasant activities, pacing activities to avoid pain flares and fatigue, and problem-solving to reduce stress. Additional components such as sleep hygiene to improve sleep quality and communication skills to reduce stressful interactions may be included. Patients are given structured homework to practice the skills and implement them in daily life.
Acceptance and mindfulness-based therapies.
There is much recent interest in acceptance and mindfulness-based approaches to chronic pain—a broad category that includes acceptance and commitment therapy (ACT) and mindfulness-focused approaches, such as mindfulness-based stress reduction (13). These approaches encourage the acceptance of one’s immediate experience, including one’s pain, rather than trying to change, control, or manage it. Acceptance is facilitated by developing mindfulness through meditation and other techniques, and helps patients reduce reactivity and rumination by becoming nonjudgmental observers of their sensations, thoughts, and feelings. ACT is conceptually and technically comprehensive, including not only mindfulness training but more broadly striving for psychological flexibility by “defusing” cognitions, using metaphor, and engaging in activities that are consistent with one’s values.
IV. Limitations and Missing Perspectives of Current Approaches
Cognitive-behavioral and acceptance / mindfulness-based approaches to chronic pain have many strengths, including conceptual models that validate patients’ experience of the stressful and disruptive nature of their pain. These approaches also activate change processes or mechanisms that generally lead to better outcomes, including providing patients a new model to understand the role of psychology in their pain, increasing patients’ self-efficacy or self-regulation abilities, reducing negative emotions, and increasing adaptive behavioral activities.
Yet we see several limitations and missing perspectives of these therapies for chronic pain. We acknowledge that debate surrounds many of these points, and space constraints preclude the extensive analysis that each deserves. These considerations, however, hold the potential to advance pain assessment and intervention, and they have greatly influenced how we conceptualize and treat chronic pain.
1. Current approaches have limited effectiveness.
Numerous randomized clinical trials and meta-analyses of those trials indicate that both CBT (10) and acceptance/mindfulness-based interventions (14) are effective for chronic pain. Yet the presence of an effect is less important than its magnitude. An important Cochrane review concluded that CBT has only small to medium effects (d ranging from −0.21 to −0.38) on pain, disability, and mood at post-treatment when compared to no treatment or treatment-as-usual, and effects are even more limited and sometimes non-significant at longer-term follow-ups and when CBT is compared with active controls (11). Similarly, acceptance and mindfulness-based therapies are effective beyond no treatment or usual care, and—given its goal of values-based action rather than pain reduction—ACT appears to have somewhat stronger effects on functioning and mood than on pain severity, which changes little (14). Overall, it appears that both CBT and acceptance / mindfulness-based approaches have similar, rather modest effects on patients with chronic pain (15–17). Although these treatments may yield greater benefits when offered by skilled clinicians outside of randomized trials, only a minority of patients has clinically significantly improvement, and even these patients continue to have some pain and impairment (18). Thus, more effective psychological treatments are needed.
2. Chronic pain is heterogeneous.
Current psychological treatments rarely differentiate types of chronic pain; “pain is pain” is a common perspective, leading clinicians to use the same basic approach with most or all patients with pain. An alternative perspective argues that chronic pain can be differentiated by etiological mechanisms, which vary in the degree of involvement of the central nervous system versus peripheral somatosensory system (19, 20). Centralized (central nervous system-based) pain (i.e., somatoform pain, central sensitization pain, or “nociplastic pain”) is predominant in fibromyalgia (FM), irritable bowel syndrome (IBS), pelvic pain, temporomandibular pain, tension or migraine headaches, and many patients with musculoskeletal presentations, particularly chronic low back and neck pain. Peripheral pain, in contrast, occurs in most patients with conditions that are nociceptive (i.e., driven by injury, inflammation, oxygen deprivation, malignancy, or other structural anomaly) such as rheumatoid arthritis, inflammatory bowel disease, erosive osteoarthritis, sickle cell disease, and cancer; or that are neuropathic (i.e., nerve-impairment pain), such as diabetic neuropathy and sciatic pain that is clearly derived from nerve compression. Although psychological processes are undoubtedly involved in all types chronic pain, and some patients have both centralized and peripheral pain, it is important to determine the extent of centralized pain a patient has, because psychological factors appear to play a stronger role in the etiology and maintenance of centralized than peripheral pain (19, 21).
3. There is a weak link between pain and findings from imaging or physical examinations.
Patients and providers often point to imaging abnormalities (e.g., disc problems, cartilage degeneration) or minor physical examination anomalies (e.g., leg length discrepancies, scoliosis, subluxations, scar tissue) and conclude that the pain is nociceptive or neuropathic—caused by the structural anomaly. Although such findings may emotionally validate patients and providers and reduce their sense of uncertainty, the abnormality is often not the cause of the pain. Such abnormalities are found in many asymptomatic people, and 85% to 99% of people with chronic back pain and other centralized syndromes have no obvious structural disorder or peripheral pathology that accounts for their pain (19, 22–24). The leading pain psychotherapy models, however, remain agnostic about the etiology of the pain and do not address patients’ incorrect attributions of pain etiology. Clinicians may believe that diagnosing pain subtype is difficult and potentially stigmatizing. Yet, the attribution that centralized pain stems primarily from peripheral tissue damage maintains patients’ fears that their pain signals dangerous bodily damage. This fearful belief can decrease patients’ motivation to engage in needed psychological and behavioral changes, thereby impeding treatment.
4. The brain not only modulates but also generates pain.
It is widely accepted that the brain—through conditioning, cognitions, and emotions—can modulate or influence the perception of peripheral nociception. Underappreciated, however, is the brain’s ability to generate pain with little or no peripheral nociception (25, 26). This proposal is supported by experimental research on pain-generating phenomena, including the nocebo effect (27), the rubber hand illusion (28), empathic pain (29), and hypnotically-induced pain (30). Predictive coding theory posits that the brain constructs the interoceptive experience of pain based upon its predictions of pain (31–33), and prior acute pain episodes shape strong expectations. Centralized pain can be attributed to activation of the brain’s “danger alarm system”—a system that creates pain in response to the presence or threat of tissue damage. Interestingly, psychological threats related to adverse experiences or conflict are closely linked to this system, and such threats can trigger the danger signal of pain in the absence of a physical injury (34, 35). Once generated, the pain can easily be learned by conditioning and reinforced by fear-motivated reactions to pain that further activate the danger signal, thus leading to chronic centralized pain.
5. Adverse life experiences and psychological conflict matter.
Chronic pain creates stress, but stressful life experiences, psychosocial adversity, and trauma also predispose to, precipitate, and perpetuate pain, especially centralized pain (36–42). The influence of psychological conflicts (e.g., intimacy or autonomy struggles, shameful secrets, perfectionism, fear of assertion, or social rejection) is under-appreciated, but such conflicts also appear to contribute to centralized pain (43–45). The emotional processes stemming from external adversities and internal conflicts appear to sensitize neural pathways that drive pain (46, 47). The leading psychological treatments for chronic pain, however, generally do not target or address the emotionally difficult life experiences that contribute to centralized pain.
6. Emotional experience and expression are important change processes.
What should be done about the emotions that are triggered by adverse experiences or psychological conflicts? Theory and research on experiential, psychodynamic, and exposure psychotherapies demonstrate the power of emotional processing—becoming aware of one’s avoided primary emotions, experiencing and expressing them in new and adaptive ways, and reflecting on and understanding links among one’s emotions, avoidance strategies, and symptoms (48–50). Yet unlike the highly effective exposure-based CBT treatments for anxiety disorders, CBT for chronic pain seeks to directly down-regulate negative emotions through techniques such as relaxation, cognitive reappraisal, or pleasant activity engagement. Acceptance-based approaches value emotional experiencing, although meditation and mindfulness are likely less emotionally-activating than experiential and exposure techniques, nor do they purposely elicit the expression of emotions.
7. Chronic pain can be substantially reduced or eliminated.
The terms “chronic” or “persistent” imply that pain lasts a long time—perhaps a lifetime. If true, then managing, accepting, or living with pain—as advocated by the leading therapies—is appropriate. Yet, thousands of case reports and testimonials claim that chronic pain has been either substantially reduced (e.g., 75% or 90% reduction) or eliminated (51–55). The possibility of reversing pain via psychological change applies mostly to centralized pain, we believe, because—in the absence of ongoing tissue damage / nociception—adaptive learning (brain neuroplasticity) is sufficient to disengage the danger alarm mechanism and reduce emotion and cognition-generated pain activation (56, 57).
V. Pain Interventions that Address These Limitations and Missing Perspectives
Given these limitations and considerations, we and others have developed and tested various treatments for chronic pain. Here, we briefly describe six promising approaches, all of which have contributed to our integrative model.
1. Pain reappraisal or reattribution therapies.
Several approaches attempt to counter the fearful belief that chronic centralized pain signals dangerous tissue damage. Sarno (51, 58, 59) popularized this approach by educating patients to attribute such pain to their brains and unconscious emotions rather than peripheral damage, and he reported very high rates of pain relief or elimination. Although we question Sarno’s view of the pain-generating mechanisms of unconscious emotions (particularly rage), and controlled studies of his approach are lacking, partial support of this model is provided by numerous trials showing the benefits of pain neuroscience education or “explaining pain”—teaching patients that chronic pain is primarily brain-based and strongly influenced by psychological factors (60, 61). The early practice of co-author HS was based on Sarno’s model and included pain neuroscience education, mindfulness techniques, and expressive writing. An uncontrolled study of 72 of HS’s patients revealed substantial benefits 6 months later: two-thirds of the patients had at least 30% pain reduction, and fully one-third had at least 70% pain reduction (62). We conducted a randomized trial of this approach among patients with FM; nearly half of treated patients (45.8%) had at least 30% pain reduction at 6-month follow-up, compared to 0% of waitlist controls (63).
2. In-vivo pain exposure therapy.
This approach is based on the fear-avoidance model of pain, which posits that unwarranted fear of pain-inducing movement or activity maintains both pain and disability (64). This therapy encourages patients to gradually increase actions that elicit pain, while challenging their fearful beliefs that such actions are dangerous. A review of several trials shows support for this approach (65). Because some patients have difficulty dealing with the negative emotions that are elicited by in-vivo pain exposure, Linton and colleagues (66, 67) developed a hybrid emotion-focused exposure treatment that incorporates emotion-regulation skills into in-vivo pain exposure therapy. In a small case series, most patients who received this hybrid therapy showed substantial improvements in both pain and physical functioning (66).
3. Expressive writing / emotional disclosure.
To address the impact of unresolved stressful life experiences or psychological conflicts on chronic pain, we and others have tested whether reversing emotional avoidance or inhibition by privately writing or speaking about stressors will reduce pain. Trials of expressive writing or emotional disclosure have found mixed results: there have been inconsistent, often null effects for people with rheumatoid arthritis (68–73), but some benefits for those with FM (74, 75), pelvic pain (76), and musculoskeletal pain (77, 78). Our review of this literature concluded that these techniques may be more helpful in patients with centralized pain than those with nociceptive pain conditions, such as rheumatoid arthritis, perhaps because of the higher levels of life stress and emotional problems in patients with centralized pain compared to RA (79).
4. Trauma-focused psychotherapies.
Trauma-focused psychotherapies are potentially powerful approaches to resolving stressful experiences. One intervention, eye movement desensitization and reprocessing (EMDR), has been examined in patients with co-morbid trauma and chronic pain (80, 81), and a review of these trials concluded that EMDR reduces and sometimes eliminates pain (80). We found that a 10-session trauma-focused emotional exposure therapy for patients with FM and trauma histories led to substantial symptom reduction in 20% of the patients, and moderate improvements in another 40% (82).
5. Intensive short-term dynamic psychotherapy (ISTDP).
This contemporary version of psychodynamic psychotherapy helps patients identify and experience unconscious emotions by overcoming defenses used to block such emotions and then facilitating patients’ understanding of the role such emotions and conflicts play in their symptoms, including pain (83). ISTDP has been tested in patients with pain disorders in a growing number of trials, demonstrating equivalence to CBT (84) and superiority to mindfulness-based stress reduction (85) for centralized pain conditions, and outperforming medical care for pelvic pain (86). Uncontrolled studies suggest the effectiveness of ISTDP for headaches (87). A meta-analysis of trials of short-term psychodynamic psychotherapy for somatic disorders, many of which included pain as a primary symptom, revealed medium to large effects, and the strongest effects occurred for those therapies that emphasized emotional experiencing (49).
6. Emotional awareness and expression therapy.
Our early pain reappraisal / reattribution-focused treatment, described above, has evolved to include a stronger focus on emotional processing of unresolved trauma and conflict, especially for patients for whom these problems are salient. Borrowing from ISTDP, experiential therapy, exposure therapy, expressive writing, and emotional rescripting (48, 79, 83, 88–91), we labeled our approach emotional awareness and expression therapy (EAET). We have tested EAET in various centralized pain conditions, helping patents experience and express their primary, adaptive emotions related to trauma or conflict, first in session and subsequently—in a balanced and moderated manner—in actual relationships. We have conducted several randomized controlled trials of EAET protocols that differ in length and format. In a recent large-scale trial of 230 patients with FM, we demonstrated that 8-session group-format EAET is superior to FM education on most outcomes at 6-month follow-up, and superior to CBT on several pain-related outcomes (92). In another trial, three sessions of individual EAET reduced symptoms and improved quality of life in IBS (93), and a 3-session group protocol that focused specifically on anger awareness and expression improved headaches (94). A single, 90-minute EAET interview reduced pain and psychological symptoms among primary care patients with medically unexplained pain and other symptoms (95), and the same protocol reduced women’s chronic pelvic pain and symptoms (96). Note that EAET, as conducted in these trials, purposely excluded cognitive-behavioral and mindfulness techniques so that we could test a theoretically “pure” emotion-focused therapy. We also did not emphasize reattributing the source of pain to the brain rather than damaged tissues or decreasing the pain / danger alarm mechanism—goals that may be more important in patients who have localized musculoskeletal pain, such as chronic low back or neck pain, than patients with FM, IBS, or headaches, for example. Our integrative model, which we describe next, includes techniques from CBT and acceptance / mindfulness-based approaches and emphasizes pain reattribution and fear reduction so that a broad range of patients with centralized pain can be successfully treated.
VI. An Integrative Assessment and Treatment Model for Centralized Pain
We now present our approach to working with patients with chronic pain, which is presented pictorially in Figure 1. We begin with an assessment to determine the degree to which patients have centralized pain and are, therefore, appropriate for our treatment approach. Treatment integrates aspects of pain neuroscience, pain reappraisal / reattribution, pain exposure therapy, expressive writing, ISTDP, and emotional awareness and expression, all of which have some empirical support, as described above. We include several cognitive-behavioral and mindfulness techniques, which are adapted to fit our conceptual framework. Below, we describe our assessment or diagnostic process and treatment, followed by clinician characteristics and attitudes that we think are important for the success of this approach. Detailed information can be found in Schubiner’s Unlearn Your Pain (52), and Abbass and Schubiner’s Hidden from View (97).
Figure. 1.
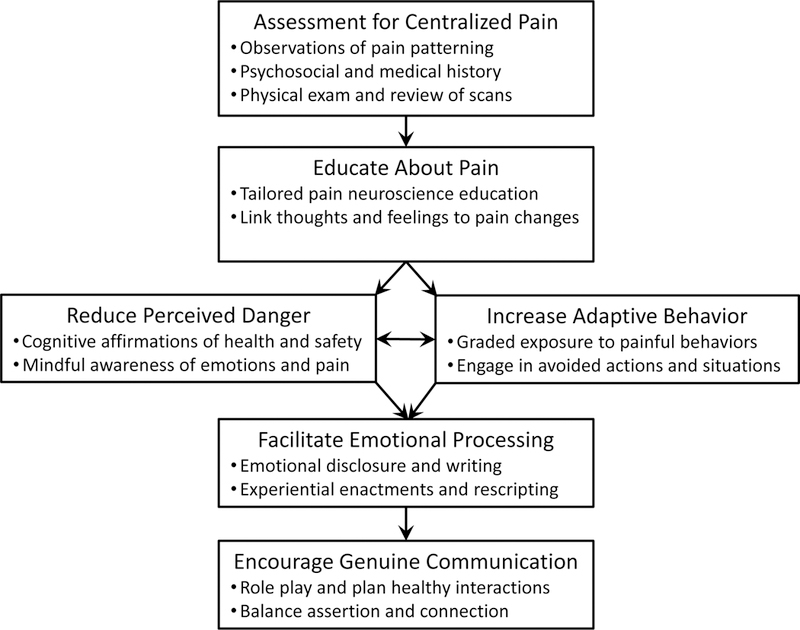
Integrative assessment and treatment framework for centralized pain.
Assessment for Centralized Pain and Patient Appropriateness for Treatment
Determining a symptom’s etiology is of paramount importance in general medical practice, and we believe this is true in chronic pain treatment as well. The objectives and techniques that we describe below are indicated for patients who have primarily centralized pain, because the role of psychological factors in the etiology and maintenance of centralized pain appears to be stronger than in pain that is primarily nociceptive, neuropathic, or inflammatory. Our approach to diagnosing centralized pain is consistent with the criteria for the classification of central sensitization pain presented in an important article by Nijs and colleagues (98), although we add several psychosocial variables that we find valuable not only for assessment but for guiding subsequent treatment. Although our assessment uses primarily interview and observation, clinicians might consider adding standardized patient-report measures, many of which are reviewed by Williams (99). In particular, the Survey for the Assessment of Fibromyalgia based on the 2011 Modification of the American College of Rheumatology’s Preliminary Diagnostic Criteria of FM (100) assesses both the degree of widespread pain and other somatic and psychiatric symptoms; this measure captures core aspects of centralization beyond the diagnosis of FM (101). The Central Sensitization Inventory (102) also is recommended (98). Other approaches for assessing centralized pain, such as the use of quantitative sensory testing, hold potential but currently are not feasible in most clinical settings (99).
We conduct a detailed interview that focuses on pain patterns, health and developmental history, psychosocial issues linked to the onset or exacerbation of pain, a review of medical records and scans (if available), and a physical examination. The findings are then integrated to determine the degree to which the patient has centralized pain.
1. Pain patterns.
Various indicators for the presence of centralized pain can be gleaned from the patterning of pain and help differentiate centralized from nociceptive pain. Centralized pain: a) usually begins either without injury or persists well after normal healing has occurred; b) has a distribution that is inconsistent with a structural disorder, such as located on one whole side of the body or the entire arm or leg; c) shifts from one location in the body to other locations or spreads from one area to adjacent regions over time; and d) varies with time of day, place, or activity in patterns related to certain triggers, such as movements, sensory input, environments, interpersonal interactions, or stress-related emotions.
Asking the patient to imagine experiencing a triggering event (e.g., turning the neck or sitting on a hard surface), without moving, often causes the painful sensation to occur. This response strongly suggests the presence of centralized pain.
2. Psychosocial and medical history.
Patients’ histories may reveal findings strongly suggestive of centralized pain, such as the presence of other central sensitization symptoms or syndromes (e.g., headaches, irritable bowel syndrome, pelvic pain, temporomandibular joint disorder, etc.), and hypersensitivity to stimuli such as bright light, sounds, smell, heat, or cold. In addition, the interview may reveal psychosocial features that are associated with centralized pain: a) significant adverse childhood experiences, which can sensitize the pain neural danger/alarm mechanisms; b) internal conflicts that create anxiety, such as excessive worry about being judged, a strong desire to please others, perfectionism, and self-criticism; c) pain onset or exacerbation associated with events or experiences that typically cause people fear, anger, grief, or guilt; and d) changes in pain and other somatic symptoms that occur during the interview when stressful experiences or conflicts are explored, especially when inhibited memories and emotions are activated. We note that these psychosocial and emotional features (a to d) are not specific to centralized pain conditions and are found in some patients with non-centralized pain and other disorders. We include them, however, because they are more likely to occur in centralized than non-centralized pain conditions and, importantly, assessing these psychosocial and emotional processes helps prepare the patient and guide the clinician for the subsequent treatment.
3. Physical examination and review of records and scans.
In centralized pain, the physical examination does not reveal objective findings, such as abnormal reflexes, decreased muscle strength, or loss of sensation. Rather, one often finds paresthesias, allodynia, hyperalgesia, or radiation of pain in response to touch or pressure on various parts of the body. It is important to exclude nociceptive or neuropathic pain, but one should be cautious attributing pain to abnormal imaging results in the absence of clear pathological findings such as inflammation, fracture, or tumor. As mentioned, non-specific findings, such as degenerative disc disease and bulging discs, are normal in the adult population and should not be taken as prima facie evidence of pain causation (9, 22). Similarly, one should be cautious of attributing pain to minor structural anomalies, such as leg length discrepancies, muscle tightness, scoliosis, or subluxations, which are often normal variants or even effects of pain, rather than causes of pain.
Integrative Psychological Treatment for Centralized Pain
The treatment described here is designed for those patients whom the assessment has identified as having primarily centralized pain, which we often label for patients as “neural pathway” pain. The treatment has five major components, as depicted in Figure 1. We usually implement these sequentially, starting with pain neuroscience education, followed by cognitive, behavioral, and mindfulness techniques. These techniques are particularly important for patients with localized musculoskeletal pain (e.g., back, neck, arm, etc.) and may prove sufficient for many of them. If their pain remains little changed, however, or unresolved trauma or psychological conflicts appear to be impeding pain reduction, then we proceed to focus on emotional and interpersonal changes. We also often move quickly to emotional and interpersonal techniques for those patients who readily acknowledge that stress and their brains, rather than their bodies, play the primary role in their symptoms, such as many patients with FM. Note that all of these interventions target two broader change processes—helping patients learn that: 1) they are not helpless bystanders but rather empowered participants in their recovery; and 2) their pain as well as their stressful life events and emotional reactions are not inherently dangerous and should be courageously approached rather than fearfully avoided.
1. Educate about pain.
This vital step begins during the intake interview and continues through early treatment sessions. The belief that the pain is due to a peripheral or structural abnormality can maintain the brain’s danger/alarm pain mechanism and reduce patients’ self-efficacy to reduce or eliminate pain. In contrast, when patients understand that their pain is real yet caused by central rather than peripheral processes, subsequent treatment is facilitated. It is critical to validate that the pain is not “imaginary” or “made up” and to emphasize that the patient is neither at fault nor suffering from a “mental condition,” but rather a neural pathway condition that is changeable. We borrow from pain neuroscience education, or the explaining pain model (61), but we enhance it by personalization or tailoring—integrating findings from the assessment into the education about the patient’s pain. Also, when patients experience changes in their pain or other symptoms coincident with imagining pain-eliciting actions, discussing difficult topics, or activating certain emotions, patients experience a powerful, first-hand demonstration of the influence of their brain on their pain. We have observed that some limited pain reduction commonly occurs in patients—and a small number of patients experience significant pain relief or even pain elimination—when they realize and accept that their body is not damaged, that their pain is driven by their central nervous system, and that they can recover. This step often needs to be reiterated during the course of treatment, as patients frequently fall back into erroneous peripheral explanations for centralized pain.
2. Reduce perceived danger.
The next step is to help patients “retrain their brain’s neural pathways” and reduce the pain danger alarm—an approach sometimes referred to as “pain reprocessing therapy.” We use various techniques to help patients reduce their fear, frustration, and excessive attention to their pain. We borrow the practice of adaptive self-statements from CBT and encourage patients to be “less fearful when experiencing pain” by creating and repeating statements that affirm their health and lack of concern about the pain (103). For example, patients are encouraged to remind themselves that “my pain is in my brain,” “there is nothing wrong with my body,” “the sensations are real but temporary,” and “there is no danger.” Mindfulness training combined with the conviction that the brain is the source of the pain can facilitate experiencing pain as a non-harmful sensation, thus further reducing the pain-fear-pain cycle. Because patients commonly have negative thoughts about their pain as well as their past and future, mindfulness techniques can help patients see such thoughts as the brain’s construction, and that disregarding them helps reduce the brain’s danger/alarm mechanism.
3. Increase adaptive behaviors.
This treatment component is usually presented simultaneously with the above techniques that reduce perceived danger, so that cognitive and behavioral changes facilitate each other. Patients often lead physically and socially restricted lives. Thus, borrowing from in-vivo pain exposure therapy, we encourage patients to engage in graded or hierarchical exposure to activities that they have avoided due to pain. In addition, patients should engage in these activities with the conviction that their bodies are not damaged and will not be injured by these activities, and that the pain is stemming from a changeable brain. Patients can help themselves reengage in both physical and social activities, despite pain, by adding health-affirming self-statements and mindfulness of harmless sensations, which further reduces fear and the danger alarm. Importantly, such behavioral activity engagement has two goals—to help patients decrease pain-specific as well as general fear and helplessness and to help them become more free or flexible in their behaviors, both of which reduce pain and improve functioning.
4. Facilitate emotional processing.
Some patients’ pain is linked to a broader pattern of avoided activities, relationships, places, memories, and other emotion-eliciting experiences stemming from conflicts or adverse life experiences. Because negative emotions—and how patients deal with them—may drive the development and persistence of centralized pain, addressing such maladaptive emotional experiences is important for many patients, especially those with classic centralized syndromes (e.g., FM, IBS, headache, pelvic pain) and those who acknowledge unresolved trauma or conflict. Using EAET techniques, we help patients disclose traumatic or conflicted experiences, including secrets, and become aware of, experience, and express the primary adaptive emotions that they have been avoiding. That is, we target for activation those emotions that are appropriate to circumstances that elicited them: anger when victimized or treated unjustly, guilt when having harmed another, sadness when losing a valued object, pride when having accomplished, love toward attachment objects, etc. We use expressive writing (particularly “free writing” and “unsent letters”) as homework assignments to facilitate access to memories and feelings related to childhood traumatic events or current stressors. Writing exercises are brought to session, where they can be used to facilitate in-session processing of avoided emotions through “experiential enactments.” That is, we help patients recall being present in the stressful experience (i.e., “go back to a specific time, place, and interaction”) and then speak and express, with voice and body, their suppressed thoughts and feelings to the imagined person involved. These emotions are expressed fully with voice, language, and body in therapy sessions, but acting out these emotions outside of the session is strongly discouraged. Importantly, patients do not just “relive” the often painful, terrifying, shameful, or hurtful experience as happened originally; rather, they “rescript” it by accessing the feelings that were present but not expressed (often including anger) and imagining and acting out alternative outcomes to create “corrective emotional experiences.” This work in the clinic, which is often emotionally intense, is commonly followed by a sense of relief and pain reduction, along with enhanced awareness of the patient’s feelings, desires, and motivation to change the way the patient relates to others in real life. These exercises also help patients more clearly identify their emotions when they have a pain exacerbation in daily life, and they can remind themselves that they are experiencing a certain emotion, and the pain is just a signal of an important emotion to which they should attend. Note that people exposed to adverse childhood events are likely to carry a mixture of feelings towards their abusers, including rage and guilt about the rage, and processing these entwined feelings is important. Many patients have difficulty with compassion and forgiveness, particularly toward themselves. Thus, we include perspective-taking techniques to facilitate self-compassion and self-forgiveness.
5. Encourage adaptive interpersonal communication.
Many patients feel stuck in family, employment, religious, or other social situations, and consistent with ACT, it is important to encourage exposure to, and reengagement in, patients’ valued activities despite the negative emotions that are generated in the process. Patients’ most important stressors usually involve other people, who often continue to serve as a source of emotional conflict—and pain. Although emotional processing techniques sometimes resolve such conflicts, many patients need help changing how they relate to others in real life. Often, patients need to balance their need for assertion or power (setting boundaries, expressing desires, declining requests) with their need for connection (expressing love, gratitude, or sadness; apologizing; opening up). Such actions are often frightening, and patients usually benefit from first conducting emotional awareness and expression toward the imagined other person in private or in the clinic, so that they are aware of their feelings and desires and more motivated to address these relationships in real life. In session, patients are first encouraged to engage in EAET exercises, as described above, then role play how they might interact with key people in their lives, and then “try it out there.” Although the in-clinic emotional processing may be intense in expression and language, we encourage patients to show balanced and moderated expression with others in real life, which we think is facilitated by healthy resolution of the emotional conflict in session
Clinician’s Perspective, Attitude, and Style
The approach we are describing is most successful when clinicians maintain certain attitudes and behaviors. Given the stigma and dualism associated with mind-body symptoms, it is vital that clinicians believe in the reality of their patients’ pain—patients absolutely do experience bodily pain—and clinicians should communicate this clearly to patients. It is unfortunately common for clinicians to harbor stigma towards patients with centralized pain—that their pain is not as “real” as peripheral or nociceptive pain. Clinicians can avoid this trap by considering the adverse life events that often precipitate and maintain their patients’ pain. The clinician should also express optimism about the possibility of pain reduction or elimination, given sufficient changes in the patient’s beliefs, actions, emotions, and relationships. A caring and empathic attitude is needed toward patients who are having difficulty understanding or adopting the model of centralized pain or making changes in their emotions and relationships. Because some patients struggle with the idea that the pain is their fault or a sign of mental illness, clinicians should normalize neural pathway pain by emphasizing its high prevalence and informing patients that mind-body symptoms occur in almost everyone at times. We also suggest that clinicians disclose to patients their own personal mind-body reactions or symptoms. Although views of this practice vary, we have found that such clinician disclosure not only serves as a model for patients but also powerfully validates them.
Eliciting the experience and expression of patient’s negative emotions can be challenging for both patients and clinicians. Interpersonally-sensitive clinicians may collude with frightened patients to avoid eliciting negative emotions, particularly healthy anger, which is often the most important—but scariest—emotion to experience and express. Clinicians should use “dosing” techniques if patients’—or their own—emotions become too strong or dysregulated—shifting into a cognitive or reflective mode or encouraging adaptive self-statements or mindfulness. But it is important for clinicians to believe that activating patients’ avoided emotions is—like centralized pain—safe rather than dangerous, and that doing so can result in improved clinical outcomes.
VII. Integrative Approach Applied to Mr. A.
We now revisit the case of Mr. A. in light our assessment and treatment model. Mr. A. had a 2-hour intake session and three follow-up treatment sessions with HS. The initial evaluation revealed that Mr. A’s pain shifted locations (alternately in his back, neck and abdomen), had spread to new locations over time, and completely remitted while on vacation. Although Mr. A. did not report significant childhood trauma, he had substantial anxiety and self-criticism, stemming in part to a conflict—fear of rejection by his father—contributing to Mr. A.’s perfectionism. Other centralized symptoms included abdominal discomfort and headaches, and stressful events preceded the onset of these symptoms. There were no objective neurological findings, and although the MRI showed abnormalities in his neck and lumbar spine, the prevalence of such degenerative or bulging discs in his pain-free age cohort is 68% and 50%, respectively, suggesting non-specific findings. Overall, the evidence strongly suggested that Mr. A’s pain was primarily centralized rather than nociceptive or neuropathic, and he was deemed appropriate for our treatment.
HS shared these findings, explaining to Mr. A that his pain was due to his brain’s neural pathways. Mr. A generally accepted this explanation, although he retained some doubts about its validity due to the severity of his pain. Yet he was excited and relieved about the possibility of recovering, because this explanation “makes more sense than what other doctors have told me.” HS then recommended affirming self-statements for Mr. A to mentally rehearse: that he “is healthy, strong, not damaged, and not afraid of the pain.” He also received training in mindful awareness of his breathing and painful sensations, to be followed by statements that he was “not damaged,” his “brain was creating these harmless sensations,” and he “will recover.” He was encouraged to begin engaging in more physical and social activities to reverse the domination that pain had over his thoughts and actions.
At session 2, Mr. A. reported having some days when his pain was much better, but other days when his pain increased. Between sessions, he had engaged in expressive writing about work stress, and the increased pain could have resulted from the activation—but not resolution—of his conflicted emotions. He was reassured that he was healthy, and that changing neural pathways requires time and effort, particularly addressing core conflicts. During session, he was encouraged to express his feelings—primarily anger—to an image of his boss in an empty chair, which provided some relief, although he experienced stomach discomfort in the process. This exercise activated childhood memories of his father, and he was encouraged to write an unsent letter to his father as homework. The session ended with another mindful awareness exercise—to experience pain without fear and to experience and accept his anger, which resulted in a dramatic reduction in pain within 10 minutes. By session 3, Mr. A’s pain was much reduced, and he reported realizing that he was still quite angry at his father for intimidating him, but also that he still loved his father and was sad about their lack of closeness. He read his unsent letter aloud and then experientially enacted a stressful boyhood interaction with his father, voicing both his anger and his sad yet loving feelings quite clearly and without much guilt. He experienced much reduced tension, and his pain ratings dropped to near zero. Session 4 focused on how he might interact with both his father and boss in healthier and more direct ways, and he reflected on changes he had made.
A follow-up telephone call 3 months later indicated that Mr. A’s pain had decreased to “minimal,” he was exercising several times per week, and he had become more assertive about his needs at work. He felt more relaxed and open while visiting his father, adding that he was able to speak more honestly to him. At a 6-month check-in, Mr. A reported being basically pain-free, with only occasional twinges of discomfort, which he countered by just observing the pain and examining his feelings.
VIII. Challenges and Solutions
There are a range of challenges to this approach. The concept that the brain not only modulates peripheral nociception but also generates pain with little or no tissue damage is counter-intuitive to most patients and providers. Clinicians often think that it is rare to encounter somatic symptoms caused by the central nervous system, but many—perhaps most—patients who seek pain treatment have centralized pain, although we recognize that some patients have a combination of centralized and peripheral contributions to their pain. We also recognize that the proposal that centralized pain might be substantially reduced or even eliminated could result in patients becoming even more hopeless and discouraged, if they do not achieve this goal. Because some patients, however, can and do show remarkable pain reductions, we think that failing to seek this goal is a disservice to patients.
It can be difficult to diagnose centralized pain, because the clinical picture may be complicated, and providers may not have the training or time to do so. Our experience, however, is that a range of clinicians—physicians, nurses, physical therapists, psychologists, social workers, and chiropractors—can be taught to make this diagnosis when the clinical scenarios clearly fit, as is often the case, such as with Mr. A. If the diagnosis is unclear, one might have further testing to rule out peripheral pathology, or engage in continued observation of the symptom patterns, which will often clarify underlying mechanisms. For patients with primarily peripheral (nociceptive, inflammatory, or neuropathic) pain—as well as those showing little or no benefit from our approach—we recommend the more widely-available pain management approaches, such as CBT or ACT. For patients with centralized pain who are not interested in our approach, we offer some basic pain neuroscience education and the option for future treatment, if patients’ alternative pursuits prove unsatisfactory. Nonetheless, once presented with the neuroscientific and clinical evidence, many patients will understand and accept the model of centralized pain and the possibility that “changing your brain can change your pain.” We think that such patients can be treated by a range of providers within their usual clinical practice, aided by published materials that describe either our approach (52, 97) or similar ones (51, 53–55, 104, 105).
In our practice and clinical trials, we have explored different durations and formats of this approach. We have offered a single assessment and education-oriented session (which may include experiential and expressive components), brief courses of therapy (e.g., 3 to 5 sessions), a 4-week “class,” and an 8-session group intervention. Many patients need more therapy than this, however, especially to reverse long-standing patterns of emotional and interpersonal avoidance or conflict. Individual treatment is easier than group therapy not only to schedule but also to implement, because patients have unique emotional issues that often need individual attention. Yet there are benefits to group approaches. Each group usually has one or more patients who not only strongly endorse the model but also have the courage to disclose their private struggles and engage in emotional expression exercises, which helps other group members do so. Group validation of one’s disclosures, expressions, and change efforts is powerful, and other group members can facilitate role playing and other interpersonal change experiences. Compared to individual therapy or to group therapy that is relatively structured and didactic, the group format of our approach requires particularly flexible and strong therapists.
IX. Conclusions
The epidemic of chronic pain continues to grow, and the limitations of current conceptual models and interventions are becoming clear. We now know that the central nervous system rather than peripheral tissue pathology plays the key role in many people’s chronic pain. Fearful and avoidant thoughts, emotions, and behaviors not only about pain but also broader and longer-standing stressors and conflicts drive and maintain neural pain networks. Distinguishing centralized from peripheral pain is possible in most patients and allows appropriately targeted treatments. For those with centralized pain, therapy such as that described here can create powerful changes, reducing fear-based avoidance of action, emotions, and relationships, which can result in dramatic reductions or even elimination of pain. Given this possibility, one should question whether the term “pain management” is too narrow or pessimistic; we think that pain “treatment” or “recovery” better describes the goal of our approach. Moreover, we wonder whether the field’s recognition of the causal links between stressful experiences and centralized pain will challenge the inefficient—and ironic—organization of many health care systems, where patients’ trauma is treated in one clinic, but pain is managed in another.
As the neuroscience of pain becomes more understood and accepted within the medical, mental health, and lay communities, we anticipate that the concepts and treatment we are advocating will become less stigmatized and more practiced. We encourage clinicians and researchers to devote greater efforts to diagnose centralized pain and implement this therapy for those patients, while also developing and testing modifications or alternatives that might have even greater impact—both efficacy and reach—for the millions who suffer from chronic pain.
Acknowledgments
We are grateful for the numerous colleagues and former students who have supported us and contributed to our work over the years, and we especially thank our current collaborators Alan Gordon, Allan Abbass, Yoni Ashar, and Tor Wager. Preparation of this manuscript was supported by the National Institutes of Arthritis, Musculoskeletal, and Skin Diseases under award number AR057808. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
MAL has no conflicts of interest. HS is the author of two books mentioned in this article, but otherwise has no conflicts of interest.
Contributor Information
Mark A. Lumley, Department of Psychology, Wayne State University, Detroit, Michigan
Howard Schubiner, Department of Internal Medicine, Providence-Providence Park Hospital, Ascension Health, and Michigan State University College of Human Medicine, Southfield, Michigan
References
- 1.Merskey H Pain terms: a list with definitions and notes on usage. Recommended by the IASP subcommittee on taxonomy. Pain 1979;6:249–52. [PubMed] [Google Scholar]
- 2.APA. Diagnostic and statistical manual of mental disorders (4th ed., Text Revision) Washigton, DC: American Psychiatric Association Press; 2000. [Google Scholar]
- 3.Lumley MA, Cohen JL, Borszcz GS, Cano A, Radcliffe AM, Porter LS, Schubiner H, Keefe FJ. Pain and emotion: a biopsychosocial review of recent research. J Clin Psychol 2011;67:942–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.APA. Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association Press; 2013. [Google Scholar]
- 5.Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: Results of an internet-based survey. J Pain 2010;11:1230–9. [DOI] [PubMed] [Google Scholar]
- 6.Council NR. Relieving pain in America: A blueprint for transforming prevention, care, education, and tesearch Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 7.Vowles KE, McEntee ML, Julnes PS, Frohe T, Ney JP, van der Goes DN. Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. Pain 2015;156:569–76. [DOI] [PubMed] [Google Scholar]
- 8.Morales-Espinoza EM, Kostov B, Salami DC, Perez ZH, Rosalen AP, Molina JO, Paz LG, Momblona JMS, Areu JB, Brito-Zeron P, Ramos-Casais M, Siso-Almirall A. Complexity, comorbidity, and health care costs associated with chronic widespread pain in primary care. Pain 2016;157:818–26. [DOI] [PubMed] [Google Scholar]
- 9.Deyo RA, Mirza SK, Turner JA, Martin BI. Overtreating chronic back pain: Time to back off? J Am Board Fam Med 2009;22:62–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoffman BM, Papas RK, Chatkoff DK, Kerns RD. Meta-analysis of psychological interventions for chronic low back pain. Health Psychol 2007;26:1–9. [DOI] [PubMed] [Google Scholar]
- 11.Williams AC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane database of systematic reviews (Online) 2012;11. [DOI] [PMC free article] [PubMed]
- 12.Ehde DM, Dillworth TM, Turner JA. Cognitive-behavioral therapy for individuals with chronic pain: Efficacy, innovations, and directions for research. Am Psychol 2014;69:153–66. [DOI] [PubMed] [Google Scholar]
- 13.McCracken LM, Vowles KE. Acceptance and commitment therapy and mindfulness for chronic pain: Model, process, and progress. Am Psychol 2014;69:178–87. [DOI] [PubMed] [Google Scholar]
- 14.Hann KEJ, McCracken LM. A systematic review of randomized controlled trials of Acceptance and Commitment Therapy for adults with chronic pain: Outcome domains, design quality, and efficacy. J Contextual Behav Sci 2014;3:217–27. [Google Scholar]
- 15.Cherkin DC, Sherman KJ, Balderson BH, Cook AJ, Anderson ML, Hawkes RJ, Hansen KE, Turner JA. Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: A randomized clinical trial. JAMA 2016;315:1240–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Veehof MM, Trompetter HR, Bohlmeijer ET, Schreurs KMG. Acceptance- and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review. Cognitive Behav Ther 2016;45:5–31. [DOI] [PubMed] [Google Scholar]
- 17.Lauche R, Cramer H, Dobos G, Langhorst J, Schmidt S. A systematic review and meta-analysis of mindfulness-based stress reduction for the fibromyalgia syndrome. J Psychosom Res 2013;75:500–10. [DOI] [PubMed] [Google Scholar]
- 18.Morley S, Williams A, Eccleston C. Examining the evidence about psychological treatments for chronic pain: Time for a paradigm shift? Pain 2013;154:1929–31. [DOI] [PubMed] [Google Scholar]
- 19.Clauw DJ. Diagnosing and treating chronic musculoskeletal pain based on the underlying mechanism(s). Best Pract Res Clin Rheumatol 2015;29:6–19. [DOI] [PubMed] [Google Scholar]
- 20.Kosek E, Cohen M, Baron R, Gebhart GF, Mico J-A, Rice ASC, Rief W, Sluka AK. Do we need a third mechanistic descriptor for chronic pain states? Pain 2016;157:1382–6. [DOI] [PubMed] [Google Scholar]
- 21.Yunus MB. Central sensitivity syndromes: A new paradigm and group nosology for fibromyalgia and overlapping conditions, and the related issue of disease versus illness. Semin Arthritis Rheum 2008;37:339–52. [DOI] [PubMed] [Google Scholar]
- 22.Brinjikji W, Luetmer PH, Comstock B, Bresnahan BW, Chen LE, Deyo RA, Halabi S, Turner JA, Avins AL, James K, Wald JT, Kallmes DF, Jarvik JG. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. Am J Neuroradiol 2015;36:811–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low back pain? JAMA 1992;268:760–5. [PubMed] [Google Scholar]
- 24.Kroenke K Patients presenting with somatic complaints: epidemiology, psychiatric co-morbidity and management. Int J Methods Psych Res 2003;12:34–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lane RD, Waldstein SR, Critchley HD, Derbyshire SWG, Drossman DA, Wager TD, Schneiderman N, Chesney MA, Jennings JR, Lovallo WR, Rose RM, Thayer JF, Cameron OG. The rebirth of neuroscience in psychosomatic medicine, Part II: clinical applications and implications for research. Psychosom Med 2009;71:135–51. [DOI] [PubMed] [Google Scholar]
- 26.Hashmi JA, Baliki MN, Huang L, Baria AT, Torbey S, Hermann KM, Schnitzer TJ, Apkarian AV. Shape shifting pain: chronification of back pain shifts brain representation from nociceptive to emotional circuits. Brain 2013;136:2751–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blasini M, Corsi N, Klinger R, Colloca L. Nocebo and pain: an overview of the psychoneurobiological mechanisms. PAIN Reports 2017;2:e585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Coleshill MJ, George DN, Mazzoni G. Placebo analgesia from a rubber hand. J Pain 2017;18:1067–77. [DOI] [PubMed] [Google Scholar]
- 29.Zaki J, Wager TD, Singer T, Keysers C, Gazzola V. The Anatomy of suffering: Understanding the relationship between nociceptive and empathic pain. Trends Cog Sciences 2016;20:249–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Derbyshire SWG, Whalley MG, Stenger VA, Oakley DA. Cerebral activation during hypnotically induced and imagined pain. NeuroImage 2004;23:392–401. [DOI] [PubMed] [Google Scholar]
- 31.Van den Bergh O, Witthöft M, Petersen S, Brown RJ. Symptoms and the body: Taking the inferential leap. Neurosci Biobehav Rev 2017;74:185–203. [DOI] [PubMed] [Google Scholar]
- 32.Barrett LF, Simmons WK. Interoceptive predictions in the brain. Nat Rev Neurosci 2015;16:419–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Prescott SA, Ma Q, De Koninck Y. Normal and abnormal coding of somatosensory stimuli causing pain. Nat Neurosci 2014;17:183–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tabor AA. Embodied pain-negotiating the boundaries of possible action. Pain 2017;158:1007–11. [DOI] [PubMed] [Google Scholar]
- 35.Gracely RH, Schweinhardt P. Programmed symptoms: disparate effects united by purpose. Curr Rheumatol Rev 2015;11:116–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Varinen A, Kosunen E, Mattila K, Koskela T, Sumanen M. The relationship between childhood adversities and fibromyalgia in the general population. J Psychosom Res 2017;99:137–42. [DOI] [PubMed] [Google Scholar]
- 37.Generaal E, Vogelzangs N, Macfarlane GJ, Geenen R, Smit JH, EJCN de Geus, BWJH Penninx, Dekker J. Biological stress systems, adverse life events and the onset of chronic multisite musculoskeletal pain: a 6-year cohort study. Ann Rheum Dis 2016;75:847–54. [DOI] [PubMed] [Google Scholar]
- 38.Nicol AL, Sieberg CB, Clauw DJ, Hassett AL, Moser SE, Brummett CM. The association between a history of lifetime traumatic events and pain severity, physical function, and affective distress in patients with chronic pain. J Pain 2016;17:1334–48. [DOI] [PubMed] [Google Scholar]
- 39.You DS, Meagher MW. Childhood adversity and pain sensitization. Psychosom Med 2016;78:1084–93. [DOI] [PubMed] [Google Scholar]
- 40.Van Houdenhove B, Luyten P, Tiber Egle U. Stress as a key concept in chronic widespread pain and fatigue disorders. J Musculoskel Pain 2009;17:390–9. [Google Scholar]
- 41.Landa A, Peterson BS, Fallon BA. Somatoform Pain: A developmental theory and translational research review. Psychosom Med 2012;74:717–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sachs-Ericsson NJ, Sheffler JL, Stanley IH, Piazza JR, Preacher KJ. When emotional pain becomes physical: Adverse childhood experiences, pain, and the role of mood and anxiety disorders. J Clin Psychol 2017;73:1403–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Luyten P, Van Houdenhove B, Lemma A, Target M, Fonagy P. Vulnerability for functional somatic disorders: A contemporary psychodynamic approach. J Psychother Integr 2013;23:250–62. [Google Scholar]
- 44.Kross E, Berman MG, Mischel W, Smith EE, Wager TD. Social rejection shares somatosensory representations with physical pain. Proc Natl Acad Sci 2011;108:6270–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Eisenberger NI, Lieberman MD. Why rejection hurts: a common neural alarm system for physical and social pain. Trends Cog Sci 2004;8:294–300. [DOI] [PubMed] [Google Scholar]
- 46.Lane RD, Waldstein SR, Chesney MA, Jennings JR, Lovallo WR, Kozel PJ, Rose RM, Drossman DA, Schneiderman N, Thayer JF, Cameron OG. The rebirth of neuroscience in psychosomatic medicine, Part I: historical context, methods, and relevant basic science. Psychosom Med 2009;71:117–34. [DOI] [PubMed] [Google Scholar]
- 47.Yunus MB. Fibromyalgia and overlapping disorders: The unifying concept of central sensitivity syndromes. Semin Arthritis Rheum 2007;36:339–56. [DOI] [PubMed] [Google Scholar]
- 48.Lane RD, Ryan L, Nadel L, Greenberg L. Memory reconsolidation, emotional arousal, and the process of change in psychotherapy: New insights from brain science. Behav Brain Sci 2015;38:e1. [DOI] [PubMed] [Google Scholar]
- 49.Abbass A, Kisely S, Kroenke K. Short-term psychodynamic psychotherapy for somatic disorders. Psychother Psychosom 2009;78:265–74. [DOI] [PubMed] [Google Scholar]
- 50.Foa EB, Kozak MJ. Emotional processing of fear: exposure to corrective information. Psychol Bull 1986;99:20–35. [PubMed] [Google Scholar]
- 51.Sarno JE. The mindbody prescription: Healing the body, healing the pain New York, New York: Hachette Book Group USA; 1998. [Google Scholar]
- 52.Schubiner H, Betzold M. Unlearn your pain: A 28-day process to reprogram your brain 3rd Edition ed. Pleasant Ridge, MI: Mind-Body Pubishing; 2016. [Google Scholar]
- 53.Schechter D Think away your pain: Your brain is the solutoin to your pain Culver City, CA: Mindbody Medicine Publications; 2014. [Google Scholar]
- 54.Selfridge N, Peterson F. Freedom from fibromyalgia: The 5 week program proven to conquer pain New York, New York: Three Rivers Press; 2001. [Google Scholar]
- 55. Hanscom D Back in control: A surgeon’s roadmap out of chronic pain, 2nd Edition. Seattle, WA: Vertus Press; 2017. [Google Scholar]
- 56.Shires A, Cayoun B, Simmons A. Immediate and lasting chronic pain reduction following a brief self-implemented mindfulness-based interoceptive exposure task: a pilot study Mindfulness; in press. [Google Scholar]
- 57.Yoshino A, Okamoto Y, Okada G, Takamura M, Ichikawa N, Shibasaki C, Yokoyama S, Doi M, Jinnin R, Yamashita H, Horikoshi M, Yamawaki S. Changes in resting-state brain networks after cognitive–behavioral therapy for chronic pain. Psychol Med 2017:1–11. [DOI] [PubMed]
- 58.Sarno JE. Mind over back pain: The mind-body connection New York: Warner Books; 1991. [Google Scholar]
- 59.Sarno JE. Mind over back pain. a radically new approach to the diagnosis and treatment of back pain New York: Harper Collins Publishers; 1982. [Google Scholar]
- 60.Louw A, Diener I, Butler DS, Puentedura EJ. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Arch Phys Med Rehab 2011;92:2041–56. [DOI] [PubMed] [Google Scholar]
- 61.Moseley GL, Butler DS. Fifteen years of explaining pain: The past, present, and future. J Pain 2015;16:807–13. [DOI] [PubMed] [Google Scholar]
- 62.Burger AJ, Lumley MA, Carty JN, Latsch DV, Thakur ER, Hyde-Nolan ME, Hijazi AM, Schubiner H. The effects of a novel psychological attribution and emotional awareness and expression therapy for chronic musculoskeletal pain: A preliminary, uncontrolled trial. J Psychosom Res 2016;81:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hsu MC, Schubiner H, Lumley MA, Stracks JS, Clauw DJ, Williams DA. Sustained pain reduction through affective self-awareness in fibromyalgia: A randomized controlled trial. J Gen Int Med 2010;25:1064–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Vlaeyen J, Linton S. Fear‐avoidance model of chronic musculoskeletal pain: 12 years on. Pain 2012;153:1144–7. [DOI] [PubMed] [Google Scholar]
- 65.Vlaeyen J, Morley S, Linton SJ, Boersma K, de Jong J. Pain-related fear: exposure based treatment for chronic pain Seattle, WA: IASP Press; 2012. [Google Scholar]
- 66.Linton SJ, Fruzzetti AE. A hybrid emotion-focused exposure treatment for chronic pain: A feasibility study. Scand J Pain 2014;5:151–8. [DOI] [PubMed] [Google Scholar]
- 67.Linton SJ, Flink IK, Schrooten MGS, Wiksell R. Understanding co-occurring emotion and pain: The role of context sensitivity from a transdiagnostic perspective. J Contemp Psychother 2016;46:1–9. [Google Scholar]
- 68.Lumley MA, Keefe FJ, Mosley-Williams A, Rice JR, McKee D, Waters SJ, Partridge RT, Carty JN, Coltri AM, Kalaj A, Cohen JL, Neely LC, Pahssen JK, Connelly MA, Bouaziz YB, Riordan PA. The effects of written emotional disclosure and coping skills training in rheumatoid arthritis: A randomized clinical trial. J Consult Clin Psychol 2014;82644–58. [DOI] [PMC free article] [PubMed]
- 69.Lumley MA, Leisen JCC, Partridge RT, Meyer TM, Radcliffe AM, Macklem DJ, Naoum LA, Cohen JL, Lasichak LM, Lubetsky MR, Mosley-Williams AD, Granda JL. Does emotional disclosure about stress improve health in rheumatoid arthritis? Randomized, controlled trials of written and spoken disclosure. Pain 2011;152:866–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Keefe FJ, Anderson T, Lumley M, Caldwell D, Stainbrook D, Mckee D, Waters SJ, Connelly M, Affleck G, Pope MS, Weis M, Riordan PA, Uhlin BD. A randomized, controlled trial of emotional disclosure in rheumatoid arthritis: Can clinician assistance enhance the effects? Pain 2008;137:164–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kelley JE, Lumley MA, Leisen JCC. Health effects of emotional disclosure in rheumatoid arthritis patients. Health Psychol 1997;16:331–40. [DOI] [PubMed] [Google Scholar]
- 72.Smyth JM, Stone AA, Hurewitz A, Kaell A. Effects of writing about stressful experiences on symptom reduction in patients with asthma or rheumatoid arthritis: A randomized trial. JAMA 1999;281:1304–9. [DOI] [PubMed] [Google Scholar]
- 73.Broderick JE, Stone AA, Smyth JM, Kaell AT. The feasibility and effectiveness of an expressive writing intervention for rheumatoid arthritis via home-based videotaped instructions. Ann Behav Med 2004;27:50–9. [DOI] [PubMed] [Google Scholar]
- 74.Gillis ME, Lumley MA, Mosley-Williams A, Leisen JCC, Roehrs T. The health effects of at-home written emotional disclosure in fibromyalgia: a randomized trial. Ann Behav Med 2006;32:135–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Broderick JE, Junghaenel DU, Schwartz JE. Written emotional expression produces health benefits in fibromyalgia patients. Psychosom Med 2005;67:326–34. [DOI] [PubMed] [Google Scholar]
- 76.Norman SA, Lumley MA, Dooley JA, Diamond MP. For whom does it work? Moderators of the effects of written emotional disclosure in a randomized trial among women with chronic pelvic pain. Psychosom Med 2004;66:174–83. [DOI] [PubMed] [Google Scholar]
- 77.Graham J, Lobel M, Glass P, Lokshina I. Effects of written anger expression in chronic pain patients: making meaning from pain. J Behav Med 2008;31:201–12. [DOI] [PubMed] [Google Scholar]
- 78.Pepe L, Milani R, Di Trani M, Di Folco G, Lanna V, Solano L. A more global approach to musculoskeletal pain: Expressive writing as an effective adjunct to physiotherapy. Psychol Health Med 2014;19:687–97. [DOI] [PubMed] [Google Scholar]
- 79.Lumley MA, Sklar ER, Carty JN. Emotional disclosure interventions for chronic pain: from the laboratory to the clinic. Translat Behav Med 2012;2:73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gerhardt A, Leisner S, Hartmann M, Janke S, Seidler GH, Eich W, Tesarz J. Eye movement desensitization and reprocessing vs. treatment-as-usual for non-specific chronic back pain patients with psychological trauma: A randomized controlled pilot study. Front Psychiatry 2016;7:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tesarz J, Janke S, Leisner S, Seidler G, Eich W, Gerhardt A. Eye movement desensitization and reprocessing in non-specific chronic back pain: a case series. OA Musculoskel Med 2014;2:20. [Google Scholar]
- 82.Lumley MA, Cohen JL, Stout RL, Neely LC, Sander LM, Burger AJ. An emotional exposure-based treatment of traumatic stress for people with chronic pain: Preliminary results for fibromyalgia syndrome. Psychother Theory Res Prac Train 2008;45:165–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Abbass A Reaching through resistance: Advancing psychotherapy techniques Kansas City, MO: Seven Leaves Press; 2015. [Google Scholar]
- 84.Chavooshi B, Saberi M, Tavallaie SA, Sahraei H. Psychotherapy for medically unexplained pain: a randomized clinical trial comparing intensive short-term dynamic psychotherapy and cognitive-behavior therapy. Psychosom 2017;58:506–18. [DOI] [PubMed] [Google Scholar]
- 85.Chavooshi B, Mohammadkhani P, Dolatshahee B. Efficacy of intensive short-term dynamic psychotherapy for medically unexplained pain: a pilot three-armed randomized controlled trial comparison with mindfulness-based stress reduction. Psychother Psychosom 2016;85:123–5. [DOI] [PubMed] [Google Scholar]
- 86.Baldoni F, Baldaro B, Trombini G. Psychotherapeutic perspectives in urethral syndrome. Stress Med 1995;11:79–84. [Google Scholar]
- 87.Abbass A, Lovas D, Purdy A. Direct diagnosis and management of emotional factors in chronic headache patients. Cephalalgia 2008;28:1305–14. [DOI] [PubMed] [Google Scholar]
- 88.Abbass A Somatization: Diagnosing it sooner through emotion-focused interviewing. J Fam Pract 2005;54:231–9. [PubMed] [Google Scholar]
- 89.Pascual-Leone A, Greenberg LS. Emotional processing in experiential therapy: Why “the only way out is through.” J Consult Clin Psychol 2007;75:875–87. [DOI] [PubMed] [Google Scholar]
- 90.Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behav Ther 2004;35:205–30. [DOI] [PubMed] [Google Scholar]
- 91.Hackmann A Imagery rescripting in posttraumatic stress disorder. Cog Behav Pract 2011;18:424–32. [Google Scholar]
- 92.Lumley MA, Schubiner H, Lockhart NA, Kidwell KM, Harte S, Clauw DJ, Williams DA. Emotional awareness and expression therapy, cognitive-behavioral therapy, and education for fibromyalgia: A cluster-randomized controlled trial. Pain 2017;158:2354–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Thakur ER, Holmes HJ, Lockhart NA, Carty JN, Ziadni MS, Doherty HK, Lackner JM, Schubiner H, Lumley MA. Emotional awareness and expression training improves irritable bowel syndrome: A randomized controlled trial. Neurogastroenterol Motil 2017;12: e13143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Slavin-Spenny O, Lumley M, Thakur E, Nevedal D, Hijazi A. Effects of anger awareness and expression training versus relaxation training on headaches: A randomized trial. Ann Behav Med 2013;46:181–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ziadni MS, Carty JN, Doherty HK, Porcerelli JH, Rapport LJ, Schubiner H, Lumley MA. A life-stress, emotional awareness and expression interview for primary care patients with medically unexplained symptoms: A randomized controlled trial. Health Psychol 2018;37:282–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Carty JN, Ziadni MS, Holmes HJ, Tomakowsky J, Peters K, Schubiner H, Lumley MA. The effects of a life-stress, emotional awareness and expression interview for women with chronic urogenital pain: A randomized controlled trial. Pain Med; in press. [DOI] [PMC free article] [PubMed]
- 97.Abbass A, Schubiner H. Hidden from view. Pleasant Ridge, MI: Psychophysiologic Press; 2018. [Google Scholar]
- 98.Nijs J, Torres-Cueco R, van Wilgen P, Lluch Girbés E, Struyf F, Roussel N, Van Oosterwijck J, Daenen L, Kuppens K, Vanderweeen L, Hemans L, Beckwee D, Voogt L, Clark J, Mononey N, Meeus M. Applying modern pain neuroscience in clinical practice: criteria for the classification of central sensitization pain. Pain Physician 2014;17:447–57. [PubMed] [Google Scholar]
- 99.Williams DA. Phenotypic features of central sensitization. J Appl Biobehav Res 2018;23:e12135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Häuser W, Katz RS, Mease P, Russell AS, Russell IJ, Winfield JB. Fibromyalgia criteria and severity scales for clinical and epidemiological studies: a modification of the ACR preliminary diagnostic criteria for fibromyalgia. J Rheumatol 2011;38:1113–22. [DOI] [PubMed] [Google Scholar]
- 101.Clauw DJ. Fibromyalgia: a clinical review. JAMA 2014;311:1547–55. [DOI] [PubMed] [Google Scholar]
- 102.Mayer TG, Neblett R, Cohen H, Howard KJ, Choi YH, Williams MJ, Perez Y, Gatchel RJ. The development and psychometric validation of the Central Sensitization Inventory. Pain Practice 2012;12:276–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Falk EB, O’Donnell MB, Cascio CN, Tinney F, Kang Y, Lieberman MD, Taylor SE, An L, Resnicow K, Strecher VJ. Self-affirmation alters the brain’s response to health messages and subsequent behavior change. Proc Natl Acad Sci 2015;112:1977–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Clarke DD. They can’t find anything wrong! 7 Keys to understanding, treating, and healing stress illness Boulder, CO: Sentient Publications; 2007. [Google Scholar]
- 105.Oldfield G Chronic pain: your key to recovery Bloomington, IN: AuthorHouse UK Ltd.; 2014. [Google Scholar]


