Abstract
Study Objective
To study the variation in opioid prescribing among emergency physicians and facilities for discharged adult ED patients.
Methods
We conducted a retrospective analysis of ED visits from five U.S. hospitals between January and May 2014 using records from Data to Intelligence (D2i). We examined physician- and facility-level variation in opioid prescription rates for discharged ED patients. We calculated unadjusted opioid prescription rates at the physician and facility levels and used a multivariable mixed-effect logistic regression model to examine within-facility physician variation in opioid prescription adjusting for patient and situational factors including time of presentation, ED census, and physician workload.
Results
In 47,304 visits across five EDs, median patient age was 40 years old (IQR 28,55), and 89% had some form of insurance. There were 17,098 (36%) ED discharges with at least one opioid prescription. The unadjusted facility-level opioid prescription rate ranged from 24%-46%. Among 253 ED physicians, the adjusted opioid prescription rate varied from 22%-76%. Increased physician workload is related to decreased odds of opioid prescription at ED discharge for the lowest (<3 patients) and moderate (6-9 patients) physician workload levels, while the association weakened with increasing levels of workload.
Conclusion
There was substantial physician and facility variation in opioid prescription for discharged adult ED patients. Emergency physicians were less likely to prescribe opioids when their workload was lower, and this effect diminished at high workload levels. Understanding situational and other factors that explain this variation is important given the rising U.S. opioid epidemic and the need for urgent intervention.
INTRODUCTION
Background
Over the past decade, there have been dramatic increases in opioid prescriptions filled in U.S. pharmacies: 259 million such prescriptions were filled in 2012, compared with 174 million in 2001.1 Increased prescribing is a primary source of opioid abuse, and rising mortality from opioid overdoses, leading to what has been termed “the U.S. opioid epidemic”.2-4 Despite efforts to reduce opioid prescribing, the amount of prescribed opioids is still relatively high over time, and there is substantial variation throughout the U.S.5
Increases in opioid prescribing have mirrored higher opioid administration and prescribing in U.S. EDs. EDs are a common location for patients obtaining prescriptions for opioids as six out of the top ten reasons for visiting EDs are for pain-related complaints.6,7 Among Medicare beneficiaries, emergency medicine physicians are one of the most common specialties to prescribe opioids,6 and prescription rates can vary widely. In 2010, 31% of ED visits involved an opioid medication being administered or prescribed compared to 21% in 2001.8,9 These visits can have long lasting effects among patients who have never taken opioids; opioid initiation in the ED increases the likelihood of recurrent use in the next year by 80%,10 and may contribute to long-term dependence.11,12 However, on the whole, emergency physicians prescribe fewer opioids than other clinical specialties.7,10
Importance
Studies have demonstrated up to 3-fold state-level variation in opioid prescribing with higher prescribing in Appalachia and in Southern and Western states, and in rural areas.1,13-15 Variation has been demonstrated for hospital-level opioid prescribing and physician-level variation in prescribing by outpatient providers.16-18 A single-center study has reported provider-level variation in opioid prescribing among 21 ED physicians.19 However, no studies, to our knowledge, have explored the impact of situational factors, such as physician workload or ED crowding. While the relationship between ED crowding and diminished emergency care quality has been extensively studied,20 physician workload may also be meaningful. Research from the field of operations management has found that increased multitasking and increasing workload may have adverse consequences for clinical performance,21 and quality of care provided.22
Goals of This Investigation
We evaluated the variation in opioid prescribing from a sample of U.S. emergency physicians in five hospitals. We hypothesized that there would be large variation in opioid prescribing across physicians and EDs, and that situational factors such as physician workload or ED crowding would explain some of the variation.
MATERIALS AND METHODS
Study Design, Data Source and Data Selection
We conducted a retrospective cohort study using a dataset from Data to Intelligence (D2i). D2i is a healthcare analytics company that aggregates electronic health record (EHR) data from more than 20 EDs in the U.S. and includes data on patient demographics, ED flow including timestamps and disposition, medications administered and prescribed, radiographic imaging, and laboratory testing.
We included five EDs (four in Michigan; one in Connecticut) which had patient demographic, operational, and medication prescribing data available for these sites. We included adult ED discharges (patient age ≥18 years old) between January 1, 2014 and May 31, 2014 who were seen by a unique attending emergency physician with at least 50 discharged patients during this time period. We selected 50 visits as a cutoff to ensure a sufficient sample of visits to represent a physician’s opioid prescribing pattern. Patient visits were excluded if demographic, date of service/discharge, pharmaceutical prescribing data, or attending emergency physician identifiers were missing. This study was approved by the Vanderbilt University Medical Center Institutional Review Board.
Emergency Physician Identification
We used the emergency physician attending of record within the EHR at time of ED visit discharge as the prescribing physician for each facility. Visits in which a physician’s identifier was missing or did not identify a specific physician were not included in the analysis.
Opioid Prescription
The prescription of an opioid at ED discharge was our primary outcome. We determined that an opioid prescription was given if the patient’s disposition status was “discharged” at the end of an ED visit, a prescription was provided as part of the visit, and the prescription for at least one opioid medication was documented. The following medications were defined as opioids: codeine, fentanyl, hydrocodone, hydromorphone, meperidine, methadone, morphine, oxycodone, and tramadol. Since quantity and dose of opioid were not available in this dataset, our primary outcome was whether any opioid was prescribed. We also report the number of opioid prescriptions in our unadjusted results.
Situational Factors
Considering that ED crowding and physician workload can affect the quality and efficiency of care provided in the ED,20,21,23 we included these variables in our models to evaluate their potential effect on our results. ED census and physician workload at patient discharge were calculated for each visit using a counting algorithm based on the ED arrival and discharge times prior to applying the exclusion criteria for our study. Census counts were calculated as a proportion to account for differing sizes of EDs and was defined as the proportion of ED beds filled relative to the size of the ED when the current patient was discharged. Physician workload at discharge was the total number of patients an attending physician was the attending of record for when a given patient was discharged.
Chief Complaints
We used the presenting chief complaint for each visit. Since these complaints were not standardized across sites and were frequently presented as free text, two of the authors (AP, MJW) who are emergency physicians, created standardized categories of chief complaints. Every visit was reviewed by one of the reviewers and assigned a chief complaint category and set to ‘other’ if the category could not be determined, or ‘unknown if no value was present. A 10% sample of category assignments was reviewed by both reviewers. Disagreements were resolved by a third reviewer (JMP).
Other Patient Characteristics
In addition to patient sex and age, we also included the following primary insurance categories: government, private, other responsibility (e.g., military), uninsured, or unknown. We also included the initial emergency severity index triage acuity score, and time of ED arrival in 6 hour blocks (midnight to 6AM, 6AM to noon, noon to 6PM, and 6PM to midnight).
Statistical Analysis
Descriptive statistics by facility and overall for situational factors and demographic characteristics were provided using median (Interquartile Range [IQR]) for continuous variables and frequency (percentage) for categorical variables. Unadjusted tests of associations between opioid prescription status and these variables were conducted using Wilcoxon rank-sum test for continuous variables and Chi-square test for categorical variables with significant threshold at 0.05. The unadjusted physician-level opioid prescription rates were calculated as the total number of visits receiving opioid prescription divided by the number of visits seen by the same physician.
The association of situational factors and receipt of an opioid prescription at ED discharge was evaluated using a multivariable mixed-effect logistic regression model with opioid prescription status as the outcome, situational factors including (1) physician workload at the time of patient discharge and (2) proportion of filled ED beds at the time of patient discharge as key independent variables of interests, and physician nested within ED as the random effect. Due to the limited number of EDs (i.e. five EDs) in the dataset, we did a sensitivity analysis in which ED was included as a fixed effect and physician as a random effect. Potential confounders included as covariates were: 1) patient age; 2) triage acuity (Emergency Severity Index); 3) patient sex (ref=Male); 4) insurance status (government [ref], private, other, uninsured, and unknown); 5) chief complaint (standardized to 18 categories with gastroenterology as the reference); and 6) time of initial ED presentation in 6 hour blocks (6AM-12PM; 12PM-6PM [ref]; 6PM-midnight; midnight-6AM). Continuous variables were fit with piecewise linear splines (i.e. age, physician workload, and ED census at discharge) with the corresponding quartiles as knots to allow for non-linear effects.24 Odds ratios (OR) and the corresponding 95% confidence intervals were reported for situational factors and adjusting covariates. The adjusted physician-level and facility-level opioid prescription rates were calculated using empirical Bayes (EB) estimates25 of the corresponding physician and facility random effects at the modal value of categorical covariates and mean value of continuous covariates. The corresponding 95% confidence intervals (Cl) are provided as well. Caterpillar plots of the EB estimates of adjusted physician-level prescription rates are provided for each facility to visually assess different sources of variation in opioid prescription. Finally, to compare the variations explained by physicians and facilities, we calculated the intraclass correlation coefficients for physicians and facilities using the threshold technique that is appropriate for binary outcomes.26 Statistical analyses were conducted using R 3.4.2 and SAS Studio, Version 3.6.
RESULTS
Visit Characteristics
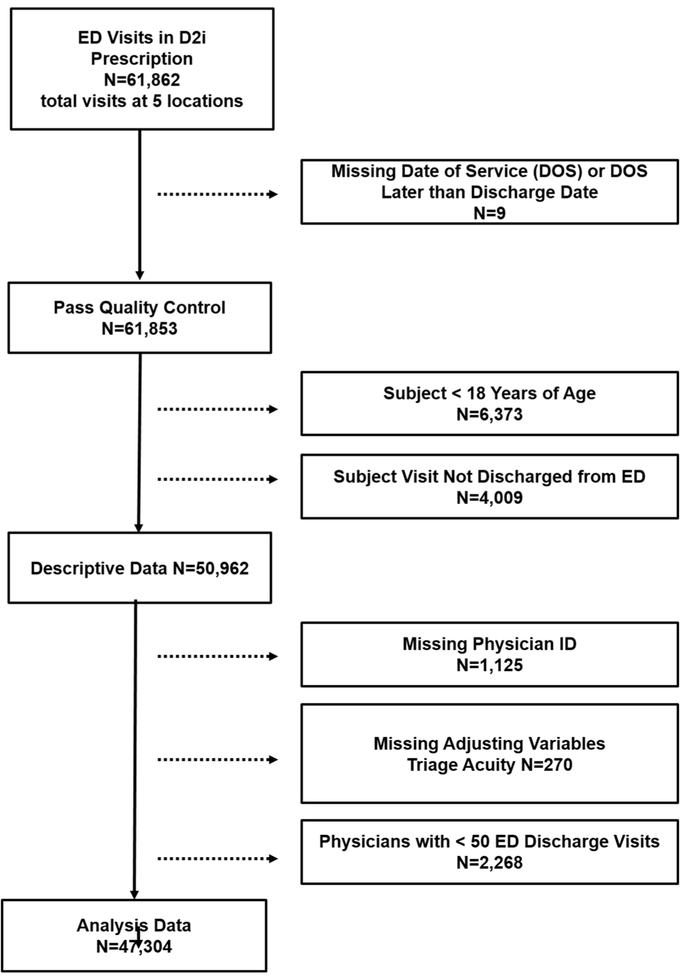
A total of 61,862 visits had prescription data with 47,304 visits from five EDs that met our inclusion criteria (Figure 1). Facilities were exclusively urban and not-for-profit, however, they varied in size, academic status, and facility capabilities (i.e., trauma center, and percutaneous coronary intervention capability; Table 1). Visit characteristics by site (Table 2) are provided. Visits that met inclusion criteria were more often for females, patients with a median age of 40 (IQR 28, 55) years old, patients triaged with an ESI acuity level of 3, and patients presenting between 12pm and 6pm. Most patients had government insurance followed by private, unknown, and no insurance. Physicians prescribed an opioid for 36% of all discharged ED visits. Hydrocodone was most frequently prescribed (59% of visits where an opioid was prescribed) followed by oxycodone (19% of opioid visits). However, these frequencies varied by facility as oxycodone was the most frequently prescribed opioid at two facilities.
Figure 1.
Flow chart of patients who met inclusion/exclusion criteria for the study population. Note: Some cases may have been excluded for more than 1 reason.
Table 1.
Descriptors of the five emergency departments included.
| Facility | State | Urban/Rural | ED Beds | Total Inpatient Beds |
For Profit Status |
Emergency Medicine Residency Program |
Trauma Center |
Percutaneous Coronary Intervention Center |
|---|---|---|---|---|---|---|---|---|
| 1 | CT | Urban | 100 | 800-900 | Not-For-Profit | Yes | Yes | Yes |
| 2 | MI | Urban | 40 | 200-300 | Not-For-Profit | Yes | No | Yes |
| 3 | MI | Urban | 30 | 300-400 | Not-For-Profit | No | No | No |
| 4 | MI | Urban | 80 | 600-700 | Not-For-Profit | Yes | Yes | No |
| 5 | MI | Urban | 50 | 200-300 | Not-For-Profit | No | No | No |
Table 2.
ED visit characteristics by site and overall excluding those with physicians having < 50 visits.
| Facility 1 | Facility 2 | Facility 3 | Facility 4 | Facility 5 | Combined | ||||
|---|---|---|---|---|---|---|---|---|---|
| N=13855 | N=10362 | N=8137 | N=4047 | N=10903 | N=47304 | ||||
| Patient sex : Female | 58% (8085) | 62% (6404) | 68% (5528) | 58% (2334) | 60% (6554) | 61% (28905) | |||
| Patient age, years (IQR) | 39 (28,52) | 43 (29,59) | 40 (26,55) | 44 (31,58) | 39 (27,55) | 40 (28,55) | |||
| Triage acuity, % (N) | |||||||||
| 1 | 0% (5) | 0% (5) | 0% (0) | 0% (18) | 0% (14) | 0% (42) | |||
| 2 | 13% (1755) | 8% (823) | 1% (88) | 7% (278) | 3% (318) | 7% (3262) | |||
| 3 | 43% (5901) | 63% (6562) | 53% (4327) | 66% (2655) | 70% (7671) | 57% (27116) | |||
| 4 | 37% (5173) | 24% (2466) | 42% (3395) | 26% (1035) | 25% (2731) | 31% (14800) | |||
| 5 | 7% (1021) | 5% (506) | 4% (327) | 2% (61) | 2% (169) | 4% (2084) | |||
| Time of service, % (N) | |||||||||
| 6AM-12PM | 33% (4574) | 26% (2739) | 24% (1938) | 26% (1060) | 25% (2713) | 28% (13024) | |||
| 12PM-6PM | 36% (4998) | 36% (3711) | 35% (2860) | 34% (1372) | 36% (3903) | 36% (16844) | |||
| 6PM-MN | 22% (3105) | 27% (2838) | 30% (2437) | 29% (1188) | 29% (3122) | 27% (12690) | |||
| MN-6AM | 9% (1178) | 10% (1074) | 11% (902) | 11% (427) | 11% (1165) | 10% (4746) | |||
| Patient insurance status, % (N) | |||||||||
| Government | 67% (9304) | 53% (5503) | 27% (2207) | 18% (730) | 31% (3331) | 45% (21075) | |||
| Private | 20% (2729) | 18% (1826) | 26% (2151) | 42% (1700) | 35% (3868) | 26% (12274) | |||
| Unknown | 11% (1514) | 11% (1168) | 30% (2434) | 28% (1117) | 14% (1543) | 16% (7776) | |||
| Uninsured | 2% (284) | 15% (1507) | 16% (1331) | 12% (484) | 16% (1698) | 11% (5304) | |||
| Other | 0% (24) | 3% (358) | 0% (14) | 0% (16) | 4% (463) | 2% (875) | |||
| Standardized chief complaint, % (N) | |||||||||
| Unknown | 2% (241) | 2% (245) | 34% (2770) | 60% (2421) | 24% (2626) | 18% (8303) | |||
| Musculoskeletal | 21% (2910) | 16% (1678) | 13% (1030) | 8% (321) | 18% (1966) | 17% (7905) | |||
| Ophthalmological | 17% (2291) | 20% (2068) | 9% (723) | 5% (207) | 14% (1530) | 14% (6819) | |||
| Trauma | 8% (1146) | 9% (952) | 7% (586) | 6% (223) | 7% (794) | 8% (3701) | |||
| Respiratory | 6% (893) | 9% (887) | 5% (428) | 3% (111) | 5% (510) | 6% (2829) | |||
| Gastrointestinal | 5% (726) | 9% (951) | 7% (554) | 3% (137) | 5% (590) | 6% (2958) | |||
| Neurological | 5% (675) | 8% (781) | 5% (400) | 3% (127) | 5% (573) | 5% (2556) | |||
| Systemic | 8% (1098) | 4% (383) | 3% (215) | 0% (1) | 2% (261) | 4% (1958) | |||
| Dermatological | 6% (847) | 6% (665) | 4% (341) | 2% (93) | 5% (594) | 5% (2540) | |||
| Multiple Complaints | 5% (703) | 0% (10) | 2% (157) | 3% (104) | 2% (225) | 3% (1199) | |||
| OB/GYN, GU | 2% (314) | 3% (283) | 3% (253) | 2% (88) | 2% (244) | 2% (1182) | |||
| Renal | 4% (568) | 3% (334) | 1% (105) | 0% (11) | 2% (246) | 3% (1264) | |||
| Cardiovascular | 4% (576) | 3% (332) | 3% (253) | 2% (83) | 2% (261) | 3% (1505) | |||
| Ear, Nose, and Throat | 1% (150) | 1% (109) | 1% (42) | 0% (8) | 1% (60) | 1% (369) | |||
| Other | 3% (360) | 1% (110) | 1% (97) | 1% (36) | 1% (99) | 1% (702) | |||
| Psychiatric | 1% (142) | 2% (234) | 1% (42) | 0% (17) | 1% (147) | 1% (582) | |||
| Lacs and Bites | 1% (174) | 2% (230) | 0% (40) | 1% (29) | 1% (124) | 1% (597) | |||
| Heme_Endo_Tox | 0% (41) | 1% (110) | 1% (101) | 1% (30) | 0% (53) | 1% (335) | |||
| ED census, proportion of ED beds (IQR) | 77 (62,91) | 20 (14,25) | 31 (23,40) | 20 (14,27) | 56 (44,66) | 41 (23,67) | |||
| Physician workload, median num. patients (IQR) | 4 (2,9) | 4 (2,7) | 6 (3,8) | 6 (4,8) | 9 (6,15) | 6 (3,10) | |||
| Opioid prescribed at discharge, % (N) | 24% (3310) | 47% (4863) | 29% (2389) | 38% (1519) | 46% (5017) | 36% (17098) | |||
Unadjusted Facility- and Physician-Level Prescription Rates
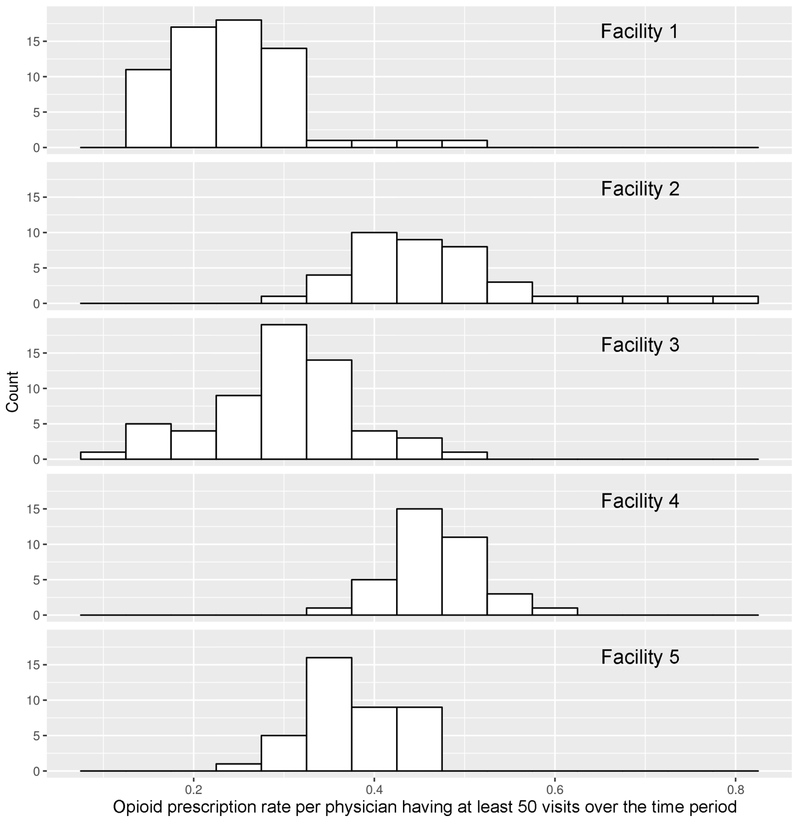
Facility-level unadjusted opioid prescription rate ranged from a low of 24% at Facility 1 up to 47% at Facility 2. There were 63, 26, 36, 43, and 26 physicians included at each facility, respectively. By facility, the range of unadjusted physician-level opioid prescription rates were as follows: Facility 1 (32%, 69%), Facility 2 (40%, 79%), Facility 3 (22%, 69%), Facility 4 (39%, 62%), and Facility 5 (41%, 58%). Unadjusted physician-level opioid prescription rates by facility are illustrated in Figure 2.
Figure 2.
Unadjusted physician opioid prescription rates by facility.
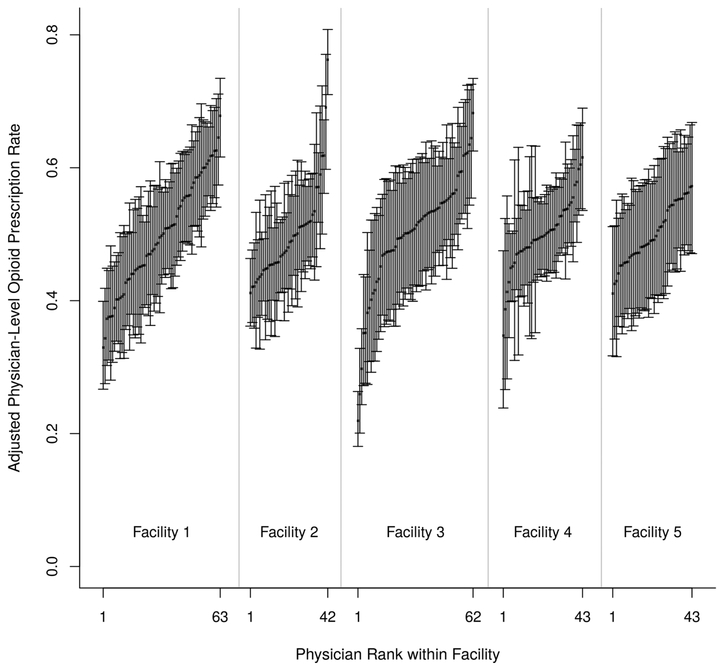
Adjusted Facility- and Physician-Level Prescription Rates
After adjusting for patient demographics (age, sex), insurance status, triage acuity, chief complaint, timing of arrival, facilities, and situational factors (physician workload and ED census), we found wide variation in physician prescribing within and between facilities (Figure 3). There were some physicians who prescribed opioids at much higher rates than is common for the facility. The adjusted physician opioid prescription rate ranged from 22% to 76%. Ranges of the adjusted physician-level opioid prescription rates were as follows: Facility 1 (33%, 68%), Facility 2 (41%, 76%), Facility 3 (22%, 68%), Facility 4 (41%, 57%), and Facility 5 (35%, 62%). The adjusted facility prescription rates ranged from 34% to 67%.
Figure 3.
Adjusted physician-level opioid prescription rates by physician workload levels for each facility.
Adjusted Results
Full results of the adjusted odds ratios are reported in Table 3. Among situational factors, we found that the effect of physician workload on opioid prescribing was nonlinear. At low physician workloads (< 3 patients, the 1st quartile), a single patient increase in a physician’s workload was associated with an 8.4% (adjusted odds ratio [aOR] 0.92 95% CI 0.89, 0.95, p<0.001) reduction in the odds of prescribing opioids at ED discharge. At higher physician workload levels, (6-9 patients, the 3rd quartile), a single patient increase in the physician’s workload was associated with only a 2.3% (aOR 0.98, 95% CI 0.96, 1.00, p=0.03) reduction in the odds of prescribing opioids. At the highest physician workload levels (≥10 patients, the 4th quartile), increased physician work load might lead to increased odds of opioid prescribing although the effect is not significant at the 0.05 significance level (aOR 1.01, 95% CI 1.00, 1.02, p=0.09). Overall ED patient census affected prescription rates when the proportion of ED beds occupied at patient discharge was in the second quartile, 44.9% to 61.9% (aOR 1.93, 95% CI 1.16, 3.19, p=0.01), which indicates a 10% increase in ED bed occupancy was associated with a 6.8% increased odds of opioid prescription.
Table 3.
Odds of physician prescribing opioids at ED discharge by variable for physicians with ≥ 50 visits.
| Variable | Adjusted Odds Ratio |
Lower CI | Upper CI | P Value |
|---|---|---|---|---|
| Physician workload, num. patients | ||||
| 0-2 | 0.92 | 0.89 | 0.95 | <0.0001 |
| 3-5 | 0.99 | 0.96 | 1.02 | 0.4255 |
| 6-9 | 0.98 | 0.96 | 1.00 | 0.0256 |
| ≥ 10 | 1.01 | 1.00 | 1.02 | 0.0851 |
| ED census, proportion of ED beds | ||||
| 0-0.449 | 1.23 | 0.82 | 1.84 | 0.3224 |
| 0.449-0.619 | 1.93 | 1.16 | 3.19 | 0.0108 |
| 0.619-0.792 | 0.81 | 0.49 | 1.33 | 0.3969 |
| ≥ 0.792 | 1.19 | 0.81 | 1.75 | 0.3727 |
| Patient Age, years | ||||
| 18-27 | 1.09 | 1.08 | 1.11 | <0.0001 |
| 28-39 | 1.02 | 1.02 | 1.03 | <0.0001 |
| 40-54 | 1.08 | 1.00 | 1.01 | 0.0052 |
| ≥55 | 0.97 | 0.97 | 0.98 | <0.0001 |
| Triage acuity | 0.88 | 0.85 | 0.92 | <0.001 |
| Female Sex (ref=M) | 0.97 | 0.93 | 1.00 | 0.10 |
| Insurance | ||||
| Government | reference | |||
| Other | 1.09 | 0.93 | 1.27 | 0.2958 |
| Uninsured | 0.96 | 0.89 | 1.04 | 0.3100 |
| Private | 0.92 | 0.87 | 0.97 | 0.0031 |
| Unknown | 0.87 | 0.80 | 0.94 | 0.0005 |
| Chief complaint | ||||
| Gastrointestinal | reference | |||
| Musculoskeletal | 3.21 | 2.98 | 3.47 | <0.0001 |
| Trauma | 2.74 | 2.50 | 3.00 | <0.0001 |
| Ear, Nose, and Throat | 2.07 | 1.86 | 2.30 | <0.0001 |
| Unknown | 1.25 | 1.16 | 1.36 | <0.0001 |
| Renal | 1.70 | 1.49 | 1.94 | <0.0001 |
| Other | 1.26 | 1.05 | 1.50 | 0.0117 |
| Lacs and bites | 0.94 | 0.78 | 1.14 | 0.5348 |
| Dermatological | 0.93 | 0.81 | 1.07 | 0.2875 |
| Heme, Endo, Tox | 0.87 | 0.69 | 1.11 | 0.2672 |
| Ob, Male GU, Gyn | 0.84 | 0.72 | 0.97 | 0.0189 |
| Cardiovascular | 0.66 | 0.60 | 0.73 | <0.0001 |
| Systemic | 0.55 | 0.48 | 0.63 | <0.0001 |
| Ophthalmological | 0.53 | 0.40 | 0.70 | <0.0001 |
| Multiple complaints | 0.50 | 0.42 | 0.60 | <0.0001 |
| Neurological | 0.45 | 0.40 | 0.51 | <0.0001 |
| Respiratory | 0.27 | 0.23 | 0.30 | <0.0001 |
| Psychiatric | 0.14 | 0.10 | 0.18 | <0.0001 |
| Hour of day | ||||
| 12PM-6PM | reference | |||
| 6PM-MN | 1.13 | 1.03 | 1.24 | 0.0126 |
| MN-6AM | 0.99 | 0.94 | 1.05 | 0.7561 |
| 6AM-12PM | 1.05 | 0.99 | 1.11 | 0.1159 |
For the remaining adjusting variables, among patients less than 55 years old, increasing age was associated with a higher likelihood to prescribe opioids at ED discharge. However, the amount of increase diminished with increased age. Less severe triage acuity (e.g., higher number) and private insurance status (compared to government) were associated with reduced odds of opioid prescription. However, arrival to the ED between 6PM and midnight (compared to 12PM – 6PM) was associated with increased odds of opioid prescription. Chief complaints had a variable effect on the odds of opioid prescription when compared with GI complaints with psychiatric complaints having the lowest odds of prescription, and musculoskeletal complaints having the highest odds of prescription. Patient sex did not affect the odds of opioid prescribing at discharge.
Facilities also affected the likelihood of opioid prescriptions at discharge. After adjusting for patient characteristics, 17% of the variance in opioid prescription was attributable to the facility (ICC=17%) and 27% of the variance was attributable to physicians (ICC=27%).Variations attributable to physicians were approximately 1.6 times the variations attributable to the facilities. Sensitivity analyses using the ED as a fixed effect found no difference in our results.
DISCUSSION
In this study, we have two key findings. First, we found a nearly two-fold variation in facility prescribing rates for opioids in discharged ED patients across five EDs. Second, situational factors involving the physician workload, but not broader environmental conditions (e.g., ED census) are more likely to impact prescription of an opioid at discharge.
Several factors may explain the observed prescribing variation. First, regional variation in prescribing practices likely exist. Four of the five facilities are in Michigan, and three of these are within a maximum of 30 miles of each other. In the sample, the lowest prescribing rate was seen in the one ED in Connecticut. Connecticut is in the 2nd lowest quartile of opioid prescriptions per 100 people compared with Michigan which is in the highest.1 Substantial interstate variation may exist due to variation in state-level policies, such as state-run prescription drug monitoring databases (PDMPs) which track controlled substances prescriptions, and how they are mandated to be used.27 However, our study also demonstrates that intra-state variation (i.e., within Michigan) also exists. This may be due to regional variation in patient populations, but also facility variation in the culture and attitudes towards opioid prescribing, local strategies to address opioid prescriptions such as the use of prescription drug monitoring programs (PDMPs),28 or how PDMPs are integrated into the electronic health records.29
We also found that even within the same facility, substantial physician variation exists. We suspect that this within-facility variation may be due to differences in training, personal attitudes toward the benefits and risks of opioids, and the way that individual physicians may respond to patient requests for specific medications. However, limited data on provider-level characteristics were available to be able to examine these relationships.
Our analysis also demonstrated that situational factors can also influence an emergency physician’s likelihood of prescribing an opioid at discharge. Specifically, we examined physician workload and ED census at patient discharge. Physician workload measured the number of patients for which the physician was the attending of record whereas ED census measured the proportion of ED beds occupied at the time of discharge. Among these two factors, low and moderate levels of physician workload affected the prescription of opioids at discharge by reducing the likelihood of prescription as workload increased, and only moderate levels of ED bed occupancy level affected the prescription of opioids by increasing likelihood of prescription with increased ED congestion. Although our findings are only significant at the 1st and 3rd quartiles, the “protective” nature of low workload diminishes as levels increase until it is gone by the highest level of workload and is no longer significant.
We suspect that this finding occurred because the decision to prescribe an opioid is a physician-dependent decision. How busy the physician is at the time of prescription decision likely has a larger effect compared with how congested the overall ED is at the time of discharge. For example, a physician that has recently arrived for a shift in a very busy ED, may be more likely to be influenced by their individual workload rather than the overall environmental conditions. Cognitive psychology provides insight into this finding and suggests that stress sometimes results in sub-optimal decision-making.30 In fact, recent work on other emergency physician decisions, such as whether to admit a patient to the hospital, was similarly influenced by working conditions.23 Unlike Gorski’s finding in which both physician workload and waiting room census influenced physician decision-making, the ED’s environmental conditions (i.e., census) was only significant at moderate ED congestion levels. This suggests that a decision to admit a patient to the hospital considers a broader set of operating conditions for a patient who will stay as an inpatient in the hospital compared with a patient who will be discharged home. Instead, the decision to prescribe a medication is more dependent upon the physician and their cognitive load at the time of the decision. In addition, our findings differ from prior work that examined the impact of ED crowding and census on opioid administration and prescriptions in the ED.31,32 Differential effects in different time periods may suggest that context-dependent prescribing decisions by physicians today have changed, due to changes in practice or increasing concerns about the dangers of opioids as well as available information. Specifically, in today’s practice of emergency care we suspect that at low to moderate workload levels, when a physician’s workload is more manageable, increased workload is associated with reduced odds of prescription because providers tend to be more conservative and may still have the time to review a PDMP, or to discuss with patients why an opioid is not being prescribed, potential non-opioid alternatives.
Our findings suggest that there are several broad directions to approach reducing opioid prescriptions. First and foremost, physicians may need better education about the benefits and risk of opioid prescribing in the setting of higher workloads. Second, emergency physician groups such as the American College of Emergency Physicians, need updated guidelines incorporating the latest evidence to guide emergency physicians. Despite the increased focus on opioid prescribing, the latest clinical policy is from 2012.33 Additionally, while emergency physicians are more likely to adhere to the 2016 CDC guidelines for prescribing opioids,34 understanding the factors that influence prescribing are needed. State-level or city-level policies such as mandating the use of PDMPs, can facilitate sharing of information among EDs to identify prior and existing controlled substance use by patients.35,36 However, automated use of PDMPs may not curb opioid prescribing.37 Finally, facility-level policies can also be a way to disseminate and implement national guidelines by addressing nuances not covered by regional or national policies. For example, St. Joseph’s hospital in Patterson, NJ has developed specific protocols for use in the ED that focus on lowering the use of opioids.38 Facilities can also evaluate their own prescribing behaviors, identify outlier physicians, offer feedback, and deliver education about strategies to reduce opioid prescriptions. For example, one facility in Boston implemented a quality improvement initiative of sharing prescriber rates and providing feedback, which reduced opioid prescription rates by 60%.39
LIMITATIONS
There are several study limitations. First, we used a secondary, retrospective dataset from 2014 to conduct this analysis. The use of retrospective data prohibits the review of individual patient charts and the acquisition of data on the quantity of pills, thestrength of each medication, and characteristics of prescribing physicians. While the scrutiny on opioid prescribing has increased since 2014, this work provides a novel insight on the role of situational factors in opioid prescribing. Second, on average, prescription rates for these five EDs were higher than prior studies. Though the average prescription rate was 36% across all facilities in this study, prior work has found that some average prescription rates were as high as 31% at the facility-level,8 and up to 35% for injury-related complaints.11 Other studies have found comparable degrees of variability among prescribing in the ED.40 Third, this analysis focused on opioid prescriptions at discharge and did not include the administration and dose of opioids (either intravenously or orally) during each patient’s ED visit, nor the quantity of opioid prescribed. Fourth, standardization was required considering the use of free text chief complaints across five facilities. This lack of standardization could have resulted in a nondifferential misclassification bias which could underestimate the relationship between our exposure variables and the prescription of an opioid. To minimize this bias, we developed a classification scheme for each variable which was adjudicated by a third reviewer. The primary outcome, receipt of opioid, had less risk for misclassification considering an established classification system for opioid types already exists. Fifth, while we accounted for physician census, we do not know how actively engaged each physician was with each patient. We only knew that the patient was still recorded as being located within the ED and that the assigned physician was the attending of record. For example, if the patient was admitted with no active issues requiring the emergency physician, this might falsely elevate the physician workload compared with fewer patients for another physician whom are all active. Even if these patients were admitted, institutional policies may vary by facility influencing how long each patient is in the ED after admission and each physician’s level of engagement. Nonetheless, we used this approach for all physicians across the five EDs. Finally, there may be unmeasured confounders (e.g., pain scores, clinical presentation) that we did not account for in this analysis which may affect a physician’s decision to prescribe an opioid.
CONCLUSION
Substantial variation exists both within and between facilities in opioid prescription for discharged ED patients in this sample. Emergency physicians were more conservative with opioid prescribing when their workload was lower, and this diminished at high workload levels. A concerted approach at both the facility- and regional levels is needed to reduce variation in ED opioid prescribing.
Acknowledgments
Funding Sources: Research reported in this publication was supported by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number K23HL127130. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Study concept and design: Ward, Pines, KC, Liu.
Acquisition, analysis, or interpretation of data: Ward, Pines, KC, Liu, Jenkins, Padaki
Drafting of the manuscript: Ward, Jenkins, Liu.
Critical revision of the manuscript for important intellectual content: Ward, Pines, KC, Liu, Jenkins, Padaki.
Statistical analysis: Jenkins, Liu.
Obtained funding: Ward
Administrative, technical, or material support: Ward. Study supervision: Ward, Pines, Liu.
Contributor Information
Michael J. Ward, Department of Emergency Medicine, Vanderbilt University School of Medicine.
Diwas KC, Information Systems & Operations Management, Goizueta Business School, Emory University.
Cathy A. Jenkins, Department of Biostatistics, Vanderbilt University School of Medicine.
Dandan Liu, Department of Biostatistics, Vanderbilt University School of Medicine.
Amit Padaki, Department of Emergency Medicine, Christiana Care Health System.
Jesse M. Pines, Departments of Emergency Medicine and Health Policy & Management, George Washington University School of Medicine and Health Sciences.
REFERENCES
- 1.Opioid Painkiller Prescribing: Where You Live Makes a Difference. . http://www.cdc.gov/vitalsigns/opioid-prescribing/. Accessed October 6, 2017.
- 2.Bohnert AS, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315–1321. [DOI] [PubMed] [Google Scholar]
- 3.Okie S A flood of opioids, a rising tide of deaths. N Engl J Med. 2010;363(21):1981–1985. [DOI] [PubMed] [Google Scholar]
- 4.Paulozzi LJ, Budnitz DS, Xi Y. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Saf. 2006;15(9):618–627. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control. National Hospital Ambulatory Medical Care Survey: 2011 Emergency Department Summary Tables. . http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2011_ed_web_tables.pdf.
- 6.Chen JH, Humphreys K, Shah NH, Lembke A. Distribution of Opioids by Different Types of Medicare Prescribers. JAMA Intern Med. 2016;176(2):259–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoppe JA, Nelson LS, Perrone J, Weiner SG, Prescribing Opioids Safely in the Emergency Department Study I, Prescribing Opioids Safely in the Emergency Department PSI. Opioid Prescribing in a Cross Section of US Emergency Departments. Ann Emerg Med. 2015;66(3):253–259 e251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mazer-Amirshahi M, Mullins PM, Rasooly I, van den Anker J, Pines JM. Rising opioid prescribing in adult U.S. emergency department visits: 2001–2010. Acad Emerg Med.2014;21(3):236–243. [DOI] [PubMed] [Google Scholar]
- 9.Mazer-Amirshahi M, Mullins PM, Rasooly IR, van den Anker J, Pines JM. Trends in prescription opioid use in pediatric emergency department patients. Pediatr Emerg Care. 2014;30(4):230–235. [DOI] [PubMed] [Google Scholar]
- 10.Hoppe JA, Kim H, Heard K. Association of emergency department opioid initiation with recurrent opioid use. Ann Emerg Med. 2015;65(5):493–499 e494. [DOI] [PubMed] [Google Scholar]
- 11.Barnett ML, Olenksi AR, Jena AB. Opioid Prescribing by Emergency Physicians and Risk of Long-Term Use. N Engl J Med. 2017;376(19):1896. [DOI] [PubMed] [Google Scholar]
- 12.Butler MM, Ancona RM, Beauchamp GA, et al. Emergency Department Prescription Opioids as an Initial Exposure Preceding Addiction. Ann Emerg Med. 2016;68(2):202–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McDonald DC, Carlson K, Izrael D. Geographic variation in opioid prescribing in the U.S. J Pain. 2012;13(10):988–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paulozzi LJ, Mack KA, Hockenberry JM. Vital signs: variation among states in prescribing of opioid pain relievers and benzodiazepines—United States, 2012. MMWR Morb Mortal Wkly Rep. 2014;63(26):563–568. [PMC free article] [PubMed] [Google Scholar]
- 15.Prunuske JP, St Hill CA, Hager KD, et al. Opioid prescribing patterns for non-malignant chronic pain for rural versus non-rural US adults: a population-based study using 2010 NAMCS data. BMC Health Serv Res. 2014;14:563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dhalla IA, Mamdani MM, Gomes T, Juurlink DN. Clustering of opioid prescribing and opioid-related mortality among family physicians in Ontario. Can Fam Physician.2011;57(3):e92–96. [PMC free article] [PubMed] [Google Scholar]
- 17.Herzig SJ, Rothberg MB, Cheung M, Ngo LH, Marcantonio ER. Opioid utilization and opioid-related adverse events in nonsurgical patients in US hospitals. J Hosp Med. 2014;9(2):73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Womer J, Zhong W, Kraemer FW, et al. Variation of opioid use in pediatric inpatients across hospitals in the U.S. J Pain Symptom Manage. 2014;48(5):903–914. [DOI] [PubMed] [Google Scholar]
- 19.Smulowitz PB, Cary C, Boyle KL, Novack V, Jagminas L. Variation in opioid prescribing patterns between ED providers. Intern Emerg Med. 2016;11(8):1121–1124. [DOI] [PubMed] [Google Scholar]
- 20.Bernstein SL, Aronsky D, Duseja R, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16(1):1–10. [DOI] [PubMed] [Google Scholar]
- 21.Kc DS. Does Multitasking Improve Performance? Evidence from the Emergency Department. Manufacturing & Service Operations Management. 2014;16(2):168–183. [Google Scholar]
- 22.Kc DS, Terwiesch C. Impact of workload on service time and patient safety: An econometric analysis of hospital operations. Management Science. 2009;55(9):1486–1498. [Google Scholar]
- 23.Gorski JK, Batt RJ, Otles E, Shah MN, Hamedani AG, Patterson BW. The Impact of Emergency Department Census on the Decision to Admit. Acad Emerg Med. 2017;24(1):13–21. [DOI] [PubMed] [Google Scholar]
- 24.Harrell FE. Regression modeling strategies : with applications to linear models, logistic regression, and survival analysis. New York: Springer; 2001. [Google Scholar]
- 25.Normand SLT, Glickman ME, Gatsonis CA. Statistical methods for profiling providers of medical care: Issues and applications. Journal of the American Statistical Association. 1997;92(439):803–814. [Google Scholar]
- 26.Tom A, Bosker TASRJ, Bosker RJ. Multilevel analysis: an introduction to basic and advanced multilevel modeling. Sage; 1999. [Google Scholar]
- 27.Elder JW, DePalma G, Pines JM. Optimal Implementation of Prescription Drug Monitoring Programs in the Emergency Department. West J Emerg Med. 2018; 19(2):387–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wright AP, Becker WC, Schiff GD. Strategies for Flipping the Script on Opioid Overprescribing. JAMA Intern Med. 2016;176(1):7–8. [DOI] [PubMed] [Google Scholar]
- 29.Connecting Prescribers and Dispensers to PDMPs through Health IT: Six Pilot Studies and Their Impact 2012. https://www.healthit.gov/sites/default/files/pdmp_pilot_studies_summary_2.pdf. Accessed January 10, 2016.
- 30.Galvan A, Rahdar A. The neurobiological effects of stress on adolescent decision making. Neuroscience. 2013;249:223–231. [DOI] [PubMed] [Google Scholar]
- 31.Hwang U, Richardson LD, Sonuyi TO, Morrison RS. The effect of emergency department crowding on the management of pain in older adults with hip fracture. J Am Geriatr Soc. 2006;54(2):270–275. [DOI] [PubMed] [Google Scholar]
- 32.Pines JM, Hollander JE. Emergency department crowding is associated with poor care for patients with severe pain. Annals of Emergency Medicine. 2008;51(1):1–5. [DOI] [PubMed] [Google Scholar]
- 33.Cantrill SV, Brown MD, Carlisle RJ, et al. Clinical policy: critical issues in the prescribing of opioids for adult patients in the emergency department. Ann Emerg Med. 2012;60(4):499–525. [DOI] [PubMed] [Google Scholar]
- 34.Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2016. MMWR Recomm Rep. 2016;65(1):1–49. [DOI] [PubMed] [Google Scholar]
- 35.Dowell D, Zhang K, Noonan RK, Hockenberry JM. Mandatory Provider Review And Pain Clinic Laws Reduce The Amounts Of Opioids Prescribed And Overdose Death Rates. Health Aff (Millwood). 2016;35(10):1876–1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Garcia MC, Dodek AB, Kowalski T, et al. Declines in Opioid Prescribing After a Private Insurer Policy Change - Massachusetts, 2011–2015. MMWR Morb Mortal Wkly Rep. 2016;65(41):1125–1131. [DOI] [PubMed] [Google Scholar]
- 37.Sun BC, Charlesworth CJ, Lupulescu-Mann N, et al. Effect of Automated Prescription Drug Monitoring Program Queries on Emergency Department Opioid Prescribing. Ann Emerg Med. 2018;71(3):337–347 e336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hoffman J An ER kicks the habit of opioids for pain. New York Times June. 2016;10. [Google Scholar]
- 39.Burton JH, Hoppe JA, Echternach JM, Rodgers JM, Donato M. Quality Improvement Initiative to Decrease Variability of Emergency Physician Opioid Analgesic Prescribing. West J Emerg Med. 2016;17(3):258–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hoppe JA, McStay C, Sun BC, Capp R. Emergency Department Attending Physician Variation in Opioid Prescribing in Low Acuity Back Pain. West J Emerg Med. 2017;18(6):1135–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]