A 52 year-old man presented with a 10-year history of scaly lesions on the elbows. He denied prior evaluation or treatment of these areas. A thorough review of systems was negative. Physical examination found sharply marginated, pinkish-brown, verrucous plaques on the bilateral extensor elbows (Fig 1). The remainder of the cutaneous examination findings were within normal limits. A punch biopsy from the edge of the right elbow plaque was obtained (Figs 2 and 3). Gomori methenamine silver and Ziehl-Neelsen stains for micro-organisms were negative. Tissue culture yielded no growth. Laboratory evaluation was notable for negative quantiFERON gold assay.
Fig 1.

Fig 2.
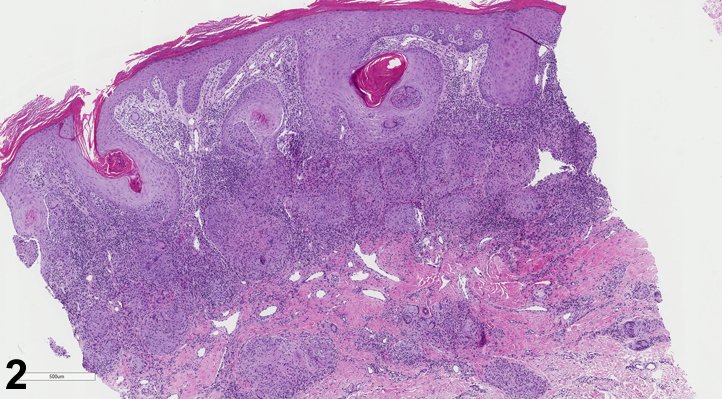
Fig 3.

Question 1: What is the diagnosis?
-
A.
Chronic cutaneous lupus erythematosus
-
B.
Hypertrophic lichen planus
-
C.
Cutaneous sarcoidosis
-
D.
Tuberculosis verrucosa cutis
-
E.
Psoriasis
Answers:
-
A.
Chronic cutaneous lupus erythematosus – Incorrect. This diagnosis would show a vacuolar interface dermatitis with follicular plugging and periadnexal lymphocytic inflammation. A granulomatous infiltrate would not be seen.
-
B.
Hypertrophic lichen planus – Incorrect. Although pseudoepitheliomatous hyperplasia (PEH) may be seen in this diagnosis, a dense lichenoid infiltrate with hypergranulosis would be expected. Hypertrophic lichen planus most commonly occurs on the shins.
-
C.
Cutaneous sarcoidosis – Correct. This patient's clinical presentation and histopathology findings are consistent with psoriasiform sarcoidosis. Sarcoidal lesions may clinically mimic those of psoriasis in approximately 1% of cases as a result of their shared helper T cell 1 immune response, which is postulated to induce epidermal hyperplasia.1, 2 In this psoriasiform variant, histopathology shows PEH with well-defined noncaseating granulomas abutting the epidermis and within the mid dermis. Similar to other clinical forms of sarcoid, the noncaseating granulomas may be cuffed by a lymphocytic inflammatory infiltrate in up to 29% of cases, giving a more tuberculoid appearance.3, 4 It is unknown what mechanism underlies the occasional lymphocytic cuffing of noncaseating granulomas in sarcoidosis or if this finding occurs more commonly in the psoriasiform variant. Exclusion of an infectious etiology with special stains and tissue culture for microorganisms is mandatory. In cases in which there is suspicion for mycobacterial infection, and stains for micro-organisms are negative, polymerase chain reaction should be performed given its higher sensitivity.5
-
D.
Tuberculosis verrucosa cutis – Incorrect. This entity occurs as a result of exogenous re-infection with Mycobacterium tuberculosis in sensitized individuals. Although histopathology typically shows PEH and dermal granulomatous inflammation, the patient's negative quantiFERON assay negates this diagnosis.
-
E.
Psoriasis – Incorrect. Although this diagnosis should be considered given the clinical presentation of psoriasiform plaques on the bilateral elbows, it is inconsistent with the histopathology in this case.
Question 2: What is the most appropriate next step in evaluation?
-
A.
Antinuclear antibody (ANA) screening
-
B.
Hepatitis C virus antibody screening
-
C.
Chest radiograph
-
D.
HIV antibody screening
-
E.
No further evaluation necessary
Answers:
-
A.
ANA screening – Incorrect. ANA testing is indicated in the evaluation of autoimmune connective tissue diseases. Although ANA may be elevated in a minority of cases of sarcoidosis, it generally has little diagnostic or prognostic utility for this condition.
-
B.
Hepatitis C virus antibody screening – Incorrect. Patients with viral hepatitis C infection may develop drug-induced cutaneous sarcoidosis as a result of interferon-α therapy. However, hepatitis C virus itself has not been directly implicated in the pathogenesis of sarcoidosis and testing is therefore not indicated in this case.
-
C.
Chest radiograph – Correct. Pulmonary involvement occurs in approximately 90% of cases of sarcoidosis, with chest radiograph classically showing bilateral hilar lymphadenopathy with or without infiltration.6 Bilateral hilar lymphadenopathy without infiltration was revealed on chest radiograph in the presented case.
-
D.
HIV antibody screening – Incorrect. An association between HIV infection and sarcoidosis has not been established, and antibody testing is therefore unnecessary.
-
E.
No further evaluation necessary – Incorrect. Sarcoidosis is a systemic granulomatous disease that may affect multiple organs. After biopsy of an affected organ, clinical evaluation with chest radiograph, pulmonary function tests, electrocardiography, ophthalmology examination, complete blood count, and serum creatinine is recommended.6
Question 3: Which of the following agents would be least effective in the treatment of this patient?
-
A.
Belimumab
-
B.
Adalimumab
-
C.
Hydroxychloroquine
-
D.
Doxycycline
-
E.
Mycophenolate mofetil
Answers:
-
A.
Belimumab – Correct. Belimumab is a fully humanized monoclonal antibody directed against soluble B lymphocyte stimulator. It is used in the treatment of systemic lupus erythematosus, not sarcoidosis.
-
B.
Adalimumab – Incorrect. Sarcoidosis is primarily driven by a helper T cell 1 cytokine profile. Therefore, it may be effectively treated with tumor necrosis factor-α inhibitors such as adalimumab.
-
C.
Hydroxychloroquine – Incorrect. Hydroxychloroquine has been found to disrupt the release of several cytokines within sarcoidal lesions and impair antigen presentation to CD4+ helper T cells.7 Because antimalarials may take several months to reach maximal efficacy, corticosteroids are often co-administered during the initial treatment phase.
-
D.
Doxycycline – Incorrect. Tetracycline, minocycline, and doxycycline may effectively treat several granulomatous dermatoses including granuloma annulare, granulomatous cheilitis, and cutaneous sarcoidosis.8 The proposed mechanism of action is prevention of granuloma formation through inhibition of protein kinase C.
-
E.
Mycophenolate mofetil – Incorrect. Mycophenolate mofetil prevents T-cell and B-cell proliferation by reversible inhibition of inosine monophosphate dehydrogenase. It is effective in managing cutaneous sarcoidosis and neurosarcoidosis.7
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Vega M.L., Abrahams J., Keller M. Psoriasiform sarcoid: collision of two entitites or expression of one common pathogenesis? J Clin Aesthet Dermatol. 2016;9(4):55–57. [PMC free article] [PubMed] [Google Scholar]
- 2.Okamoto H. Epidermal changes in cutaneous lesions of sarcoid. Am J Dermatopathol. 1999;21(3):229–233. doi: 10.1097/00000372-199906000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Ball N.J., Kho G.T., Martinka M. The histologic spectrum of cutaneous sarcoidosis: a study of 28 cases. J Cutan Pathol. 2004;31:160–168. doi: 10.1111/j.0303-6987.2004.00157.x. [DOI] [PubMed] [Google Scholar]
- 4.Miida H., Ito M. Tuberculoid granulomas in cutaneous sarcoidosis: a study of 49 cases. J Cutan Pathol. 2010;37(4):504–506. doi: 10.1111/j.1600-0560.2009.01337.x. [DOI] [PubMed] [Google Scholar]
- 5.Reja A.H., Biswas N., Biswas S. Fite-Faraco staining in combination with multiplex polymerase chain reaction: a new approach to leprosy diagnosis. Indian J Dermatol Venereol Leprol. 2013;79(5):693–700. doi: 10.4103/0378-6323.116740. [DOI] [PubMed] [Google Scholar]
- 6.Iannuzzi M.C., Rybicki B.A., Teirstein A.S. Sarcoidosis. New Engl J Med. 2007;357:2153–2165. doi: 10.1056/NEJMra071714. [DOI] [PubMed] [Google Scholar]
- 7.Beegle S.H., Barba K., Gobunsuyn R., Judson M.A. Current and emerging pharmacological treatments for sarcoidosis: a review. Drug Des Devel Ther. 2013;7:325–338. doi: 10.2147/DDDT.S31064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sapadin A.N., Fleischmajer R. Tetracyclines: Nonantibiotic properties and their clinical implications. J Am Acad Dermatol. 2006;54(2):258–265. doi: 10.1016/j.jaad.2005.10.004. [DOI] [PubMed] [Google Scholar]


