Dear Editor
Diabetes is a chronic metabolic disease that has become a major epidemic worldwide.1 High blood glucose is thought to be the primary cause of most devastating long-term complications of diabetes.2 In addition to strict glycemic control, a number of therapeutics have been used to slow down the progression of diabetic complications.3 However, a majority of current therapies for most diabetic complications have shown disappointing results in clinical trials. Because these complications arise from a number of pathological processes, targets for early interventions that could lead to effective treatments are largely unknown. Clarification of existing pathways and elucidation of new mechanisms, especially those involved in the early stages of diabetic complications, are sorely needed to design preventative treatments. Interestingly, diabetic complications and ciliopathies share a number of symptoms, such as retinal degeneration and respiratory dysfunction.3 Therefore, we hypothesized that ciliary defects may underlie a subset of diabetic complications.
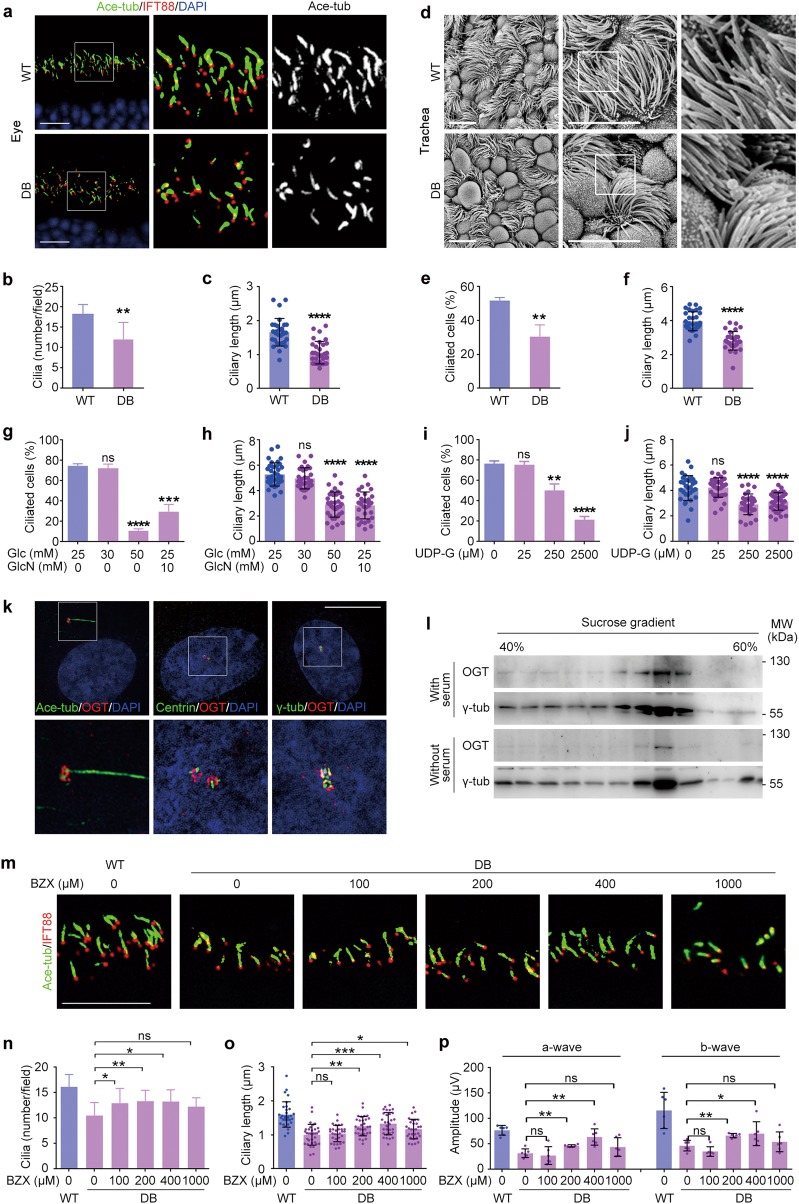
To test this hypothesis, we first examined the morphology of cilia in mice harboring spontaneous diabetic mutation in the leptin receptor gene (referred to as DB mice). The blood glucose level was significantly increased in DB mice (Supplementary information, Fig. S1a). Immunostaining revealed apparent ciliary defects in DB mice; for example, compared to wild-type (WT) mouse eyes, cilia were fewer and shorter in DB mouse eyes (Fig. 1a–c), with retinal dysfunction as detected by electroretinography (Supplementary information, Fig. S1b-d). We also found fewer and shorter cilia in DB mouse trachea and skin, but not in the testis (Supplementary information, Fig. S1e-j). Scanning electron microscopy of the trachea confirmed the loss of ciliated cells and the decrease in ciliary length (Fig. 1d–f). In addition, substantially more mucus was present on the surface of DB mouse trachea, suggesting the impairment of ciliary functions (Supplementary information, Fig. S1f). Furthermore, we observed ciliary defects both in non-obese diabetic (NOD) mice and in diet/streptozotocin-induced diabetic mice (Supplementary information, Fig. S1k-q). These data, together with the recently reported defects in ependymal cilia of diabetic mice,4 suggest that ciliary defects are more widespread in diabetes than previously appreciated.
Fig. 1.
High glucose causes O-GlcNAcylation-dependent ciliary defects. a–c WT and DB mouse eyes were subjected to immunofluorescence microscopy (a), and ciliary density (b, n = 10) and length (c, n = 30) were quantified. d–f Tracheal epithelial tissues from WT and DB mice were subjected to scanning electron microscopy (d), and the percentage of ciliated cells (e, n = 100) and ciliary length (f, n = 30) were quantified. g–j RPE-1 cells cultured in media containing the indicated concentrations of glucose (Glc) and/or glucosamine (GlcN) (g, h) or UDP-GlcNAc (UDP-G) (i, j) were serum-starved for 48 h. The percentage of ciliated cells (g and i, n = 100) and ciliary length (h and j, n = 30) were quantified. k RPE-1 cells were subjected to immunofluorescence microscopy. l RPE-1 cells were cultured in media with or without serum for 24 h, and lysates were fractionated on sucrose gradients and subjected to immunoblotting. m–o Eyes from WT or DB mice treated with the indicated concentrations of BZX for 15 days were subjected to immunofluorescence microscopy (m), and ciliary density (n, n = 10) and length (o, n = 30) were quantified. p Eyes from WT or DB mice treated with BZX for 15 days were examined with electroretinography, and the amplitudes of a-wave and b-wave were obtained. Scale bars, 10 μm. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001 Student’s t-test; ns, not significant. Error bars indicate SEM
We next explored whether glucose concentrations affect ciliogenesis. Human retinal pigment epithelial (RPE-1) cells were cultured without serum to induce primary cilia in the presence of different glucose concentrations. A high level of glucose (50 mM) significantly reduced the percentage of ciliated cells from ~75% to < 20%, and ciliary length was also significantly decreased (Fig. 1g, h and Supplementary information, Fig. S2a).
Protein O-GlcNAc modification has been shown to serve as a nutrient sensor that is especially sensitive to environmental glucose.5 Consistently, treatment of RPE-1 cells with increasing concentrations of glucose resulted in increased levels of protein O-GlcNAcylation (Supplementary information, Fig. S2b). These changes also occurred in vivo, as levels of O-GlcNAcylation changed dramatically both in diabetic mice (Supplementary information, Fig. S2c, d) and in diabetic patients.6
Glucose can be converted to UDP-GlcNAc, the donor substrate for O-GlcNAcylation. Therefore, we next determined whether UDP-GlcNAc was responsible for the impact of glucose on ciliogenesis. We found that addition of glucosamine, a precursor of UDP-GlcNAc, into the culture medium of RPE-1 cells significantly increased the levels of O-GlcNAcylation and impaired ciliogenesis (Fig. 1g, h and Supplementary information, Fig. S2a, b). Furthermore, addition of excess UDP-GlcNAc to the culture medium also led to increased O-GlcNAcylation and decreased ciliogenesis (Fig. 1i, j and Supplementary information, Fig. S2e, f). In agreement with previous findings,7 glucose deprivation decreased ciliary length (Supplementary information, Fig. S2g, h). Strikingly, glucose deprivation-induced ciliary defect was almost completely rescued by addition of appropriate levels of UDP-GlcNAc (Supplementary information, Fig. S2g, h). These results suggest that exquisite regulation of O-GlcNAcylation is critical for ciliary formation.
We further investigated the role of O-GlcNAcylation in ciliogenesis by manipulating the levels or activities of O-GlcNAcase (OGA) and O-GlcNAc transferase (OGT) in RPE-1 cells. We found that siRNA-mediated knockdown of OGA expression or inhibition of OGA activity with ThiametG (TMG) resulted in fewer and shorter cilia (Supplementary information, Fig. S3a-h), suggesting that increasing O-GlcNAcylation could impair ciliogenesis. Surprisingly, decreasing O-GlcNAcylation by siRNA-mediated knockdown of OGT expression or inhibition of OGT activity with a chemical compound containing a benzoxazolinone core (BZX), which specifically inhibits OGT activity,8 also inhibited ciliogenesis (Supplementary information, Fig. S3i-p). These data underscore the importance for tight regulation of O-GlcNAcylation in ciliogenesis.
We then assessed the localization of OGT and found that OGT accumulated around the basal body from which cilia protrude (Fig. 1k and Supplementary information, Fig. S4a). In contrast, OGA localized throughout the cytoplasm (Supplementary information, Fig. S4b). OGT co-fractionated with γ-tubulin on the sucrose gradients of lysates from RPE-1 cells cultured with or without serum, providing further support for its localization to the basal body/centrosome (Fig. 1l). Interestingly, upon serum starvation, there was a substantial decrease of OGT in isolated centrosomes (Supplementary information, Fig. S4c). Immunostaining confirmed this change; localization of OGT to the basal body appeared to peak during initiation of ciliogenesis, followed by a gradual decrease (Supplementary information, Fig. S4d, e). These data suggest that OGT may primarily function at early stages of ciliogenesis.
To gain more insights into the ciliary function of OGT, we inhibited its activity at different stages during ciliogenesis. RPE-1 cells were subjected to serum starvation, followed by addition of BZX at predefined intervals (Supplementary information, Fig. S4f). We found that only inhibition of OGT at the very beginning of ciliogenesis (0 h after serum removal, PS0) reduced the percentage of ciliated cells dramatically. However, independent of the time period of OGT inhibition, ciliary length was significantly shorter (Supplementary information, Fig. S4f-h). These results confirm that OGT is needed primarily at the initiation of ciliogenesis. In addition, the data indicate that OGT is also needed for ciliary elongation.
We then sought to investigate whether proper control of O-GlcNAcylation level could rescue ciliary defects caused by high glucose. We found that treatment of RPE-1 cells with proper amount of the OGT inhibitor BZX could decrease O-GlcNAcylation level and rescue ciliary defects caused by high glucose (Supplementary information, Fig. S5a-d). Furthermore, treatment of DB mice with proper amount of BZX could decrease O-GlcNAcylation level and partially rescue ciliary defects and retinal dysfunction in eyes (Fig. 1m–p and Supplementary information, Fig. S5e). Taken together, these data suggest protein O-GlcNAcylation as a potential target for treatment of diabetic complications.
In conclusion, we describe a previously undiscovered mechanism that could explain the overlapping symptoms of diabetic complications and ciliopathies. Our data suggest that there is an optimal zone within which cellular O-GlcNAcylation levels must be maintained for normal ciliary functions and that ciliary defects caused by O-GlcNAcylation dysregulation may contribute to diabetic complications (Supplementary information, Fig. S6). These findings have important implications for the development of novel therapeutic strategies to control the progression of diabetic complications.
Materials and methods are available in Supplementary information, Data S1.
Electronic supplementary material
Supplementary information, Figures S1-S6
Acknowledgements
This work was supported by grants from the National Key R&D Program of China (2017YFA0503500) and the National Natural Science Foundation of China (31730050, 31701169, 31741039, and 31471262).
Author contributions
Yu and Zhou designed the experiments and wrote the manuscript. Yu, Guo, Li, Ran, and Zhao performed the experiments. Li and Liu helped with data analysis. Yan, Yang, and Zhu commented on the manuscript. Zhou supervised the project.
Competing interests
The authors declare no competing interests.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41422-018-0114-7.
References
- 1.Zimmet P, Alberti KG, Magliano DJ, Bennett PH. Nat. Rev. Endocrinol. 2016;12:616–622. doi: 10.1038/nrendo.2016.105. [DOI] [PubMed] [Google Scholar]
- 2.Sheetz MJ, King GL. JAMA. 2002;288:2579–2588. doi: 10.1001/jama.288.20.2579. [DOI] [PubMed] [Google Scholar]
- 3.Forbes JM, Cooper ME. Physiol. Rev. 2013;93:137–188. doi: 10.1152/physrev.00045.2011. [DOI] [PubMed] [Google Scholar]
- 4.Bachor TP, et al. Neurobiol. Dis. 2017;108:13–28. doi: 10.1016/j.nbd.2017.07.010. [DOI] [PubMed] [Google Scholar]
- 5.Hardiville S, Hart GW. Cell Metab. 2014;20:208–213. doi: 10.1016/j.cmet.2014.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Banerjee PS, Ma J, Hart GW. Proc. Natl Acad. Sci. USA. 2015;112:6050–6055. doi: 10.1073/pnas.1424017112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Takahashi, K., Nagai, T., Chiba, S., Nakayama, K. & Mizuno, K. J. Cell Sci. 131, pii: jcs208769 (2018). [DOI] [PubMed]
- 8.Jiang J, Lazarus MB, Pasquina L, Sliz P, Walker S. Nat. Chem. Biol. 2011;8:72–77. doi: 10.1038/nchembio.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information, Figures S1-S6