Abstract
As the incidence of chronic diseases such as diabetes and hypertension increases, complications such as decreased renal function are also increasing in many patients. Nutritional management in hemodialysis patients is a very important factor for prognosis and quality of life. The purpose of this study was to investigate the differences in nutritional status and dietary management according to hemodialysis duration. A total of 145 patients were divided into 4 groups according to hemodialysis duration: less 1 year (D1), 1–5 years (D2), and above 5 years (D3). The rates of protein-energy wasting were 31.1% in D1 group, 49.5% in D2 group, and 47.6% in D3 group. However, there was no significant difference between the 3 groups. Nutrient intake analysis showed that protein, iron, and vitamin C were significantly lower in the D3 group than in the D1 group. Protein intake in all 3 groups was insufficient compared to the recommended dietary amount for dialysis patients. The most difficult aspect in dietary management was cooking with low sodium. In the D3 group, which had the longest duration of dialysis, the practice of diet therapy and self-perceived need for nutrition education was lowest. Observations of nutritional status are necessary to maintain the health status of dialysis patients. In addition, education plans should be prepared to mediate the nutrient intakes and identify the patient's difficulties and provide practical help.
Keywords: Renal dialysis, Nutritional status, Nutrients, Diet therapy
INTRODUCTION
Patients with chronic kidney disease have progressive impairment of renal function and end stage renal disease (ESRD) patients must undergo renal replacement therapy (hemodialysis, peritoneal dialysis, and kidney transplantation). The prevalence of ESRD patients is increasing worldwide; this increases morbidity and mortality, including cardiovascular complications. Approximately 74% of the Korean ESRD patients manage daily life with the support of hemodialysis. Among patients with ESRD, the proportions of patients on dialysis for less than 1 year (D1), 1–5 years (D2), and above 5 years (D3) are 29%, 50%, and 21%, respectively [1,2]. Hemodialysis can remove a majority of waste products in a short time period. However, useful nutrients are also lost from the body with this process; uremia is accompanied by symptoms such as anorexia, nausea, and food absorption disorders [3].
Dietary management is essential for maintaining a dialytic stability stable dialysis. Such patients require sufficient calorie and protein intakes and adequate amounts of salt, sodium, potassium, phosphorus, and water [4]. Implementation of diet therapy improves survival rates in hemodialysis patients and leads to better dialysis adequacy, but can cause psychological stress in patients. In practice, many difficulties are associated with changing individual eating habits, such as the lack of family support, change in taste, and the lack of knowledge [5,6]. Nutritional status is also known to play an important role in long-term survival of hemodialysis patients [7,8].
In patients with end-stage renal disease, protein-energy malnutrition varies from 10% to 70%; in approximately 25% of hemodialysis patients, energy intake is less than 75% of the recommended dietary energy intake [9,10]. Hemodialysis patients are malnourished but are clinically characterized by mild symptoms and good nutritional status; clinical symptoms can only be detected after malnutrition becomes severe in the future [11]. Nutritional status is related to the quality of life of the individual, and therefore, quick and accurate identification of nutritional status in the patients is very important to implement appropriate nutritional management [12]. However, nutritional status of hemodialysis patients has rarely been studied in detail. In the present study, we investigated the nutritional status of hemodialysis patients in Korea. Even Kidney Disease Outcomes Quality Initiative 2008 has guidelines on nutrition counseling for patients who started dialysis but there is no management standard for dialysis duration. The effect of dialysis duration on nutrition status needs to be analyzed.
The purpose of this study was to investigate the differences in nutritional status and nutrient intake according to hemodialysis duration. With this study, we aimed to help improve nutrition education and counseling methods.
MATERIALS AND METHODS
Study subjects
This study was performed in patients on maintenance hemodialysis (3 times per week) who visited the artificial kidney unit of Soonchunhyang University Bucheon Hospital from March 2011 to September 2015. A total of 145 patients who agreed to the purpose and contents of the study were included. Patients were divided into 3 groups according to duration of hemodialysis: D1, 58 patients; D2, 45 patients; and D3, 42 patients. This study was a retrospective study on dietary survey and data did not the case of the mandatory approval period. So, approval of the Institutional Review Board committee in Soonchunhyang University Hospital was exempted.
Study variables
In general, subjects were examined for age, sex, and body mass index (BMI) calculated using anthropometry. Comorbidities were obtained by calculating the Charlson comorbidity index (CCI). The patients' nutritional status was assessed by a clinical dietitian using a subjective global assessment method. Nutritional determinations were divided into weight change, dietary intake change, gastrointestinal symptoms, functional impairment, comorbidities, and fat and muscle wasting part and scored in each part. A nutritional status was classified as well-nourished, moderate to mild protein-energy wasting (PEW) and severe PEW. In order to evaluate nutrient intake, 24-hour recall method was conducted and analyzed using the computer-aided nutritional analysis program (CAN-Pro 4.0; Korean Nutrition Society, Seoul, Korea). Adherence to diet management and education demand related to the patients' usual diet were investigated. The questions were based on previous research articles and were reviewed by the researchers [13,14]. The questions were: ‘Have you ever received nutritional education or counseling?’, ‘Do you think that diet could play a role in maintaining stable dialysis?,’ ‘Are you controlling your diet now?,’ ‘Why do you control your diet?,’ ‘What is most difficult in diet management?,’ and ‘Do you want nutritional education and professional nutrition management?’
Statistics analysis
SPSS 18.0 programs (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis to identify differences among the 3 groups, means and standard deviations were analyzed by 1-way analysis of variance and frequency was analyzed by χ2 test. All results were considered statistically significant at p < 0.05.
RESULTS
Baseline characteristics
Mean age of the subjects was 62.5 years. Distribution of BMI was significantly difference between groups.. Mean CCI was significantly higher in group D3 than in group D1. Nutritional deficiencies were detected in 31.1% of the patients in group D1, 48.9% of the patients in group D2, and 47.6% of the patients in group D3. The D3 group showed high rates of severe malnutrition, but these rates were not significantly different among the 3 groups (Table 1).
Table 1. Subjects' characteristics according to hemodialysis duration.
| Characteristics | D1 (n = 58) | D2 (n = 45) | D3 (n = 42) | p value | |
|---|---|---|---|---|---|
| Age, yr | 61.5 ± 11.9 | 62.1 ± 10.7 | 63.0 ± 9.4 | 0.780 | |
| Sex | 0.664 | ||||
| Male | 26 (42.1) | 22 (48.0) | 20 (45.5) | ||
| Female | 32 (57.9) | 23 (52.0) | 22 (54.5) | ||
| BMI | 0.003 | ||||
| < 18.5 | 3 (5.2) | 8 (17.8) | 12 (28.6) | ||
| 18.5–22.9 | 34 (58.6) | 21 (46.7) | 24 (57.1) | ||
| > 22.9 | 21 (36.2) | 16 (35.6) | 6 (14.3) | ||
| eGFR, mL/min/1.73 m2 | 18.4 ± 10.2 | 16.1 ± 8.3 | 15.8 ± 9.6 | 0.328 | |
| CCI | 3.4 ± 1.4 | 4.1 ± 1.7 | 4.6 ± 2.2 | 0.002* | |
| SGA | 0.107 | ||||
| Severe PEW | 4 (6.9) | 5 (11.1) | 6 (14.3) | ||
| Moderate to mild PEW | 14 (24.2) | 17 (37.8) | 14 (33.3) | ||
| Well-nourished | 40 (68.9) | 23 (51.1) | 22 (52.4) | ||
Data represented as mean ± standard deviation and number (%).
The p value by ANOVA test (continuous variables) or χ2 test (categorical variables).
D1, less 1 year; D2, 1–5 years; D3, above 5 years; BMI, body mass index; eGFR, estimated glomerular filtration rate; CCI, Charlson comorbidity index; SGA, subjective global assessment; PEW, protein-energy wasting; ANOVA, analysis of variance.
*There exists the significant difference between D1 and D3 groups.
Analysis of nutritional status
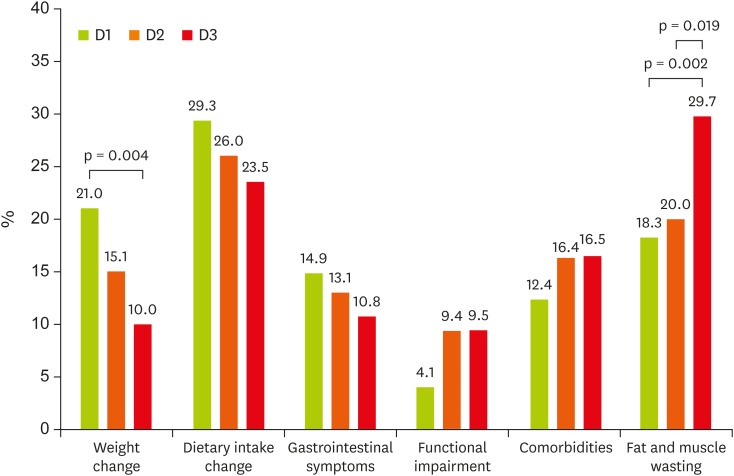
Factors associated with malnutrition were compared among the 3 groups and the overall score was calculated as a percentage of the nutritional assessment sub-section. The association between nutritional status and weight change, dietary intake change, and gastrointestinal symptoms were higher in the D1 group. In the D3 group, nutritional status was more strongly associated with functional impairment, comorbidities, and fat and muscle wasting. There were significant differences in weight change and fat and muscle wasting among groups (Figure 1).
Figure 1. Distribution of SGA components according to hemodialysis duration. The p value by χ2 test (categorical variables).
SGA, subjective global assessment; D1, less 1 year; D2, 1–5 years; D3, above 5 years.
Comparison of nutrient intakes
Table 2 shows the comparison of nutrient intakes among the 3 groups. Protein, iron, sodium, and vitamin C intakes were significantly different among the 3 groups. Protein, iron, and vitamin C intakes were significantly lower in the D3 group than in the D1 group. Sodium intake was significantly higher in the D3 group than in the D2 group. The energy intakes per body weight were 30.8 kcal in the D1 group, 29.2 kcal in the D2 group, and 27.4 kcal in the D3 group. Protein intake was the lowest in the D3 group (0.89 kcal) while protein intakes of D1 and D2 were 1.01 kcal and 1.09 kcal, respectively (Table 2).
Table 2. Nutrient intakes according to hemodialysis duration.
| Characteristics | D1 (n = 58) | D2 (n = 45) | D3 (n = 42) | p value |
|---|---|---|---|---|
| Energy, kcal | 1,717.4 ± 408.4 (30.8 kcal/BW) | 1,683.5 ± 384.7 (29.2 kcal/BW) | 1,594.8 ± 439.3 (27.4 kcal/BW) | 0.126 |
| Protein, g | 63.4 ± 17.5 (1.09 g/BW) | 58.7 ± 21.1 (1.01 g/BW) | 51.7 ± 18.0 (0.89 g/BW) | 0.023* |
| Fat, g | 50.9 ± 18.6 | 48.1 ± 14.7 | 49.7 ± 24.4 | 0.407 |
| Carbohydrate, g | 239.5 ± 49.2 | 241.9 ± 50.2 | 223.0 ± 43.8 | 0.218 |
| Fiber, g | 11.1 ± 7.5 | 12.7 ± 6.1 | 10.1 ± 8.7 | 0.361 |
| Calcium, mg | 426.3 ± 225.0 | 402.8 ± 252.4 | 353.5 ± 104.9 | 0.148 |
| Phosphorous, mg | 1,033.9 ± 324.3 | 985.7 ± 306.9 | 1,138.9 ± 351.3 | 0.706 |
| Iron, mg | 11.4 ± 4.9 | 10.9 ± 5.7 | 9.1 ± 3.5 | 0.004* |
| Sodium, mg | 4,145.6 ± 1,257.3 | 3,506.5 ± 1,750.5 | 4,695.9 ± 1,256.4 | 0.044† |
| Potassium, mg | 2,784.5 ± 506.9 | 2,511.0 ± 854.8 | 2,340.9 ± 435.7 | 0.530 |
| Zinc, mg | 8.9 ± 6.8 | 9.6 ± 6.9 | 8.8 ± 7.0 | 0.428 |
| Vitamin A, µg RE | 617.9 ± 403.1 | 614.6 ± 361.0 | 537.6 ± 310.3 | 0.067 |
| Vitamin B1, mg | 1.03 ± 0.25 | 1.02 ± 0.14 | 1.02 ± 0.04 | 0.512 |
| Vitamin B2, mg | 1.02 ± 0.40 | 0.98 ± 0.44 | 1.03 ± 0.35 | 0.426 |
| Vitamin B6, mg | 1.57 ± 0.90 | 1.44 ± 0.85 | 1.36 ± 0.97 | 0.259 |
| Niacin, mg NE | 13.6 ± 6.1 | 12.54 ± 6.6 | 12.70 ± 5.8 | 0.371 |
| Vitamin C, mg | 94.7 ± 55.0 | 83.8 ± 46.7 | 75.9 ± 35.8 | 0.015* |
| Folic acid, mg | 253.3 ± 101.5 | 296.5 ± 85.3 | 224.1 ± 70.2 | 0.129 |
| Vitamin E, mg | 12.9 ± 4.0 | 11.0 ± 3.5 | 11.6 ± 3.2 | 0.366 |
| Cholesterol, mg | 280.7 ± 157.3 | 301.3 ± 125.4 | 266.6 ± 131.5 | 0.248 |
Data represented as mean ± standard deviation and number (%). The p value by ANOVA test (continuous variables) or χ2 test (categorical variables).
D1, less 1 year; D2, 1–5 years; D3, above 5 years; BW, body weight; RE, retinol equivalent; NE, niacin equivalent; ANOVA, analysis of variance.
*There exists a significant difference between groups D1 and D3; †There exists a significant difference between groups D2 and D3.
Difficulty in the dietary management
Table 3 shows the results of the subjects' normal dietary adjustment. More than 70% of subjects previously received nutrition education. The D3 group showed a significantly lower agreement to the role of diet in maintaining stable dialysis and lower rate of patients currently controlling their current diet compared to the other 2 groups. Regarding the question about the reason for controlled eating, the D1 and D2 groups showed the highest response rates for electrolyte control whereas the D3 group showed the highest response rate for blood glucose control; there were significant differences among the 3 groups. The most difficult dietary factor to control was restricting salt while cooking. The second most difficult factor for the D1 group was that everything had to be controlled, the D2 group found restricting foods high in potassium was difficult, and the D3 group perceived food preparation and the economic difficulties hindered diet management. The D3 group ranked the lowest in terms of demands for continuous nutrition education and management, but the differences were not significant (Table 3).
Table 3. Adherence of diet management and education demand according to hemodialysis duration.
| Question | D1 (n = 58) | D2 (n = 45) | D3 (n = 42) | p value | |
|---|---|---|---|---|---|
| 1) Do you received nutritional education and counseling? | 42 (72.4) | 32 (71.1) | 32 (76.1) | 0.624 | |
| 2) Do you think that diet could play a role in maintaining stable dialysis? | 52 (89.7) | 36 (80.0) | 25 (59.5) | 0.004 | |
| 3) Are you controlling your diet now? | 41 (70.7) | 22 (48.9) | 18 (42.9) | 0.018 | |
| 4) Why do you control your diet? | 0.030 | ||||
| For electrolyte control | 33 (43.4) | 20 (44.4) | 10 (33.3) | ||
| For blood pressure control | 17 (22.4) | 12 (26.8) | 5 (16.7) | ||
| For blood glucose control | 19 (25.0) | 11 (24.4) | 12 (40.0) | ||
| For anemia prevention | 4 (5.3) | 2 (4.4) | 2 (6.7) | ||
| Etc. | 3 (3.9) | 0 (0.0) | 1 (3.3) | ||
| 5) What is the most difficult to control in diet management? | 0.257 | ||||
| Cooking with low salt | 23 (25.8) | 26 (28.0) | 19 (24.1) | ||
| Restriction of high potassium food | 5 (5.6) | 16 (17.2) | 6 (7.6) | ||
| Restriction of high phosphorus food | 7 (7.9) | 8 (8.6) | 5 (6.3) | ||
| High quality protein consumption | 15 (16.9) | 8 (8.6) | 7 (8.9) | ||
| Restriction of water | 10 (11.2) | 7 (7.5) | 5 (6.3) | ||
| Cooking food by myself | 9 (10.1) | 12 (12.8) | 13 (16.5) | ||
| Economic problem | 4 (4.5) | 6 (6.5) | 13 (16.5) | ||
| Everything should be controlled | 16 (18.0) | 10 (10.8) | 11 (13.8) | ||
| 6) Do you want nutritional education or professional management? | 25 (43.1) | 19 (42.2) | 14 (33.3) | 0.189 | |
The results of 1), 2), and 3) number in the 3 groups are the percentages that answered “yes” to the question. Data are presented as number (%). The p value by χ2 test (categorical variables).
D1, less 1 year; D2, 1–5 years; D3, above 5 years.
DISCUSSION
The purpose of this study was to investigate dietary intakes and compliance with dietary management during dialysis to improve dietary management in hemodialysis patients. All study subjects had normal BMI. But underweight ratio in the D3 group was higher than that in other 2 groups. Malnutrition rate was not significantly different, but we found that malnutrition rates increased with increasing hemodialysis duration. This result was higher than the rate reported by Kwon et al. [15].
On analyzing factors associated with malnutrition, we found that changes in weight and dietary intakes were common in the D1 and D2 groups, but fat and muscle metabolism was common in the D3 group. There was no statistical significance but it is expected that there was a difference in the number of subjects, so continuous analysis is needed. It has been reported that worsening nutritional status is associated with a longer dialysis period, and the resulting malnutrition directly affects prognoses of dialysis patients, increases dialysis-associated prevalence and mortality rates, and lowers the quality of the life [16]. Therefore, the nutritional status of hemodialysis patients should be observed closely on a periodic basis. Prognostic factors for mortality in dialysis patients include nutritional status, age, adequacy of dialysis, and presence of co-morbidities; many dialysis patients also have chronic diseases such as hypertension or diabetes. The CCI is scored according to the age and the presence of accompanying diseases, such as cardiovascular, cerebrovascular, lung, and gastrointestinal diseases and diabetes mellitus [17]. In this study, comorbid diseases were more common in the D3 group than in the other 2 groups; therefore, prolonged hemodialysis required more medical treatment.
We analyzed nutrient intake status of the subjects. The energy requirement in dialysis patients is 30–35 kcal per ideal body weight, and protein requirement is 1.2 g per ideal body weight [18]. In all 3 groups, calorie and protein intakes were insufficient compared to the dietary intakes recommended for dialysis patients. Protein, iron, and vitamin C intakes were significantly lower in the D3 group than in the other 2 groups. In addition, calcium, vitamin A, vitamin B1, vitamin B6, niacin, vitamin C, and folic acid were consumed inadequately compared with the intake levels recommended by the dietary guidelines for Korean [19].
In all 3 groups, the rate of nutrition education was higher than 70%; however, the current dietary control rates decreased significantly with increasing dialysis duration. In addition, at the beginning of dialysis, patients complained of the difficulty in controlling low-salt diets or of the burden of eating control itself; however, the rates of oneself cooking and economic difficulties increased with increasing dialysis duration. At the beginning of dialysis, the emphasis is on salt and electrolyte control, and after 5 years, the diet control is loosened and the salt intake is increased. The intake of sodium in this study was higher than that reported by Kim et al. [5]. There were not many papers related to this study and it was difficult to compare the results.
The major causes of malnutrition in dialysis patients are low frequency of intake of 3 meals, inadequate nutrient intake, changes in taste, and limitations with respect to consuming many food items. Such prolonged treatment is known to cause burdens and psychological problems [20].
This study has limitations. Our findings did not reflect dietary adjustments according to accompanying complications, or dialysis adequacy. However, this study was performed on patients who were treated for various time periods; thus, it was meaningful to examine the causes for impaired nutritional status considering various aspects of dialysis treatment. Our results suggest that management methods for hemodialysis patients should be chosen according to hemodialysis duration and level of nutrition education, even though proper nutrition intervention is necessary during the treatment.
CONCLUSION
In patients with hemodialysis, nutrient intake and compliance with meal control decreases with increasing dialysis duration. Therefore, continuous malnutrition screening of long-term care patients is necessary in addition to appropriate nutritional intervention.
Footnotes
Conflict of Interest: The authors declare that they have no competing interests.
References
- 1.Jin DC. Current status of dialysis therapy for ESRD patients in Korea. J Korean Med Assoc. 2013;56:562–568. [Google Scholar]
- 2.ESRD Registry Committee, The Korean Society of Nephrology. Current renal replacement therapy in Korea - Insan Memorial Dialysis Registry, 2017 [Internet] 2018. [cited 2018 October 19]. Available from http://www.ksn.or.kr/rang_board/list.html?code=sinchart_eng.
- 3.Ju A, Unruh ML, Davison SN, Dapueto J, Dew MA, Fluck R, Germain M, Jassal SV, Obrador G, O'Donoghue D, Tugwell P, Craig JC, Ralph AF, Howell M, Tong A. Patient-reported outcome measures for fatigue in patients on hemodialysis: a systematic review. Am J Kidney Dis. 2018;71:327–343. doi: 10.1053/j.ajkd.2017.08.019. [DOI] [PubMed] [Google Scholar]
- 4.Cunningham SE, Verkaik D, Gross G, Khazim K, Hirachan P, Agarwal G, Lorenzo C, Matteucci E, Bansal S, Fanti P. Comparison of nutrition profile and diet record between veteran and nonveteran end-stage renal disease patients receiving hemodialysis in veterans affairs and community clinics in metropolitan south-central Texas. Nutr Clin Pract. 2015;30:698–708. doi: 10.1177/0884533615575046. [DOI] [PubMed] [Google Scholar]
- 5.Kim H, Lim H, Choue R. A better diet quality is attributable to adequate energy intake in hemodialysis patients. Clin Nutr Res. 2015;4:46–55. doi: 10.7762/cnr.2015.4.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shapiro BB, Bross R, Morrison G, Kalantar-Zadeh K, Kopple JD. Self-reported interview-assisted diet records underreport energy intake in maintenance hemodialysis patients. J Ren Nutr. 2015;25:357–363. doi: 10.1053/j.jrn.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blumberg Benyamini S, Katzir Z, Biro A, Cernes R, Shalev B, Chaimy T, Barnea Z. Nutrition assessment and risk prediction in dialysis patients-a new integrative score. J Ren Nutr. 2014;24:401–410. doi: 10.1053/j.jrn.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 8.Ikizler TA, Cano NJ, Franch H, Fouque D, Himmelfarb J, Kalantar-Zadeh K, Kuhlmann MK, Stenvinkel P, TerWee P, Teta D, Wang AY, Wanner C International Society of Renal Nutrition and Metabolism. Prevention and treatment of protein energy wasting in chronic kidney disease patients: a consensus statement by the International Society of Renal Nutrition and Metabolism. Kidney Int. 2013;84:1096–1107. doi: 10.1038/ki.2013.147. [DOI] [PubMed] [Google Scholar]
- 9.Nazar CM, Anderson J. Extent of malnutrition in end-stage renal disease patients. J Nephropharmacol. 2014;3:27–28. [PMC free article] [PubMed] [Google Scholar]
- 10.Pupim LB, Cuppari L. Malnutrition in end-stage renal disease: beyond inadequate nutrient intake. Nephrol News Issues. 2003;17:66–71. [PubMed] [Google Scholar]
- 11.Kang SS, Chang JW, Park Y. Nutritional status predicts 10-year mortality in patients with end-stage renal disease on hemodialysis. Nutrients. 2017;9:e399. doi: 10.3390/nu9040399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nitoi LC, Aspazia Stefan A, Ionita C, Andrei C, Vulpoi C. The impact of socioeconomic status and nutritional biochemical markers on quality of life of chronic dialysis patients? Rev Med Chir Soc Med Nat Iasi. 2016;120:812–817. [PubMed] [Google Scholar]
- 13.Pisani A, Riccio E, Bellizzi V, Caputo DL, Mozzillo G, Amato M, Andreucci M, Cianciaruso B, Sabbatini M. 6-Tips diet: a simplified dietary approach in patients with chronic renal disease. A clinical randomized trial. Clin Exp Nephrol. 2016;20:433–442. doi: 10.1007/s10157-015-1172-5. [DOI] [PubMed] [Google Scholar]
- 14.Roach LA, Lambert K, Holt JL, Meyer BJ. Diet quality in patients with end-stage kidney disease undergoing dialysis. J Ren Care. 2017;43:226–234. doi: 10.1111/jorc.12215. [DOI] [PubMed] [Google Scholar]
- 15.Kwon YE, Kee YK, Yoon CY, Han IM, Han SG, Park KS, Lee MJ, Park JT, Han SH, Yoo TH, Kim YL, Kim YS, Yang CW, Kim NH, Kang SW. Change of nutritional status assessed using subjective global assessment is associated with all-cause mortality in incident dialysis patients. Medicine (Baltimore) 2016;95:e2714. doi: 10.1097/MD.0000000000002714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Waal D, Heaslip E, Callas P. Medical nutrition therapy for chronic kidney disease improves biomarkers and slows time to dialysis. J Ren Nutr. 2016;26:1–9. doi: 10.1053/j.jrn.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 17.Liu J, Huang Z, Gilbertson DT, Foley RN, Collins AJ. An improved comorbidity index for outcome analyses among dialysis patients. Kidney Int. 2010;77:141–151. doi: 10.1038/ki.2009.413. [DOI] [PubMed] [Google Scholar]
- 18.Therrien M, Byham-Gray L, Beto J. A review of dietary intake studies in maintenance dialysis patients. J Ren Nutr. 2015;25:329–338. doi: 10.1053/j.jrn.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 19.The Korean Nutrition Society. Dietary reference intakes for Koreans 2015. Sejong: Ministry of Health and Welfare; 2016. [Google Scholar]
- 20.Su CY, Wang T, Lu XH, Ma S, Tang W, Wang PY. Low-dose dialysis combined with low protein intake can maintain nitrogen balance in peritoneal dialysis patients in poor economies. Clin Nephrol. 2017;87:84–92. doi: 10.5414/CN108960. [DOI] [PubMed] [Google Scholar]